Abstract
Background
Evidence suggests that caries prevention reduces caries in adults. This study tested the frequency of recommended caries prevention agents for children compared to adult patients.
Methods
This study surveyed 467 Dental Practice-Based Research Network general dentists who practice within the United States and treat both pediatric and adult patients. Dentists were asked the percentage of their patients who are administered or recommended dental sealants, in-office and at-home fluoride, chlorhexidine rinse, and xylitol gum.
Results
Adults were less likely to receive in-office caries preventive agents compared to pediatric patients. However, the rate of recommendation for at-home preventive regimens was very similar. Dentists with a conservative approach to caries treatment were the most likely to use caries prevention at similar rates in adults as in children. In addition, practices with a greater number of patients with dental insurance were significantly less likely to provide in-office fluoride or sealants to adult patients than to their pediatric patients.
Conclusion
In-office caries prevention agents are more commonly used by general dentists for their pediatric patients compared to their adult patients.
Practice Implications
Some general dentists should consider providing additional in-office prevention agents for their adult patients who are at increased risk for dental caries.
Keywords: Caries, Prevention, Adults
INTRODUCTION
A report issued by the Centers for Disease Control and Prevention (CDC) in the United States has stated that fluoride works primarily after teeth have erupted, especially when small amounts are maintained constantly in dental plaque and saliva (1). These conclusions have strong implications for prevention and indicate that adults also benefit from fluoride, rather than only children as was previously speculated. In addition to prevention, current emphasis is on recognizing a carious lesion in its earliest stage before demineralization has produced a cavitated lesion that requires restoration by a dentist (2,3). Data from the Third National Health and Nutritional Survey Interview Survey confirm that dental caries is a major oral health problem beyond childhood and throughout adulthood (4), and imply that optimal caries prevention and management is equally important for both adults and children.
A recent consensus statement regarding caries management indicates that even persons at moderate risk for caries will benefit from caries prevention agents, such as fluoride and antibacterial therapy (5). Several Cochrane reviews have assessed the effectiveness of fluoride toothpastes, gels, varnishes, and mouth rinses and concluded that the evidence on the beneficial effects of topical fluorides is consistent and strong (6). Although most of the studies focused on children and adolescents, a review by Griffin et al. (7) supports the preventive use of fluoride in adults. Additionally, an expert panel assembled by the American Dental Association Council on Scientific Affairs made similar recommendations for the use of topically-applied fluoride for adults as well as children of ages 6-18 years (8). The use of dental sealants is another approach for preventing caries that is well-recognized for children (9,10). Sealants prevent caries onset and arrest caries progression by providing a physical barrier that inhibits microorganisms and food particles from collecting on pits and fissures of tooth surfaces. Evidence-based recommendations by the American Dental Association Council on Scientific Affairs indicate that, in at-risk adults, sealants should be placed on pits and fissures and on early carious lesions to reduce progression (11).
Considering that caries risk continues into adulthood, that fluoride works primarily after teeth have erupted, and that sealants may be as effective in reducing caries in adults as children, it is reasonable to expect the use of preventive agents in adults to reach a level similar to that for children, given equal levels of risk. The Dental Practice-Based Research Network (DPBRN), a large multi-region consortium of practicing dentists allowed us to test this hypothesis in a large sample of general practitioners from multiple areas in the United States. Therefore, the aim of this report is to test the following hypotheses: 1) that dentists use specific caries preventive agents for a greater percentage of pediatric patients than on adult patients; 2) dentists who have the highest rates of preventive agent usage for their pediatric patients are also more likely to use preventive agents for their adult patients, 3) dentists with a more-conservative treatment orientation use caries preventive agents in adults in a frequency more similar to their use in children than dentists with a less-conservative approach, and 4) dentist/patient characteristics and practice patterns are significantly associated with use of child and adult prevention agents.
METHODS
Network Dentists
The DPBRN is a consortium of participating practices and dental organizations committed to advancing knowledge of dental practice and ways to improve it. DPBRN comprises five regions: AL/MS - Alabama/Mississippi; FL/GA - Florida/Georgia; MN - dentists employed by HealthPartners and private practitioners in Minnesota; PDA - Permanente Dental Associates in cooperation with Kaiser Permanente Center for Health Research; and SK - Denmark, Norway, and Sweden (12). Participants of DPBRN were recruited through continuing education courses and mass mailings to licensed dentists from the participating regions. As part of enrollment in DPBRN, all practitioner-investigators completed an enrollment questionnaire about their practice characteristics and themselves. We have demonstrated that DPBRN dentists have much in common with dentists at large (13).
