Abstract
This paper describes the generation of monoclonal antibodies directed to immunogenic nucleoprotein N epitopes of Rift Valley fever virus (RVFV), and their application in diagnostics, both for antibody detection in competitive eLISA and for antigen capture in a sandwich eLISA. Monoclonal antibodies (mAbs) were generated after DNA immunization of Balb/c mice and characterized by western blot, ELISA and cell immunostaining assays. At least three different immunorelevant epitopes were defined by mAb competition assays. Interestingly, two of the mAbs generated were able to distinguish between RVFV strains from egyptian or South African lineages. these monoclonal antibodies constitute useful tools for diagnosis, especially for the detection of serum anti-RVFV antibodies from a broad range of species by means of competitive ELISA.
Key words: RVF, nucleoprotein, competitive ELISA, RVFV lineages
Introduction
Rift Valley fever virus (RVFV) is a mosquito-borne bunyavirus affecting several species of ruminants and man. This virus causes severe epizootics/epidemics in sub-Saharan African countries, and has been traditionally associated with heavy rainfall seasons, favoring infected floodwater mosquito populations to expand and disseminate the virus to livestock and secondary transmission vectors.1 Since RVF has been reported outside subtropical African countries, its possible spread and emergence in northern countries, including those of the Mediterranean basin is now a cause for concern. This circumstance is aggravated since RVFV replication competent mosquito vectors can be found in many European countries, perhaps favored by novel climatic conditions.2,3 Implementation of surveillance systems based on routine diagnostic methods might contribute in avoiding epizootic spread of the disease in susceptible areas.
The virus is transmitted to livestock and humans by mosquito bites or aerosol spills, i.e., when tissues or blood from infected animals are manipulated. The disease caused by RVFV infection in livestock is characterized by acute hepatitis and massive abortion and mortality rates in young animals.4,5 In man, the disease may not be diagnosed since symptoms are usually related with a self-limited febrile illness, but severe complications may occur including retinal degeneration, encephalitis or even hemorrhagic fever.6,7 The virus replicates efficiently in many vector species as well as in a number of different vertebrate species, including wildlife and other experimentally infected animals, whose role in the epidemiology of the disease remains obscure.8 Therefore specific immunodiagnostic assays to test the presence of anti-RVFV antibodies in non-livestock species may be difficult and laborious, relying on neutralization assays.9 Recently, alternative methods for detection of antibodies against RVFV in several species, including wild ruminants, have been developed based on inhibition/competition ELISA assay.10,11
RVFV has a single-stranded, tripartite RNA genome composed of a large (L), medium (M) and small (S) segments. While the L segment encodes an RNA-dependent RNA polymerase, the M segment encodes four proteins, two mature envelope glycoproteins (G1/Gc and G2/Gn), involved in virus-cell interaction, along with two non structural proteins of 14 and 78 kDa. The S segment of RVFV uses an ambisense strategy to code for the nucleocapsid protein, N, in the antigenomic sense, and for a non structural protein, NSs, in the genomic sense.12 The RVFV N protein, as in the case of many other nucleoproteins of negative strand RNA viruses, acts as a scaffold for the packaging of viral, genomic, RNA(-) segments. An essential requirement for the controlled RNA packaging in mature particles is the oligomerization of N monomers to provide the adequate template for RNA binding.13 As is the case with other viral examples,14,15 the RVFV nucleocapsid protein is highly immunogenic. Antibodies against N are readily detected early after infection and in convalescent individuals, providing robust basis for diagnostic detection of the disease.
As described here, we generated a set of monoclonal antibodies (mAbs) directed against immunogenic N epitopes by DNA immunization in order to mimic the host’s immune response to RVFV antigens and ensuring the generation of a repertoire of antibodies similar to that of serum from convalescent animals. The mAbs were characterized and, particularly, their ability to bind to the immunogenic epitopes on the nucleoprotein N was tested in competition assays. The use of this mAb-based approach may improve the current techniques for the assessment of the immune status of many different animal populations at risk of RVFV infection.
Results
Expression of RVFV nucleoprotein N in mammalian and bacterial cells.
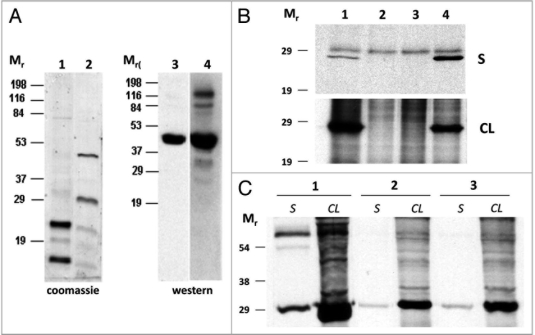
A recombinant Trx-N fusion protein from RVFV was detected using SDS-PAGE in the form of two major polypeptides of 29 and 51 kDa as judged by Coomassie staining (Fig. 1A and columns 1, 2) of pTrx-N transformed bacterial cell extracts. Expressed Trx-N protein was further purified using a nickel-NTA purification column. Immunoblotting using an anti-histidine tag mAb detected two polypeptides of around 51 kDa and 29 kDa, respectively (not shown). However, only the 51 KDa polypeptide was detected by western blotting when a rabbit anti-RVFV was used (Fig. 1A and columns 3, 4), indicating that the 29 KDa polypeptide lacked the epitope(s) of the larger protein recognized by the antiserum. This suggests that the smaller polypeptide may be an incomplete or degraded protein product. Identical result was obtained by western blot, when a sheep anti-RVFV was used instead (Fig. 1A). Expression of the RVFV nucleoprotein gene coded by pCMV-N plasmid was detected at 24 hours post-transfection by immunocytochemistry of cell extracts using a rabbit polyclonal anti-RVFV serum. A strong cytoplasmic immunostaining was detected in transfected cells but not in negative controls transfected with pCMV-GFP (not shown). To analyze the size of the expressed polypeptide, an immunoprecipitation assay was conducted, using either infected or transfected cell extracts. A similar sized polypeptide was immunoprecipitated from pCMV-N transfected and RVFV MP12 infected cell extracts, indicating the proper translation and processing of the cloned nucleocapsid gene. Interestingly, higher amounts of nucleoprotein N were detected in the supernatant of transfected cells compared to those found in the supernatant of MP12 infected cells (Fig. 1B).
