Abstract
The present study addressed the following questions: (a) To what extent do different methods of measuring the family environment converge onto a single latent construct? (b) How are the constructs of positive and of negative family environment related? (c) Do the associations among various methods of measuring the family environment differ as a function of children's gender or of risk? and (d) How are the latent constructs of family environment related to depression in mothers and their children? Participants were 240 children (mean age = 11.86 years, SD = 0.57) and their mothers, who varied with regard to their history of depression. Family environment was measured with self-report questionnaires completed separately by mothers and by children, observations of mother–child interactions, and a 5-min speech sample of each mother talking about her child. Confirmatory factor analyses revealed that different methods for assessment of the family environment converged and that the constructs of positive and of negative family environments were significantly related to each other and to depression in both mothers and their children. These findings may help inform future intervention efforts by highlighting specific parenting dimensions that are strongly associated with maternal and with child depression.
Keywords: family environment, depression, adolescents, multimethod assessment
Offspring of depressed parents are at increased risk for psychopathology, in particular for mood disorders, compared with children of nondepressed parents (Beardslee, Versage, & Gladstone, 1998). The familial transmission of psychopathology from parents to children is likely the result of both genetic and environmental factors, particularly in the family context (Goodman & Gotlib, 1999). A growing empirical literature has shown that relationships between depressed parents and their children are disrupted during infancy, childhood, and adolescence (Goodman & Gotlib, 1999; Hammen, 1991). The extent and form of the disruption, however, vary depending on operationalization and the method of measuring the family environment, which has been assessed with self-report questionnaires completed by parents and/or children, by behavioral observation, or by coding family members' comments about one another (ex-pressed emotion). Our primary purpose in the current study was to explore these distinct methods of assessing the family environment in relation to each other and to depression in mothers and their children.
Family environments characterized by high levels of negativity, conflict, disengagement, or otherwise adverse relationships have been found to be associated with higher levels of depression in youths (e.g., Sheeber, Hops, & Davis, 2001). Studies using adolescent-report measures of the family environment have shown that perceptions of a negative family milieu (e.g., not cohesive, unsupportive, or enmeshed) were associated with more depressive symptoms and disorders (e.g., Cumsille & Epstein, 1994). Similarly, studies that assessed the family environment with parent-report measures have shown a significant relation between low-quality parenting (e.g., low levels of supportive–positive or high levels of harsh-negative parenting behaviors) and greater levels of depressive symptoms in the children (e.g., Dallaire et al., 2006). Finally, studies that used two methods (e.g., Allen et al., 2006; Millikan, Wamboldt, & Bihun, 2002) or three methods (e.g., Sheeber, Hops, Alpert, Davis, & Andrews, 1997; Sheeber & Sorensen, 1998) for assessment of the family environment have found a significant association between a negative family milieu and depression in youths. The current study examined the extent to which a single latent construct of the family environment comprising four different methods covaried with both maternal and child depression.
In the present study, the four methods of assessing the family environment were parent self-report, child self-report, observation of mother–child interactions, and speech samples from the mother about the child. The family environment has most commonly been assessed via questionnaires completed by parents and/or children. For example, studies using parent reports (Billings & Moos, 1983) have found that depressed parents describe their family atmosphere more negatively than do nondepressed parents. Observational studies have shown that parent–child interaction patterns are substantially different for depressed compared with nondepressed mothers and their children (Hops et al., 1987; Lovejoy, Graczyk, O'Hare, & Neuman, 2000), and such negative interactions have been linked with poorer psychosocial functioning in offspring (e.g. Goodman, Adamson, Riniti, & Cole, 1994).
Another method of measuring the family environment involves a 5-min speech sample used for assessment of the parent's level of expressed emotion (EE) about the child. EE has been defined as “a measure of family atmosphere assessed by an interview with the patient's most important family members” (Hooley, 2004, p. 202); typically, it is coded with regard to the affective qualities of speech content, tone of voice, and positive and negative remarks. The indices of EE most commonly used in child samples have been criticism and emotional overinvolvement, with criticism being more often related to child outcomes. Depressed mothers exhibit higher levels of criticism than do nondepressed mothers (Frye & Garber, 2005; Goodman et al., 1994), and high EE in depressed mothers is associated with higher rates of psychopathology in their children (Schwartz, Dorer, Beardslee, & Lavori, 1990) than in the offspring of depressed mothers with low EE.
Studies that used these various methods of measurement have not yielded an altogether uniform pattern of results, however (e.g., Goodman et al., 1994; Gordon et al., 1989). This lack of consistency may be because studies typically have measured the family environment with different assessment methods (i.e., child or parent self-report and/or behavioral observation) and often have used only one or two of these methods at a time. Few studies have included multiple reporters or multiple methods with the same sample.
In a search of the PsycInfo database from 1984 to 2006 and of reference lists from relevant studies, we identified over 100 empirical studies that had assessed some aspect of the family environment. For each study, we tabulated the number of methods used; self-report from children and from parents were counted as two different methods. The final tally showed that 69% (n = 70) of the studies reviewed used only one method for assessment of the family environment, 21% used two methods, and only 11% used three methods. No single study examined simultaneously the relations among the four particular methods described here.
A limitation of studies with a single informant is the problem of method variance and of reporter bias, which can lead to the spurious inflation of associations among theoretically related constructs (e.g., Lorenz, Conger, Simon, & Whitbeck, 1991). To address this problem, researchers have recommended using different informants and methods of assessment and testing the relations among them (e.g., Millikan et al., 2002; Sheeber et al., 1997). Consistent with this suggestion, we assessed the family environment using multiple informants and methods. Our first aim in the present study was to examine the degree to which these different methods of measuring the family environment converged onto a similar underlying construct.
Positive features of the family typically include cohesion, engagement, and warmth, whereas negative features include criticism, hostility, and overcontrol. What is known about the relation between these positive and negative features? Whereas some studies have found negligible or moderate correlations between measures of positive and of negative family environments (e.g., Dallaire et al., 2006; Eisenberg et al., 2001; Harrist, Pettit, Dodge, & Bates, 1994), with a range from −.10 to −.43, others have found that positive and negative family environments appear to be two components of a broader construct; they either have shown large correlations between the two (e.g., −.75 in Sheeber et al., 1997) or have aggregated the two constructs into one variable (e.g., Forgatch & DeGarmo, 1999). Our second goal in this study was to examine the association between the latent constructs of positive and of negative family environments as measured with multiple methods.
