Abstract
This study investigated the resilience resources and coping profiles of diabetes patients. A total of 145 patients with diabetes completed a questionnaire packet including two measurements of coping (COPE and Coping Styles questionnaires), and personal resources. Glycosylated hemoglobin (HbA1c) was also assessed. Resilience was defined by a factor score derived from measures of self-esteem, self-efficacy, self-mastery, and optimism. All of the maladaptive coping subscales were negatively associated with resilience (r's range from −.34 to −.56, all p's <.001). Of the adaptive coping subscales, only acceptance, emotional support, and pragmatism were positively associated with resilience. The upper, middle, and lower tertiles of the resilience factor were identified and the coping profiles of these groups differed significantly, with low resilience patients favoring maladaptive strategies much more than those with high or moderate resilience resources. Resilience groups did not differ in HbA1c levels; correlation coefficients of the coping subscales with HbA1c were explored. This study demonstrates a link between maladaptive coping and low resilience, suggesting that resilience impacts one's ability to manage the difficult treatment and lifestyle requirements of diabetes.
Keywords: Diabetes, Resilience, Coping, HbA1c
Diabetes patients face adjustment to their disease at many stages over the course of their illness, and not simply at its onset. For example, fluctuations in daily life stress, changes in their physical health, or feelings of burnout, may cause disease management to become even more difficult and burdensome. However, some patients are better able than others to maintain their mental and physical health over the course of their disease.
Positive psychosocial variables have been found to influence the psychological adjustment and physical health of diabetes patients (Fournier, De Ridder, & Bensing, 2002; Johnston-Brooks, Lewis, & Garg, 2002; Sousa, Zauszniewski, Musil, Price Lea, & Davis, 2005). One such construct, resilience, defined as an individual's capacity to maintain psychological and physical well-being in the face of adversity, has flourished across many disciplines of psychology and health because of the rising popularity of positive psychology in these areas. Although sparsely studied in the diabetes population, in other areas of chronic illness and stress such as HIV+ men, survivors of violent trauma, or battered women in shelters, resilience has been found to be associated with better emotional and physical health (Connor, Davidson, & Lee, 2003; Humphreys, 2003; Vedhara & Nott, 1996).
In a previous study of diabetes patients (Yi, Vitaliano, Smith, Yi, & Weinger, 2008), resilience was defined by personality variables that have been shown to increase adaptive capacity in the face of stressful events. Using a factorial composite derived from measures of self-efficacy, self-esteem, self-mastery, and optimism, 111 diabetes patients were followed over a one-year period to assess changes in glycemic control. They found that baseline resilience predicted future glycosylated hemoglobin levels and buffered worsening glycemic control and self-care behaviors in the face of rising distress levels. Specifically, those with low resilience showed increases in HbA1c levels, while those with high resilience did not. It thus appears that resilience is linked to important changes in diabetes patients that have strong implications for their well-being.
Despite this finding, the mechanisms involved in these salutary effects have not been explored in diabetes patients, and are, in fact, still understudied in much of the research involving resilience in general (Kinard, 1998; Rutter, 1987). As first put forth by leading resilience researcher Michael Rutter, the “why” and “how” of resilience is crucial in understanding processes involved in responding to circumstances of risk (Rutter, 1987). Despite this plea, resilience is still predominantly defined as a “constellation of traits” (Jacelon, 1997, p. 128). Understanding the processes of resilience in patients with chronic illness such as diabetes may be useful in aiding prevention and intervention work targeting satisfactory quality of life and physical health.
Therefore, this study investigates coping as a potential mechanism of resilience in diabetes patients. Coping involves the cognitions and behaviors designed to master, tolerate, or reduce internal and external demands. Previous research has identified adaptive and maladaptive coping strategies and inspired the development of appropriate self-report measures to assess individual differences in coping strategies and skills (Carver, 1989; Folkman & Lazarus, 1980; Peyrot & McMurry, 1985). Adaptive and maladaptive coping strategies have, in turn, been found to differ in persons with varying levels of resilience in other populations, suggesting that coping may indeed contribute to resilience in the face of stress (Yi, Smith, & Vitaliano, 2005).
Previous research on coping patterns in diabetes patients has found adaptive, or problem-focused, coping strategies such as planning and active coping to be linked with less depression and anxiety (Macrodimitris & Endler, 2001) and lower glycosylated hemoglobin levels (Graue, Wentzel-Larsen, Bru, Hanestad, & Ovisk, 2004; Hartemann-Heurtier, Sultan, Sachon, Bosquet, & Grimaldi, 2001; Rose, Fliege, Hildenbrandt, Schirop, & Klapp, 2002). Maladaptive, or emotion-focused, coping strategies such as avoidance and disengagement have been associated with poorer metabolic control, quality of life, and psychological adjustment, as well as increased anxiety and depression (Coelho, Amorim, & Prata, 2003; Graue et al., 2004; Macrodimitris & Endler, 2001).
Linking coping to psychosocial resources can elucidate the “why” and “how” of resilience. Despite the passing of two decades since Rutter's original statement (1987), little progress has been made in the understanding of resilience mechanisms. Whether coping may contribute to positive psychosocial resources such as resilience is unclear, although Rose et al. (2002) did find that those with higher self-efficacy and optimism showed more active coping behavior. Our research aimed to expand on these findings by using a person-focused analysis to explore whether varying levels of resilience resources differentiated the coping profiles of diabetes patients.
