Abstract
The objective of this study is to demonstrate the utility of the scratch collapse test (SCT) in localizing the point of maximal compression in cubital tunnel syndrome. From January 1, 2004 to December 1, 2005, 64 adult patients with cubital tunnel syndrome were evaluated by a single surgeon. Cubital tunnel syndrome was diagnosed based upon symptoms of numbness, tingling, and/or pain in the ulnar nerve distribution or by the presence of weakness or wasting of the ulnar-innervated intrinsic hand muscles. All diagnoses were confirmed with electrodiagnostic studies. As part of the physical examination, the SCT was performed along three subdivided segments in the region of the cubital tunnel. Results of the SCT were recorded and correlated with intraoperative findings. Of the 64 patients evaluated, 44 had a positive SCT that was either more profound or solely present a few centimeters distal to the medial epicondyle in the region of Osborne’s band. All of these patients subsequently underwent anterior submuscular transposition and were found to have a tight compression point at Osborne’s band corresponding to their preoperative SCT. This study suggests that the scratch collapse test may be a reliable physical examination technique for localizing the point of maximal nerve compression in patients with cubital tunnel syndrome. That point, in this series, corresponded with Osborne’s band.
Keywords: Cubital tunnel syndrome, Scratch-collapse test, Osborne’s band, Physical examination, Ulnar nerve transposition
Introduction
Cubital tunnel syndrome refers to symptoms of ulnar nerve compression in the area of the fibro-osseus tunnel along the ulnar groove of the medial epicondyle of the humerus. This term was introduced by Feindel and Stratford in 1958 [8]. Although incidence and prevalence numbers are not known, it is the second most commonly diagnosed nerve entrapment disorder with numbers climbing annually [3]. It is estimated at 25 cases per 100,000 person-years or 75,000 cases annually in the USA [2]. The exact etiology and ideal management of cubital tunnel syndrome continues to be heavily debated. In fact, several entrapment sites in the region of the cubital tunnel have been described. The current study demonstrates the possible utility of a new provocative examination modality, the scratch collapse test (SCT), in precisely localizing the region of entrapment in patients suffering from cubital tunnel syndrome. The SCT is a provocative test, which has been adopted by the senior author from the functionally based examination paradigm introduced by John L. Beck, MD [5]. Our first communication regarding this examination modality was recently published demonstrating its efficacy in the physical examination armamentarium for both carpal and cubital tunnel syndrome [6]. The current communication illustrates its additional capacity to precisely localize the site of entrapment in cubital tunnel syndrome.
The Scratch Collapse Test
The scratch collapse examination involves having the patient take a seated posture with the arms at the sides and elbows bent at 90°. The patient is then asked to resist the examiner’s attempt to medially rotate the arms (Fig. 1). After assessing the baseline resistance provided by the patient, the region overlying the potential entrapment point is then stroked and immediately, the test is repeated. Upon repeat testing, a qualitative change in resistance is assessed ipsilateral to the entrapment point assessed. Most commonly, the patient is at least as aware as the examiner of the change in their ability to resist. Not uncommonly, they are quite surprised by the sudden change in strength. This effect only lasts a few seconds, and longer delays may produce a false negative. Accordingly, pauses as short as 10 to 15 s are usually sufficient prior to repeating the test as the effect of the prior trial should have decayed sufficiently in this interval.
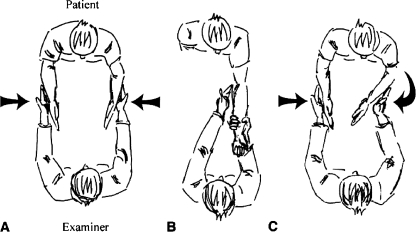
Figure 1.