The present study also explored two potential moderators of the association between, and factor loadings within, positive and negative family environments: gender and risk. Gender was tested because there is some evidence that the measurement models of family process variables differ for males and for females. Sheeber et al. (1997) found that female and male adolescents differed significantly in the factor loadings of several observed variables onto the latent family process variable (i.e., familial support and familial conflict, respectively). Other studies, however, have not reported gender differences in the measurement models of family process variables (e.g., Eisenberg et al., 2001).
A second potential moderator is risk, defined here as the presence (high risk) or absence (low risk) of a mother with a history of a diagnosed mood disorder. Although there is considerable evidence of low-quality relationships in families with a depressed mother (e.g., Goodman & Gotlib, 1999; Lovejoy et al., 2000), much less is known about the extent to which different methods of assessing the family environment similarly cohere in high-risk and in low-risk families. Methodologically, there is some evidence that less well-functioning families have lower rates of agreement among family members (e.g., Gribble et al., 1993; Kerig, 1995). Conceptually, high-risk families may be characterized in one of the following ways relative to low-risk families: (a) lower levels of positive emotions and of other positive family processes (positivity); (b) higher levels of negative emotions and of other negative family processes (negativity); (c) lower levels of positivity and higher levels of negativity; or (d) higher levels of positivity and higher levels of negativity. In high-risk families that fall into the first two categories, as opposed to low-risk families, we would expect a lower association (closer to 0) between positive and negative family environments. However, if high-risk families fell into either of the latter two categories, we would expect stronger associations between positive and negative family environments (closer to −1.0 or +1.0, respectively). The present study explored the potential moderating roles of gender and of risk in the measurement of and association between the positive and negative family environment constructs assessed here.
In summary, studies have not yet specifically examined the relations among parent and child perceptions, observations of parent–child interactions, and parents' verbalizations (expressed emotions) in families with a depressed parent, yet all of these measurement methods are presumed to reflect the family environment. Our primary purpose in this study was to examine the convergent validity of these different methods of assessing the family environment and their relation to depression in mothers and their children. The following questions were addressed: (a) To what extent do the different methods of measuring the family environment converge onto a single latent construct? (b) How are the constructs of positive and of negative family environment related? (c) Do the associations among various methods of measuring the family environment differ as a function of children's gender or of risk? and (d) How are the latent constructs of family environment related to depression in mothers and their children?
Method
Participants
Participants were 240 children, who were assessed in the sixth grade (M = 11.86 years of age, SD = 0.57), and their mothers. The sample of children was 54.2% female and was 82% Caucasian, 14.7% African American, and 3.3% other (Hispanic, Asian, Native American). Families were predominantly working class (e.g., nurse's aide, salesclerk) to middle class (e.g., store manager, teacher) with a mean socioeconomic status (Hollingshead, 1975) of 41.84 (SD = 13.25). A majority of the mothers were married or cohabiting (61%) and had less than a college education (61%).
Procedure
Parents of children finishing the fifth grade in metropolitan public schools were invited to participate in a study about parents and children. A brief health history questionnaire comprising 24 medical conditions (e.g., heart disease, depression) and 34 medications from several classes of medications (e.g., antihypertensives, antidepressants) was sent with a letter describing the project to over 3,500 families. Of the 1,495 mothers who indicated an interest in participation, the 587 who endorsed a history of depressive symptoms, use of antidepressants, or no psychopathology were interviewed further by telephone. The remaining families were excluded, because the mother did not indicate depression or indicated either other kinds of psychiatric problems without depression or serious medical illness (e.g., cancer, multiple sclerosis). On the basis of these screening calls, 349 mothers were identified who reported either a history of depressive symptoms (n = 247) or no history of psychiatric problems (n = 102). We interviewed them in person with the Structured Clinical Interview for DSM–III–R diagnoses (SCID; Spitzer, Williams, Gibbon, & First, 1990) to confirm the presence or absence of a lifetime diagnosis of a depressive disorder. On the basis of these SCID interviews, 109 families were excluded for the following reasons: They did not indicate sufficient symptoms to meet criteria for a depressive disorder (38%); they had other psychiatric disorders that did not include a depressive disorder (19%); they or the target child had a serious medical condition (14%); they were no longer interested (21%); the target child either was in the wrong grade or was in special education (6%); or the family had moved out of the area (2%). The final sample consisted of 185 mothers who had been diagnosed with depressive disorders (e.g., major depressive disorder, dysthymia) and 55 mothers who were lifetime free of psychiatric diagnoses.
A research assistant who was unaware of the mothers' psychiatric history administered a battery of questionnaires separately to the mothers and to the adolescents. All data were collected in participants' homes. Informed consent was obtained from all participating parents and children; the study protocol was approved by the Vanderbilt University Institutional Review Board. Measures relevant to the current study are described below.
Measures
Mother/child self-report family measures
Each mother and child completed the following family measures: the Family Environment Scale (FES; Moos & Moos, 1986), the Family Assessment Device–General Functioning subscale (FAD–GF; Epstein, Baldwin, & Bishop, 1983), the Conflict Behavior Questionnaire (CBQ; Prinz, Foster, Kent, & O'Leary, 1979), and the Children's Report of Parent Behavior Inventory (CRPBI; Schaefer, 1965; Schludermann & Schludermann, 1970). The three 9-item subscales (Cohesion, Expressiveness, Conflict) comprising the Relationship Index of the FES were used. The Cohesion subscale measures support and commitment provided by family members; the Expressiveness subscale measures the degree to which family members are encouraged to express their emotions directly; and the Conflict subscale measures the extent to which anger and conflict characterize the family. The 12 items of the FAD–GF subscale have a response category ranging from 1 to 4, with a mean greater than 2 indicating difficulty in functioning. The CBQ contains 20 items endorsed either by “yes” or by “no,” with higher scores indicating greater conflict. The 108-item CRPBI has three dimensions: acceptance/rejection, autonomy/psychological control, and firm/lax control. Each child and mother rated the degree of similarity between the behavior described and that of the mother, using a 3-point scale (0 = like, 1 = somewhat like, 2 = not like). The acceptance/rejection scale was used in this study.
