Abstract
Background
Recent discussions about health care reform have raised questions regarding the value of advance directives.
Methods
We used data from survey proxies in the Health and Retirement Study involving adults 60 years of age or older who had died between 2000 and 2006 to determine the prevalence of the need for decision making and lost decision-making capacity and to test the association between preferences documented in advance directives and outcomes of surrogate decision making.
Results
Of 3746 subjects, 42.5% required decision making, of whom 70.3% lacked decision-making capacity and 67.6% of those subjects, in turn, had advance directives. Subjects who had living wills were more likely to want limited care (92.7%) or comfort care (96.2%) than all care possible (1.9%); 83.2% of subjects who requested limited care and 97.1% of subjects who requested comfort care received care consistent with their preferences. Among the 10 subjects who requested all care possible, only 5 received it; however, subjects who requested all care possible were far more likely to receive aggressive care as compared with those who did not request it (adjusted odds ratio, 22.62; 95% confidence interval [CI], 4.45 to 115.00). Subjects with living wills were less likely to receive all care possible (adjusted odds ratio, 0.33; 95% CI, 0.19 to 0.56) than were subjects without living wills. Subjects who had assigned a durable power of attorney for health care were less likely to die in a hospital (adjusted odds ratio, 0.72; 95% CI, 0.55 to 0.93) or receive all care possible (adjusted odds ratio, 0.54; 95% CI, 0.34 to 0.86) than were subjects who had not assigned a durable power of attorney for health care.
Conclusions
Between 2000 and 2006, many elderly Americans needed decision making near the end of life at a time when most lacked the capacity to make decisions. Patients who had prepared advance directives received care that was strongly associated with their preferences. These findings support the continued use of advance directives.
Advance directives document Patients' wishes with respect to life-sustaining treatment (in a living will), their choice of a surrogate decision maker (in a durable power of attorney for health care), or both. First sanctioned in 1976, advance directives were designed to protect patient autonomy1 under the belief that patients who lose decision-making capacity are more likely to receive the care they want if they choose a surrogate decision maker, document their wishes in advance, or both. To promote the use of advance directives, Congress passed the Patient Self-Determination Act in 19902 mandating that all Medicare-certified institutions provide written information regarding patients' right to formulate advance directives. More recently, a proposal to reimburse providers for these activities through Medicare3 stirred controversy and raised concern that advance directives would lead to denial of necessary care.
Currently, up to 70% of community-dwelling older adults have completed an advance directive.4 The popularity of advance directives has grown tremendously, despite debate about their effectiveness.5 Early evidence suggested that living wills have little effect on decisions to withhold or withdraw care6-10 and do little to increase consistency between care received and patients' wishes.11 More recently, studies have shown that patients with advance directives are less likely to receive life-sustaining treatment or to die in a hospital,4,12 but it is unclear whether these outcomes were consistent with patients' wishes. Data on the effectiveness of a durable power of attorney for health care are limited.
In addition, it is unclear how often the circumstance in which advance directives would apply actually occurs — that is, how often patients face a treatable, life-threatening condition while lacking decision-making capacity. The prevalence of lost decision-making capacity and the frequency of surrogate decision making about life-sustaining therapies are unknown.
To better judge the need for and value of advance directives, we sought to determine the prevalence and predictors of lost decision-making capacity and decision making at the end of life. We also studied the association between advance directives and care received at the end of life, including the agreement between preferences stated in advance directives and the type of surrogate decision maker and decisions made at the end of life.
Methods
Data Sources and Study Population
We used data from the Health and Retirement Study,12 a biennial longitudinal survey of a nationally representative cohort of U.S. adults 51 years of age or older.13 We limited our study to persons 60 years of age or older who had died between 2000 and 2006 and for whom a proxy (a family member or knowledgeable informant) answered a study-directed exit interview after the participant's death. For most of these respondents, exit interviews occurred within 24 months after the subject's death. For more details about the Health and Retirement Study sampling, data-collection procedures, and measures, see Juster and Suzman13 or http://hrsonline.isr.umich.edu. Oral informed consent was obtained from both subjects and proxies in the original study. The institutional review board of the University of Michigan waived the requirement for review of this study.
