Abstract
Objectives: To examine whether Oppositional Defiant Disorder (ODD) rather than CD may explain the comorbidity between behavioral disorders and depression; to test whether distinct affective and behavioral dimensions can be discerned within the symptoms of ODD; and to determine if an affective dimension of ODD symptoms is specifically predictive of later depression.
Method: The dimensions of ODD and their prediction to later CD and depression were examined in a community sample of 2,451 girls between the ages of 5 and 8, followed up annually over a five year period, using parent, child and teacher questionnaire ratings of the severity of symptoms of psychopathology.
Results: Dimensions of negative affect, oppositional behavior and antagonistic behavior were found within ODD symptoms. Negative affect predicted later depression. Oppositional and antagonistic behavior predicted CD overall, and for Caucasian girls, negative affect also predicted later CD. CD was not predictive of later depression, controlling for comorbid conditions.
Conclusions: ODD plays a key role in the early development of psychopathology. It is central in the comorbidity between internalizing and externalizing psychopathology, which may be due to a dimension of negative affective symptoms within ODD. How this dimension relates to later CD appears to vary by race.
Keywords: Oppositional Defiant Disorder, Depression, Conduct Disorder, Comorbidity
Conduct Disorder (CD) has long been observed to be frequently comorbid with depression,1,2 giving rise to a number of differing explanatory models. Rutter and colleagues (1970; as cited in Puig-Antich, 1982)3 described 21% of the children in the Isle of Wight study as “mixed” in terms of conduct and emotional problems, noting that they were more similar to children with CD than depression. However, others4 described the behavioral problems shown by those with comorbid depression and conduct problems as “soft core” behavioral problems, and described their comorbidity as “masked depression,” implying that the primary difficulties for the child were symptoms of depression.4
Some have suggested that the comorbidity between CD and depression should be classified as a distinct diagnostic entity altogether.3 Although such a diagnostic category has not been included in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV),5 Depressive Conduct Disorder has been identified as a separate disorder in the International Classification of Diseases (ICD-10).6 The evidence for distinguishing such a disorder separately from Major Depressive Disorder and CD is not clear.
How the disorders typically develop may provide important information about the nature and implications of their comorbidity. If conduct problems act as a mask for underlying depression, it might be expected that depression symptoms tend to precede behavioral problems, and there is some support for this.7 However, other evidence suggests that CD precedes depression, and further that negative life events associated with CD may mediate the links between CD and depression.8-9 Oppositional Defiant Disorder (ODD), on the other hand, temporally precedes both CD and Depression,8, 10-11 and is also commonly comorbid with both.1-2
Because Oppositional Defiant Disorder (ODD) temporally precedes both CD and depression, and is commonly comorbid with both, an alternative model of the comorbidity of the latter two conditions is that ODD may represent a common early precursor condition. An examination of the developmental comorbidity among boys in a clinic-referred sample found that, over 10 assessment waves, ODD symptoms predicted depression symptoms in the following year.8 In contrast, after accounting for ODD and for negative life events, CD symptoms were no longer predictive of depression. Similar results were found in a community sample of boys and girls;9 after accounting for negative life events, delinquency was not predictive of depression, whereas oppositionality showed a direct relationship with later depression. ODD in adolescence has also been found to predict depression in adulthood.12
Attempting to clarify the nature of the links between ODD and depression, Burke13 postulated that specific features of ODD may help to explain these direct links. Factor analyses using a clinic-referred sample of boys, the Developmental Trends Study (DTS), suggested that ODD symptoms loaded on two dimensions: negative affect and oppositional behavior. Negative affect consisted of the symptoms touchy, angry, and spiteful. The symptoms of loses temper, defies and argues loaded onto a separate factor of oppositional behavior. The symptoms annoys others and blames others were not consistently associated with either factor. When these symptoms were summed to create separate constructs, negative affect symptoms predicted depression, whereas oppositional behavior predicted later CD symptoms. Thus, not only were there distinct dimensions, but they were specific in their prediction of later psychopathology in a homotypic fashion. It is possible that negative affective symptoms of ODD explain the previously observed comorbidity between CD and depression. If so, negative affective symptoms might also serve as an early precursor to later internalizing psychopathology, and may provide important information about the risks for comorbidity among children with ODD or CD.
This finding has implications beyond whether and why the comorbidity of ODD and depression explains observed links between CD and depression. Negative affective symptoms of ODD may highlight important distinctions among children with ODD in terms of course, prognosis and risk for comorbid conditions. They may also indicate links between early temperament and childhood psychopathology. Recently, Stringaris and Goodman14 examined similar ad hoc ODD dimensions. However, notable differences were the inclusion of loses temper on the affective dimension, and moving spiteful and vindictive to a separate third dimension. Consistent with the findings from the DTS, their affective dimension predicted later emotional psychopathology, but in contrast all three dimensions predicted later CD, including the affective dimension.14 Mick and colleagues15 examined a construct of irritability created of the symptoms of loses temper, angry and touchy – thus identical to that of Stringaris & Goodman.14 In Mick and colleagues15 study however, irritability was not associated with increased risk for later mood disorder.