Figure 1.
Expression and detection of nucleoprotein N. (A) of recombinant Trx (1) and Trx-N fusion protein (2) in E. coli cells as detected by Coomassie staining of Ni-NTA column purified bacterial extracts, or by anti-RVFV rabbit (3) or sheep (4) hyperinmune sera. (B) Inmunoprecipitation of BHK21 cell supernatants (S) and cell lysates (CL) with a rabbit anti-RVFV polyclonal serum. (1) MP12 infected cells, (2) mock infected cells, (3) pCMV transfected cells and (4) pCMV-N transfected cell extracts. (C) Inmunoprecipitation of supernatant (S) and cell lysates (CL) of MP12 infected BHK21 cells using serum from mice immunized with pCMV-N (2 and 3) or sheep anti-RVFV hyperinmune serum (1). Mr: relative molecular mass in kilodaltons.
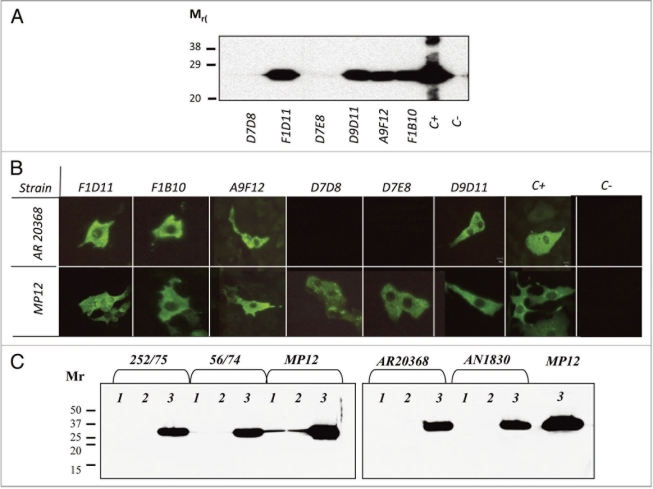
Figure 2.
Detection of nucleoprotein N in infected cells. (A) Western blot of MP12 infected cellular extracts and inmunoblotting with six different mAb supernatants. C+: mouse hyperimmune anti-RVFV serum; C-: preinmmune mouse serum. Relative molecular mass (Mr) is given in kilodaltons. (B) Immunofluorescence of MP12 and South African RVFV strain AR20368 infected Vero cells using the six mAb supernatants tested in (A). (C) Immunoprecipitation of nucleoprotein N expressed in BHK-21 cells infected with ZH548-MP12 or with South African virulent isolates, using mAbs D7D8 (1) and D7E8 (2). A polyclonal mouse anti-RVFV serum (3) was used as positive control. Detection of the immunoprecipitated antigen was performed by western blot using the purified D9D11 mAb conjugated to peroxidase.
Production and characterization of anti-N mAbs.
Once expression of nucleoprotein N in mammalian cells was confirmed, the pCMV-N construct was used to immunize Balb/c mice in order to generate mAbs against the RVFV nucleocapsid protein. The mouse sera were able to immunoprecipitate a polypeptide of the expected size from RVFV infected cell extracts (Fig. 1C), indicating that the antibodies generated were able to recognize virus-induced N protein. Undiluted hybridoma cell supernatants were screened for anti-RVFV-N specific antibodies by antigen capture or indirect recombinant Trx-N ELISA. After subsequent cloning and further expansion and stabilization of the positive hybridomas, six different hybridoma cultures were selected on the basis of their growth kinetics and stability, and their supernatants titrated using both antigen capture and indirect recombinant Trx-N ELISA assays (Table 1). All six mAbs showed reactivity in antigen capture ELISA, but when using indirect recombinant Trx-N ELISA, mAbs D7E8 and D7D8 showed lower or null reactivity. This differential reactivity is suggestive of a differential epitope exposure on the N-protein depending on the assay performed.
Table 1.
Characterization of mAbs anti-RVFV nucleoprotein
| Immunogen | Name | Rec ELISAa | Capture ELISAa | WBb | ICCb | IIFb | Ig isotype |
| DNA only | D7D8 | ⩽3 | 27 | − | + | + | IgG2a/K |
| DNA only | D9D11 | 2187 | ⩾2187 | + | + | + | IgG2a/K |
| DNA only | D7E8 | − | 27 | − | + | + | IgG2a/K |
| DNA only | A9F12 | 2187 | ⩾2187 | + | + | + | IgG2a/K |
| DNA + protein | F1D11 | 27 | 81 | + | + | + | IgG2a/K |
| DNA + protein | F1B10 | 243 | 729 | + | + | + | IgG2a/K |
mean reciprocal dilution of three sample replicates which generates an OD450 nm reading of 1.5.
cells infected with RVFV MP12 strain. WB, western blot; ICC, immunocytochemistry; IIF, indirect immunofluorescence.
The differential epitope recognition by these two mAbs was also illustrated by western blot assays (Fig. 2A). While most anti-N mAbs were able to react to nucleoprotein N in western blotting, mAbs D7E8 and D7D8 failed to recognise the denatured nucleoprotein, thus suggesting that their corresponding epitopes might be conformation dependent. In contrast, these two mAbs were still able to label cells infected with the Egyptian origin MP12 strain by indirect immunofluorescence (IIF) (Fig. 2B, lower). The staining pattern was consistently similar in all mAbs tested, characterized by a homogeneous distribution across the cytoplasm of the infected cell.
