Abstract
Objective
To demonstrate the capability of directly visualizing the entire ocular surface and the entire contact lens on the eye using spectral domain optical coherence tomography (SD-OCT).
Methods
A custom built, high speed and high resolution SD-OCT was developed with extended scan depth and width. The eye was imaged before and after wearing a toric soft contact lens (PureVision, Bausch & Lomb, Rochester, NY). A lubricant eye drop (Soothe, Bausch & Lomb) was instilled in the eye to enhance the image contrast on the lens. The same toric soft contact lens immersed in the contact lens solution was also imaged with a contrast enhancement medium (0.5% Intralipid).
Results
Cross-sectional OCT images of the entire ocular surface were acquired with high resolution 2048×2048 pixels. Quantitative surface height map of the ocular surface was obtained from a radial scan dataset containing 32 B-scans. With the contrast enhancement agent, the entire toric soft contact lens was clearly visualized both in vitro and on the eye. The surfaces of the lens were detected and used to generate the thickness maps of the soft contact lens.
Conclusions
SD-OCT with extended scan depth and width is a promising tool for imaging the entire ocular surface shape and soft contact lenses. This successful demonstration suggests that the extended depth SD-OCT is effective in studying ocular surface shape and its interaction with a soft contact lens. The novel method is helpful for contact lens fitting evaluation and lens design.
Keywords: OCT, contact lens
INTRODUCTION
The relationship of a soft lens with the ocular surface (lens fit) can affect wearing comfort and contact lens marketability. Ocular discomfort is the main reason for premature discontinuation of lens wear.1,2 The patients’ experience of inadequate comfort may have arisen from a variety of causes. Among them, one of the most important is inappropriate lens fit.3 Visual observation of lens centration, movement, and coverage using slit- lamp microscopy provides some quantitative details of contact lens fit determination.4
It is known that lenses composed of different materials and designs may have unique fitting characteristics that could impact the interaction between the lens and ocular surface, resulting in different levels of ocular comfort and affecting ocular health after prolonged contact lens wearing. Currently, there are no reported studies on imaging the entire lens cross-section on the eye for characterizing the contact lens’ fitting, mainly due to the lack of suitable measuring tool that could quantify the lens fitting on the entire surface. Wolffsohn and associates evaluated contact lens fit using video capturing. 4 No cross-sectional image of the entire lens on the eye could be imaged using their method.4 Apparently, OCT may be well suitable for this task.
With technological advancements in optical coherence tomography (OCT), we have demonstrated that our custom built ultra-high resolution spectral domain OCT (SD-OCT) with 3 μm axial resolution can be use to visualize the tear dynamic at the central location and around the lens edge.5 Technologic advancements also enable us to develop an OCT system with prolonged scan depth of 7.2 mm and extended wide scan width up to 20 mm. The purpose of this study was to demonstrate the capabilities of this new technology to image entire ocular surface and the contact lens both in vitro and on the eye and obtain the quantitative topography of the ocular surface and thickness of contact lens.
SUBJECTS AND METHODS
The study was approved by the research review board of the University of Miami. The subject enrolled in this study had no previously diagnosed dry eye and no dry eye symptoms or ocular surface disease. Informed consent was obtained from the subject who was treated in accordance with the tenets of the Declaration of Helsinki.
