Abstract
Background/Aims
Maintenance dialysis is made decreased the death rate of patients with end-stage renal disease; however, mortality is still high. The aim of this study was to identify the association between clinical parameters at the start of hemodialysis with survival and compare these findings with data from patients who underwent hemodialysis about 15 years ago at the same dialysis center.
Methods
We reviewed 117 patients who started hemodialysis between 2000 and 2004. We analyzed medical histories, laboratory findings, and clinical outcomes, and compared them with patients who started hemodialysis 15 years ago at the same center.
Results
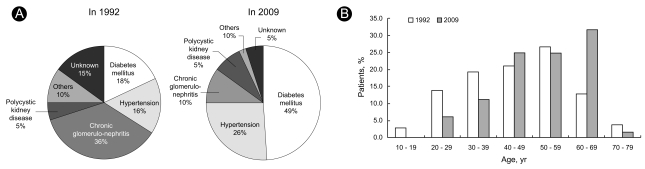
The proportion of elderly patients and those with diabetes increased from 17% and 18% in the previous study to 33% and 49% in this study, respectively. Elderly and patients with diabetes had much higher mortalities than their counterparts. Nevertheless, the overall survival rate (66% vs. 71% at 5 years) and survival of patients with diabetes improved (55% vs. 75% at 1.5 years). Common causes of death were infection and cardiovascular disease in the present study; however, inadequate dialysis accounted for 25% of deaths in the previous study.
Conclusions
The overall survival rate of patients undergoing hemodialysis has improved over the 15-year interval, even with an increased proportion of elderly patients and patients with diabetes. Adequate dialysis and further medical improvements could ameliorate mortality in patients undergoing dialysis.
Keywords: Renal dialysis, Mortality, Survival analysis
INTRODUCTION
Maintenance dialysis is made decreased the death rate associated with end-stage renal disease (ESRD); however, mortality remains high in patients on hemodialysis. Once renal replacement therapy is initiated, the range of expected life span according to the United States Renal Data System report is approximately 8 years for patients aged 40 to 44 undergoing dialysis and approximately 4.5 years for those 60 to 64 years of age [1]. The most common cause of death is cardiovascular disease, and comorbid conditions such as diabetes mellitus, ischemic heart disease [1-4], inadequate dialysis [5,6], long duration on dialysis [7], serum potassium level less than 4.0 or greater than 5.6 mEq/L [8], and malnourished state [6] are factors known to be correlated with decreased survival. Survival and quality of life in ESRD patients are expected to be improved by determining the correctable factors associated with inadequate dialysis and malnu-trition such as Kt/V, body mass index, serum albumin, cholesterol, potassium, and hemoglobin level.
Over the past decade, a number of large-scale studies have examined the impact of several factors at the initiation of dialysis on the survival of individuals with ESRD. However, little information is available on the changes in survival patterns among Asian patients with ESRD over time.
Therefore, the aim of this study was to identify associations between clinical parameters at the initiation of hemodialysis with survival by assessing these parameters in patients who began dialysis at Soonchunhyang Cheonan Hospital from January 2000 to January 2004 and comparing the results with data from patients who underwent hemodialysis about 15 years ago at the same dialysis center.
METHODS
Materials
The medical records of patients with ESRD who began dialysis at Soonchunhyang Cheonan Hospital from January 2000 to January 2004 were reviewed retrospectively. Among these patients, those without complete medical records were excluded. Additionally, patients who had died within 3 months after starting hemodialysis were excluded. Finally, 117 patients were enrolled in this study.
We compared our findings with those of a previous retrospective study [9]. The previous study included 109 patients who underwent hemodialysis about 15 years ago (from June 1984 to December 1990) at the same dialysis center.