Procedure
An “Assessment of Caries Diagnosis and Caries Treatment” questionnaire was sent to eligible DPBRN dentists. The questionnaire asked a range of questions, including caries-related diagnostic and clinical decision-making processes, caries risk assessment, and use of prevention techniques. A preliminary version of the questionnaire was administered to 16 DPBRN dentists to assess feasibility and comprehension of each questionnaire item. A subsequent pilot study finalized documentation of comprehension and item test-retest reliability across 15 days using a sample of 35 DPBRN dentists. All items in the final version met a test-retest reliability cutoff of kappa > 0.7. This current report presents results on the use of preventive agents. The full questionnaire is available at http://www.dpbrn.org/users/publications/Supplement.aspx.
Pre-printed survey packages were sent to the 932 network dentists who had completed the DPBRN Enrollment Questionnaire and reported doing at least some restorative dentistry. Dentists were asked to complete the questionnaire and return it to their assigned Regional Coordinator in a pre-addressed envelope. Once returned, questionnaires were reviewed for completeness, with practitioners contacted to verify illegible or unclear responses.
Practitioner-investigators were asked to return the questionnaire within three weeks. A reminder letter was sent after the third week if the questionnaire had not been returned. After an additional three weeks, a second reminder was sent. After a final three-week waiting period, it was assumed that he or she was not interested in participating.
This study reports on the 467 practitioner-investigators who practiced within the United States, were general dentists, and who reported that they perform in their practices restorative dentistry procedures on both adult and pediatric patients. Dentists from the Scandinavian region were excluded because of potential differences in practice patterns associated with greater prevention orientation of these countries (14).
Measures
Table 1 presents the series of questions about the use of caries preventive agents. A child-adult prevention index was defined as the difference between the percentages of children and adults that receive each preventive agent by that dentist. A positive value reflects greater use of preventive agents in children relative to adult patients, 0 would reflect equal rates of use, and a negative number means greater use in adult patients.
Table 1.
Questions asked about caries prevention.
ADULTS: Of patients more than 18 years old with at leastone posterior tooth, for what percentage do you:
|
|
CHILDREN: Of patients 6 to 18 years old for what percentage do you: The same questions as asked above, but replacing the first questions with:
|
Dentist/patient/practice characteristics of gender, years since dental school graduation, number of chairs in the office, percent of practice time spent on non-implant restorations, number of days a new patient has to wait for a new patient examination appointment, payment type (percent of patients that use dental insurance, public insurance, self-payment), percent of patients that are given individualized caries preventive treatment, whether caries risk is assessed in any way, and percent of patients in each age cohort (1-17, 18-44, 45-64, 65+) were assessed.
Practice patterns included whether caries risk assessment was performed for individual patients, importance of age when deciding on a treatment plan (asked for patients ages 6-17 and 18 and older), the percentage of patients that are interested in individualized preventive treatment, the percentage of patients that receive individualized preventive treatment, and the dentist’s rating of the importance of age when deciding on a treatment plan (asked for patients ages 6-17 and 18 and older).
Treatment decision scenarios
Dentists were asked to select the treatment codes they would recommend for clinical scenarios involving an existing restoration (Figure 1) and un-restored coronal caries (Figures 2). Response for the treatment choices are shown in Table 2.
Figure 1. Restoration scenario.
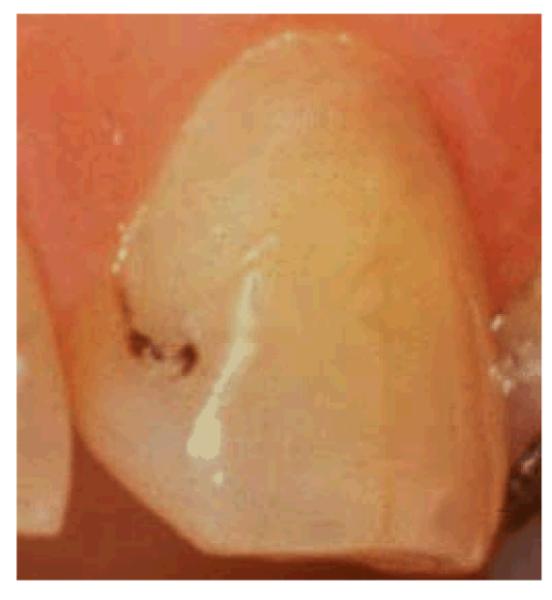
The patient is a 30-year old female with no relevant medical history. She has no complaints and is in your office today for a routine visit. She has attended your practice on a regular basis for the past 6 years. She has no other restorations than the one shown, no dental caries, and is not missing any teeth.
Reprinted from Mjör and Toffenetii, 2000,33 with permission
Figure 2. Coronal caries scenario.
