Abstract
BACKGROUND
Recent changes to Medicaid policy may have unintended consequences in the education system. This study estimated the potential financial impact of the Deficit Reduction Act (DRA) on school districts by calculating Medicaid-reimbursed behavioral health care expenditures for school-aged children in general and children in special education in particular.
METHODS
Medicaid claims and special education records of youth ages 6 to 18 years in Philadelphia, PA, were merged for calendar year 2002. Behavioral health care volume, type, and expenditures were compared between Medicaid-enrolled children receiving and not receiving special education.
RESULTS
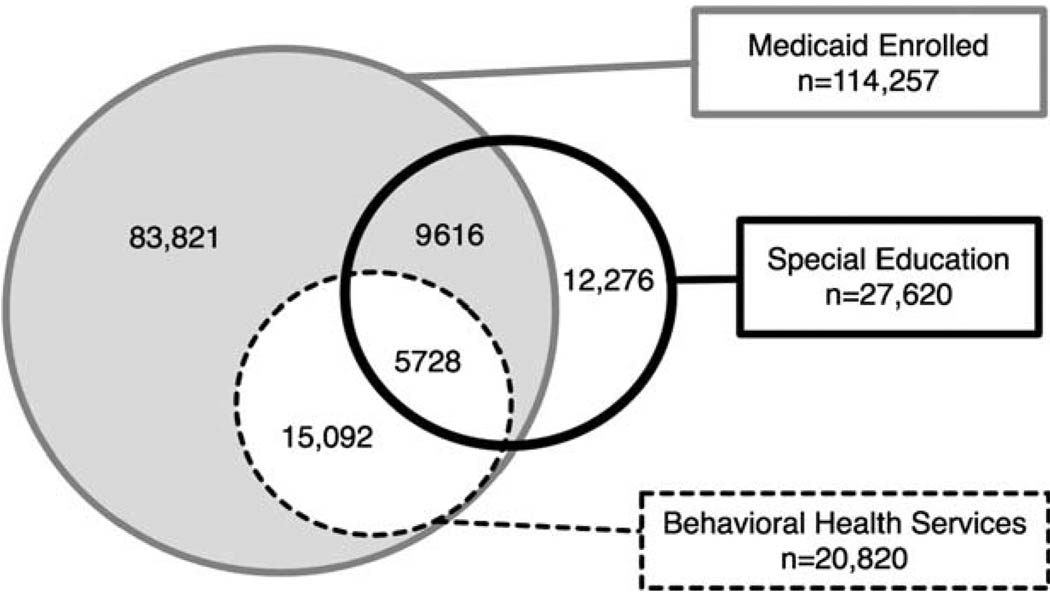
Significant overlap existed among the 126,533 children who were either Medicaid enrolled (114,257) or received special education (27,620). Medicaid-reimbursed behavioral health care was used by 21% of children receiving special education (37% of those Medicaid enrolled) and 15% of other Medicaid-enrolled children. Total expenditures were $197.8 million, 40% of which was spent on the 5728 children in special education and 60% of which was spent on 15,092 other children.
CONCLUSIONS
Medicaid-reimbursed behavioral health services disproportionately support special education students, with expenditures equivalent to 4% of Philadelphia’s $2 billion education budget. The results suggest that special education programs depend on Medicaid-reimbursed services, the financing of which the DRA may jeopardize.