Outcomes
Our outcomes of interest were obtained from the responses of the proxies to the Health and Retirement Study exit surveys regarding the decedent's circumstances at death; specifically, whether the subject had completed a living will or durable power of attorney for health care, maintained decision-making capacity, and needed decision making at the end of life. For subjects who needed decision making, data were collected on the decisions made and on the person who made them. For subjects who had a durable power of attorney for health care, data were collected on the person the subject appointed. Questions used to determine the patient-appointed decision maker and the actual decision maker were similarly worded. Data were collected regarding the preferences of subjects who completed a living will. Questions used to determine outcomes of decision making mirrored those used to determine preferences. We examined predictors of and preferences for all care possible (“all care possible under any circumstances in order to prolong life”), limited care (“limit[ed] care in certain situations”), and comfort care (“comfortable and pain-free [while forgoing] extensive measures to prolong life”). The original questions are provided in the Supplementary Appendix, available with the full text of this article at NEJM.org.
Predictors
We investigated the influence of clinical and sociodemographic characteristics reported by subjects before death and by the proxy after the subject's death. Clinical factors included cognitive impairment (“fair” or “poor” memory 1 month before death), chronic conditions (cancer, lung disease, heart disease, cerebrovascular disease, or depression), the presence of pain (“often troubled with pain during the last year of life”), the duration of illness, and the year of death. Sociodemographic factors included age, sex, race or ethnic group (white, black, or other), marital status (married, living with a partner, or other), and educational level (less than high-school graduate, high-school graduate, or some college or more).
Statistical Analysis
For the entire sample, we tabulated the frequency of end-of-life decision making, completion of advance directives (stratified according to the type of advance directive), and preferences for treatment and a surrogate decision maker. In addition, for subjects who required decision making, we tabulated the prevalence of lost decision-making capacity. Among subjects who needed decision making and had lost decision-making capacity, we determined the prevalence of completion of advance directives. We tabulated the treatment preferences of the subpopulation of subjects who required decision making and had completed living wills, as well as the preference for a surrogate decision maker in the subpopulation of subjects who required decision making and had a durable power of attorney for health care.
Using multivariable logistic regression, we investigated the clinical and sociodemographic predictors of the requirement for decision making and the loss of decision-making capacity.
For subjects who required decision making and had lost decision-making capacity, we tested the association between the presence or absence of a living will or durable power of attorney for health care and the outcomes of decision making (hospitalization, all care possible, limited care, and comfort care), using multivariable logistic regression with adjustment for clinical and sociodemographic characteristics.
For subjects with living wills, we tested the association between preferences and outcomes, using multivariable logistic-regression analyses with adjustment for confounding by sociodemographic and clinical characteristics and stratification according to the type of preference. We also determined agreement between preferences and decisions made, using McNemar's test to account for matched data.
For subjects who had appointed a durable power of attorney for health care, we used the symmetry command in Stata software to examine the percent agreement between the appointed decision maker and the actual decision maker.
In all calculations and analyses, we accounted for the complex sampling design of the Health and Retirement Study13,14 by using the appropriate sampling weight from the subject's last interview before death (while the subject was living in the community) as listed in the 2006 tracker file of the Health and Retirement Study. All percentages that include a confidence interval were derived with the use of sampling weights; these results may differ from unweighted results. All statistical analyses were performed with the use of Stata software (Stata/IC10.0).
Results
Study Population
A total of 4246 respondents to the Health and Retirement Study died between 2000 and 2006 according to their proxies, National Death Index data, or both. The Health and Retirement Study obtained exit data on 3963 of those decedents from proxies (93.3%); 3746 of the decedents (88.2%) were 60 years of age or older at the time of death. Characteristics of the decedents are summarized in Table 1. These data are representative of approximately 12 million deaths in the United States during the study period.
Table 1. Characteristics of the Study Subjects *.