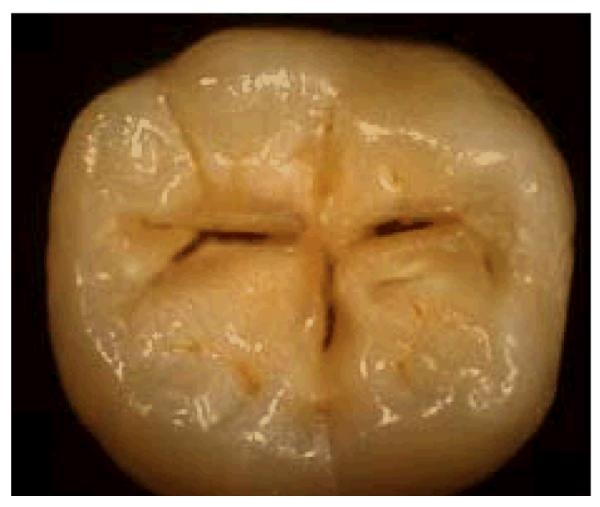
The patient is a 30-year old female with no relevant medical history. She has no complaints and is in your office today for a routine visit. She has attended your practice on a regular basis for the past 6 years. She has no other teeth with dental restoration or dental caries and is not missing any teeth.
Reprinted from Espelid et al, 1997,34 with permission
Table 2.
Treatment scenarios and use of preventive agents.
| Treatment choice | n (%) | Child-adult prevention index |
|---|---|---|
| Restoration scenario (n=455) | ||
| Prevention and polish/repair | 56 (12%) | 18%a |
| Prevention only | 26 (6%) | 38% a |
| Polish/repair only | 185 (41%) | 51%b |
| Replace restoration | 167 (37%) | 54% b |
| No treatment | 21 (5%) | 60% b |
| Coronal caries scenario (n=463) | ||
| Prevention only | 11 (2%) | 35% a |
| Drill/prevention | 230 (51%) | 44% a |
| No treatment | 22 (5%) | 51% |
| Restoration | 201 (53%) | 53% b |
Nine dentists did not complete the restoration scenario and one failed to complete the coronal caries scenario.
Values with different superscripts are significantly different at p. < .05.
Dentists who endorsed multiple treatment choices are scored as the most invasive treatment (e.g., restoration and a method of prevention are scored as having chosen restoration).
Restoration scenario. Treatment choices included no treatment; fluoride; sealant; chlorhexidine; polish, resurface or repair restoration but not replace; and replace restoration. Coded “not replace”=1 and “replace”=2 in the multivariate models.
Coronal caries scenario. Treatment choices of minimal drilling and sealant, minimal drilling and preventive resin restoration, air abrasion and a sealant, and air abrasion and preventive resin restoration are shown as drill/prevention. Coded “not restore”=1 and “restore”=2 in the multivariate models.
Statistical methods
The percentages for each caries prevention methodology were coded to the categories’ median to maintain the interval nature of the data so that parametric statistics could be used: 0 percent=0, 1-24 percent=12.5, 25-49 percent=37, 50-74 percent=62, 75-99 percent=87, 100 percent=100. As hypothesis #1 proposes a within-subject comparison (that each dentist uses a specific caries preventive agent on a greater percentage of pediatric patients than adult patients), paired samples t-tests were used. The Spearman correlation coefficient was used to test for an association between the use of specific caries prevention agents in children and adults within each practice (hypothesis #2). To test hypotheses 3 and 4, first correlation coefficients were calculated between patient/dentist characteristics, practice pattern, and clinical scenario variables and the child-adult prevention index. Variables that were significant at the univariate level (p < .05) were carried forward to multivariate regression models for each preventive agent. All analyses were performed with SPSS Version 17.
RESULTS
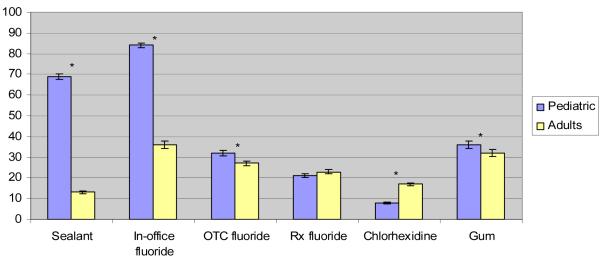
Of the 932 DPBRN practitioner-investigators who were eligible, a total of 534 responded, for an overall return rate of 57 percent. There were no participation differences by gender, area of specialty, or years since dental school graduation. Practice characteristics of participating dentists are presented in Table 3. Table 4 and Figure 3 present the frequency of preventive techniques by network practices on adult and pediatric patients. Dental sealants and in-office fluorides were used more often in pediatric patients than in adult patients (P. < .001). Non-prescription fluoride rinse and xylitol gum was recommended more often for pediatric patients than adults patients (P. < .001). There was no difference in the percentage of pediatric or adult patients who were provided with a prescription for some form of fluoride (P. = .06). An at-home regimen of chlorhexidine rinse was recommended to significantly less pediatric patients than adult patients (P. < .001).
