Abstract
Context: American health policy is increasingly relying on consumerism to improve its performance. This article examines a neglected aspect of medical consumerism: the extent to which consumers respond to problems with their health plans.
Methods: Using a telephone survey of five thousand consumers conducted in 2002, this article assesses how frequently consumers voice formal grievances or exit from their health plan in response to problems of differing severity. This article also examines the potential impact of this responsiveness on both individuals and the market. In addition, using cross-group comparisons of means and regressions, it looks at how the responses of “empowered” consumers compared with those who are “less empowered.”
Findings: The vast majority of consumers do not formally voice their complaints or exit health plans, even in response to problems with significant consequences. “Empowered” consumers are only minimally more likely to formally voice and no more likely to leave their plan. Moreover, given the greater prevalence of trivial problems, consumers are much more likely to complain or leave their plans because of problems that are not severe. Greater empowerment does not alleviate this.
Conclusions: While much of the attention on consumerism has focused on prospective choice, understanding how consumers respond to problems is equally, if not more, important. Relying on consumers’ responses as a means to protect individual consumers or influence the market for health plans is unlikely to be successful in its current form.
Keywords: Consumerism, responsive consumerism, health plans, voice, exit, markets
Despite some skepticism about the benefits of market-based medical care (Nichols et al. 2004), the United States’ current health policy continues to rely on individual consumers to improve the performance of its health system. This is evident in the recent design of Medicare Part D (Hanoch and Rice 2006), the continuing emphasis on plan choice under Medicaid (NASHP 2001), the emphasis on public reporting of quality data (Marshall et al. 2003), and the use of consumer-driven health plans and health savings accounts in employer-sponsored insurance (Gabel, Lo Sasso, and Rice 2002; Havlin et al. 2003). Recently proposed policies from the current Democratic-controlled Congress and the Obama administration continue to rely on consumer empowerment as an integral part of their health reform efforts. Public policies that promote consumer engagement are expected to improve performance by (1) providing consumers with timely performance measures so that they can select the health plans and providers that best match their preferences and (2) helping consumers recognize and take appropriate action when products or services are substandard.
The first aspect of consumerism, which we term prospective choice, has received most of the attention of researchers and policymakers. As a result, the criteria for adequate consumer involvement are reasonably well defined: consumers must have timely access to reliable measures of performance, be able to use these measures to identify desirable alternatives, and translate their assessments into choices (Hibbard et al. 2002; Hibbard, Stockard, and Tusler 2005). A substantial body of research has documented the extent to which various groups of consumers meet these criteria (Dranove and Sfekas 2008; Hibbard et al. 1998; Lake, Kvam, and Gold 2005; Lubalin and Harris-Kojetin 1999; Neuman and Langwell 1999; Scanlon et al. 2002). State and federal governments continue to adopt new policies designed to enhance this aspect of consumer empowerment, by creating new report cards for health plans, hospitals, physicians, and nursing homes; incentives for employers to offer more options to their workers; and incentives for consumers to make cost-effective choices (Stevenson 2006; Thorpe 2005).
By contrast, consumers’ reactions to shortfalls in their own care, which we term responsive consumerism, have received relatively little attention from either researchers or policymakers. As a result, expectations for effective empowerment are ill defined. Little is known about the extent to which consumers recognize problems when they occur or how they respond to them.
The conventional emphasis on prospective choice is problematic because it neglects key ways in which consumers can draw on their own experiences to improve the quality of their care or insurance coverage. We develop this claim in the next section of this article, after which we (1) describe the distinctive features of responsive consumerism and two sets of expectations (consumer protection and market signaling) for effective consumer responses to problems and (2) propose criteria to determine whether consumer behaviors meet these expectations.
Using a national survey of the health care experiences of five thousand Americans, we examined responsive consumerism with respect to health plans in expressing grievances (voicing) or switching to a competing plan (exiting) in the aftermath of perceived problems. We found that consumers’ current responses neither safeguard individual enrollees (consumer protection) nor reliably signal the most problematic plan practices (market signaling). We then modeled the responses of two more empowered subsets of consumers to determine whether consumers’ empowerment initiatives might improve their responses. Our findings suggest that these would be more effective for enhancing voice than for exit but still would have only a limited impact on either response. From these findings, we made some policy-relevant conclusions about consumers’ responses to problematic experiences involving health plans.
Forms, Norms, and Expectations for Responsive Medical Consumerism
In this section we explain our rationale for focusing on responsive consumerism and identify our criteria for assessing consumers’ responses to problems with their health plans.
Why Prospective Choice Is Not Sufficient to Improve Quality for Serious Illnesses
Strategies for consumer involvement cannot rely solely, or even primarily, on consumers’ selecting the best-quality health plans before their enrollment, for three reasons. Together, they suggest that at best, prospective choice among plans would have only a modest influence on quality of care and even less influence on the care of the most serious health problems.
First, prospective measures of plan performance present information about quality of care at a time when it has little salience to most consumers; that is, many of them have not been seriously ill or in need of medical care. Moreover, even consumers who have this information often do not use it (Kaiser Family Foundation and Agency for Healthcare Research and Quality 2004, 2006), and such information generally has only little influence on the choice of a plan (Abraham et al. 2006; Beaulieu 2002; Chernew and Scanlon 1998; Scanlon et al. 2002; Uhrig and Short 2002/2003; Wedig and Tai-Seale 2002).
Second, even if more consumers paid close attention to most quality ratings, they would learn little about the plans’ ability to care for the most serious illnesses. Report card performance measures, particularly those based on consumers’ rating of their own experiences, disproportionately report on the much more common minor illness or routine care, as opposed to more serious illnesses. Condition-specific scores such as HEDIS (Healthcare Effectiveness Data and Information Set) measures are more relevant to serious conditions, but unless consumers have those particular conditions, the HEDIS measures will seem largely irrelevant to them.
The third limitation on prospective choice stems from consumers’ limited ability to process information. Most people have a hard time evaluating multiple dimensions of performance across health plans, and these cognitive constraints become even more pronounced as more plans are considered (Hanoch and Rice 2006). Unable to fully process information about their choices, most consumers fall back on simplified decision heuristics that emphasize performance measures unrelated to quality of care, such as cost-sharing provisions, provider panels, and scope of treatment coverage (Hibbard et al. 1997; Scanlon et al. 2002; Tumlinson et al. 1997). Given these difficulties, it is clear that prospectively choosing a health plan will not be based on quality of care in the manner that analysts generally consider most meaningful. Next we consider the decision processes that consumers use when their health care experiences fall short of their expectations, which should have a more direct relationship to the quality of care that they can subsequently expect.
Responsive Consumerism and Its Potential Influence on Quality
Responsive consumerism refers to consumers’ actions after experiencing a problem with their health plan. This form of consumerism differs from prospective choice in the actions that consumers take, the influence these actions might have on the health plan's performance, and the standards for assessing adequate consumer engagement.
Distinctive Consumer Behaviors
Responsive consumerism also involves choice. Consumers who perceive a shortfall in quality or service must decide how best to remedy the problem and/or reduce the risk of its recurrence. They can “exit,” or switch, to another plan that they believe can better meet their needs or “voice” their concerns by expressing their dissatisfaction to the plan's administrators to encourage the plan to change its practices (Annas 1997; Hirschman 1970, 1980; Rodwin 2001). These complaints can take a variety of forms, including informal interactions with representatives of the plan, formal grievances to plans and state agencies, and engaging third parties, such as family members, clinicians, or employers who might act as advocates for the aggrieved enrollee (Schlesinger, Mitchell, and Elbel 2002).
Although prospective choice has a more powerful influence on current health policy, particularly at the federal level, recent state efforts to pursue market-oriented health care reforms embody both voice and exit. These efforts include the required reporting of formal complaint and disenrollment rates to consumers at the state (private insurance and Medicaid) (Tapay, Feder, and Dallek 1998) and federal (Medicare) levels, although we know relatively little about how such requirements might affect either voice or exit as forms of responsive consumerism. Past research does show that voice is a more common response than exit for consumers who have had problems with their health plans. That is, aggrieved enrollees are eight to ten times more likely to contact a plan in response to a problem than to switch plans, and they are two to three times more likely to file a formal grievance or complaint than to switch plans (Schlesinger, Mitchell, and Elbel 2002).
Influence on Plan Performance
Prospective choice means matching a health plan's performance to individual preferences. Consumers are effectively engaged when they can identify those performance differences that are relevant to their perceived needs or health-related concerns and are able to select the plans that match those preferences. If prospective consumerism meets its proponents’ expectations, as health plans compete they can be expected to alter their medical coverage and administrative practices to better match consumers’ preferences and attract new enrollees.
Responsive consumerism is expected to improve plan performance and enhance enrollees’ well-being in quite different ways. We identify two such mechanisms in the literature, each with its own expected benefits; these two are often combined or obscured in the current policy discourse. Proponents of the “consumer protection” paradigm suggest that the foremost goal of consumer engagement is safeguarding the well-being of individual enrollees. This requires that each consumer be able to seek suitable recourse (through either exit or voice) when he or she has been treated inappropriately (Meier 1987; Miller 1998; Tapay, Feder, and Dallek 1998; Webb 1995).
Many proponents of medical markets hold quite different expectations for consumer responsiveness, which we label market signaling. Viewed from this perspective, consumers are adequately protected if at least some of them respond to problematic plan practices by either filing a grievance or switching their plan. By so doing, poorly performing plans are “marked” by the actions of these aggrieved enrollees, allowing other consumers, purchasers, and the firms themselves to respond to these “red flags.”
Not surprisingly, proponents of the market signaling notion of responsive consumerism tend to be more sanguine about the prospects for medical markets than are those who endorse the consumer protection paradigm. With market signaling, actions by a modest number of consumers might suffice if their actions (switching plans or filing grievances) were reliable markers for poorly functioning health plans. Other consumers, even if less well informed, could benefit from the actions of these active consumers, who effectively “police” the market.
Criteria for Assessing Successful Consumerism
Assessments of prospective choice have measured consumers’ ability to foresee their future health needs (Klinkman 1991; Robinson and Gardner 1996), to understand ratings on report cards (Hibbard et al. 1998; Vaiana and McGlynn 2002), and to make choices based on these performance ratings (Beaulieu 2002; Scanlon et al. 2002; Uhrig and Short 2002/2003). Assessing the effectiveness of responsive consumerism requires a different set of standards.
Viewed from the consumer protection paradigm, a reasonable threshold for consumer engagement is that most of the consumers who have serious problems take action to remedy the problem or to reduce the risk of its being repeated. Many scholars would also hold essential, for the sake of equity, that the probability of taking action be distributed reasonably evenly throughout the population. This is so certain vulnerable groups are not “trapped” in bad plans by a low propensity to respond to problematic experiences. If consumers neglect both exit and voice, they will be unable to safeguard their own well-being.
By contrast, the market signaling paradigm indicates that consumers’ involvement is adequate if either exit or voice signals which plans have elevated levels of serious problems. To be an effective signal, consumers’ responses to serious problems must not be “adulterated” by their responses to more trivial concerns. That is, if many consumers complain about minor annoyances or switch health plans whenever they are inconvenienced by paperwork, plans that cause more serious harms may prove difficult to detect.
Readers who are familiar with diagnostic testing for medical conditions will recognize a rough analogy between these two standards and the criteria conventionally used to evaluate diagnostic tests.1 The consumer protection paradigm is analogous to the “sensitivity” of a diagnostic test, that is, its ability to indicate reliably when a particular medical condition exists, by generating low rates of “false negatives.” In contrast, the market signaling paradigm corresponds to the specificity of a diagnostic test—the propensity for either disenrollment or grievances to signal a problem that is truly serious, rather than a “false positive” involving only a minor annoyance or irritation.
We now apply these criteria to provide the first examination using nationally representative data on the prevailing levels of responsive consumerism in the American health care system. We focus on those consumers who could arguably be labeled as the most empowered—those who are best able to respond adequately when they have a problem. These consumers become our standard for assessing the potential of future efforts to enhance responsive consumer empowerment in medical care.