Keywords: Medicaid, special education, mental health, policy, Deficit Reduction Act
Low-income children with psychiatric and developmental disabilities receive assistance through a combination of health care, educational, and social programs, organized at the local, state, and federal level, that together are intended to form a supportive ecology of services. The ability of these public programs to interact with one another in mutually supportive ways represents an important test of their utility; for children with psychiatric and developmental disabilities, health care plays a pivotal role in both reducing symptoms and enabling appropriate academic progress.1–3 In turn, these educational outcomes are associated with many other long-term health outcomes. For example, at least 2 studies have shown that disparities in educational attainment account for between 25% and 60% in differences in mortality and disability from heart disease, cancer, injury, and stroke.4,5
Within this system of supports for children with psychiatric and developmental disabilities, the special education and Medicaid programs predominate. The right to special education services for all children who need them to ensure a “free and appropriate education” resulted from the Education of all Handicapped Children Act of 1975, renamed the Individuals with Disabilities Education Act (IDEA) in 1990. During the 2003–2004 academic year, IDEA special education programs served more than 7 million children, constituting 11% of all children in the public education system.6 Among children in special education, behavioral and emotional health conditions affect 60% to 80% of this population.7,8 The IDEA explicitly bars the use of federal education funds for medical treatment of children in special education programs. Instead, these children rely on public and private insurers to pay for medical care that affects their academic functioning. Yet, private health insurance typically limits coverage of services for chronic behavioral conditions9,10 and may exclude payment altogether if services are deemed “educational,” as occurs when otherwise-covered behavioral health services are furnished as educational accommodations.11
Unlike private health insurance, Medicaid historically has embraced the task of financing health care services for Medicaid-enrolled children in special education and has been specifically structured to be compatible with the mission and operational aspects of the IDEA. Medicaid is a vast program, serving 1 in 4 US children,12 almost all of whom are either in low-income households, are in state custody, or have disabilities, each of which increases the risk for educationally disabling conditions.3,13 In addition to being the largest insurer of American children, Medicaid-covered services are uncharacteristically broad. For example, the Early and Periodic Screening Diagnosis and Treatment (EPSDT) program within Medicaid covers comprehensive developmental, vision, dental, and hearing assessments as well as provision of health care services encompassed within the definition of “medical assistance.” Included within EPSDT are targeted case management services that help Medicaid-enrolled children access and coordinate medical, educational, or social services. In addition to its broad coverage, Medicaid historically has prohibited patient cost sharing in the case of children.12,14
Because of the breadth of Medicaid services and minimal cost sharing requirement, the program is a powerful means of financing therapies for children with psychiatric or developmental disabilities.15,16 Importantly, Medicaid routinely pays for covered services to be delivered in schools. Amendments in 1986 clarified that Medicaid funds be used to pay for medically necessary covered services that are listed in a child’s individualized education plan that outlines required educational supports for children served through IDEA.11,17–19 This mechanism of Medicaid financing of medical services in school settings enables treatment of impairing behavioral and emotional problems to be provided more immediately and accessibly, thereby limiting children’s removal from the classroom and reducing restrictive placements.20,21
The Deficit Reduction Act (DRA) of 2005 (P.L. 109–171) changed federal policy that may affect how Medicaid and IDEA-financed services work in concert in 2 specific ways. First, the DRA permitted states to enroll eligible children in “alternative benefit plans” equivalent to state employee or State Children’s Health Insurance Program plans. For enrolled children, EPSDT wraparound coverage would be available to address service gaps because these plans traditionally have more limited coverage of mental, dental, and vision health care services and services not delivered in office settings; and yet, how the EPSDT requirements would be enforced and what barriers to care would be introduced by states choosing these wraparound plans is unknown. Second, the DRA prohibited states from making medical assistance payments for targeted case management if payments are available “as reimbursement under a medical, social, educational, or other program.”22 These 2 changes cast doubt on whether many Medicaid-reimbursed services will continue to be delivered to special education students, particularly when those services are delivered in schools.
Although many children rely on both Medicaid and special education to improve well-being, the DRA legislation was passed in the absence of information regarding the fiscal relationship between Medicaid and other programs, particularly special education. In particular, there has been to date no systematic governmental or private effort to align the data from the special education and the Medicaid systems and examine the relationship between the 2 programs. We therefore estimated empirically the fiscal overlap between these 2 systems in 1 major city in the United States in order to describe the nature of behavioral health services financed by Medicaid generally and specifically examine their use by children in special education.
METHODS
Protection of Human Subjects
Both the University of Pennsylvania and City of Philadelphia institutional review boards approved this study.