Table 3.
Practice characteristics
| Variable | Mean or % |
|---|---|
| Gender (male) | 85% (n=392) |
| Years since dental school graduation | 23.1 (SD=10.5) |
| Full-time (32+ hours per week in patient care) | 84% (n=389) |
| Dental chairs per office (n=457) | 4.5 (SD=2.1) |
| Race/ethnicity of dentist (n=460) | |
| White | 90% (n=414) |
| African American | 4% (n=16) |
| Hispanic | 2% (n=11) |
| Asian | 2% (n=9) |
| Other | 2% (n=9) |
| Time spent on non-implant restorations (n=457) | 61% (SD=19) |
| Days wait for examination appointment (n=449) | 11.3 (SD=15) |
| Patients seen each week (n=450) | 48.5 (SD=27) |
| Age of patients | |
| Percent of patients ages 1-18 years (n=451) | 19% (SD=12) |
| Percent of patients ages 19-44 years (n=451) | 32% (SD=13) |
| Percent of patients ages 45-64 years (n=451) | 33% (SD=12) |
| Percent of patients ages 65 years and older (n=448) | 16% (SD=13) |
| Patients who self-pay (n=435) | 23% (SD=18) |
| Patients who have dental insurance (n=445) | 62% (SD=22) |
| Dentists who provide some form of caries risk assessment (n=467) | 69% |
| Patients who receive individual caries prevention (n=467) | 51% (SD=29) |
Table 4.
Percent of patients within a practice for each caries preventive agent.
| Pediatric patients Mean % (SD) |
Adult patients Mean % (SD) |
Difference (95% CI) Child– Adult Index* |
|
|---|---|---|---|
| Dental sealant | 69.5% (28.1) | 13.6% (17.9) | 55.8% (53.2, 58.4) |
| In-office fluoride | 84.1% (22.8) | 36.2% (34.7) | 47.9% (44.7, 51.2) |
| Non-prescription fluoride | 31.4% (27.1) | 26.3% (24.4) | 5.0% (3.0, 7.0) |
| Prescription fluoride | 21.2% (21.1) | 23.0% (20.4) | −1.7% (−3.4, 0.1) |
| Chlorhexidine rinse | 7.7% (7.8) | 17.3% (14.7) | −9.6% (−10.9, −8.4) |
| Xylitol gum | 35.3% (37.0) | 32.2% (34.8) | 3.2% (1.6, 4.7) |
The child-adult prevention index is also the difference score which is testing in the paired samples t-test.
Figure 3.
Percent of pediatric and adult patients receiving caries risk prevention.
* Significant difference p<.001. Error bars are SE.
Significant positive correlations were found for all adult-pediatric pairs for each of the caries preventive agents supporting hypothesis #2. The correlation coefficients were as follows: sealant, r=.36, P < .001; in-office fluoride, r=.32, P < .001; non-prescription fluoride rinse, r=.66, P < .001; prescription fluoride, r=.62, P < .001; chlorhexidine rinse, r=.39, P < .001; sugarless or xylitol gum, r=.90, P < .001. This suggests that dentists’ propensities for using and recommending caries prevention were similar for all of the preventive agents, but the pattern was strongest for the at-home treatments.
Factors associated with child-adult prevention differences
The child-adult prevention index was calculated for sealants (55.8%), in-office fluorides (47.9%), non-prescription fluoride (5.0%), prescription fluoride (−1.7%), and chlorhexidine rinse (−9.6%), xylitol gum (3.2%) (see Table 4).
Regression coefficients are presented in Table 5. For sealants, practices with a higher percentage of patients with dental insurance (β = 2.645) and fewer-days wait for an examination appointment (β = −.378) were associated with a higher child-adult prevention index. For in-office fluoride, dentist’s male gender (β = −12.289), a higher percentage of patients with dental insurance (β = 2.794), fewer days wait for an examination appointment (β = −.422), greater time spent performing non-implant restorations (β = 1.821), not performing risk assessment (β = −15.824), providing individualized caries prevention (β = −.164), as well as the replacement clinical scenario (β = 2.280) and the new restoration scenario (β = 2.267) were associated with a higher child-adult prevention index. For prescription fluoride, dentist’s female gender (β = −7.964) and a higher percentage of patients who self-pay (β = −.818) were associated with a higher child-adult prevention index. For chlorhexidine, dentist’s female gender (β = −4.725), a higher percentage of patients who self-pay (β = −.706), time spent performing non-implant restorations (β = 1.744), and performing risk assessment (β = 3.647) were associated with a higher child-adult prevention index.
Table 5.
