Abstract
Objective
Current research suggests that older cancer patients report less distress compared to younger cancer patients. However, this research has generally not teased apart the differences between general distress, anxiety, and depression.
Methods
We conducted a secondary analysis of merged datasets using cross-sectional data on 736 men with prostate cancer (Mean Age 68±10 years of age, range 50 to 93). Approximately half the participants were recruited from doctors’ offices throughout the United States and the other half from Memorial Sloan-Kettering Cancer Center (New York, NY). Participants were asked to complete the Distress Thermometer, the Hospital Anxiety and Depression Scale (HADS), the FACT-P Quality of Life questionnaire, and a demographic questionnaire.
Results
Aging was related to reduced distress (r=−0.14), less anxiety (r=−0.22), and increased emotional quality of life (r= 0.16). In contrast, aging was associated with greater depressive symptoms in these cancer patients (r= 0.18). The mean depression scores of 5-year cohorts consistently trended upward. The significant association between age and depression remained after controlling for stage of disease, hormone therapy use, time since diagnosis, and social, physical and functional well-being.
Conclusions
Despite theoretical and empirical evidence that older cancer patients may cope more effectively than younger cancer patients, depressive symptoms remain an important concern for aging cancer patients and greater attention to this area is warranted. The increase in depression is in contrast to some findings in the general aging literature, raising the possibility that this trend is unique to older cancer patients.
Keywords: Psychological distress, Depression, Anxiety, Prostate Cancer, Aging
Introduction
Aging issues in cancer are becoming more prominent as age projections suggest the number of geriatric cancer patients will increase in the next 20 to 30 years. Currently, the elderly comprise 61% of cancer survivors1, while 60% of new cancer diagnoses and 70% of cancer deaths occur in people over the age of 65. For the elderly, there are a number of physical and social factors that may compound a diagnosis of cancer, making it more difficult to cope, contemplate different treatment options, and deal with the side effects of these treatments.
With the difficulties associated with aging, it may not be surprising that depression is relatively common among the elderly. Physically healthy older individuals experience significant levels of depression (10–20% in the community and primary care settings2). Among the elderly with chronic illness, depression (15–25% or greater in medically ill groups2) often interferes with the ability to make treatment decisions and adhere to lengthy treatment regimens3–7. A diagnosis of cancer is often accompanied by an increase in distress, depressive symptoms, and uncertainty 8,9. For older patients, the presence of physical aging-related problems, co-morbid medical conditions, and their symptom burden, can overwhelm their coping ability, potentially leading to increased vulnerability to distress, anxiety, and depression10, 11.
Despite this increased vulnerability, initial research has shown that younger adults with cancer have a higher risk of reporting psychological distress than older adults with cancer.9,12 Although there is still relatively little research on the effects of aging on cancer and survivorship, age appears to be related to the overall cancer experience 9, 13, 14, 15. To illustrate, in a study of psychological distress in ovarian cancer patients, all women in the sample experienced a significant amount of anxiety, however younger patients experienced more distress than older patients16. Younger cancer survivors have been found to be more negatively affected by the cancer experience than older adults, and are more likely to change their resulting behaviors because of it. 9, 17, 18
Some authors have suggested that age may serve as a protective factor against psychological distress related to cancer9. Blank and Bellizzi outline three broad theories which help explain why older patients may handle a cancer diagnosis better than younger patients 9. The three theories are 1) Erikson’s psychosocial theory, focusing specifically on increased wisdom in later adulthood; 2) specific developmental tasks such as shorter time perspective for goals, and 3) different life trajectories and experiences. As individuals age, they often become more inwardly-focused,19, 20; develop a shortened time horizon 21, become more selective in their goals aimed at improving emotion regulation and prioritization; and are better able to manage their emotions22–24. Taken together, these perspectives provide a theoretical explanation as to why older cancer patients report lower distress than younger adults with cancer, and may be better equipped to deal with the psychological distress associated with this new life challenge.
