Abstract
Anatomic variation of the trapeziometacarpal joint stabilizing structures is one of the concepts proposed to explain the pathogenesis of trapeziometacarpal arthritis. We undertook this study to test the hypothesis that septation of the first extensor compartment or variation of the abductor pollicis longus (APL) tendon (supernumerary insertions) are more frequently associated with the progression or severity of trapeziometacarpal arthritis. Septation within the first extensor compartment was significantly associated with trapeziometacarpal arthritis (p = 0.013), whereas supernumerary APL insertions (trapezium or thenar) did not reveal a significant association (p = 0.811 and p = 0.937, respectively). The results of this study do not support a role for variations of APL tendon insertions in trapeziometacarpal arthritis. Yet, the presence of septation within the first extensor compartment may play an important role in the pathogenesis of trapeziometacarpal arthritis.
Keywords: First extensor compartment, Septum, Supernumerary APL tendons, Trapeziometacarpal arthritis
Introduction
The trapeziometacarpal joint is the second most common hand structure affected by arthritis [25], but due to the unique features of thumb range of motion, it represents the most common site for surgical treatment [17]. Numerous hypotheses have been proposed to explain the pathogenesis of trapeziometacarpal arthritis including anatomic variation of joint structures, ligaments or supernumerary APL tendon insertions [3, 5, 6, 18–21, 30]. However, the etiology remains unclear and one of the most intriguing theories is probably the role of APL supernumerary slips in the initiation and progression of the disease. Brunelli and Brunelli [5] suggested that the absence of the trapezial supernumerary slip of APL predisposes to trapeziometacarpal arthritis, whereas Zancolli [30] reported good postoperative results with tenotomy of supernumerary APL tendons. Even though other cadaveric studies failed to support a role for the supernumerary APL insertions in the etiology of trapeziometacarpal arthritis [3, 19–21], anatomic variation of the APL remains a practical and attractive theory.
During the surgical treatment of trapeziometacarpal arthritis, we often have noticed a septum within the first extensor compartment in the absence of any other hand complaint. However, anatomic variation of the first extensor compartment (septation) has been frequently associated with the development and progression of a distinct entity, De Quervain's tenosynovitis, where narrowing of the extensor pollicis brevis tunnel leads to impaired gliding resistance [12].
The presence of a septum between the two tendons of the first extensor compartment divides it into two separate narrowed tunnels. We wanted to test the hypothesis that a septum more frequently associates with trapeziometacarpal arthritis on the assumption that a narrowed APL tunnel would enhance the resistance of different APL tendon slips excursion [12] and subsequently increase compressive and shearing forces between the trapezium and thumb MC, predisposing to trapeziometacarpal arthritis. Therefore, we aimed to test if a septum within the first extensor compartment more commonly associates with trapeziometacarpal arthritis. Our secondary aim was to test the association between trapeziometacarpal arthritis and distal insertions of the supernumerary APL slips.
Materials and Methods
The study was conducted in the anatomy department at the Michigan State University. Fifty fresh and frozen cadaveric hands with absent signs of pre-mortem or post-mortem procedures were dissected. Of these, 48 hands were matched (24 specimens) and two were unmatched (two specimens) resulting in 13 men with a mean age of 78 years (49–91 years) and 13 women with a mean age of 71 years (52–94 years).
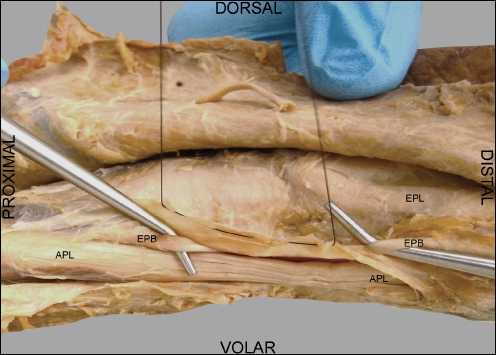
The dissections were performed starting with the proximal border of the extensor retinaculum and ending with the interphalangeal joint of the thumb. After the skin and fat tissue were removed, the extensor retinaculum was exposed and the presence of both tendons of the first extensor compartment was identified proximally at the entrance in the extensor retinaculum and distally, at the exit to the base of the thumb. A longitudinal incision was performed on the radial side of the first extensor compartment on its entire length, exposing the APL tendon in the extensor retinaculum. The roof of the first extensor compartment was reflected ulnarly in order to expose the tendons. Septation was noticed as a thick and well-defined fibrous ridge arising from the floor of the extensor retinaculum to the roof and separating the tendons into two separate fibrous compartments (Fig. 1). Furthermore, the septum was categorized into complete or partial based on whether the entire length or only the distal part of the first extensor compartment was divided.