Materials and Methods
Participants
A convenience sample of 145 patients between the ages of 18 and 75 having diabetes for one year or longer were recruited either by mail or during a medical appointment at the Joslin Diabetes Center (JDC) in Boston, MA. The JDC Committee on Human Studies approved the protocol and voluntary written informed consent was obtained from each participant before the study. The patients completed a questionnaire packet of coping scales and personal resources, and had HbA1c assessed. Depending on the survey instrument, 97-99% of the sample were included in the analysis.
Measures
Resilience Factor
Resilience resources were defined by a “resilience factor” score which was derived from personal, protective resources that are commonly associated with, or used to define, resilience (Cederblad, Dahlin, Hagnell, & Hansson, 1994; Cicchetti, Rogosch, Lynch, & Holt, 1993; Rutter, 1985). These variables included optimism, self-esteem, self-efficacy and self-mastery, and were chosen as they have been used in previous research on resilience and coping in diabetes (Vedhara & Nott, 1996; Wagnild & Young, 1993; Yi et al., 2008)..
Optimism was measured by the Life Orientation Test (LOT), an eight-item self-report measure assessing generalized expectancies. Cronbach's alpha for the scale was .71 and adequate levels of convergent and discriminant validity have been reported (Scheier & Carver, 1987).
Self-esteem was measured using the Rosenberg Self-Esteem Scale (Rosenberg, 1979), which assesses global self-esteem and feelings of personal self-worth. Cronbach's alpha was .91. This is the most widely used scale to measure global self-esteem in research studies.
Self-efficacy was measured with the Confidence in Diabetes Self-care scale (Van Der Ven et al., 2003, CIDS), a questionnaire assessing diabetes-specific self-efficacy with type 1 diabetes. A modified version was administered to type 2 patients. Internal consistency was high (Cronbach's alpha = .90).
Self-mastery was measured by Pearlin and Schooler's (1978) Self-Mastery Scale (SMS). This 7-item questionnaire measures the extent to which a person generally feels as though he or she has personal mastery over life outcomes. Internal consistency was high (Cronbach's alpha = .81). Its basic psychometric properties have been well established (Pearlin & Schooler, 1978).
The four scales were entered into a principal components analysis, and 62% of the variance was explained by a single component, which was designated as the “resilience factor.” This procedure been used previously and verified via structural equation modeling (Yi et al., 2008), and closely related psychosocial resources such as these have been analyzed and reported as a single factor in many other studies investigating resilience (Hull, Lehn, & Tedlie, 1991; Major, Richards, Cooper, Cozzarelli, & Zubek, 1998; Vedhara & Nott, 1996). Two participants had insufficient item-level data for the calculation of the resilience factor.
The Coping Styles Questionnaire (CSQ) is a 15-item measure assessing coping styles (Peyrot & McMurry, 1985; Wilson, Moore, Randolph, & Hanson, 1982). In the current sample, Cronbach alpha,ranged from .54 to .75 (average = .64), similar to Peyrot and McMurry's report (1992). The CSQ was deconstructed to two factors: 1) emotional arousability, including the subscales anxiety, anger, and impatience, and 2) self-control, including the subscales pragmatism and stoicism (Peyrot and McMurry 1985, 1992, Peyrot et al, 1999). Adaptive coping in diabetes patients using the CSQ has been defined by the self-control subscales, and maladaptive coping has been defined by the emotional arousability subscales (Peyrot et al, 1999).
The Brief COPE inventory was also used to assess coping patterns (Carver, 1997). The items of the Brief COPE yielded 11 subscales: active coping, acceptance, emotional support, instrumental support, positive reframing, planning, self-distraction, denial, behavioral disengagement, venting, and self-blame. Each subscale included two items for scoring purposes, and Cronbach's alpha ranged from .52 to .76 (average = .66). Given the importance of taking an active role in self-management with chronic illnesses such as diabetes, the Brief COPE subscales hypothesized as being adaptive included: active coping, acceptance, emotional support, instrumental support, and positive reframing, and the hypothesized maladaptive strategies included: self-distraction, denial, behavioral disengagement, venting, and self-blame. These subscales have been similarly categorized as either adaptive or maladaptive in other chronic illness and stress research and have been linked with general health, quality of life, and anxiety and distress (Gilbar, Or-Han, & Plivazky, 2005; Llewellyn, McGurk, & Weinman, 2005; Vosvick et al., 2003).
Glycemic Control was measured by glycosylated hemoglobin (HbA1c). HbA1c measures glycemic control over the prior 2 to 3 months and is used in all major clinical trials of diabetes (Diabetes Control and Complications Trial Research Group, 1993). Higher HbA1c indicates poorer control. The JDC laboratory in Boston, MA analyzed all samples using high-performance liquid chromatography ion capture (Tosch Medics, San Francisco, CA; reference range: 4.0-6.0%). These methods conform to the Diabetes Control and Complications Trial Research Group (1993) standardized methods.