Methods
We retrospectively reviewed the medical records and laboratory findings at the beginning of hemodialysis. The patient characteristics included age, gender, cigarette smoking, body mass index, comorbid conditions at the time of initiating hemodialysis (diabetes mellitus, hypertension, ischemic heart disease, congestive heart failure, left ventricular hypertrophy, cerebrovascular accident, and chronic liver disease), number of antihypertensive medications (angiotensin-converting enzyme inhibitor/angiotensin II receptor blockers, calcium channel blockers, beta-blockers, minoxidil, and diuretics, which were regarded as one class of antihypertensives each), biochemical markers (blood urea nitrogen, creatinine, calcium, phosphorus, sodium, potassium, uric acid, albumin, total cholesterol), arterial blood gases, hemoglobin, hematocrit, leukocyte, and platelet counts. The vascular access method for the first hemodialysis was classified as arteriovenous fistula/graft, jugular venous catheter, subclavian catheter, femoral catheter, or tunneled catheter. Furthermore, we recorded patient survival based on the survival duration up to April 30, 2009, including the observation period to death, cause of death, and morbidity during the follow-up period.
The patients who were transferred to local dialysis facilities were followed by questionnaires sent to the facilities, and information on survival, date of death, and cause of death were recorded. If the data were not available from the facilities, they were obtained from the ESRD Registry Committee of the Korean Society of Nephrology.
Statistical analysis
Data are presented as the mean ± standard deviation for continuous variables and as frequencies (percent) for categorical variables. Statistical analyses were performed using SPSS version 14.0 (SPSS Inc., Chicago, IL, USA), and all p values < 0.05 were considered statistically significant. The differences between groups were compared with the Student's t test or analysis of variance (ANOVA) for continuous variables and by the χ2 test or Fisher's exact test for categorical variables. The dependence between variables was analyzed using a bivariate correlation analysis. Multiple logistic regression analyses were used to determine the factors affecting survival duration after the initiation of hemodialysis. The results of the logistic regression analyses were recorded as odds ratios with 95% confidence intervals. The Kaplan-Meier analysis was used to compare the survival rate between groups. The survival duration was measured from the start of hemodialysis to death or to April 30, 2009.
RESULTS
Baseline patient characteristics
The most common renal disease leading to ESRD was diabetes mellitus (48.7%), followed by hypertension, chronic glomerulonephritis, and polycystic kidney disease.
The method of vascular access for the first hemodialysis was arteriovenous fistula/graft (31.6%), jugular venous catheter (47.3%), subclavian catheter (16.7%), femoral catheter (0.9%), and tunneled catheter (3.5%).
The numbers of antihypertensive medications used before the initiation of hemodialysis were 0 (11.8%), 1 (28.8%), 2 (28.8%), 3 (18.9%), 4 (10.8%), and 5 (0.9%). Patients were most commonly taking calcium channel blockers (53.0%), followed by angiotensin-converting enzyme inhibitor/angiotensin II receptor blockers (49.6%), diuretics (42.7%), beta-blockers (31.6%), and minoxidil (3.4%).
Most patients had anemia (91.9%, hemoglobin level < 11.0 g/dL) and metabolic acidosis (77.4%, bicarbonate level less than 20 mEq/L) at the initiation of hemodialysis.
Risk factors affecting patient survival
The causes of death were infection (43.8%), cardiovascular disease (21.9%), and cerebrovascular accident (9.4%). However, those of a previous study reported in 1992 [9] were cerebrovascular accident (32.1%) and discontinuation of dialysis (25.0%).
Patients who died demonstrated higher average age (48.9 ± 13.0 vs. 57.3 ± 9.4 years, p = 0.001), increased leukocyte count (7,101.8 ± 2,369.4 vs. 8,647.5 ± 4,438.9 /L, p = 0.050), and decreased platelet (190.7 ± 81.9 vs. 235.9 ± 112.9 × 103 /µL, p = 0.025) and creatinine levels (9.3 ± 4.4 vs. 6.8 ± 2.9 mg/dL, p = 0.002). However, there was no difference in survival associated to gender, initial body mass index, blood urea nitrogen, serum albumin, total cholesterol, ferritin level, hemoglobin, or hematocrit.
A logistic regression analysis was performed for comorbid conditions as predictors of mortality. Diabetes, ischemic heart diseases, and left ventricular hypertrophy were related to increased mortality rate. However, only diabetes (p = 0.019) and left ventricular hypertrophy (p = 0.035) were statistically significant in the multivariate logistic regression analysis. Other factors such as cigarette smoking, cerebrovascular accidents, liver disease, the method of vascular access for the first hemodialysis, and the number of antihypertensive medications were not significantly different between the survivors and the patients who died.