Figure 1.
Radial view of the left hand of a specimen with full septation of the first extensor compartment. Both tendons of the compartment are in separate tunnels. The margin of the first extensor compartment was dorsally reflected (black suture) to visualize the full separation of the tendons.
Within the first extensor compartment, we aimed to determine the number of slips of the APL tendon. However, since the APL slips intertwine within the first extensor compartment, the number of APL slips being different at the proximal and distal part of the extensor retinaculum, we recorded only the number of distinct tendons traveling within the first extensor compartment. Similarly, the number of APL slips in the first extensor compartment was different from the number of distal insertions of the tendon since multiple APL slips can converge into a single distal insertion or can diverge into separate distal insertions within the compartment. Therefore, the distal insertions of the APL tendon were recorded and categorized based on the anatomic structure of insertion. In order to minimize the bias of knowing ahead about the presence or absence of a septum, the dissections at the joint level and assessment of arthritic changes were performed by different members of the team.
At the end of the dissection, after the trapeziometacarpal joint was hinged open, the degenerative changes were macroscopically evaluated. Subsequently, arthritis was staged as mild–moderate (25–74% trapeziometacarpal surface involvement) or advanced (75–100% trapeziometacarpal surface involvement). Assessment of degenerative changes of the scaphotrapezial joint was also performed and the dissection concluded with the identification of the thumb MC osteophyte, which represents a particular prominence of the ulnar base of the thumb MC, located between the thumb and second metacarpal [16, 29].
Descriptive statistics are presented as frequencies and relative frequency for categorical variables, and means and range for continuous variables. Because of the inclusion of bilateral hands, a generalized estimating equation adjustment was used with the ordinal logistic regression to analyze the associations between disease presence or severity and variables like age, gender, type of distal insertions of the APL tendon, septation of the first extensor compartment, scaphotrapezial joint arthritis or thumb MC osteophyte.
Results
The overall frequency of septation (partial or complete) within the first extensor compartment was 72% (36/50 dissected specimens) and in 71.4% of the cases the septum was bilateral. Median number of supernumerary APL distal insertions was one (one insertion 72%, two insertions 24%, and three insertions 2%). Other anatomic characteristics with regards to the type of distal APL insertions are specified in Table 1.
Table 1.
Distribution of the first extensor compartment septation and distal insertions of the APL tendon for the dissected specimens.
| Trapeziometacarpal arthritis | Septum (n = 36; 72%) | APL distal insertions | |||
|---|---|---|---|---|---|
| Base of thumb MC (n = 50) | Trapezium (n = 38) | APB (n = 19) | Opponens pollicis (n = 3) | ||
| No arthritis | 1 | 5 | 2 | 3 | 1 |
| Mild–moderate arthritis | 20 | 22 | 19 | 6 | 1 |
| Advanced arthritis | 15 | 23 | 17 | 10 | 1 |
Septation of the first extensor compartment was significantly associated with the presence or severity of the disease (p = 0.013). Age of the specimens in the group with arthritis and no arthritis was 52–91 and 49–80 years old, respectively. Age was associated with the severity of the trapeziometacarpal arthritis (p = 0.001) whereas gender did not demonstrate a significant trend (p = 0.415). At the same time, supernumerary APL insertions (trapezium or thenar) were not associated with the presence or severity of the disease (p = 0.811 and p = 0.937, respectively). In terms of accompanying degenerative changes, the scaphotrapezial cartilage damage and the thumb MC osteophyte significantly associated with the severity of the disease (p = 0.034, OR 5.7, 95%CI 1.1–28.5 and p = 0.043, OR 4.9, 95%CI 1–23.7, respectively). Distribution of the scaphotrapezial degeneration and the thumb MC osteophyte in trapeziometacarpal arthritis is illustrated in Table 2.
Table 2.