Statistical Analyses
Principal components analysis was used to derive the resilience factor (Yi et al., 2008). Student t-tests were used to investigate sex differences and differences between type 1 and type 2 diabetes patients. In order to isolate those with low, moderate, and high resilience resources, the upper, middle, and lower tertiles of the resilience factor were identified. Forty-seven participants were labeled as having “low resilience” (LO; range = −2.95 to −.29), 47 participants were considered to have moderate levels of resilience (MOD; range = −.24 to .51), and 49 participants were labeled as having “high resilience” (HI; range = .56 to 2.18). Multivariate analysis of variance and chi-square tests were used to compare the resilience groups on demographic characteristics.
Pearson correlation coefficients and Student t-tests were used to estimate associations between coping subscales, demographic variables, and resilience. Pearson correlation coefficients were also estimated to examine associations between coping subscales and HbA1c overall. Multivariate analysis of variance was used to calculate an overall test of a difference in profiles between resilience groups (Yi et al., 2005), and univariate contrasts were used to investigate the resilience group differences for each of the coping subscales. To reduce Type 1 error, a Bonferroni correction was employed for the multiple coping strategy comparisons (“Coping Profiles” section), yielding an appropriately conservative p-value (.05 divided by 15 tests yielded significant p< .003).
Results
Demographic characteristics
Demographic characteristics of the sample are presented in Table 1. Patients with type 1 diabetes differed from those with type 2 diabetes in expected directions for age (T1: 44.35 ± 14.18, T2: 58.30 ± 12.3; t= −5.93, p<.001), duration of diabetes (T1: 23.05 ± 12.87, T2: 11.66 ± 10.39; t=5.40, p<.001), and HbA1c (T1: 8.02 ± 1.26; T2: 7.45 ± 1.59; t=2.25, p<.05). However, all resilience attributes and coping variables were similar, and associations between key variables for type 1 and type 2 patients were comparable; therefore, all patients were considered together. Table 1 also shows demographics stratified by resilience group. No differences existed between the resilience groups, with the exception of sex, such that the low resilience group had more women than the moderate or high resilience groups (χ2= 6.57, p<.05).
Table 1.
Means (M) or Percentages, Standard Deviations (SD), and Ranges of Demographic Variables for Combined Sample, and by Resilience Group
| All (n=145) |
Low (n=47) |
Moderate (n=47) |
High (n=49) |
||
|---|---|---|---|---|---|
| Variable | M (or %) ± SD | Range | M (or %) ± SD | ||
| Age | 49.4 ± 15.1 | 18-77 | 45.21 ± 12.51 | 51.00 ± 15.75 | 51.46 ± 16.26 |
| Education (yrs) | 15.3 ± 2.9 | 8-20 | 14.64 ± 2.72 | 15.67 ± 2.91 | 15.63 ± 3.02 |
| Baseline HbA1c (%) | 7.8 ± 1.4 | 4.6-13.2 | 8.03 ± 1.45 | 7.57 ± 1.33 | 7.92 ± 1.40 |
| Duration of DM (yrs) | 18.9 ± 13.2 | 1-53 | 18.05 ± 13.04 | 16.78 ± 11.55 | 21.22 ± 14.47 |
| Sex (% female) | 57 | 72* | 55 | 47 | |
| Ethnicity (% Caucasian) | 88 | 83 | 88 | 91 | |
| Type of DM (% Type 1) | 63 | 66 | 57 | 65 | |
| Presence of Complications (% Yes) |
46 | 55 | 45 | 37 | |
Note. Two patients had insufficient item-level data for the calculation of the resilience factor.
p<.05.
Descriptive statistics and associations with resilience
Means and standard deviations for each of the coping subscales are presented in Table 2. To explore associations between the resilience factor and demographic characteristics, Pearson correlation coefficients and independent t-tests are also presented in Table 2. Men, older patients, and those with more education had higher resilience resources. All maladaptive coping subscales of the COPE were negatively associated with the resilience factor. Of these, self-distraction and venting also correlated with age, such that older patients used less of these variables. Self-distraction and self- blame were used more in females than males, and self-distraction was used more in less educated patients. Those with longer duration of diabetes tended to use denial less (Table 2).
Table 2.