Patient survival by underlying renal disease and age
After censoring at the time of death, 94 patients were available to evaluate survival duration at a mean follow-up of 68.3 ± 32.7 months (range, 4 to 111).
No significant differences were found in survival duration of the patients who had died according the method of vascular access for the first hemodialysis (p = 0.247) or the number of antihypertensive medications taken (p = 0.739).
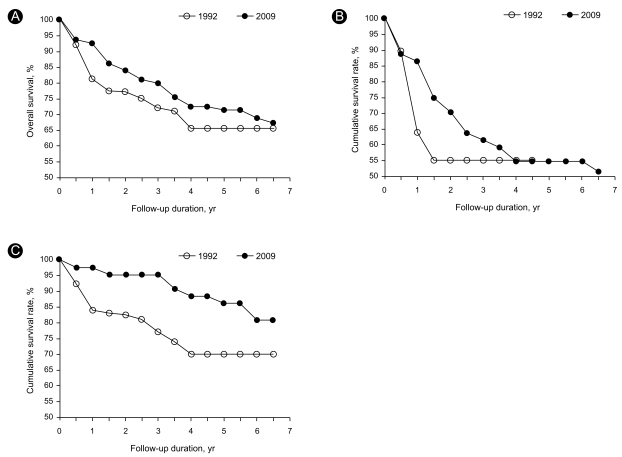
Renal diseases leading to ESRD were classified as diabetic versus nondiabetic and analyzed by the Kaplan-Meier method. The cumulative survival rates were 95%, 92%, and 87% in the nondiabetic group, and 83%, 62%, and 55% in the diabetic group at 1, 3, and 5 years, respectively (Fig. 1). The mean survival duration (diabetes mellitus, 25.2 ± 21.9 months; hypertension, 55.6 ± 13.5 months; polycystic kidney disease, 17.7 ± 17.2 months; one-way ANOVA, p = 0.014) and cumulative survival rates according to each underlying renal disease demonstrated statistically significant differences. The cumulative survival rates at 1 year were 74% in patients with diabetes mellitus, 75% in those with polycystic kidney disease, and 100% in those with hypertension and chronic glomerulonephritis. At 3 years they were 60%, 63%, and 100%, and at 5 years they were and 55%, 63%, 90%, respectively.
Figure 1.
Comparison of survival rates between our study and a previous study at the same center in 1992. (A) Overall 5-year survival was 66% in the previous study vs. 71% in this study. (B) The percentage of surviving patients with diabetes was 64% in the previous study vs. 86% in this study at 1 year and 55% vs. 61% at 3 years. (C) The percentage of surviving nondiabetic patients was 84% in the previous study vs. 98% in this study at 1 year, and 77% vs. 95% at 3 years.
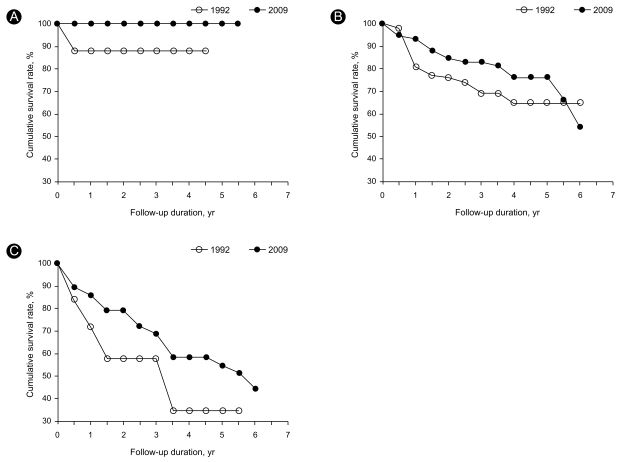
According to the age at the start of hemodialysis, patients were classified as less than 30 years of age, 31 to 60 years, or over 60 years of age. The cumulative survival rates at 1 year were 100% in patients less than 30 years of age, 93% in those 31 to 60 years, and 86% in those over 60 years of age. The cumulative survival rates at 3 years were 100%, 83%, and 69%; at 5 years, they were 100%, 76%, and 55%; and at 7 years, they were 50%, 39%, 24%, respectively (Fig. 2). Older patients (p = 0.001) and patients with diabetes (p = 0.001) had a much higher mortality rate than their counterparts.