Interestingly, by immunofluorescence assay (IFA), both D7E8 and D7D8 mAbs failed to react with BHK-21 cells infected with the AR20368 RVFV isolate from South African origin (Fig. 2B, upper). Identical results were obtained with the other three South African isolates (not shown). Similar results were obtained when the antigen capture ELISA was set up using the South African isolates instead of the MP12 strain as the source of viral antigen, confirming that D7D8 and D7E8 mAbs were specific only for the MP12 attenuated strain (data not shown). Moreover, immunoprecipitation and subsequent western blot assay confirmed the lack of binding of both D7D8 and D7E8 mAbs to the RVFV N protein expressed upon infection of Vero cells with South African isolates, but not when infected with the Egyptian RVFV strain (Fig. 2C). To identify amino acid positions potentially involved in the differential binding of these mAbs, the N ORFs from both the MP12 and the four South African strains were sequenced. Noticeably, the MP12 strain carried G159, while the rest of South African isolates sequenced bore E159 (Fig. 3A).
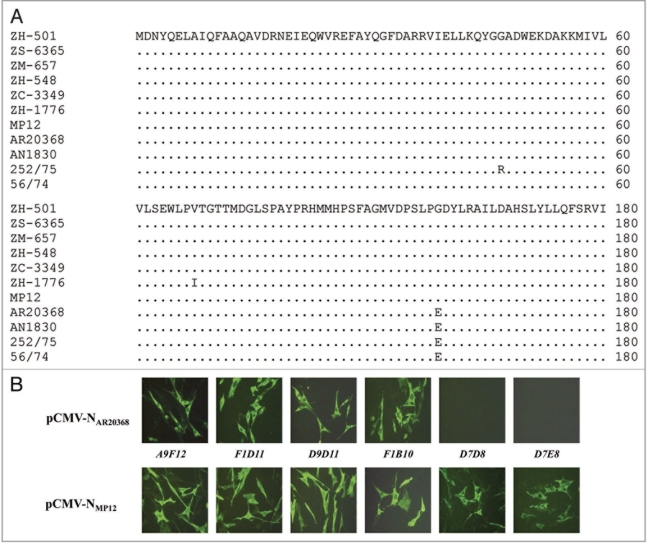
Figure 3.
(A) Conservation plot of the 1–60 (upper) and 121–180 (lower) amino acid regions of the RVFV nucleoprotein N from several Egyptian lineage isolates and the South African strains used in this study. Only the regions of the primary sequence in which amino acid changes were found are showed. (B) Immunofluorescence of transfected BHK-21 cells with pCMV-NAR20368 and pCMV-NMP12 constructs. Expression of N protein was detected with the indicated mAbs.
To exclude the possibility that the observed lack of reactivity was due to lower expression levels or other factors influencing the accessibility of N protein epitopes expressed by the South African strains, the complete N ORF from both the AR20368 strain and MP12, differing only in the amino acid residue 159 were expressed in BHK-21 cells upon transfection with plasmids pCMV-NAR20368 and pCMV-NMP12, respectively. Immunofluorescence data confirmed the previous results, and excluded the lack of reactivity against NAR20368 as a consequence of lower expression levels upon infection with the South African isolates (Fig. 3B). These data suggest that the amino acid residue 159 might influence the binding of mAbs D7E8 and D7D8. Furthermore, a comparison of all RVFV nucleoprotein sequences available at GenBank showed that only Egyptian strains maintained this non-conserved substitution (Fig. 3A). These data would support the value of these mAbs as a diagnostic tool to discriminate strains from the Egyptian lineage.
A further epitope mapping of these antibodies was performed by competitive assay among the mAbs. As shown in Table 2, these mAbs define at least three antigenic sites on the nucleoprotein N based on the percent of inhibition, ranging from high (⩾70%), low (20–50%) or no competition at all (⩽10%). Following this criteria, a first antigenic region may be defined by mAbs F1B10, D9D11 and F1D11, indicating that similar or overlapping epitope(s) are involved. A second region is defined by mAb A9F12. As expected, mAbs D7D8 and D7E8 defined a third antigenic region in nucleoprotein N. Interestingly, these two mAbs could be further differentiated on the basis of their competition with mAb A9F12, suggesting a close relationship among these two antigenic regions. Unfortunately, the specificity of mAbs D7D8, D7E8 and F1B10, was affected when subjected to purification procedures based on acid pH elution, precluding further peroxidase labelling.
Table 2.
Percent of binding inhibition of labelled antibodies in competitive ELISA
| Labelled mAb | |||
| Competitor mAb | A9F12-HRP | F1D11-HRP | D9D11-HRP |
| A9F12 | 92% | 73% | 89% |
| F1D11 | 88% | 95% | 95% |
| D9D11 | 91% | 71% | 89% |
| D7D8 | 43% | 1% | 10% |
| D7E8 | 49% | 0% | 8% |
| F1B10 | 86% | 75% | 91% |
Analysis of mAbs in a competitive binding ELISA assay.
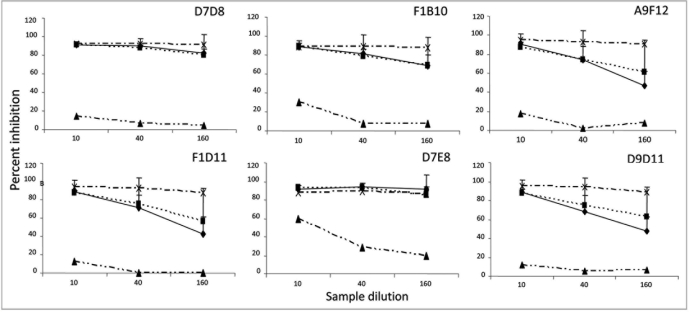
Since all six antibodies demonstrated binding specificity to the RVFV nucleoprotein N in antigen capture ELISA, we then analyzed whether their binding epitopes were also recognized by convalescent sheep serum, in order to design and develop a serological assay based on these mAbs. A preliminary study with different positive sera, including reference sheep field sera, experimental vaccine sera or a hyperimmune rabbit polyclonal serum was carried out. Sera were set to compete for the binding of each mAb to the viral antigen captured in ELISA. Four-fold dilutions of these competitive sera were assayed, ranging from 1/10 to 1/160. Figure 4 shows the mean percentage of binding inhibition of each mAb after incubation with different anti-RVFV sera. All serum dilutions assayed were able to inhibit, with varying degrees, the binding of all the mAbs assayed. In all cases, a clear difference in the percent inhibition values could be established for the negative serum with respect to the positive sera tested. These results indicate that the epitopes recognised by our mAbs are represented in the antibody repertoire generated following immunization or natural/experimental infections.