The scratch collapse test. The figure illustrates the scratch collapse test. The patient faces the examiner with arms adducted, elbows flexed, and forearms parallel to one another with wrists at neutral. Step A: The patient resists bilateral internal rotation forces applied by the examiner. Step B: Next, the examiner “scratches” or swipes with fingertips over the course of the nerve (ulnar nerve at elbow illustrated). Step C: Step A is immediately repeated. Brief unilateral reduction in the patient’s resistance to internal rotation is considered a positive scratch collapse test. Reprinted with permission [6].
The utility of this examination tool with respect to the more well-established Tinel’s and elbow-flexion provocative tests was recently reviewed and is summarized in Table 1. With respect to ulnar nerve entrapment at the elbow, the scratch collapse was found to be 69% sensitive and 99% specific. This is compared with significantly lower sensitivity values of 54% and 46% for Tinel’s and elbow-flexion provocation, respectively. The specificities of all of these examinations were found to be 99%. With an estimated accuracy of 82% and 89%, respectively, the scratch collapse test has proven to be a useful adjunct in the clinical diagnosis of carpal tunnel syndrome and cubital tunnel syndrome [6].
Table 1.
Sensitivity, specificity, and predicted values of clinical nerve compression tests.
| Sensitivity (%) | Specificity (%) | Positive predictive Value (%) | Negative predictive Value (%) | Accuracy (%) | |
|---|---|---|---|---|---|
| Wrist Tinel | 32* | 99 | 96 | 59 | 65 |
| Wrist provocative | 44* | 99 | 98 | 65 | 72 |
| Wrist scratch collapse | 64 | 99 | 99 | 73 | 82 |
| Elbow Tinel | 54* | 99 | 97 | 98 | 84 |
| Elbow provocative | 46* | 99 | 96 | 78 | 81 |
| Elbow scratch collapse | 69 | 99 | 99 | 86 | 89 |
Prevalence of carpal tunnel syndrome, 70%; prevalence of cubital tunnel syndrome, 32%
*p < 0.001 compared with scratch collapse test
Reprinted with permission[6]
Further experience with this test has allowed us to reliably elicit responses in more focal positions along the nerve being assessed. While a broad stroke encompassing the region of proposed entrapment is usually sufficient to elicit the response, we have found that shorter and more localized strokes over a region of the nerve in question will elicit a response at a specific reliable site. This precise position has anecdotally been confirmed with a strong interexaminer reliability.
Ulnar Nerve Anatomy
The ulnar nerve approaches the medial epicondyle between the medial head of the triceps and the humerus. It then enters the postcondylar groove under the cover of the cubital retinaculum. After leaving the ulnar sulcus, the ulnar nerve passes between the humeral and ulnar heads of the flexor carpi ulnaris (FCU) as it enters the forearm. Osborne’s band, described by Geoffrey Osborne in 1957, is the fibrous continuation of the retinaculum as it approaches the region between the two heads of the FCU [18]. Here, the FCU is invested in a superficial and deep fascial layer. The thickened convergence of these fascial layers is referred to as Osborne’s band. After passing under this band, the nerve pierces the fascia and continues between the FCU and FDS muscles [22].
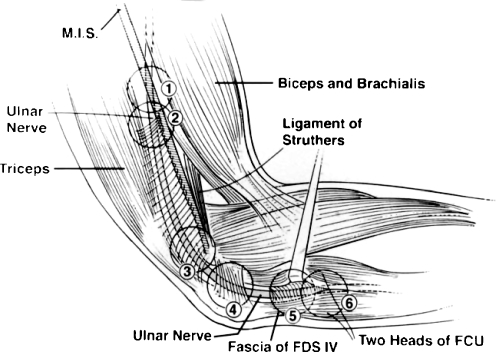
Numerous regions have been proposed as sites of compression for the ulnar nerve about the elbow (Fig. 2).
The region in which the nerve pierces the medial intermuscular septum (MIS) has been offered by several authors as an entrapment point when thin ligamentous bands are present within this zone [12, 27–31].