Analytic Methods
To assess the state of responsive consumerism, we used a national survey of Americans’ health care experiences to determine the prevalence of consumer behaviors (voice and exit) in response to problems blamed on the health plan, identifying subsets of “empowered” consumers to determine how different forms of empowerment can enhance responsiveness.
Data for Measuring Consumer Experiences and Responsiveness
We used a telephone survey, fielded between June 26 and September 20, 2002, which assessed Americans’ experiences with health care. Although the survey was designed primarily to study other aspects of health system performance (Schlesinger, Mitchell, and Gray 2004a, 2004b), it contains detailed questions about problems with health care, consumers’ assessment of those problems, and their responses (if any). We interviewed five thousand people for an average of thirty minutes. The response rate on the survey was 49.5 percent (calculated by the AAPOR method). Because the survey was designed to assess enrollees’ interactions with their health plans, we surveyed only respondents enrolled in some form of health plan (as a result, we excluded 18.7 percent of the potential respondents and interviewed Medicare and Medicaid enrollees only if their benefits were administered through a managed care plan). The survey oversampled people with chronic and serious physical illnesses to identify Americans most likely to interact with their health care providers and health plans. No incentives were offered for the respondents’ participation, and the survey completion rates were quite high (98.3 percent).
Identifying Problems Related to Respondents' Health Plan
Our analysis examined respondents who reported having at least one of fifteen listed negative events in the last year.2 Slightly more than half of all respondents reported at least one such problem, and those who reported one problem typically reported several (on average, 3.5 of the 15 problems probed in the survey). The frequency with which these problems were reported is presented in the two left-hand columns in table 1 for (1) all respondents and (2) those respondents who reported at least one problem.
TABLE 1.
Prevalence and Impact of Problems with Health Plans and Health Care
| Impact of Problem |
||||||
|---|---|---|---|---|---|---|
| Prevalence of Problems |
(Percentage of Those Reporting at Least One Problem) |
|||||
| Nature of Problem | Among All Respondents | Among Respondents with at Least One Problem | Focal Problema | Blamed in Part on Health Plan | Caused Health Decline | Caused Costs >$500 |
| Limited Access | ||||||
| Unable to get needed care | 10.1 | 17.9 | 17.5 | 12.5 | 5.8 | 3.6 |
| Unable to see specialist(s) | 10.9 | 19.2 | 8.0 | 5.5 | 1.2 | 0.8 |
| Unable to get specific medication | 11.5 | 20.3 | 10.8 | 8.4 | 1.6 | 0.9 |
| 36.3 | 26.4 | 8.6 | 5.3 | |||
| Quality Shortfalls | ||||||
| Delays getting appointments when ill | 15.0 | 26.5 | 9.5 | 4.0 | 1.3 | 0.2 |
| Delays getting referrals to specialist(s) | 10.3 | 18.2 | 2.4 | 1.2 | 0.2 | 0 |
| Experienced serious quality problem | 8.3 | 14.6 | 6.9 | 3.4 | 1.4 | 0.9 |
| Disagreement about treatment | 8.9 | 15.9 | 6.1 | 2.6 | 0.3 | 0.3 |
| Treated with disrespect | 12.1 | 21.4 | 0 | 0 | 0 | 0 |
| Difficult getting answers to medical care | 13.0 | 23.0 | 1.2 | 0.8 | 0.07 | 0.1 |
| Health unexpectedly worsened | 11.3 | 20.1 | 2.8 | 0.2 | 0.04 | 0.5 |
| 28.9 | 12.2 | 3.3 | 2 | |||
| Cost Concerns | ||||||
| Told insurance won't cover treatment | 21.7 | 38.5 | 17.5 | 14.6 | 0.7 | 3.9 |
| Asked to pay more than can afford | 13.7 | 24.3 | 4.4 | 3.6 | 0.2 | 0 |
| Misunderstandings about coverage | 14.9 | 26.4 | 3.8 | 3.0 | 0.1 | 0.3 |
| Difficulty getting answers about insurance | 13.9 | 24.7 | 2.2 | 1.9 | 0 | 0.3 |
| Issues with paperwork, billing, payment | 23.0 | 40.7 | 7.1 | 5.2 | 0.1 | 0.2 |
| 35.0 | 28.3 | 1.1 | 4.7 | |||
| n = 5,000 | n = 2,805 | |||||
| Sample with at Least One Problem | 100.2 | 66.9 | 13.0 | 12.0 | ||
Note:
For individuals with more than one problem, the focal problem was selected to be the one that the average consumer judged to be the most consequential (as reported on a prior survey).
To make these problems easier to understand, we placed them in three groups identified through an exploratory factor analysis: (1) (three) problems related to access barriers, (2) (seven) problems related to quality of care, and (3) (five) problems related to medical costs or the ways in which insurance benefits are administered. Several problems overlap these categories (in the sense of loading on multiple factors), including all three problems categorized as access barriers (those involving clinical services correlated with quality problems and those related to drug coverage correlated with cost problems), disagreements regarding treatment (which had a secondary correlation with cost concerns), and limits on coverage (which had a strong secondary loading on the factor connected to access barriers). Coverage and billing problems clearly were the most common, but problems getting answers to questions regarding both care and coverage as well as access issues, considered in the aggregate, also were quite prevalent.
To explore in more detail how consumers responded to these problems, we analyzed one problem for each person. For those respondents reporting more than one problem, we selected the problem identified in an earlier survey (Kaiser Family Foundation 1999) as the most important to consumers. The prevalence of focal problems is reported in the middle column of table 1. Costs and denials of access were equally common focal problems (each representing roughly 35 percent of focal problems for those reporting at least one problem), with quality shortfalls only slightly less common.
For the focal problem, we asked the respondents the extent (on a four-point Likert scale ranging from none to complete) to which they blamed the problem on their physicians, other physicians, the physician's office staff, their health plan or health insurer, their hospital (if the problem had been associated with treatment in a hospital), themselves, the Medicare or Medicaid programs (if they were beneficiaries of these programs), or any other party they wished to identify.
Given our examination of problems with health plans, we restricted our analytic subsample to those respondents who held their health plan at least somewhat to blame for the problem. This represented roughly two-thirds (67 percent) of those who reported at least one problem. The respondents most frequently blamed the health plan when the problem was related to costs and paperwork (80 percent of all problems in this category) and least frequently when it was related to quality of care (40 percent of problems in this category).
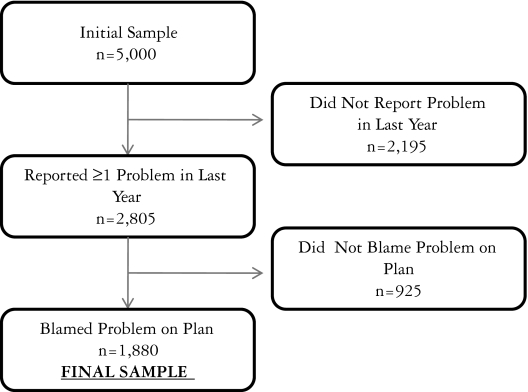
These combined sample restrictions, shown in figure 1, yielded a working sample of 1,880 respondents. Table 2 describes this analytic subsample. Approximately 67 percent of the respondents were female. Because the survey was administered only to people with health insurance, our sample's household income was higher than the U.S. population's average. Our sample was 73.1 percent white, with 44 percent having one or more chronic conditions. Just under 20 percent of our sample rated their health status as fair or poor, and half our sample had been with their health plan for less than three years at the time they reported the problem.
Figure 1.
Description of Study Sample
TABLE 2.
Characteristics of Study Sample (n= 1,880)
| Percent | |
|---|---|
| Female | 67 |
| Age | |
| 18–30 | 15 |
| 31–45 | 41 |
| 46–60 | 33 |
| 61+ | 11 |
| Yearly Household Income | |
| <30K | 15 |
| 30–49K | 22 |
| 50–74K | 21 |
| 75–99K | 13 |
| 100K+ | 17 |
| Missing (set to the mean) | 12 |
| Married | 63 |
| Number of Chronic Conditions | |
| 0 | 56 |
| 1 | 28 |
| 2 or more | 16 |
| Race | |
| Black | 9 |
| Hispanic | 10 |
| Asian | 2 |
| Other | 7 |
| White | 73 |
| Health Status | |
| Excellent | 18 |
| Very good | 33 |
| Good | 29 |
| Fair | 15 |
| Poor | 5 |
| Time with Health Plan | |
| <1 year | 13 |
| More than 1 to 3 years | 36 |
| More than 3 to 7 years | 25 |
| More than 7 years | 26 |
Note: Sample of 1,880 respondents who reported in the last year at least one problem with their health care that was blamed on their health plan.
Responsive consumers should react most strongly to the most serious problems. Past studies suggest that consumers determine the seriousness of a problem in two ways: first, if it produces more deleterious short-term effects and, second, if it is repeated over time (Kolodinsky 1992, 1993; Mulcahy and Tritter 1998). We examined both experiential measures.
Our survey measured the problem's deleterious short-term consequences according to whether consumers reported that this problem required them to pay more or whether it caused a decline in their health. As table 3 shows, 47 percent of our sample said that the problem had some financial impact (8 percent said it cost them more than $1,000 in additional spending). Eighteen percent of those with plan-related problems reported some sort of health decline, with half those declines assessed by the respondents as “somewhat serious” or “very serious.” According to table 1, cost and administrative problems were the most likely to be associated with large out-of-pocket expenses, whereas access barriers were the most frequently associated with subsequent declines in health.
TABLE 3.
Consumers’ Reports of Problematic Experiences
| Characteristics of Problems | Of Those That Reported a Problem (%) |
|---|---|
| Impact of Focal Problem | |
| Cost Impact | |
| None | 53 |
| Less than $500 | 28 |
| From $501 to $1,000 | 10 |
| More than $1,000 | 8 |
| Health Impact | |
| None | 82 |
| Not very serious | 9 |
| Somewhat or very serious | 9 |
| Assessment of Health Plan | |
| Number of Separate Problems | |
| 1 | 25 |
| 2 to 3 | 33 |
| 4 to 5 | 19 |
| 6+ | 23 |
| Dissatisfaction with Plan | |
| Very satisfied | 27 |
| Somewhat satisfied | 43 |
| Somewhat dissatisfied | 13 |
| Very dissatisfied | 18 |
Note: Sample of 1,880 respondents who reported in the last year at least one problem with their health care that was blamed on their health plan.
We also identified “persisting problems” with the health plan by using two measures: the total number of problematic events the enrollee experienced over the past year and the enrollee's overall dissatisfaction with his or her health plan. Approximately 42 percent of our sample indicated that they had had four or more problems over the past year. Only 31 percent of the sample were dissatisfied with their plan (18 percent very dissatisfied), despite reporting that they blamed their problem at least in part on their plan.
We used multiple measures of problematic experiences because each captures somewhat different facets of the consumers’ experiences. Because we identified the focal problems by emphasizing episodes with more consequential outcomes, we obtained a clearer picture of how consumers respond to more serious concerns. But this may also distort our picture of consumerism if the responses were driven more by consumers’ accumulated experiences with a health plan or its affiliated clinicians. Our second set of measures (“persisting problems”) was intended to capture these latter circumstances.
Measuring Consumer Protection and Market Signaling
Our measure of the reliability of consumer protection is the proportion of all individuals with a problem who responded through exit or voice; we also examined the differential response by the severity of the problem. Our measure of the fidelity of market signaling is the proportion of voice or exit associated with more serious problems—that is, those causing a decline in health, substantial additional spending, frequently repeated problems, or dissatisfaction with the plan—compared with voice or exit not associated with problems of greater severity. Market signaling improves as the percentage of complaints resulting from these serious problems increases.
Voice and Exit in Response to Problematic Experiences
Consumers who had had a plan-related problem were asked about a variety of possible responses. We measured exit according to whether the respondents said that they had switched health plans specifically in response to the problem in question (6 percent had) or had filed “a formal complaint or appeal” with their health plan (17 percent had). We focused on complaints to health plans, as opposed to state regulatory agencies, because the latter were fairly rare (less than 3 percent of all problems; not all states have agencies with a clear mandate to receive such grievances). We examined the scope and determinants of complaints to state authorities in another paper (Schlesinger forthcoming). We use the terms formal complaints, formal grievances, and formal voice interchangeably to describe these, since some state regulations explicitly refer to these as grievance procedures, others as complaint mechanisms. They must be written requests in order for a plan practice or decision to be reconsidered.