Figure 2.
Comparison of survival rates according to age at the start of hemodialysis between our study and the previous study in 1992. (A) The percentage of surviving patients less than 30 years of age was 88% in the previous study vs. 100% in this study at 3 years. (B) The percentage of surviving patients between 31 and 60 years of age was 81% in the previous study vs. 93% in this study at 1 year and 69% vs. 83% at 3 years. (C) The percentage of surviving patients over 60 years of age was 72% in the previous study vs. 86% in this study at 1 year and 58% vs. 69% at 3 years.
Additionally, patients were classified into four groups according to whether they had diabetes and their age at the start of hemodialysis. The cumulative survival rates in the group with diabetes and over 60 years of age were 36% at 3 years and 28% at 7 years, which were much lower than the 97% survival rate at 3 years and 93% at 7 years in the group without diabetes and who were less than 60 years of age.
DISCUSSION
Maintenance dialysis has decreased the death rate associated with ESRD; however, the mortality in patients on hemodialysis remains high. The ESRD Registry Committee of the Korean Society of Nephrology reported that, among patients on hemodialysis, the cumulative survival rates were 94%, 83%, and 73% in nondiabetic patients, and 93%, 70%, and 53% in patients with diabetes at 1, 3, and 5 years, respectively [10]. In comparison, in the present study, the nondiabetic group had higher and the diabetic group had lower survival rates (95%, 92%, and 87% in nondiabetic group; 83%, 62%, and 55% in the diabetic group at 1, 3, and 5 years, respectively). The finding for diabetic patients was consistent with the findings of previous studies and the USRDS data [1]. This result suggests that diabetes mellitus at the initiation of hemodialysis is a predictor of increased mortality.
Our center is located in a rural town and has been in operation since 1984. It may be important to analyze survival at a single center to maintain the quality of hemodialysis. In a previous study of 109 patients who underwent dialysis from June 1984 to December 1990 at the same center, the cumulative survival rates were 81% at 1 year and 66% at 5 years [9] compared to 95% and 86% in this study. These findings suggest that the overall survival rates have improved over the 15-year interval, as both studies were conducted at the same center and in the same region. However, the proportion of patients over 60 years of age undergoing hemodialysis increased from 17% in the previous study reported in 1992 to 33% in the present study. Moreover, the most common underlying renal disease has changed from chronic glomerulonephritis (36%) to diabetes mellitus (49%). Consequently, the proportion of patients with diabetes as a cause of ESRD has increased from 18% to 49% over the 15-year interval. The earlier study reported that diabetes mellitus was a predictor of poorer outcome, with a cumulative survival rate of patients with diabetes of 55% at 1.5 years [9]. However, the patients with diabetes in this study demonstrated improved cumulative survival rates (83% at 1 year and 55% at 5 years, Fig. 1). Therefore, the overall survival rate of hemodialysis patients has improved over the past 15 years even with the increased proportion of elderly patients (17% vs. 33% over 60 years of age) and of those with diabetes mellitus (18% vs. 49%, Fig. 3). The reasons for improved survival might be the increased proportion of patients undergoing adequate dialysis due to improved quality management and the remarkable progress of medical science, as well as improved instrumentation, dialysis membranes, dialysates, and the quality of water [11,12]. In fact, dialysis membranes used in the previous study were the GC-150M (cuprammonium rayon; surface area, 1.0 m2; ultrafiltr ation rate [UFR], 4.0 mL/Hg.h) and CF Model 12.11 (cuprophan; surface area, 0.8 m2; UFR, 4.0 mL/Hg.h) [9] with surface areas no more than 1.0 m2. In the present study, the dialysis membranes were Polyamix™ (polyarylethersulfone, polyvinylpyrrolidone, polyamide blend; surface area, 1.7 to 2.1 m2; ultrafiltration coefficient, 70 to 85 mL/h.mmHg) and Helixone®(polysulfone high flux; surface area, 1.4 to 1.8 m2; ultrafiltration coefficient 46 to 59 mL/h.mmHg) with surface areas more than 1.4 m2. Moreover, the previous study had no standard definition for "adequate dialysis," and most patients underwent hemodialysis twice per week. Furthermore, many patients could not continue dialysis or increase dialysis frequency due to the economic burden, even though their uremic condition was aggravated. Consequently, inadequate dialysis accounted for up to 25% of deaths reported in the previous study. Currently, we maintain dialysis quality by monitoring the Kt/V regularly, and most patients continue dialysis without excessive economic problems.