The arcade of Struthers is a musculotendinous arch often quoted to exist between 3 and 10 cm proximal to the medial humeral epicondyle [12, 26, 29]. Existence of a true “arcade,” however, is controversial, and Mackinnon and Dellon, in over 300 ulnar nerve surgeries never found the band to exist [7]. Despite this controversy, proximal dissection, at least 8 cm, is necessary as recurrence after failed transposition is noted to occur here presumably due to kinking of the nerve after incomplete release of the brachial fascia [18].
The insertion of the medial head of the triceps into the MIS can be a point of compression if the medial head is large [2]. Additionally, the arcade of Struthers, as noted above, has been described to occur as proximally as this point 3 cm from the medial epicondyle [26].
The leading edge of the cubital tunnel retinaculum can constrict the nerve as the elbow flexes and the aponeurotic fascia tightens [2, 32]. Rarely, anconeus epitrochlearis muscle will exist at this site and can stenose the entrance to this tunnel causing compression [7, 10]. Rheumatoid disease and other arthropathies as well as posttraumatic elbow deformities can also lead to constriction in this area [1, 7, 19, 23, 25].
Some authors cite the fascial origin of the flexor digitorum superficialis of the ring finger (FDS IV) as another proposed area of entrapment [15]. Others, including our senior author, include this fascia in the description of Osborne’s band discussed later.
Thickening of the FCU and FDS fascial layers can form a fibrous band at the junction of the two heads of FCU. This is referred to as Osborne’s band and is suspected by many to be the most common culprit in the etiology of cubital tunnel syndrome [8, 21, 33]. Miller localized this site of compression “1.5- to 3.5-cm distal to the medial epicondyle” and cited anatomical and physiological evidence for this conclusion [20]. Although not universally present, Dellon found this band in 73% of 104 dissected specimens [7].
Figure 2.
Proposed points of entrapment along the cubital tunnel. Six proposed sites of ulnar nerve entrapment in the area of the cubital tunnel: (1) the medial intermuscular septum (MIS) where the ulnar nerve pierces the septum; (2) the thickened proximal, leading edge of the arcade of Struthers; (3) the entire arcade of Struthers, transversely attaching the deep fascia of the distal triceps and its tendon of insertion to the medial intermuscular septum; (4) the bony retrocondylar groove and the overlying cubital retinaculum; (5) the fascial origin of the flexor digitorum superficialis (FDS) of the ring finger; and (6) Osborne’s band at the confluence of the flexor carpi ulnaris (FCU) fascial layers and the two heads of the FCU. Reprinted with permission [14, 17].
Materials and Methods
From January 1, 2004 to December 1, 2005, 64 adult patients were diagnosed with cubital tunnel syndrome by a single surgeon. Cubital tunnel syndrome was diagnosed based upon symptoms of numbness, tingling, and/or pain in the ulnar nerve distribution with or without weakness or wasting of the ulnar-innervated intrinsic hand muscles. The study population was limited to those patients with confirmatory electrodiagnostic studies. In addition, patients with clinical or electrodiagnostic evidence of cervical nerve root impingement, those who had prior intervention at the cubital tunnel, and those with evidence for compression at Guyon’s canal were excluded. As part of the physical examination, the scratch collapse test was performed. Subsequently, all of the patients underwent anterior intramuscular transposition of the ulnar nerve by the senior author (S. E. M.). The same procedure was undertaken in all patients and involved a musculofascial lengthening technique with removal of the following structures: the medial intramuscular septum, the fascial septae within the flexor pronator mass, and the common aponeurosis of the flexor carpi ulnaris and the flexor digitorum superficialis [1]. Intraoperative findings were noted and compared with the findings of the preoperative scratch collapse test.
As discussed previously, the SCT is performed with the patient seated facing the examiner. The patient is positioned with his elbows at his side, the palms facing one another and the forearms in parallel. The patient is asked to keep the arms in this position while the examiner, grasping the wrists, applies medially-directed pressure as if to bring the palms together (Fig. 1). This resistance is tested for a baseline comparison. The skin overlying the area of nerve compression is then stroked and, immediately following, medially-directed pressure is again applied to the patient’s wrists. A positive scratch collapse corresponds to a transient decrement in resistance in the ipsilateral extremity. The affected extremity “collapses” against his or her body.