Many more respondents (70 percent) had contacted their health plan in less formal ways about their problem. We focused on formal complaints to health plans for two reasons. First, this is the form of voice observable to state regulators, purchasers, or potential enrollees. Second, informal contacts were often intended simply to clarify the situation rather than to resolve the problem and so offer little if any protection for consumers.
Identifying Empowered Consumers
Our goal was not just to identify the level of consumer protection or the fidelity of market signaling. We also wanted to know how much these could be improved within the structural arrangements for medical markets and regulation by efforts to better inform consumers or enhance their sense of self-efficacy. To do so, we found two groups of consumers who could be considered more “empowered” in their consumerism and thus more likely to respond in a manner suitable for improving consumer protection and/or market signaling. The first had the capability to respond (functional empowerment), based on three sets of attributes that past research had identified as necessary conditions for consumer activism (Hibbard and Weeks 1987). The second group was defined based on their expressed understanding of their problem (psychological empowerment), since consumers’ responses are more likely to be inhibited if individuals are confused about why the problem emerged or who ought to be held responsible (Annas 1997; Rosenthal and Schlesinger 2002).
Functional Empowerment
Past research suggests that effective medical consumerism requires access to independent sources of information, a willingness to take an active role in choosing treatment, and the opportunity to exercise either exit or voice (Hibbard, Greene, and Tusler 2008). We labeled those consumers who met all three of these criteria based on their survey responses as being functionally empowered.
We measured the availability of information by whether respondents indicated that they would know what to do if they had four common problems with their health care: finding an error in the medical bill, seeking an answer to a question about their health benefits, wanting to learn more about a medical condition, and knowing what to do if they thought their physician was making an error in their treatment. Sixty-three percent of the sample stated that they definitely knew what to do in all four circumstances. Independent decision making means that respondents preferred to choose their own health care (as opposed to leaving it to their physician; 86 percent of the sample favored this active role).
We measured opportunities for action differently for voice and exit. For voice, we asked whether the respondents were aware of their plan's formal grievance procedure and felt confident in their ability to use it (32 percent of the sample were and did). For exit, we asked respondents whether they had a choice of plans during their last open enrollment period and were satisfied with these options (42 percent of our sample had and were). Twenty-three percent of our sample met all of these conditions for voice; 25 percent for exit.
Psychological Empowerment
Consumers not able to make sense of the causes of a problem are often uncertain how they should respond (Hibbard, Greene, and Tusler 2008). Part of this understanding is knowing (or at least believing that one knows) whom to blame for a problem. Past research demonstrates that assigning blame is a strong predictor of consumers’ responses to problems (Rosenthal and Schlesinger 2002). To assess this understanding in our respondents, we asked them, for each party they held responsible, how confident they were in this attribution of blame. We labeled consumers as being psychologically empowered if they reported holding only the plan responsible for the problems and being very confident in this attribution of blame. Whether or not these attributions were accurate, consumers’ understanding of the problem will predispose them to take some action involving the plan. Further, their confidence in this attribution should enhance their perceived self-efficacy, which has been shown in previous research to be associated with more active consumerism. Using these criteria of blame attribution, 23 percent of our sample were psychologically empowered to be a responsive consumer.
Analytic Approach
We calculated the percentage of consumers who formally voiced and exited for both the sample as a whole and the appropriate subgroups. In examining the differences in consumer responses between the empowered and less empowered subsets of consumers, we controlled for factors that could be confounding the relationship between being empowered and consumers’ responses to problems (Rosenthal and Schlesinger 2002; Schlesinger, Druss, and Thomas 1999; Schlesinger, Mitchell, and Elbel 2002). These multivariate models included an interaction term between being empowered and the various problem characteristics (included in the model as dummy variables; each problem characteristic was included in a separate regression). Given the difficulty in interpreting and calculating the standard errors of interaction terms with nonlinear models (Ai and Norton 2003), we estimated linear probability models (estimating logistic regressions did not change the results). The factors shown in previous studies to be important in examining consumer behavior (Rosenthal and Schlesinger 2002; Schlesinger, Druss, and Thomas 1999; Schlesinger, Mitchell, and Elbel 2002) included sociodemographic characteristics: marital status, family income, age, sex, race, and ethnic group. We controlled for both self-reported health status and a count of the respondents’ chronic conditions. We also controlled for the source of insurance (acquired through an employer, a government program, or individual purchase) as well as two aspects of social support: whether the respondents had friends or family who could help with difficult decisions and whether they had friends or family who could help them obtain information needed to make decisions.
Past research also suggests that exit and voice are influenced by the length of time that consumers have been enrolled in a plan or have been seeing their current physician(s). We controlled for both these factors. Finally, to control for the community's familiarity with managed care plans, we included the number of HMOs in the county in 2002 (as captured from the Area Resource File). The appendix contains the full set of linear probability models.
Findings: The Responsiveness of Exit and Voice to Problematic Health Plan Experiences
We first present the findings for our sample as a whole and then for the empowered and less empowered subgroups. We begin with the propensity of consumers to respond to problems and then consider the reliability of these actions as signals for other consumers or relevant parties.
The Prevalence of Exit and Voice among Typical Health Care Consumers
Consumer Protection
As table 4 shows, the average consumer is not particularly responsive to problematic experiences with his or her health plan. Even for problems blamed on the plan that caused out-of-pocket costs of more than $1,000 or led to a serious decline in health, fewer than 40 percent of individuals complained to the plan about the problem. Exit was less sensitive. Even for problems that had the most severe financial or health implications, fewer than 15 percent of the respondents switched plans.
TABLE 4.
Consumers’ Responses to Problems with Health Plans: Consumer Protection
| Characteristics of Problems | Formal Voice (%) | Exit (%) | Either Voice or Exit (%) | Sample Size |
|---|---|---|---|---|
| Problem Assessment | ||||
| Cost Impact | ||||
| None | 15 | 5 | 19 | 996 |
| Less than $500 | 14 | 4 | 17 | 526 |
| From $500 to $1,000 | 28 | 9 | 34 | 188 |
| More than $1,000 | 35 | 11 | 41 | 150 |
| Health Impact | ||||
| None | 15 | 5 | 19 | 1,542 |
| Not very serious | 18 | 8 | 23 | 169 |
| Somewhat or very serious | 34 | 11 | 41 | 169 |
| General Plan Assessment | ||||
| Number of Separate Problems | ||||
| 1 | 10 | 4 | 13 | 470 |
| 2 to 3 | 15 | 5 | 18 | 620 |
| 4 to 5 | 17 | 4 | 21 | 357 |
| 6+ | 29 | 11 | 36 | 432 |
| Dissatisfaction with Plan | ||||
| Very satisfied | 14 | 4 | 17 | 508 |
| Somewhat satisfied | 15 | 6 | 20 | 808 |
| Somewhat dissatisfied | 17 | 5 | 21 | 244 |
| Very dissatisfied | 29 | 10 | 35 | 338 |
Note: Percentages indicate the proportion of respondents with each type of problematic experience who filed a grievance (formal voice) or switched health plans (exit) or did both (either formal voice or exit).
Consumer responsiveness also was limited for persisting problems. Among those enrollees who had had six or more problems in the past year or who were most dissatisfied, fewer than 30 percent had filed a grievance with their plan and fewer than 12 percent had switched plans as a result of the problem. When both forms of response are considered together (the third column in table 4), 60 to 65 percent of consumers who experienced problems with deleterious effects neither complained nor switched plans.
Market Signaling
Aggregate rates of consumer responses are a useful signal of plan performance if, and only if, those with the most severe problems represent a dominant share of responses. Although it is evident from table 4 that both exit and voice are related to the severity of the problems, table 3 shows that minor problems are most common. The combined effects of problem frequency and consumer response are captured in table 5. The percentages in this table reflect the percentage of all enrollees who filed a grievance or switched health plans who met the criteria for a serious problem, with each row representing a different criterion for the problem's severity. For example, 31 percent of the grievances filed with a health plan pertained to problems that had increased the enrollees’ out-of-pocket medical spending by more than $500.
TABLE 5.
Percentage of Consumer Responses Resulting from Serious Problems: Market Signals
| Responses Resulting from Serious Problem |
||
|---|---|---|
| Measures of Seriousness | Formal Voice (%) | Exit (%) |
| Added out-of-pocket costs of $500+ | 31 | 31 |
| Subsequent decline in health | 26 | 26 |
| Five or more problems in the past year | 36 | 37 |
| Dissatisfied with health plan | 38 | 46 |
Note: The percentages in this table convey the proportion of all formal voice (grievances) or exit (plan switching) that met the criterion for more serious problems identified in that row. For example, (top row of table) only 31 percent of grievances filed with a health plan resulted from problems that caused >$500 in added costs.
One might have expected exit to provide a more specific measure of serious problems, since switching plans requires that enrollees learn how to use a whole new health plan, a burden that would not be taken lightly. Yet we found that exit and voice were about equally specific to more severe problems and thus equally (un)reliable signals of serious problems with the plan. The percentage of formal grievances or exit resulting from the problems that we identified as severe ranged from 26 to 46 percent, depending on the definition of severity. For neither form of consumer response did we find that severe problems were the most common circumstance leading to exit or voice.
The Potential for More Fully Empowering Responsive Consumers
To determine how interventions to empower consumers might enhance consumers’ responsiveness, we recalculated our measures of consumer protection and market signaling for our functionally (tables 6 and 7) and psychologically (tables 8 and 9) empowered subgroups of consumers. We then compared consumer behaviors for empowered and less empowered respondents, controlling statistically (in tables 6 and 8) for other attributes that might affect their propensity toward exit or voice.
TABLE 6.
Functional Empowerment and Consumer Protection
| Probability That Consumer Voices or Exits |
||||
|---|---|---|---|---|
| Empowered Sample |
Less Empowered Sample |
|||
| Characteristics of Problems | Formal Voice (%) | Exit (%) | Formal Voice (%) | Exit (%) |
| Specific Problem Assessment | ||||
| Cost Impact | ||||
| None | 19* | 3* | 14 | 5 |
| Less than $500 | 18 | 5 | 13 | 4 |
| From $500 to $1,000 | 40 | 9 | 26 | 6 |
| More than $1,000 | 40 | 12 | 33 | 10 |
| Health Decline | ||||
| None | 20** | 5 | 14 | 5 |
| Not very serious | 19 | 1*** | 17 | 8 |
| Somewhat or very serious | 41 | 14 | 31 | 7 |
| General Plan Assessment | ||||
| Number of Separate Problems | ||||
| 1 | 17** | 6 | 8 | 4 |
| 2 to 3 | 13 | 4 | 15 | 5 |
| 4 to 5 | 25* | 2 | 15 | 4 |
| 6+ | 39** | 9 | 26 | 9 |
| Dissatisfaction with Plan | ||||
| Very satisfied | 17 | 4 | 13 | 4 |
| Somewhat satisfied | 21** | 6 | 14 | 7 |
| Somewhat dissatisfied | 19 | 7 | 17 | 5 |
| Very dissatisfied | 33 | 3 | 27 | 8 |
| Sample Size | n = 432 | n = 1,448 | n = 1,410 | |
Notes: Difference indicated between empowered and less empowered groups: *p < 0.10; **p < 0.05; ***p < 0.01.
Authors’ calculations of predicted probabilities from a linear probability model, holding all other variables at their mean. Statistically significant differences are calculated for differences in the predicated probability between the empowered group and the less empowered group (e.g., percent of formal voicing for those with no cost impact in the empowered group versus percent of formal voicing for those with no cost impact in the less empowered group). The empowered sample are those who understand how to deal with health care problems, want to be active decision makers, and either know how to formal voice (for voicing models) or have and are satisfied with their alternative plan options (for exit models). Each reported probability is from one of eight separate regressions that includes interactions between the problem characteristic and empowerment and has been regression-adjusted to control for marital status; family income; age; sex; race and ethnic group; region; whether their health insurance was individually purchased, provided through an employer, or through a government program; self-reported health status; the number of chronic conditions the respondent reported; the number of HMO plans in the county; social support available for helping to address problems; the length of time they had been treated by their current physician; and the length of time they had been enrolled in the health plan in which they experienced the problem. See appendix for full results.
