Abstract
Inflammatory bowel diseases (IBDs) are chronic inflammatory disorders of the bowel, including ulcerative colitis and Crohn’s disease. A single etiology has not been identified, but rather the pathogenesis of IBD is very complex and involves several major and minor contributors, employing different inflammatory pathways which have different roles in different patients. Although new and powerful medical treatments are available, many are biological drugs or immunosuppressants, which are associated with significant side effects and elevated costs. As a result, the need for predicting disease course and response to therapy is essential. Major attempts have been made at identifying clinical characteristics, concurrent medical therapy, and serological and genetic markers as predictors of response to biological agents. Only few reports exist on how mucosal/tissue markers are able to predict clinical behavior of the disease or its response to therapy. The aim of this paper therefore is to review the little information available regarding tissue markers as predictors of response to therapy, and reevaluate the role of tissue factors associated with disease severity, which can eventually be ranked as “tissue factor predictors”. Five main categories are assessed, including mucosal cytokines and chemokines, adhesion molecules and markers of activation, immune and non-immune cells, and other mucosal components. Improvement in the design and specificity of clinical studies are mandatory to be able to classify tissue markers as predictors of disease course and response to specific therapy, obtain the goal of achieving “personalized pathogenesis-oriented therapy” in IBD.
Keywords: Inflammatory bowel disease, Crohn’s disease, Ulcerative colitis, Disease course predictors, Cytokines, Chemokines, Intestinal mucosa
INTRODUCTION
During the past decade, major insights into the pathogenesis of inflammatory bowel disease (IBD) have been achieved, and investigators generally agree that factors including the external environment, genetic makeup, intestinal microbial flora, and immune system are all involved and functionally integrated in the generation of the chronic intestinal inflammatory reaction that characterizes IBD[1].
Among all factors, those considered to contribute mainly to IBD pathogenesis are genetics, along with mucosal immunity. New insights in mucosal immunity have allowed for the introduction of biological agents, which have led to great changes in clinical management of IBD, as well as the course of the disease.
Biological drugs block key molecules that are involved in the induction and maintenance of intestinal chronic inflammation through several pathways, differently represented among patients. However, although considered pathogenesis-oriented drugs, a lot still needs to be done in order to achieve “personalized pathogenesis-oriented therapy” in IBD. The complex pathogenesis that involves several major and minor contributors, involves different inflammatory pathways that can have diverse roles in different patients.
These components should be taken into consideration, when choosing from the variety of emerging therapies available for IBD patients, especially biological agents and immunosuppressants. These potent treatments may be associated with significant side effects, in particular serious infections and increased risk of malignancy. In addition, they might not be needed for the subgroup of patients destined to have a more benign course. Their high cost also requires optimal treatment-to-patient adjustment.
As a consequence, there is a pressing need to differentiate between patients who may have more aggressive phenotypes from those with a potentially more benign course[2], with the use of markers that are capable of predicting therapeutic responses.
Major attempts regarding the prediction of therapeutic efficacy have been made on clinical characteristics (e.g. smoking is associated with lower response rates[3]), concurrent medical therapy, serological markers (anti-Saccharomyces cerevisiae antibody and anti-neutrophil cytoplasmic antibody[4-6], outer membrane porin C, CBir1-flagellin, antibodies against I2 protein and the anti-glycan antibodies) and genetic markers[2]. All the above markers have been assessed for their response to anti-tumor necrosis factor (TNF)-α therapy. Emerging evidence, mostly related to the capacity of biological agents to induce mucosal healing, has suggested that mechanisms related to mucosal disease/healing are helpful in completing the scenario of predictors of specific therapy in IBD.
However, how mucosal and tissue inflammatory pathways can influence or predict the disease remains largely unknown, therefore making both prediction of disease course and clinical management of IBD a challenging task.
In fact, only few reports exist on how mucosal/tissue markers can predict clinical response, mostly related to infliximab treatment (summarized in Table 1 and briefly reported below).
Table 1.
Studies assessing tissue markers as predictors of disease severity or drug response
| Target | Techniques | Use | Ref. |
| Osteoprotegerin, STC1, PTGS2, IL13Rα2 and IL11 | Microarray and PCR on mucosal extract | Predict response to IFX in UC | Arijs et al[7] |
| TNF-α levels and IL8, IL18 | PCR and Immunohistochemistry on mucosal biopsies, ELISA on organ culture | Clinical/endoscopic remission in UC, response to corticosteroids, response to therapy in CD | Olsen et al[10] |
| Ishiguro et al[12] | |||
| Arsenescu et al[11] | |||
| Schmidt et al[9] | |||
| RelA, A20, pIgR | PCR and Immunohistochemistry on mucosal biopsies | Severe disease and poor responses to immunosuppressive and anti-TNF-α therapy in 69 CD patients | Arsenescu et al[11] |
| GR expression | RT-PCR on mucosal biopsies | Decreased in biopsies from UC patients non responsive to glucocorticosteroids | Raddatz et al[14] |
| Mean histological inflammation and steroid use | Histology on colon biopsies | For univariate analysis, were predictors of colectomy in 561 patients UC | Hefti et al[15] |
| Mucosal IL-8 level | ELISA on mucosal biopsies culture | In multivariate analysis, independent risk factors for future relapse in patients with quiescent UC | Yamamoto et al[16] |
GR: Glucocorticosteroid receptor; UC: Ulcerative colitis; CD: Crohn’s disease; TNF: Tumor necrosis factor; IL: Interleukin; pIgR: Polymeric immunoglobulin receptor; ELISA: Enzyme-linked immunosorbent assay; RT-PCR: Reverse transcriptase polymerase chain reaction; IFX: Infliximab.
Arijs et al[7] have shown that mucosal extracts that overexpress five genes, which encode osteoprotegerin (TNFRSF11B), stanniocalcin-1, prostaglandin-endoperoxide synthase 2, interleukin (IL)-13 receptor α 2 and IL-11, predict response to infliximab therapy with 89% accuracy in patients with refractory ulcerative colitis (UC). Notably, those genes encode for proteins involved in signaling in the adaptive immune response, inflammation and TNF-α pathways.
Another study from Van den Brande et al[8] has suggested that higher levels of apoptosis in the intestinal mucosa, as shown by 99mTc-annexin V uptake SPECT-CT images comparing before and after infliximab infusion, correlated with clinical response to infliximab in active Crohn’s disease (CD) patients.
Schmidt et al[9] have demonstrated that, in 19 steroid-refractory CD patients treated with infliximab or cyclophosphamide, lower mucosal TNF-α concentration predicted long-term remission with a sensitivity of 100% and a specificity of 87.5%.
Similar to the study mentioned above, Olsen et al[10] have reported that an inverse association between pretreatment TNF-α expression levels and clinical/endoscopic remission following infliximab treatment exists in UC patients with moderate to severe disease activity. In the same study, neither age, sex, steroid therapy, immunosuppression, pancolitis, endoscopic sub-score, disease duration, C-reactive protein, IL-4, IL-10 nor interferon (IFN) predicted mucosal or clinical remission.
Arsenescu et al[11] have revealed that, in a cohort of 69 CD patients, those with low levels of RelA subunit of nuclear factor (NF)-κB, A20 (a negative regulator of NF-κB), polymeric immunoglobulin receptor (pIgR), TNF-α and IL-8, had moderate to severe disease and poor responses to immunosuppressive and anti-TNF-α therapy, while patients characterized by low expression of RelA, A20, and pIgR, normal TNF-α and elevated IL-8, had acute inflammation that responded well to therapy.
Few reports are available on tissue factors as predictors of response to corticosteroids. Ishiguro[12] have found a higher protein level of IL-6 and TNF-α in biopsies from patients with intractable disease who were receiving corticosteroids compared to those with non-intractable disease receiving corticosteroids; these findings have not been confirmed in other studies[13].