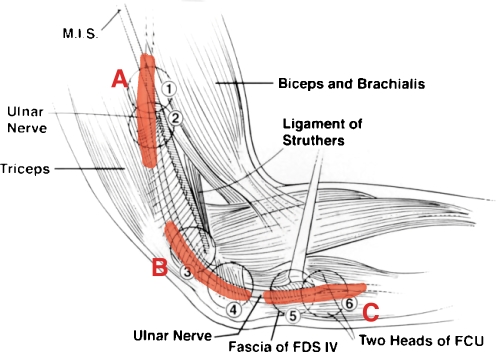
Testing was performed over three distinct areas corresponding to commonly proposed sites of ulnar nerve compression. A proximal segment was selected corresponding to the region where the intermuscular septum is traversed. A medial segment proximal to and across the ulnar groove was then tested overlying the cubital retinaculum. The distal region which was tested corresponded to the junction of the FCU heads (or Osborne’s band) starting about 1–2 cm distal to the medial epicondyle and stroking distally. The patients were scratched over approximately a 2 cm segment along each of the three areas, and results were recorded (Fig. 3).
Figure 3.
Scratch collapse test for cubital tunnel, three subsegments of testing. Three segments of possible entrapment tested in current study: (A) Proximal segment corresponds to area of the distal arcade of Struthers (regions 1 and 2); (B) Middle segment overlies cubital retinaculum (regions 3 and 4; C) Distal segment in area of Osborne’s band (regions 5 and 6). Adapted with permission [14, 17].
Results
Demographic data for all of the patients is presented in Table 2. Forty-four of the 64 patients with cubital tunnel syndrome were found to have a positive scratch collapse test. In all 44 patients in this series, the collapse was reproducible at the distal site of nerve entrapment, corresponding to Osborne’s band. None of the patients collapsed at either of the more proximal sites when the swipe was limited to those segments. Any accidental continuation of these proximal strokes, such as the knuckles or small fingers brushing over the distal site following the intentional scratch, though, could induce a “collapse,” resulting in a false positive.
Table 2.
Demographic data of study group.
| Subjects with cubital tunnel syndrome, n | 64 |
|---|---|
| Men/women, n (%) | 35/29 (55/45) |
| Mean age in years (range) | 49 (24–86) |
| Mean BMI in kg/m2 (range) | 29 (18–45) |
| No. affected hands, dominant/nondominant | 45/41 |
| Mean symptom duration in months | 42 |
| Diabetes mellitus, n (%) | 6 (9) |
| Tobacco use, n (%) | 18 (28) |
| Workers’ compensation, n (%) | 34 (53) |
| Litigation, n (%) | 6 (9) |
BMI body mass index
Reprinted with permission [6]
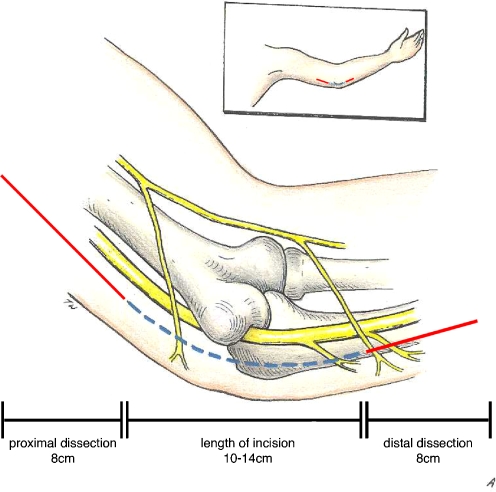
All of the 44 patients with a positive preoperative scratch collapse test were found, intraoperatively, to have thickening of Osborne’s band creating a tight area of nerve compression. With careful inspection of the entire exposed region of the ulnar nerve, this appeared to be the most clearly compressive region along its course in all of these patients. The region of the nerve explored includes the length of nerve from midhumeral level to midforearm level. Figure 4 illustrates our senior author’s preferred surgical incision. Though incision is contained within the area of the cubital retinaculum, proximal dissection at least eight more centimeters is necessary in order to completely release the brachial fascia.