Sample
Special education records from the School District of Philadelphia, Pennsylvania, were merged with Medicaid data for children 6 to 18 years of age for calendar year 2002. The resulting data set included all children, ages 6 to 18 years, who were Medicaid enrolled or receiving special education services for calendar year 2002.
Variables
Receipt of special education services included all children coded by the School District of Philadelphia into 1 of the following 12 categories: autism, hearing and visual impairment, emotionally disturbed, hearing impairment, multiple disabilities, mental retardation, other health impairment, orthopedic impairment, specific learning disability, speech/language impairment, traumatic brain injury, or visual impairment.
- Receipt of behavioral health services included all children with at least 1 Medicaid claim associated with an International Classification of Diseases, 10th Edition code of 290 through 319. Use of behavioral health services was further examined using the following categories:
- Psychotropic medication use included claims for medications in the following therapeutic classes: anticholinergics, anticonvulsants or mood stabilizers, antidepressants, antipsychotics, benzodiazepines, sedatives, or stimulants.
- Behavioral health rehabilitation services (BHRS), sometimes referred to as “wraparound,” included behavioral health services delivered in nontraditional settings such as schools, homes, and the community. As such, these services are particularly important for children with special education needs.
- Case management included claims in which the service type associated with a given claim was for case management.
- Inpatient psychiatric hospitalization included claims in which the provider type was a private psychiatric hospital, public psychiatric hospital, or extended acute psychiatric care facility. The classification also encompassed psychiatric care furnished in a general hospital, with claims data indicating payment for an overnight stay.
- Partial psychiatric hospitalization included claims in which the service furnished was partial hospitalization care.
Behavioral health care expenditures were abstracted from the reimbursed Medicaid claims and comprised the sum of total reimbursed charges. Expenditures were also summed separately for each of the service categories described above.
Demographics, including age, sex, and race/ethnicity, were abstracted from the Medicaid eligibility files and the special education database.
Data Analysis
Data first were analyzed to examine the use of behavioral health services among all Medicaid-enrolled children and then to examine use of these services among Medicaid-enrolled children who also received special education services. First, a Venn diagram of the overlap of Medicaid eligibility, behavioral health service use, and special education service use was created using cross-tabulations. Next, the use of different types of behavioral health services and related expenditures were calculated separately for those receiving and not receiving special education services. Expenditures were further examined by examining the distribution of individual-level expenditures among children receiving and not receiving special education services, and calculating the Gini index for both groups (along with the bootstrapped 95% confidence interval [CI] for the index, implemented with the “ineqerr” command in Stata 9.2). The Gini index is a measure of statistical dispersion that provides a measure of inequality of distribution of economic resources. Values range between 0 and 1. A low Gini coefficient indicates more equal distribution, while a high Gini coefficient indicates more unequal distribution. In the current study, 0 would correspond to all subjects having exactly the same expenditure and 1 would correspond with 1 subject accounting for all expenditures.
Finally, demographic characteristics were described using means and frequencies, as appropriate for those above and below the median expenditure for behavioral health services. Analyses were conducted using SPSS 13 (SPSS Inc., Chicago, Ill) and Stata 9.2 (Stata-Corp, College Station, Tex).
RESULTS
In Philadelphia in calendar year 2002, there was a substantial overlap in the use of Medicaid and special education services among the 126,533 children who were either Medicaid enrolled (114,257) or received special education services (27,620); 13.4% of children enrolled in Medicaid received special education services, while 55.6% of children in special education were Medicaid enrolled (Figure 1).Medicaid-reimbursed behavioral health services were used by a substantial proportion of children in both programs; 18.2% of Medicaid-enrolled children and 20.7% of children receiving special education.
Figure 1.
