Abstract
Background/Aims
Acute kidney injury (AKI) is a common and serious complication in critically ill patients, especially in the intensive care unit (ICU). The present study was performed to evaluate the occurrence rate of AKI using the RIFLE (increasing severity classes risk, injury, and failure, and the two outcome classes loss and end-stage kidney disease) classification, to define factors associated with AKI and hospital mortality.
Methods
We performed a retrospective study of all ICU patients over a 6-month period at Keimyung University Dongsan Hospital, Daegu, Korea. AKI was evaluated according to the RIFLE classification.
Results
AKI occurred in 156 of the 378 patients (41.3%) during their ICU stay, with maximum RIFLE-R, I, and F in 13.8%, 12.4%, and 15.1%, respectively. In univariate analysis, the proportion of medical admission and maximum Sequential Organ Failure Assessment (SOFA) score (SOFAmax) were significantly higher in patients with AKI than in those without. However, these factors did not remain significant in a multivariate analysis. The overall mortality rate of ICU patients was 25.7%. In multivariate analysis, mean age, occurrence of AKI, SOFAmax score, pulmonary disease, and malignancy were independent risk factors for hospital mortality.
Conclusions
In these ICU patients, AKI is associated with increased hospital mortality. The RIFLE classification is a simple and useful clinical tool to detect and stratify the severity of AKI, and may aid in the prediction of outcome.
Keywords: Kidney failure, Intensive care units, Risk factors
INTRODUCTION
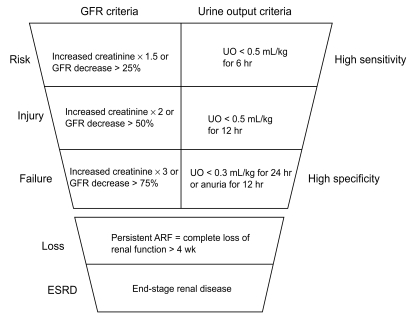
Acute kidney injury (AKI) is a common and serious complication in critically ill patients. The mortality rate in AKI patients remains high despite significant advances in medical care [1-4]. Recently, the Acute Dialysis Quality Initiative (ADQI) work group, comprised of experts in the fields of nephrology and critical care medicine, proposed a multilevel classification system for AKI, the "RIFLE" classification [5], which stands for the increasing severity classes Risk, Injury, and Failure, and the two outcome classes Loss and End-stage kidney disease (Fig. 1). Several studies have shown the RIFLE classification to be a simple, readily available clinical tool to classify acute kidney injury in different populations [6].
Figure 1.
The risk, injury, failure, and the two outcome classes loss and end-stage kidney disease (RIFLE) classification separates criteria for serum creatinine and urine output. GFR, glomerular filtration rate; UO, urine output; ARF, acute renal failure.
In addition to the RIFLE classification, several instruments for scoring illness severity, such as the Sequential Organ Failure Assessment (SOFA), Acute Physiology And Chronic Health Evaluation (APACHE) II and III, and Simplified Acute Physiology Score (SAPS) II, are widely used in critically ill patients; they weigh kidney dysfunction variously [2]. Among these scoring systems, the SOFA score may be used to describe the time course of organ dysfunction in individual patients and is useful to evaluate morbidity [7].
Risk factors associated with hospital mortality in critically ill patients with AKI have been evaluated in several studies. The main risk factors identified were advanced age, use of vasopressors, mechanical ventilation, septic shock, hepatorenal syndrome, and cardiogenic shock [6,8].
The present study was performed to apply the RIFLE classification to patients in intensive care units (ICUs), to identify risk factors related to the development of AKI, and factors associated with hospital mortality in ICU patients.
METHODS
Study population
We constructed a retrospective study of all ICU patients over a 6-month period (July 1, 2007 to December 31, 2007) at the Keimyung University Dongsan Hospital, Daegu, Korea. During the study period, in total, 1,280 patients were admitted to the ICU and the records of all patients were reviewed. We excluded patients who remained in the ICU for less than 48 hours, those readmitted to the ICUs, those admitted after an uncomplicated operation, and those with a history of chronic renal failure requiring renal replacement therapy.