Figure 4.
Surgical dissection for ulnar nerve decompression at the elbow. The figure illustrates our senior authors preferred incision for ulnar nerve decompression. Though the incision is only 10–14 cm, proximal and distal dissection should extend approximately 1 finger-breadth, or 8 cm, beyond this point in order to achieve complete fascial release. Original art by Terry Watkinson.
Discussion
The present observation illustrates the potentially precise localizing ability of this new modality of peripheral nerve examination. Based on the results of this study, the authors believe that the scratch collapse test can precisely localize the site of ulnar nerve entrapment. Anecdotally, we can report that this same effect appears to be demonstrable for most nerves throughout the body from the greater occipital nerve to the tibial nerve in the tarsal tunnel.
Though the exact mechanism of the scratch collapse test is unknown, we believe it may represent a gross physical manifestation of the “cutaneous silent period.” This EMG-demonstrated phenomenon is observed following noxious stimuli. A brief pause of voluntary muscle contraction is demonstrated following stimulation of a cutaneous nerve [24]. The scratch collapse yields a similar reflex response. We propose that as the nervi-nervorum at the site of neuritis are stimulated, an ipsilateral central inhibition is transiently activated. It is not surprising that this response would be most robust at the focus of the neuritis.
The scratch collapse examination shares several features with the cutaneous silent period. Both phenomena occur after a noxious stimulus, are very resistant to habituation, are able to override voluntary muscle contraction, and result in a deferment in resistance in a pattern that corresponds to the withdrawal of the extremity into a position of protection (e.g., in this case, internally rotating the arms in against the body) [9, 11, 13, 16, 17]. From an evolutionary standpoint, such a reflex would be important in survival.
The predominant intraoperative finding of a thickened FCU aponeurosis or Osborne’s band causing the entrapment for the ulnar nerve is not unique to our experience [4, 7, 8, 20–22, 33]. Osborne’s band, while tauter with elbow flexion, represents a good candidate for chronic compression because compression is commonly present at this site even in elbow extension. None of the patients in this series had any anatomical aberrations or elbow deformities that would predispose them to ulnar neuropathy. The study population, therefore, is likely representative of patients with classic cubital tunnel syndrome as described by Osborne in 1957 and probably corresponds to the most common clinical presentation of cubital tunnel syndrome today [18]. It is worth noting that this study population possessed a single common compression site, and therefore, no controls were available with alternative sites of scratch collapse positivity. Additionally, those who have not demonstrated a scratch collapse who did require surgery had the same site of compression. Notwithstanding, we can relate anecdotally that this test has also been useful in identifying different sites of compression and can be particularly useful in a failed transposition. The site of scratch collapse in this situation has been found to correspond with the site of kinking which is generally distant from the site of Osborne’s band.
Although we are not presenting an argument for the simple decompression approach to ulnar neuritis, the published success of this procedure lends further credence to the proposition that Osborne’s band may be the most common culprit in this particular compression neuropathy [4, 7, 8, 20–22, 33, 34]. If Osborne’s band is indeed the sole site of compression in the majority of cases of cubital tunnel syndrome, then any operation (decompression or transposition) that releases this compression point without creating new kink points along the course of the nerve will be effective in treating this disease. Indeed, the cumulative success of all operative methods has been found to be high and similar: simple decompression, 86%; medial epicondylectomy, 89%; intramuscular transposition, 85%; submuscular transposition, 85%; and subcutaneous transposition, 76%. [15] (Fig. 5).