Some discussion has been given to the question of whether and how girls might differ from boys in the manner in which they manifest conduct problems. Boys meet criteria for CD at much higher rates, and show higher levels of physical aggression than girls.16-18 Girls have been speculated to engage in more socially directed aggression,19-21 although recent evidence finds no gender difference in the rate of relational aggression (Keenan, Coyne & Lahey, 2008).22 Aggressive boys are more likely than girls to become involved in delinquency and violent crime.23 On the other hand, although rates of ODD are higher among boys than girls in childhood, girls show rates equal to boys by adolescence.10 Some have speculated that discrepant prevalence rates observed for CD may be due to the symptoms by which conduct problems are assessed. If so, it may be hypothesize that the mechanisms of comorbidity between ODD and CD and depression might differ for girls.
Likewise, girls show higher rates of depression than boys, as well as showing a different course of depression symptoms over time. From early adolescence the gender ratio for depression increases greatly, when girls' rates begin to exceed those for boys'. 16, 24-27 As a result, the developmental associations between depression and other disorders may be anticipated to differ between girls and boys.
Finally, previous examination of negative affective symptoms of ODD13 has been conducted using a clinic-referred sample of boys alone. Such a sample would be expected to represent more extreme levels of antisocial behavior. The observed relationship between negative affective symptoms of ODD and depression in that sample may therefore also differ for a community sample. Berkson's bias,28 a selection bias associated with the increased likelihood that individuals in a sample drawn from a hospitalized population will show more than one disease condition, should be absent in a community sample. This may be especially relevant for studies of ODD and CD, since it appears that rates of CD without ODD differ markedly between community and clinical samples.13
The present study sought to replicate prior findings13 within a large community sample of girls, the Pittsburgh Girls Study. Based on previous findings, we hypothesize that factor analyses of ODD symptoms would show two underlying dimensions, a negative affective dimension consisting of being angry, touchy and spiteful, and a behavioral dimension of losing temper, arguing and defying. We hypothesize that the negative affective, but not the behavioral, dimension would predict levels of depression. In contrast, we expected that the behavioral, but not the negative affective, dimension would predict CD symptoms. We hypothesize that this relationship would not change with increasing age. Finally we hypothesize that these relationships would hold up even when controlling for other commonly comorbid psychopathology (Attention Deficit Hyperactivity Disorder (ADHD) and anxiety), as well as family and demographic covariates.
Method
Data for these analyses were from the Pittsburgh Girls Study (PGS), a longitudinal study of a community sample of girls recruited following the enumeration of 103,238 households in the city of Pittsburgh. Every household in low-income neighborhoods (based on 1990 Census data on poverty) were enumerated, and 50% of households in all other neighborhoods were enumerated. A total of 2,451 girls agreed to participate, of a total of 2,876 girls who were age-eligible at the start of the study. In the overlapping cohort design of the study, cohorts included 588 five year olds, 630 six year olds, 611 seven year olds, and 622 eight year olds. The present study uses data from Years 1 through 5 of the study, with follow-up retention rates that ranged from 97.2% to 93.1%.
Each girl and a caregiver (in 85.2% of cases, the biological mother, followed by 6.1% father, 2.3% grandmother, and 2.5 adoptive mother) were interviewed annually. Forty five percent of the girls were African American, 50% Caucasian and 5% identified themselves as either belonging to another racial group or as multiracial. For the present analyses, a variable was constructed to contrast minority racial status with Caucasian. In Year 1, more than half (54.7%) of parents were reported to have had more than 12 years of formal education, 27.7% of households received public assistance, and 32.9% lived in a household headed by a single female parent.
Approval for all study procedures was obtained from the University of Pittsburgh Institutional Review Board. Written informed consent from the caregiver and verbal assent from the child were obtained prior to data collection. Annual interviews were conducted separately for the parent and child in the home by trained interviewers using a laptop computer. Parents also completed a pen-and-paper booklet containing questionnaires. All participants were reimbursed for their participation. Measures.
Demographics
Socio-demographic data were collected via parent report using a format developed for the Pittsburgh Youth Study,29 which included questions about the girls' age, race, low parental education, single parenthood and whether or not the household was in receipt of public assistance (e.g., WIC, food stamps, welfare).
Psychopathology Constructs
Information on psychopathology was collected using the Child Symptom Inventory – IV (CSI-IV)30 to assess symptoms of ODD, CD, ADHD and depression. The CSI-IV is a standardized behavioral rating scale which maps directly onto DSM-IV symptoms, and yields both symptom counts and severity scores, as symptoms are rated on a four point scale. The measure has been shown to have good reliability, including internal consistencies of .90 for ODD, .80 for CD, and .94 for ADHD Combined Type, and test-retest reliability for symptom counts of .70 for ADHD, .78 for ODD, and .53 for CD.30 For the present analyses, symptom severity scores were chosen because they provided greater variability, particularly in CD scores at younger ages, which we anticipated would yield greater stability in statistical models.