Alternately, Raddatz et al[14] have found that, in patients with IBD, glucocorticosteroid receptor (GR) expression was not different from controls, although it was decreased in biopsies from UC patients who were non-responsive to glucocorticosteroids. In those patients, the inhibitory subtype GRb was expressed 100-1000 times less than GRa. On the contrary intercellular adhesion molecule-1 (ICAM-1) mRNA expression, although elevated in biopsies from UC patients with active disease, was no different in responders or patients with impaired response[14].
Another study has shown by univariate analysis that, in a total population of 561 UC patients evaluated with a median follow-up of 21.4 years since disease onset, mean histological inflammation and steroid use were predictors of colectomy[15].
Moving to tissue markers as predictors of disease relapse, Yamamoto et al[16] have shown by multivariate analysis that higher rectal mucosal IL-8 level, younger age, and greater number of prior relapses were independent significant risk factors for future relapse in patients with quiescent UC. In the same study, IL-1, IL-6 and TNF-α levels in the rectal mucosa were not associated with relapse.
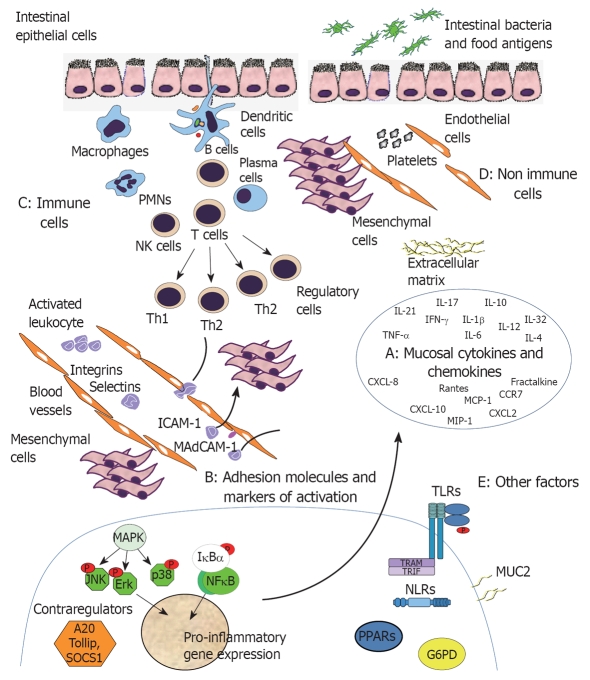
In light of these experiments, the aim of this paper is to review the role of tissue factors associated with disease severity, which may eventually be ranked as predictors of disease course and response to specific therapy. A schematic representation of the five proposed main categories of mucosal biomarkers, including mucosal cytokines and chemokines, adhesion molecules and markers of activation, immune and non-immune cells, and other mucosal components, is shown in Figure 1.
Figure 1.
Mucosal biomarkers in inflammatory bowel disease (IBD). Based on available data from IBD pathogenesis, there are five major categories of mucosal biomarkers which can be assessed as predictors of disease severity and also response to therapy. A: Mucosal cytokines and chemochines [tumor necrosis factor (TNF)-α, interleukin (IL)-6, CXCL-2, etc.]; B: Adhesion molecules (MadCAM, ICAM-1, etc.) and intracellular markers of activation [mitogen-activated protein kinase (MAPK), nuclear factor (NF)-κB, A20, etc.]; C: Immune cells (dendritic cells, monocytes, macrophages, lymphocytes, NK, plasma cells, etc.); D: Non immune cells (endothelial cells, mesenchymal cells, platelets, etc.); E: Other factors [toll-like receptors (TLRs), NLRs, mucin (MUC), G6PD, etc.].
MUCOSAL CYTOKINES AND CHEMOKINES
Alterations in the production of many cytokines have been described in patients with active IBD[17]. Although the significance of these findings in the pathogenesis of IBD remains a controversial issue, as it is unclear whether they are primary or secondary defects in the regulation of the intestinal immune system, they can be considered as markers in the differentiation of groups of patients.
In active IBD, a disturbed balance between regulatory and effector cells has been described, which mainly involves effector T cells (Th1 and Th2) and regulatory T cells (Tregs, Th3). CD is associated with a Th1 T-cell cytokine profile, including IFN-γ, TNF-α and IL-12[18], whereas UC is associated with a modified Th2 type response cytokine profile including IL-15 and IL-10[18]. In addition, these findings have been recently complemented by the discovery of the IL-23/IL-17 axis that is part of the effector T cell immunological response, and seems to be involved in IBD. Levels of expression of IL-23 and IL-17 are increased in patients with active IBD[19].
TNF-α, IL-1, IL-6
IL-1 and TNF-α share a multitude of pro-inflammatory properties and are crucial in the amplification of mucosal inflammation in IBD. Both cytokines, primarily secreted by monocytes and macrophages, activate intestinal macrophages, neutrophils, fibroblasts, and smooth-muscle cells, inducing them to secrete prostaglandins, proteases, and other soluble mediators of inflammation and injury, as well as other chemotactic cytokines[20].
TNF-α is increased in the colorectal mucosa and stools of both forms of IBD[21,22], and correlates with a higher endoscopic inflammation score[23]. TNF-α is significantly increased in the non-inflamed mucosa of CD patients compared to controls[13,21], as well as in organ culture taken from macroscopically normal mucosa[24].
Other studies[13,22] have shown that several cytokines other than TNF-α are also upregulated in the intestinal mucosa of active IBD patients, including IL-1 and IL-6. In addition TNF-α, IL-1β and IL-6 mRNA expression is increased compared to controls, with IL-6 being particularly high in the inflamed mucosa.
IL-4
IL-4 seems to play a crucial role in the Th2 response. One study has found that IL-4 is expressed in most biopsies from UC patients but not in CD[25], whereas others have not found any association between IL-4 levels and any form of IBD[13,26], probably due to technical issues[27].
IL-10
IL-10 is an anti-inflammatory cytokine produced by T cells, which inhibits the production of IL-1, IL-6 and TNF-α. Although a polymerase chain reaction (PCR)-based qualitative study on IL-10 in IBD has revealed that IL-10 is less frequently detected in UC compared to controls and CD[25], other studies have reported elevated mucosal IL-10 expression in UC and CD[28,29] or in UC alone[13,30,31].
IFN-γ
IFN-γ is elevated in all genetic animal models of IBD and is crucial in the development of Th1 responses. Mucosal IFN-γ expression is elevated in clinically active CD[32] but not in UC[33-35], which supports the theory that an imbalance in cytokine expression occurs in UC and CD; however, other studies have not reported such differences between UC and CD patients[36,37].
Other mucosal cytokines and chemokines
Other cytokines in the intestinal mucosa that are associated with active IBD include IL-21, IL-18, IL-8, monocyte chemotactic protein (MCP)-1, RANTES, epithelial neutrophil activating protein 78 (ENA-78), and IL-32[38].
Western blotting analysis of biopsies from patients with IBD and controls has demonstrated that IL-21 (a cytokine involved in the Th17 response) is overproduced in the inflamed intestine of patients with CD, in comparison to patients with UC and normal controls[39].
IL-18 is upregulated in intestinal mucosal cells of patients with IBD[40], and animal models have shown to benefit from anti-IL-18 antibody therapy with reduced severity in colitis[41].
In the proximal and distal regions of the colonic mucosa of UC patients, there was a greater than 10-fold increase in IL-8 levels compared to control subjects. A 3-5-fold increase in leukotriene B4 levels was observed along with a significant increase in myeloperoxidase levels throughout the colonic mucosa in patients with UC[42].
Other studies have reported elevated levels of MCP-1 and MCP-3, ENA-78, macrophage inflammatory proteins 1a and 1b, IFN inducible protein 10, stromal cell derived factor 1, and fractalkine[43-49].