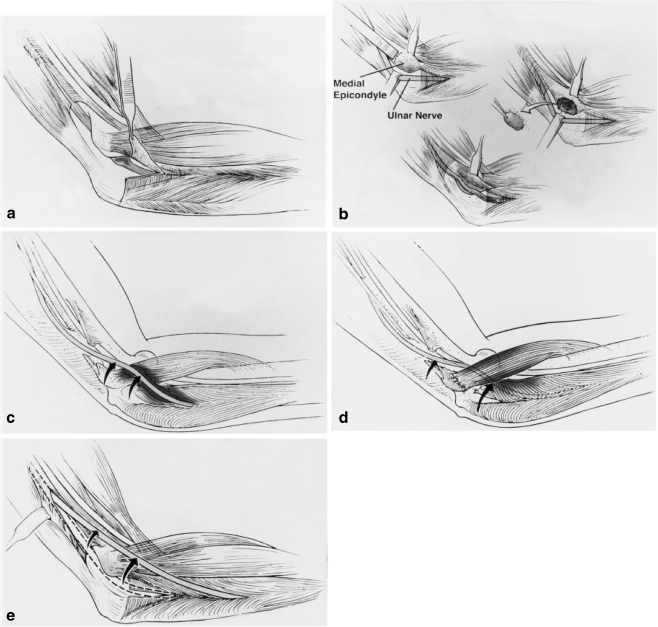
Figure 5.
Surgical procedures for cubital tunnel syndrome. The combined clinical success rates for each of the commonly performed surgical procedures used for cubital tunnel syndrome are similar. a Simple decompression, 86%; b medial epicondylectomy, 89%; c intramuscular transposition, 85%; d submuscular transposition, 85%; e subcutaneous transposition, 76%. It is difficult for the student of peripheral nerve surgery to select a procedure for a specific patient based on these reports alone. Reprinted with permission [14].
Conclusion
The scratch collapse test is a simple physical examination maneuver that has been shown to be similar in sensitivity to other common examination modalities in diagnosing cubital tunnel syndrome. The test offers an advantage over these other tests in that it appears to precisely localize the site of nerve compression. In our study, the proximal forearm was the site which elicited a collapse in all cases of cubital tunnel syndrome, preoperatively. This area corresponded to the site of Osborne’s band, which was found to be the site of nerve compression in all of the patients with a positive preoperative scratch collapse. Although there are clearly cases which fall outside of what was demonstrated in this series, we believe that these findings do indicate the most common clinical scenario. In addition to adding to the clinicians’ armamentarium for diagnosing nerve entrapment syndromes, the scratch collapse test may provide the added benefit of helping to identify those patients most likely to benefit from simple nerve decompression versus those who require a more extensive operation.
Acknowledgment
We would like to thank Brendan Mackinnon-Patterson who did the chart reviews and statistics for this study.
