Abstract
A 62-year-old patient presented with dizzy spells after her dual chamber pacemaker (Medtronic Enrhythm P1501DR), implanted for complete AV block, had been reprogrammed to deliver antitachycardia therapy (ATP) for paroxysmal atrial tachycardia. Her symptoms were caused by inhibition of ventricular backup pacing during ATP, leading to ventricular asystoles. Inhibition was the result of premature ventricular beats occurring prior to ATP: when ventricular backup pacing is left in the default setting, this pacemaker withholds backup pacing if any of the four preceding events is a sensed event. This case illustrates the possibly hazardous effects of default pacemaker settings, especially in pacemaker-dependent patients. (Neth Heart J 2010;18:323–6.)
Keywords: Cardiac Pacing, Arrhythmias, Pacemaker, Ventricular Function
When implanting and programming a pacemaker, the default settings of the specific pacemaker type should be known to the cardiologist and pacemaker technician, and possible risks of these settings in an individual patient should be considered. We present a case that illustrates how unawareness of the exact default settings of a pacemaker can be hazardous to a patient.
Case
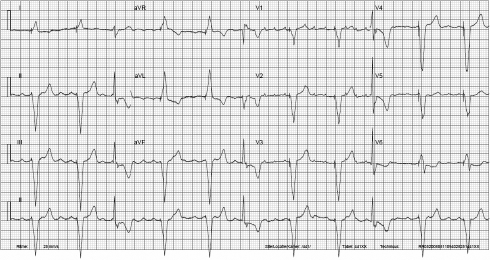
A 62-year-old female patient with a medical history of hypertension and paroxysmal atrial fibrillation presented to the emergency department with haemodynamic instability due to viral myocarditis complicated by complete atrioventricular block. She was successfully resuscitated and a temporary transvenous ventricular pacing electrode was inserted. After the patient recuperated, a Medtronic Enrhythm P1501DR dual chamber pacemaker was implanted. During follow-up, pacemaker interrogation showed that the patient remained completely pacemaker-dependent. Frequent paroxysms of atrial tachycardia were recorded by the pacemaker, with a good response to oral amiodarone. Unfortunately, amiodarone had to be discontinued because of side effects. At the next check-up several months later, pacemaker diagnostics revealed long episodes of atrial tachycardia, leading to frequent mode switches of the pacemaker to DDI mode. A sustained atrial tachycardia was terminated at the outpatient clinic by using the pacemaker’s manual antitachycardia pacing function. AT/AF detection and therapy settings were programmed to ‘On’, so that termination of new episodes of atrial tachycardia by antitachycardia pacing (ATP) could be attempted. The pacemaker was programmed to classify a supraventricular rate of >133 beats per minute as AT/AF. A ramp of 20 atrial stimuli was programmed to be delivered one minute after detection of atrial tachycardia. This relatively long ramp sequence (the nominal value is six stimuli per ramp sequence) was chosen because the sustained atrial tachycardia mentioned before had not responded to ramp sequences of less than 20 stimuli. The initial ramp stimulus was to be delivered after an interval of 94% of the detected A-A interval, with an interval decrement of 10 msec for subsequent stimuli and a minimum stimulus interval of 150 msec. If necessary, a second ramp with equal parameters was to be delivered. Because the patient was completely pacemaker-dependent, ventricular backup pacing in VVI mode was left in the default setting ‘On (Auto Enable)’ with a lower rate of 70 beats/min, to preserve ventricular stimulation during ATP delivery (figure 1).
Figure 1.
Programmed parameters for supraventricular tachycardia detection and therapy.
Two weeks later, the patient presented to the outpatient clinic complaining of dizzy spells. Pacemaker interrogation showed that the pacemaker was functioning normally. No ventricular tachycardia had been registered in the past month, but a lot of single premature ventricular beats (PVBs) had been recorded, with an incidence that was evidently higher than before.