Imaging the entire contact lens on the eye requires a deep scan depth and wide scan width to cover the contact lens from the apex of the lens to the lens edges and entire ocular surface. A, high speed and high resolution SD-OCT with extended scan depth and extended scan width was custom built for this purpose. A superluminescent diode light source (SLD by Superlum) with center wavelength of 840 nm and full-width at half maximum (FWHM) bandwidths of 50 nm is used for the system. The total exposure power (1.30 mW) at the surface of the cornea is adjusted to below the safe cut-off value for long exposure to the eye according to ANSI Z136.1 (the light was focused on the anterior segment not the retina). The beam passes through an optical isolator and is split by a 50:50 fiber coupler into a reference and a sample arm. A telecentric design optical scanning probe allowing a scan width up to 20 mm was mounted on a modified slit lamp with a video camera for aiming the eye. Based on our previous OCT technology developed for anterior segment imaging, we constructed a custom spectrometer to achieve an extended depth range of 7.2mm. In the spectrometer, a CCD camera (Aviiva-SM2010 by Atmel, 2048 pixels) was used with a volume holographic diffraction grating (1800 lines/mm; Wasatch Photonics, USA) to span the fringe over 2048 sensor pixels on the camera. The camera operates at a frame rate of 24k fps (frames per second). The resolution of the SD-OCT system is axially ~6.0μm in the eye and transversally ~15μm. X-Y cross aiming was applied to align the scanning position through the iris during imaging which is critical to image the ocular surface for proper alignment. An internal fixation target controlled by a computer was displayed on a miniature LCD monitor.
One eye of a healthy subject (left eye) was imaged before and after wearing a toric soft contact lens (PureVision, Bausch & Lomb, Rochester, NY) with an 8.7mm base curve, −3.00 D sph/−1.75 D cyl and a diameter of 14.0mm. To highlight the contrast of the lens on the eye, a lubricant eye drop (Soothe, Bausch & Lomb, Rochester, NY) was instilled into the eye. In order to image the contact lens in vitro, the lens was immersed in contact lens solution which contained 0.5% Intralipid to enhance the contrast of the lens image.
In order to obtain quantitative information about the topography of ocular surface and the thickness of contact lens, the scanning protocol of 32 radial B-scans with 2048 A-scans was chosen for this purpose. To perform the quantitative analysis, the boundaries of the contact lens and anterior surface of cornea were segmented out from all cross-sectional 3-D images from the data set based on the signal peaks at the interfaces. The image distortion due to refraction and transition of the group index at the air-contact lens interface was removed using a custom de-warping algorithm.6 From the de-warped images, the thickness of contact lens was measured as the distance between the anterior and posterior lens surfaces along lines perpendicular to the anterior surface at the point of measurement. The contact lens thickness map and the topographic map of the ocular surface were calculated and smoothed by interpolation.
RESULTS
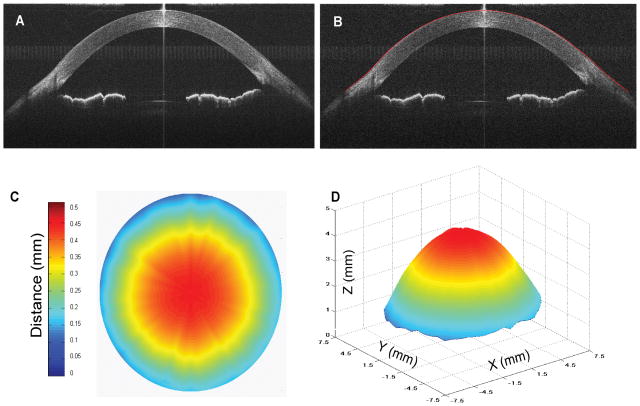
One of the most important features of the system is its capability to measure the entire ocular surface together with the iris and anterior surface of the crystalline lens (Fig. 1A). The cross-sectional image consists of 2048×2048 pixels. The image quality is sufficient to detect the entire ocular surface shape. The structural elements including the cornea, limbus, iris, the lens and the ciliary body can be clearly visualized. The boundary of ocular surface (Fig. 1B) was well detected from the cross-sectional image by our algorithm. The ocular surface height map was generated by post-processing the 3-D image data (Fig. 1C and D). Fig. 1A was obtained with 2-D horizontal scan mode and with the entire scan width of 20 mm. Due to eyelid and eyelashes partially covering the vertical meridian, 15 mm diameter was chosen for the height map.
Figure 1. OCT image of entire ocular surface and its 3-D topography obtained by SD-OCT.