Overlap of Medicaid-Reimbursed Behavioral Health Care or Special Education Services for Children of Ages 6 to 18 Years in Philadelphia, PA, for Calendar Year 2002 (n = 126,533)
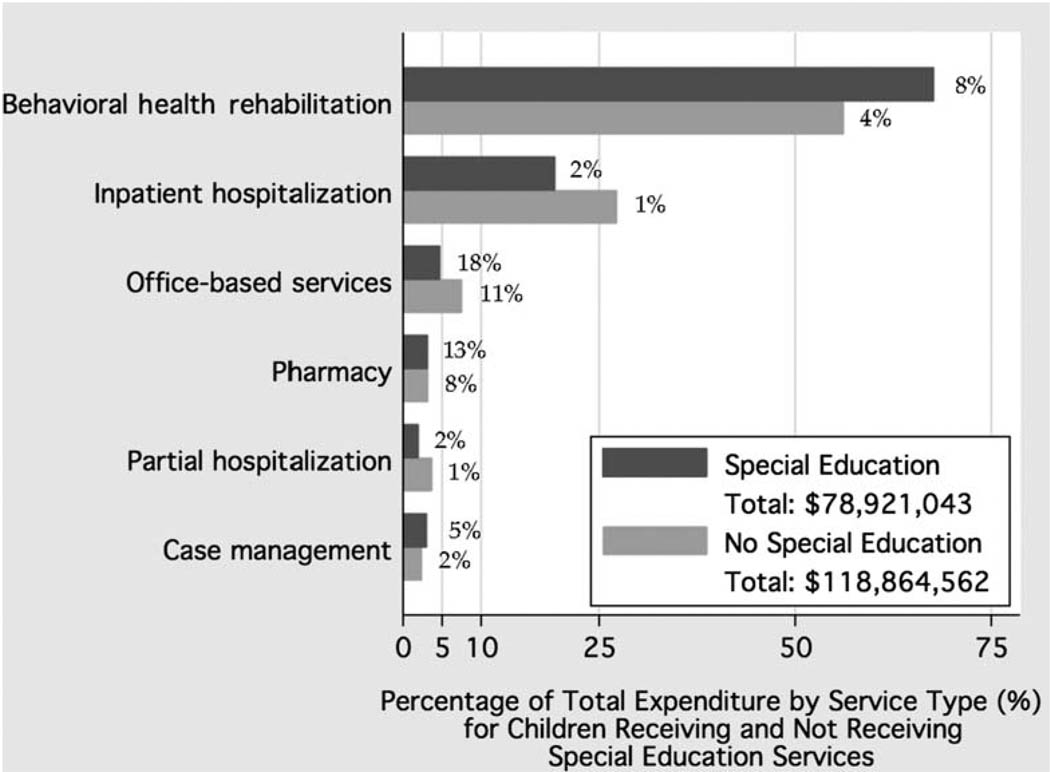
Children receiving special education services were more likely to use the various types of behavioral health services compared to Medicaid-enrolled children who did not receive special education (Figure 2). The most commonly used service in both groups was office-based therapy, followed by psychotropic medications (pharmacy) and BHRS. Although 21% of all children in special education (37% of those who were Medicaid enrolled) used any behavioral health care, compared with 15% of other Medicaid-enrolled children, children in special education were approximately twice as likely as other children to use each type of service.
Figure 2.
Medicaid-Reimbursed Behavioral Health Expenditures for Children Aged 6 to 18 Years in Philadelphia, PA, for Calendar Year 2002*
*Percentages associated with each bar indicate the percentage of children using that type of service. All differences between children in special education and other children signicant at p < .01.