Good reliability and validity have been found for the FES (Moos & Moos, 1986), the FAD (Miller, Epstein, Bishop & Keitner, 1985), the CBQ (Robin & Foster, 1989), and the CRPBI (Schludermann & Schludermann, 1970). Because the FES and the CBQ items are scored in a dichotomous manner, tetrachoric reliability analyses were conducted in the current sample: cohesion (child = .90; mother = .93), expressiveness (child = .59; mother = .68), and conflict (child = .86; mother = .88). On the CBQ, the tetrachoric correlations for children's ratings of conflict with the mother were .97; mothers' ratings of conflict with the child were .97. In this sample, Cronbach's alphas were .86 (child) and .90 (mother) for the FAD–GF subscale and were .95 (children's report) and .87 (mothers' report) for the CRPBI Acceptance subscale.
Observation
The Conflict-Resolution Task involved a 10-min videotaped interaction, during which the parent and the child discussed and worked to resolve some issue that both indicated was a problem between them. In the current study, nine trained raters coded both the mother and the child on 14 items that reflected positive relations and negativity (e.g., expresses positive emotions, displays negative facial expressions). Mothers also were rated on 3 items assessing parental control (e.g., issues orders to the child). Children also were rated on 5 items measuring compliance (e.g., displays defiant body posture, complies with parent's wishes).
Following Simpson, Ickes, and Blackstone (1995), we assessed interrater reliabilities by treating the nine raters as items and then calculating an alpha reliability coefficient for each 9-item variable. Because the interrater reliabilities were high for all variables (mean αs = .91 for mothers and .93 for children), the 9 ratings for each variable were averaged together. Exploratory factor analyses of these composites (17 ratings of mothers and 19 ratings of children) revealed three distinct factors for mothers and for children separately: negativity, positive relations, and active involvement. The negativity and positive relations factors were used in the present study. Factor scores were based on unit-weighted composites of variables with factor loading above .60 on a given factor.
Speech samples; expressed emotion
Using the Five-Minute Speech Sample (FMSS; Magana, Goldstein, Karno, & Miklowitz, 1986), we asked mothers to talk for 5 min about the target child and their relationship. The FMSS yields ratings of overall EE, criticism, and emotional overinvolvement. Critical comments are statements of dissatisfaction with the child or his/her behaviors that contain negative or hostile emotions on the basis of verbal content or of vocal quality. A high emotional overinvolvement score is given if the mother makes comments that suggest her emotional well-being and affect regulation are strongly predicated on her child's emotional state. In the present study, the number of criticisms and number of positive remarks were used in the analyses.
The FMSS has adequate interrater reliability and concurrent validity with the Camberwell Family Interview, an in-depth 90-min interview originally designed for assessment of EE (Magana et al., 1986). The audiotaped recordings in this study were scored by individuals with extensive EE coding experience from Michael Goldstein's laboratory at the University of California, Los Angeles. Interrater reliability was scored on a random subset of tapes by a second trained rater. Both raters were unaware of study hypotheses, participants' risk group, and each other's ratings. Kappas were > .84.
Maternal depression
Mothers' current depressive symptoms were assessed with the Beck Depression Inventory (BDI; Beck, Ward, Mendelson, Mock, & Erbaugh, 1961), the negative affect scale of the Positive and Negative Affect Scale (PANAS; Watson, Clark, & Tellegen, 1988), and the six-item Depression subscale of the Brief Symptom Inventory (BSI; Derogatis, 1982). All three measures have been found to have good psychometric properties (Beck, Steer, & Garbin, 1988; Derogatis, 1982; Watson et al., 1988). Alpha coefficients in this sample were .91 for the BDI, .91 for the PANAS—Negative, and .90 for the BSI Depression subscale.
Children's depression
Children's depressive symptoms were assessed with the Children's Depression Inventory (CDI; Kovacs, 1981), the parent version of the CDI (P–CDI; Garber, 1984), and a revised version of the Children's Depression Rating Scale (CDRS; Poznanski, Mokros, Grossman, & Freeman, 1985). The CDI and the P–CDI contain 27 items measuring cognitive, affective, somatic, and behavioral symptoms of depression. The 15 items of the CDRS ask about the extent of children's depressive symptoms during the previous 2 weeks. All three measures have been found to have adequate reliability and validity (Carey, Faulstich, Gresham, Ruggiero, & Enyart, 1987; Garber, 1984; Saylor, Finch, Spirito, & Bennett, 1984). Internal consistency in this sample was .81 for the CDI, .87 for the P–CDI, and .72 for the CDRS.
Results
Descriptive statistics and correlations for all study measures related to positive and to negative family environment, respectively, are presented in Table 1.
Table 1.
Zero-Order Correlations, Means, and Standard Deviations of Family Environment Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Positivity | ||||||||||||||||||
| 1. FES, cohesion: child | — | |||||||||||||||||
| 2. FES, expressiveness: child | .40 | — | ||||||||||||||||
| 3. CRPBI, acceptance: child | .56 | .34 | — | |||||||||||||||
| 4. FES, cohesion: mother | .29 | .19 | .31 | — | ||||||||||||||
| 5. FES, expressiveness: mother | .09 | .08 | .22 | .52 | — | |||||||||||||
| 6. CRPBI, acceptance: mother | .21 | .15 | .35 | .49 | .32 | — | ||||||||||||
| 7. Observed positive: child | .11 | .18 | .20 | .15 | .12 | .14 | — | |||||||||||
| 8. Observed positive: mother | .18 | .20 | .28 | .26 | .07 | .27 | .67 | — | ||||||||||
| 9. Number of positive remarks | .08 | .21 | .20 | .24 | .19 | .20 | .15 | .27 | — | |||||||||
| Negativity | ||||||||||||||||||
| 10. FAD: child | −.66 | −.50 | −.65 | −.30 | −.12 | −.27 | −.25 | −.24 | −.12 | — | ||||||||
| 11. CBQ: child | −.53 | −.26 | −.75 | −.19 | −.16 | −.26 | −.17 | −.22 | −.09 | .51 | — | |||||||
| 12. FES, conflict: child | −.62 | −.41 | −.45 | −.22 | −.06 | −.14 | −.22 | −.25 | −.09 | .59 | .52 | — | ||||||
| 13. FAD: mother | −.21 | −.10 | −.26 | −.68 | −.51 | −.46 | −.18 | −.23 | −.15 | .31 | .11 | .12 | — | |||||
| 14. CBQ: mother | −.19 | −.15 | −.36 | −.51 | −.31 | −.55 | −.32 | −.38 | −.19 | .22 | .34 | .14 | .41 | — | ||||
| 15. FES, conflict: mother | −.22 | −.14 | −.23 | −.55 | −.20 | −.49 | −.12 | −.24 | −.08 | .29 | .16 | .23 | .54 | .47 | ||||
| 16. Observed negativity: child | −.28 | −.21 | −.36 | −.26 | −.04 | −.20 | −.44 | −.47 | −.10 | .37 | .34 | .36 | .17 | .37 | .26 | — | ||
| 17. Observed negativity: mother | −.12 | −.08 | −.13 | −.10 | −.02 | −.27 | −.37 | −.52 | −.18 | .18 | .14 | .15 | .10 | .31 | .22 | .53 | — | |
| 18. Number of criticisms | −.28 | −.25 | −.26 | −.28 | −.21 | −.27 | −.09 | −.14 | −.29 | .23 | .29 | .17 | .19 | .33 | .15 | .14 | .20 | — |
| M | 7.18 | 4.24 | 2.57 | 6.80 | 5.59 | 2.57 | 3.14 | 3.23 | 4.13 | 1.92 | 2.88 | 2.72 | 1.81 | 5.51 | 3.35 | 2.09 | 1.86 | 0.36 |
| SD | 1.97 | 1.74 | 0.35 | 2.39 | 1.67 | 0.19 | 0.74 | 0.62 | 2.97 | 0.49 | 3.75 | 2.16 | 0.46 | 4.90 | 2.25 | 0.75 | 0.71 | 0.78 |
Note. FES = Family Environment Scale; CRPBI = Children's Report of Parent Behavior Inventory; FAD = Family Assessment Device; CBQ = Conflict Behavior Questionnaire. Correlations ≥ |.14|, p < .05. Correlations ≥ |.19|, p < .01. Correlations ≥ |.23|, p < .001.