Regression coefficients for dentist/patient characteristics and practice patterns associated with the child-adult prevention index.
| Predictor | β (SE) | P value |
|---|---|---|
| Sealants [F (8,432) = 10.384, p<.001, R2 = 10.4] | ||
| Percentage of patients with dental insurance | 2.645 (.572) | < .001 |
| Days wait for examination appointment | −.378 (.181) | .044 |
| In-office fluoride [F (9,421) = 9.458, p<.001,R2 = 13.9] | ||
| Gender | −12.289 (4.681) | .009 |
| Percentage of patients with dental insurance | 2.794 (1.371) | .042 |
| Days wait for examination appointment | −.422 (.108) | <.001 |
| Percentage of time spent on non-implant restorations | 1.821 (.899) | .043 |
| Caries risk assessment is performed | −15.824 (2.820) | <.001 |
| Give individualized caries prevention | −.164 (.050) | .001 |
| Clinical replacement scenario | 2.280 (.873) | .009 |
| Clinical new restoration scenario | 2.267 (1.128) | .045 |
| Prescription fluoride [F (4,439) = 7.787, p<.001,R2 = 8.8] | ||
| Gender | −7.964 (2.500) | .002 |
| Percentage of patients who self-pay | −.818 (.407) | .045 |
| Chlorhexidine [F (7,431) = 11.000, p<.001, R2 = 12.1] | ||
| Gender | −4.725 (1.809) | .009 |
| Percentage of patients who self-pay | −.706 (.296) | .018 |
| Percent age of time spent on non-implant restorations | 1.744 (.351) | .001 |
| Caries risk assessment is performed | 3.647 (1.056) | .001 |
Large positive values for thechild-adult prevention index (the dependent variable) indicates a higher percentage of children receive that preventive agent compared to adults.
β should be interpreted to represent the increase in percentage of the index when the predictor variable is increased 1 unit (e.g., one day additional wait time for an examination appointment).
Dichotomous variables were coded as follows: Gender (male=1, female=2), Caries risk assessment (performed =1, not performed=2), Replacement scenario (not replace=1, replace=2), Coronal caries scenario (not restore=1, restore=2).
DISCUSSON
Many studies have reported on the use of caries preventive agents in children (6,11,15-20) whereas others have reported on their effectiveness in achieving improved oral outcomes (9,21-24). Fewer studies have focused on the use of prevention in adults (25-28). This study found that dentists report that adults are significantly less likely to receive in-office caries preventive treatments compared to pediatric patients. Specifically, pediatric patients are more than twice as likely to receive an in-office treatment involving fluoride and four times as likely to have a dental sealant applied than adults. These findings seem to go against recent practice recommendations that support similar risk-based treatment decision making for children as adults (4,8). We did find that dentists who most often used caries preventive agents in children were also the most frequent users for adults, and the pattern was strongest for at-home treatments. The variability in preventive rates for children compared to adult patients within practices suggests a wide range of caries prevention philosophies.
From these data it appears that dentists may not view in-office caries prevention to be as effective for adults as for children, despite the current view that these treatments are useful in not only prevention of caries onset, but also in preventing the progression of early non-cavitated carious lesions (1-3). Our treatment scenarios identified that a subset of dentists who practice a conservative approach to caries treatment were those who most commonly use in-office fluoride with adults.
A study of Indiana dentists and hygienists provides a look at the extent to which the CDC report influenced clinical use of fluoride in adults using data from two cross-sectional surveys (29). These researchers surveyed oral heath practitioners prior to the 2001 release of recommendations for the use of fluoride, and in 2005, four years later following the release of this information. They found that 4 years after the release of these recommendations, a considerable proportion of dental professionals in Indiana still did not understand fluoride’s predominant mode of action. This study also failed to find a correlation between correctly identifying fluoride’s predominant mode of action and the frequency of providing fluoride for adults at moderate or high caries risk. In both 2000 and 2005, 61 percent of dentists said they “always or usually” use fluoride on adults with recent or active caries.
To our surprise, increased use of in-office preventive agents in adults was not associated with recency of graduation from dental school. Certainly, educational organizations including the American Dental Education Association currently support increased use of caries prevention in adults (30). However, clinical training may differ from national-level recommendations. In a review of dental school curriculum, Brown (30) reported that although 65 percent of schools included re-mineralization procedures in their clinical courses, only 38 percent specifically re-evaluated this outcome. Brown acknowledges the existence of several barriers in achieving changes in teaching of prevention and speculated that faculty lack awareness of the existing evidence base. He suggested that some faculty perceive profitability of the oral health care system as negatively impacted since the fee-for-service-driven treatments do not always change with information on disease etiology and outcomes.