Figure 3.
(A) The causes of end stage renal disease in the present study demonstrated a much higher frequency of diabetes mellitus compared to the previous study in 1992. (B) The age distribution showed an increased proportion of elderly patients.
Over the past decade, a number of large-scale studies have analyzed the survival rate of elderly patients with ESRD [13,14]. In this study, elderly patients with ESRD had much higher mortality rates than did younger patients; the mortality rates at 5 years were 0.0% in patients less than 30 years of age, 23.7% in those between 31 and 60 years, and 44.8% in those over 60 years of age (p = 0.008). Therefore, close observation and management are needed in patients starting dialysis who are over 60 years of age.
The cumulative survival rates revealed an association between dialysis duration and increased risk of death: 95% survival at 1 year of dialysis, 90% at 3 years, 86% at 5 years, 72% at 6 years, and 57% at 7 years of dialysis. These results suggest that increased age, diabetes mellitus, and increased length of time on dialysis were significant risk factors for death.
Previous studies have reported inadequate dialysis, long dialysis duration, and serum potassium levels less than 4.0 or greater than 5.6 mEq/L [5-8] as predictors for increased mortality. Comorbid conditions such as diabetes mellitus, ischemic heart disease [1-4,15], late referral to nephrologists [16], and malnourished state [6,15], particularly a serum albumin level less than 3.0 g/dL and lower body mass index [6,17], are factors correlated with morbidity and decreased survival. We found no significant differences in survival according to the initial body mass index, serum albumin, total cholesterol, potassium level, and hematocrit. However, the serum albumin levels were low in both groups (3.2 ± 0.6 g/dL in the survivors, 3.0 ± 0.5 g/dL in the patients who died) suggesting that malnutrition was already advanced at the beginning of hemodialysis. In the group of patients who died, the leukocyte count increased and creatinine decreased, consistent with previous reports, indicating that chronic inflammation and malnutrition are associated with decreased survival [18]. Therefore, early dialysis management is needed before patients develop malnutrition and chronic inflam-mation.
Comorbid conditions such as ischemic heart disease and left ventricular hypertrophy were associated with an increased risk of death, consistent with the findings of a previous study [19]. Therefore, screening for cardiovascular disease is needed in this group of patients.
Unlike the findings reported in other studies [1,10], the most common cause of death was infections (43.8%), followed by cardiovascular disease (21.9%) and cerebrovascular accidents (9.4%). This result was different from the data in the ESRD Registry Committee of Korean Society of Nephrology, which reported, in order, cardiologic origin (31.7%), vascular origin (17.8%), and infectious origin (20.2%) [10] as the most common causes of death. These differences are likely due to data management and the censoring of data. We obtained data from the ESRD Registry Committee of the Korean Society of Nephrology, but information was missing as well. Only 59.3% of all 535 dialysis centers were available to provide data. Therefore, unified registries of the data on patients with ESRD must improve, just the management of them does.