How Are Different Methods of Measuring the Family Environment Related?
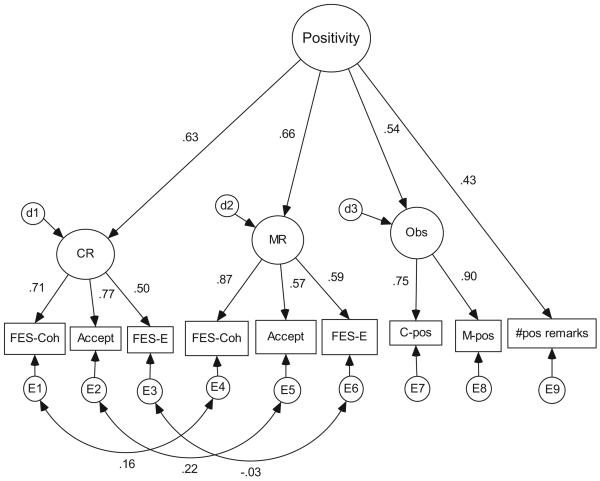
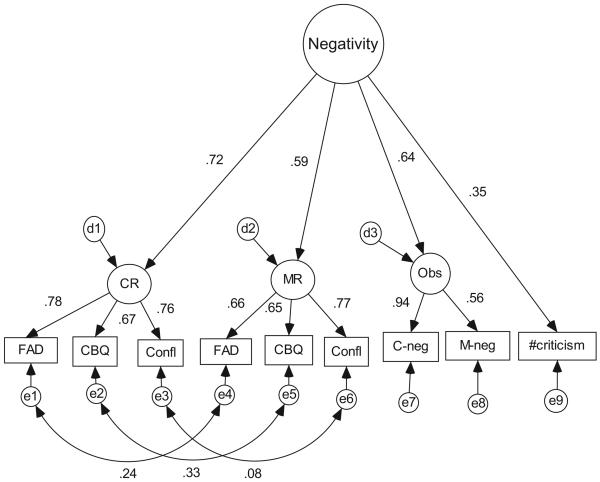
We conducted a second-order confirmatory factor analysis (CFA) to examine the relations among the various measures of positive and of negative family environment, respectively. The same hierarchical structure was imposed on measures that reflect the positive (see Figure 1) and the negative (see Figure 2) family environments, in which the first-order latent factor indicated the method of measurement (e.g., questionnaire, observation, speech sample) and the second-order latent factor indicated quality of the family environment (positive or negative). The positivity construct comprised the child and mother reports on the FES Cohesion and Expressiveness subscales, the CRPBI Acceptance scale, observed positive relations (mother, child), and the total number of positive remarks by the mother on the FMSS. The negativity construct consisted of child and mother reports on the FAD–GF subscale, the CBQ, and the FES Conflict subscale, observed negativity (mother, child), and number of critical remarks by the mother on the FMSS.
Figure 1.
Confirmatory factor analysis model for positive family environment. d = disturbance; CR = child report; MR = mother report; Obs = observed relations; FES–Coh = Family Environment Scale, Cohesion; Accept = acceptance; FES–E = Family Environment Scale, Expressiveness; C-pos = child positive relations; M-pos = mother positive relations; #pos remarks = number of positive remarks; E = error.
Figure 2.
Confirmatory factor analysis model for negative family environment. d = disturbance; CR = child report; MR = mother report; Obs = observed relations; FAD = Family Assessment Device; CBQ = Conflict Behavior Questionnaire; Confl = Family Environment Scale, Conflict; C-neg = child negativity; M-neg = mother negativity; e = error.
For positive family environment, the CFA results indicated that the model fit the data very well, χ2(22, N = 240) = 32.97, p > .05, incremental fit index (IFI) = .98, Tucker–Lewis index (TLI) = .95, comparative fit index (CFI) = .98, root-mean-square error of approximation (RMSEA) = .046. All factor loadings were significant at p < .001. (Because of a negative error variance, we constrained the loadings on the observational measures to be equal.) The negative family environment model also fit the data well, χ2(21, N = 240) = 46.12, p = .001, IFI = .95, TLI = .90, CFI = .95, RMSEA = .07 (see Figure 2). All factor loadings were significant at p < .001. Thus, with respect to the first research question, these results indicate that different methods of measuring positive and negative family environments, respectively, converged onto their respective latent constructs.