A: Cross-sectional image of the entire ocular surface, anterior chamber and anterior surface of crystalline lens in a normal eye. The image was acquired in the horizontal meridian with 20 mm scan width. B: The boundary of ocular surface (red curve) segmented from the cross-sectional image. C: Height map of ocular surface with a diameter of 15 mm and D: its 3-D topography generated from 32 B-scan images with 2048 A-scans each.
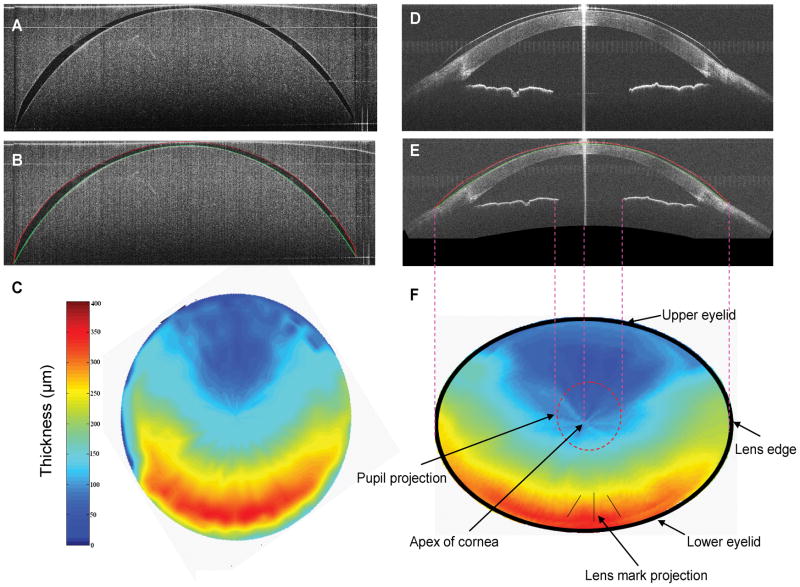
Another feature of the system is to image the entire soft contact lens in vitro and on the eye. Fig. 2A shows the toric soft contact lens immersed in contact lens solution. The contrast of the contact lens image is enhanced by the 0.5% Intralipid allowing the shape of the entire contact to be clearly visualized. The thickness map of the contact lens in vitro (Fig. 2C) was generated by segmenting the boundaries of the anterior and posterior surfaces (Fig. 2B) from 32 B-scans images. Due to the similar refractive indices of the enhancement medium and the contact lens, the boundaries of contact lens surfaces (Fig. 2B) were segmented from the original SD-OCT image (Fig. 2A). The same eye fitted with the toric soft contact lens was imaged with a horizontal scan (Fig. 2D). The scan width was set to 20 mm. The lens on the eye was also enhanced by the lubricant eye drop. The shape of the entire contact lens and the interaction between the lens and ocular surface were all clearly imaged. The thickness map (Fig. 2F) was generated from segmented lens surfaces of 32 B-scans images after correcting the distortion due to the refraction (Fig. 2E).
Figure 2. Imaging entire contact lens in vitro and on the eye.
A: Cross-sectional OCT image of a toric soft contact lens immersed in contact lens solution. The contact lens image is enhanced by 0.5% Intralipid in the solution. The scan width of 15.6 mm was applied. B: The segmented surfaces of the contact lens from Fig. 2A. Red curve: anterior surface of lens. Green curve: posterior surface of lens. C: Thickness map of the soft toric contact lens in vitro. D: Cross-sectional OCT image of a toric soft contact lens on a healthy eye acquired in horizontal meridian. The lens image was enhanced by a lubricant eye drop. A scan width of 20 mm was applied for 3-D radial scan. E: The segmented surfaces of the contact lens from Fig. 2D after correcting the distortion due to the refraction. Red curve: anterior surface of lens. Green curve: posterior surface of lens. F: Thickness map of lens on the eye. The map is similar to that of lens in vitro.