Frequency of scaphotrapezial arthritis and thumb MC osteophyte.
| Trapeziometacarpal arthritis | Scaphotrapezial arthritis | Thumb MC osteophyte |
|---|---|---|
| No arthritis | 0/5 (0%) | 0/5 (0%) |
| Mild–moderate arthritis | 10/22 (45.4%) | 6/22 (27.2%) |
| Advanced arthritis | 18/23 (81.8%) | 14/23 (63.6%) |
Discussion
Classically, according to the human anatomy texts, the insertion of the APL tendon is considered at the base of the thumb MC. Numerous authors described variations of the APL tendon insertions, APL being considered one of the most variable anatomic tendinous structures [3, 5, 9, 10, 13, 14, 19–21, 30]. A review of the cadaveric studies in the literature identifies a single APL insertion on the base of the thumb MC in 2–28% of the dissected specimens (Table 3). Supernumerary slips, which are defined as distal APL insertions in addition to the classical thumb base insertion, are encountered in 72–98% of the cases (Table 4) [3, 5, 9, 13, 20, 21]. As our study also demonstrates, the common APL insertion profile appears to be as one constant distal insertion on the base of the thumb MC and variable supernumerary insertions on different surrounding structures. Supernumerary tendons are actually the rule rather than the exception and therefore, on dissection/surgery we should expect to find at least two distinct distal insertions of the APL in more than 70% of the cases.
Table 3.
Frequency and distribution of supernumerary APL tendon slips in the literature.
| Study | Singular insertion on thumb metacarpal base | Number of supernumerary APL slips | ||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | ||
| Lacey et al. [13] | 7/38 (18%) | 19/38 (50%) | 10/38 (26%) | 2/38 (5%) | ||
| Jackson et al. [9] | 83/300 (28%) | 181/300 (60%) | 29/300 (10%) | 6/300 (2%) | 1/300 (0.3%) | |
| Roush et al. [20] | 2/61 (3%) | 12/61 (20%) | 41/61 (67%) | 6/61 (10%) | ||
| Schulz et al. [21] | 3/73 (4%) | 36/73 (49%) | 26/73 (36%) | 5/73 (7%) | 2/73 (3%) | 1/73 (1%) |
| Bouchlis et al. [3] | 7/104 (7%) | |||||
| Brunelli and Brunelli [5] | 2/100 (2%) | 2/100 (2%) | 13/100 (13%) | 30/100 (30%) | 49/100 (49%) | 4/100 (4%) |
| Present study | 1/50 (2%) | 36/50 (72%) | 12/50 (24%) | 1/50 (2%) | ||
Table 4.
Frequency and distribution of supernumerary APL tendon insertions in the literature.
| Study | Base of thumb MC | Supernumerary APL insertions | |
|---|---|---|---|
| Trapezium | Thenar structures | ||
| Lacey et al. [13] | 38/38 (100%) | 16/38 (42%) | 28/38 (73%) |
| Roush et al. [20] | 61/61 (100%) | 55/61 (90%) | 48/61 (79%) |
| Schulz et al. [21] | 73/73 (100%) | 24/73 (33%) | 31/73 (43%) |
| Bouchlis et al. [3] | 104/104 (100%) | 70/104 (70%) | 43/104 (42%) |
| Brunelli and Brunelli [5] | 100/100 (100%) | 71/100 (71%) | 75/100 (75%) |
| Roh et al. [19] | 68/68 (100%) | 35/68 (51%) | |
| Zancolli [30] | 43/43 (100%) | 13/43 (32%) | 35/43 (83%) |
| Present study | 50/50 (100%) | 37/50 (76%) | 22/50 (44%) |
With regards to the characteristics of the supernumerary insertions of the APL tendon, a review of the literature including our current study reveals a difference of opinion about the site of the most common supernumerary APL distal insertion [3, 5, 13, 19–21, 30]. We found that trapezium was the most common site for supernumerary tendon insertion in our cadaver study (76%), whereas the thenar structures were second (44%) to the trapezial insertion. The opponens pollicis and abductor pollicis brevis muscles, as well as their fascia are the structures included in the thenar group. In the literature, only few studies make a clear distinction between a digastric opponens or abductor pollicis and a regular insertion on those muscles. This could account for the existent dichotomy with regards to the most common supernumerary distal insertion of the APL tendon. Yet, in seven out of ten cases, we should expect to find a minimum of two separate insertions for the APL tendon, one constant at the MC base and at least one supernumerary insertion located either at the trapezium or thenar musculature.
During APL suspension arthroplasty for the trapeziometacarpal arthritis, the first extensor compartment is dissected in order to allow the harvest of a slip of the APL. As we commonly perform this type of procedure in our practice, we have noticed a high frequency of septum within the first extensor compartment in patients with trapeziometacarpal arthritis but without signs of De Quervain's tenosynovitis. Therefore, we wanted to test the hypothesis that there is an association between the presence of a septum within the first extensor compartment and trapeziometacarpal arthritis.