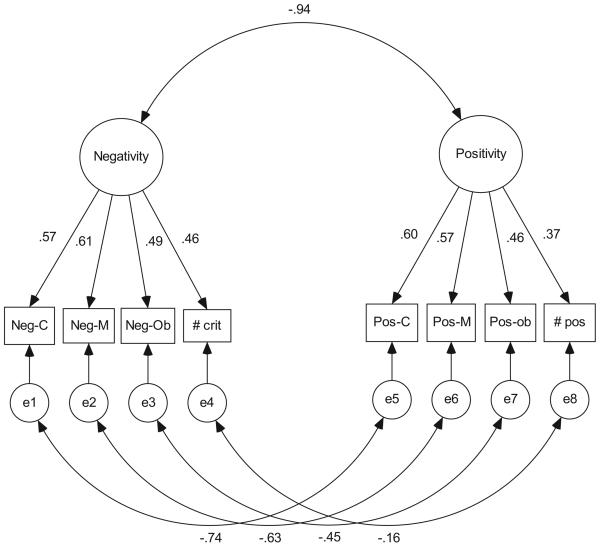
What Is the Relation Between Positivity and Negativity?
To combine the two models in a parsimonious manner, we created standardized (i.e., summed z scores) composite scores for child report, mother report, and observed relations (see Table 2). We used the resulting variables in another CFA model to examine the relation between overall negativity and positivity (see Figure 3). This model fit the data very well, χ2 (15, N = 240) = 22.79, p > .05, IFI = .99, TLI = .97, CFI = .99, RMSEA = .047. Then, we examined the relation between the latent constructs of positivity and of negativity and found the correlation to be −.94 (SE = .03). This model was statistically indistinguishable from a model in which the factor correlation was fixed at −1.00, Δχ2(1, N = 240) = 3.68, p > .05. These results indicate that the relation between the positive and the negative dimensions of the family environment was strongly and negatively correlated.
Table 2.
Zero-Order Correlations, Means, and Standard Deviations of Composite Family Environment Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. Negativity: child | — | |||||||
| 2. Negativity: mother | .32*** | — | ||||||
| 3. Negativity: observed | .35*** | .33*** | — | |||||
| 4. Number of criticisms | .27*** | .28*** | .19* | — | ||||
| 5. Positivity: child | −.81*** | −.32*** | −.28*** | −.33*** | — | |||
| 6. Positivity: mother | −.29*** | −.74*** | −.21** | −.32*** | .33*** | — | ||
| 7. Positivity: observed | −.30*** | −.33*** | −.56*** | −.13 | .26*** | .24*** | — | |
| 8. Number of positive remarks | −.12 | −.17* | −.15* | −.29*** | .21** | .26*** | .23** | — |
| M | 0 | 0 | 0 | .36 | 0 | 0 | 0 | 4.13 |
| SD | 2.49 | 2.40 | 1.75 | 0.78 | 2.35 | 2.35 | 1.82 | 2.97 |
p < .05.
p < .01.
p < .001.
Figure 3.
Relation between positive and negative family environment. Neg-C = negativity, child; Neg-M = negativity, mother; Neg-Ob = negativity, observed relations; # crit = number maternal criticisms; Pos-C = positivity, child; Pos-M = positivity, mother; Pos–ob = positivity, observed; # pos = number positive remarks; e = error.
Multigroup Analyses: Testing for Moderating Effects of Gender and Risk
We conducted separate multigroup CFA analyses for children's gender and for risk, using the combined positivity–negativity model described above. The multigroup analyses revealed no significant gender differences in any of the model parameters: Δχ2(17, N = 240) = 23.64, p > .05, or in the strength of the correlation between the latent positivity and negativity variables across the high- and low-risk groups. Equivalency constraints on the factor correlations alone and on both the factor correlations and the factor loadings did not significantly affect the fit of this model. However, high- and low-risk groups had significant differences in intercepts: Δχ2(8, N = 240) = 42.18, p > .001. A series of t tests indicated that the high-risk group had significantly higher negativity and lower positivity scores than did the low risk group (see Table 3). Thus, neither children's gender nor their risk status was a significant moderator of the relation between positive and negative family environments. However, high- and low-risk children did differ significantly in mean levels of positive and of negative family processes in the expected directions.
Table 3.
Mean Differences From Multigroup Analysis by Risk Status
| Measure | High risk | Low risk | t |
|---|---|---|---|
| Positivity: child | |||
| M | −0.29 | 0.98 | 4.12*** |
| SD | 2.41 | 1.86 | |
| Positivity: mother | |||
| M | −0.34 | 1.15 | 5.20*** |
| SD | 2.44 | 1.58 | |
| Positivity: observation | |||
| M | −0.25 | 0.90 | 3.90*** |
| SD | 1.77 | 1.72 | |
| Number of positive remarks | |||
| M | 3.85 | 4.98 | 2.00* |
| SD | 2.68 | 3.61 | |
| Negativity: child | |||
| M | 0.29 | −0.99 | −3.96*** |
| SD | 2.57 | 1.94 | |
| Negativity: mother | |||
| M | 0.41 | −1.40 | −5.84*** |
| SD | 2.40 | 1.82 | |
| Negativity: observation | |||
| M | 0.19 | −0.68 | −3.40*** |
| SD | 1.78 | 1.45 | |
| Number of criticisms | |||
| M | 0.43 | 0.13 | −3.54*** |
| SD | 0.87 | 0.33 |
p < .05.
p < .01.
p < .001.
What Is the Relation Between the Family Environment and Depression?
Relations between positive and negative family environments and depression were tested separately for mothers and for children. A latent maternal depression factor was extracted from the mothers' BDI, PANAS—Negative, and BSI Depression subscale; it was allowed to correlate freely with positivity and negativity factors. This model fit the data well, Δχ2(37, N = 240) = 65.59, p < .05, CFI = .98, IFI = .98, TLI = .96, RMSEA = .06. The correlation of maternal depression with negativity was .54 (p < .001) and with positivity was −.61 (p < .001). This model was compared with a nested model in which positivity and negativity measures loaded onto a single factor; the comparison forced the implied correlation of depression with negativity and with positivity to be equal. These added constraints did not harm the model fit, Δχ2(2, N = 240) = 5.19, p < .05.
In a second model, a latent child depression factor was extracted from the CDI, the P–CDI, and the CDRS; it was allowed to correlate freely with the positivity and the negativity factors. This model also fit the data well, Δχ2(33, N = 240) = 46.02, p > .05, CFI = .98, IFI = .99, TLI = .97, RMSEA = .04. The correlation of child depression with negativity was .76 (p < .001) and with positivity was −.73 (p < .001). This model was compared with a nested model in which positivity and negativity measures loaded onto a single factor. The added constraints did not harm the model fit, Δχ2(2, N = 240) = 3.79, p > .05. The strength of the association between the family environment and depression was significantly stronger (Steiger's Z = 3.13, p < .01, Hotelling's T2 = 4.29, p < .001) for children (r = 1.731 − 1.761) than for mothers (r = 1.541 − 1.611). Thus, these results show that both positive and negative family environments, respectively, were significantly related to mother's current depression as well as to children's current depression. However, the relation between family environment and current depression was stronger in children than in mothers.