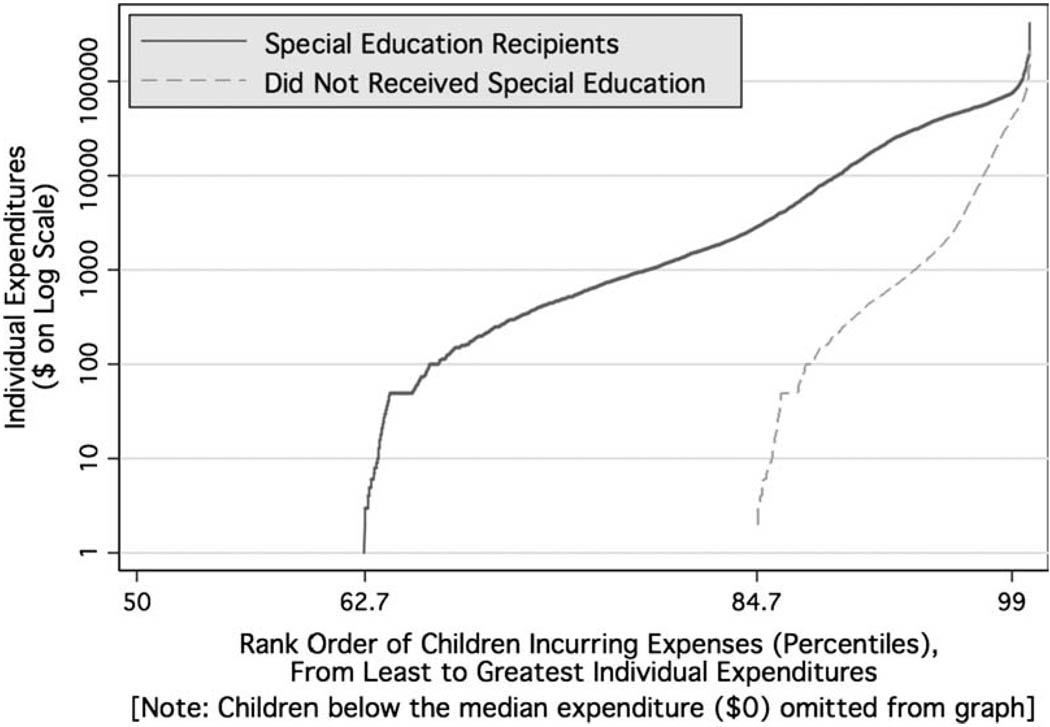
Examining behavioral health care expenditures for particular types of services provides additional perspectives on the overlap of Medicaid and special education (Figure 2). Total behavior health care expenditures for calendar year were $197.8 million, 40% of which was spent on the 5728 children receiving special education services and 60% of which was spent on the 15,092 other Medicaid-enrolled children. Sixty-eight percent of expenditures among children in special education were for BHRS, compared with 56% for other children (p < .001). The second greatest expenditure category in both groups was inpatient hospitalization, followed by office-based therapy. Among Medicaid-enrolled children, behavioral health services were used by a larger portion of children receiving special education (37.3%) and with greater individual expenditures than by other Medicaid-enrolled children (Figure 3); the resulting profile of individual expenditures was more evenly distributed among children receiving special education (Gini index 0.76; 95% CI, 0.75 to 0.77), and concentrated in a smaller group of Medicaid-enrolled children who did not receive special education (Gini index 0.83; 95% CI, 0.82 to 0.83).
Figure 3.
Total Behavioral Health Care Expenditures Plotted Against the Percentage of Children, Ordered by Their Expenditures
Certain demographic characteristics of children who did not use any behavioral health services differed significantly from those who were either low or high utilizers, defined as individuals either below or above the median level of individual expenditure (Table 1); while the age of the children was not associated with use of behavioral health services, high utilizers were more likely to be male and white for both children receiving and not receiving special education services. Among children in special education, children in the “emotional disturbance category” were more likely than other children to have expenditures above the median, and those in the specific learning disability/specific language impairment categories were less likely to have expenditures above the median.
Table 1.