| Variable | All Subjects (N = 3746) |
|---|---|
| Sex — % (95% CI) | |
| Female | 53.2 (51.6–54.7) |
| Male | 46.8 (45.3–48.4) |
| Race or ethnic group — % (95% CI)† | |
| White | 86.6 (84.1–89.2) |
| Black | 10.3 (8.3–12.4) |
| Hispanic | |
| Mexican American | 3.1 (1.4–4.7) |
| Other | 1.6 (1.1–2.0) |
| Other | 3.1 (2.0–4.1) |
| Education — % (95% CI) | |
| Less than high-school graduate | 41.7 (39.6–43.9) |
| High-school graduate | 43.5 (41.6–45.3) |
| Some college or more | 14.8 (13.5–16.1) |
| Marital status — % (95% CI) | |
| Married or living with a partner | 42.3 (40.4–44.2) |
| Widowed | 43.8 (41.9–45.8) |
| Divorced or separated | 9.8 (8.7–11.0) |
| Single, never married | 4.0 (3.1–4.9) |
| Place of death — % (95% CI) | |
| Hospital | 38.9 (36.8–41.1) |
| Home | 27.3 (25.3–29.2) |
| Nursing home | 24.6 (22.6–26.5) |
| Hospice | 6.0 (4.8–7.3) |
| Assisted-living facility | 0.8 (0.5–1.0) |
| Other | 2.4 (1.8–3.1) |
| Nursing home resident — % (95% CI) | 34.3 (32.4–36.2) |
| Age at death — yr | |
| Mean | 80.5 |
| Interquartile range | 73.1–87.9 |
| Living children — no. | |
| Mean | 3.2 |
| Interquartile range | 2.0–4.0 |
Percentages are weighted and were derived with the use of sampling weights from the Health and Retirement Study. Totals may not sum to 100% because of rounding.
Race or ethnic group was self-reported.
According to the study respondents, most deaths were “expected at about the time [they] occurred”13 (58.6%; 95% confidence interval [CI], 56.4 to 60.7); in 67.9% of the subjects (95% CI, 62.8 to 72.9), there was a week or more between the time of diagnosis and death. Before death, subjects commonly had heart disease (53.7%; 95% CI, 51.8 to 55.6), depression (48.0%; 95% CI, 45.5 to 50.4), cancer (35.0%; 95% CI, 33.4 to 36.6), cerebrovascular disease (25.6%; 95% CI, 24.1 to 27.1), lung disease (24.1%; 95% CI, 22.4 to 25.9), or cognitive impairment (45.7%; 95% CI, 43.5 to 47.8). The subjects were most likely to have died in hospitals (38.9%; 95% CI, 36.8 to 41.1), in their homes (27.3%; 95% CI, 25.3 to 29.2), or in nursing homes (24.5%; 95% CI, 22.6 to 26.5%).
Proxy Respondents
Proxy respondents were adult children (48.9%; 95% CI, 45.0 to 53.0), spouses (32.5%; 95% CI, 30.6 to 34.3), or other relatives (13.5%; 95% CI, 11.1 to 16.1), who were most often interviewed by telephone (71.2%; 95% CI, 68.1 to 74.4) or in person (28.3%; 95% CI, 25.2 to 31.3) a mean (±SD) of 13±8.4 months (range, 0 to 76) after the subject's death. Three fourths of the interviews occurred between 1 and 19 months after the subject died. Proxies of decedents who required surrogate decision making were the decedent's actual decision maker 79.5% of the time (95% CI, 76.8 to 82.1).
Need for Decision Making at the End of Life
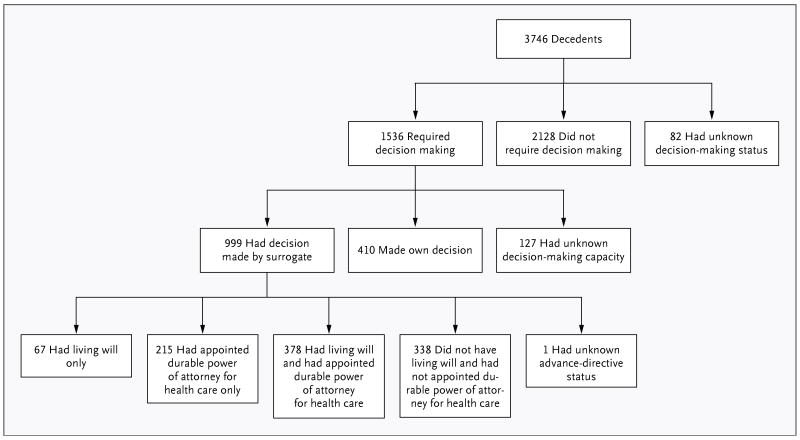
Of 3746 decedents, 42.5% (95% CI, 39.9 to 44.5) required decision making about treatment in the final days of life (Fig. 1). After adjustment for sociodemographic and clinical covariates, memory deficits (adjusted odds ratio, 1.27; 95% CI, 1.06 to 1.53; P=0.01), cerebrovascular disease (adjusted odds ratio, 1.40; 95% CI, 1.21 to 1.63; P<0.001), nursing home status (adjusted odds ratio, 1.36; 95% CI, 1.17 to 1.58; P<0.001), and loss of a spouse (adjusted odds ratio, 1.35; 95% CI, 1.14 to 1.60; P<0.001) were associated with an increased likelihood of the need for decision making.