Discussion
In the present study, we investigated four major methods (child self-report, mother self-report, behavioral observation, and EE speech sample) and two key conceptual dimensions (positive and negative) that were designed for assessment of the family environment to examine the degree of convergence (or divergence) among these various methods and dimensions, respectively. We also explored the potential moderating effects of children's gender and of risk on the relations among the different measures and the dimensions of the family environment. Finally, we examined the validity of the family constructs in relation to maternal and child depression.
Confirmatory factor analyses (CFAs) indicated that the different methods and measures for assessment of the family environment converged in terms of both method and dimension. Three different questionnaire measures of the family environment converged separately onto the latent constructs for mother report and for child report. Moreover, the mother and child self-report constructs, the behavioral observation measures, and the speech sample indicators all converged onto their respective dimensions of positive and of negative family environment. Thus, we found empirical evidence for both methodological and conceptual convergence on these procedurally distinct measures of positivity and of negativity in the family environment.
These findings are a unique contribution to the literature, in that prior studies have not examined relations among family environment measures using more than three assessment methods; the current investigation involved four separate methods and found convergence consistent with previous studies using two methods (e.g., McCarty, Lau, Valeri, & Weisz, 2004). Although we labeled the dimensions slightly differently, our findings regarding conceptual convergence are consistent with those of other studies of different dimensions of the family environment (e.g., Dallaire et al., 2006; Sheeber et al., 1997). In the current study, we extended this work by using multiple informants and methods to help minimize shared method variance and reporter bias (e.g., Lorenz et al., 1991) and by using the CFA modeling technique, which captures measurement error.
The CFA results further indicated that the positive and the negative dimensions of the family environment were strongly and negatively correlated. Some prior studies have found strong associations (e.g., r = −.75) between similar dimensions of the family environment, such as “familial support” and “familial conflict” (Sheeber et al., 1997), although other studies have found only moderate or negligible associations between dimensions of the family environment (e.g., Dallaire et al., 2006; Eisenberg et al., 2001). The strength of this correlation may indicate that the constructs of a positive and a negative family environment, as measured in the present study, are not orthogonal or distinct but rather may be opposite ends of the same continuum. This interpretation should be viewed with caution, however, until this result is replicated.
It also is possible that the measures used in the current study were tapping only one of several possible parenting dimensions. Some of the most frequently studied parenting dimensions have included support (e.g., acceptance/rejection, warmth/hostility, responsiveness), control (demanding, autonomy granting/psychologically controlling), and monitoring (firm/lax; e.g., Baumrind, 1971; Schaefer, 1965). One reason for the high correlation between positivity and negativity found in the present study may be that the measures used here reflected primarily the parenting dimension of support/rejection; had we included measures of other parenting dimensions, the correlations likely would have been smaller.
The multigroup CFA analyses indicated that the strength of the relation between positive and negative family environment did not significantly differ as a function of children's gender or risk status. The family measures converged in a meaningful way for both boys and girls and across high- and low-risk groups. The lack of a moderator effect for gender is consistent with previous research that examined the factor structure of different aspects of the family environment (e.g., Eisenberg et al., 2001), although other studies (e.g., Sheeber et al., 1997) have found gender differences on factor loadings for family process variables. Given the differences across these studies in the samples and measures used, future research should continue to test gender as a potential moderator, especially because girls tend to have a greater relational orientation and sensitivity to a wider range of interpersonal environments (Nolen-Hoeksema & Girgus, 1994).
The different methods of assessing the family environment also cohered in both high- and low-risk families. Thus, these various assessment methods appear to be tapping similar constructs for children at different levels of risk. High- and low-risk children, however, did differ significantly in the mean levels of positive and of negative family processes. High-risk families had lower levels of positive emotions and of other positive family processes (positivity) and higher levels of negative emotions and of other negative family processes (negativity) compared with low-risk families. These differences are consistent with the growing literature that shows lower quality interactions in families with a depressed parent (e.g., Lovejoy et al., 2000). This pattern of results fits one of the four proposed conceptualizations of high-risk families (i.e., lower levels of positivity and higher levels of negativity, with stronger associations between positive and negative family environments, closer to r = −1.0). Thus, although the relations between family positivity and negativity were not significantly different as a function of risk, high- and low-risk families were significantly different in their levels of these family characteristics.
Finally, positive and negative family environments each were strongly associated with both mothers' and children's depression in the expected directions. The strength of the overall association between the family environment and depression was significantly stronger for children than it was for mothers. The relative strength of the associations of positive versus negative family environments to depression in both mothers and children, however, was not significantly different.
Limitations of this study highlight directions for future research. First, the results may be specific to the measures of the family environment used in the present study. All possible methods of assessing the family environment were not included. Nevertheless, given that the multiple methods used here converged onto latent constructs, it is likely that these measures were tapping into some underlying commonalities across measures and methods. Second, the sample was predominantly Caucasian, which thus limits the extent to which these findings can generalize to more diverse populations. Empirical examinations of the convergence of various methods of assessing the family environment should be conducted with ethnic minority samples to ascertain whether the same relations hold and to test for possible ethnic or cultural variations. Third, because the sample was predominantly high risk, these results may not generalize to a purely community-based population. Moreover, the low-risk group was relatively small, which may have limited our ability to detect significant moderator effects by risk. Fourth, data on family size was not collected in this study, but this factor should be considered in future research because it may influence the occurrence and the expression of maternal depression. Fifth, the results may be specific to depression in mothers; family environment factors related to depression in fathers may differ and merit investigation as well. Finally, because of the cross-sectional nature of the data, conclusions about the direction of effects cannot be made regarding the relation between the family environment and depression in mothers and children. A logical next step would be to examine these relations longitudinally.
Implications of these results should be noted. First, these four different methods of assessing the family environment converged according to emotional valence and quality; thus, they likely tap similar underlying constructs related to positivity and to negativity in the family environment. Nevertheless, each method still may contribute uniquely to our understanding of the family milieu, and therefore the methods likely cannot be used interchangeably. Second, negative and positive family environments, as measured here, may represent two ends of a bipolar continuum; therefore, it may be appropriate to create a single composite variable that reflects both dimensions. Theoretically, we may still preserve the anchor points of this qualitative continuum (e.g., “positive” and “negative” family environment), although given some information about the level of positivity, it may be possible for us to estimate the level of negativity as well (i.e., the two will likely share a significant inverse association). Several interesting questions remain with regard to this relation. For instance, should positive and negative aspects of the family environment be combined into one measure? Is the absence of a negative family environment similar to the presence of a positive family environment with regard to its relation to other constructs of interest (e.g., psychopathology)? What other dimensions (besides “negative” and “positive”) characterize families, and how do they relate to depression?