TABLE 7.
Functional Empowerment and Market Signaling (Percentage of All Responses That Involve Serious Problems)
| Empowered Sample |
Less Empowered Sample |
|||
|---|---|---|---|---|
| Measures of Seriousness | Formal Voice (%) | Exit (%) | Formal Voice (%) | Exit (%) |
| Added out-of-pocket costs $500+ | 28 | 29 | 30 | 25 |
| Subsequent decline in health | 25 | 30 | 33 | 27 |
| Five or more problems in the past year | 28 | 26 | 36 | 37 |
| Dissatisfied with health plan | 33 | 18 | 38 | 35 |
Note: Here we present the percentage of formal voicing and exit associated with more serious problems, as defined by our four measures of severity and separating out the functionally empowered consumers from those who are less empowered.
TABLE 8.
Psychological Empowerment and Consumer Protection
| Probability That Consumer Voices or Exits |
||||
|---|---|---|---|---|
| Empowered Sample |
Less Empowered Sample |
|||
| Characteristics of Problems | Formal Voice (%) | Exit (%) | Formal Voice (%) | Exit (%) |
| Specific Problem Assessment | ||||
| Cost Impact | ||||
| None | 19* | 5 | 13 | 5 |
| Less than $500 | 14 | 9** | 14 | 3 |
| From $500 to $1,000 | 31 | 8 | 28 | 6 |
| More than $1,000 | 40 | 12 | 33 | 10 |
| Health Decline | ||||
| None | 20** | 7 | 14 | 5 |
| Not very serious | 11 | 9 | 19 | 6 |
| Somewhat or very serious | 44 | 8 | 31 | 8 |
| General Plan Assessment | ||||
| Number of Separate Problems | ||||
| 1 | 11 | 6 | 10 | 4 |
| 2 to 3 | 20** | 6 | 13 | 4 |
| 4 to 5 | 22 | 6 | 17 | 3 |
| 6+ | 31 | 11 | 28 | 9 |
| Dissatisfaction with Plan | ||||
| Very satisfied | 16 | 4 | 13 | 4 |
| Somewhat satisfied | 18 | 9 | 14 | 6 |
| Somewhat dissatisfied | 24 | 5 | 15 | 5 |
| Very dissatisfied | 29 | 5 | 29 | 8 |
| Sample Size | n = 432 | n = 1,448 | ||
Notes: Difference indicated between empowered and less empowered groups: *p < 0.10; **p < 0.05; ***p < 0.01.
TABLE 9.
Psychological Empowerment and Market Signaling (Percentage of All Responses That Involve Serious Problems)
| Empowered Sample |
Less Empowered Sample |
|||
|---|---|---|---|---|
| Measures of Seriousness | Formal Voice (%) | Exit (%) | Formal Voice (%) | Exit (%) |
| Added out-of-pocket costs $500+ | 26 | 18 | 30 | 29 |
| Subsequent decline in health | 24 | 23 | 33 | 28 |
| Five or more problems in past year | 23 | 24 | 38 | 38 |
| Dissatisfied with health plan | 34 | 12 | 38 | 39 |
Note: Here empowerment is defined as those that blamed only their health plan for their problem and were highly confident in their attribution of blame. See note in table 7 for greater explanation and interpretation.
Functionally Empowered Patients and Consumer Response
Consumers who regarded themselves as being informed, autonomous decision makers and having options with respect to their health plan were generally more likely to voice their concerns to their current plan, compared with the less empowered but otherwise comparable enrollees; this difference was not always statistically significant (table 6). But voice was not common even among the most empowered consumers. In the functionally empowered group, generally less than 40 percent of enrollees complained to the plan, even when facing severe problems or being extremely dissatisfied. Exit appeared even less responsive to this method of empowerment. Functionally empowered enrollees (who reported being informed, autonomous, and having options to act) were more likely than other enrollees to switch plans if their health seriously declined owing to a plan-related problem, but (1) 90 percent of this group still failed to exit and (2) for all other strata of problem severity, structural empowerment was associated with no increase in exit at all.
Functionally Empowered Patients and Market Signaling
We might think that the most empowered consumers would more reliably differentiate between severe and trivial problems, responding more often and vigorously to the former. However, functional empowerment actually reduced the fidelity of market signals for six of our eight strata of problem severity, and in one case (seriousness as measured by plan dissatisfaction), the fidelity of empowered consumers was only about half that of less empowered enrollees (table 7). The problem is that this method of empowerment increases responsiveness almost as much for trivial problems as for serious ones. Since there are many more trivial problems, the specificity of both exit and voice was reduced in the empowered sample and was markedly lower for half our measures.
Psychologically Empowered Patients and Consumer Response
Recall that psychologically empowered consumers were confident of their attribution of blame and designated the health plan as the only blameworthy party (i.e., they considered the plan to be responsible for the problem and did not consider any other party culpable). As table 8 suggests, these consumers were more likely to voice their complaints, although these differences rarely reached statistical significance. Even in the most severe cases, only about 40 percent of empowered consumers filed complaints with their health plan, and this form of empowerment seemed to have no impact on their switching plans.
Psychologically Empowered Patients and Market Signaling
Psychological empowerment also holds the same problematic consequences for market signaling as functional empowerment does. After taking into account the greater prevalence of minor problems, the empowerment effects were larger for more trivial concerns (table 9). Indeed, the degraded fidelity of market signals was more pronounced with this form of empowerment, consistently for both exit and voice for each of our strata of problem severity. These declines are substantial: on average, the fidelity of consumers’ response in the empowered sample was less than three-quarters the level of the less empowered sample. In one case (exit in response to dissatisfaction with health plan), the fidelity in the empowered sample was less than a third that of the less empowered sample.
Discussion and Conclusion
Relatively few consumers voice their concerns through formal complaints or exit their health plan in response to even the most severe problems. Given that the costs of such action might outweigh the limited benefits of doing so, this does not mean that consumers are making poor judgments in this regard. But even if these choices can be explained at the individual level, they may not have a public benefit in either reducing the risk of future problems for these individuals (consumer protection) or identifying health plans that are performing poorly (market signaling).
Many observers have asserted that American medicine can best be improved by informing and empowering consumers. This claim is most often made by those in the federal government (Cooper and Vladeck 2000). For example, in a March 2004 speech to the U.S. Chamber of Commerce, President George W. Bush announced, “I believe that the best health care policy is one that trusts and empowers consumers and one that understands the market” (Toner 2004). President Barack Obama, who professes a quite different approach to health policy, nonetheless promotes the choice of health plans and physicians as a central aspect of reform (White House 2009).
Our findings suggest that if one really understands the market, one learns not to trust empowerment strategies too much. Even if every American were magically endowed with the skills and awareness of the most empowered consumers in our sample, consumer responsiveness would not rise dramatically, even in response to severe problems. Greater empowerment also does little to improve responsiveness to more persistent problems and appears to decrease the specificity of response by encouraging voice for less consequential problems. These findings raise serious doubts about relying on consumer empowerment as a principal means of improving American health care. To be clear, we are not suggesting that either empowerment strategies in particular or market-oriented health policies in general have no useful role. We seek only to caution against treating these strategies as transformational, as claimed by some of their advocates, or as reliable as would be needed to have them serve as the foundation for quality assurance.
More specifically, we do see real potential for responsive medical consumerism in health policy if it is correctly understood and realistically implemented. From the standpoint of consumer protection, voice appears to be a somewhat more reliable avenue of consumer response than exit. Both the empowerment strategies we identified were associated with a somewhat greater propensity for consumers to file grievances in response to problems. But even at its best, responsive consumerism with respect to health plans appears limited.
The failure to recognize the limitations of policies based on responsive consumerism makes their application a potential concern. Surely a medical diagnostic test that is capable of identifying less than half of even the most severe cases of a disease would be seen at best as appropriate only as a supplement to other tests. And clinicians would certainly think twice about using a diagnostic test that registers “false positives” more than two-thirds of the time. Yet that is precisely the reliability and fidelity of exit and voice in response to health plans’ problematic practices. Unfortunately, no law requires the equivalent of a Food and Drug Administration review of policy ideas, that is, an assessment of the realistic impact of the proposed policy change on patients’ well-being. Policymakers can thus blithely and repeatedly propose initiatives that have, at best, a checkered track record or prospect of future impact, without worry that these claims will be subject to a public test of efficacy or safety.
How Much Responsiveness Is Necessary?
Defenders of market reforms in medical care might argue that this assessment is unduly pessimistic. Our results indicate that up to 40 percent of enrollees with the most serious problems either formally voice or exit and that about a third of the reported disenrollment or grievances were in response to relatively serious problems. Although neither response meets what most would consider an ideal of empowered consumerism, arguably each represents a significant source of inducement for plans to change their practices. This is true, but not always in ways that would actually enhance quality of care for enrollees. If the enrollees with problems have chronic conditions that predict high costs, it is actually in the plan's financial interests to encourage disenrollment, especially if other prospective enrollees with these chronic conditions are thereby deterred from ever enrolling in the plan.
Moreover, we must caution that our findings concerning consumer responsiveness err on the side of being overly optimistic in regard to the capacity of responsive consumerism to provide either effective consumer protection or market signaling. We now briefly reconsider the criteria for each of these paradigms in light of our findings.
Responsive Consumerism as Protection for Individual Consumers
In our analyses, we considered only those problems that consumers notice and blame on their health plan. But consumers may not recognize many of the problems associated with medical care or incorrectly believe them not to be caused by the plan (Goold and Klipp 2002; Rosenthal and Schlesinger 2002; Schlesinger, Mitchell, and Elbel 2002). If consumers fail to recognize that a problem exists or do not understand that the plan is to blame, consumer responsiveness will be even weaker than we describe. A second factor to consider that is relevant to consumer protection is the efficacy of exit and voice. Past research suggests that about two-thirds of enrollees who voice their concerns have the problem resolved to their satisfaction but that only about 22 percent of those who switch plans report an equally positive outcome (Schlesinger, Mitchell, and Elbel 2002).
Considered together, these factors suggest that even the most effective empowerment strategies offer far less than a fifty-fifty chance of enhancing the welfare of people who have had a problem with their health plan. Voicing has the greater promise in this regard. By contrast, the option of exit borders on worthless at safeguarding individual consumers’ well-being. Even the most aggrieved enrollees rarely switch plans and, when they do, may not resolve their problem if their new plan subjects them to the same constraints on coverage or access as did their previous plan.
To be sure, there may be other ways in which consumers’ responses trigger actions by other relevant parties and thus indirectly enhance consumer protection. Aggrieved patients, for example, might voice their concerns to either employers or clinicians in addition to their health plan. In earlier work, we noted that these complementary avenues for voice were used only moderately by consumers with problematic medical experiences (reported by 16 percent and 28 percent, to employers and clinicians, respectively). And while voice to physician was associated with a moderate increase in the probability that consumers' problems would be resolved, voice to employers did not seem to help resolve individual consumers’ complaints at all (Schlesinger, Mitchell, and Elbel 2002).
Responsive Consumerism as a Market Signal
Our findings initially appear more promising with respect to market signaling. For both exit and voice, about a third of all consumer responses reflect more serious or chronic problems with the health plan. Even if only a subset of aggrieved consumers respond in these ways, as long as this proportion stays constant across plans, even this partial response becomes a useful way of distinguishing plans’ performance relative to one another. Here again, however, a more complete consideration of the implications of our findings reveals that even when comparing relative performance, disenrollment has serious shortcomings as a signal of plan performance.