Of particular interest is the demonstration that RANTES expression is not only increased in human IBD, but also plays a crucial role in the transition of acute to chronic disease in experimental models of colitis. In addition, RANTES triggers leukocyte adhesion to the inflamed intestinal microvasculature[50-52].
Furthermore, Kawashima et al[53] have observed a significant increase in CCR7 receptor only in CD and not in UC patients or healthy subjects. These observations are consistent with the reported increase in CC ligand expression in CD.
Studies assessing mucosal cytokine/chemokine panels
Several studies have attempted to explore the possibility of detecting tissue factors as predictors of disease severity by combining the analysis of different components simultaneously. However, none of these approaches has been validated and none are used for clinical purposes.
Real-time PCR quantification of CXCL8, CXCL10, calgranulin B and CXCL2 in colonic biopsies correlated with clinical activity index and endoscopic activity index in 27 UC patients, which suggests the use of these molecules as biomarkers and objective tools in clinical trials for the evaluation of anti-inflammatory and immunomodulatory regimens[54].
Another study with real-time PCR analysis (some confirmed by western blotting and enzyme-linked immunosorbent assay) of biopsy specimens from patients with UC and CD has shown increased expression levels of IFN-γ, TNF-α, IL-6, IL-15, IL-18, and IL-23 in affected and unaffected areas of IBD mucosa, compared to those found in healthy controls. Conversely, IL-1β, IL-6, IL-12, and IL-27 levels were higher in affected areas compared to unaffected ones in UC mucosa, but not in CD. A correlation between cytokine mRNA levels and inducible nitric oxide synthase and granzyme B has been observed[43].
ADHESION MOLECULES AND MARKERS OF ACTIVATION
Lymphocyte infiltration into the intestinal tract in IBD is mostly mediated by the interaction between α4β7 integrin expressed on lymphocytes and its specific ligand, mucosal vascular addressin CAM-1 (MAdCAM-1), which is expressed on the endothelial cells of the microvasculature in the inflamed intestinal tissue. Integrins form a large family of transmembrane proteins that are required for leukocyte-endothelium interaction, as well as cell-cell interactions in the intestinal mucosa. These molecules together with the NF responsible for the signaling transduction pathway, such as NF-κB and mitogen-activated protein kinase (MAPK), are particularly abundant in the inflamed mucosa in UC and CD.
In one study[55], MAdCAM-1-expressing venules were more abundant in CD than in UC, whereas E-selectin was equally expressed in both diseases. Furthermore, CD was characterized by the presence of MAdCAM-1-expressing venules deep into the intestinal tissue, mainly localized in lymphoid aggregates.
Another group has reported[56] increased endothelial ICAM-1 expression in areas with dense lymphocyte infiltration, and areas close to crypt abscesses and ulcerations in the intestinal mucosa of active IBD patients. Ulcerations were covered by a continuous layer of macrophages and epithelial cells expressing ICAM-1.
We have reported previously[57] CD40 overexpression on mucosal endothelium in CD patients, which was reduced markedly after infliximab treatment, and reached a level similar to that seen in the normal mucosa of control subjects. In the same study, we reported vascular cell adhesion molecule-1 overexpression in the intestinal microvasculature of CD patients, which also disappeared after infliximab treatment.
Nikolaus et al[58] have shown that CD patients that relapse after induction of remission following infliximab administration, are characterized by increased TNF-α secretory capacity and mucosal nuclear NF-κB p65 before reactivation of clinical symptoms. Conversely, extended downregulation of nuclear concentrations of colonic mucosal NF-κB p65 is associated with sustained induction of remission.
Our group has reported increased phosphorylation of all three MAPKs (p38, extracellular signal-regulated kinase and Jun N-terminal kinase) in the microvasculature and mesenchymal cells of bowel preparations from patients with CD and UC, compared to controls and non-inflamed IBD mucosa[59]. In the same study, activation of these major signal transduction pathways was associated, in vitro, with increased production of inflammatory cytokines, as well as increased leukocyte adhesiveness to intestinal endothelial cells and fibroblasts.
IMMUNE CELLS
The uncontrolled inflammatory reaction in IBD is most likely the result of the interplay between genetic deficiencies in the innate immune system and an exaggerated T-cell-driven adaptive immune response[20].
IL-17-positive cells have been detected by immunohistochemical staining in the inflamed mucosa of CD and UC patients[60]. A recent study has confirmed the presence of Th17 cells in CD mucosa but the authors also found a previously unreported subset of mucosal T cells that share features with Th1 and Th17 cells (i.e. cells concomitantly producing IFN-γ and IL-17)[61].
Abnormalities in Tregs in human IBD have been described but are unclear because of the few inconclusive studies reported so far. It has been reported that, in the course of active UC and CD, the number of circulating Tregs is decreased compared to controls[62-64], but these differences do not persist during remission, which suggests that, in active IBD, Tregs migrate to the inflamed gut. In fact, paralleling the clinical activity of the disease, the number of Tregs during UC and CD has been reported to increase in the intestinal lamina propria and mesenteric lymph nodes[62,63,65-67]. One study from Japan has found that the relative proportion of CD4+CD25+ Tregs is significantly increased in patients with active IBD[68], whereas a German study has demonstrated that the frequency of CD4+CD25+ Tregs varies according to IBD activity[62]. In the latter study, Tregs were functional, but their number was reduced in the peripheral circulation and only moderately expanded in the inflamed mucosa.
Neutrophils and monocytic cells also play an important role in the pathogenesis of IBD and in the maintenance of active inflammation. Recently[69], infliximab has been reported to decrease histological disease activity in Crohn’s ileocolitis, by lowering the number of neutrophils and mononuclear cells in intestinal mucosal biopsies. Furthermore, the number of lamina propria mononuclear cells is also reduced because of a global reduction in CD4(+) and CD8(+) T lymphocytes and CD68(+) monocytes.
Mucosal dendritic cells (DCs), the main antigen-presenting cells in the gut, display an activated phenotype in IBD tissues, which is indicative of their involvement in the local chronic inflammatory reaction. In particular, they have been shown to express elevated levels of CD40 in mucosal extracts from UC and CD patients. These levels decrease after patients are treated with anti-TNF-α[70]. Another group[71] has reported an imbalance in intestinal DC subpopulations in a group of pediatric CD patients that underwent surgical bowel resection, following different therapies. In particular, immature DCs (CD11c+CD83-CD68-DC-SIGN+) were only found in non-inflamed control colonic tissue, whereas mature (CD11c+CD83+CD68+DC-SIGN+) DCs were markedly reduced (60% and 30%) in CD tissue samples compared to controls. In addition, tissue samples from CD patients undergoing corticosteroid therapy display marked depletion of DCs compared to tissue from untreated patients or those treated with other drugs. Colonic tissue with severe inflammation shows reduced numbers of CD11c+ and CD83+ DCs in the lamina propria and submucosal compartments, with a concomitant increase in DCs in the muscularis, compared to moderately inflamed and non-inflamed CD tissue[71].
Active CD is also associated with an increased number of macrophages in the ileal and colonic mucosa. A recent study[72] has shown increased numbers of macrophages expressing the scavenger receptor CD163 in colonic mucosa of CD patients concomitantly affected by spondyloarthritis. Macrophages or DCs that express RANK (receptor activator of NF-κB ligand), CD68 and S100 protein are increased in the colon of CD patients, particularly in inflamed areas compared to normal colon[73].
NON-IMMUNE CELLS
Other important cell types that participate in the chronic inflammatory response of IBD, include epithelial, mesenchymal and endothelial cells, and platelets, which exert many of the functions traditionally attributed to classical immune cells, such as cytokine production or expression of major histocompatibility complex class II antigens[18].