In the current study, septation of the first extensor compartment proved to be significantly associated with the presence of arthritis (p = 0.013), patients being more likely to have disease if septum is present. There is no literature data with regards to this association but there is abundant evidence for the correlation between septum and De Quervain's tenosynovitis [2, 9, 15, 28]. Finkelstein [7] was one of the first to notice the increased association between septum and De Quervain's tenosynovitis and it was based on personal surgical experience. Many more research studies followed and confirmed this association, but even after more than 70 years since this correlation has been noticed, the literature is still scarce with regards to the underlying mechanism [12].
Both these associations have been observed through the experience of surgical treatments for the respective diseases and there is no scientific proof for their mechanisms but only assumptions. It is possible that the association of septum–De Quervain's tenosynovitis was discovered first since the surgical intervention for De Quervain's tenosynovitis was initially done in 1895 by De Quervain himself [7], long time before the APL suspension arthroplasty for trapeziometacarpal arthritis would be performed [22]. It would probably not be surprising that the same anatomic variation (septum of the first extensor compartment) would play an important role in two separate pathologic entities.
There is substantial electromyographic and anatomic evidence for independent function of the APL slips. Multiple muscle bellies of the APL tendon are innervated by separate branches of the posterior interosseous nerve [26, 27]. The different slips of the APL tendon can be grouped into a superficial and a deep group, inserting on the thumb MC or trapezium and thenar structures, respectively [11]. There is no connection between the fibers of the superficial and deep divisions and a large bursa between the two groups of tendons can be found [11, 25] suggesting separate functioning of the various divisions [11]. Van Oudenaarde [25] suggested that the deep division of the APL is important to support the trapezium as a platform upon which the thumb MC is extended by the superficial division of the APL. Therefore, the presence of a septum between the two tendons within the first extensor compartment narrows the APL tunnel and the intertendinous shifting in the extensor compartment, normally occurring during independent function of the APL divisions, may be impeded. Subsequently, the deep division of the APL, which acts as support for the trapezium during regular isometric contraction [25], may destabilize the synergic action of thumb MC and trapezium, creating shearing forces between the thumb MC and trapezium. Yet, more research is necessary to characterize the mechanisms behind the stability of the thumb basal joint.
Our study found a significant association between severity of the disease and age of the specimens, which is in accordance with the majority of the literature studies. We would also expect the prevalence of arthritis to be higher in the female specimens, a fact that would support hormonal imbalance as a potential cause of arthritis. However, presence or severity of the disease did not show any difference with regards to the gender of the specimens, results that are similar with other studies [1, 19]. We also have not been able to demonstrate an association between supernumerary APL distal insertions and trapeziometacarpal arthritis and therefore, our results rejected the hypothesis with regards to the role of supernumerary APL slips in the etiology of this disease.
During our dissections, we aimed to characterize the frequency of scaphotrapezial joint degenerative changes. We found that 45.4% of the mild–moderate trapezio-metecarpal arthritis and 81.8% of the advanced trapeziometacarpal arthritis had simultaneous scaphotrapezial changes. It was almost six times more likely to find scaphotrapezial degenerative changes in advanced rather than in early trapeziometacarpal arthritis. Our findings are in accordance to similar studies where significant involvement of scaphotrapezial and scapho-trapezoidal degenerative changes were found not only in severe trapeziometacarpal arthritis but also in early stages of the disease [1, 4, 16]. As suggested by Brown et al. [4] postoperative pain with surgical intervention for trapeziometacarpal arthritis may be attributed to residual degenerative changes in the surrounding joints.
In the study conducted by Sirotakova et al., postoperative residual pain was owed to the failure to address the thumb MC osteophyte at the time of surgery [23]. It was not surprising since we found the thumb MC osteophyte in 63.6% of the advanced stages of the disease. Moreover, even though it was five times more likely to find the osteophyte in advanced stages of trapeziometacarpal arthritis, in a significant number of cases the osteophyte was present also with early arthritic changes (27.2%). Therefore, regardless of the stage of trapeziometacarpal arthritis, it would be advisable to identify any concurrent scaphotrapezial changes or osteophytes at the thumb MC, which could dictate a different approach towards the treatment of this disease.