Figure 1. Schematic Representation of the Study Population.
Actual numbers of subjects in the study are shown.
Prevalence of Lost Decision-Making Capacity
Of the 1536 decedents who required decision making, complete data were available for 1409, and of those subjects, 70.3% (95% CI, 67.3 to 73.2) lacked decision-making capacity. In a multivariate logistic-regression analysis of the predictors of decision-making capacity, subjects who were less likely to retain decision-making capacity were those with cognitive impairment (adjusted odds ratio, 0.42; 95% CI, 0.33 to 0.53; P<0.001), those with cerebrovascular disease (adjusted odds ratio, 0.56; 95% CI, 0.39 to 0.82; P=0.003), and those residing in nursing homes (adjusted odds ratio, 0.67; 95% CI, 0.51 to 0.88, P=0.003). At least 76.6% (95% CI, 75.0 to 78.2) of the overall population had at least one of these characteristics.
Advance Directives and Stated Preferences
Of 999 decedents who needed decision making and lacked decision-making capacity (29.8% [95% CI, 26.8 to 32.7] of the subjects in the overall sample for whom complete data were available), 67.5% (95% CI, 63.1 to 72.0) had an advance directive; 6.8% (95% CI, 4.6 to 8.9) had appointed a living will only, 21.3% (95% CI, 17.9 to 24.8) had appointed a durable power of attorney for health care only, and 39.4% (95% CI, 35.7 to 43.1) had both prepared a living will and appointed a durable power of attorney for health care (Table 2). Among decedents who had living wills, 1.9% (95% CI, 0.6 to 3.3) had requested all care possible, 92.7% (95% CI, 90.1 to 95.3) had requested limited care, and 96.2% (95% CI, 94.7 to 97.7) had requested comfort care. Among decedents who had appointed a durable power of attorney for health care, 64.6% (95% CI, 60.4 to 67.5) had appointed a child or grandchild, 26.9% (95% CI, 23.1 to 30.0) had appointed a spouse or partner, 6.6% (95% CI, 4.4 to 8.6) had appointed another relative, and 1.9% (95% CI, 0.1 to 2.1) had appointed a person who was not a relative. In a subgroup of women who had not been widowed, 67.0% (95% CI, 59.4 to 74.5) had appointed spouses most often. The preferences of the subjects in the overall population were similar to those in the subgroup of subjects who required decision making and lacked decision-making capacity.
Table 2. Completion of and Preferences in Advance Directives *.
| Variable | All Decedents (N=3746) | Decedents Who Required Surrogate Decision Making (N=999) | |
|---|---|---|---|
| percent | |||
| Completed living will | 44.9 | 46.4 | |
| Comfort care only | 93.8 | 96.2 | |
| Limited care | 91.3 | 92.7 | |
| All care possible | 3.0 | 1.9 | |
| Assigned durable power of attorney for health care | 54.3 | 61.0 | |
| Child or grandchild | 60.3 | 64.6 | |
| Spouse or partner | 29.6 | 26.9 | |
| Other relative | 7.6 | 6.6 | |
| Nonrelative | 2.7 | 1.9 | |
Percentages are weighted and were derived with the use of sampling weights from the Health and Retirement Study.
Living wills were completed a median of 20 months before death (range, 0 to 399; mean, 43.5±57.5). A durable power of attorney for health care was completed a median of 19 months before death (range, 0 to 1202; mean, 42.9±68.4).
Living Wills and Care Received by Incapacitated Subjects
Incapacitated subjects who had prepared a living will (regardless of preferences) were less likely to receive all treatment possible (adjusted odds ratio, 0.33; 95% CI, 0.19 to 0.56) and more likely to receive limited treatment (adjusted odds ratio, 1.79; 95% CI, 1.28 to 2.50) than subjects without a living will (Table 3). Living wills were associated with increased odds of receiving comfort care (adjusted odds ratio, 2.59; 95% CI, 1.06 to 6.31) and, although not significant, a trend toward decreased odds of dying in a hospital (adjusted odds ratio, 0.71; 95% CI, 0.47 to 1.07).