Demographics of Children of Ages 6 to 18 Years Using Behavioral Health Care in Philadelphia, PA, Calendar Year 2002 as a Function of Median Split in Behavioral Health Expenditures*
| Children in Special Education (n = 27,620) | Other Medicaid-Enrolled Children (n = 99,130) | |||||
|---|---|---|---|---|---|---|
| $0 Users (n = 21,892) |
Low Users (n = 2226) |
High Users (n = 3502) |
$0 Users (n = 83,821) |
Low Users (n = 8401) |
High Users (n = 6908) |
|
| Age in years (SD) | 12.3 (3.0) | 12.1 (2.9) | 11.9 (2.7) | 11.5 (3.4) | 11.6 (3.4) | 11.5 (3.1) |
| Male (%)† | 58 | 67 | 74 | 47 | 55 | 65 |
| Race/ethnicity (%)† | ||||||
| Black | 69 | 62 | 63 | 68 | 62 | 67 |
| Latino | 5 | 7 | 8 | 6 | 7 | 7 |
| Asian | 3 | 1 | 1 | 5 | 2 | 1 |
| White | 15 | 19 | 20 | 13 | 18 | 16 |
| Other | 8 | 11 | 8 | 8 | 11 | 9 |
| Special education category (%)† | ||||||
| Specific learning disability/ specific language impairment |
60 | 61 | 51 | — | — | — |
| Emotional disturbance | 4 | 11 | 27 | — | — | — |
| Mental retardation | 12 | 15 | 11 | — | — | — |
| Other | 24 | 13 | 11 | — | — | — |
Low users had individual expenditures below the median individual expenditure among users, whereas high users had individual expenditures above the median individual expenditure among users. Differences were tested separately for children in special education and other Medicaid-enrolled children.
Indicates differences among groups on that variable at p < .01.
DISCUSSION
This study provides a novel description of Medicaid financing of health care for children receiving special education services. In Philadelphia during calendar year 2002, Medicaid contributed significantly to ensuring that children in special education received necessary health care. Among Medicaid-enrolled children, those in special education were about 2.5 times as likely to use behavioral health services and, among service users, had average expenditures that were 1.75 times as high as students not in special education. While in both groups, a relatively small percentage of children accounted for the majority of expenditures, expenditures were more evenly spread among children in special education, such that cuts in Medicaid support would disproportionately affect a larger proportion of these children.
When interpreting our findings, several limitations of the study should be kept in mind. First, these results rely on the accuracy of Medicaid claims data, both for expenditure information and to identify children who used behavioral health services. Because Philadelphia has a fee-for-service behavior health care carve out, however, incentives for submitting claims are high. Similarly, we relied on data from the Philadelphia Department of Education to identify students in special education. Discussion with city staff suggests that these data are a slight underrepresentation of children receiving special education services. If children receiving special education services but not listed as such are equally likely to receive behavioral health services as those listed, then the estimates presented here underestimate the role of Medicaid-reimbursed services in supplementing special education services. If the reverse is true, then they may be a slight overestimation. Finally, the generalizability of these findings to other school districts is not known, with state and local policies and practices affecting Medicaid implementation. Nonetheless, given Medicaid’s broad coverage, the common practice of providing health care in schools and the poverty of urban children, we expect that most large city school systems in the United States would show similar relationships.
These caveats notwithstanding, our analysis underscores what may be at stake in the Center for Medicare and Medicaid Services (CMS) implementation of the DRA. For the past 2 decades, Congressional efforts resulted in the deliberate overlap of Medicaid and special education activities, aiming to maximize the use of federal IDEA funding for educational services while insisting on coordination with health insurance as a means of ensuring access to the necessary medical care that is central to appropriate educational accommodations. Federal law specifically prohibits CMS from denying coverage for otherwise Medicaid–covered services because they also are listed in a child’s IEP.17 In other words, Congress intended to ensure that Medicaid, not the education system, would pay for covered services when furnished as part of an IEP.