The limitations of our study are mainly due to its cadaveric design. A direct correlation of our findings with symptomatic arthritis of the thumb could not be made. As with any cadaveric study, the number of patients in the young population was limited [8, 19–21]. As arthritis strongly correlates with age, the number of unaffected hands was limited as well. However, by adjusting the comparisons to the age and gender of the specimens, some of these impediments were controlled.
To our knowledge, we demonstrated, for the first time, an association between septation within the first extensor compartment and trapeziometacarpal arthritis. To what extent this anatomic variation contributes to the development and progression of trapeziometacarpal arthritis remains to be investigated.
References
- 1.Bade H, Koebke J. Arthrosis in the peritrapezial joints of the hand. Surg Radiol Anat. 1996;18(3):209–214. doi: 10.1007/BF02346129. [DOI] [PubMed] [Google Scholar]
- 2.Bahm J, Szabo Z, Foucher G. The anatomy of de Quervain's disease. A study of operative findings. Int Orthop. 1995;19(4):209–211. doi: 10.1007/BF00185223. [DOI] [PubMed] [Google Scholar]
- 3.Bouchlis G, Bhatia A, Asfazadourian H, Touam C, Vacher C, Oberlin C. Distal insertions of abductor pollicis longus muscle and arthritis of the first carpometacarpal joint in 104 dissections. Ann Chir Main Memb Super. 1997;16(4):326–338. doi: 10.1016/S0753-9053(97)80047-6. [DOI] [PubMed] [Google Scholar]
- 4.Brown GD, 3rd, Roh MS, Strauch RJ, Rosenwasser MP, Ateshian GA, Mow VC. Radiography and visual pathology of the osteoarthritic scaphotrapezio-trapezoidal joint, and its relationship to trapeziometacarpal osteoarthritis. J Hand Surg [Am] 2003;28(5):739–743. doi: 10.1016/S0363-5023(03)00258-2. [DOI] [PubMed] [Google Scholar]
- 5.Brunelli GA, Brunelli GR. Anatomical study of distal insertion of the abductor pollicis longus. Concept of a new musculo-tendinous unit: the abductor carpi muscle. Ann Chir Main Memb Super. 1991;10(6):569–576. doi: 10.1016/S0753-9053(05)80330-8. [DOI] [PubMed] [Google Scholar]
- 6.Eaton RG, Littler JW. Ligament reconstruction for the painful thumb carpometacarpal joint. J Bone Jt Surg Am. 1973;55(8):1655–1666. [PubMed] [Google Scholar]
- 7.Finkelstein H. Stenosing tendovaginitis at the radial styloid process. J Bone Jt Surg Am. 1930;12:509–540. [Google Scholar]
- 8.Giles KW. Anatomical variations affecting the surgery of de Quervain's disease. J Bone Jt Surg Br. 1960;42-B:352–355. doi: 10.1302/0301-620X.42B2.352. [DOI] [PubMed] [Google Scholar]
- 9.Jackson WT, Viegas SF, Coon TM, Stimpson KD, Frogameni AD, Simpson JM. Anatomical variations in the first extensor compartment of the wrist. A clinical and anatomical study. J Bone Jt Surg Am. 1986;68(6):923–926. [PubMed] [Google Scholar]
- 10.Kaarela O, Raatikainen T. Abductor pollicis longus tendon interposition arthroplasty for carpometacarpal osteoarthritis of the thumb. J Hand Surg [Am] 1999;24(3):469–475. doi: 10.1053/jhsu.1999.0469. [DOI] [PubMed] [Google Scholar]
- 11.Kauer JM. Functional anatomy of the carpometacarpal joint of the thumb. Clin Orthop Relat Res. 1987;220:7–13. [PubMed] [Google Scholar]
- 12.Kutsumi K, Amadio PC, Zhao C, Zobitz ME, An KN. Gliding resistance of the extensor pollicis brevis tendon and abductor pollicis longus tendon within the first dorsal compartment in fixed wrist positions. J Orthop Res. 2005;23(2):243–248. doi: 10.1016/j.orthres.2004.06.014. [DOI] [PubMed] [Google Scholar]
- 13.Lacey T, II, Goldstein LA, Tobin CE. Anatomical and clinical study of the variations in the insertions of the abductor pollices longus tendon, associated with stenosing tendovaginitis. J Bone Jt Surg Am. 1951;33-A(2):347–350. [PubMed] [Google Scholar]