Table 3. Key Outcomes According to Advance-Directive Status among 999 Subjects *.
| Outcome | Living Will (N = 444) | No Living Will (N=552) | Adjusted Odds Ratio (95% CI) | DPAHC (N = 589) | No DPAHC (N=407) | Adjusted Odds Ratio (95% CI) |
|---|---|---|---|---|---|---|
| % of subjects | % of subjects | |||||
| Death in a hospital | 38.8 | 50.4 | 0.71 (0.47–1.07) | 38.2 | 55.8 | 0.72 (0.55–0.93) |
| All care possible | 8.1 | 27.7 | 0.33 (0.19–0.56) | 13.4 | 27.0 | 0.54 (0.34–0.86) |
| Limited care | 80.6 | 66.0 | 1.79 (1.28–2.50) | 75.4 | 68.1 | 1.18 (0.75–1.85) |
| Comfort care | 96.8 | 91.3 | 2.59 (1.06–6.31) | 95.9 | 90.6 | 2.01 (0.89–4.52) |
Percentages are weighted and were derived with the use of sampling weights from the Health and Retirement Study. DPAHC denotes durable power of attorney for health care.
Among 435 incapacitated subjects who had prepared living wills and who had expressed a preference for or against all care possible, there was strong agreement between their stated preference and the care they received (McNemar's chi-square test with 1 degree of freedom, 17.86; P<0.001). However, outcomes appeared to vary according to the type of choice made. Of 425 subjects who did not indicate a preference for all care possible, 30 (7.1%, unweighted percentage) received it; among the 10 subjects who did indicate a preference for all care possible, 5 (50.0%, unweighted percentage) did not receive their choice. Of those subjects who did not receive their choice, four had appointed a durable power of attorney. Subjects who had requested all care possible were more likely to receive it than subjects who did not request it (adjusted odds ratio, 22.62; 95% CI, 4.45 to 115.00).
Of the 398 incapacitated subjects who had prepared a living will and had requested limited care, 331 (83.2%, unweighted percentage) received it; of the 36 subjects who had not requested limited care, 17 (47.2%, unweighted percentage) received it (McNemar's chi-square test with 1 degree of freedom, 29.76; P<0.001). In adjusted analyses, subjects who had requested limited care were more likely to receive it than subjects who had not requested limited care (adjusted odds ratio, 8.11; 95% CI, 3.23 to 20.32).
Of 417 incapacitated subjects who had requested comfort care, 405 (97.1%, unweighted percentage) received it. Of the 29 subjects who did not request comfort care, 15 (51.7%, unweighted percentage) received it. (McNemar's chi-square test with 1 degree of freedom, 0.33; P=0.56). However, in adjusted analyses, subjects who had requested comfort care were more likely to receive comfort care than subjects who had not requested it (adjusted odds ratio, 11.57; 95% CI, 1.34 to 99.81).
A total of 89.0% of the proxies (95% CI, 86.0 to 92.1) reported that the living will was applicable to most decisions faced by surrogates. A total of 13.6% of proxies (95% CI, 10.5 to 16.7) reported problems in following the subject's instructions (see the Supplementary Appendix for the exact wording of the question).
Durable Power of Attorney, Surrogate Decision Maker, and Treatment Received
Among subjects who required decision making, had lost decision-making capacity, and had appointed a durable power of attorney for health care, in 91.5% of subjects (95% CI, 89.1 to 93.9) the actual decision maker matched the appointed surrogate. In a test of symmetry, there was no difference between the actual and appointed decision maker (chi-square test with 7 degrees of freedom, 11.42; P = 0.12).
Subjects who had appointed a durable power of attorney for health care were less likely to die in a hospital (adjusted odds ratio, 0.72; 95% CI, 0.55 to 0.93) or receive all care possible (adjusted odds ratio, 0.54; 95% CI, 0.34 to 0.86) than those who had not appointed a durable power of attorney (Table 3). There were no significant differences between the two groups of subjects with respect to the receipt of limited or comfort care, after adjustment for potential confounding.