DISCUSSION
OCT is a rapid developing technique for imaging the anterior segment of the eye. Many studies in this field have been reported using commercial and custom-built OCT instruments.7–10 OCT may also be a useful tool in the evaluation of contact lens fitting. Using high speed spectral domain SD-OCT, contact lenses on the eye have been studied.11,12 Recently, we demonstrated the capability of ultra-high resolution SD-OCT for imaging tears around contact lenses and the interactions between the ocular surface and contact lens edges.5 However, there are no reports of OCT imaging of entire contact lenses on the eye due to the difficulty of extending the imaging depth and width to cover the entire contact lens and anterior chamber.
The detailed information of ocular surface shape is very useful in the diagnosis of corneal ectatic disorders such as keratoconus,13 in rigid and soft contact lens fitting,14,15 and in the screening of refractive surgery candidates.16 However, most studies of ocular surface shape have only investigated the central 6 mm of the cornea. Although data from the central cornea are obviously the most important for vision, this represents only approximately one fourth of the cornea’s total surface area. Information from the peripheral cornea is particularly important in the design and fitting evaluation of contact lenses. For a soft contact lens, the range of diameters is between 14 mm to 15 mm, which means its edges overlap the limbus. Though the computer-assisted videokeratoscopes can measure much larger area larger than that of the traditional keratometer,17 topography is obtained from the combined central and peripheral corneal data. In this study, the OCT instrument with extended scan depth and width shows its capability of imaging the entire ocular surface up to 20 mm.
This new technique also shows its capability to image the entire soft contact lens in vitro and on the eye. To the best of our knowledge, this is the first report of using SD-OCT for directly imaging the entire contact lens in 3D. With high speed and high resolution of the current SD-OCT instrument, we successfully obtained the 3-D image data sets consisting 32 B-scans with 2048 A-scans each and generated a thickness map of the contact lens both in vitro and on the eye.. This technique has the capability of precise evaluation of the lens centration and coverage which are especially important for determining contact lens fitting. It also has the resolution to image and measure conjunctival compression from the lens edge. In the future, the shape of the ocular surface will be characterized in a large normal group and its interaction with soft contact lens will be studied to improve the lens design and contact fitting. Future research using this technique to measure the ocular surface shape in subjects undergoing corneal refractive surgery or orthokeratology may also improve our understanding of the changes to the peripheral cornea accompanying these procedures.
In summary, this experiment has demonstrated the capability of imaging the entire ocular surface up to 20 mm, and imaging a soft contact lens in vitro and on the eye. Developments of both hardware and software are in progress that will refine and extend the measurement capability of the ocular surface shape and its interaction with the soft contact lens. This novel method may open a new field in studying contact lens design and contact lens fitting.
Acknowledgments
Grant/financial support: This study was supported by research grants from Bausch & Lomb, Allergan, NIH Center Grant P30 EY014801 and Research to Prevent Blindness (RPB).
Footnotes
Commercial relationship: Jianhua Wang is a recipient of the research grants.
Financial Disclosures: The authors have no proprietary interest in any materials or methods described within this article.