The CSI-4 was initially administered to girls in the study at age 6. However, questions about the validity of the responses being given by the girls at that age were raised, and not all 6 year olds completed the measure. As a result the present analyses use girls' self-report data from age 7 years onwards. Additionally, in Year 1, parents were asked whether each CSI-4 symptom was ever present, and if so, if it was present in the last two months. Thus, they were not asked to report on the presence or absence of the symptom over the past year, which is not consistent with the subsequent waves of data. The data in the present analyses include all waves from years 1 through 5 in the model. To check whether the different time parameters of the symptom queries in Year 1 affected the results, models excluding data from Year 1 were also tested. These two methods yielded substantially identical results, which may be obtained from the first author.
To measure anxiety, the total score by parent report on the Screen for Child Anxiety and Related Emotional Disorders (SCARED)31,32 was used. The 41 items tap generalized anxiety, separation anxiety, panic/somatic, school and social phobia. Items are scored using 3 point scales (0-2) with an answer format of not/hardly ever true to very true. The SCARED has shown good reliability, with an ICC for the total score of .86, and ICCs for the individual factors ranging from .70 to .90, and has been found to significantly discriminate between anxiety, depression and disruptive disorders, as well as within individual anxiety disorders.31,32
Finally, maternal self-report of depression was assessed using the Beck Depression Inventory II. 33 The BDI-II is a 21 item measure that assesses the severity of depressive symptomatology. Each item is rated on a 4 point scale. Internal consistency for the measure has been shown to be high (alpha = .91), and the kappa correspondence with the BDI-I was .70. 34
Analyses
The analyses were conducted using Stata Release 10.35 We examined prediction from one age to the next using general linear regression models, clustering by participant to account for correlated error among observations within individuals. Because we were interested in how the predictors influenced the outcome one year later controlling for the concurrent level of the outcome, we examined transitional marginal models. In each model, we tested tolerance and variance inflation factors to determine if multicollinearity was a threat to the integrity of the model. Due to the large sample size, we adopted a more conservative alpha criterion level of p = .01 to determine significance.
Results
Factor Analyses of ODD Symptoms and Symptom Severity Scores
To explore whether there are dimensions underlying ODD symptoms consistent with previous studies, factor analyses of the symptoms of ODD were conducted, using data separately from each of Years 1 through 4. It should be noted that that Year 1 data differ in that symptoms were queried as to whether they were ever present, rather than being restricted to the past year. Because of the dichotomous nature of the symptoms, we first developed a tetrachoric correlation matrix of the symptoms. We conducted an exploratory factor analysis of this matrix, specifying a principal factors method of estimation. To determine the true maximum number of factors that could be extracted, we used a parallel analysis strategy,36-38 specifying 1,000 replications of the analysis on randomly generated data sets of the same number of cases and variables. Finally, we employed an oblique promax rotation for interpretation of the factors, with a cutoff of .4 for interpretation of items loading onto factors.
In years 1 through 3, the parallel analyses indicated that up to four factors could be extracted from the data, but in all three years, after promax rotation, no variables loaded on a fourth factor at greater than .4. We thus considered a three factor model to be preferable. In year 4, the parallel analysis suggested a maximum of three factors could be extracted. Across years 1 through 4, variables loaded onto three factors in a consistent fashion: losing temper, arguing and defying loaded onto one factor, being touchy, angry and spiteful loaded onto a second factor, and annoying and blaming others loaded onto a third factor. One exception: In Year 1, blaming others cross-loaded on the second and third factors. Table 1 shows the average loading of each symptom over the four years, restricted only to average loadings over .4.
Table 1.
Average symptom factor loadings across years 1 through 4
| ODD Symptoms | Factor 1: Oppositional Behavior | Factor 2: Negative Affect | Factor 3: Antagonistic Behavior |
|---|---|---|---|
| Loses temper | 0.70 | ||
| Argues | 0.84 | ||
| Defies | 0.66 | ||
| Annoys others | 0.60 | ||
| Blames others | 0.56 | ||
| Touchy | 0.62 | ||
| Angry | 0.74 | ||
| Spiteful | 0.68 |
Note: Average symptom loadings lower than .4 were omitted. ODD = Oppositional Defiant Disorder
We also conducted corresponding factor analyses on symptom severity scores instead of dichotomous symptoms, using polychoric, rather than tetrachoric correlation matrices. The results were essentially the same as those of the symptom based factor analyses, with the slight difference that the parallel analyses tended to indicate a maximum of three factors rather than four could be extracted. The pattern in which the items loaded onto the three factors was identical to that described above regarding symptoms.
The factors and constituent items identified here are consistent with the analyses of the clinical sample of boys in the DTS13 described above in terms of the first and second factors. In the DTS, the items annoying and blaming others did not load together onto a third factor and were excluded from subsequent analyses. Thus, despite the fact that these data are from a community sample of girls, and the DTS is a clinical sample of boys, largely consistent loading patterns are observed. We refer to the factor which includes the items of being angry, touchy and spiteful as Negative Affect (NA), and the factor which includes losing temper, arguing and defying as Oppositional Behavior (OB). The factor including annoying others and blaming others we refer to as Antagonistic Behavior (AB). We created constructs in accord with the factor analyses by summing the symptom severity scores from the CSI-4 for the items within each factor.