Immunohistochemical studies have shown that intestinal epithelial cells (IECs) inappropriately express the class II antigen HLA-DR in actively inflamed mucosa of UC and CD patients[74]. More recently, IBD IECs have been reported to inappropriately express members of the B7 family of costimulatory molecules[56], a finding that suggests alterations in B7-ICOS costimulatory pathways in IBD.
Other studies have shown that, in IECs, expression of toll-like receptor (TLR)3 is significantly downregulated in active CD but not in UC, whereas TLR4 is strongly upregulated in both CD and UC[75]. In the mucosa of patients with postcolectomy active pouchitis, expression of TLR2 and TLR4 is also strongly upregulated[76]. In addition, patients with CD show a reduced content of defensins in the affected ileum, and this reduction is independent from the degree of mucosal inflammation[77].
The involvement of fibroblasts in IBD traditionally has been viewed as being restricted to the production of extracellular matrix components and the pathogenesis of a common and serious complication, such as intestinal fibrosis[78]. However, fibroblasts are also involved in gut injury because they represent a major source of matrix metalloproteinases (MMPs), a family of proteolytic enzymes that are directly responsible for the tissue destruction that occurs during inflammation.
In the course of IBD, upregulation of MMPs occurs in the intestinal tissue, and this increase is lowered significantly by the anti-TNF-α antibody infliximab. These observations have been confirmed by the work of Meijer et al[79]. They have reported increased expression of MMP and tissue inhibitor of metalloproteinase (TIMP) in the intestinal mucosa from patients with IBD, compared with control samples. Furthermore, infliximab downregulated expression of MMP-1, -3 and -9 but not TIMP-1 and -2, depending on genotype.
Wang et al[80] have confirmed these findings. They have shown that mRNA and protein expression of MMP-1 and TNF-α in the ulcerated and inflamed colon mucosa of patients with UC is significantly higher than that in non-inflamed mucosa of normal controls. Furthermore, the expression of MMP-1 and TNF-α in the ulcerated area is significantly higher than that in the inflamed area of patients with UC.
Endothelial cells play an essential role in inflammation as a result of their central gatekeeper function, which controls the quality and quantity of leukocytes that transmigrate from the vasculature into the interstitial space. This process is complex and is mediated by a number of molecules, including cytokines, chemokines and adhesion molecules.
Bardin et al[81] have shown that, in active disease, high expression of CD146 is observed on endothelial cells in intestinal biopsies from patients with CD and UC. In addition, there is a decrease in the soluble form of CD146 in relation to active disease and extent of CD and UC. Lower levels of soluble CD31 have also been detected in UC, but not in CD. This suggests CD146 as a novel marker of the endothelial intercellular junction, which reflects endothelial remodeling more effectively than soluble CD31 does.
Angiogenesis has been suggested to play an integral part in IBD pathology[82]. Vascular endothelial growth factor (VEGF) has long been considered to play a central specific role in angiogenesis. Our group has reported[82] increased microvessel density in IBD mucosa, with an increase in αVβ3 expression on new mucosal vessels. These observations are associated with increased mucosal levels of VEGF, which in turn are able to induce increased angiogenesis in corneal and chorioallantoic membrane assays. Other groups[83] have confirmed our findings, and have shown increased VEGF expression in CD and UC compared to controls. Furthermore, immunohistochemical staining for CD146 is also higher in both forms of IBD, as well as CD34 expression, which indicates a possible role of angiogenesis in the pathogenesis of IBD.
Endothelial junction adhesion molecules, such as CD146, recently have been suggested to play a role in angiogenesis. CD34 is expressed on the vascular endothelium, and is upregulated in IBD.
In active CD and UC, a loss in the expression of endothelial EPCR (the receptor for protein C) and thrombomodulin has been reported, therefore impairing the activated protein C pathway in the intestinal microvasculature[84].
OTHER MUCOSAL COMPONENTS
A positive correlation has been found between mucosal levels of total lactate dehydrogenase (LDH) isoenzyme M monomers and LDH 5 monomers for each of the histological subgroups of UC, while glucose-6-phosphate dehydrogenase activity seems to be independent of inflammatory changes[85].
Peroxisome proliferator-activated receptors (PPARs) are members of the nuclear hormone receptor superfamily of transcription factors whose activities are regulated by high affinity binding of small lipophilic ligands such as steroid hormones. PAR2 methylation status in rectal mucosa has been shown to correlate with more severe disease phenotypes of UC[86].
Mucin 2 (MUC2) precursor biosynthesis and total MUC2 levels are significantly decreased in UC patients with active inflammation, compared to controls. In contrast, both these parameters returned to control values during remission from inflammation, which demonstrates that colonic biosynthesis and total amounts of MUC2 vary according to disease activity. However, MUC2 mRNA levels are similar in all patients and are independent of disease activity, which indicates that these variations in MUC2 synthesis are regulated post-transcriptionally[87].
Immunohistochemical analysis[88] of cryostat sections, using polyclonal and monoclonal antibodies specific for TLR2, TLR4 and CD14, have shown a significant increase in TLR2 expression in the terminal ileum of patients with inactive and active UC compared with controls. Significant upregulation of TLR4 expression relative to controls has been found in the terminal ileum and rectum of UC patients in remission and in the terminal ileum of CD patients with active disease. CD14 expression is upregulated in the terminal ileum of patients with active and inactive CD. It is also upregulated in the cecum of UC patients in remission and with active disease, and in the rectum of patients with active UC.
CONCLUSION
The identification of tissue markers, together with other predictors, is crucial for clinical assessment and management of IBD. Although several attempts have been made, it is clear that more efforts should be made in creating a wider analysis, which involves more IBD centers and patients. To achieve this, a prospective observational study to identify precursors for each subgroup of patients is necessary. More consistent data from immunohistochemistry or western blotting of cytokines on mucosal extracts are needed. Interesting data also can be derived from tissue indicators of activation, such as NF-κB, MAPK or markers of other pathways, which are also involved in IBD pathogenesis. Finally identifying whether an immune or non-immune cell type is involved in mucosal inflammation through specific markers of activation/function, also represents another important aspect to be addressed by further research.
In conclusion, we must admit that, to date, despite great potential, no tissue factor can be considered as a predictor of disease progression or response to therapy in everyday clinical practice devoted to the management of patients with IBD.