It is likely that economics are considered in dentist’s treatment decisions. These data indicated that busier offices and those with a greater number of patients who have dental insurance were associated with increased use of in-office fluoride in adults. Fiset and colleagues (31) examined the influence of reimbursement in the use of fluoride. They tested whether reimbursement increased general dentists’ use of fluoride varnish before and after the institution of payment for fluoride varnish in the state of Washington. Thirty-two percent of dentists used fluoride varnish regularly before reimbursement began, whereas 44 percent of dentists regularly used fluoride varnish 2 years after the program began. The fact that there was no change in dentists’ rates of use of other caries-control services (chlorhexidine rinses for caries control and adult pit-and-fissure sealants) suggests that the increase was specific to the reimbursement for fluoride, not an overall increase in the use of prevention. However, fluoride varnish was still only used by a minority of dentists in the study.
Several limitations to this data should be noted. First, it is unknown to what extent decisions to use preventive agents versus restore or replace the restoration in a 30-year-old patient will be generalizable to young adults, middle-aged people, elderly and the frail elderly. Although the differences in rates for prescribing fluoride or recommending xylitol gum may be statistically different, these differences are small. It should be noted that the majority of the sample is male; however, this reflects the current gender distribution of the dental profession in the United States. Additionally, the study sample is not a random sample of general dentists in the United States. Consequently, the extent to which these findings generalize to this population cannot be stated with certainty. Based on comparisons to dentists who responded to the 2004 ADA Survey of Dental Practice, DPBRN dentists have much in common with dentists at large (13). The only key characteristic with a statistically significant difference seems to be that DPBRN dentists tend to have a more-recent year of graduation from dental school than dentists at large. DPBRN dentists certainly represent a substantial diversity with regard to practice settings, patient populations, rural-urban area of residence, and geographic locations. Participation rate was lowest in the AL/MS region and the majority of dentists recruited in that region were enrolled in DPBRN to participate in other studies before DPBRN became a network that comprises five regions, and this may explain their lower participation rate. However, the interpretation of these results was similar in exploratory analyses in which dentists from this region were not included. This paper is based in the assumption that pediatric and adult patients seen in each practice have approximately the same risk profiles. Dentists who use caries prevention in equivalent percentages of pediatric and adult patients represent practices with a more-conservative philosophy of caries treatment for adults and subscribe to the premise that caries prevention is as important for adults as it is for pediatric patients.
Summary and recommendations
This study suggests that most general dentists have not increased the use of in-office prevention agents for adults, whereas at-home regimens are equally recommended for adults as for pediatric patients. The use of preventive agents in general clinical practice must be promoted by the continual education and endorsement through public health agencies, dental schools, and state and national dental associations.
This study found that:
For children, fluoride is used for in-office caries prevention more than twice as often as for adults, and they are four times as likely as adults to have a dental sealant applied.
The frequency of use of at-home fluorides was relatively similar between children and adults.
Chlorhexidine rinse was infrequently recommended, and seldom to children.
Dentists who often used and recommended caries prevention for children were most likely to also use or recommend them for adults.
Dentists with a conservative approach to caries treatment were the most likely to use in-office caries prevention at similar rates in adults as in children.
Acknowledgement
This investigation was supported by National Institutes of Health, National Institute of Dental and Craniofacial Research grants U01-DE-16746 and U01-DE-16747. An Internet site devoted to details about DPBRN is located at www.DPBRN.org. Opinions and assertions contained herein are those of the authors and are not to be construed as necessarily representing the views of the respective organizations or the National Institutes of Health. The informed consent of all human subjects who participated in this investigation was obtained after the nature of the procedures had been explained fully.
Footnotes
The DPBRN Collaborative Group comprises practitioner-investigators, faculty investigators, and staff members who contributed to this DPBRN activity. A list of these persons is at http://www.dpbrn.org/users/publications/Default.aspx
Contributor Information
Joseph L. Riley, III, Department of Community Dentistry and Behavioral Science, College of Dentistry, University of Florida, Gainesville, Florida, USA..
Valeria V. Gordan, Department of Operative Dentistry, College of Dentistry, University of Florida, Gainesville, Florida, USA..
D. Brad Rindal, HealthPartners, Minneapolis, Minnesota, USA..
Jeffrey L. Fellows, Center for Health Research, Kaiser Permanente Northwest, Portland, Oregon, USA..
O. Dale Williams, Professor and Director of the Division of Preventive Medicine, University of Alabama at Birmingham, Birmingham, Alabama, USA.
Lloyd K. Ritchie, Jr., Private Practitioner in Pensacola, Florida, USA.
Gregg H. Gilbert, Department of General Dental Sciences, School of Dentistry, University of Alabama at Birmingham, Birmingham, Alabama, USA..