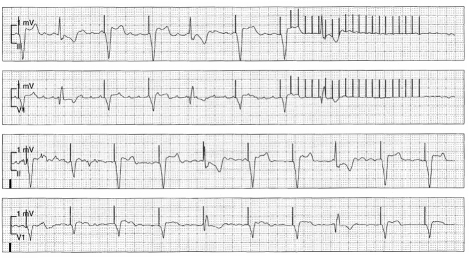
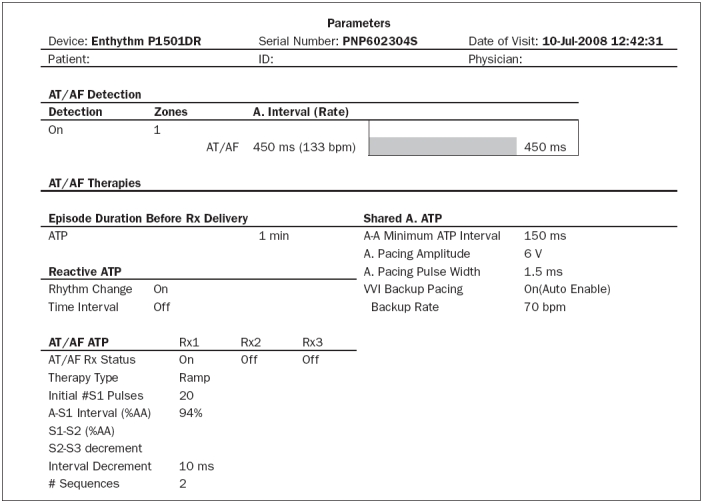
Echocardiography showed normal dimensions and a slightly impaired LV function. Twenty-four hour ambulatory electrocardiography revealed normal sinus rhythm with sequential ventricular pacing, and frequent single ventricular premature beats. Later that month the patient was admitted to the hospital because of persisting dizzy spells. Electrocardiography on admission showed atrial tachycardia with a rate of 250 beats/min, with ventricular (DDI) pacing at a rate of 70 beats/min. Multiple monomorphic PVBs with a relatively narrow QRS duration (probably originating near the His bundle) were recorded on the same ECG registration (figure 2). Still, no clear cause of the dizzy spells could be determined and the patient was observed with telemetry. Not much later, the cause of her dizzy spells was clarified: ventricular asystoles occurred during ATP for atrial tachycardia (figure 3). Careful reading of the pacemaker reference manual explained this phenomenon: The default setting for ventricular backup pacing during ATP in this specific type of pacemaker is ‘On (Auto Enable)’, meaning that the pacemaker does not automatically start ventricular backup pacing when AF/AT therapy is delivered: It withholds backup pacing if any of the four preceding ventricular events is not a paced event.1 Because of a PVB (sensed ventricular event) occurring prior to ATP delivery in this patient, ventricular backup pacing was withheld during ATP, leading to a ventricular asystole of 3.4 seconds. This particular asystole was shortened by 840 msec due to another PVB occurring during ATP delivery (had this PVB not occurred, the pause would have lasted about 4.3 seconds). The problem was easily solved by programming ventricular backup pacing to ‘On (Always)’. In this setting, backup pacing is delivered during every ATP therapy, regardless of preceding ventricular events.
Figure 2.
Electrocardiogram on admission for dizzy spells.
Figure 3.
Telemetry strip recorded during dizzy spell: asystole during ATP.
Discussion
This case illustrates the deleterious effects a default pacemaker setting can have when the cardiologist or pacemaker technician is unaware of the exact details of this nominal (factory) setting. Inhibition of ventricular pacing in a pacemaker-dependent patient can result in dizziness, syncope or even more catastrophic events. Possible other causes of undesirable inhibition of ventricular output are ventricular sensing of an external signal such as muscular activity, atrioventricular crosstalk and even ventricular oversensing of far-field atrial activity.2
In this case, the symptoms were not caused by inhibition of normal ventricular output, but by inhibition of ventricular backup pacing during ATP delivery. This was the result of the default setting for ventricular backup pacing: ‘On (Auto-Enable)’. This setting is normally advised by the manufacturer and preferred over the (non-default) ‘On (Always)’ setting, because in patients with an underlying ventricular rhythm VOO backup pacing can cause competitive ventricular pacing due to a post-atrial blanking period of 30 msec occurring after every ATP stimulus. This algorithm was initially developed for the Medtronic Gem ICD family: since most ICD patients are not pacemaker-dependent, competitive ventricular pacing can be more of a concern in this patient group. But when a patient is fully dependent on ventricular pacing, one should realise that the hazard of possible inhibition of ventricular backup pacing during ATP outweighs the risk of competitive ventricular pacing during ATP with ventricular backup pacing. In this patient, backup pacing was inhibited because one of the four preceding ventricular events was a PVB. The maximum duration of an asystole in this patient could have been much longer in case of ATP for a slower atrial tachycardia: if no PVBs occur during successful ATP for an atrial tachycardia with a rate of 133 beats/min, maximum asystole duration would be 500 msec (the synchronisation interval before ATP delivery) + 6600 msec (the sum of 20 ATP stimulus intervals of 0.94 x 451 msec with an interval decrement of 10 msec) followed by a post-ATP synchronisation interval equal to the lower rate interval (1000 msec), resulting in a ventricular standstill of 8.1 seconds!
This case illustrates that careful reading of the pacemaker manual and full knowledge of the implications of default settings is mandatory when implanting and programming a pacemaker. A default setting is not necessarily the optimal setting for an individual patient and can even be dangerous, especially in a pacemaker-dependent patient. Similar problems due to unawareness of default settings leading to unwanted inhibition of ventricular backup pacing during ATP have previously been described in an ICD/CRT patient after AV nodal ablation, and in a patient who developed AV block after implantation of a DDDR pacemaker for sick sinus syndrome.3,4 We feel that the pacemaker manual should recommend ventricular backup pacing to be programmed ‘On (Always)’ in patients who are (or may become) pacemaker-dependent.
References
- 1.Medtronic EnrhythmTM P1501DR Reference Manual. [Google Scholar]
- 2.Ruiter JH, Barrett MJ, Weteling L, Jansen R. Inhibition of a dual chamber pacemaker by oversensing of far-field atrial depolarisation in a patient after His-bundle ablation. Neth Heart J. 2004;12;543-6. [PMC free article] [PubMed] [Google Scholar]
- 3.Herweg B, Barold SS. Ventricular asystole during atrial antitachycardia pacing by implanted cardioverter-defibrillator. Pacing Clin Electrophysiol. 2005;28;432-3. [DOI] [PubMed] [Google Scholar]
- 4.Navarrete A. Failure to pace: pacemaker malfunction? J Cardiovasc Electrophysiol. 2008;19;100-1. [DOI] [PubMed] [Google Scholar]