In conclusion, the overall survival rate of patients undergoing hemodialysis has improved over the past 15 years, even with the increased proportion of elderly patients and those with diabetes mellitus in the current group. Compared with patients 15 years ago, improvements in dialysis membranes, adequacy of dialysis, and medical science appear to have ameliorated mortality in patients under-going dialysis.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Collins AJ, Foley RN, Herzog C, et al. United States Renal Data System 2008 Annual Data Report. Am J Kidney Dis. 2009;53:S1–S374. doi: 10.1053/j.ajkd.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 2.Causes of death. United States Renal Data System. Am J Kidney Dis. 1998;32(2 Suppl 1):S81–S88. doi: 10.1053/ajkd.1998.v32.pm9713410. [DOI] [PubMed] [Google Scholar]
- 3.Parfrey PS, Foley RN. The clinical epidemiology of cardiac disease in chronic renal failure. J Am Soc Nephrol. 1999;10:1606–1615. doi: 10.1681/ASN.V1071606. [DOI] [PubMed] [Google Scholar]
- 4.Goldsmith DJ, Covic A. Coronary artery disease in uremia: etiology, diagnosis, and therapy. Kidney Int. 2001;60:2059–2078. doi: 10.1046/j.1523-1755.2001.00040.x. [DOI] [PubMed] [Google Scholar]
- 5.Charra B, Calemard E, Ruffet M, et al. Survival as an index of adequacy of dialysis. Kidney Int. 1992;41:1286–1291. doi: 10.1038/ki.1992.191. [DOI] [PubMed] [Google Scholar]
- 6.Owen WF, Jr, Lew NL, Liu Y, Lowrie EG, Lazarus JM. The urea reduction ratio and serum albumin concentration as predictors of mortality in patients undergoing hemodialysis. N Engl J Med. 1993;329:1001–1006. doi: 10.1056/NEJM199309303291404. [DOI] [PubMed] [Google Scholar]
- 7.Chertow GM, Johansen KL, Lew N, Lazarus JM, Lowrie EG. Vintage, nutritional status, and survival in hemodialysis patients. Kidney Int. 2000;57:1176–1181. doi: 10.1046/j.1523-1755.2000.00945.x. [DOI] [PubMed] [Google Scholar]
- 8.Kovesdy CP, Regidor DL, Mehrotra R, et al. Serum and dialysate potassium concentrations and survival in hemodialysis patients. Clin J Am Soc Nephrol. 2007;2:999–1007. doi: 10.2215/CJN.04451206. [DOI] [PubMed] [Google Scholar]
- 9.Choo WS, Kim KW, Yang DH, Hong SY. The survival rate and causes of death in patients with chronic renal failure on hemodialysis. Korean J Nephrol. 1992;11:56–61. [Google Scholar]
- 10.ESRD Registry Committee, Korean Society of Nephrology. Current renal replacement therapy in Korea-Insan memorial dialysis 2007. Korean J Nephrol. 2007;26(suppl):S459–S481. [Google Scholar]
- 11.Eknoyan G, Beck GJ, Cheung AK, et al. Effect of dialysis dose and membrane flux in maintenance hemodialysis. N Engl J Med. 2002;347:2010–2019. doi: 10.1056/NEJMoa021583. [DOI] [PubMed] [Google Scholar]
- 12.Allon M, Depner TA, Radeva M, et al. Impact of dialysis dose and membrane on infection-related hospitalization and death: results of the HEMO Study. J Am Soc Nephrol. 2003;14:1863–1870. doi: 10.1097/01.asn.0000074237.78764.d1. [DOI] [PubMed] [Google Scholar]
- 13.McDonald M, McPhee PD, Walker RJ. Successful self-care home dialysis in the elderly: a single center's experience. Perit Dial Int. 1995;15:33–36. [PubMed] [Google Scholar]
- 14.Yang JW, Kim JS, Kim BR, et al. Clinical characteristics and survival analysis of elderly patients undergoing continuous ambulatory peritoneal dialysis. Korean J Nephrol. 2008;27:348–357. [Google Scholar]
- 15.Song YS, Jung H, Shim J, et al. Survival analysis of Korean end-stage renal disease patients according to renal replacement therapy in a single center. J Korean Med Sci. 2007;22:81–88. doi: 10.3346/jkms.2007.22.1.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kang WH, Oh HY, Shin YJ, et al. Impact of early nephrology referral on factors correlated with hemodialysis patients' survival. Korean J Nephrol. 2006;25:243–250. [Google Scholar]
- 17.Dwyer JT, Larive B, Leung J, et al. Are nutritional status indicators associated with mortality in the hemodialysis (HEMO) study? Kidney Int. 2005;68:1766–1776. doi: 10.1111/j.1523-1755.2005.00593.x. [DOI] [PubMed] [Google Scholar]
- 18.Lee KB. Malnutrition-inflammation complex syndrome in hemodialysis ratients. Korean J Nephrol. 2006;25(Suppl 2):S546–S549. [Google Scholar]
- 19.Song YR, Kim SG, Kim EJ, et al. The prevalence of coronary artery disease in patients with end stage renal disease at the initiation of dialysis and the accuracy of noninvasive tests. Korean J Nephrol. 2007;26:327–333. [Google Scholar]