Third, both negative and positive family environments, when assessed with these multiple methods and informants, were significantly associated with depression in mothers and in children. Although more research is required for determination of the direction of effects, these findings may assist clinicians in identifying possible targets for intervention. For example, increasing positivity and/or decreasing negativity in the family environment may help to decrease depressive symptoms in family members. On the other hand, interventions aimed at reducing depressive symptoms in mothers or children may contribute to a more congenial family atmosphere. One model for simultaneously addressing both the family environment and a family member's affective illness is a strengths-based, family support program (e.g., Beardslee & Knitzer, 2004) that uses a clinician-facilitated, psychoeducational approach to increase family communication and understanding as well as to enhance parenting. The current findings may help inform such intervention efforts by highlighting specific parenting dimensions that are strongly associated with maternal and child depression.
In summary, the present study provided empirical evidence of the convergence and the utilization of multiple methods in assessing positivity and negativity in the family environment of mothers and their young adolescent off-spring. The constructs of positive and of negative family environments were not orthogonal but rather were highly related; thus, they may have tapped a similar dimension. High-risk children had a less positive and more negative family milieu compared with low-risk children, but the relations among the various measures of the family environment did not differ as a function of risk. Finally, positive and negative family environments were significantly associated with depressive symptoms in both mothers and their children. Future research should address the direction of these relations and should examine how the family environment might protect mothers and their children from depression or place them at greater risk for it.
Acknowledgments
This work was supported in part by National Institute of Mental Health Grants K02 MH66249 and R29 MH45458 and by William T. Grant Foundation Grant 173096. Preparation of this article was funded in part by a National Institute of Mental Health training grant (T32-MH18921) and by National Institute of Child Health and Human Development Grant P30HD15052.
We appreciate the cooperation of the Nashville Metropolitan School District, Drs. Binkley and Crouch, and the parents and children who participated in the project. We also thank Katie Gallerani for her assistance in the literature search on multimethod studies of the family environment, David Cole for his insights on the analyses, and Kerstin Blomquist for her feedback on previous versions of this article.
References
- Allen JP, Insabella G, Porter MR, Smith FD, Land D, Phillips N. A social interactional model of the development of depressive symptoms in adolescence. Journal of Consulting and Clinical Psychology. 2006;74:55–65. doi: 10.1037/0022-006X.74.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumrind D. Current patterns of parental authority. Developmental Psychology Monographs. 1971;4:1–102. [Google Scholar]
- Beardslee W, Knitzer J. Mental health services: A family systems approach. In: Maton KI, Schellenbach CJ, Leadbeater BJ, Solarz AL, editors. Investing in children, youth, families, and communities: Strengths-based research and policy. American Psychological Association; Washington, DC: 2004. pp. 157–171. [Google Scholar]
- Beardslee WR, Versage EM, Gladstone TRG. Children of affectively ill parents: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:1134–1141. doi: 10.1097/00004583-199811000-00012. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Billings A, Moos RH. Comparisons of children of depressed and nondepressed parents: A social–environmental perspective. Journal of Abnormal Child Psychology. 1983;11:463–485. doi: 10.1007/BF00917076. [DOI] [PubMed] [Google Scholar]
- Carey MP, Faulstich ME, Gresham FM, Ruggiero L, Enyart P. Children's Depression Inventory: Construct and discriminant validity across clinical and nonreferred (control) populations. Journal of Consulting and Clinical Psychology. 1987;55:755–761. doi: 10.1037//0022-006x.55.5.755. [DOI] [PubMed] [Google Scholar]
- Cumsille PE, Epstein N. Family cohesion, family adaptability, social support, and adolescent depressive symptoms in outpatient clinic families. Journal of Family Psychology. 1994;8:202–214. [Google Scholar]
- Dallaire DH, Pineda AQ, Cole DA, Ciesla JA, Jacquez F, LaGrange B, Bruce AE. Relation of positive and negative parenting to children's depressive symptoms. Journal of Clinical Child and Adolescent Psychology. 2006;35:313–322. doi: 10.1207/s15374424jccp3502_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR. BSI: Administration, scoring, and procedures manual for the Brief Symptom Inventory—First Edition. National Computer Systems; Minneapolis, MN: 1982. [Google Scholar]
- Eisenberg N, Gershoff ET, Fabes RA, Shepard SA, Cumberland AJ, Losoya SH, et al. Mothers' emotional expressivity and children's behavior problems and social competence: Mediation through children's regulation. Developmental Psychology. 2001;37:475–490. doi: 10.1037//0012-1649.37.4.475. [DOI] [PubMed] [Google Scholar]
- Epstein NB, Baldwin LM, Bishop DS. The McMaster family assessment device. Journal of Marital and Family Therapy. 1983;9:171–180. [Google Scholar]
- Forgatch MS, DeGarmo DS. Parenting through change: An effective prevention program for single mothers. Journal of Consulting and Clinical Psychology. 1999;67:711–724. doi: 10.1037//0022-006x.67.5.711. [DOI] [PubMed] [Google Scholar]
- Frye AA, Garber J. The relations among maternal depression, maternal criticism, and adolescents' externalizing and internalizing symptoms. Journal of Abnormal Child Psychology. 2005;33:1–11. doi: 10.1007/s10802-005-0929-9. [DOI] [PubMed] [Google Scholar]
- Garber J. The developmental progression of depression in female children. In: Cicchetti D, Schneider-Rosen K, editors. Childhood depression: A special edition of “New Directions for Child Development”. Jossey-Bass; San Francisco: 1984. pp. 29–58. [Google Scholar]