The literature to date has examined the differences between younger and older cohorts of patients. Yet, there has been little research focusing on how distress is related to age within an older cohort of patients. In addition, previous research has generally examined “distress” as opposed to distinguishing the differences among anxiety, depression, and distress. This is not surprising since there is often a lack of clarity in the literature about what is meant by “distress” or “emotional well-being.” Distress is generally considered to be a combination of feelings such as worry, anxiety, fear, and depression. The most common assessment of distress is an efficient one-question screen (i.e. The Distress Thermometer) which is used to determine if further evaluation should be considered25. Emotional-well being is commonly assessed within quality-of-life measures, and like distress, also combines the constructs of anxiety and depression 26. Emotional well-being scales are usually longer (around 4 or 5 questions) and are considered more psychometrically sound as compared to the one-question distress measures. Although these concepts and scales are useful for indentifying general distress, they lack the ability to make the distinction between anxiety and depression. We believe this distinction is important in order to assist clinicians to better understand and treat psychological difficulties in this population.
Given that there are over 180,000 men diagnosed with prostate cancer and over 30,000 deaths occur from the disease on a yearly basis 27, it is important to aim research efforts at examining the role of psychological distress, anxiety, and depression in this group. Based on the literature reported above, we hypothesized that distress, anxiety and depression would decrease as patients grow older, whereas emotional well-being would increase across these age ranges.
METHODS
Participants
The study is a secondary analysis of the combination of two separate samples, both investigating distress, anxiety, and depression in men with early and late-stage prostate cancer. The first database (as previously described in Roth et al., 2003), consists of data from 385 men diagnosed with prostate cancer who were recruited from genitourinary clinics throughout the United States 28. The second database (as described in Roth et al., 2006) is based on 367 men drawn from the Urologic and Genito-Urinary Medical Oncology clinics at Memorial Sloan-Kettering Cancer Center 29.
When combining both databases, 752 subjects were available for this pool. Of these subjects, 16 subjects were missing data on one or more of the measures used in this study, and as a result, 736 participants were included in the analysis. The eligibility requirements for both studies included English fluency, diagnosis of prostate cancer, age greater than 18 years, and monitoring of prostate serum antigen (PSA) levels. Men who met these requirements were informed of the risks and benefits of study participation and provided written informed consent.
Procedure
Patients who met the eligibility criteria stated above were asked to complete a series of seven self-report questionnaires as they waited for their doctor’s visit. The questionnaires were completed before they received the results of their PSA test for that specific visit. Data from four of these questionnaires were analyzed in this study: The Distress Thermometer 25, the Functional Assessment of Cancer Therapy Scale-Prostate Cancer Version (FACT-P) 26, the Hospital Anxiety and Depression Scale (HADS) 30, and a demographics questionnaire which included treatment course and co-morbidities.
The Distress Thermometer is a 1-item visual analog scale (picture of thermometer), which asks patients to rate their distress on a 0 to 10 scale with higher numbers indicating more distress. The FACT-P is a questionnaire consisting of a 27-item quality-of-life scale (FACT-G) 31, 32, divided into four groups (Physical Well-Being, Social/Family Well-Being, Emotional Well-Being, and Functional Well-Being), and 12 items specific to prostate cancer 26. The HADS is a 14-item questionnaire with two 7-item Depression and Anxiety sub-scales.
Statistical Analysis
Descriptive statistics were reported for the demographic information. Correlation coefficients were calculated for the relationship between age and psychological variables. We divided the sample into 5-year cohorts to graph the relationship between age and the mean scores of the study variables. Multiple regression was used to control for potential confounding variables.
RESULTS
Participant Characteristics
The average age of the 736 prostate cancer patients was 68±10 (50 to 93) years of age. The majority of the sample was Caucasian (88%), while 8% were African-American 2% were Hispanic, 1% identified as Asian, and 1% identified as “Mixed.” Most participants were married (83%), and 58% had at least a college degree. Approximately sixty percent of the sample had early stage prostate cancer (58%) and the mean time since diagnosis was 4.5± 4 years.
Relationship among age, distress, emotional well-being, anxiety, and depression
Aging was related to reduced distress as measured by the Distress Thermometer (r=−0.14, p < 0.01), lower scores on the HADS Anxiety subscale (r=−0.22, p < 0.01), and higher scores on the FACT-P Emotional Quality of Life subscale quality (r= 0.16, p < 0.01). In contrast, aging was associated with greater scores on the HADS Depression subscale in these cancer patients (r= 0.18, p < 0.01).