Data collection
Demographic and laboratory data were retrieved from an electronic hospital database. In total, 378 patients were included. After merging data from the different sources, we performed automated and manual data verification. Patient data included demographic, administrative, physiological, laboratory, and hospital outcome information.
RIFLE classification
All patients included in the study were classified according to the highest RIFLE criteria during the first 7 days in the ICU. Patients who presented with neither oliguria nor marked increases in serum creatinine were included in the non-AKI group. When baseline serum creatinine level was unknown in a patient with no history of chronic kidney insufficiency, we calculated the baseline creatinine using the modification of diet in renal disease (MDRD) equation, as recommended by the ADQI, assuming a glomerular filtration rate of 75 mL/min / 1.73 m2 [5,9].
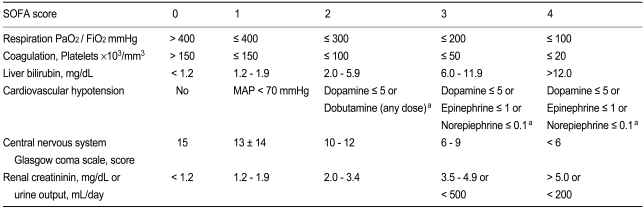
SOFA score
Organ failure was defined by the SOFA score, based on six different scores, one for each of the respiratory, cardiovascular, hepatic, coagulation, renal, and neurological systems (Table 1) [10]. We observed the changes in SOFA score every 24 hours during the first 7 days in the ICU. The worst values for each parameter in any 24-hour period were recorded.
Table 1.
SOFA score
SOFA, sequential organ failure assessment; MAP, mean arterial pressure.
aAdrenergic agents administered for at least 1 hr (doses given in µg/kg·min).
Statistical analyses
Data were analyzed using the SPSS version 12.0 (SPSS Inc., Chicago, IL, USA). Categorical data are expressed as proportions, and subgroups were analyzed using the χ2 test. Risk factors were evaluated by univariate analysis and in a multivariate analysis with a multiple logistic stepwise regression procedure. The relationships between different factors and mortality were evaluated using a Cox Proportional Hazards model, and survival curves were constructed. Variables with p < 0.05 were included in the model. Odds ratios were estimated form the b coefficients obtained, with respective 95% confidence intervals. In all comparisons, p values < 0.05 were deemed to indicate statistical significance.
RESULTS
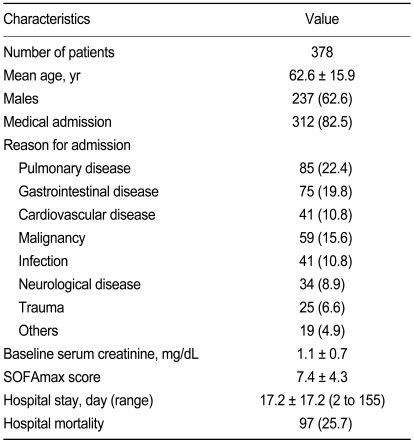
Patient baseline characteristics
Patient baseline characteristic are summarized in Table 2. In total, 378 patients were included in this study. The mean age of the patients was 62.6 ± 15.9 years and they comprised 237 men (62.7%) and 141 women (37.3%). Regarding the type of ICU admission, 312 (82.5%) cases were medical admissions. Reasons for admission to the ICU included pulmonary disease (n = 85, 22.4%), gastrointestinal disease (n = 75, 19.8%), cardiovascular disease (n = 41, 10.8%), malignancy (n = 59, 15.6%), infection (n = 41, 10.8%), neurological disease (n = 34, 8.9%), trauma (n = 25, 6.6%), endocrinological disease (n = 13, 3.4%), acute intoxication (n = 5, 1.3%), and obstetric and gynecological disease (n = 1, 0.2%). The baseline serum creatinine level was 1.1 ± 0.7 mg/dL, and the mean SOFAmax score was 7.4 ± 4.3. The mean length of hospital stay was 17.2 ± 17.2 days (range, 2 to 155) and the overall hospital mortality rate of the ICU patients was 25.7%.