Contributor Information
Justin M. Brown, Email: brownjm@nsurg.wustl.edu
Maristella S. Evangelista, Phone: 714-456-5253, Email: evangelm@uci.edu
References
- 1.Adson AL. The surgical treatment of progressive ulnar paralysis. Minn Med. 1918;1:455–460. [Google Scholar]
- 2.Apfelberg DB, Larson SJ. Dynamic anatomy of the ulnar nerve at the elbow. Plast Reconstr Surg. 1973;51:76–81. doi: 10.1097/00006534-197301000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Bartels RHMA, Menovsky T, Overbeeke JJ, et al. Surgical management of ulnar nerve compression at the elbow: an analysis of the literature. J Neurosurg. 1998;89:722–727. doi: 10.3171/jns.1998.89.5.0722. [DOI] [PubMed] [Google Scholar]
- 4.Bartels RHMA, Verhagen WIM, Wilt GJ, et al. Prospective randomized controlled study comparing simple decompression versus anterior subcutaneous transposition for idiopathic neuropathy of the ulnar nerve at the elbow: part 1. Neurosurgery. 2005;56:522–530. doi: 10.1227/01.NEU.0000154131.01167.03. [DOI] [PubMed] [Google Scholar]
- 5.Beck JL. The P.A.N.E. process: basic principles and the first three tests. Practical application of neuropostural evaluations. Pract Pain Manage. 2008;8(7):47–53. [Google Scholar]
- 6.Cheng CJ, Mackinnon-Patterson B, Beck JL, Mackinnon SE. Scratch collapse test for evaluation of carpal and cubital tunnel syndrome. J Hand Surg [Am] 2008;33(9):1518–1524. doi: 10.1016/j.jhsa.2008.05.022. [DOI] [PubMed] [Google Scholar]
- 7.Dellon AL. Musculotendinous variations about the medial humeral epicondyle. J Hand Surg. 1986;11B:175–181. doi: 10.1016/0266-7681(86)90254-8. [DOI] [PubMed] [Google Scholar]
- 8.Feindel W, Stratford J. Cubital tunnel compression in tardy ulnar palsy. CMAJ. 1958;78:351–353. [PMC free article] [PubMed] [Google Scholar]
- 9.Floeter MK, Gerloff C, Kouri J, Hallett M. Cutaneous withdrawal reflexes of the upper extremity. Muscle Nerve. 1998;21:591–598. doi: 10.1002/(SICI)1097-4598(199805)21:5<591::AID-MUS5>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 10.Hirasawa Y, Sawamura H, Sakakida K. Entrapment neuropathy due to bilateral epitrochleoanconeus muscles: a case report. J Hand Surg. 1979;4:181–184. doi: 10.1016/s0363-5023(79)80139-2. [DOI] [PubMed] [Google Scholar]
- 11.Inghilleri M, Conte A, Frasca V, Berardelli A, Manfredi M, Cruccu G. Is the cutaneous silent period an opiate-sensitive nociceptive reflex? Muscle Nerve. 2002;25:695–699. doi: 10.1002/mus.10101. [DOI] [PubMed] [Google Scholar]
- 12.Kane E, Kaplan EB, Spinner M. Observations on the course of the ulnar nerve in the arm. Ann Chir. 1973;27:470–496. [PubMed] [Google Scholar]
- 13.Kaneko K, Kawai S, Taguchi T, Fuchigami Y, Yonemura H, Fujimoto H. Cortical motor neuron excitability during cutaneous silent period. Electroencephalogr Clin Neurophysiol. 1998;109:364–368. doi: 10.1016/S0924-980X(98)00031-9. [DOI] [PubMed] [Google Scholar]
- 14.Kleinman WB. Revision ulnar neuroplasty. Hand Clin. 1994;10(3):461–477. [PubMed] [Google Scholar]
- 15.Kleinman WB. Cubital tunnel syndrome: anterior transposition as a logical approach to complete nerve decompression. J Hand Surg. 1999;24(5):886–897. doi: 10.1053/jhsu.1999.0886. [DOI] [PubMed] [Google Scholar]
- 16.Kofler M, Glocker FX, Leis AA, Seifert C, Wissel J, Kronenberg MF, Fuhr P. Modulation of upper extremity motoneuron excitability following noxious finger tip stimulation in man: a study with transcranial magnetic stimulation. Neurosci Lett. 1998;246:97–100. doi: 10.1016/S0304-3940(98)00243-2. [DOI] [PubMed] [Google Scholar]