- 14.Loomis LK. Variations of stenosing tenosynovitis at the radial styloid process. J Bone Jt Surg Am. 1951;33-A(2):340–346. [PubMed] [Google Scholar]
- 15.Nagaoka M, Matsuzaki H, Suzuki T. Ultrasonographic examination of de Quervain's disease. J Orthop Sci. 2000;5(2):96–99. doi: 10.1007/s007760050134. [DOI] [PubMed] [Google Scholar]
- 16.North ER, Eaton RG. Degenerative joint disease of the trapezium: a comparative radiographic and anatomic study. J Hand Surg [Am] 1983;8(2):160–166. doi: 10.1016/s0363-5023(83)80008-2. [DOI] [PubMed] [Google Scholar]
- 17.Pellegrini VD., Jr Osteoarthritis at the base of the thumb. Orthop Clin North Am. 1992;23(1):83–102. [PubMed] [Google Scholar]
- 18.Pellegrini VD., Jr Osteoarthritis of the trapeziometacarpal joint: the pathophysiology of articular cartilage degeneration. I. Anatomy and pathology of the aging joint. J Hand Surg [Am] 1991;16(6):967–974. doi: 10.1016/S0363-5023(10)80054-1. [DOI] [PubMed] [Google Scholar]
- 19.Roh MS, Strauch RJ, Xu L, Rosenwasser MP, Pawluk RJ, Mow VC. Thenar insertion of abductor pollicis longus accessory tendons and thumb carpometacarpal osteoarthritis. J Hand Surg [Am] 2000;25(3):458–463. doi: 10.1053/jhsu.2000.6463. [DOI] [PubMed] [Google Scholar]
- 20.Roush TF, Aldridge JM, Berger RA, Rizzo M. No correlation between trapeziometacarpal arthritis and abductor pollicis longus insertion. Clin Orthop Relat Res. 2005;434:138–142. doi: 10.1097/01.blo.0000154180.33471.73. [DOI] [PubMed] [Google Scholar]
- 21.Schulz CU, Anetzberger H, Pfahler M, Maier M, Refior HJ. The relation between primary osteoarthritis of the trapeziometacarpal joint and supernumerary slips of the abductor pollicis longus tendon. J Hand Surg [Br] 2002;27(3):238–241. doi: 10.1054/jhsb.2002.0765. [DOI] [PubMed] [Google Scholar]
- 22.Sigfusson R, Lundborg G. Abductor pollicis longus tendon arthroplasty for treatment of arthrosis in the first carpometacarpal joint. Scand J Plast Reconstr Surg Hand Surg. 1991;25(1):73–77. doi: 10.3109/02844319109034926. [DOI] [PubMed] [Google Scholar]
- 23.Sirotakova M, Figus A, Elliot D. A new abductor pollicis longus suspension arthroplasty. J Hand Surg [Am] 2007;32(1):12–22. doi: 10.1016/j.jhsa.2006.10.016. [DOI] [PubMed] [Google Scholar]
- 24.Swanson AB, Swanson GD. Osteoarthritis in the hand. J Hand Surg [Am] 1983;8(5):669–675. doi: 10.1016/s0363-5023(83)80242-1. [DOI] [PubMed] [Google Scholar]
- 25.Oudenaarde E. Structure and function of the abductor pollicis longus muscle. J Anat. 1991;174:221–227. [PMC free article] [PubMed] [Google Scholar]
- 26.Oudenaarde E, Oostendorp R. Significance of the innervation pattern of the human abductor pollicis longus muscle. J Anat. 1992;181(Pt 1):155–159. [PMC free article] [PubMed] [Google Scholar]
- 27.Oudenaarde E, Oostendorp RA. Functional relationship between the abductor pollicis longus and abductor pollicis brevis muscles: an EMG analysis. J Anat. 1995;186(Pt 3):509–515. [PMC free article] [PubMed] [Google Scholar]
- 28.Visuthikosol V, Chanyasawat S. Surgical treatment of de Quervain's diseases: a clinical review of 42 cases. J Med Assoc Thail. 1988;71(11):637–639. [PubMed] [Google Scholar]
- 29.Watson H, Weinzweig J. The Wrist. Carpometacarpal tendon arthroplasty. In: Watson HK, Weinzweig J, editors. The wrist. Philadelphia: Lippincott Williams and Wilkins; 2001. pp. 797–802. [Google Scholar]
- 30.Zancolli EA. The trapeziometacarpal joint. Tenotomy of the accessory tendons in early osteoarthritis. Hand Clin. 2001;17(1):13–43. [PubMed] [Google Scholar]