Whether CMS will implement the DRA in a manner consistent with Congress’ historic efforts to link education and health care policy in the case of low-income children remains shrouded by several unanswered but crucial question. For example, will CMS honor the explicit requirement that Medicaid continue to function as the primary payer for covered services listed in a child’s IEP, or will CMS rely on the DRA’s third-party liability recovery amendments to override this specific statutory “coordination of benefits” provision? If CMS takes the latter course, then the financial burden shifted onto public education systems could be significant. For example, the $79 million spent by the Pennsylvania Medicaid program on Philadelphia’s special education students would constitute 4% of the Philadelphia school district’s $2 billion annual budget. Yet, this daunting shift in burden may be what was contemplated by a recent Congressional Budget Office report, which estimated that the new “benefit flexibility” will save $6 billion over a 10-year period primarily by reducing access to certain services, especially mental health care.23
Similarly, will CMS clarify that services listed in an individualized education plan that fall within the federal definition of medical assistance must be covered as EPSDT wraparound services even if they are not covered through a child’s alternative benefit plan? The alternative benefit plan provisions of the DRA introduce the term wraparound into law for the first time. No definition is contained in the statute, but Congressional correspondence in the wake of DRA passage suggests that lawmakers did not intend to narrow the scope of EPSDT.24 Even if EPSDT continues to cover all services that fall within the “medical assistance” definition (including those that may be excluded by a child’s benchmark plan), CMS could still permit states with alternative benefit plans to accept a lesser EPSDT coverage standard than previous law required. This has led groups such as the American Academy of Pediatrics to voice concern that access to services not covered by benchmark plans will be limited.25
In the absence of comprehensive data on the relationships between Medicaid and special education services, anticipating the effects of the DRA is difficult. Although currently there are no federal reporting requirements under children’s programs, such requirements could be enacted and thereby enabling the measurement of separate programs’ impact and assessment of the programs’ interactive and mutually supportive purposes assigned to them by Congress. Aligning data systems and establishing regular communication between the Center for Medicare and Medicaid Services and the Office of Special Education would likely be a critical first step in this endeavor to improve assessment and to serve as a federal template for states to follow.
Our findings provide empirical evidence that changes to Medicaid coverage at the federal level will require states and local municipalities to take on a greater responsibility to oversee and finance behavioral health and other EPSDT services for children with their own coffers. The large percentage of American children relies on these programs to grow and develop into healthy, productive adults contributing to the labor force. Current debates about transferring funding responsibility for programs designed to benefit children from the federal government to the states should consider the long-term consequences for state budgets and the unmet health and educational needs of American children.
Contributor Information
David S. Mandell, Email: mandelld@mail.med.upenn.edu.
Aliza Machefsky, Email: maliza@sas.upenn.edu.
David Rubin, Email: rubin@email.chop.edu.
Chris Feudtner, Email: feudtner@email.chop.edu.
Susmita Pita, Email: pati@email.chop.edu.
Sara Rosenbaum, Email: sarar@gwu.edu.
REFERENCES
- 1.Taras H, Potts-Datema W. Childhood asthma and student performance at school. J Sch Health. 2005;75(8):296–312. doi: 10.1111/j.1746-1561.2005.00041.x. [DOI] [PubMed] [Google Scholar]
- 2.Taras H, Potts-Datema W. Obesity and student performance at school. J Sch Health. 2005;75(8):291–295. doi: 10.1111/j.1746-1561.2005.00040.x. [DOI] [PubMed] [Google Scholar]
- 3.Taras H, Potts-Datema W. Chronic health conditions and student performance at school. J Sch Health. 2005;75(7):255–266. doi: 10.1111/j.1746-1561.2005.00034.x. [DOI] [PubMed] [Google Scholar]