Symptom Severity Over Age
The average symptom severity scores for each psychopathology construct are shown in Figures 1 and 2. Generally stable rates of severity for each condition are observed, with relatively pronounced declines evident in the severity of anxiety and ADHD.
Figure 1.
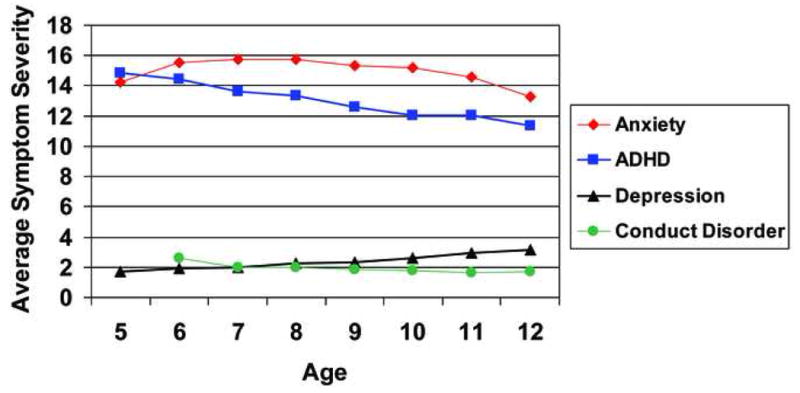
Average symptom severity over years 1 through 5 for anxiety, Attention Deficit Hyperactivity Disorder (ADHD), depression, and Conduct Disorder.
Figure 2.
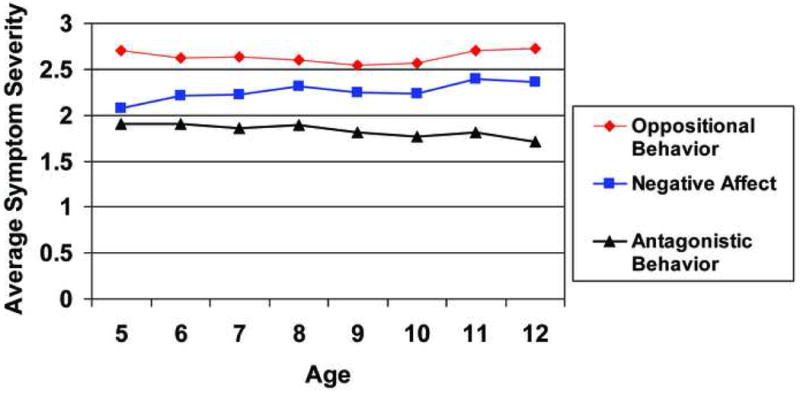
Average symptom severity level over years 1 through 5 for the Oppositional Defiant Disorder dimensions of negative affect, oppositional behavior and antagonistic behavior.
Prediction from negative affect to depression symptom severity
Depression severity scores were not normally distributed. We examined Poisson models, but found that they did not adequately account for the overdispersion in the model, which was confirmed using the technique described by Hardin and Hilbe.39 As a result, we used negative binomial regression to model the data.
Testing a model with only ODD based constructs predicting depression, controlling for prior depression and age found that OB (IRR = 1.02, se = .01, p = .06) was not significantly predictive of depression, whereas NA (IRR = 1.05, se = .01, p < .001) and AB were (IRR = 1.04, se = .01, p = .004). However, including the remaining measures of psychopathology (CD, ADHD, and anxiety) resulted in AB (IRR = 1.02, se = .02, p = .335) no longer being significantly predictive of later depression, whereas NA remained a significant predictor (IRR = 1.05, p < .001). We then introduced the demographic covariates along with maternal self-report of depression. After stepwise removal of non-significant predictors, the final model predicting depression is shown in Table 2. NA, anxiety, ADHD and maternal age were retained as significant predictors of depression.
Table 2.
Predictors of depression symptom severity.
| IRR | se | p | 95% CI | ||
|---|---|---|---|---|---|
| Depression | 1.14 | .006 | <.001 | 1.13 | 1.15 |
| NA | 1.05 | .008 | <.001 | 1.04 | 1.07 |
| Anxiety | 1.02 | .001 | <.001 | 1.02 | 1.02 |
| ADHD | 1.02 | .002 | <.001 | 1.01 | 1.02 |
| Maternal Depression | 1.01 | .002 | <.001 | 1.01 | 1.01 |
| Age | 1.09 | .011 | <.001 | 1.06 | 1.11 |
Note: All predictors, excluding age, were lagged one year relative to the outcome. NA = negative affect, ADHD = Attention Deficit Hyperactivity Disorder, IRR = incident rate ratio; CI = confidence interval
Prediction to CD symptom severity
As anticipated, and as with models of depression symptom severity, CD symptom severity scores deviated markedly from a normal distribution. We explored modeling the data by specifying a Poisson mean distribution, but suspected that overdispersion might render a Poisson model inappropriate for these data. A procedure for testing overdispersion in the Poisson model39 confirmed our suspicions, and thus the Poisson model assumption of variance equal to the mean would be violated. As a result, we modeled the data specifying a negative binomial mean distribution.