Footnotes
Peer reviewers: Dr. Kris Chadee, BSc (Hons), MSc, PhD, Professor, Department of Microbiology and Infectious Diseases, University of Calgary, 3330 Hospital Drive NW, Calgary, T2N 4N1, Canada; Dr. John B Schofield, MB, BS, MRCP, FRCP, Department of Cellular Pathology, Preston Hall, Maidstone, Kent, ME20 7NH, United Kingdom
S- Editor Wang YR L- Editor Kerr C E- Editor Zheng XM
References
- 1.Scaldaferri F, Fiocchi C. Inflammatory bowel disease: progress and current concepts of etiopathogenesis. J Dig Dis. 2007;8:171–178. doi: 10.1111/j.1751-2980.2007.00310.x. [DOI] [PubMed] [Google Scholar]
- 2.Dotan I. Disease behavior in adult patients: are there predictors for stricture or fistula formation? Dig Dis. 2009;27:206–211. doi: 10.1159/000228551. [DOI] [PubMed] [Google Scholar]
- 3.Parsi MA, Achkar JP, Richardson S, Katz J, Hammel JP, Lashner BA, Brzezinski A. Predictors of response to infliximab in patients with Crohn's disease. Gastroenterology. 2002;123:707–713. doi: 10.1053/gast.2002.35390. [DOI] [PubMed] [Google Scholar]
- 4.Su C, Lichtenstein GR. Are there predictors of Remicade treatment success or failure? Adv Drug Deliv Rev. 2005;57:237–245. doi: 10.1016/j.addr.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 5.Esters N, Vermeire S, Joossens S, Noman M, Louis E, Belaiche J, De Vos M, Van Gossum A, Pescatore P, Fiasse R, et al. Serological markers for prediction of response to anti-tumor necrosis factor treatment in Crohn's disease. Am J Gastroenterol. 2002;97:1458–1462. doi: 10.1111/j.1572-0241.2002.05689.x. [DOI] [PubMed] [Google Scholar]
- 6.Taylor KD, Plevy SE, Yang H, Landers CJ, Barry MJ, Rotter JI, Targan SR. ANCA pattern and LTA haplotype relationship to clinical responses to anti-TNF antibody treatment in Crohn's disease. Gastroenterology. 2001;120:1347–1355. doi: 10.1053/gast.2001.23966. [DOI] [PubMed] [Google Scholar]
- 7.Arijs I, Li K, Toedter G, Quintens R, Van Lommel L, Van Steen K, Leemans P, De Hertogh G, Lemaire K, Ferrante M, et al. Mucosal gene signatures to predict response to infliximab in patients with ulcerative colitis. Gut. 2009;58:1612–1619. doi: 10.1136/gut.2009.178665. [DOI] [PubMed] [Google Scholar]
- 8.Van den Brande JM, Koehler TC, Zelinkova Z, Bennink RJ, te Velde AA, ten Cate FJ, van Deventer SJ, Peppelenbosch MP, Hommes DW. Prediction of antitumour necrosis factor clinical efficacy by real-time visualisation of apoptosis in patients with Crohn's disease. Gut. 2007;56:509–517. doi: 10.1136/gut.2006.105379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schmidt C, Giese T, Hermann E, Zeuzem S, Meuer SC, Stallmach A. Predictive value of mucosal TNF-alpha transcripts in steroid-refractory Crohn's disease patients receiving intensive immunosuppressive therapy. Inflamm Bowel Dis. 2007;13:65–70. doi: 10.1002/ibd.20012. [DOI] [PubMed] [Google Scholar]
- 10.Olsen T, Goll R, Cui G, Christiansen I, Florholmen J. TNF-alpha gene expression in colorectal mucosa as a predictor of remission after induction therapy with infliximab in ulcerative colitis. Cytokine. 2009;46:222–227. doi: 10.1016/j.cyto.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 11.Arsenescu R, Bruno ME, Rogier EW, Stefka AT, McMahan AE, Wright TB, Nasser MS, de Villiers WJ, Kaetzel CS. Signature biomarkers in Crohn's disease: toward a molecular classification. Mucosal Immunol. 2008;1:399–411. doi: 10.1038/mi.2008.32. [DOI] [PubMed] [Google Scholar]
- 12.Ishiguro Y. Mucosal proinflammatory cytokine production correlates with endoscopic activity of ulcerative colitis. J Gastroenterol. 1999;34:66–74. doi: 10.1007/s005350050218. [DOI] [PubMed] [Google Scholar]
- 13.Raddatz D, Bockemühl M, Ramadori G. Quantitative measurement of cytokine mRNA in inflammatory bowel disease: relation to clinical and endoscopic activity and outcome. Eur J Gastroenterol Hepatol. 2005;17:547–557. doi: 10.1097/00042737-200505000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Raddatz D, Middel P, Bockemühl M, Benöhr P, Wissmann C, Schwörer H, Ramadori G. Glucocorticoid receptor expression in inflammatory bowel disease: evidence for a mucosal down-regulation in steroid-unresponsive ulcerative colitis. Aliment Pharmacol Ther. 2004;19:47–61. doi: 10.1046/j.1365-2036.2003.01802.x. [DOI] [PubMed] [Google Scholar]
- 15.Hefti MM, Chessin DB, Harpaz NH, Steinhagen RM, Ullman TA. Severity of inflammation as a predictor of colectomy in patients with chronic ulcerative colitis. Dis Colon Rectum. 2009;52:193–197. doi: 10.1007/DCR.0b013e31819ad456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yamamoto T, Umegae S, Kitagawa T, Matsumoto K. Systemic and local cytokine production in quiescent ulcerative colitis and its relationship to future relapse: a prospective pilot study. Inflamm Bowel Dis. 2005;11:589–596. doi: 10.1097/01.mib.0000161917.97136.e2. [DOI] [PubMed] [Google Scholar]
- 17.Targan SR, Landers CJ, Yang H, Lodes MJ, Cong Y, Papadakis KA, Vasiliauskas E, Elson CO, Hershberg RM. Antibodies to CBir1 flagellin define a unique response that is associated independently with complicated Crohn's disease. Gastroenterology. 2005;128:2020–2028. doi: 10.1053/j.gastro.2005.03.046. [DOI] [PubMed] [Google Scholar]
- 18.Danese S, Fiocchi C. Etiopathogenesis of inflammatory bowel diseases. World J Gastroenterol. 2006;12:4807–4812. doi: 10.3748/wjg.v12.i30.4807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nielsen OH, Kirman I, Rüdiger N, Hendel J, Vainer B. Upregulation of interleukin-12 and -17 in active inflammatory bowel disease. Scand J Gastroenterol. 2003;38:180–185. doi: 10.1080/00365520310000672. [DOI] [PubMed] [Google Scholar]
- 20.Bosani M, Ardizzone S, Porro GB. Biologic targeting in the treatment of inflammatory bowel diseases. Biologics. 2009;3:77–97. [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 21.Akazawa A, Sakaida I, Higaki S, Kubo Y, Uchida K, Okita K. Increased expression of tumor necrosis factor-alpha messenger RNA in the intestinal mucosa of inflammatory bowel disease, particularly in patients with disease in the inactive phase. J Gastroenterol. 2002;37:345–353. doi: 10.1007/s005350200048. [DOI] [PubMed] [Google Scholar]
- 22.Casellas F, Papo M, Guarner F, Antolín M, Armengol JR, Malagelada JR. Intraluminal colonic release of immunoreactive tumour necrosis factor in chronic ulcerative colitis. Clin Sci (Lond) 1994;87:453–458. doi: 10.1042/cs0870453. [DOI] [PubMed] [Google Scholar]
- 23.Olsen T, Goll R, Cui G, Husebekk A, Vonen B, Birketvedt GS, Florholmen J. Tissue levels of tumor necrosis factor-alpha correlates with grade of inflammation in untreated ulcerative colitis. Scand J Gastroenterol. 2007;42:1312–1320. doi: 10.1080/00365520701409035. [DOI] [PubMed] [Google Scholar]