Table 2.
Patient baseline characteristics
Values are presented as number (%) or mean ± SD.
SOFAmax, maximum sequential organ failure assessment.
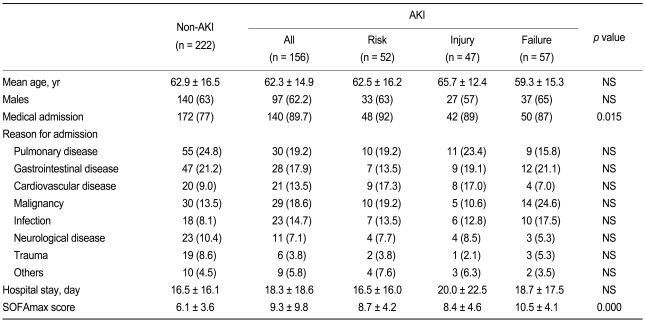
Comparison of patient characteristics according to the RIFLE classification
The AKI and non-AKI groups consisted of 156 cases (41.3%) and 222 cases (58.7%), respectively. The AKI group was also classified according to RIFLE as follows: risk (n = 52, 13.8%), injury (n = 47, 12.4%), and failure (n = 57, 15.1%). The mean age, gender, reason for admission, and length of hospital stay were not significantly different between the four groups. However, the proportion of medical admissions was significantly higher in the AKI group than in the non-AKI group. The SOFAmax score during the first week after admission was significantly higher in the AKI group than in the non-AKI group (Table 3). However, in a multivariate analysis, neither medical admission nor SOFAmax score were independent risk factors for the occurrence of AKI.
Table 3.
Baseline characteristics of patients classified according to RIFLE criteria
Values are presented as number (%) or mean ± SD.
Tested by one-way analysis of variance among groups.
RIFLE, risk, injury, failure, and the two outcome classes loss and end-stage kidney disease; AKI, acute kidney injury; NS, not significant; SOFAmax, maximum sequential organ failure assessment.
Hospital mortality and survival rates
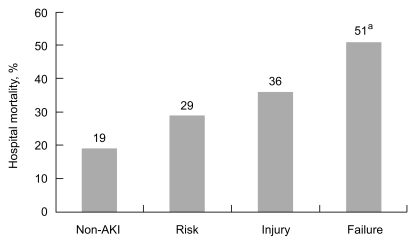
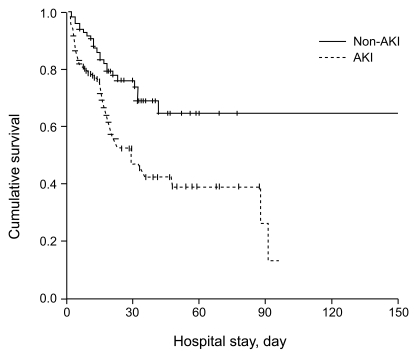
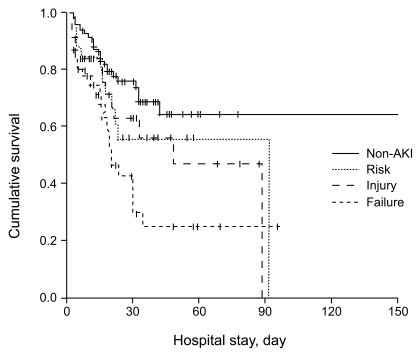
The overall mortality among patients studied was 25.7% (97 / 378). The hospital mortality rate was 19% for non-AKI patients, 29% for risk patients, 36% for injury patients, and 51% for failure patients (p < 0.005, Fig. 2). Cumulative survival rates differed significantly for non-AKI versus AKI patients (p < 0.001, Fig. 3). Patients with risk, injury, and failure had 90-day cumulative survival rates of 56.6%, 47.0%, and 25.2%, respectively, compared with 68.5% for non-AKI patients. There was a progressive and significant decrease in cumulative survival rate associated with increasing RIFLE classification among all patients (p < 0.001, Fig. 4).