References
- 1.Centers for Disease Control and Prevention Recommendations for using fluoride to prevent and control dental caries in the United States. MMWR. 2001;50(RR-14):1–42. [PubMed] [Google Scholar]
- 2.Anusavice KJ. Present and future approaches for the control of caries. J Dent Educ. 2005;69(5):538–54. [PubMed] [Google Scholar]
- 3.Bader JD, Shugars DA. The evidence supporting alternative management strategies for early occlusal caries and suspected occlusal dentinal caries. J Evid Based Dent Pract. 2006;6(1):91–100. doi: 10.1016/j.jebdp.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 4.Macek MD, Heller KE, Selwitz RH, Maz MC. Is 75 percent of dental caries really found in 25 percent of the population? J Public Health Dent. 2004;64(1):20–5. doi: 10.1111/j.1752-7325.2004.tb02721.x. [DOI] [PubMed] [Google Scholar]
- 5.Young DA, Featherstone JD, Roth JR, Anderson M, Autio-Gold J, Christensen GJ, Fontana M, Kutsch VK, Peters MC, Simonsen RJ, Wolff MS. Caries management by risk assessment: implementation guidelines. J Calif Dent Assoc. 2007;35(11):799–805. [PubMed] [Google Scholar]
- 6.Marinho VC, Higgins JP, Logan S, Sheiham A. Systematic review of controlled trials on the effectiveness of fluoride gels for the prevention of dental caries in children. J Dent Educ. 2003;67(4):448–58. [PubMed] [Google Scholar]
- 7.Griffin SO, Regnier E, Griffin PM, Huntley V. Effectiveness of fluoride in preventing caries in adults. J Dent Res. 2007;86(5):410–5. doi: 10.1177/154405910708600504. [DOI] [PubMed] [Google Scholar]
- 8.American Dental Association Council on Scientific Affairs Professionally applied topical fluoride: Evidence-based clinical recommendations. JADA. 2006;137:1151–59. doi: 10.14219/jada.archive.2006.0356. [DOI] [PubMed] [Google Scholar]
- 9.Ahovuo-Saloranta A, Hiiri A, Nordblad A, Worthington H, Mäkelä M. Pit and fissure sealants for preventing dental decay in the permanent teeth of children and adolescents. Cochrane Database Syst Rev. 2004;(3) doi: 10.1002/14651858.CD001830.pub2. CD001830. [DOI] [PubMed] [Google Scholar]
- 10.Simonsen RJ. Pit and fissure sealant: review of the literature. Pediatr Dent. 2002;24(5):393–414. [PubMed] [Google Scholar]
- 11.Beauchamp J, Caufield PW, Crall JJ, Donly K, Feigal R, Gooch B, Ismail A, Kohn W, Siegal M, Simonsen R, American Dental Association Council on Scientific Affairs Evidence-based clinical recommendations for the use of pit-and-fissure sealants: a report of the American Dental Association Council on Scientific Affairs. JADA. 2008;139(3):257–68. doi: 10.14219/jada.archive.2008.0155. [DOI] [PubMed] [Google Scholar]
- 12.Gilbert GH, Williams OD, Rindal DB, Pihlstrom DJ, Benjamin PL, Wallace MC, DPBRN Collaborative Group The creation and development of The Dental Practice-Based Research Network. JADA. 2008;139(1):74–81. doi: 10.14219/jada.archive.2008.0024. [DOI] [PubMed] [Google Scholar]
- 13.Makhija SK, Gilbert GH, Rindal DB, Benjamin PL, Richman JS, Pihlstrom DJ, for the DPBRN Collaborative Group Dentists in practice-based research networks have much in common with dentists at large: evidence from The Dental Practice-Based Research Network. Gen Dent. 2009;57(3):270–275. [PMC free article] [PubMed] [Google Scholar]
- 14.Burt BA. Prevention policies in the light of the changed distribution of dental caries. Acta Odontol Scand. 1998;56(3):179–86. doi: 10.1080/000163598422956. [DOI] [PubMed] [Google Scholar]
- 15.Brown LJ, Kaste LM, Selwitz RH, Furman LJ. Dental caries and sealant usage in U.S. children, 1988-1991: selected findings from the Third National Health and Nutrition Examination Survey. JADA. 1996;127:335–43. doi: 10.14219/jada.archive.1996.0203. [DOI] [PubMed] [Google Scholar]
- 16.Primosch RE, Barr ES. Sealant use and placement techniques among pediatric dentists. JADA. 2001;132(10):1442–51. doi: 10.14219/jada.archive.2001.0061. [DOI] [PubMed] [Google Scholar]