Discussion
We found that surrogate decision making is often required for elderly Americans at the end of life. Among our subjects, 42.5% needed decision making about medical treatment before death; in this group, 70.3% of subjects lacked the capacity to make those decisions themselves. In short, 29.8% required decision making at the end of life but lacked decision-making capacity. These findings suggest that more than a quarter of elderly adults may need surrogate decision making before death. Our data indicate that predicting which people will need surrogate decision making may be difficult. In our multivariate logistic-regression analysis, cognitive impairment, cerebrovascular disease, and residence in a nursing home were associated with lost decision-making capacity before death; however, these characteristics were present in 76.6% of the entire study population.
Among subjects who needed surrogate decision making, 67.6% had an advance directive. This result confirms previous findings3 and shows a great increase in the use of advance directives since the Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments8 first reported that only 21% of seriously ill, hospitalized patients had an advance directive. The fact that so many elderly adults complete advance directives suggests that they find these documents familiar, available, and acceptable. Moreover, it suggests that elderly patients, their families, and perhaps their health care providers think that advance directives have value.
Subjects who had completed living wills and requested all care possible were much more likely to receive all care possible than were those who had not requested such care. Similarly, subjects who had requested limited or comfort care were more likely to receive such care than were subjects who had not indicated those preferences. In addition, most subjects who had appointed a durable power of attorney for health care had a surrogate decision maker who matched their choice. Although a causal relationship cannot be inferred, our findings suggest that advance directives do influence decisions made at the end of life.
Among the few subjects who wanted aggressive care, however, half did not receive it. Some persons might suggest that this finding indicates that advance directives are used to deny preferred health care. We believe that would be a misinterpretation of our findings, because our regression analyses showed that documenting a preference for aggressive care significantly increased the likelihood of receiving such care as compared with not expressing such a preference. What might explain these findings? First, for many subjects, aggressive care may not have been an option regardless of their preferences. Second, among subjects who wanted all care possible, most had a durable power of attorney for health care to make real-time decisions on their behalf. Surrogates frequently override previously stated preferences, but usually because the circumstances require it, and data indicate that patients want it that way.15 We suggest a more favorable interpretation of our data — namely, that living wills have an important effect on care received and that a durable power of attorney for health care is necessary to account for unforeseen factors. If we accept a durable power of attorney for health care as an extension of the patient, then we must also accept surrogate decisions as valid expressions of the patient's autonomy, even when those decisions conflict with the patient's written preferences before the onset of the terminal illness (as long as the durable power of attorney for health care acts with the patient's best interests in mind).
There were some important limitations of our study. The proxies who provided key data were subject to recall and social-desirability biases, especially with regard to subjective details such as patients' preferences. However, proxy reports are frequently used for death data and medical records quite often do not contain sufficient detail on the content of discussions about advance care planning or patients' preferences with respect to treatment.4,16 Future studies of advance directives and advance care planning would benefit from prospective designs to improve the reliability of data.
Another limitation of our study was the lack of data on preferences for subjects who did not have advance directives. This lack of data limited our ability to compare outcomes with and without advance directives while controlling for preferences.
Finally, our findings cannot be generalized to younger adults — a population that may not have the same need for surrogate decision making at the end of life.
In summary, we found that more than a quarter of elderly adults may require surrogate decision making at the end of life. Both a living will and a durable power of attorney for health care appear to have a significant effect on the outcomes of decision making. Thus, advance directives are important tools for providing care in keeping with patients' wishes. For more patients to avail themselves of these valuable instruments, the health care system should ensure that providers have the time, space, and reimbursement to conduct the time-consuming discussions necessary to plan appropriately for the end of life. Data suggest that most elderly patients would welcome these discussions.17-19
Supplementary Material
Acknowledgments
Supported by core funds from the Ann Arbor Veterans Affairs Center for Clinical Management Research and the Division of General Medicine at the University of Michigan (to Dr. Silveira); a grant (R01 AG027010) from the National Institute on Aging and a Paul Beeson Physician Faculty Scholars in Aging Research award (to Dr. Langa); a grant (U01 AG09740) from the National Institute on Aging for the Health and Retirement Study, which was performed at the Survey Research Center, Institute for Social Research, University of Michigan; and a Greenwall Faculty Scholarship in Bioethics (to Dr. Kim).
We thank Mohammed Kabeto, M.S., for his advice on data management and analysis and Jenny Chen for editorial assistance.
Footnotes
No potential conflict of interest relevant to this article was reported.
The views expressed are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the U.S. government.