Figure 4.
Competitive ELISA assay (C-ELISA). Inhibition percentages of six mAb supernatants plotted against different dilutions of the competing sera. OVI reference anti-RVFV pooled sheep sera (♦); sera from experimentally MP12 vaccinated sheep (▪); hyperinmune rabbit anti-RVFV serum (x) and negative pooled sheep sera (▲). Data represent the mean ± SD from three replicate experiments.
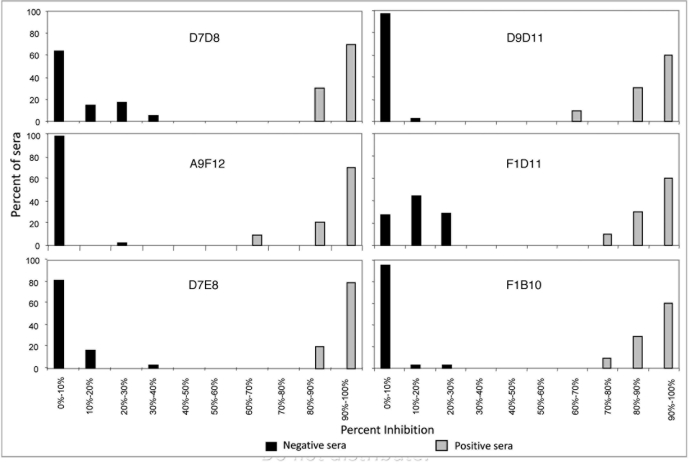
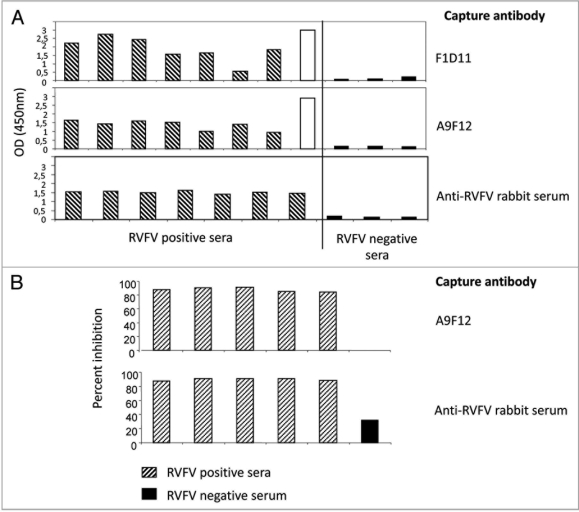
To further estimate a cut off value for discrimination of positive and negative samples, RVFV positive (n = 12) and negative (n = 41) sera were assayed in competition with all six mAbs. The distribution of the inhibition percentages observed for positive and negative samples indicates that the percentage of inhibition of positive sera is ⩾60% whereas inhibition by negative sera is ⩽40%. Therefore, a cut off value in the 40–60% range interval could be assigned for any of the mAbs tested in the competition assay (Fig. 5). Two mAbs, A9F12 and F1D11, were also selected for further characterization due to the high yield of immunoglobulin production by their corresponding hybridoma cells. These mAbs were also evaluated for their ability to concentrate viral antigen from non-purified samples. Figure 6A shows that both F1D11 (upper) and A9F12 (middle) were able to capture viral antigen in a similar way to the rabbit anti-RVFV hyperinmune serum (lower) as judged by the specific binding of hyperimmune sheep or rabbit anti-RVFV sera.
Figure 5.
(A) Discrimination of RVFV positive and negative serum samples in C-ELISA. the percentages of inhibition obtained for each mAb were grouped in classes and plotted against the respective percentage of confirmed RVFV negative (solid bars) and positive (open bars) serum samples.
To check the efficacy of a capture assay in a sandwich ELISA or in competitive assay, purified A9F12 was used to capture virus antigen from MP12 infected cell culture. For detection, A9F12 was peroxidase labeled. In Figure 6B, the ability of A9F12 mAb to discriminate positive sera in a competitive ELISA is shown. The results obtained were very similar to those obtained when rabbit polyclonal sera was used as a capture antibody, indicating the reliability of this format. In particular, lower inhibition values for negative serum are shown when the mAb is used for capture.
Figure 6.
(A) Performance of mAb F1D11 and A9F12 as capture antibodies in ELISA. Positive (experimentally vaccinated sheep, shaded bars and rabbit anti-RVFV hyperinmune serum, open bar) and negative sheep sera (1/120 dilution) were tested in ELISA for their ability to bind to mAb captured viral antigen from infected cell culture supernatants. An anti-sheep HRP-conjugated (diluted to 1/6,000) was used for detection of the inmunocomplexes. (B) Competitive using either purified A9F12 mAb or rabbit anti-RVFV serum as capture antibodies. experimental sera from vaccinated sheep were used to compete the binding of A9F12-HRP labelled antibody.