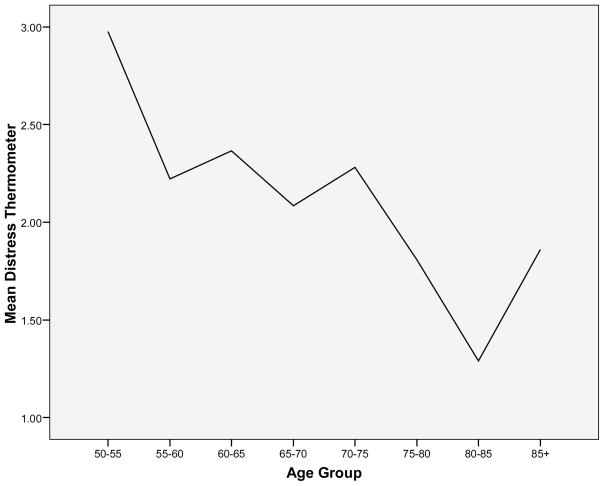
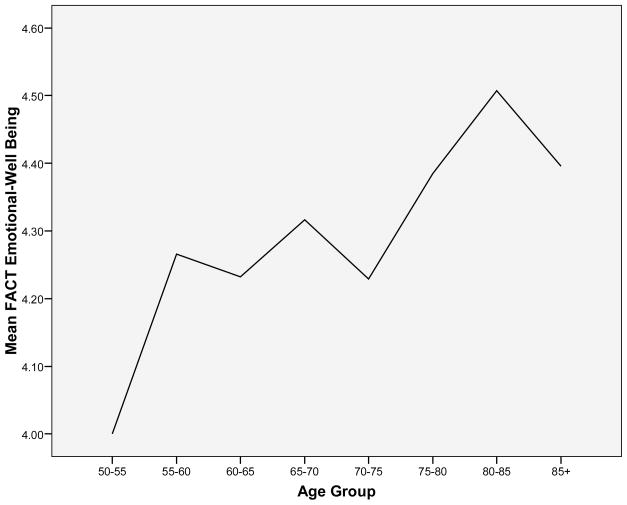
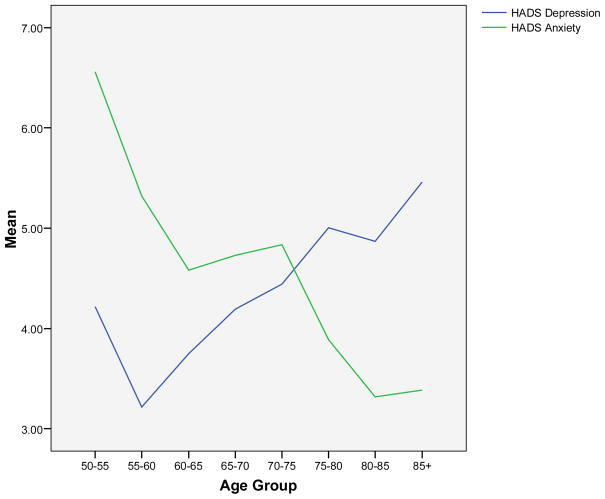
To graphically illustrate these relationships, we divided the sample into 5-year cohorts. The specific age cohort and number of subjects in each cohort are displayed in Table 1. We then graphed the relationship between age and the mean scores for each 5-year cohort for each variable. Figure 1 and Figure 2 display the relationship between age and Distress Thermometer scores, and age and FACT-P Emotional Well-Being scores, respectively. The relationship between Age and the HADS Anxiety and Depression scales are depicted in Figure 3.
Table 1.
Age cohorts and number of subjects in each cohort.
| Age Cohort | N |
|---|---|
| 50 to 54 | 44 |
| 55 to 69 | 95 |
| 60 to 64 | 112 |
| 65 to 79 | 150 |
| 70 to 74 | 141 |
| 75 to 79 | 102 |
| 80 to 84 | 46 |
| 85 to 93 | 26 |
Figure 1.