Figure 2.
Hospital mortality rates for intensive care unit (ICU) patients without acute kidney injury and ICU patients with increasing risk, injury, failure, and the two outcome classes loss and end-stage kidney disease (RIFLE) criteria. ap < 0.005, tested by oneway analysis of variance among groups. AKI, acute kidney injury.
Figure 3.
Hospital survival. Cumulative survival rates differed significantly for non-AKI versus AKI patients. p<0.001, tested by Log rank test. AKI, acute kidney injury.
Figure 4.
Hospital survival rate based on risk, injury, failure, and the two outcome classes loss and end-stage kidney disease (RIFLE) classification. There were a progressive and significant decrease in cumulative survival rate associated with increasing RIFLE classification among all patients. p < 0.001, tested by Log rank test. AKI, acute kidney injury.
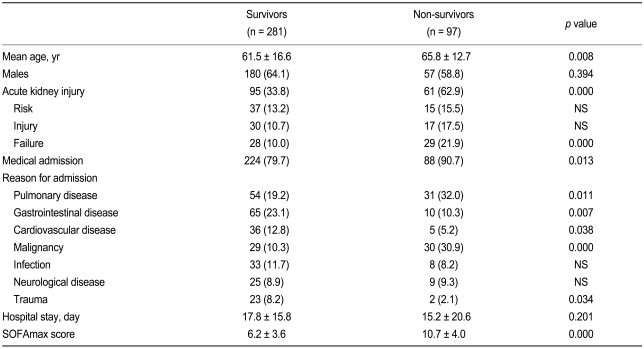
Factors associated with hospital mortality
Non-survivors were older than survivors (65.8 ± 12.7 vs. 61.5 ± 16.6 years, respectively, p = 0.008) and more commonly developed AKI during the ICU stay (62.9% vs. 33.8%, respectively; p < 0.001). The SOFAmax score was significantly higher in non-survivors than in survivors (10.7 ± 4.0 vs. 6.2 ± 3.6, respectively; p < 0.001). The proportions of medical admission, pulmonary disease, and malignancy as reasons for admission were significantly higher in non-survivors than in survivors. However, the proportions of gastrointestinal disease, cardiovascular disease, and trauma were significantly lower in non-survivors than in survivors. Neither length of hospital stay nor gender was significantly different between survivors and non-survivors (Table 4).
Table 4.
Univariate analysis of risk for hospital mortality
Values are presented as number (%) or mean ± SD.
NS, not significant; SOFAmax, maximum sequential organ failure assessment.
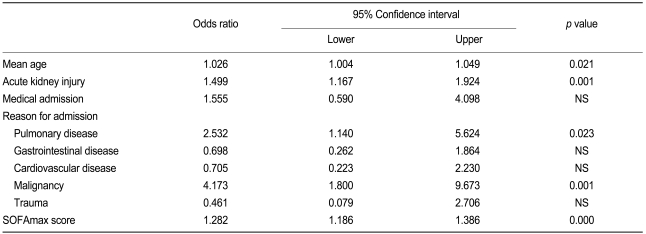
In the multivariate analysis, increasing age, occurrence of AKI, increasing SOFA score, pulmonary disease, and malignancy were independent risk factors for hospital mortality (Table 5).
Table 5.
Multivariate analysis of risk for hospital mortality
NS, not significant; SOFAmax, maximum sequential organ failure assessment.