- 17.Kofler M, Fuhr P, Leis AA, Glocker FX, Kronenberg MF, Wissel J, Stetkarova I. Modulation of upper extremity motor evoked potentials by cutaneous afferents in humans. Clin Neurophysiol. 2001;112:1053–1063. doi: 10.1016/S1388-2457(01)00540-5. [DOI] [PubMed] [Google Scholar]
- 18.MacKinnon SE, Dellon AL. Ulnar nerve entrapment at the elbow. In: MacKinnon SE, Dellon AL, editors. Surgery of the peripheral nerve. New York: Thieme Medical Publishers Inc; 1988. [Google Scholar]
- 19.McGowan AJ. The results of transposition of the ulnar nerve for traumatic ulnar neuritis. J Bone Joint Surg. 1950;32B:293–301. doi: 10.1302/0301-620X.32B3.293. [DOI] [PubMed] [Google Scholar]
- 20.Miller RG. The cubital tunnel syndrome: diagnosis and precise localization. Ann Neurol. 1979;6:56–59. doi: 10.1002/ana.410060113. [DOI] [PubMed] [Google Scholar]
- 21.Osborne GV. The surgical treatment of tardy ulnar neuritis. J Bone Joint Surg Br. 1957;39B:782. [Google Scholar]
- 22.Polatsch DB, Melone CP, Beldner S, Incorvaia A. Ulnar nerve anatomy. Hand Clin. 2007;23:283–289. doi: 10.1016/j.hcl.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 23.Richards RL. Traumatic ulnar neuritis: the results of anterior transposition of the ulnar nerve. Edinb Med J. 1945;52:14–21. [Google Scholar]
- 24.Shahani BT, Young RR. Studies of the normal human silent period. In: Desmedt JE, editor. New developments in electromyography and clinical neurophysiology. Basel: Karger; 1973. pp. 589–602. [Google Scholar]
- 25.Sheldon WD. Tardy palsy of the ulnar nerve. Med Clin North Am. 1921;5:499–509. [Google Scholar]
- 26.Siquera MG, Martins RS. The controversial arcade of Struthers. Surg Neurol. 2005;64(Suppl 1:S1):17–20. doi: 10.1016/j.surneu.2005.04.017. [DOI] [PubMed] [Google Scholar]
- 27.Spinner M. Management of nerve compression lesions in the upper extremity. In: Omer GE Jr, Spinner M, editors. Management of peripheral nerve problems. Philadelphia: WB Saunders Co; 1980. [Google Scholar]
- 28.Spinner M, Kaplan EB. The relationship of the ulnar nerve to the medial intermuscular septum in the arm and its clinical significance. Hand. 1976;8:239–242. doi: 10.1016/0072-968X(76)90008-5. [DOI] [PubMed] [Google Scholar]
- 29.Spinner M, Spencer PS. Nerve compression lesions of the upper extremity: a clinical and experimental review. Clin Orthop Relat Res. 1974;104:46–68. doi: 10.1097/00003086-197410000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Struthers J. On a peculiarity of the humerus and humeral artery. Month J Med Sci. 1848;28:264–267. doi: 10.1016/j.jhsb.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 31.Stuthers J. On some points in the abnormal anatomy of the arm. Br For Med Chir Rev. 1854;14:170–179. [PMC free article] [PubMed] [Google Scholar]
- 32.Vanderpool DW, Chalmers J, Lamb DW, Whistson TB. Peripheral compression lesions of the ulnar nerve. J Bone Joint Surg. 1968;50B:792–802. [PubMed] [Google Scholar]
- 33.Wadsworth TG. The external compression syndrome of the ulnar nerve at the cubital tunnel. Clin Orthop Relat Res. 1977;124:189–204. [PubMed] [Google Scholar]
- 34.Zlowodzki M, Chan S, Bhandari M, Kalliainen L, Schubert W. Anterior transposition compared with simple decompression for treatment of cubital tunnel syndrome. A meta-analysis of randomized, controlled trials. J Bone Joint Surg Am. 2007;89:2591–2598. doi: 10.2106/JBJS.G.00183. [DOI] [PubMed] [Google Scholar]
Further Reading
- 35.Mackinnon SE, Novak CB. Operative findings in reoperation of patients with cubital tunnel syndrome. Hand (N Y) 2007;2:137–143. doi: 10.1007/s11552-007-9037-3. [DOI] [PMC free article] [PubMed] [Google Scholar]