Means, Standard Deviations, and Correlation Coefficients for the Resilience Factor (RF) with Coping Subscales of the COPE and Coping Styles Questionnaires
| Correlation Coefficients | T-tests | ||||||
|---|---|---|---|---|---|---|---|
| Variable | M ± SD | RF | Age | Duration | Education | Type (1=Type 2, 2=Type 2) |
Sex (0=Male, 1=Female) |
| Resilience Factor Score (RF) | 0 ± 1 | -- | .24** | .07 | .19* | −.74 | 2.61* |
| COPE: Maladaptive | |||||||
| Self-distraction | 4.52 ± 1.94 | −.43*** | −.24** | −.08 | −.20* | −.21 | −3.06** |
| Denial | 2.65 ± 1.26 | −.34*** | −.10 | −.19* | −.13 | −1.89 | −1.10 |
| Behavioral Disengagement | 3.01 ± 1.41 | −.45*** | −.13 | −.15 | −.16 | −1.06 | −.65 |
| Venting | 4.05 ± 1.59 | −.38*** | −.19* | .001 | −.05 | .72 | −1.93 |
| Self-blame | 4.13 ± 1.88 | −.56*** | −.09 | −.05 | −.06 | −1.20 | −3.35** |
| COPE: Adaptive | |||||||
| Active coping | 5.90 ± 1.61 | −.09 | .10 | −.04 | −.05 | −.98 | −1.05 |
| Acceptance | 6.74 ± 1.45 | .32*** | .18* | −.01 | .17* | −.47 | −.54 |
| Emotional support | 5.02 ± 1.86 | .21* | −.12 | −.14 | .05 | 1.04 | .52 |
| Instrumental support | 4.64 ± 1.61 | −.07 | −.19* | −.19* | .07 | .43 | −.18 |
| Positive reframing | 4.85 ± 1.70 | −.03 | −.09 | .11 | .07 | .33 | −1.29 |
| Planning | 5.42 ± 1.69 | −.04 | .001 | .08 | .13 | −1.81 | −.94 |
| Coping Styles: Maladaptive | |||||||
| Anger | 39.58 ± 24.33 | −.54*** | −.15 | .04 | −.14 | −.30 | −.45 |
| Anxiety | 44.06 ± 28.80 | −.47*** | −.08 | .19* | −.18* | −2.02* | −2.30* |
| Impatience | 44.10 ± 25.38 | −.41*** | −.21* | .18* | −.12 | .03 | −2.21* |
| Coping Styles: Adaptive | |||||||
| Stoicism | 53.40 ± 23.44 | .01 | .15 | .02 | .02 | .34 | −.23 |
| Pragmatism | 57.06 ± 25.45 | .43*** | .13 | −.13 | .14 | .49 | 1.56 |
Note. COPE subscales range = 1-8. Coping Styles range = 0-100.
p<.05,
p<.01,
p<.001.
Two adaptive subscales of COPE, acceptance and emotional support, were positively associated with resilience (Table 2). Of these, acceptance was used more frequently in older and more educated patients. Duration of diabetes was negatively associated with both instrumental support and planning, such that those who have less years of duration used these more.
Similar to the responses from the COPE, all maladaptive coping responses from the Coping Styles questionnaire were negatively associated with resilience (Table 2). Impatience was also correlated with age, such that older patients were less likely to use impatience, and both anxiety and impatience were more likely to be used by less educated patients. Of the adaptive coping responses from the Coping Styles questionnaire, only pragmatism was positively associated with resilience (Table 2).
Coping profiles
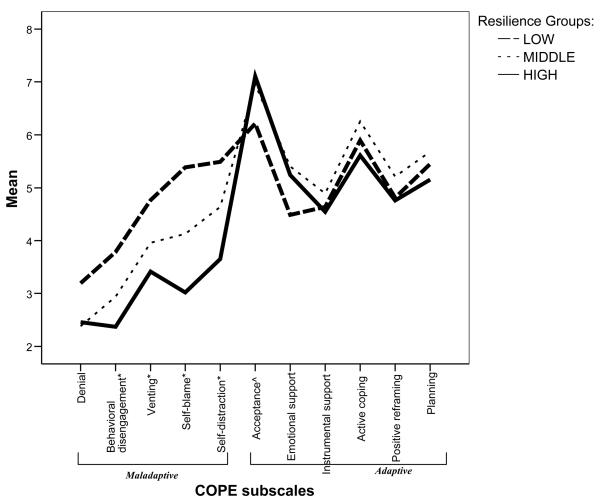
To examine differences in coping profiles between the resilience groups, we computed a one-way multivariate analysis of variance on the COPE subscale mean scores. This test yielded a significant effect for Groups, F (22,250) = 3.79, p<.001, indicating different patterns of coping in the groups (Figure 1). Those with the lowest resilience resources revealed a profile that showed the highest use of all maladaptive coping strategies compared to the high and moderate resilience groups. Univariate contrasts revealed that the low resilience group had the highest scores for: behavioral disengagement (F (2,138) = 13.71, p<.001), venting (F (2,138) = 9.47, p<.001), self-blame (F (2,138) = 24.68, p<.001), and self-distraction (F (2,138) = 12.59, p<.001). The groups did not differ on adaptive subscales, although there was a trend for the low resilience group to score lowest in acceptance (F (2,138) = 5,59, p<.01). Mean item coping strategy scores for the resilience groups are presented in profile form in Figure 1.
Figure 1.
Coping mean item score profiles for the high, middle, and low resilience groups on the COPE.
Note. P-values reflect univariate contrasts between resilience groups. Overall F (22,250) = 3.79, p<.001. COPE subscales range 1-8.
*p<.001, ^p<.01.