- Goodman SH, Adamson LB, Riniti J, Cole S. Mothers' expressed attitudes: Associations with maternal depression and children's self-esteem and psychopathology. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33:1265–1274. doi: 10.1097/00004583-199411000-00007. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Gordon D, Burge D, Hammen C, Adrian C, Jaenicke C, Hiroto D. Observations of interactions of depressed women with their children. American Journal of Psychiatry. 1989;146:50–55. doi: 10.1176/ajp.146.1.50. [DOI] [PubMed] [Google Scholar]
- Gribble PA, Cowen EL, Wyman PA, Work WC, Wannon M, Raoof A. Parent and child views of parent–child relationship qualities and resilient outcomes among urban children. Journal of Child Psychology and Psychiatry. 1993;34:507–519. doi: 10.1111/j.1469-7610.1993.tb01032.x. [DOI] [PubMed] [Google Scholar]
- Hammen C. Depression runs in families: The social context of risk and resilience in children of depressed mothers. Springer-Verlag; New York: 1991. [Google Scholar]
- Harrist AW, Pettit GS, Dodge KA, Bates JE. Dyadic synchrony in mother–child interaction: Relation with children's subsequent kindergarten adjustment. Family Relations. 1994;43:417–424. [Google Scholar]
- Hollingshead AB. Four Factor Index of Social Status. A. B. Hollingshead, Department of Sociology, Yale University, P. O. Box 1965; New Haven, CT 06520: 1975. Available from. [Google Scholar]
- Hooley J. Do psychiatric patients do better clinically if they live with certain kinds of families? Current Directions in Psychological Science. 2004;13:202–205. [Google Scholar]
- Hops H, Biglan A, Sherman L, Arthur J, Friedman L, Osteen V. Home observations of family interactions of depressed women. Journal of Consulting and Clinical Psychology. 1987;55:341–346. doi: 10.1037//0022-006x.55.3.341. [DOI] [PubMed] [Google Scholar]
- Kerig PK. Triangles in the family circle: Effects of family structure on marriage, parenting, and child adjustment. Journal of Family Psychology. 1995;9:28–43. [Google Scholar]
- Kovacs M. Rating scales to assess depression in school-aged children. Acta Paedopsychiatrica: International Journal of Child and Adolescent Psychiatry. 1981;46:305–315. [PubMed] [Google Scholar]
- Lorenz FO, Conger RD, Simon RL, Whitbeck LB. Economic pressure and marital quality: An illustration of the method variance problem in the causal modeling of family processes. Journal of Marriage and the Family. 1991;53:375–388. [Google Scholar]
- Lovejoy MC, Graczyk PA, O'Hare E, Neuman G. Maternal depression and parenting: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Magana AB, Goldstein MJ, Karno M, Miklowitz DJ. A brief method for assessing expressed emotion in relatives of psychiatric patients. Psychiatry Research. 1986;17:203–212. doi: 10.1016/0165-1781(86)90049-1. [DOI] [PubMed] [Google Scholar]
- McCarty CA, Lau AS, Valeri SM, Weisz JR. Parent–child interactions in relation to critical and emotionally overinvolved expressed emotion (EE): Is EE a proxy for behavior? Journal of Abnormal Child Psychology. 2004;32:83–93. doi: 10.1023/b:jacp.0000007582.61879.6f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller IW, Epstein NB, Bishop DS, Keitner GI. The McMaster Family Assessment Device: Reliability and Validity. Journal of Marital and Family Therapy. 1985;11:345–356. [Google Scholar]
- Millikan E, Wamboldt MZ, Bihun JT. Perceptions of the family, personality characteristics, and adolescent internalizing symptoms. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:1486–1494. doi: 10.1097/00004583-200212000-00021. [DOI] [PubMed] [Google Scholar]
- Moos RH, Moos BS. Family Environment Scale manual. 2nd ed. Consulting Psychologists Press; Palo Alto, CA: 1986. [Google Scholar]
- Nolen-Hoeksema S, Girgus JS. The emergence of gender differences in depression during adolescence. Psychological Bulletin. 1994;115:424–443. doi: 10.1037/0033-2909.115.3.424. [DOI] [PubMed] [Google Scholar]
- Poznanski E, Mokros HB, Grossman J, Freeman LN. Diagnostic criteria in childhood depression. American Journal of Psychiatry. 1985;142:1168–1173. doi: 10.1176/ajp.142.10.1168. [DOI] [PubMed] [Google Scholar]
- Prinz RJ, Foster S, Kent RN, O'Leary KD. Multivariate assessment of conflict in distressed and non-distressed mother–adolescent dyads. Journal of Applied Behavior Analysis. 1979;12:691–770. doi: 10.1901/jaba.1979.12-691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robin AL, Foster SL. Negotiating parent–adolescent conflict: A behavioral–family systems approach. Guilford Press; New York: 1989. [Google Scholar]
- Saylor CF, Finch AJ, Spirito A, Bennett B. The Children's Depression Inventory: A systematic evaluation of psychometric properties. Journal of Consulting and Clinical Psychology. 1984;52:955–967. doi: 10.1037//0022-006x.52.6.955. [DOI] [PubMed] [Google Scholar]
- Schaefer ES. Children's reports of parental behavior: An inventory. Child Development. 1965;36:413–424. [PubMed] [Google Scholar]
- Schludermann E, Schludermann S. Replicability of factors in children's report of parent behavior (CRPBI) Journal of Psychology. 1970;76:239–249. [Google Scholar]
- Schwartz CE, Dorer DJ, Beardslee WR, Lavori PW. Maternal expressed emotion and parental affective disorder: Risk for childhood depressive disorder, substance abuse, or conduct disorder. Journal of Psychiatric Research. 1990;24:231–250. doi: 10.1016/0022-3956(90)90013-g. [DOI] [PubMed] [Google Scholar]
- Sheeber L, Hops H, Alpert A, Davis B, Andrews J. Family support and conflict: Prospective relations to adolescent depression. Journal of Abnormal Child Psychology. 1997;25:333–344. doi: 10.1023/a:1025768504415. [DOI] [PubMed] [Google Scholar]
- Sheeber L, Hops H, Davis B. Family processes in adolescent depression. Clinical Child and Family Psychology Review. 2001;4:19–35. doi: 10.1023/a:1009524626436. [DOI] [PubMed] [Google Scholar]
- Sheeber L, Sorensen E. Family relationships of depressed adolescents: A multi-method assessment. Journal of Clinical Child Psychology. 1998;27:268–277. doi: 10.1207/s15374424jccp2703_4. [DOI] [PubMed] [Google Scholar]
- Simpson JA, Ickes W, Blackstone T. When the head protects the heart: Empathic accuracy in dating relationships. Journal of Personality and Social Psychology. 1995;69:434–446. [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M, First MB. User's guide for the structured clinical interview for DSM–III–R. American Psychiatric Press; Washington, DC: 1990. [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]