DISCUSSION
We conducted a single-center study with 378 ICU patients to characterize AKI, defined by RIFLE classification, and related this classification to mortality in critically ill patients. In the present study, 41.3% of the ICU patients developed AKI, which was associated with increased mortality, compared with those who did not develop AKI. Hoste et al. [2] reported that AKI occurred in 67% of ICU patients, with maximum RIFLE classes of risk, injury, and failure in 12%, 27%, and 28% of cases, respectively. The incidence of almost 70% may appear inconsistent with the existing literature [5,11-13]. The incidence of AKI in the present study was somewhat lower than those in other studies [2,14] using the same RIFLE classification. The most likely explanations are differences in the patient case mix, factors related to a single-center versus multicenter study, and differences in the type of admission (i.e., medical vs. surgical). Hoste et al. [2] suggested that medical admission was less likely to result in AKI, compared with surgical admission [4]. Medical admission accounted for less than 50% of cases in a multicenter cohort study of AKI [4], and the rate was about 78% in a single-center cohort study [14]. In the present study, medical admission accounted for the majority of ICU patients. Hoste et al. [2] reported that increasing age, greater severity of illness (APACHE III, SOFA), preexisting chronic kidney insufficiency, and previous admission to a non-ICU ward were associated with significant mortality rates, ranging from 20% to 80%, and associated with increased risk for the occurrence of AKI.
Importantly, even a mild degree of kidney dysfunction, RIFLE class risk or injury, was associated with elevated mortality rate, compared with patients who maintained normal function. In the present study, the overall hospital mortality rate of ICU patients was 25.7%, which was significantly higher for AKI patients versus non-AKI patients. We also found that ICU mortality ranged from 29% in risk patients, 36% in injury patients, and 51% in failure patients. Factors associated with mortality in our ICU patients included advanced age, development of AKI, baseline severity of illness, and the presence of pulmonary disease and malignancy. These findings were consistent with previous reports [2,3,15]. Hoste et al. [2] demonstrated the association of AKI with increased hospital mortality in a general ICU population and demonstrated that there was increasing mortality risk over RIFLE classes, although these ICU patients had similar comorbidity rates, as reflected by non-renal SOFA scores. They also proposed that the pathophysiological changes resulting from kidney insufficiency and adverse effects of renal replacement treatment may be associated with increased mortality rate [2,16,17]. Uchino et al. [3] reported that there was an almost linear increase in hospital mortality rate with increasing RIFLE class, with patients in the risk group having a mortality rate more than three times higher than that of patients without AKI. In multivariate analysis, the risk group showed an odds ratio of hospital mortality of 2.5, that of the injury group was 5.4, and that of the failure group was 10.1 [3]. They suggested that the development of AKI has greater prognostic implications than the need for ICU or mechanical ventilation, and the development of failure is one of the most powerful identifiable outcome predictors for hospitalized patients [3]. Abosaif et al. [18] also reported that ICU mortality rate increased from 38.3% among patients in the risk group to 50% in the injury group and to 74.5% among patients in the failure group. Our study confirmed that even a mild degree of kidney dysfunction posed a significant risk of hospital mortality.
This study has some limitations. First, it was a retrospective study using existing medical records, which in itself caused some difficulty in the assessment of AKI and the statistical analyses. Second, we classified patients according to the highest RIFLE criteria during the first 7 days in the ICU, similar to the study reported previously by Hoste et al. [2]. More recently, the Acute Kidney Injury Network (AKIN) group proposed refinements to the RIFLE classification [13]. In particular, the AKIN group sought to increase the sensitivity of the RIFLE classification by setting a 48-hour window on the first documentation of criteria and broadening the risk category of RIFLE to include increases in serum creatinine of ≥ 0.3 mg/dL even if this does not reach the 50% cutoff [13].