We first examined a model with NA, OB and AB predicting CD, controlling for age. Examining the diagnostics for the model suggested significant concerns, particularly in the fitted values and deviance residuals. Exploration of transformations using the multivariate fractional polynomial command in Stata did not suggest that any polynomial transformations of the predictors be used, but did indicate that a transformation of the lagged CD score (adding a constant, dividing the score by 10, and taking the natural log) led to markedly improved model diagnostics, particularly fitted values and residuals. This transformation of the lagged CD score was included in the remaining models. In each regression model, we used a probability, or sampling, weight to adjust for the over-sampling of low-income neighborhoods.
ODD Predictors of CD
In the model with only lagged CD, ODD based predictors and age included, OB (IRR = 1.01, se = .01, p = .19) was not significantly predictive, while NA (IRR = 1.04, se = .01, p = .001) and AB (IRR = 1.14, se = .02, p < .001) were predictive of later CD. However, as other variables were introduced into the model, it was observed that the introduction of Race into the model had a specific and dramatic effect on OB and NA. Introducing Race into the model of ODD predictors led to NA becoming non-significant (IRR = 1.03, se = .01, p = .02), and OB (IRR = 1.04, se = .01, p < .001) and AB (IRR = 1.12, se = .02, p< .001) significantly predictive. We examined interactions to try to understand these changes associated with the introduction of Race into the model, and found a significant interaction between Race and NA. This interaction term was included in all remaining models predicting CD.
We next included in the model the remaining demographic variables: Low Parental Education, Single Parenthood and Public Assistance. After removing nonsignificant variables (Depression and Anxiety), the resulting model is as shown in Table 3. In addition to ODD predictors and ADHD, the demographic variables of public assistance, low parental education and single parenthood were retained in the model.
Table 3.
Predictors of Conduct Disorder Severity
| IRR | se | p | 95% CI | ||
|---|---|---|---|---|---|
| CD (transformed) | 2.03 | .05 | <.001 | 1.93 | 2.13 |
| OB | 1.03 | .01 | .001 | 1.02 | 1.05 |
| AB | 1.10 | .02 | <.001 | 1.07 | 1.13 |
| NA | 1.08 | .02 | <.001 | 1.05 | 1.11 |
| Minority Race* | 1.56 | .08 | <.001 | 1.41 | 1.73 |
| NA × Minority Race | 0.92 | .01 | <.001 | 0.90 | 0.95 |
| ADHD | 1.01 | .00 | <.001 | 1.01 | 1.02 |
| Public Assistance | 1.09 | .03 | .002 | 1.03 | 1.15 |
| Low Parental Education | 1.10 | .03 | <.001 | 1.04 | 1.15 |
| Single Parenthood | 1.09 | .03 | .001 | 1.04 | 1.15 |
| Age* | 1.02 | .01 | .037 | 1.00 | 1.05 |
Note: All predictors apart from minority race and age were lagged by one year relative to the outcome. CD = Conduct Disorder, OB = oppositional behavior, AB = antagonistic behavior, NA = negative affect, ADHD = Attention Deficit Hyperactivity Disorder, IRR = incident rate ratio; CI = confidence interval
To examine the interaction between race and NA, we ran the models separately by race. For girls in the Caucasian group, NA was significantly predictive of later CD (IRR = 1.05, se = .02, p = .007), whereas for girls in the minority race group, NA was not (IRR = 1.01, se = .01, p = .56). Other changes to the model for Caucasian girls: low parental education (p = .26) was no longer significant, and was removed from the model. For minority racial group girls, single parenthood (p = .04) and public assistance (p = .14) were removed from the model.
Discussion
Consistent with recent studies,8-9, 13 the present findings suggest that CD symptoms are not significantly associated with later depression symptoms, whereas ODD symptoms are. In particular, the comorbidity between ODD and depression appears to be specifically attributable to the relationship between a specific set of ODD symptoms that may reflect a separate dimension of negative affectivity.
The present analyses on girls are consistent with previous results from a clinical sample of boys13 in finding that the DSM-IV ODD symptoms of loses temper, argues and defies load on one factor, separate from a second factor consisting of touchy, spiteful and angry. Novel results from the present data suggest that annoying others and blaming others load on a third factor. As predictors of later depression, the present analyses are consistent with the results from both prior studies,13-14 showing that the negative affective dimension of ODD symptoms predicts later depression, whereas the oppositional behavior dimension does not (and in the present analyses, neither does the third dimension of antagonistic behavior). Although the findings are consistent in terms of the implication that depression is predicted by a component of ODD symptoms indicative of irritability or negative affect, it is noteworthy that the construct (Irritable) used by Stringaris and Goodman14 differed from the present, empirically-derived construct (Negative Affect). Specifically, Irritable consisted of the symptoms angry and resentful, touchy, and loses temper. Thus, it included loses temper and excluded spiteful and vindictive in comparison to Negative Affect.