Discussion
The epidemic potential of Rift Valley fever virus is a matter of international concern for livestock trade and human health. Currently, the risk of unexpected RVF outbreaks in non-endemic areas may be increased by changing climate conditions, including warming oceanic-derived rainfall and increased temperatures, allowing for the establishment of competent vector species in naïve or virgin areas.16 Therefore reliable, fast and versatile diagnostic assays are needed. The RVFV induces a potent antibody response against the nucleoprotein N, but to a much lesser extent to both mature structural glycoproteins. Since the nucleocapsid protein is highly conserved among all sequenced RVFV isolates, this antigen was an obvious choice for newer developments in diagnostic procedures.10,17,18 A recombinant nucleoprotein N-based ELISA test has been recently reported, showing more sensitivity than classical neutralization and haemagglutination-inhibition tests in detecting antibody responses against RVFV infection.18 This method avoids the use of live virus production for subsequent use as ELISA antigen, which is of interest in disease-free areas; however, the use of recombinant antigens may not ensure the proper folding of the protein, thus compromising the sensitivity of an ELISA assay. Two mAbs (D7D8 and D7E8) did not react with the Trx-N fusion protein by ELISA as they did with virus-induced nucleoprotein. Since these mAbs recognise a conformational epitope on the nucleoprotein, it is reasonable to assume that the conformation adopted by the recombinant N differs slightly from that of the virus or solid phase adsorbed N may induce different exposure of epitopes. Similar data were obtained when a baculovirus expressed protein was tested instead of E. coli-derived N (H. Boshra, et al. unpublished observations).
The ability of the virus to replicate in many vertebrate hosts can favour the establishment of the virus in other areas distinct from subtropical Africa. The use of diagnostic tools allowing for virus detection in as many vertebrate species as possible is therefore highly desirable. These tools are of particular importance, since several species of ruminants including cattle, sheep, buffaloes and camels are usually affected; furthermore, ruminant wildlife susceptibility has yet to be determined. The most current assays for the detection of IgM or IgG antibodies have been validated for sheep, goats, cattle and humans, but their usefulness for antibody detection in other susceptible ruminant species, such as camels or wild ruminants should be carefully addressed. The availability of serological assays in which samples can be tested irrespective of their origin, such as the competitive ELISA designed here, may facilitate the determination of the role of other non-livestock species in the RVF enzootic cycle.
In our study, we show the ability of anti-N mAbs to compete with the binding of immune serum to nucleoprotein epitopes exposed by antigen capture ELISA. The ability of the described mAbs to compete is remarkable and may be indicative of the presence of immunogenic epitope(s) located in the nucleocapsid protein. The DNA based immunization strategy used for the generation of mAbs may have contributed to the proper exposure of surrogate determinant(s) mimicking the natural antigens. Studies are in progress to determine the exact location of the corresponding epitope(s). Preliminary data indicate that these epitopes map at the second half of the N polypeptide, when expressed in a baculovirus system (H. Boshra, et al. unpublished observations). Previous reports indicated the generation of monoclonal antibodies against structural elements of the virus particles.19–25 Thus, antibodies against glycoproteins were generated, along with nucleoprotein specific mAbs.25 These antibodies were generated after inmunization with inactivated virus preparations, therefore multiple mAb specificities were found. Our inmunization scheme ensured a directed antibody response towards nucleoprotein N.
The two highest producing hybridomas (A9F12 and F1D11) were selected for further downstream applications. In particular, these mAbs could efficiently capture virus antigen in a similar manner as the polyclonal rabbit serum used in this study as well as for detection of virus in tissues from experimentally infected animals (R. Martín-Folgar, et al. unpublished observations). The use of mAbs in diagnostic tests offers obvious advantages over methods based on the use of polyclonal serum either as capture or detecting antibodies. Therefore, these mAbs may constitute useful tools for improving current tests for identification of RVFV in biological samples and for studies on virus pathogenesis and/or virus cycle functions.
The development of these mAbs might allow for the identification of virus from different geographical origins. In particular, two of the mAbs generated can readily recognise the Egyptian derived mutagenized strain MP12, but not four isolates from S. African origin. Results obtained with these mAbs (D7D8, D7E8) in transfection assays with pCMV-N20368, would confirm their capability to distinguish between Egyptian and South African strains of RVFV. Due to the high degree of conservation displayed by N sequences, this was completely unexpected. Although more viral strains should be tested to confirm this result, it is reasonable to suggest that the location of the epitope(s) defined by D7E8 and D7D8 might be related by residue 159. Interestingly, this is not a conserved amino acid substitution since transition from glycine to glutamic acid implies a significant increase in polarity and charge as well. The relevance of this change in the function of N should be further explored.
The data presented here show that a competitive, mAb-based ELISA (C-ELISA) assay can be designed for detection of RVFV antiserum using mAbs directed against the immunogenic nucleocapsid protein. Further validation of this C-ELISA is required, using a larger number of positive and negative serum samples from animal or human origin.
Material and Methods
Cells and virus.
BHK-21 and Vero cells were maintained in Dulbecco’s modified minimum essential medium (DMEM) (Invitrogen) containing 10% fetal calf serum (FCS). Penicillin (100 U/ml), streptomycin (100 µg/ml) (Invitrogen) and non-essential amino acids were added to the media. The myeloma cell line SP2/0-Ag14 was grown in RPMI medium supplemented with 10% FCS (Sigma). The mutagenized RVFV vaccine strain ZH-548 MP12,26 and 4 virulent South African strains of RVFV, designed AR 20368, AN 1830, 252/75 and 56/74 were propagated in BHK-21 cells at a multiplicity of infection (m.o.i.) of 0.2. When cytophatic effect (cpe) was extensive, cell monolayers were harvested and supernatant fluids were clarified at 3,000 xg for 30 minutes.
Plasmid construction and expression of recombinant antigens.