It is safe to assume that enrollees rarely file a formal complaint unless they feel somehow aggrieved. By contrast, as we alluded to earlier, studies suggest that less than a quarter of all disenrollment in employer-based insurance is a consequence of dissatisfaction with the plan (Cunningham and Kohn 2000). Most disenrollment reflects other considerations, including employers changing the plans offered to their workers, plans withdrawing from public programs, people switching jobs, and Medicaid enrollees losing eligibility as their family income increases or they are otherwise dropped from the program (Cunningham and Kohn 2000; Riley, Ingber, and Tudor 1997; Silberman et al. 2002). Factoring in these other sources of disenrollment significantly reduces the specificity of exit as a signal of serious problems in health plan practices.
Methodological Limitations and Directions for Future Research
Several limitations of this study are important to note. First, the data are based on respondents’ self-report from a telephone survey with an approximately 50 percent response rate. Given the proliferation of call screening, this response rate is reasonably good for a survey of the public. Nonetheless, a 50 percent response rate could be a concern if it systematically underrepresented or overrepresented either the nature of consumers’ problems with medical care or the forms of their responses to those problems. For some of consumers’ experiences or practices, we might worry that asking respondents to recall a full year of events might lead to underreporting. This does not seem likely for medical care, however, since problematic experiences appeared highly salient to our respondents. Indeed, our interviewers reported often having difficulty getting the respondents off the phone, and the survey's discontinuation rates were very low.
Given the various sample restrictions that we used for our analysis (and the fact that the sample included only those respondents with some form of insurance), we could not explore with analytic precision the relative reliability of responsive consumerism for minority populations. Previous research, however, does suggest that voice might be more constrained among disadvantaged groups (limited resources inhibit aggressive use of grievance mechanisms, and lesser trust in health care professionals inhibits engaging them as advocates in the voicing process) and may also discourage exit (if all plans are presumed to mistreat less advantaged patients, consumers will see little benefit in switching). But these implications are speculative; more research needs to be done on the relationship between social advantage and responsive consumerism.
Also of note are the implications of using cross-sectional data, as we do here. With survey data of this type, we cannot objectively confirm the chronological order in which consumers responded to various parties or took various actions. It would be useful, in future research, to construct a more longitudinal portrait of consumer responses or to use qualitative methods to assess more closely the narrative histories of patients’ responsiveness. In addition, future work should examine the role of specific market characteristics as they relate to consumers’ involvement more generally. In earlier work, we found that state laws did influence response, at least if consumers knew about these regulations. But other contextual factors may matter as well, other than familiarity with managed care plans (which we controlled for statistically here) (Schlesinger, Mitchell, and Elbel 2002).
It also is important to recognize that our measures identifying “empowered” consumers have limitations, since they were based on self-reports by survey respondents. It could be argued that there are some considerable and consequential differences with regard to empowerment, between consumers who think they are well informed about medical concerns and those who actually are well informed. We attempted to capture this with our distinction between functional and psychological empowerment, but since even the functional measures are self-reported (we know only whether consumers think that they have access to good information supporting choice and cannot determine for certain whether they actually do), we could argue that all our measures are really more psychological. Of course, since most efforts to “activate” consumers depend on this sort of psychological engagement, it is useful to focus in this manner (Hibbard, Greene, and Tusler 2008). But it still is possible that other public policies might facilitate empowerment in ways that we could not measure here—for instance, by promoting access to information about other consumers’ experiences (anecdotal accounts) in the same locale.
Conversely, it is possible that our comparisons of “empowered” and “less empowered” consumers actually overstate the potential for empowerment initiatives to alter responsive consumerism. Our subgroups of consumers may well have differed on the basis of other unmeasured characteristics. As an example, consumers who reported being empowered because they had more complete information about health care may have acted differently in response to problems, not because they had this information, but because they had some intrinsic motivation (e.g., a sense of self-efficacy). This motivation may have caused them both to seek out information and to respond differently to problematic health care experiences. These deeper-rooted personality traits are almost certainly less influenced by policy initiatives, however well designed. This may render the behavioral differences induced by empowerment initiatives even smaller than those reported here.
Finally, we note a few ways in which we were not able to estimate precisely the total amount of exit and/or voice. First, we observed only the responses to the principal problem. Individuals with more than one problem might have responded to these other problems, adding to the total amount of exit and/or voice. And since the focal problem (for which we had adequate measures of consumer response) was chosen as being the most consequential of potential problems, it is unlikely that these additional responses would increase the overall fidelity of the market signal. Put differently, these additional responses were more likely to be for less consequential problems, leading to a likely overestimation of the specificity of consumer response. Second, related specifically to exit, many individuals switch health plans every year for reasons completely unrelated to dissatisfaction, such as job changes, marriage, or divorce. This also dilutes the market signal. Third, and working in the opposite direction, given the timing of our data collection and the typical time of open enrollment periods, we could be missing some consumers who might exit when this period begins. To examine this possibility, we compared the 6 percent exit figure for our entire analytic sample with the 10 percent exit figure for those who purchased insurance in the private market (and did not have an open enrollment period). While this private market rate is somewhat larger, it does not appear to warrant any alterations to our overall conclusions, particularly considered in conjunction with the above two underestimations of the true exit rate.
Policy Implications
The realistic potential for consumer responsiveness, particularly plan switching, seems far more limited than promised by many advocates of market-oriented medical care who portray it as the primary bulwark for quality assurance. Our evidence makes this seem quite unrealistic. That does not necessarily mean that competition among plans might not improve medical care through pathways involving plans’ influence over medical practice that are not mediated by consumers’ assessments (e.g., clinicians seeking to avoid public embarrassment about poor performance). But there certainly are many dimensions of medical care and plan performance for which assessments by individual patients and/or plan enrollees are crucial to assessing that performance (Mobley et al. 2007).
Nor do the shortcomings identified in our analyses imply that we should abandon empowerment strategies. In our assessment, the appropriate policy responses need to be more nuanced and will differ in important ways for the goals of market signaling and consumer protection. They may also differ as the focus of empowerment strategies shifts from choice among health plans to choice among clinicians and clinician groups, as it increasingly has in recent years. Although the context and salient patient preferences for clinician choice will clearly differ from those for plan choice, we believe that the analytic distinction between consumer protection and market signaling remains useful, as does the notion that policymakers need to realistically assess patients’ capacity to engage as responsive consumers.
Using exit or voice as a market signaling mechanism is a rather imprecise measure of health plan performance for those who care the most about severe or harmful episodes. Because not all enrollees will be equally willing or able to respond and some consequences (debilitating health effects from the problem) could impede exit and voice, these forms of consumer influence will be seriously constrained. Under these circumstances, policymakers should seek other avenues for signaling poor performance—for example, through regular surveys of enrollees’ experiences or by engaging other advocates such as physicians or employers who can convey consumers’ concerns (Sofaer 2009). We also could consider a better recording in formal complaint systems of the type, severity, and consequences of the problem. This is the approach advocated in the Medicare Advantage voluntary disenrollment survey and does show some promise (Mobley et al. 2007).
But if we care at all about protecting the individual consumer, it is difficult to identify any plausible mechanisms that can serve as an alternative to consumer-initiated responses. Any imaginable system of surveying or monitoring enrollee well-being cannot effectively reach every consumer without being extremely costly and problematically intrusive. So consumer protection will likely continue to depend on enrollees’ taking action in their own defense.
Our findings suggest that voicing has clear advantages over exit in this regard. It is two to three times more sensitive as a marker for serious problems, and it appears to have greater potential for improving consumer responsiveness through additional consumer empowerment. As mentioned earlier, previous research suggests that some state regulatory policies can enhance the efficacy of voice as long as enrollees know that those policies are in place (Schlesinger, Mitchell, and Elbel 2002). That said, the same empowerment that enhances consumer protection will likely adulterate market signaling even more.
A realistic view of responsive consumer behavior with respect to health plans requires recognizing its limitations as well as its realistic potential for improvement. Market-based reforms can never fully substitute for regulatory oversight or professional norms as a safeguard for vulnerable patients. These additional forms of protection become more vital if individual consumer protection is given greater importance as compared to market signaling. Policymakers need to take a more careful look at the capabilities of consumers to properly determine how best to meet their needs.
Acknowledgments
This article benefited from comments at the Health Policy Seminar of the Yale School of Public Health and from the written feedback from Nicole Quon and Kate Ellingson. We are grateful for the thoughtful comments of Hal Luft (who took editorial responsibility for the Quarterly for the review of this manuscript), as well as those of four anonymous reviewers. We are also grateful for the Atlantic Philanthropies' support of the survey used in this analysis, as well as for the contributions of Bradford Gray, who recused himself from decisions regarding this manuscript, and Shannon Mitchell and Marsha Rosenthal for their assistance in the development of the survey.
Appendix
The following is the results for all the linear probability models used to calculate the predicted probabilities for examining empowerment. These models were run with (4) region-fixed effects. The standard errors are clustered at the MSA level; n= 1,880. These results were used to calculate the probability of consumer response for our empowered versus less empowered groups by keeping all other variables at their means.
The definitions of all the control variables are as follows:
Married = 1 if subjects are married.
Income: Household income, 1 = <$20K, 2 =$20 to $30K, 3 =$30 to $40K, 4 =$40 to $50K, 4.5 = individual did not answer and subjects were imputed to be 4.5 (representing $45K), 5 =$50 to $75K, 6 =$75 to $100K, 7 =$100K+.
Number of Chronic Conditions = Count of the following chronic conditions diagnosed in subject: heart disease or stroke not counting high blood pressure, mental illness, cancer, diabetes, serious breathing disorder, chronic back pain, HIV/AIDS.
Medicaid Plan = 1 if in a Medicaid health plan.
Medicare Plan = 1 if in a Medicare health plan.
Nongroup Plan = 1 if in a nongroup health plan.
Plan Count = Number of health plans in county of residence in 2002 per area resource file.
Black = Subject identifies as black (white is the excluded group for all racial categories).
Hispanic = Subject identifies as Hispanic.
Asian = Subject identifies as Asian.
Other Race = Subject identifies as other (white is the excluded group).
Age in Years = Represented as a continuous variable.
Female = 1 if female.
Support Index = Measure ranging from 0 to 2, indicating level of external support available to help understand problem (0 to 1) and make decision (0 to 1).
Time with Primary MD: Time in years with primary doctor.
Time with Main MD in Years (10 = ten or more years).
Time in Plan = Time enrolled in plan in years.