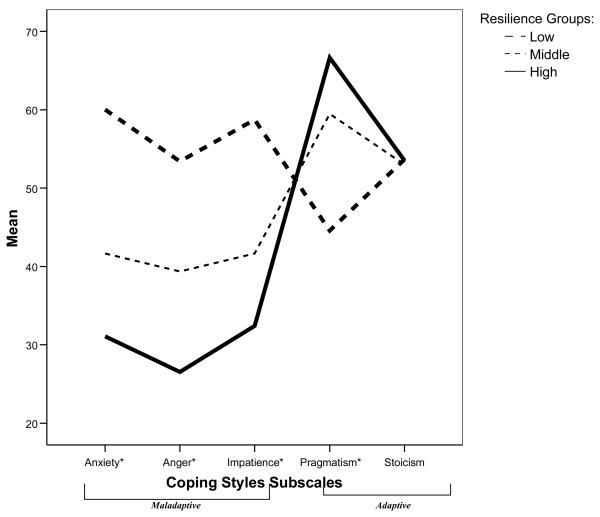
The profiles for the resilience groups on the subscales of the Coping Styles are presented in Figure 2. The overall test for differences in profiles for resilience groups among the Coping Styles subscales was significant (F (10,270) = 6.09, p<.001). Univariate tests show that those with low resilience resources showed much higher use of maladaptive coping styles than the moderate or high resilience groups in: anxiety (F (2,142) = 14.62, p<.001), anger (F (2,142) = 18.03, p<.001), and impatience (F (2,142) = 15.78, p<.001). Of the adaptive coping styles, pragmatism was lowest for those with low resilience resources (F (2,142)=10.54, p<.001), and stoicism was not differentiated by group status.
Figure 2.
Coping mean item score profiles for the high, middle, and low resilience groups on the Coping Styles Questionnaire.
Note. P-values reflect univariate contrasts between resilience groups. Overall F (10, 270) = 6.09, p<.001. Coping Styles subscales range 0-100.
*p<.001.
Associations with glycemic control
Resilience groups did not differ in their mean HbA1c levels (LO = 8.03 ± 1.48, MOD = 7.57 ± 1.33, HI = 7.92 ± 1.40; F(2,140) = 1.39, p=NS); nor did the resilience factor as a linear variable associate with HbA1c (r=−.11, p=NS). Exploring the associations between coping subscales and HbA1c revealed that overall, use of anger coping style was associated with higher HbA1c levels (r=.22, p<.05). No other coping subscales were associated with HbA1c.
Discussion
Diabetes is a chronic illness that must be acknowledged and cared for over the course of one's lifetime. Some patients manage to cope with daily life stress without having it affect their diabetes-related outcomes better than others. Research in stress and coping has showed that emotion-focused coping is considered less adaptive when the stressor can be controlled (Vitaliano, DeWolfe, Maiuro, Russo, & Katon, 1990), as is the case in coping with diabetes. Thus, this study was designed to investigate resilience resources and coping patterns as potential sources for these individual differences.
Not surprisingly, several demographic variables were associated with coping patterns. Maladaptive coping patterns were typically more common in women, younger patients, those with less years of education and those with less years of diabetes duration. This is consistent with other coping research showing that younger adults and women use more emotion-focused coping than older adults or men (Jensen, Nygren, Gamberale, Goldie, & Westerholm, 1994; Tamres, Janicki, & Helgeson, 2002; Yeung & Fung, 2007). We also found that women had lower resilience resources than men. This finding is consistent with others that suggest men have more personal resources than women (e.g., Kling, Hyde, Showers, & Buswell, 1999). Interestingly, increased attention to the genetics of resilience has revealed the heritability of resilience to be higher in men versus women (Boardman, Blalock, & Button, 2008). Given this, more research is needed exploring the bolstering of resilience in women in particular, as clinicians may benefit further understanding of sex differences in this area on therapy and intervention.
Of the adaptive coping patterns, older and more educated patients tended to use more acceptance coping. Perhaps these characteristics are signs of more “coping maturity” in these patients. Interestingly, those with longer duration of diabetes were less likely to use instrumental support and planning. It may be that these particular strategies of coping only have benefit to those who have been diagnosed more recently. One study investigating patients with breast cancer found that younger women had poorer psychological adjustment near the time of initial diagnosis, but this association was no longer significant at follow-up visits (Compas et al., 1999). As newly diagnosed patients with diabetes are more prone to being overwhelmed by the rigid self-management and lifestyle requirements, our results similarly seem to indicate that coping strategies influential to this adjustment (such as instrumental support and planning) were of more benefit to those newly diagnosed patients. Further research is needed to elucidate these findings.
Previous research has shown that high levels of resilience resources buffer, or protect, diabetes patients from worsening HbA1c or self-care behaviors in the face of rising distress (Yi et al., 2008). To explore coping patterns as a potential mechanism of this finding, we first investigated the association between coping and resilience. Interestingly, every maladaptive coping subscale from both the COPE and Coping Styles Questionnaires was negatively associated with levels of resilience resources. Clearly, the use of maladaptive coping strategies was exacerbated by low levels of resilience, although directionality is still unclear. In fact, we found that the coping profiles of these groups differed, and this difference was primarily driven by the vast differences in use of maladaptive coping. The high resilience group seemed to adopt maladaptive coping strategies extremely infrequently as compared to adaptive strategies. The use of self-blame, anxiety, impatience and behavioral disengagement were the most notable differences between the resilience groups. While prior research has shown relations among these maladaptive strategies and poor glycemic control, quality of life, and psychological adjustment (Coelho et al., 2003; Graue et al., 2004; Peyrot, McMurry, & Kruger, 1999), no study to our knowledge has linked maladaptive coping strategies to fewer personal resources, such as resilience. Given the mixed results in the effectiveness of coping interventions in chronic illness patients (de Ridder & Schreurs, 2001), our finding may help target the specific patients who would benefit from an intervention with a coping modification component.