- 17.Dasanayake AP, Li Y, Philip S, Kirk K, Bronstein J, Childers NK. Utilization of dental sealants by Alabama Medicaid children: barriers in meeting the year 2010 objectives. Pediatr Dent. 2001;23(5):401–6. [PubMed] [Google Scholar]
- 18.Helminen SK, Vehkalahti MM. Does caries prevention correspond to caries status and orthodontic care in 0- to 18-year-olds in the free public dental service? Acta Odontol Scand. 2003;61(1):29–33. doi: 10.1080/ode.61.1.29.33. [DOI] [PubMed] [Google Scholar]
- 19.Cherry-Peppers G, Gift HC, et al. Sealant use and dental utilization in U.S. children. J Dent Child. 1995;62:250–5. [PubMed] [Google Scholar]
- 20.Siegal MD, Garcia AI, Kandray DP, Giljahn LK. The use of dental sealants by Ohio dentists. J Public Health Dent. 1996;56(1):12–21. doi: 10.1111/j.1752-7325.1996.tb02389.x. [DOI] [PubMed] [Google Scholar]
- 21.Oong EM, Griffin SO, Kohn WG, Gooch BF, Caufield PW. The effect of dental sealants on bacteria levels in caries lesions: a review of the evidence. JADA. 2008;139(3):271–8. doi: 10.14219/jada.archive.2008.0156. [DOI] [PubMed] [Google Scholar]
- 22.Mejàre I, Lingström P, Petersson LG, Holm AK, Twetman S, Källestål C, Nordenram G, Lagerlöf F, Söder B, Norlund A, Axelsson S, Dahlgren H. Caries-preventive effect of fissure sealants: a systematic review. Acta Odontol Scand. 2003;61(6):321–30. doi: 10.1080/00016350310007581. [DOI] [PubMed] [Google Scholar]
- 23.Zhang Q, van Palenstein Helderman WH, van’t Hof MA, Truin GJ. Chlorhexidine varnish for preventing dental caries in children, adolescents and young adults: a systematic review. Eur J Oral Sci. 2006;114(6):449–55. doi: 10.1111/j.1600-0722.2006.00392.x. [DOI] [PubMed] [Google Scholar]
- 24.Petersson LG, Twetman S, Dahlgren H, Norlund A, Holm AK, Nordenram G, Lagerlöf F, Söder B, Källestål C, Mejàre I, Axelsson S, Lingström P. Professional fluoride varnish treatment for caries control: a systematic review of clinical trials. Acta Odontol Scand. 2004;62(3):170–6. doi: 10.1080/00016350410006392. [DOI] [PubMed] [Google Scholar]
- 25.Brennan DS, Spencer AJ. Service patterns associated with coronal caries in private general dental practice. J Dent. 2007;35(7):570–7. doi: 10.1016/j.jdent.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 26.Brennan DS, Spencer AJ. The role of dentist, practice and patient factors in the provision of dental services. Community Dent Oral Epidemiol. 2005;33(3):181–95. doi: 10.1111/j.1600-0528.2005.00207.x. [DOI] [PubMed] [Google Scholar]
- 27.Simecek JW, Diefenderfer KE, Ahlf RL, Ragain JC., Jr. Dental sealant longevity in a cohort of young U.S. naval personnel. JADA. 2005;136(2):171–8. doi: 10.14219/jada.archive.2005.0138. [DOI] [PubMed] [Google Scholar]
- 28.Fiset L, Grembowski D, Del Aguila M. Third-party reimbursement and use of fluoride varnish in adults among general dentists in Washington State. JADA. 2000;131(7):961–8. doi: 10.14219/jada.archive.2000.0314. [DOI] [PubMed] [Google Scholar]
- 29.Yoder KM, Maupome G, Ofner S, Swigonski NL. Knowledge and use of fluoride among Indiana dental professionals. J Public Health Dent. 2007;67(3):140–7. doi: 10.1111/j.1752-7325.2007.00037.x. [DOI] [PubMed] [Google Scholar]
- 30.Brown JP. A new curriculum framework for clinical prevention and population health, with a review of clinical caries prevention teaching in U.S. and Canadian dental schools. J Dent Educ. 2007;71(5):572–8. [PubMed] [Google Scholar]
- 31.Fiset L, Grembowski D. Adoption of innovative caries-control services in dental practice: a survey of Washington state dentists. JADA. 1997;128:337–45. doi: 10.14219/jada.archive.1997.0197. [DOI] [PubMed] [Google Scholar]
- 32.Pitts NB. Clinical diagnosis of dental caries: a European perspective. J Dent Educ. 2001;65(10):972–8. [PubMed] [Google Scholar]
- 33.Mjör IA, Toffenetti F. Secondary caries: A literature review with case reports. Quintessence Int. 2000;31:165–179. [PubMed] [Google Scholar]
- 34.Espelid I, Tveit AB, Mejáre I, Nyvad B. Caries - New knowledge or old truths? Nor Dent J. 1997;107:66–74. [Google Scholar]