- 4.Huisman M, Kumst A, Bopp M, et al. Educational inequalities in cause specific mortality in middle-aged and older men and women in eight western European populations. Lancet. 2005;365:493–500. doi: 10.1016/S0140-6736(05)17867-2. [DOI] [PubMed] [Google Scholar]
- 5.Steenland K, Henley J, Thun M. All-cause and cause-specific death rates by educational status for two million people in two American Cancer Society cohorts, 1959–1996. Am J Epidemiol. 2002;156:11–21. doi: 10.1093/aje/kwf001. [DOI] [PubMed] [Google Scholar]
- 6.US Department of Education. Jessup, Md: Bureau of Special Education; Twenty-Seventh Annual Report to Congress on the Implementation of the Individuals with Disabilities Education Act. 2005
- 7.Dery M, Toupin J, Pauze R, Verlaan P. Frequency of mental health disorders in a sample of elementary school students receiving special educational services for behavioural difficulties. Can J Psychiatry. 2004;49(11):769–775. doi: 10.1177/070674370404901108. [DOI] [PubMed] [Google Scholar]
- 8.Garland A, Hough R, McCabe K, Yeh M, Wood P, Aarons G. Prevalence of psychiatric disorders in youths across five sectors of care. J Am Acad Child Adolesc Psychiatry. 2001;40(4):409–418. doi: 10.1097/00004583-200104000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Barry C, Gabel J, Frank R, Hawkins S, Whitmore H, Pickreign J. Design of mental health benefits: still unequal after all these years. Health Affairs. 2003;22(5):127–137. doi: 10.1377/hlthaff.22.5.127. [DOI] [PubMed] [Google Scholar]
- 10.Kapphahn C, Morreale M, Rickert V, Walker L. Financing mental health services for adolescents: a background paper. J Adolesc Health. 2006;39(3):318–327. doi: 10.1016/j.jadohealth.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 11.Koppelman J. Children with mental disorders: making sense of their needs and the systems that help them. NHPF Issue Brief. 2004;799:1–24. [PubMed] [Google Scholar]
- 12.Johnson P. Medicaid: Medicaid: eligibility—2005. End of Year Issue Brief. Issue Brief Health Policy Track Serv. 2006:1–15. [PubMed] [Google Scholar]
- 13.Leventhal T, Fauth R, Brooks-Gunn J. Neighborhood poverty and public policy: a 5-year follow-up of children’s educational outcomes in the New York City moving to opportunity demonstration. Devel Psychol. 2005;41(6):933–952. doi: 10.1037/0012-1649.41.6.933. [DOI] [PubMed] [Google Scholar]
- 14.American Academy of Pediatrics Committee on Children’s Health Financing. Medicaid policy statement. Pediatrics. 2005;116(1):274–280. [Google Scholar]
- 15.Rosenbaum S, Sonosky C, Shaw K, Mauery D. Behavioral health and managed care contracting under SCHIP. Policy Brief George Wash Univ Cent Health Serv Res Policy. 2002;5:1–35. [PubMed] [Google Scholar]
- 16.Semansky R, Koyanagi C, Vandivort-Warren R. Behavioral health screening policies in Medicaid programs nationwide. Psychiatr Serv. 2003;54(5):736–739. doi: 10.1176/appi.ps.54.5.736. [DOI] [PubMed] [Google Scholar]
- 17.Noel D, Shreve D. Special ed squeeze: the feds are cutting the Medicaid funds many states rely on to provide health services for disabled students. State Legislatures. 2006;32(10):28–29. [PubMed] [Google Scholar]
- 18.Parrish T, Harr J, Wolman J, Anthony J, Merickel A, Esra P. Palo Alto, Calif: American Institutes for Research; State Special Education Finance Systems, 1999–2000. 2004
- 19.Rodman J, Weill K, Driscoll M, et al. A nationwide survey of financing health-related services for special education students. J Sch Health. 1999;69(4):133–139. doi: 10.1111/j.1746-1561.1999.tb04169.x. [DOI] [PubMed] [Google Scholar]
- 20.Friedman R. Mental health policy for children. In: Levin B, Petrila J, editors. Mental Health Services. A Public Health Perspective. New York, NY: Oxford University Press; 1996. pp. 234–248. [Google Scholar]
- 21.Paternite C. School-based mental health programs and services: overview and introduction to the special issue. J Abnorm Child Psychol. 2005;33(6):657–663. doi: 10.1007/s10802-005-7645-3. [DOI] [PubMed] [Google Scholar]
- 22.Rubin D, Halfon N, Raghavan R, Rosenbaum S. Seattle, Wash: Casey Foundation; Protecting Children in Foster Care: Why Proposed Medicaid Cuts Harm Our Nation’s Most Vulnerable Youth. 2006
- 23.Congressional Budget Office. Deficit Reduction Act of 2005. 2006 [Google Scholar]
- 24.Uninsured TKCoMat. Medicaid and Budget Reconciliation: Implications of the Conference Report; Kaiser Family Foundation; Washington, DC. 2006. [Google Scholar]
- 25.American Academy of Pediatrics. Washington, DC: American Academy of Pediatrics; Deficit Reduction Act of 2005 (DRA): Analysis of Medicaid Provisions. 2006