Adaptive coping strategies were not as strongly related to resilience as maladaptive strategies, such that those with the lowest resilience resources used adaptive coping patterns the least. Literature in chronic pain and illness have reported adaptive coping to be associated with better outcomes (McCracken & Eccleston, 2003) (Zalewska, Miniszewska, Chodkiewicz, & Narbutt, 2007). We did not find a particularly strong link for those with high levels of resilience to use adaptive coping strategies significantly more than those with lower resilience resources. It may be the case that having ample resilience resources is sufficient for managing the ups and downs of living with diabetes, and the choice and use of coping strategies is not as critical for these patients as it is for those who have low levels of personal resources.
We did not find an association between resilience and HbA1c in our study, nor did we find strong associations between coping strategies and glycemic control. However, in our previous study, we found that resilience predicted change in glycemic control over time (Yi et al., 2008). Thus, future research should continue to investigate changes over time in these critical variables, and should be explored in relation to both resilience and coping. We did find that anger coping style associated with glycemic control, such that more use of anger coping associated with higher HbA1c levels. This finding corroborates previous reports on the detrimental effects of anger coping (Yi, Yi, Vitaliano, & Weinger, 2008). Other research has reported active coping patterns to be linked with lower HbA1c levels (Graue et al., 2004; Hartemann-Heurtier et al., 2001; Rose et al., 2002). As this study is cross-sectional, further research is needed to understand the long-term effects of coping on resilience on diabetes-specific outcomes such as HbA1c, and how resilience may protect individuals from worsening levels.
Taken together, these results may suggest a “double whammy” effect for persons undergoing chronic illness. In analyses of the planned univariate contrast tests, differences were truly driven by the high levels of maladaptive coping used by the low resilience groups. Thus, it may be the case that maladaptive coping is exacerbated by the lack of resilience resources, although causality is not determined in this study. Interventions targeting those patients with poor glycemic control can benefit from understanding the resources and mechanisms involved with diabetes outcomes. Our work suggests that identifying those with low resilience resources may inform a psychoeducational coping skills intervention designed specifically to reduce maladaptive coping strategies and instead teach patients how to choose and effectively execute coping strategies which may in turn improve long-term glycemic outcomes. Given the mixed results in the effectiveness of coping interventions in chronic illness patients (de Ridder & Schreurs, 2001), our findings may help target the specific low-resilience patients who would benefit from an intervention with a coping modification component. In sum, our study expands on existing work by highlighting the importance of coping in diabetes patients and informs tailored-interventions by identifying the specific individuals that may benefit most from the improvement of coping skills.
Acknowledgments
This research was supported by the National Science Foundation (National Science Foundation Graduate Research Fellowship Grant), the National Institute of Mental Health (R01 MH57663), and the Harvard Medical School Priscilla White Fellowship, National Institute of Diabetes and Digestive and Kidney Diseases (R01 NIDDK60115, P30 NIDDK36836).
References
- Boardman JD, Blalock CL, Button TM. Sex differences in the heritability of resilience. Twin Research and Human Genetics. 2008;11:12–27. doi: 10.1375/twin.11.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS. How should multifaceted personality constructs be tested? Issues illustrated by self-monitoring, attributional style and hardiness. Journal of Personality and Social Psychology. 1989;56(4):577–585. doi: 10.1037//0022-3514.56.4.577. [DOI] [PubMed] [Google Scholar]
- Carver CS. You want to measure coping but your protocol's too long: consider the Brief COPE. International Journal of Behavioral Medicine. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Cederblad M, Dahlin L, Hagnell O, Hansson K. Salutogenic childhood factors reported by middle-aged individuals. European Archives of Psychiatry and Clinical Neuroscience. 1994;244:1–11. doi: 10.1007/BF02279805. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Lynch M, Holt KD. Resilience in maltreated children: Processes leading to adaptive outcome. Development and Psychopathology. 1993;5:629–647. [Google Scholar]