A DNA SalI/XhoI fragment encoding the nucleoprotein N ORF was excised from a previously generated pXL-TOPO-N construct,27 digested, and subsequently cloned into pET32a (Novagen) to generate a thioredoxin (Trx) fused N ORF (pTrx-N), using the following forward and reverse primers: 5′-ACG CGT CGA CAT GGA CAA CTA TCA AGA GCT TGC GAT CCA-3′ and 5′-CCG CTC GAG GGC TGC TGT CTT GTA AGC CTG AGC GGC TGC CA-3′. The generation of the pCMV-N construct has been described previously.27 The identity and proper insertion of DNA fragments was confirmed by automated DNA sequencing on both strands. For bacterial expression analysis the plasmid was transformed in BL21 cells and expression was induced by addition of 1 mM isopropyl-β-thiogalactoside (IPTG) to the culture medium with constant shaking for 4 hours. Bacterial cultures were then centrifuged, lysed with lysozyme (2 mg/ml) in phosphate buffered saline (PBS) and purified using Ni-NTA resin (Qiagen). Samples were analyzed by SDS-PAGE. Purified proteins from bacterial extracts were visualized after Coomassie staining and their identity confirmed by western blotting using both polyclonal sera against RVFV, or anti-histidine tag mAbs. Monolayers of BHK-21 cells were transfected with the pCMV-N construct using Lipofectamine reagent (Invitrogen) using manufacturer’s instructions. Expression of transfected cells was confirmed by immunocytochemistry analysis using a rabbit polyclonal anti-RVFV serum. A pCMV vector expressing the green fluorescent protein (pCMV-GFP) was used as a negative expression control to assess transfection efficiencies.
Immunization of Balb-c mice and hybridoma cell production.
The pCMV-N construct was used to carry out immunization of Balb-c mice. Two mice were inoculated, by the intramuscular (i.m.) route, with 100 µg of endotoxin free DNA in 100 µl of saline solution. Mice received a total of three doses, every two weeks. Ten days after the last inoculation, mice were bled and the sera were analyzed by immunoprecipitation and/or ELISA. An additional DNA boost was given to one mouse while the other received a subcutaneous boost with an emulsion of recombinant N protein (70 µg) in Freund’s incomplete adjuvant and a last boost, by the intraperitoneal (i.p.) route, of a Percoll-purified MP12 virus preparation (125 µg). Three days later, spleens were aseptically removed for hybridoma preparation following standard procedures.28 The positive wells were initially screened by antigen capture and recombinant ELISA and further cloned. Immunoglobulin isotyping was performed using the Monoclonal Antibody Isotyping Kit (Pierce).
Antibody purification and labelling.
The supernatants of hybridoma cultures were collected, clarified by centrifugation (20,000 × g, 20 min, 4°C) and filtered through a 0.22 µm membrane filter (Millipore). NaCl was added to reach 3 M, equilibrated in 50 mM sodium borate/boric acid buffer, pH 8.9. The resulting solution was loaded on an Econo-Pac protein-A affinity column (Bio-Rad,) pre-equilibrated with five column volumes of NaCl 3 M, 50 mM sodium borate/boric acid buffer. Bound antibodies were eluted stepwise with five column volumes each of PBS and sodium citrate/citric acid buffer 75 mM pH 3.2. Both eluates were collected separately, neutralized to pH 7.2 with HEPES buffer when needed, and analyzed by SDS-PAGE. The antibody containing fractions were pooled and stored for further use.
Labelling of purified Ig was performed as follows. Briefly, horseradish peroxidase (HRP) (Sigma) was dissolved at 50 mg/ml in water. To this solution sodium acetate/acetic acid buffer pH 5.5 (final concentration 15 mM) and sodium periodate (final concentration 3 mM) were added sequentially. The oxidation was allowed to proceed for 7 minutes at 37°C in the dark and was stopped by adding EPPS buffer pH 7.5 (final concentration 25 mM) followed by sodium arsenite (final concentration 13 mM). This solution was mixed with an equal volume of affinity-purified antibody solution (1 mg/ml of immunoglobulin in 75 mM sodium cyanoborohydride, 0.1 M HEPES pH 7.5) and incubated for 12 hours at 37°C. The conjugation reaction was sttoped with ethanolamine (final concentration 6 mM), incubating 15 min at room temperature, and then sodium borohydride (final concentration 2 mM). The entire reaction mixture was loaded on a gravity fed Econo-Pac 10 DG Gel filtration column (Bio-Rad), which was eluted with 15 ml of phosphate buffered saline solution. The fraction eluting at the void volume was collected and assayed for peroxidase activity.
Western blot and immunodetection in infected cells.
Viral proteins (supernatants and cell lysates from BHK-21 cells infected with RVFV-MP12 strain) separated by SDS-PAGE were electrophoretically transferred onto nitrocellulose membranes (Whattman). After overnight blocking with 5% fat-free milk powder in PBS, the membranes were incubated with monoclonal antibodies from hybridoma culture supernatants for 1 h at 37°C. After being washed 3 times with washing solution (5% milk PBS; 0.1% Tween 20), HRPO-conjugated anti-mouse IgG (Sigma) diluted 1:10,000 was added to the membranes and incubated for 1 h at 37°C, washed three times and developed with ECL (Pierce).
For cell immunostaining infected BHK21 cells were fixed in 4% paraformaldehide and permeabilised with 0.25% Triton X-100. After blocking with 20% Fetal Bovine Serum (FBS) the primary mAb was used at 1/2 prior to adding an HRP-conjugated 1:1,000 or Alexa 488 conjugated 1:1,500 secondary antibodies. The HRP-conjugated secondary antibody was visualized using 3-amino-9-ethyl-carbazole as a substrate.
Immunoprecipitation assay was carried out as described earlier.27 Briefly, RVFV MP12 infected BHK-21 cell monolayers were metabolically labeled with [35S]-methionine for 16 h. Supernatants and cell lysates were harvested and incubated with 10 µl of a rabbit anti-RVFV polyclonal serum for 1 h at 37°C and subsequently incubated for 1 h at 37°C with 50 µl protein-G agarose beads (Sigma). Immunocomplexes were analyzed by autoradiography after separation by SDS-PAGE.
A non-radiolabeled immunoprecipitation assay was performed using detergent extracts from Vero cells infected with the South African lineage RVFV isolates or the ZH548-MP12 attenuated RVFV strain (Egyptian lineage). Extracts were incubated, simultaneously, with paramagnetic beads conjugated-protein G (Invitrogen) and mAbs D7D8 and D7E8 for 1 hour. After washing three times with PBS, immunocomplexes were separated by SDS-PAGE and analyzed by western-blot using the D9D11 peroxidase-conjugated mAb.