| Formal Voice |
Exit |
|||||
|---|---|---|---|---|---|---|
| Beta | sig | SE | Beta | sig | SE | |
| Functional Empowerment: Costs | ||||||
| Intercept | 0.159966 | ** | 0.076565 | 0.064045 | ** | 0.050073 |
| Empowered: Functional | 0.050129 | 0.032586 | −0.02105 | * | 0.012721 | |
| Paid <$500 | −0.00495 | 0.021896 | −0.01099 | 0.013735 | ||
| Paid $500 to $1K | 0.122241 | *** | 0.035888 | 0.010267 | 0.020586 | |
| Paid more than $1K | 0.195036 | *** | 0.047166 | 0.046029 | 0.030604 | |
| Emp*Paid <$500 | 0.002533 | 0.04341 | 0.029793 | 0.023658 | ||
| Emp*Paid $500 to $1K | 0.095743 | 0.091444 | 0.048438 | 0.054947 | ||
| Emp*Paid $1K+ | 0.017982 | 0.096006 | 0.041573 | 0.080565 | ||
| Married | 0.057622 | *** | 0.018002 | 0.007707 | 0.012063 | |
| Income | 0.006644 | 0.005486 | −0.00015 | 0.003455 | ||
| No. of Chronic Conditions | 0.020234 | 0.012821 | 0.020542 | *** | 0.00745 | |
| Medicaid Plan | 0.156328 | ** | 0.068402 | 0.095889 | ** | 0.063025 |
| Medicare Plan | −0.00944 | 0.035108 | 0.021963 | 0.027127 | ||
| Nongroup Plan | −0.02933 | 0.031147 | 0.041598 | 0.026089 | ||
| Plan Count | 0.000508 | 0.001737 | 0.00107 | 0.001071 | ||
| Black | 0.016363 | 0.03353 | 0.026473 | 0.019276 | ||
| Hispanic | 0.06114 | 0.042279 | 0.061092 | *** | 0.01919 | |
| Asian | −0.04012 | 0.048482 | −0.02244 | 0.029154 | ||
| Other Race | 0.07555 | 0.051828 | 0.013581 | 0.027776 | ||
| Health Status: Fair | −0.0232 | 0.060451 | −0.0009 | 0.035008 | ||
| Health Status: Good | −0.03123 | 0.05133 | −0.00621 | 0.032964 | ||
| Health Status: Very Good | −0.06356 | 0.054762 | 0.013966 | 0.033185 | ||
| Health Status: Excellent | −0.07016 | 0.054366 | 0.022352 | 0.03768 | ||
| Age in Years | −0.00172 | ** | 0.000829 | −0.0003 | 0.000478 | |
| Female | −0.01331 | 0.018337 | −0.00316 | 0.013653 | ||
| Support Index | −0.02958 | ** | 0.013551 | −0.01236 | 0.009099 | |
| Time with Primary MD | 0.004113 | 0.002581 | −0.0009 | 0.001739 | ||
| Time with Plan | 0.001283 | 0.002497 | −0.00535 | *** | 0.001825 | |
| Functional Empowerment: Health Decline | ||||||
| Intercept | 0.100163 | 0.07602 | 0.038316 | 0.049811 | ||
| Empowered: Functional | 0.056868 | ** | 0.025488 | −0.00597 | 0.012634 | |
| Small Health Decline | 0.032242 | 0.035462 | 0.027418 | 0.027723 | ||
| Large Health Decline | 0.166381 | *** | 0.049794 | 0.012688 | 0.024162 | |
| Emp*Small Decline | −0.04487 | 0.083734 | −0.06854 | 0.031583 | ||
| Emp*Large Decline | 0.042242 | 0.116272 | 0.084192 | 0.063784 | ||
| Married | 0.04261 | ** | 0.017156 | 0.012283 | 0.011961 | |
| Income | 0.013303 | ** | 0.005397 | −7.2E-05 | 0.003268 | |
| No. of Chronic Conditions | 0.019999 | 0.012426 | 0.021229 | *** | 0.006823 | |
| Medicaid Plan | 0.13548 | ** | 0.066545 | 0.090679 | 0.058549 | |
| Medicare Plan | 0.002513 | 0.0399 | 0.017385 | 0.02574 | ||
| Nongroup Plan | 0.006968 | 0.030516 | 0.078657 | *** | 0.03019 | |
| Plan Count | −0.00072 | 0.001827 | 0.001656 | 0.001179 | ||
| Black | 0.021753 | 0.030999 | 0.020376 | 0.016989 | ||
| Hispanic | 0.060528 | 0.039268 | 0.0586 | *** | 0.018426 | |
| Asian | −0.06133 | 0.046754 | −0.0306 | 0.029083 | ||
| Other Race | 0.06949 | 0.048299 | 0.018904 | 0.023289 | ||
| Health Status: Fair | 0.021156 | 0.057533 | 0.00819 | 0.033048 | ||
| Health Status: Good | 0.01779 | 0.04908 | 0.0036 | 0.032126 | ||
| Health Status: Very Good | −0.00986 | 0.052615 | 0.030089 | 0.033712 | ||
| Health Status: Excellent | −0.01618 | 0.050994 | 0.038649 | 0.036154 | ||
| Age in Years | −0.00137 | * | 0.00081 | −0.00019 | 0.000493 | |
| Female | −0.01371 | 0.016595 | −0.00857 | 0.015151 | ||
| Support Index | −0.02385 | * | 0.014134 | −0.01083 | 0.009096 | |
| Time with Primary MD | 0.001683 | 0.002612 | −0.00131 | 0.001675 | ||
| Time with Plan | 0.000349 | 0.00231 | −0.00598 | *** | 0.001694 | |
| Functional Empowerment: Number of Problems | ||||||
| Intercept | 0.043091 | 0.076277 | 0.016575 | 0.053858 | ||
| Empowered: Functional | 0.086649 | ** | 0.037519 | 0.017291 | 0.020757 | |
| 2 to 3 Problems | 0.067431 | *** | 0.023034 | 0.01038 | 0.017641 | |
| 4 to 5 Problems | 0.064698 | ** | 0.026375 | 0.003307 | 0.017527 | |
| 6+ Problems | 0.171327 | *** | 0.03092 | 0.053162 | 0.018737 | |
| Emp*2 to 3 Problems | −0.11303 | ** | 0.049159 | −0.02547 | 0.028823 | |
| Emp*4 to 5 Problems | 0.016013 | 0.069755 | −0.0364 | 0.028117 | ||
| Emp*6+ Problems | 0.042546 | 0.080379 | −0.01585 | 0.044463 | ||
| Married | 0.040633 | ** | 0.018081 | 0.012987 | 0.011973 | |
| Income | 0.012755 | ** | 0.005463 | −0.00027 | 0.003267 | |
| No. of Chronic Conditions | 0.015315 | 0.012063 | 0.019946 | *** | 0.006795 | |
| Medicaid Plan | 0.16301 | ** | 0.066863 | 0.091849 | 0.058539 | |
| Medicare Plan | 0.001505 | 0.03948 | 0.019372 | 0.025475 | ||
| Nongroup Plan | 8.83E-05 | 0.030433 | 0.073974 | ** | 0.030089 | |
| Plan Count | −0.00058 | 0.001843 | 0.001528 | 0.001182 | ||
| Black | 0.022791 | 0.0326 | 0.020356 | 0.017118 | ||
| Hispanic | 0.05684 | 0.039129 | 0.058089 | *** | 0.018401 | |
| Asian | −0.04775 | 0.044043 | −0.02565 | 0.028297 | ||
| Other Race | 0.063697 | 0.048672 | 0.014992 | 0.023857 | ||
| Health Status: Fair | 0.002219 | 0.055944 | 0.013069 | 0.03242 | ||
| Health Status: Good | −0.0134 | 0.048362 | 0.006689 | 0.030218 | ||
| Health Status: Very Good | −0.03164 | 0.051542 | 0.035484 | 0.031661 | ||
| Health Status: Excellent | −0.03543 | 0.051328 | 0.045156 | 0.033939 | ||
| Age in Years | −0.00121 | 0.000825 | −0.00015 | 0.000497 | ||
| Female | −0.00796 | 0.016089 | −0.00831 | 0.014323 | ||
| Support Index | −0.01545 | 0.013197 | −0.00877 | 0.008922 | ||
| Time with Primary MD | 0.003173 | 0.002689 | −0.00101 | 0.001714 | ||
| Time with Plan | 0.001068 | 0.002224 | −0.00592 | *** | 0.001699 | |
| Functional Empowerment: Dissatisfaction with Plan | ||||||
| Intercept | 0.165789 | * | 0.084986 | 0.039745 | 0.050758 | |
| Empowered: Functional | 0.035423 | 0.040002 | −0.00311 | 0.016619 | ||
| Some Satisfaction with Plan | 0.005549 | 0.020346 | 0.028155 | * | 0.014889 | |
| Some Dissatisfaction | 0.037056 | 0.035271 | 0.01097 | 0.019851 | ||
| Much Dissatisfaction | 0.137486 | *** | 0.034434 | 0.042439 | ** | 0.021202 |
| Emp*Some Satisfaction | 0.033925 | 0.053202 | 0.000452 | 0.029294 | ||
| Emp*Some Dissatisfaction | −0.01476 | 0.072445 | 0.027535 | 0.037375 | ||
| Emp*Much Dissatisfaction | 0.028736 | 0.070187 | −0.04589 | 0.036822 | ||
| Married | 0.044204 | ** | 0.018659 | 0.012953 | 0.013135 | |
| Income | 0.012987 | ** | 0.005963 | −0.00149 | 0.003507 | |
| No. of Chronic Conditions | 0.020417 | 0.012927 | 0.021987 | *** | 0.007129 | |
| Medicaid Plan | 0.12122 | * | 0.069281 | 0.096434 | 0.06496 | |
| Medicare Plan | 0.016652 | 0.041251 | 0.024805 | 0.027406 | ||
| Nongroup Plan | 0.007729 | 0.030647 | 0.069431 | ** | 0.031269 | |
| Plan Count | −0.00052 | 0.002031 | 0.001692 | 0.001211 | ||
| Black | 0.026601 | 0.032583 | 0.022075 | 0.017412 | ||
| Hispanic | 0.057666 | 0.04053 | 0.062392 | *** | 0.019765 | |
| Asian | −0.06894 | 0.046963 | −0.0306 | 0.03161 | ||
| Other Race | 0.073156 | 0.051009 | 0.024485 | 0.026508 | ||
| Health Status: Fair | −0.04115 | 0.058003 | 0.006214 | 0.034955 | ||
| Health Status: Good | −0.04993 | 0.052133 | −0.00255 | 0.032696 | ||
| Health Status: Very Good | −0.08271 | 0.05362 | 0.023255 | 0.033583 | ||
| Health Status: Excellent | −0.09711 | * | 0.052798 | 0.034146 | 0.03633 | |
| Age in Years | −0.00198 | ** | 0.000777 | −0.00038 | 0.000505 | |
| Female | −0.01022 | 0.017239 | −0.00795 | 0.014266 | ||
| Support Index | −0.0215 | 0.013713 | −0.01231 | 0.009903 | ||
| Time with Primary MD | 0.002269 | 0.002871 | −0.00063 | 0.00178 | ||
| Time with Plan | 0.00206 | 0.002391 | −0.00583 | *** | 0.001804 | |
| Psychological Empowerment: Costs | ||||||
| Intercept | 0.138894 | * | 0.076674 | 0.067268 | 0.049623 | |
| Empowered: Psych. | 0.061226 | ** | 0.030764 | 0.007054 | 0.015619 | |
| Paid <$500 | 0.009244 | 0.023724 | −0.01428 | 0.01153 | ||
| Paid $500 to $1K | 0.143689 | *** | 0.03877 | 0.018818 | 0.021949 | |
| Paid more than $1K | 0.20067 | *** | 0.047363 | 0.052403 | 0.0353 | |
| Emp*Paid <$500 | −0.06294 | 0.054756 | 0.051836 | 0.034906 | ||
| Emp*Paid $500 to $1K | −0.02567 | 0.084782 | 0.009972 | 0.050565 | ||
| Emp*Paid $1K+ | 0.002961 | 0.099868 | 0.01265 | 0.063073 | ||
| Married | 0.058807 | *** | 0.017983 | 0.007816 | 0.011958 | |
| Income | 0.007388 | 0.005453 | −0.00081 | 0.0034 | ||
| No. of Chronic Conditions | 0.02263 | * | 0.013353 | 0.020329 | *** | 0.007381 |
| Medicaid Plan | 0.161411 | ** | 0.069292 | 0.098355 | 0.06165 | |