References
- 1.Brown BA. The history of advance directives: a literature review. J Gerontol Nurs. 2003;29:4–14. doi: 10.3928/0098-9134-20030901-04. [DOI] [PubMed] [Google Scholar]
- 2.Pub Law No. 101-508. 1990. Omnibus Budget Reconciliation Act of 1990. [Google Scholar]
- 3.O'Brien M. Finance committee to drop end-of-life provision. [March 5, 2010];The Hill. 2009 August 13; http://thehill.com/homenews/senate/54617-finance-committee-to-drop-end-of-life-provision.
- 4.Teno JM, Gruneir A, Schwartz Z, Nanda A, Wetle T. Association between advance directives and quality of end-of-life care: a national study. J Am Geriatr Soc. 2007;55:189–94. doi: 10.1111/j.1532-5415.2007.01045.x. [DOI] [PubMed] [Google Scholar]
- 5.Fagerlin A, Schneider CE. Enough: the failure of the living will. Hastings Cent Rep. 2004;34:30–42. [PubMed] [Google Scholar]
- 6.Smedira NG, Evans BH, Grais LS, et al. Withholding and withdrawal of life support from the critically ill. N Engl J Med. 1990;322:309–15. doi: 10.1056/NEJM199002013220506. [DOI] [PubMed] [Google Scholar]
- 7.Schneiderman LJ, Kronick R, Kaplan RM, Anderson JP, Langer RD. Effects of offering advance directives on medical treatments and costs. Ann Intern Med. 1992;117:599–606. doi: 10.7326/0003-4819-117-7-599. [DOI] [PubMed] [Google Scholar]
- 8.Teno JM, Lynn J, Phillips RS, et al. Do formal advance directives affect resuscitation decisions and the use of resources for seriously ill patients? J Clin Ethics. 1994;5:23–30. [PubMed] [Google Scholar]
- 9.Lo B, Saika G, Strull WM, Thomas E, Showstack J. ‘Do not resuscitate’ decisions: a prospective study at three teaching hospitals. Arch Intern Med. 1985;145:1115–7. [PubMed] [Google Scholar]
- 10.Goodman MD, Tarnoff M, Slotman GJ. Effect of advance directives on the management of elderly critically ill patients. Crit Care Med. 1998;26:701–4. doi: 10.1097/00003246-199804000-00018. [DOI] [PubMed] [Google Scholar]
- 11.Danis M, Southerland LI, Garrett JM, et al. A prospective study of advance directives for life-sustaining care. N Engl J Med. 1991;324:882–8. doi: 10.1056/NEJM199103283241304. [DOI] [PubMed] [Google Scholar]
- 12.Degenholtz HB, Rhee YJ, Arnold RM. The relationship between having a living will and dying in place. Ann Intern Med. 2004;141:113–7. doi: 10.7326/0003-4819-141-2-200407200-00009. [DOI] [PubMed] [Google Scholar]
- 13.Juster FT, Suzman R. An overview of the Health and Retirement Study. J Hum Resour. 1995;30 Suppl:S7–S56. [Google Scholar]
- 14.Soldo BJ, Hurd MD, Rodgers WL, Wallace RB. Asset and health dynamics among the oldest old: an overview of the AHEAD Study. J Gerontol B Psychol Sci Soc Sci. 1997;52:1–20. doi: 10.1093/geronb/52b.special_issue.1. [DOI] [PubMed] [Google Scholar]
- 15.Sehgal A, Galbraith A, Chesney M, Schoenfeld P, Charles G, Lo B. How strictly do dialysis patients want their advance directives followed? JAMA. 1992;267:59–63. [PubMed] [Google Scholar]
- 16.Teno JM, Clarridge BR, Casey V, et al. Family perspectives on end-of-life care at the last place of care. JAMA. 2004;291:88–93. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- 17.Smucker WD, Ditto PH, Moore KA, Druley JA, Danks JH, Townsend A. Elderly outpatients respond favorably to a physician-initiated advance directive discussion. J Am Board Fam Pract. 1993;6:473–82. [PubMed] [Google Scholar]
- 18.Edinger W, Smucker DR. Outpatients' attitudes regarding advance directives. J Fam Pract. 1992;35:650–3. [PubMed] [Google Scholar]
- 19.Steinhauser KE, Christakis NA, Clipp EC, et al. Preparing for the end of life: preferences of patients, families, physicians, and other care providers. J Pain Symptom Manage. 2001;22:727–37. doi: 10.1016/s0885-3924(01)00334-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.