Age and Mean Distress Thermometer Scores
Figure 2.
Age and FACT Emotional-Well Being Subscale
Figure 3.
Age and HADS Depression/Anxiety Scale
Since we were most interested in anxiety and depression, and the notion that anxiety decreases while depression increases seemed most incongruent with initial assumptions, we decided to focus on anxiety and depression in multivariate analyses. We selected potential confounding variables by reviewing the literature in cancer, and where possible specifically in prostate cancer, that identified variables that have a potential relationship with anxiety and depression33–36. These variables are: stage of disease, hormone therapy, time since diagnosis, social networks, physical function, and loss of functional ability. As such, along with age, we included stage of disease (early vs. late), use of hormone therapy (currently using hormone therapy or history of hormone therapy vs. other), time since diagnosis, the FACT Social Well-Being subscale, the FACT Physical Well-Being subscale, and the FACT Functional subscale in two multiple regression analyses, one predicting anxiety and the other predicting depression. When predicting anxiety scores, the regression equation was significant (F= 38.69, p < 0.01) and explained 31% of the variance in anxiety scores. Importantly, age remained a significant predictor of anxiety scores (standardized beta = −0.23, p <0.01) and accounted for 5% of the variance in anxiety scores (i.e. change in R2). The other significant variables were FACT Social and FACT Functional. FACT Functional was the strongest predictor explaining 11% of the variance in anxiety scores. The variables that were not significant predictors were disease stage, hormone therapy, time since diagnosis, and FACT Physical. When predicting depression scores, the regression equation was also significant (F = 54.80, p < 0.01) and explained 39% of the variance in depression scores. Importantly, age remained a significant predictor of depression in this equation (standardized beta=0.18, p < 0.01) accounting for 3% of the variance in depression scores. The other variables that were significant predictors were disease stage, FACT Physical, and FACT Functional. Again, FACT Functional was the strongest predictors explaining 15% of the variance. The variables that were not significant in this model were hormone therapy, time since diagnosis, and FACT Social.
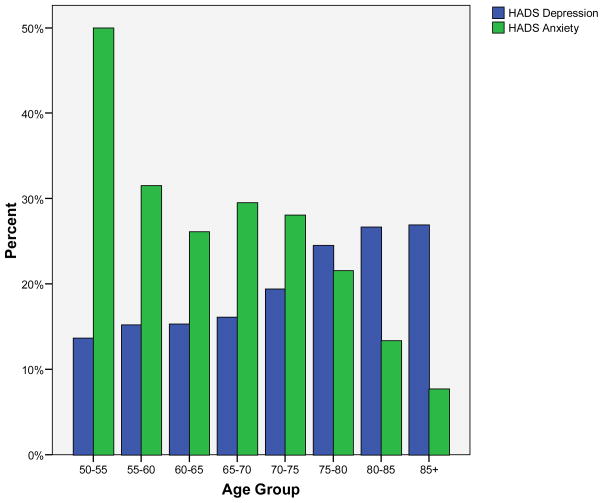
We were also interested in understanding if these trends in anxiety and depression were clinically meaningful. Figure 4 displays the percentage of men scoring at or above the cutoff score of 7 to indicate clinically meaningful levels of anxiety or depression on the HADS subscales. Cutoff scores of 7 and 8 have both been proposed for the HADS subscales 37. We choose the lower cutoff score because our work in defining clinically meaningful cutoff scores suggests that lower scores on the HADS depression subscale are more accurate in predicting depressive symptoms for those 70 years of age and older38. As depicted in Figure 4, the percentage of men scoring over the cutoff for anxiety consistently decreases with age, while those scoring above the cutoff for depression consistently increases with age.
Figure 4.
Percentage who meet cut-off scores of ≥ 7
When examining both the means of anxiety and depression (Figure 3) and those scoring above the designated cut-off (Figure 4), a shift from anxiety to depression seems to occur at age 75. Before age 75, the percent scoring above the cutoff for anxiety is higher than depression. After 75, this shifts, and percentages are higher for depression than anxiety. We used this natural separation point to assess if this change in those scoring above the cutoffs was statistically significant. The percentage of men who scored above the cutoff for anxiety who were under the age of 75 was higher than those over 75 (31% vs. 17%, χ2 = 11.97, p < .01). For depression, less men scored above the cutoff score who were under age of 75 than those who were older than 75 (17% vs. 25%, χ2 = 6.81, p < .01).