The role of irritability in the present findings, and more generally across constructs of psychopathology, remain frustratingly inscrutable. Here, we have considered negative affect as a distinct dimension of ODD, separate from other psychopathology. In that fashion, we have regarded negative affect as a predictor of later depression, which may explain the observed rates of comorbidity between depression and the disruptive behavior disorders. On the other hand, it may be that our construct of negative affect is equivalent to or captures some aspect of irritability more generally. The diagnostic criteria for depression5 have long included irritability in children as an alternative to depressed mood, although the evidence for considering irritability and depressed mood as equivalent for children, and also for not doing so for adults, is not clear. Furthermore, irritability is ubiquitous across psychopathology and normal development (see e.g. Leibenluft40). In the present analyses, the substitution of irritability for depressed mood was not manifestly allowed while assessing diagnostic criteria for depression. It is possible that irritability is a latent aspect of depression, giving rise to the present findings.
It may, on the other hand, be erroneous to assume that irritability and depressed mood are equivalent, or at least it may be too simplistic to assert that irritability stands in place of depressed mood as an indicator of depression for children. For some girls in the present study, namely Caucasian girls, negative affect was also predictive of later CD symptoms. Likewise, Stringaris and Goodman14 found that their ODD dimension of “Irritable” predicted both affective and behavioral psychopathology, and Mick et al.15 found that “Irritability” indicated by those same ODD symptoms did not indicate increased rates of mood disorder. Thus, evidence does not fully support a strict cleaving of irritability or negative affect from ODD as a distinct early aspect of mood disorder.
It has been observed that irritability is ubiquitous among categories of psychopathology and normal development40, and not simply within mood disorders, which may also suggest that it is something other than necessarily an early indicator of mood disorder. Liebenluft and colleagues40 determined that irritability could be distinguished as either chronic or episodic, and found that over two years in adolescence, chronic irritability predicted ODD and ADHD, whereas episodic irritability predicted mania. (In that study, follow up over 9 years, from parent and child report in adolescence, to child report in young adulthood alone, yielded somewhat contradictory findings.) Further investigation of the nature of affective dysregulation, both within ODD and more generally across psychiatric disorders, is needed to ascertain whether different types of irritability underlie different disorders and whether they are causal or are outcomes of the impairments of those disorders.
As efforts to develop DSM V move forward, questions have been raised about whether ODD should be eliminated as a diagnosis separate from CD. The present findings suggest that ODD has a distinct and important role in the development of both affective and behavioral psychopathology. What remains to be addressed is whether ODD is a conglomeration of separate processes of behavioral and affective dysregulation, which should be disentangled, or whether it is an apt characterization of a distinct disorder involving global dysregulation difficulties. Part of the resolution of this question will rely on further information about the prediction to later psychopathology from these dimensions. Is there more evidence for homotypic continuity, with affective features predictive of later affective psychopathology and behavioral features predictive of behavioral disorders? Alternatively, are outcomes of ODD reflective of multifinality from a common starting point, perhaps influenced by other individual and environmental conditions? To address these questions, it will be important to determine if distinct latent classes of children can be identified based on the presence or absence of these dimensions, and if so, whether these groups face different risks for different types of later psychopathology.
A number of significant implications for clinical practice arise from the present findings. First, the present findings are consistent with an etiological model for the comorbidity between CD and depression in which ODD serves as the explanatory link between the two. The risk for depression associated with ODD has likely not previously been fully appreciated, and clinicians and their patients may benefit from increased vigilance for associated affective disorders after identifying ODD in a child or adolescent. Since the onset of ODD is typically earlier than depression, it may be possible to incorporate affective ODD symptoms into a screening process for risk of depression and thus more effectively target preventive interventions. This may be of particular utility given recent finding that show that early engagement in cognitive behavioral treatment reduces the onset of depression in vulnerable youth.41 Finally, these results suggest that it is important to assess for symptoms of ODD even if criteria for CD are met, since ODD symptoms may provide more useful prognostic information than CD symptoms about the risk for comorbid affective disorder.
There are several limitations to keep in mind regarding the present study and the interpretations of these findings. First, the analyses focused on symptom severity scores from self-report measures rather than diagnostic symptom counts or categorical diagnoses. Although this does place some limits on the interpretation of these findings, the DSM V development is proceeding with an interest in incorporating dimensionality in the diagnostic framework (e.g. Moffit et al., 2008). Thus, it is important to have evidence of similarities and differences regarding dimensional versus categorical approaches to the measurement of these conditions. Another limitation is the relatively low base-rate for antisocial behaviors in this community sample. We feel we have addressed the issues associated with low base-rate phenomena reasonably well in these analyses, and that the statistical models are sound. Nevertheless, rates of the symptoms of interest would differ in clinical and community samples, and it remains important to study these associations in different types of data sets. Finally, the data set consists entirely of girls. There are interesting similarities and differences in these results compared to analyses conducted in samples of boys. Again, such differences must be resolved through replication using varied data sets.