- Coelho R, Amorim I, Prata J. Coping styles and quality of life in patients with non-insulin-dependent diabetes mellitus. Psychosomatics. 2003;44:312–318. doi: 10.1176/appi.psy.44.4.312. [DOI] [PubMed] [Google Scholar]
- Compas BE, Stoll MF, Thomsen AH, Oppedisano G, Epping-Jordan JE, Krag DN. Adjustment to breast cancer: age-related differences in coping and emotional distress. Breast Cancer Research and Treatment. 1999;54:195–203. doi: 10.1023/a:1006164928474. [DOI] [PubMed] [Google Scholar]
- Connor KM, Davidson JR, Lee L-C. Spirituality, resilience, and anger in survivors of violent trauma: A community survey. Journal of Traumatic Stress. 2003;16:487–494. doi: 10.1023/A:1025762512279. [DOI] [PubMed] [Google Scholar]
- de Ridder D, Schreurs K. Developing interventions for chronically ill patients: is coping a helpful concept? Clinical Psychology Review. 2001;21:205–240. doi: 10.1016/s0272-7358(99)00046-x. [DOI] [PubMed] [Google Scholar]
- Diabetes Control and Complications Trial Research Group The effect of intensive treatment of diabetes on the development and progressions of long-term complications in insulin-dependent diabetes mellitus. New England Journal of Medicine. 1993;329:977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- Folkman S, Lazarus RS. An analysis of coping in a middle-aged community sample. Journal of Health and Social Behavior. 1980;21:219–239. [PubMed] [Google Scholar]
- Fournier M, De Ridder D, Bensing J. Optimism and adaptation to chronic disease: The role of optimism in relation to self-care options of type 1 diabetes mellitus, rheumatoid arthritis and multiple sclerosis. British Journal of Health Psychology. 2002;7:409–432. doi: 10.1348/135910702320645390. [DOI] [PubMed] [Google Scholar]
- Gilbar O, Or-Han K, Plivazky N. Mental adjustment, coping strategies, and psychological distress among end-stage renal disease patients. Journal of Psychosomatic Research. 2005;58:471–476. doi: 10.1016/j.jpsychores.2005.01.004. [DOI] [PubMed] [Google Scholar]
- Graue M, Wentzel-Larsen T, Bru E, Hanestad BR, Ovisk O. The coping styles of adolescents with type 1 diabetes are associated with degree of metabolic control. Diabetes Care. 2004;27:1313–1317. doi: 10.2337/diacare.27.6.1313. [DOI] [PubMed] [Google Scholar]
- Hartemann-Heurtier A, Sultan S, Sachon C, Bosquet F, Grimaldi A. How type 1 diabetic patients with good or poor glycemic control cope with diabetes-related stress. Diabetic Medicine. 2001;27:553–559. [PubMed] [Google Scholar]
- Hull JC, Lehn DA, Tedlie JC. A general approach to testing multifaceted personality constructs. Journal of Personality and Social Psychology. 1991;61:932–945. doi: 10.1037//0022-3514.61.6.932. [DOI] [PubMed] [Google Scholar]
- Humphreys J. Resilience in sheltered battered women. Issues in Mental Health Nursing. 2003;24:137–152. doi: 10.1080/01612840305293. [DOI] [PubMed] [Google Scholar]
- Jacelon CS. The trait and process of resilience. Journal of Advanced Nursing. 1997;25:123–129. doi: 10.1046/j.1365-2648.1997.1997025123.x. [DOI] [PubMed] [Google Scholar]
- Jensen I, Nygren A, Gamberale F, Goldie I, Westerholm P. Coping with long-term musculoskeletal pain and its consequences: is gender a factor? Pain. 1994;57:167–172. doi: 10.1016/0304-3959(94)90220-8. [DOI] [PubMed] [Google Scholar]
- Johnston-Brooks CH, Lewis MA, Garg S. Self-efficacy impacts self-care and HbA1c in young adults with type 1 diabetes. Psychosomatic Medicine. 2002;64:43–51. doi: 10.1097/00006842-200201000-00007. [DOI] [PubMed] [Google Scholar]
- Kinard EM. Methodological issues in assessing resilience in maltreated children. Child Abuse and Neglect. 1998;22:669–680. doi: 10.1016/s0145-2134(98)00048-9. [DOI] [PubMed] [Google Scholar]
- Kling KC, Hyde JS, Showers CJ, Buswell BN. Gender differences in self-esteem: a meta-analysis. Psychological Bulletin. 1999;125:470–500. doi: 10.1037/0033-2909.125.4.470. [DOI] [PubMed] [Google Scholar]
- Llewellyn CD, McGurk M, Weinman J. Head and neck cancer: to what extent can psychological factors explain differences between health-related quality of life and individual quality of life? The British Journal of Oral and Maxillofacial Surgery. 2005;44:351–357. doi: 10.1016/j.bjoms.2005.06.033. [DOI] [PubMed] [Google Scholar]
- Macrodimitris SD, Endler NS. Coping, control, and adjustment in Type 2 diabetes. Health Psychology. 2001;20:208–216. [PubMed] [Google Scholar]
- Major B, Richards C, Cooper ML, Cozzarelli C, Zubek J. Personal resilience, cognitive appraisals, and coping: An integrative model of adjustment to abortion. Journal of Personality and Social Psychology. 1998;74:735–752. doi: 10.1037//0022-3514.74.3.735. [DOI] [PubMed] [Google Scholar]
- McCracken LM, Eccleston C. Coping or acceptance: what to do about chronic pain? Pain. 2003;105:197–204. doi: 10.1016/s0304-3959(03)00202-1. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Schooler C. The structure of coping. Journal of Health and Social Behavior. 1978;19:2–21. [PubMed] [Google Scholar]