Antigen capture and indirect recombinant ELISA.
For antigen capture ELISA, plate wells were coated overnight with two different dilutions of rabbit anti-RVFV polyclonal serum (1/2,500, 1/8,000), blocked with 5% fat free milk powder in PBS for 1 h at 37°C and incubated with 5 × 103 pfu of MP12 virus per well. For recombinant N ELISA, immunoplates were coated with 50 ul/well of purified recombinant Trx-N protein in PBS (3 µg/ml), incubated overnight at 4°C and blocked with 10% fat free milk powder in PBS for 1 h at 37°C. Hybridoma culture supernatants were then incubated for 1 hour at 37°C. After washing, a 2 × 10−3 dilution of an anti mouse HRP-conjugated IgG (Sigma) was added. Alternatively, sheep or rabbit hyperinmune sera were detected with anti-sheep (Zymed) or anti-rabbit (Sigma) HRP conjugates. Plates were incubated for 1 h at 37°C, washed 3 times, and 50 µl of soluble tetra methyl benzidine (TMB) substrate (Sigma) was added to each well. Plates were then incubated in the dark at room temperature for a further 5 min. The reactions were stopped by the addition of 50 ul of H2SO4 3 N and the optical density (OD) was determined at 450 nm.
Competitive binding assays.
Different anti-RVFV sera, either from experimentally immunized sheep, rabbit or sheep anti-RVFV reference serum (kindly provided by the Onderstepoort Veterinary Institute (OVI), South Africa) were assayed in a capture ELISA as described above. After 30 min of incubation at 37°C, a non saturating dilution of hybridoma supernatants, i.e., a dilution corresponding to an OD450 nm value ⩽1.5, was added to the wells, and the plates were incubated for 1 h at 37°C. Thereafter, mAb binding was detected following a further 1 h incubation at 37°C in the presence of a 2 × 10−3 dilution of anti-mouse HRP-conjugated IgG (Sigma) and the assay continued as described above. Inhibition percentages were calculated according to the following equation:
.
Cloning and sequencing of nucleoprotein ORFs.
Total RNA from cells infected with the RVFV strains AR 20368, AN 1830, 252/75 and 56/74 was isolated using Tri Reagent (Sigma) and RT-PCR was performed using specific primers described previously27 to obtain cDNA fragments including the complete N ORF. PCR amplification products were purified and subsequently cloned into pGEM-T Easy vector system (Promega). Plasmid containing inserts were sequenced on both strands. For eukaryotic cell expression assay, the AR 20368 N sequence was subcloned in the pCMV plasmid upon digestion with Not I restriction enzyme to generated pCMV-N20368. The proper insertion of the fragment was confirmed by sequencing. pCMV-N20368 was then used to transfect BHK-21 monolayers using the protocol indicated previously.
Acknowledgements
This work was funded by the Spanish Ministry of Science-INIA grant RTA 2005-00017 and from the EU Network of Excellence EPIZONE (Contract no CT2006-016236). R.M.’s work was funded by a fellowship from INIA. H.B. is a recipient of a Juan de la Cierva research program. We thank E. Brocchi (Istituto Zooprofilattico Sperimentale Lombardia ed Emilia-Romagna) for helpful discussions and Dr. T. Gerdes (Onderstepoort Veterinary Institute, OVI) for supplying sheep anti-RVFV sera and RVFV isolates.
Disclosure statement: mAbs D7E8 and D7D8 undergoing preliminary patent application.
Footnotes
Previously published online: www.landesbioscience.com/journals/mabs/article/11676
References
- 1.Gerdes GH. Rift Valley fever. Rev Sci Tech. 2004;23:613–623. doi: 10.20506/rst.23.2.1500. [DOI] [PubMed] [Google Scholar]
- 2.Moutailler S, Krida G, Schaffner F, Vazeille M, Failloux AB. Potential vectors of Rift Valley fever virus in the Mediterranean region. Vector Borne Zoonotic Dis. 2008;8:749–753. doi: 10.1089/vbz.2008.0009. [DOI] [PubMed] [Google Scholar]
- 3.López-Vélez R, Molina R. Climate change in Spain and risk of infectious and parasitic diseases transmitted by arthropods and rodents. Rev Esp Salud Pública. 2005;79:177–190. doi: 10.1590/s1135-57272005000200006. [DOI] [PubMed] [Google Scholar]
- 4.Coetzer JA, Ishak KG. Sequential development of the liver lesions in new-born lambs infected with Rift Valley fever virus I. Macroscopic and microscopic pathology. Onderstepoort J Vet Res. 1982;49:103–108. [PubMed] [Google Scholar]
- 5.Coetzer JA, Ishak KG, Calvert RC. Sequential development of the liver lesions in new-born lambs infected with Rift Valley fever virus II. Ultrastructural findings. Onderstepoort J Vet Res. 1982;49:109–122. [PubMed] [Google Scholar]
- 6.Arthur RR, el-Sharkawy MS, Cope SE, Botros BA, Oun S, Morrill JC, et al. Recurrence of Rift Valley fever in Egypt. Lancet. 1993;342:1149–1150. doi: 10.1016/0140-6736(93)92128-g. [DOI] [PubMed] [Google Scholar]
- 7.Al-Hazmi M, Ayoola EA, Abdurahman M, Banzal S, Ashraf J, El-Bushra A, et al. Epidemic Rift Valley fever in Saudi Arabia: a clinical study of severe illness in humans. Clin Infect Dis. 2003;36:245–252. doi: 10.1086/345671. [DOI] [PubMed] [Google Scholar]
- 8.Bird BH, Ksiazek TG, Nichol ST, Maclachlan NJ. Rift Valley fever virus. J Am Vet Med Assoc. 2009;234:883–893. doi: 10.2460/javma.234.7.883. [DOI] [PubMed] [Google Scholar]