- 24.Reimund JM, Wittersheim C, Dumont S, Muller CD, Kenney JS, Baumann R, Poindron P, Duclos B. Increased production of tumour necrosis factor-alpha interleukin-1 beta, and interleukin-6 by morphologically normal intestinal biopsies from patients with Crohn's disease. Gut. 1996;39:684–689. doi: 10.1136/gut.39.5.684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nielsen OH, Køppen T, Rüdiger N, Horn T, Eriksen J, Kirman I. Involvement of interleukin-4 and -10 in inflammatory bowel disease. Dig Dis Sci. 1996;41:1786–1793. doi: 10.1007/BF02088746. [DOI] [PubMed] [Google Scholar]
- 26.Niessner M, Volk BA. Altered Th1/Th2 cytokine profiles in the intestinal mucosa of patients with inflammatory bowel disease as assessed by quantitative reversed transcribed polymerase chain reaction (RT-PCR) Clin Exp Immunol. 1995;101:428–435. doi: 10.1111/j.1365-2249.1995.tb03130.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fukushima K, West G, Fiocchi C. Adequacy of mucosal biopsies for evaluation of intestinal cytokine-specific mRNA. Comparative study of RT-PCR in biopsies and isolated cells from normal and inflamed intestine. Dig Dis Sci. 1995;40:1498–1505. doi: 10.1007/BF02285198. [DOI] [PubMed] [Google Scholar]
- 28.Autschbach F, Braunstein J, Helmke B, Zuna I, Schürmann G, Niemir ZI, Wallich R, Otto HF, Meuer SC. In situ expression of interleukin-10 in noninflamed human gut and in inflammatory bowel disease. Am J Pathol. 1998;153:121–130. doi: 10.1016/S0002-9440(10)65552-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Akagi S, Hiyama E, Imamura Y, Takesue Y, Matsuura Y, Yokoyama T. Interleukin-10 expression in intestine of Crohn disease. Int J Mol Med. 2000;5:389–395. doi: 10.3892/ijmm.5.4.389. [DOI] [PubMed] [Google Scholar]
- 30.Inoue S, Matsumoto T, Iida M, Mizuno M, Kuroki F, Hoshika K, Shimizu M. Characterization of cytokine expression in the rectal mucosa of ulcerative colitis: correlation with disease activity. Am J Gastroenterol. 1999;94:2441–2446. doi: 10.1111/j.1572-0241.1999.01372.x. [DOI] [PubMed] [Google Scholar]
- 31.Melgar S, Yeung MM, Bas A, Forsberg G, Suhr O, Oberg A, Hammarstrom S, Danielsson A, Hammarstrom ML. Over-expression of interleukin 10 in mucosal T cells of patients with active ulcerative colitis. Clin Exp Immunol. 2003;134:127–137. doi: 10.1046/j.1365-2249.2003.02268.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Desreumaux P, Brandt E, Gambiez L, Emilie D, Geboes K, Klein O, Ectors N, Cortot A, Capron M, Colombel JF. Distinct cytokine patterns in early and chronic ileal lesions of Crohn's disease. Gastroenterology. 1997;113:118–126. doi: 10.1016/s0016-5085(97)70116-1. [DOI] [PubMed] [Google Scholar]
- 33.Fuss IJ, Neurath M, Boirivant M, Klein JS, de la Motte C, Strong SA, Fiocchi C, Strober W. Disparate CD4+ lamina propria (LP) lymphokine secretion profiles in inflammatory bowel disease. Crohn's disease LP cells manifest increased secretion of IFN-gamma, whereas ulcerative colitis LP cells manifest increased secretion of IL-5. J Immunol. 1996;157:1261–1270. [PubMed] [Google Scholar]
- 34.Wilde DB, Prystowsky MB, Ely JM, Vogel SN, Dialynas DP, Fitch FW. Antigen-reactive cloned helper T cells. II. Exposure of murine cloned helper T cells to IL 2-containing supernatant induces unresponsiveness to antigenic restimulation and inhibits lymphokine production after antigenic stimulation. J Immunol. 1984;133:636–641. [PubMed] [Google Scholar]
- 35.Camoglio L, Te Velde AA, Tigges AJ, Das PK, Van Deventer SJ. Altered expression of interferon-gamma and interleukin-4 in inflammatory bowel disease. Inflamm Bowel Dis. 1998;4:285–290. doi: 10.1002/ibd.3780040406. [DOI] [PubMed] [Google Scholar]
- 36.Bisping G, Lügering N, Lütke-Brintrup S, Pauels HG, Schürmann G, Domschke W, Kucharzik T. Patients with inflammatory bowel disease (IBD) reveal increased induction capacity of intracellular interferon-gamma (IFN-gamma) in peripheral CD8+ lymphocytes co-cultured with intestinal epithelial cells. Clin Exp Immunol. 2001;123:15–22. doi: 10.1046/j.1365-2249.2001.01443.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Autschbach F, Giese T, Gassler N, Sido B, Heuschen G, Heuschen U, Zuna I, Schulz P, Weckauf H, Berger I, et al. Cytokine/chemokine messenger-RNA expression profiles in ulcerative colitis and Crohn's disease. Virchows Arch. 2002;441:500–513. doi: 10.1007/s00428-002-0684-z. [DOI] [PubMed] [Google Scholar]
- 38.Fantini MC, Monteleone G, Macdonald TT. New players in the cytokine orchestra of inflammatory bowel disease. Inflamm Bowel Dis. 2007;13:1419–1423. doi: 10.1002/ibd.20212. [DOI] [PubMed] [Google Scholar]
- 39.Monteleone G, Monteleone I, Fina D, Vavassori P, Del Vecchio Blanco G, Caruso R, Tersigni R, Alessandroni L, Biancone L, Naccari GC, et al. Interleukin-21 enhances T-helper cell type I signaling and interferon-gamma production in Crohn's disease. Gastroenterology. 2005;128:687–694. doi: 10.1053/j.gastro.2004.12.042. [DOI] [PubMed] [Google Scholar]
- 40.Pizarro TT, Michie MH, Bentz M, Woraratanadharm J, Smith MF Jr, Foley E, Moskaluk CA, Bickston SJ, Cominelli F. IL-18, a novel immunoregulatory cytokine, is up-regulated in Crohn's disease: expression and localization in intestinal mucosal cells. J Immunol. 1999;162:6829–6835. [PubMed] [Google Scholar]
- 41.Siegmund B, Fantuzzi G, Rieder F, Gamboni-Robertson F, Lehr HA, Hartmann G, Dinarello CA, Endres S, Eigler A. Neutralization of interleukin-18 reduces severity in murine colitis and intestinal IFN-gamma and TNF-alpha production. Am J Physiol Regul Integr Comp Physiol. 2001;281:R1264–R1273. doi: 10.1152/ajpregu.2001.281.4.R1264. [DOI] [PubMed] [Google Scholar]
- 42.Izzo RS, Witkon K, Chen AI, Hadjiyane C, Weinstein MI, Pellecchia C. Interleukin-8 and neutrophil markers in colonic mucosa from patients with ulcerative colitis. Am J Gastroenterol. 1992;87:1447–1452. [PubMed] [Google Scholar]
- 43.León AJ, Gómez E, Garrote JA, Bernardo D, Barrera A, Marcos JL, Fernández-Salazar L, Velayos B, Blanco-Quirós A, Arranz E. High levels of proinflammatory cytokines, but not markers of tissue injury, in unaffected intestinal areas from patients with IBD. Mediators Inflamm. 2009;2009:580450. doi: 10.1155/2009/580450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Reinecker HC, Loh EY, Ringler DJ, Mehta A, Rombeau JL, MacDermott RP. Monocyte-chemoattractant protein 1 gene expression in intestinal epithelial cells and inflammatory bowel disease mucosa. Gastroenterology. 1995;108:40–50. doi: 10.1016/0016-5085(95)90006-3. [DOI] [PubMed] [Google Scholar]