- Peyrot MF, McMurry JF. Psychosocial factors in diabetes control: Adjustment of insulin-treated adults. Psychosomatic Medicine. 1985;47:542–557. doi: 10.1097/00006842-198511000-00004. [DOI] [PubMed] [Google Scholar]
- Peyrot MF, McMurry JF, Kruger DF. A biopsychosocial model of glycemic control in diabetes: Stress, coping and regimen adherence. Journal of Health and Social Behavior. 1999;40:141–158. [PubMed] [Google Scholar]
- Rose M, Fliege H, Hildenbrandt M, Schirop T, Klapp BF. The network of psychological variables in patients wth diabetes and their importance for quality of life and metabolic control. Diabetes Care. 2002;25:35–42. doi: 10.2337/diacare.25.1.35. [DOI] [PubMed] [Google Scholar]
- Rosenberg M. Conceiving the self. Basic Books; New York: 1979. [Google Scholar]
- Rutter M. Resilience in the face of adversity: Prospective factors and resistance to psychiatric disorder. British Journal of Psychiatry. 1985;147:598–611. doi: 10.1192/bjp.147.6.598. [DOI] [PubMed] [Google Scholar]
- Rutter M. Psychosocial resilience and protective mechanisms. American Orthopsychiatric Association. 1987;57:316–331. doi: 10.1111/j.1939-0025.1987.tb03541.x. [DOI] [PubMed] [Google Scholar]
- Scheier M, Carver C. Dispositional optimism and physcial well-being: the influence of generalized outcome expectancies on health. Journal of Personality. 1987;55:169–210. doi: 10.1111/j.1467-6494.1987.tb00434.x. [DOI] [PubMed] [Google Scholar]
- Sousa VD, Zauszniewski JA, Musil CM, Price Lea PJ, Davis SA. Relationships among self-care agency, self-efficacy, self-care, and glycemic control. Research and Theory for Nursing Practice. 2005;19:217–230. doi: 10.1891/rtnp.2005.19.3.217. [DOI] [PubMed] [Google Scholar]
- Tamres LK, Janicki D, Helgeson VS. Sex differences in coping behavior: a meta-analytic review and an examination of relative coping. Personality and Social Psychology Review. 2002;6:2–30. [Google Scholar]
- Van Der Ven N, Weinger K, Yi J, Pouwer F, Ader H, Van Der Ploeg HM, Snoek FJ. The confidence in diabetes self-care scale: Psychometric properties of a new measure of diabetes-specific self-efficacy in Dutch and US patients with type 1 diabetes. Diabetes Care. 2003;26(3):713–718. doi: 10.2337/diacare.26.3.713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vedhara K, Nott KH. Psychosocial vulnerability to stress: A study of HIV-positive homosexual men. Journal of Psychosomatic Research. 1996;41(3):255–267. doi: 10.1016/0022-3999(96)00096-7. [DOI] [PubMed] [Google Scholar]
- Vitaliano PP, DeWolfe D, Maiuro RD, Russo J, Katon W. Appraised changeability of a stressor as a modifier of the relationship of coping and depression: A test of the hypothesis of fit. Journal of Personality and Social Psychology. 1990;59:582–590. doi: 10.1037//0022-3514.59.3.582. [DOI] [PubMed] [Google Scholar]
- Vosvick M, Koopman C, Gore-Felton C, Thoresen C, Krumboltz J, Spiegel D. Relationship of functional quality of life to strategies for coping with the stress of living with HIV/AIDS. Psychosomatics. 2003;44:51–58. doi: 10.1176/appi.psy.44.1.51. [DOI] [PubMed] [Google Scholar]
- Wagnild GM, Young HM. Development and psychometric evaluation of the resilience scale. Journal of Nursing Measurement. 1993;1(2):165–178. [PubMed] [Google Scholar]
- Wilson JF, Moore RW, Randolph S, Hanson BJ. Behavioral preparation of patients for gastrointestinal endoscopy: Information, relaxation, and coping style. Journal of Human Stress. 1982;8:13–23. doi: 10.1080/0097840X.1982.9936114. [DOI] [PubMed] [Google Scholar]
- Yeung DY, Fung HH. Age differences in coping and emotional responses toward SARS: a longitudinal study of Hong Kong Chinese. Aging and Mental Health. 2007;11:579–587. doi: 10.1080/13607860601086355. [DOI] [PubMed] [Google Scholar]
- Yi JP, Smith RE, Vitaliano PP. Stress-resilience, illness, and coping: A person-focused investigation of young women athletes. Journal of Behavioral Medicine. 2005;28:257–265. doi: 10.1007/s10865-005-4662-1. [DOI] [PubMed] [Google Scholar]
- Yi JP, Vitaliano PP, Smith RE, Yi JC, Weinger K. The role of resilience on psychological adjustment and physical health in patients with diabetes. British Journal of Health Psychology. 2008;13:311–325. doi: 10.1348/135910707X186994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi JP, Yi JC, Vitaliano PP, Weinger K. How does anger coping style affect glycemic control in diabetes patients? International Journal of Behavioral Medicine. 2008;15:167–172. doi: 10.1080/10705500802219481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zalewska A, Miniszewska J, Chodkiewicz J, Narbutt J. Acceptance of chronic illness in psoriasis vulgaris patients. Journal of the European Academy of Dermatology and Venereology. 2007;21:235–242. doi: 10.1111/j.1468-3083.2006.01912.x. [DOI] [PubMed] [Google Scholar]