Acknowledgments
This research was supported by research grants MH74148 from the National Institute of Mental Health to Dr. Burke and MH56630 from the National Institute of Mental Health and DA12237 from the National Institute on Drug Abuse to Dr. Loeber.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Angold A, Costello EJ, Erkanli A. Comorbidity. J Child Psychol Psychiatry. 1999;40(1):57–87. [PubMed] [Google Scholar]
- 2.Maughan B, Rowe R, Messer J, Goodman R, Meltzer H. Conduct disorder and oppositional defiant disorder in a national sample: developmental epidemiology. J Child Psychol Psychiatry. 2004;45(3):609–621. doi: 10.1111/j.1469-7610.2004.00250.x. [DOI] [PubMed] [Google Scholar]
- 3.Puig-Antich J. Major depression and conduct disorder in prepuberty. J Am Acad Child Adolesc Psychiatry. 1982;21:118–128. doi: 10.1016/s0002-7138(09)60910-9. [DOI] [PubMed] [Google Scholar]
- 4.Carlson GA, Cantwell DP. Unmasking masked depression in children and adolescence. Am J Psychiatry. 1980;137:445–449. doi: 10.1176/ajp.137.4.445. [DOI] [PubMed] [Google Scholar]
- 5.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th. Washington, D. C.: American Psychiatric Association; 1994. [Google Scholar]
- 6.International Statistical Classification of Diseases and Related Health Problem, Tenth Revision. World Health Organization; Geneva: World Health Organization; 1992. [PubMed] [Google Scholar]
- 7.Beyers JM, Loeber R. Untangling developmental relations between depressed mood and delinquency in male adolescents. J Abnorm Child Psychol. 2003;31(3):247–266. doi: 10.1023/a:1023225428957. [DOI] [PubMed] [Google Scholar]
- 8.Burke JD, Loeber R, Lahey BB, Rathouz PJ. Developmental transitions among affective and behavioral disorders in adolescent boys. J Child Psychol Psychiatry. 2005;46(11):1200–1210. doi: 10.1111/j.1469-7610.2005.00422.x. [DOI] [PubMed] [Google Scholar]
- 9.Rowe R, Maughan B, Eley TC. Links between antisocial behavior and depressed mood: The role of life events and attributional style. J Abnorm Child Psychol. 2006;34(3):293–302. doi: 10.1007/s10802-006-9032-0. [DOI] [PubMed] [Google Scholar]
- 10.Boylan K, Vaillancourt T, Boyle M, Szatmari P. Comorbidity of internalizing disorders in children with oppositional defiant disorder. Eur Child Adolesc Pscyhiatry. 2007;16(8):484–494. doi: 10.1007/s00787-007-0624-1. [DOI] [PubMed] [Google Scholar]
- 11.Nock MK, Kazdin AE, Hiripi E, Kessler RC. Lifetime prevelance, correlates, and persistence of oppositional defiant disorder: Results form the National Comorbidity Survey Replication. J Child Psychol Psychiatry. 2007:1–11. doi: 10.1111/j.1469-7610.2007.01733.x. [DOI] [PubMed] [Google Scholar]
- 12.Copeland WE, Shanahan L, Costello EJ, Angold A. Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Arch Gen Psychiatry. 2009;66(7):764–772. doi: 10.1001/archgenpsychiatry.2009.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burke JD. Relationship between conduct disorder and oppositional defiant disorder and their continuity with antisocial behaviors: Evidence from longitudinal clinical studies. In: Shaffer D, Leibenluft E, Rohde LA, editors. Externalizing Disorders of Childhood: Refining the Research Agenda for DSM-V. Arlington, VA: American Psychiatric Association; in press. [Google Scholar]
- 14.Stringaris A, Goodman R. Three dimensions of oppositionality in youth. J Child Psychol Psychiatry. 2009;50:216–233. doi: 10.1111/j.1469-7610.2008.01989.x. [DOI] [PubMed] [Google Scholar]
- 15.Mick E, Spencer T, Wozniak J, Biederman J. Heterogeneity of irritability in attention-deficit/hyperactivity disorder subjects with and without mood disorders. Biol Psychiatry. 2005;58(7):576–582. doi: 10.1016/j.biopsych.2005.05.037. [DOI] [PubMed] [Google Scholar]
- 16.Cohen P, Cohen J, Kasen S, et al. An epidemiological study of disorders in late childhood and adolescence: I. Age- and gender-specific prevalence. J Child Psychol Psychiatry. 1993;34:851–867. doi: 10.1111/j.1469-7610.1993.tb01094.x. [DOI] [PubMed] [Google Scholar]
- 17.Mandel HP. Conduct disorder and underachievement. New York: Wiley; 1997. [Google Scholar]
- 18.Offord DR, Boyle MH, Szatmari P, et al. Ontario Child Health Study. II. Six-month prevalence of disorder and rates of service utilization. Arch Gen Psychiatry. 1987;44(9):832–836. doi: 10.1001/archpsyc.1987.01800210084013. [DOI] [PubMed] [Google Scholar]