- 9.Evans A, Gakuya F, Paweska JT, Rostal M, Akoolo L, Van Vuren PJ, et al. Prevalence of antibodies against Rift Valley fever virus in Kenyan wildlife. Epidemiol Infect. 2008;136:1261–1269. doi: 10.1017/S0950268807009806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paweska JT, van Vuren PJ, Kemp A, Buss P, Bengis RG, Gakuya F, et al. Recombinant nucleocapsid-based ELISA for detection of IgG antibody to Rift Valley fever virus in African buffalo. Vet Microbiol. 2008;127:21–28. doi: 10.1016/j.vetmic.2007.07.031. [DOI] [PubMed] [Google Scholar]
- 11.Paweska JT, Mortimer E, Leman PA, Swanepoel R. An inhibition enzyme-linked immunosorbent assay for the detection of antibody to Rift Valley fever virus in humans, domestic and wild ruminants. J Virol Methods. 2005;127:10–18. doi: 10.1016/j.jviromet.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 12.Flick R, Bouloy M. Rift Valley fever virus. Curr Mol Med. 2005;5:827–834. doi: 10.2174/156652405774962263. [DOI] [PubMed] [Google Scholar]
- 13.Le May N, Gauliard N, Billecocq A, Bouloy M. The N terminus of Rift Valley fever virus nucleoprotein is essential for dimerization. J Virol. 2005;79:11974–11980. doi: 10.1128/JVI.79.18.11974-11980.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koser ML, McGettigan JP, Tan GS, Smith ME, Koprowski H, Dietzschold B, Schnell MJ. Rabies virus nucleoprotein as a carrier for foreign antigens. Proc Natl Acad Sci USA. 2004;101:9405–9410. doi: 10.1073/pnas.0403060101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mebatsion T, Koolen MJ, de Vaan LT, de Haas N, Braber M, Romer-Oberdorfer A, et al. Newcastle disease virus (NDV) marker vaccine: an immunodominant epitope on the nucleoprotein gene of NDV can be deleted or replaced by a foreign epitope. J Virol. 2002;76:10138–10146. doi: 10.1128/JVI.76.20.10138-10146.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gould EA, Higgs S. Impact of climate change and other factors on emerging arbovirus diseases. Trans R Soc Trop Med Hyg. 2009;103:109–121. doi: 10.1016/j.trstmh.2008.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Paweska JT, Jansen van Vuren P, Swanepoel R. Validation of an indirect ELISA based on a recombinant nucleocapsid protein of Rift Valley fever virus for the detection of IgG antibody in humans. J Virol Methods. 2007;146:119–124. doi: 10.1016/j.jviromet.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 18.Jansen van Vuren P, Potgieter AC, Paweska JT, van Dijk AA. Preparation and evaluation of a recombinant Rift Valley fever virus N protein for the detection of IgG and IgM antibodies in humans and animals by indirect ELISA. J Virol Methods. 2007;140:106–114. doi: 10.1016/j.jviromet.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 19.Meegan JM, Digoutte JP, Peters CJ, Shope RE. Monoclonal antibodies to identify Zinga virus as Rift Valley Fever virus. Lancet. 1983;1:641. doi: 10.1016/s0140-6736(83)91807-x. [DOI] [PubMed] [Google Scholar]
- 20.Besselaar TG, Blackburn NK, Meenehan GM. Antigenic analysis of Rift Valley fever virus isolates: monoclonal antibodies distinguish between wild-type and neurotropic virus strains. Res Virol. 1991;142:469–474. doi: 10.1016/0923-2516(91)90069-f. [DOI] [PubMed] [Google Scholar]
- 21.Besselaar TG, Blackburn NK. Topological mapping of antigenic sites on the Rift Valley fever virus envelope glycoproteins using monoclonal antibodies. Arch Virol. 1991;121:111–124. doi: 10.1007/BF01316748. [DOI] [PubMed] [Google Scholar]
- 22.Blackburn NK, Besselaar TG. A study of the effect of chemical inactivants on the epitopes of Rift Valley fever virus glycoproteins using monoclonal antibodies. J Virol Methods. 1991;33:367–374. doi: 10.1016/0166-0934(91)90036-y. [DOI] [PubMed] [Google Scholar]
- 23.Besselaar TG, Blackburn NK. The synergistic neutralization of Rift Valley fever virus by monoclonal antibodies to the envelope glycoproteins. Arch Virol. 1992;125:239–250. doi: 10.1007/BF01309641. [DOI] [PubMed] [Google Scholar]
- 24.Besselaar TG, Blackburn NK. The effect of neutralizing monoclonal antibodies on early events in Rift Valley fever virus infectivity. Res Virol. 1994;145:13–19. doi: 10.1016/s0923-2516(07)80002-1. [DOI] [PubMed] [Google Scholar]
- 25.Zaki A, Coudrier D, Yousef AI, Fakeeh M, Bouloy M, Billecocq A. Production of monoclonal antibodies against Rift Valley fever virus Application for rapid diagnosis tests (virus detection and ELISA) in human sera. J Virol Methods. 2006;131:34–40. doi: 10.1016/j.jviromet.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 26.Caplen H, Peters CJ, Bishop DH. Mutagen-directed attenuation of Rift Valley fever virus as a method for vaccine development. J Gen Virol. 1985;66:2271–2277. doi: 10.1099/0022-1317-66-10-2271. [DOI] [PubMed] [Google Scholar]
- 27.Lorenzo G, Martin-Folgar R, Rodriguez F, Brun A. Priming with DNA plasmids encoding the nucleocapsid protein and glycoprotein precursors from Rift Valley fever virus accelerates the immune responses induced by an attenuated vaccine in sheep. Vaccine. 2008;26:5255–5262. doi: 10.1016/j.vaccine.2008.07.042. [DOI] [PubMed] [Google Scholar]
- 28.Galfre G, Milstein C. Preparation of monoclonal antibodies: strategies and procedures. Methods Enzymol. 1981;73:3–46. doi: 10.1016/0076-6879(81)73054-4. [DOI] [PubMed] [Google Scholar]