| Medicare Plan | −0.00617 | 0.035318 | 0.023726 | 0.026511 | ||
| Nongroup Plan | −0.03071 | 0.030816 | 0.039839 | 0.026142 | ||
| Plan Count | 0.000698 | 0.001713 | 0.001086 | 0.001066 | ||
| Black | 0.02526 | 0.034807 | 0.027052 | 0.019128 | ||
| Hispanic | 0.065692 | 0.042111 | 0.063134 | *** | 0.01917 | |
| Asian | −0.0415 | 0.048398 | −0.01817 | 0.029219 | ||
| Other Race | 0.07608 | 0.051017 | 0.015727 | 0.028086 | ||
| Health Status: Fair | −0.02806 | 0.060993 | −0.00049 | 0.034607 | ||
| Health Status: Good | −0.03354 | 0.051587 | −0.00745 | 0.032101 | ||
| Health Status: Very Good | −0.06329 | 0.055621 | 0.010429 | 0.032753 | ||
| Health Status: Excellent | −0.06621 | 0.055073 | 0.020391 | 0.036883 | ||
| Age in Years | −0.00167 | ** | 0.000838 | −0.00038 | 0.00049 | |
| Female | −0.01384 | 0.018685 | −0.00395 | 0.013654 | ||
| Support Index | −0.02421 | * | 0.013894 | −0.01315 | 0.009072 | |
| Time with Primary MD | 0.003966 | 0.002655 | −0.00092 | 0.001801 | ||
| Time with Plan | 0.001263 | 0.002505 | −0.00555 | *** | 0.00184 | |
| Psychological Empowerment: Health Decline | ||||||
| Intercept | 0.081801 | 0.076348 | 0.042752 | 0.049683 | ||
| Empowered: Psych. | 0.057309 | ** | 0.02285 | 0.018052 | 0.013308 | |
| Small Health Decline | 0.050423 | 0.036263 | 0.010896 | 0.019529 | ||
| Large Health Decline | 0.170322 | *** | 0.03956 | 0.034483 | 0.025838 | |
| Emp*Small Decline | −0.13589 | * | 0.069248 | 0.014068 | 0.054069 | |
| Emp*Large Decline | 0.066901 | 0.122407 | −0.02263 | 0.078741 | ||
| Married | 0.043358 | * | 0.016981 | 0.013089 | 0.012038 | |
| Income | 0.014187 | *** | 0.005257 | −0.00058 | 0.003235 | |
| No. of Chronic Conditions | 0.02176 | 0.013458 | 0.020937 | *** | 0.006943 | |
| Medicaid Plan | 0.142688 | ** | 0.067182 | 0.088061 | 0.057354 | |
| Medicare Plan | 0.005501 | 0.040107 | 0.021219 | 0.025992 | ||
| Nongroup Plan | 0.008285 | 0.029736 | 0.076806 | ** | 0.03032 | |
| Plan Count | −0.0004 | 0.001788 | 0.001633 | 0.001183 | ||
| Black | 0.027692 | 0.031431 | 0.02247 | 0.016908 | ||
| Hispanic | 0.065201 | * | 0.038392 | 0.060795 | *** | 0.018576 |
| Asian | −0.06635 | 0.047372 | −0.0307 | 0.029673 | ||
| Other Race | 0.07462 | 0.047764 | 0.017444 | 0.023427 | ||
| Health Status: Fair | 0.01187 | 0.057468 | 0.009975 | 0.032713 | ||
| Health Status: Good | 0.013104 | 0.049064 | 0.002307 | 0.03216 | ||
| Health Status: Very Good | −0.01475 | 0.052948 | 0.02822 | 0.034082 | ||
| Health Status: Excellent | −0.01743 | 0.051742 | 0.036853 | 0.03664 | ||
| Age in Years | −0.00131 | 0.000822 | −0.00029 | 0.000496 | ||
| Female | −0.01175 | 0.016786 | −0.01041 | 0.015113 | ||
| Support Index | −0.01874 | 0.013951 | −0.01197 | 0.009148 | ||
| Time with Primary MD | 0.001577 | 0.002669 | −0.00126 | 0.001732 | ||
| Time with Plan | 0.000282 | 0.002336 | −0.00621 | *** | 0.001689 | |
| Psychological Empowerment: Number of Problems | ||||||
| Intercept | 0.054673 | 0.082519 | 0.02518 | 0.050986 | ||
| Empowered: Psych. | 0.010729 | 0.033596 | 0.014543 | 0.022001 | ||
| 2 to 3 Problems | 0.027339 | 0.02788 | 0.003358 | 0.014954 | ||
| 4 to 5 Problems | 0.064901 | 0.030214 | −0.00892 | 0.014961 | ||
| 6+ Problems | 0.181839 | *** | 0.03574 | 0.045546 | *** | 0.016189 |
| Emp*2 to 3 Problems | 0.054561 | 0.0455 | −0.00282 | 0.030841 | ||
| Emp*4 to 5 Problems | 0.0392 | 0.057216 | 0.010346 | 0.030706 | ||
| Emp*6+ Problems | 0.011958 | 0.066826 | 0.011794 | 0.042221 | ||
| Married | 0.045505 | ** | 0.019878 | 0.01255 | 0.012021 | |
| Income | 0.014065 | ** | 0.005585 | −0.0006 | 0.00323 | |
| No. of Chronic Conditions | 0.010063 | 0.013992 | 0.019872 | *** | 0.00673 | |
| Medicaid Plan | 0.188017 | ** | 0.078726 | 0.093124 | 0.058247 | |
| Medicare Plan | 0.014596 | 0.040778 | 0.020319 | 0.025533 | ||
| Nongroup Plan | 0.00252 | 0.033084 | 0.074143 | ** | 0.030146 | |
| Plan Count | −0.00054 | 0.001958 | 0.001627 | 0.00116 | ||
| Black | 0.01402 | 0.032055 | 0.021769 | 0.016982 | ||
| Hispanic | 0.050221 | 0.034848 | 0.059525 | *** | 0.018483 | |
| Asian | −0.0517 | 0.044439 | −0.02601 | 0.02835 | ||
| Other Race | 0.074192 | 0.050624 | 0.015395 | 0.023738 | ||
| Health Status: Fair | −0.00578 | 0.058004 | 0.011507 | 0.032384 | ||
| Health Status: Good | −0.01939 | 0.052236 | 0.004309 | 0.029998 | ||
| Health Status: Very Good | −0.04334 | 0.055581 | 0.032149 | 0.031494 | ||
| Health Status: Excellent | −0.03687 | 0.056606 | 0.042436 | 0.033576 | ||
| Age in Years | −0.00152 | 0.00088 | −0.00018 | 0.000504 | ||
| Female | 0.002846 | 0.016651 | −0.00892 | 0.014313 | ||
| Support Index | −0.01048 | 0.014982 | −0.00939 | 0.008859 | ||
| Time with Primary MD | 0.004416 | 0.002929 | −0.00102 | 0.001777 | ||
| Time with Plan | 0.001032 | 0.002468 | −0.00603 | *** | 0.00171 | |
| Psychological Empowerment: Dissatisfaction with Plan | ||||||
| Intercept | 0.150083 | * | 0.084068 | 0.037786 | 0.051001 | |
| Empowered: Psych. | 0.030527 | 0.040168 | 0.007017 | 0.021577 | ||
| Some Satisfaction with Plan | 0.006207 | 0.022042 | 0.020774 | 0.015054 | ||
| Some Dissatisfaction | 0.020221 | 0.034582 | 0.018693 | 0.018981 | ||
| Much Dissatisfaction | 0.152572 | *** | 0.034777 | 0.044797 | ** | 0.022109 |
| Emp*Some Satisfaction | 0.012574 | 0.053132 | 0.029888 | 0.034746 | ||
| Emp*Some Dissatisfaction | 0.058461 | 0.078943 | −0.0088 | 0.041729 | ||
| Emp*Much Dissatisfaction | −0.0302 | 0.076138 | −0.03246 | 0.039252 | ||
| Married | 0.046168 | ** | 0.01862 | 0.012703 | 0.012843 | |
| Income | 0.013855 | ** | 0.005919 | −0.00147 | 0.003475 | |
| No. of Chronic Conditions | 0.022156 | 0.013511 | 0.022523 | *** | 0.007125 | |
| Medicaid Plan | 0.120178 | 0.070569 | 0.097856 | 0.064235 | ||
| Medicare Plan | 0.018156 | 0.041123 | 0.025069 | 0.027475 | ||
| Nongroup Plan | 0.008511 | 0.030543 | 0.068648 | ** | 0.031236 | |
| Plan Count | −0.00035 | 0.001998 | 0.001809 | 0.001232 | ||
| Black | 0.033527 | 0.03301 | 0.024076 | 0.017373 | ||
| Hispanic | 0.057645 | 0.040246 | 0.062706 | *** | 0.019832 | |
| Asian | −0.07388 | 0.045919 | −0.03197 | 0.031591 | ||
| Other Race | 0.074393 | 0.050506 | 0.021132 | 0.025834 | ||
| Health Status: Fair | −0.04314 | 0.059038 | 0.005063 | 0.034891 | ||
| Health Status: Good | −0.05182 | 0.053364 | −0.00309 | 0.032251 | ||
| Health Status: Very Good | −0.08332 | 0.055434 | 0.022981 | 0.03343 | ||
| Health Status: Excellent | −0.09514 | * | 0.054419 | 0.034411 | 0.036196 | |
| Age in Years | −0.00192 | ** | 0.000801 | −0.00037 | 0.000505 | |
| Female | −0.00938 | 0.017517 | −0.00884 | 0.014207 | ||
| Support Index | −0.01765 | 0.013801 | −0.01272 | 0.009865 | ||
| Time with Primary MD | 0.002148 | 0.002874 | −0.00081 | 0.001798 | ||
| Time with Plan | 0.001827 | 0.002388 | −0.00588 | *** | 0.001788 | |
Note:
p < 0.10;
p < 0.05;
p < 0.01.
Endnotes
The following may be helpful to some readers: Diagnostic Term Description False positive Does not have a problem but responds Specificity True positive Has a problem and responds Sensitivity False negative Has a problem but does not respond Sensitivity True negative Does not have a problem and does not respond Specificity
Individuals were asked whether they experienced the following in the last twelve months: (1) Have you been unable to get medical care that you believed was needed? (2) Did you experience serious problems with the quality of your medical care? (3) Were you unable to get to see the specialist who was best for your condition? (4) Were you unable to get a specific medication that you needed? (5) Have you been told that your insurance did not cover a particular treatment or service that you needed? (6) Did you experience long delays in getting an appointment when you were sick? (7) Did you have a disagreement or misunderstanding about the type of treatment that you needed? (8) Did you experience delays in getting referrals to specialists? (9) Have you been asked to pay more for your medical services than you could afford? (10) Did you have a misunderstanding over which health services were covered by your insurance plan? (11) Did someone in the health care system treat you in a manner that was insensitive or disrespectful? (12) Did you have difficulty getting someone to answer your questions about your medical care? (13) Did you have difficulty getting someone to answer your questions about your health insurance? (14) Did you have problems with paperwork regarding billing or payment for services? (15) Did you have a health problem that got unexpectedly worse in a way that seriously affected your well-being?