- 45.Uguccioni M, Gionchetti P, Robbiani DF, Rizzello F, Peruzzo S, Campieri M, Baggiolini M. Increased expression of IP-10, IL-8, MCP-1, and MCP-3 in ulcerative colitis. Am J Pathol. 1999;155:331–336. doi: 10.1016/S0002-9440(10)65128-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Muehlhoefer A, Saubermann LJ, Gu X, Luedtke-Heckenkamp K, Xavier R, Blumberg RS, Podolsky DK, MacDermott RP, Reinecker HC. Fractalkine is an epithelial and endothelial cell-derived chemoattractant for intraepithelial lymphocytes in the small intestinal mucosa. J Immunol. 2000;164:3368–3376. doi: 10.4049/jimmunol.164.6.3368. [DOI] [PubMed] [Google Scholar]
- 47.Keshavarzian A, Fusunyan RD, Jacyno M, Winship D, MacDermott RP, Sanderson IR. Increased interleukin-8 (IL-8) in rectal dialysate from patients with ulcerative colitis: evidence for a biological role for IL-8 in inflammation of the colon. Am J Gastroenterol. 1999;94:704–712. doi: 10.1111/j.1572-0241.1999.00940.x. [DOI] [PubMed] [Google Scholar]
- 48.Z'Graggen K, Walz A, Mazzucchelli L, Strieter RM, Mueller C. The C-X-C chemokine ENA-78 is preferentially expressed in intestinal epithelium in inflammatory bowel disease. Gastroenterology. 1997;113:808–816. doi: 10.1016/s0016-5085(97)70175-6. [DOI] [PubMed] [Google Scholar]
- 49.Katsuta T, Lim C, Shimoda K, Shibuta K, Mitra P, Banner BF, Mori M, Barnard GF. Interleukin-8 and SDF1-alpha mRNA expression in colonic biopsies from patients with inflammatory bowel disease. Am J Gastroenterol. 2000;95:3157–3164. doi: 10.1111/j.1572-0241.2000.03289.x. [DOI] [PubMed] [Google Scholar]
- 50.Ajuebor MN, Hogaboam CM, Kunkel SL, Proudfoot AE, Wallace JL. The chemokine RANTES is a crucial mediator of the progression from acute to chronic colitis in the rat. J Immunol. 2001;166:552–558. doi: 10.4049/jimmunol.166.1.552. [DOI] [PubMed] [Google Scholar]
- 51.Sans M, Danese S, de la Motte C, de Souza HS, Rivera-Reyes BM, West GA, Phillips M, Katz JA, Fiocchi C. Enhanced recruitment of CX3CR1+ T cells by mucosal endothelial cell-derived fractalkine in inflammatory bowel disease. Gastroenterology. 2007;132:139–153. doi: 10.1053/j.gastro.2006.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Danese S, de la Motte C, Sturm A, Vogel JD, West GA, Strong SA, Katz JA, Fiocchi C. Platelets trigger a CD40-dependent inflammatory response in the microvasculature of inflammatory bowel disease patients. Gastroenterology. 2003;124:1249–1264. doi: 10.1016/s0016-5085(03)00289-0. [DOI] [PubMed] [Google Scholar]
- 53.Kawashima D, Oshitani N, Jinno Y, Watanabe K, Nakamura S, Higuchi K, Arakawa T. Augmented expression of secondary lymphoid tissue chemokine and EBI1 ligand chemokine in Crohn's disease. J Clin Pathol. 2005;58:1057–1063. doi: 10.1136/jcp.2004.024828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zahn A, Giese T, Karner M, Braun A, Hinz U, Stremmel W, Ehehalt R. Transcript levels of different cytokines and chemokines correlate with clinical and endoscopic activity in ulcerative colitis. BMC Gastroenterol. 2009;9:13. doi: 10.1186/1471-230X-9-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Arihiro S, Ohtani H, Suzuki M, Murata M, Ejima C, Oki M, Kinouchi Y, Fukushima K, Sasaki I, Nakamura S, et al. Differential expression of mucosal addressin cell adhesion molecule-1 (MAdCAM-1) in ulcerative colitis and Crohn's disease. Pathol Int. 2002;52:367–374. doi: 10.1046/j.1440-1827.2002.01365.x. [DOI] [PubMed] [Google Scholar]
- 56.Vainer B, Horn T, Nielsen OH. Colonic epithelial cell expression of ICAM-1 relates to loss of surface continuity: a comparative study of inflammatory bowel disease and colonic neoplasms. Scand J Gastroenterol. 2006;41:318–325. doi: 10.1080/00365520510024241. [DOI] [PubMed] [Google Scholar]
- 57.Danese S, Sans M, Scaldaferri F, Sgambato A, Rutella S, Cittadini A, Piqué JM, Panes J, Katz JA, Gasbarrini A, et al. TNF-alpha blockade down-regulates the CD40/CD40L pathway in the mucosal microcirculation: a novel anti-inflammatory mechanism of infliximab in Crohn's disease. J Immunol. 2006;176:2617–2624. doi: 10.4049/jimmunol.176.4.2617. [DOI] [PubMed] [Google Scholar]
- 58.Nikolaus S, Raedler A, Kühbacker T, Sfikas N, Fölsch UR, Schreiber S. Mechanisms in failure of infliximab for Crohn's disease. Lancet. 2000;356:1475–1479. doi: 10.1016/s0140-6736(00)02871-3. [DOI] [PubMed] [Google Scholar]
- 59.Scaldaferri F, Sans M, Vetrano S, Correale C, Arena V, Pagano N, Rando G, Romeo F, Potenza AE, Repici A, et al. The role of MAPK in governing lymphocyte adhesion to and migration across the microvasculature in inflammatory bowel disease. Eur J Immunol. 2009;39:290–300. doi: 10.1002/eji.200838316. [DOI] [PubMed] [Google Scholar]
- 60.Fujino S, Andoh A, Bamba S, Ogawa A, Hata K, Araki Y, Bamba T, Fujiyama Y. Increased expression of interleukin 17 in inflammatory bowel disease. Gut. 2003;52:65–70. doi: 10.1136/gut.52.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Annunziato F, Cosmi L, Santarlasci V, Maggi L, Liotta F, Mazzinghi B, Parente E, Filì L, Ferri S, Frosali F, et al. Phenotypic and functional features of human Th17 cells. J Exp Med. 2007;204:1849–1861. doi: 10.1084/jem.20070663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Maul J, Loddenkemper C, Mundt P, Berg E, Giese T, Stallmach A, Zeitz M, Duchmann R. Peripheral and intestinal regulatory CD4+ CD25(high) T cells in inflammatory bowel disease. Gastroenterology. 2005;128:1868–1878. doi: 10.1053/j.gastro.2005.03.043. [DOI] [PubMed] [Google Scholar]
- 63.Saruta M, Yu QT, Fleshner PR, Mantel PY, Schmidt-Weber CB, Banham AH, Papadakis KA. Characterization of FOXP3+CD4+ regulatory T cells in Crohn's disease. Clin Immunol. 2007;125:281–290. doi: 10.1016/j.clim.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 64.Yokoyama Y, Fukunaga K, Fukuda Y, Tozawa K, Kamikozuru K, Ohnishi K, Kusaka T, Kosaka T, Hida N, Ohda Y, et al. Demonstration of low-regulatory CD25High+CD4+ and high-pro-inflammatory CD28-CD4+ T-Cell subsets in patients with ulcerative colitis: modified by selective granulocyte and monocyte adsorption apheresis. Dig Dis Sci. 2007;52:2725–2731. doi: 10.1007/s10620-006-9560-z. [DOI] [PubMed] [Google Scholar]
- 65.Makita S, Kanai T, Nemoto Y, Totsuka T, Okamoto R, Tsuchiya K, Yamamoto M, Kiyono H, Watanabe M. Intestinal lamina propria retaining CD4+CD25+ regulatory T cells is a suppressive site of intestinal inflammation. J Immunol. 2007;178:4937–4946. doi: 10.4049/jimmunol.178.8.4937. [DOI] [PubMed] [Google Scholar]
- 66.Yu QT, Saruta M, Avanesyan A, Fleshner PR, Banham AH, Papadakis KA. Expression and functional characterization of FOXP3+ CD4+ regulatory T cells in ulcerative colitis. Inflamm Bowel Dis. 2007;13:191–199. doi: 10.1002/ibd.20053. [DOI] [PubMed] [Google Scholar]