References
- 1.Pritchard N, Fonn D, Brazeau D. Discontinuation of contact lens wear: a survey. Int Contact Lens Clin. 1999;26:157–162. doi: 10.1016/s0892-8967(01)00040-2. [DOI] [PubMed] [Google Scholar]
- 2.Pritchard N, Fonn D, Weed K. Ocular and subjective responses to frequent replacement of daily wear soft contact lenses. CLAO J. 1996;22:53–59. [PubMed] [Google Scholar]
- 3.Young G. Why one million contact lens wearers dropped out. Cont Lens Anterior Eye. 2004;27:83–85. doi: 10.1016/j.clae.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 4.Wolffsohn JS, Hunt OA, Basra AK. Simplified recording of soft contact lens fit. Cont Lens Anterior Eye. 2009;32:37–42. doi: 10.1016/j.clae.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 5.Wang J, Jiao S, Ruggeri M, Shousha MA, Chen Q. In situ visualization of tears on contact lens using ultra high resolution optical coherence tomography. Eye Contact Lens. 2009;35:44–49. doi: 10.1097/ICL.0b013e31819579f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Westphal V, Rollins A, Radhakrishnan S, Izatt J. Correction of geometric and refractive image distortions in optical coherence tomography applying Fermat’s principle. Opt Express. 2002;10:397–404. doi: 10.1364/oe.10.000397. [DOI] [PubMed] [Google Scholar]
- 7.Wang J, Aquavella J, Palakuru J, Chung S. Repeated measurements of dynamic tear distribution on the ocular surface after instillation of artificial tears. Invest Ophthalmol Vis Sci. 2006;47:3325–3329. doi: 10.1167/iovs.06-0055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li Y, Shekhar R, Huang D. Corneal pachymetry mapping with high-speed optical coherence tomography. Ophthalmology. 2006;113:792–799. doi: 10.1016/j.ophtha.2006.01.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mohamed S, Lee GK, Rao SK, Wong AL, Cheng AC, Li EY, Chi SC, Lam DS. Repeatability and reproducibility of pachymetric mapping with Visante anterior segment-optical coherence tomography. Invest Ophthalmol Vis Sci. 2007;48:5499–5504. doi: 10.1167/iovs.07-0591. [DOI] [PubMed] [Google Scholar]
- 10.Gora M, Karnowski K, Szkulmowski M, Kaluzny BJ, Huber R, Kowalczyk A, Wojtkowski M. Ultra high-speed swept source OCT imaging of the anterior segment of human eye at 200 kHz with adjustable imaging range. Opt Express. 2009;17:14880–14894. doi: 10.1364/oe.17.014880. [DOI] [PubMed] [Google Scholar]
- 11.Kaluzny BJ, Fojt W, Szkulmowska A, Bajraszewski T, Wojtkowski M, Kowalczyk A. Spectral optical coherence tomography in video-rate and 3D imaging of contact lens wear. Optom Vis Sci. 2007;84:1104–1109. doi: 10.1097/OPX.0b013e31815b9e0e. [DOI] [PubMed] [Google Scholar]
- 12.Kaluzny BJ, Kaluzny JJ, Szkulmowska A, Gorczynska I, Szkulmowski M, Bajraszewski T, Targowski P, Kowalczyk A. Spectral optical coherence tomography: a new imaging technique in contact lens practice. Ophthalmic Physiol Opt. 2006;26:127–132. doi: 10.1111/j.1475-1313.2006.00371.x. [DOI] [PubMed] [Google Scholar]
- 13.Schwiegerling J, Greivenkamp JE. Keratoconus detection based on videokeratoscopic height data. Optom Vis Sci. 1996;73:721–728. doi: 10.1097/00006324-199612000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Reddy T, Szczotka LB, Roberts C. Peripheral corneal contour measured by topography influences soft toric contact lens fitting success. CLAO J. 2000;26:180–185. [PubMed] [Google Scholar]
- 15.Szczotka LB, Roberts C, Herderick EE, Mahmoud A. Quantitative descriptors of corneal topography that influence soft toric contact lens fitting. Cornea. 2002;21:249–255. doi: 10.1097/00003226-200204000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Ambrosio R, Jr, Klyce SD, Wilson SE. Corneal topographic and pachymetric screening of keratorefractive patients. J Refract Surg. 2003;19:24–29. doi: 10.3928/1081-597X-20030101-05. [DOI] [PubMed] [Google Scholar]
- 17.Read SA, Collins MJ, Carney LG, Franklin RJ. The topography of the central and peripheral cornea. Invest Ophthalmol Vis Sci. 2006;47:1404–1415. doi: 10.1167/iovs.05-1181. [DOI] [PubMed] [Google Scholar]