References
- Abraham JM, Feldman R, Carlin C, Christianson J. The Effect of Quality Information on Consumer Health Plan Switching: Evidence from the Buyers Health Care Action Group. Journal of Health Economics. 2006;25(4):762–81. doi: 10.1016/j.jhealeco.2005.11.004. [DOI] [PubMed] [Google Scholar]
- Ai C, Norton EC. Interaction Terms in Logit and Probit Models. Economics Letters. 2003;80:123–29. [Google Scholar]
- Annas GJ. Patients’ Rights in Managed Care—Exit, Voice, and Choice. New England Journal of Medicine. 1997;337(3):210–15. doi: 10.1056/NEJM199707173370323. [DOI] [PubMed] [Google Scholar]
- Beaulieu ND. Quality Information and Consumer Health Plan Choices. Journal of Health Economics. 2002;21(1):43–63. doi: 10.1016/s0167-6296(01)00126-6. [DOI] [PubMed] [Google Scholar]
- Chernew M, Scanlon DP. Health Plan Report Cards and Insurance Choice. Inquiry. 1998;35:9–22. [PubMed] [Google Scholar]
- Cooper BS, Vladeck BC. Perspective: Bringing Competitive Pricing to Medicare. Health Affairs. 2000;19(5):49–54. doi: 10.1377/hlthaff.19.5.49. [DOI] [PubMed] [Google Scholar]
- Cunningham PJ, Kohn L. Health Plan Switching: Choice or Circumstance? Health Affairs. 2000;19(3):158–64. doi: 10.1377/hlthaff.19.3.158. [DOI] [PubMed] [Google Scholar]
- Dranove D, Sfekas A. Start Spreading the News: A Structural Estimate of the Effects of New York Hospital Report Cards. Journal of Health Economics. 2008;27(5):1201–7. doi: 10.1016/j.jhealeco.2008.03.001. [DOI] [PubMed] [Google Scholar]
- Gabel JR, Lo Sasso AT, Rice T. Consumer-Driven Health Plans: Are They More Than Talk Now? Health Affairs. 2002 doi: 10.1377/hlthaff.w2.395. web exclusive. Available at http://content.healthaffairs.org/cgi/content/full/hlthaff.w2.395v1/DC1accessed July 9, 2009. [DOI] [PubMed] [Google Scholar]
- Goold SD, Klipp G. Managed Care Members Talk about Trust. Social Science & Medicine. 2002;54(6):879–88. doi: 10.1016/s0277-9536(01)00070-3. [DOI] [PubMed] [Google Scholar]
- Hanoch Y, Rice T. Can Limiting Choice Increase Social Welfare? The Elderly and Health Insurance. The Milbank Quarterly. 2006;84(1):37–73. doi: 10.1111/j.1468-0009.2006.00438.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havlin LJ, McAllister MF, Slavney DH, Studer Q. How to Inject Consumerism into Your Existing Health Plans: How Healthcare Wins with Consumers Who Want More. Employee Benefits Journal. 2003;28(3):7–14. [PubMed] [Google Scholar]
- Hibbard JH, Berkman N, McCormack LA, Jael E. The Impact of a CAHPS Report on Employee Knowledge, Beliefs, and Decisions. Medical Care Research and Review. 2002;59(1):104–16. doi: 10.1177/107755870205900106. [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Greene J, Tusler M. Plan Design and Active Involvement of Consumers in Their Own Health and Healthcare. American Journal of Managed Care. 2008;14(11):729–36. [PubMed] [Google Scholar]
- Hibbard JH, Jewett JJ, Engelmann S, Tusler M. Can Medicare Beneficiaries Make Informed Choices? Health Affairs. 1998;17(6):181–93. doi: 10.1377/hlthaff.17.6.181. [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Jewett JJ, Legnini MW, Tusler M. Choosing a Health Plan: Do Large Employers Use the Data? Health Affairs. 1997;16(6):172–80. doi: 10.1377/hlthaff.16.6.172. [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Stockard J, Tusler M. Hospital Performance Reports: Impact on Quality, Market Share, and Reputation. Health Affairs(Millwood) 2005;24(4):1150–60. doi: 10.1377/hlthaff.24.4.1150. [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Weeks EC. Consumerism in Health Care: Prevalence and Predictors. Medical Care. 1987;25(11):1019–32. doi: 10.1097/00005650-198711000-00001. [DOI] [PubMed] [Google Scholar]
- Hirschman AO. Exit, Voice, and Loyalty: Responses to the Decline of Firms, Organizations and States. Cambridge, Mass: Harvard University Press; 1970. [Google Scholar]
- Hirschman AO. Exit, Voice, and Loyalty: Further Reflections and a Survey of Recent Contributions. The Milbank Memorial Fund Quarterly/Health and Society. 1980;58(3):430–53. [PubMed] [Google Scholar]
- Kaiser Family Foundation. National Survey of Consumer Experiences with Health Plans. Menlo Park, Calif.: Kaiser Family Foundation; 1999. [Google Scholar]
- Kaiser Family Foundation and Agency for Healthcare Research and Quality. National Survey on Consumers' Experiences with Patient Safety and Quality Information. Menlo Park, Calif.: Kaiser Family Foundation; 2004. [Google Scholar]
- Kaiser Family Foundation and Agency for Healthcare Research and Quality. 2006 Update on Consumers’ Views of Patient Safety and Quality Information. Menlo Park, Calif.: Kaiser Family Foundation; 2006. [Google Scholar]
- Klinkman MS. The Process of Choice of Health Care Plan and Provider: Development of an Integrated Analytic Framework. Medical Care Review. 1991;48(3):295–330. doi: 10.1177/002570879104800304. [DOI] [PubMed] [Google Scholar]
- Kolodinsky J. A System for Estimating Complaints, Complaint Resolution and Subsequent Purchases of Professional and Personal Services. Journal of Consumer Satisfaction, Dissatisfaction and Complaining Behavior. 1992;5:36–44. [Google Scholar]
- Kolodinsky J. Complaints, Redress, and Subsequent Purchases of Medical Services by Dissatisfied Consumers. Journal of Consumer Policy. 1993;16:193–214. [Google Scholar]
- Lake T, Kvam C, Gold M. Literature Review: Using Quality Information for Health Care Decisions and Quality Improvement. Washington, D.C.: Mathematic Policy Research; 2005. [Google Scholar]
- Lubalin JS, Harris-Kojetin LD. What Do Consumers Want and Need to Know in Making Health Care Choices? Medical Care Research and Review. 1999;56(suppl. 1):67, 102. doi: 10.1177/1077558799056001S04. discussion 103–12. [DOI] [PubMed] [Google Scholar]
- Marshall MN, Shekelle PG, Davies HT, Smith PC. Public Reporting on Quality in the United States and the United Kingdom. Health Affairs(Project Hope) 2003;22(3):134–48. doi: 10.1377/hlthaff.22.3.134. [DOI] [PubMed] [Google Scholar]
- Meier KJ. The Political Economy of Consumer Protection: An Examination of State Legislation. Western Political Quarterly. 1987;40(2):345–59. [Google Scholar]
- Miller TE. Center Stage on the Patient Protection Agenda: Grievance and Appeal Rights. Journal of Law, Medicine and Ethics. 1998;26:89–99. doi: 10.1111/j.1748-720x.1998.tb01665.x. [DOI] [PubMed] [Google Scholar]
- Mobley LR, McCormack LA, Wang J, Squire C, Kenyon A, Lynch JT, Heller A. Voluntary Disenrollment from Medicare Advantage Plans: Valuable Signals of Market Performance. American Journal of Managed Care. 2007;13(12):677–84. [PubMed] [Google Scholar]
- Mulcahy L, Tritter JQ. Pathways, Pyramids and Icebergs? Mapping Links between Dissatisfaction and Complaints. Sociology of Health and Illness. 1998;20(6):825–47. [Google Scholar]
- National Academy of State Health Policy (NASHP) Medicaid Managed Care: A Guide from the States. Portland, Maine: 2001. [Google Scholar]
- Neuman P, Langwell KM. Medicare's Choice Explosion? Implications for Beneficiaries. Health Affairs. 1999;18(1):150–60. doi: 10.1377/hlthaff.18.1.150. [DOI] [PubMed] [Google Scholar]
- Nichols LM, Ginsburg PB, Berenson RA, Christianson J, Hurley RE. Are Market Forces Strong Enough to Deliver Efficient Health Care Systems? Confidence Is Waning. Health Affairs. 2004;23(2):8–21. doi: 10.1377/hlthaff.23.2.8. [DOI] [PubMed] [Google Scholar]
- Riley GF, Ingber MJ, Tudor CG. Disenrollment of Medicare Beneficiaries from HMOs. Health Affairs. 1997;16(5):117–24. doi: 10.1377/hlthaff.16.5.117. [DOI] [PubMed] [Google Scholar]
- Robinson JC, Gardner LB. Involuntary Health Plan Switching: Case Study of a Corporate Health Benefits Program. Medical Care Research and Review. 1996;52(2):225–39. doi: 10.1177/107755879605300206. [DOI] [PubMed] [Google Scholar]
- Rodwin M. Consumer Voice and Representation in Managed Healthcare. Journal of Health Law. 2001;34(2):223–76. [Google Scholar]
- Rosenthal M, Schlesinger M. Not Afraid to Blame: The Neglected Role of Blame Attribution in Medical Consumerism and Some Implications for Health Policy. The Milbank Quarterly. 2002;80(1):41–95. doi: 10.1111/1468-0009.00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scanlon DP, Chernew M, McLaughlin C, Solon G. The Impact of Health Plan Report Cards on Managed Care Enrollment. Journal of Health Economics. 2002;21(1):19–41. doi: 10.1016/s0167-6296(01)00111-4. [DOI] [PubMed] [Google Scholar]
- Schlesinger M. The Canary in the Gemeinschaft: The Public Voice of Patients as a Means of Enhancing Health System Performance. In: Grob R, Hoffman B, Schlesinger M, Tomes N, editors. Impatient Voices: Patients as Actors in U.S. Health Care. New Brunswick, N.J.: Rutgers University Press; Forthcoming. [Google Scholar]
- Schlesinger M, Druss B, Thomas T. No Exit? The Effect of Health Status on Dissatisfaction and Disenrollment from Health Plans. Health Services Research. 1999;34(2):547–76. [PMC free article] [PubMed] [Google Scholar]
- Schlesinger M, Mitchell S, Elbel B. Voices Unheard: Barriers to Expressing Dissatisfaction to Health Plans. The Milbank Quarterly. 2002;80(4):709–55. doi: 10.1111/1468-0009.00029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlesinger M, Mitchell S, Gray BH. Public Expectations of Nonprofit and For-Profit Ownership in American Medicine: Clarifications and Implications. Health Affairs(Project Hope) 2004a;23(6):181–91. doi: 10.1377/hlthaff.23.6.181. [DOI] [PubMed] [Google Scholar]
- Schlesinger M, Mitchell S, Gray BH. Restoring Public Legitimacy to the Nonprofit Sector: A Survey Experiment Using Descriptions of Nonprofit Ownership. Nonprofit and Voluntary Sector Quarterly. 2004b;33(4):673–710. [Google Scholar]
- Silberman P, Poley S, James K, Slifkin R. Tracking Medicaid Managed Care in Rural Communities: A Fifty-State Follow-Up. Health Affairs. 2002;21(4):255–63. doi: 10.1377/hlthaff.21.4.255. [DOI] [PubMed] [Google Scholar]
- Sofaer S. Navigating Poorly Charted Territory: Patient Dilemmas in Health Care Nonsystems. Medical Care Research and Review. 2009;66(1):75S–93S. doi: 10.1177/1077558708327945. [DOI] [PubMed] [Google Scholar]
- Stevenson DG. Is a Public Reporting Approach Appropriate for Nursing Home Care? Journal of Health Politics, Policy and Law. 2006;31(4):773–810. doi: 10.1215/03616878-2006-003. [DOI] [PubMed] [Google Scholar]
- Tapay N, Feder J, Dallek G. Protection for Consumers in Managed Care Plans: A Comparison of Medicare, Medicaid, and the Private Insurance Market. Menlo Park, Calif.: Kaiser Family Foundation; 1998. [Google Scholar]
- Thorpe KE. The Rise in Health Care Spending and What to Do about It. Health Affairs(Project Hope) 2005;24(6):1436–45. doi: 10.1377/hlthaff.24.6.1436. [DOI] [PubMed] [Google Scholar]
- Toner R. Biggest Divide? Maybe It's Health Care. 2004. The New York Times, May 14. Available at http://www.nytimes.com/2004/05/14/politics/campaign/14health.html?ex=1399953600&en=3c17777767870fd7&ei=5007&partner=USERLANDaccessed August 12, 2009.
- Tumlinson A, Bottigheimer H, Mahoney P, Stone EM, Hendricks A. Choosing a Health Plan: What Information Will Consumers Use? Health Affairs (Project Hope) 1997;16(3):229–38. doi: 10.1377/hlthaff.16.3.229. [DOI] [PubMed] [Google Scholar]
- Uhrig J, Short P. Testing the Effect of Quality Reports on the Health Plan Choices of Medicare Beneficiaries. Inquiry. 2002;39(4):355–71. doi: 10.5034/inquiryjrnl_39.4.355. /2003. [DOI] [PubMed] [Google Scholar]
- Vaiana M, McGlynn E. What Cognitive Science Tells Us about the Design of Reports from Consumers. Medical Care Research and Review. 2002;59(1):3–35. doi: 10.1177/107755870205900101. [DOI] [PubMed] [Google Scholar]
- White House. 2009. Health Care. Available at http://www.whitehouse.gov/issues/health_care/accessed June 19, 2009.
- Webb B. A Study of Complaints by Patients of Different Age Groups in an NHS Trust. Nursing Standard(Royal College of Nursing) 1995;9(42):34–37. doi: 10.7748/ns.9.42.34.s36. [DOI] [PubMed] [Google Scholar]
- Wedig GJ, Tai-Seale M. The Effect of Report Cards on Consumer Choice in the Health Insurance Market. Journal of Health Economics. 2002;21(6):1031–48. doi: 10.1016/s0167-6296(02)00075-9. [DOI] [PubMed] [Google Scholar]