In conclusion, in these ICU patients, acute kidney risk, injury, and failure, as defined by the recently developed RIFLE classification, were associated with increased hospital mortality rates. The RIFLE classification is a simple and useful clinical tool to detect and stratify the severity of AKI, and possibly to predict outcome.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Ympa YP, Sakr Y, Reinhart K, Vincent JL. Has mortality from acute renal failure decreased? A systematic review of the literature. Am J Med. 2005;118:827–832. doi: 10.1016/j.amjmed.2005.01.069. [DOI] [PubMed] [Google Scholar]
- 2.Hoste EA, Clermont G, Kersten A, et al. RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: a cohort analysis. Crit Care. 2006;10:R73. doi: 10.1186/cc4915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Uchino S, Bellomo R, Goldsmith D, Bates S, Ronco C. An assessment of the RIFLE criteria for acute renal failure in hospitalized patients. Crit Care Med. 2006;34:1913–1917. doi: 10.1097/01.CCM.0000224227.70642.4F. [DOI] [PubMed] [Google Scholar]
- 4.Uchino S, Kellum JA, Bellomo R, et al. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA. 2005;294:813–818. doi: 10.1001/jama.294.7.813. [DOI] [PubMed] [Google Scholar]
- 5.Bellomo R, Ronco C, Kellum JA, et al. Acute renal failure-definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8:R204–R212. doi: 10.1186/cc2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ricci Z, Cruz D, Ronco C. The RIFLE criteria and mortality in acute kidney injury: a systematic review. Kidney Int. 2008;73:538–546. doi: 10.1038/sj.ki.5002743. [DOI] [PubMed] [Google Scholar]
- 7.Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001;286:1754–1758. doi: 10.1001/jama.286.14.1754. [DOI] [PubMed] [Google Scholar]
- 8.Mehta RL, Pascual MT, Gruta CG, Zhuang S, Chertow GM. Refining predictive models in critically ill patients with acute renal failure. J Am Soc Nephrol. 2002;13:1350–1357. doi: 10.1097/01.asn.0000014692.19351.52. [DOI] [PubMed] [Google Scholar]
- 9.National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39:S1–S266. [PubMed] [Google Scholar]
- 10.Vincent JL, Moreno R, Takala J, et al. The Sepsis-related Organ Failure Assessment (SOFA) score to describe organ dysfunction / failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22:707–710. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 11.Liaño F, Pascual J Madrid Acute Renal Failure Study Group. Epidemiology of acute renal failure: a prospective, multicenter, community-based study. Kidney Int. 1996;50:811–818. doi: 10.1038/ki.1996.380. [DOI] [PubMed] [Google Scholar]
- 12.Brivet FG, Kleinknecht DJ, Loirat P, Landais PJ. Acute renal failure in intensive care units - causes, outcome, and prognostic factors of hospital mortality: a prospective, multicenter study. French Study Group on Acute Renal Failure. Crit Care Med. 1996;24:192–198. doi: 10.1097/00003246-199602000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Mehta RL, Kellum JA, Shah SV, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11:R31. doi: 10.1186/cc5713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Perez Valdivieso JR, Bes-Rastrollo M, Monedero P, De Irala J, Lavilla FJ. Evaluation of the prognostic value of the risk, injury, failure, loss and end-stage renal failure (RIFLE) criteria for acute kidney injury. Nephrology. 2008;13:361–366. doi: 10.1111/j.1440-1797.2008.00950.x. [DOI] [PubMed] [Google Scholar]
- 15.de Mendonça A, Vincent JL, Suter PM, et al. Acute renal failure in the ICU: risk factors and outcome evaluated by the SOFA score. Intensive Care Med. 2000;26:915–921. doi: 10.1007/s001340051281. [DOI] [PubMed] [Google Scholar]
- 16.Klahr S, Miller SB. Acute oliguria. N Engl J Med. 1998;338:671–675. doi: 10.1056/NEJM199803053381007. [DOI] [PubMed] [Google Scholar]
- 17.Hoste EA, Kellum JA. Acute renal failure in the critically ill: impact on morbidity and mortality. Contrib Nephrol. 2004;144:1–11. doi: 10.1159/000078872. [DOI] [PubMed] [Google Scholar]
- 18.Abosaif NY, Tolba YA, Heap M, Russell J, El Nahas AM. The outcome of acute renal failure in the intensive care unit according to RIFLE: model application, sensitivity, and predictability. Am J Kidney Dis. 2005;46:1038–1048. doi: 10.1053/j.ajkd.2005.08.033. [DOI] [PubMed] [Google Scholar]