- 19.Bjorkqvist K, Osterman K, Kaukiainen K. The development of direct and indirect aggressive strategies in males and females. In: Bjorkqvist K, Niemela P, editors. Of mice and women: Aspects of female aggression. San Diego, CA: Academic Press; 1992. pp. 51–64. [Google Scholar]
- 20.Crick NR, Grotpeter JK. Relational aggression, gender, and social-psychologial adjustment. Child Dev. 1995;66:710–722. doi: 10.1111/j.1467-8624.1995.tb00900.x. [DOI] [PubMed] [Google Scholar]
- 21.Underwood MK. Social aggression among girls. New York: Guilford; 2003. [Google Scholar]
- 22.Keenan K, Coyne C, Lahey BB. Should relational aggression be included in DSM V? J Am Acad Child Adolesc Psychiatry. 2008;47(1):86–93. doi: 10.1097/chi.0b013e31815a56b8. [DOI] [PubMed] [Google Scholar]
- 23.Moffitt TE, Caspi A, Rutter M, Silva PA. Sex differences in antisocial behaviour: Conduct disorder, delinquency, and violence in the Dunedin longitudinal study. Cambridge, UK: Cambridge University Press; 2001. [Google Scholar]
- 24.Angold A, Costello EJ, Worthman C. Puberty and depression: The roles of age, pubertal status and pubertal timing. Psychol Med. 1998;28:51–61. doi: 10.1017/s003329179700593x. [DOI] [PubMed] [Google Scholar]
- 25.Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal study. J Abnorm Psychol. 1998;107:128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- 26.Lewinsohn PM, Rohde P, Seeley JR. Adolescent psychopathology. 3. The clinical consequences of comorbidity. J Am Acad Child Adolesc Psychiatry. 1995;34:510–519. doi: 10.1097/00004583-199504000-00018. [DOI] [PubMed] [Google Scholar]
- 27.Peterson AC, Compas BE, Brooks-Gunn J, Stemmler M, Ey S, Grant KE. Depression in Adolescence. Am Psychol. 1993;48(2):155–168. doi: 10.1037//0003-066x.48.2.155. [DOI] [PubMed] [Google Scholar]
- 28.Berkson J. Limitations of the application of fourfold table analysis to hospital data. Biometrics Bulletin. 1946;2:47–53. [PubMed] [Google Scholar]
- 29.Loeber R, Farrington DP, Stouthamer-Loeber M, Van Kammen WB. Antisocial behaviour and mental health problems: Explanatory factors in childhood and adolescence. Mahwah, NJ: Lawrence Erlbaum Associates; 1998. [Google Scholar]
- 30.Gadow KD, Sprafkin J. Child Symptom Inventories manual. Stony Brook, NY: Checkmate Plus; 1994. [Google Scholar]
- 31.Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. J Am Acad Child Adolesc Psychiatry. 1999 Oct;38(10):1230–1236. doi: 10.1097/00004583-199910000-00011. 1999. [DOI] [PubMed] [Google Scholar]
- 32.Birmaher B, Khetarpal S, Brent D, et al. The Screen for Child Anxiety Related Emotional Disorders (SCARED): scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry. 1997 Apr;36(4):545–553. doi: 10.1097/00004583-199704000-00018. 1997. [DOI] [PubMed] [Google Scholar]
- 33.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 34.Dozois DJA, Dobson K, Ahnberg JL. A psychometric evaluation of the Beck Depression Inventory-II. Psychological Assessment. 1998;10(2):83–89. [Google Scholar]
- 35.StataCorp. Stata Statistical Software: Release 10.0. College Station, TX: Stata Corporation LP; 2007. [Google Scholar]
- 36.Lance CE, Butts M, Michels L. The sources of four commonly reported cutoff criteria: What did they really say? Organizational Research Methods. 2006;9:202–220. [Google Scholar]
- 37.O'Connor BP. SPSS and SAS programs for determining the number of components using parallel analysis and Velicer's MAP test. Behavior Research Methods, Instrumentation, and Computers. 2000;32:396–402. doi: 10.3758/bf03200807. [DOI] [PubMed] [Google Scholar]
- 38.Velicer WF, Eaton CA, Fava JL. Construct explication through factor or component analysis: A review and evaluation of alternative procedures for determining the number of factors or components. In: Goffin RD, Helmes E, editors. Problems and solutions in human assessment. Boston: Kluwer; 2000. [Google Scholar]
- 39.Hardin JW, Hilbe JM. Generalized Linear Models and Extensions. 2nd. College Station TX: Stata Press; 2007. [Google Scholar]
- 40.Leibenluft E, Cohen P, Corrindo T, Brook JS, Pine DS. Chronic versus episodic irritability in youth: a community-based, longitudinal study of clinical and diagnostic associations. J Child Adolesc Psychopharmacol. 2006;16(4):456–466. doi: 10.1089/cap.2006.16.456. [DOI] [PubMed] [Google Scholar]
- 41.Garber J, Clarke GN, Weersing VR, et al. Prevention of depression in at-risk adolescents: a randomized controlled trial. JAMA. 2009;30(21):2215–2224. doi: 10.1001/jama.2009.788. [DOI] [PMC free article] [PubMed] [Google Scholar]