- 67.Holmén N, Lundgren A, Lundin S, Bergin AM, Rudin A, Sjövall H, Ohman L. Functional CD4+CD25high regulatory T cells are enriched in the colonic mucosa of patients with active ulcerative colitis and increase with disease activity. Inflamm Bowel Dis. 2006;12:447–456. doi: 10.1097/00054725-200606000-00003. [DOI] [PubMed] [Google Scholar]
- 68.Makita S, Kanai T, Oshima S, Uraushihara K, Totsuka T, Sawada T, Nakamura T, Koganei K, Fukushima T, Watanabe M. CD4+CD25bright T cells in human intestinal lamina propria as regulatory cells. J Immunol. 2004;173:3119–3130. doi: 10.4049/jimmunol.173.5.3119. [DOI] [PubMed] [Google Scholar]
- 69.Baert FJ, D'Haens GR, Peeters M, Hiele MI, Schaible TF, Shealy D, Geboes K, Rutgeerts PJ. Tumor necrosis factor alpha antibody (infliximab) therapy profoundly down-regulates the inflammation in Crohn's ileocolitis. Gastroenterology. 1999;116:22–28. doi: 10.1016/s0016-5085(99)70224-6. [DOI] [PubMed] [Google Scholar]
- 70.Hart AL, Al-Hassi HO, Rigby RJ, Bell SJ, Emmanuel AV, Knight SC, Kamm MA, Stagg AJ. Characteristics of intestinal dendritic cells in inflammatory bowel diseases. Gastroenterology. 2005;129:50–65. doi: 10.1053/j.gastro.2005.05.013. [DOI] [PubMed] [Google Scholar]
- 71.Silva MA, López CB, Riverin F, Oligny L, Menezes J, Seidman EG. Characterization and distribution of colonic dendritic cells in Crohn's disease. Inflamm Bowel Dis. 2004;10:504–512. doi: 10.1097/00054725-200409000-00003. [DOI] [PubMed] [Google Scholar]
- 72.Demetter P, De Vos M, Van Huysse JA, Baeten D, Ferdinande L, Peeters H, Mielants H, Veys EM, De Keyser F, Cuvelier CA. Colon mucosa of patients both with spondyloarthritis and Crohn's disease is enriched with macrophages expressing the scavenger receptor CD163. Ann Rheum Dis. 2005;64:321–324. doi: 10.1136/ard.2003.018382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Franchimont N, Reenaers C, Lambert C, Belaiche J, Bours V, Malaise M, Delvenne P, Louis E. Increased expression of receptor activator of NF-kappaB ligand (RANKL), its receptor RANK and its decoy receptor osteoprotegerin in the colon of Crohn's disease patients. Clin Exp Immunol. 2004;138:491–498. doi: 10.1111/j.1365-2249.2004.02643.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Selby WS, Janossy G, Mason DY, Jewell DP. Expression of HLA-DR antigens by colonic epithelium in inflammatory bowel disease. Clin Exp Immunol. 1983;53:614–618. [PMC free article] [PubMed] [Google Scholar]
- 75.Cario E, Podolsky DK. Differential alteration in intestinal epithelial cell expression of toll-like receptor 3 (TLR3) and TLR4 in inflammatory bowel disease. Infect Immun. 2000;68:7010–7017. doi: 10.1128/iai.68.12.7010-7017.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Toiyama Y, Araki T, Yoshiyama S, Hiro J, Miki C, Kusunoki M. The expression patterns of Toll-like receptors in the ileal pouch mucosa of postoperative ulcerative colitis patients. Surg Today. 2006;36:287–290. doi: 10.1007/s00595-005-3144-y. [DOI] [PubMed] [Google Scholar]
- 77.Wehkamp J, Salzman NH, Porter E, Nuding S, Weichenthal M, Petras RE, Shen B, Schaeffeler E, Schwab M, Linzmeier R, et al. Reduced Paneth cell alpha-defensins in ileal Crohn's disease. Proc Natl Acad Sci USA. 2005;102:18129–18134. doi: 10.1073/pnas.0505256102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Stallmach A, Schuppan D, Riese HH, Matthes H, Riecken EO. Increased collagen type III synthesis by fibroblasts isolated from strictures of patients with Crohn's disease. Gastroenterology. 1992;102:1920–1929. doi: 10.1016/0016-5085(92)90314-o. [DOI] [PubMed] [Google Scholar]
- 79.Meijer MJ, Mieremet-Ooms MA, van Duijn W, van der Zon AM, Hanemaaijer R, Verheijen JH, van Hogezand RA, Lamers CB, Verspaget HW. Effect of the anti-tumor necrosis factor-alpha antibody infliximab on the ex vivo mucosal matrix metalloproteinase-proteolytic phenotype in inflammatory bowel disease. Inflamm Bowel Dis. 2007;13:200–210. doi: 10.1002/ibd.20051. [DOI] [PubMed] [Google Scholar]
- 80.Wang YD, Mao JW. Expression of matrix metalloproteinase-1 and tumor necrosis factor-alpha in ulcerative colitis. World J Gastroenterol. 2007;13:5926–5932. doi: 10.3748/wjg.v13.i44.5926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bardin N, Reumaux D, Geboes K, Colombel JF, Blot-Chabaud M, Sampol J, Duthilleul P, Dignat-George F. Increased expression of CD146, a new marker of the endothelial junction in active inflammatory bowel disease. Inflamm Bowel Dis. 2006;12:16–21. doi: 10.1097/01.mib.0000194181.46930.88. [DOI] [PubMed] [Google Scholar]
- 82.Danese S, Sans M, de la Motte C, Graziani C, West G, Phillips MH, Pola R, Rutella S, Willis J, Gasbarrini A, et al. Angiogenesis as a novel component of inflammatory bowel disease pathogenesis. Gastroenterology. 2006;130:2060–2073. doi: 10.1053/j.gastro.2006.03.054. [DOI] [PubMed] [Google Scholar]
- 83.Tsiolakidou G, Koutroubakis IE, Tzardi M, Kouroumalis EA. Increased expression of VEGF and CD146 in patients with inflammatory bowel disease. Dig Liver Dis. 2008;40:673–679. doi: 10.1016/j.dld.2008.02.010. [DOI] [PubMed] [Google Scholar]
- 84.Scaldaferri F, Sans M, Vetrano S, Graziani C, De Cristofaro R, Gerlitz B, Repici A, Arena V, Malesci A, Panes J, et al. Crucial role of the protein C pathway in governing microvascular inflammation in inflammatory bowel disease. J Clin Invest. 2007;117:1951–1960. doi: 10.1172/JCI31027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Vatn MH, Jellum E, Elgjo K, Bergan A. Enzyme activity and protein patterns as premalignant markers in mucosal biopsy specimens from the large intestine. Scand J Gastroenterol Suppl. 1985;107:1–7. doi: 10.3109/00365528509099746. [DOI] [PubMed] [Google Scholar]
- 86.Tahara T, Shibata T, Nakamura M, Yamashita H, Yoshioka D, Okubo M, Maruyama N, Kamano T, Kamiya Y, Fujita H, et al. Promoter methylation of protease-activated receptor (PAR2) is associated with severe clinical phenotypes of ulcerative colitis (UC) Clin Exp Med. 2009;9:125–130. doi: 10.1007/s10238-008-0025-x. [DOI] [PubMed] [Google Scholar]
- 87.Tytgat KM, van der Wal JW, Einerhand AW, Büller HA, Dekker J. Muc2 in ulcerative colitis: a quantitative study. Biochem Soc Trans. 1995;23:531S. doi: 10.1042/bst023531s. [DOI] [PubMed] [Google Scholar]
- 88.Frolova L, Drastich P, Rossmann P, Klimesova K, Tlaskalova-Hogenova H. Expression of Toll-like receptor 2 (TLR2), TLR4, and CD14 in biopsy samples of patients with inflammatory bowel diseases: upregulated expression of TLR2 in terminal ileum of patients with ulcerative colitis. J Histochem Cytochem. 2008;56:267–274. doi: 10.1369/jhc.7A7303.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]