Discussion
The current study helps clarify the relationship between age and psychological variables such as distress, anxiety and depression within a sample of older prostate cancer patients. Results support a pattern suggesting overall distress and anxiety decreased with age, whereas depressive symptoms significantly and consistently increased with age. Additionally, emotional well-being increased with age. These findings in a sample of men with prostate cancer elucidate how age may be related to anxiety, depression and distress in a consistent and predictable fashion. The strength of the relationships reported here are considered small (i.e., correlations between 0.14 to 0.22, and age accounted for between 3 and 5% of the variance in anxiety and depression scores), however the fact that age remains a significant predictor of anxiety and depression after controlling for multiple variables including functional well-being in older cancer patients lends support for the significance of these findings.
When placing these findings in the context of cancer, these results are important and potentially surprising because current research suggests that older cancer patients report lower levels of psychological distress than younger cancer patients9. A natural conclusion from this literature supports the focusing of psychosocial services toward younger cancer patients. However, this literature has generally not teased apart the differences between general distress, anxiety, and depression, and has not looked within an aging sample. Our data suggest that older cancer patients report less distress and anxiety in addition to improved emotional well-being as they age. It is also important to note that the Distress Thermometer is used as a clinical screening tool, and the subscale of QOL measures that assesses emotional well-being are often used in research as a primary measure of the psychological state of cancer patients. From the data presented in this analysis, it appears that distress and emotional well-being are loading more on anxiety than depression. In fact, of the 5 questions on the FACT Emotional Well-being scale, 3 assess anxiety symptoms, 1 assesses sadness, and 1 assesses hope. These primary assessment tools may be distracting attention from increased depression, potentially masking the need for services for older cancer patients.
It is also surprising to see the crossover between anxiety and depressive symptoms as these two symptoms are generally thought to be co-morbid39. As stated in the introduction, older adults as compared to younger adults demonstrate better emotion regulation, a more generative perspective, and a shifting of goals19, 21, 40. Of note, there appears to be a larger emphasis on an inwardly-focused rather than externally-focused perspective in later adulthood 22. Thus, it may be possible that as cancer patients age, they become more inwardly focused and reduce their interaction and responsibilities with the external world. This implies that not only do the issues related to cancer (e.g., cancer diagnosis, fear of recurrence, deciding on treatment, coping with the lasting side effects of treatment) impact older cancer patients differently than younger cancer patients, but also that older cancer patients may have developed a distinct way of coping with these issues. For older cancer patients decreasing emphasis on externally-focused perspective may explain the reduction in anxiety and general distress (e.g., cancer has less impact on work, family responsibilities, other activities related to external responsibilities), yet the inward focus and less interaction with the outside world may leave older cancer patients alone in coping with a cancer diagnosis, fear of recurrence, deciding on cancer treatments, and managing the side effects of treatment. The general result for older cancer patients may be increased susceptibility to depressive symptoms as opposed to younger cancer patients.
Theses data also support the important emphasis on depression in the general aging literature. The aging literature indicates that depression is one of the most frequent causes of emotional distress in older adults and is one of the top five concerns faced by the elderly today 41, 42. Given that the average time since diagnosis for men in this analysis was 4.5 years post diagnosis, it is important to compare these results to those in the general literature on age and psychological adjustment. However, the literature examining changes in depression and anxiety by age has produced inconsistent results with a number of studies supporting the hypothesis of improved psychological adjustment as adults grow older43–49. For example, in a comprehensive review of epidemiologic studies across the life span, Jorm (2000) concludes that aging seems to be associated with a decreased susceptibility to distress, anxiety, and depression, measuring each construct separately.44 Scott et al. (2008) reported in a sample of over 42,000 adults worldwide that depression and anxiety disorders decreased from the ages of 50 to 90 despite the prevalence of chronic physical or pain conditions in older adults43. Nguyen et al (2006) report in a sample of over 2,000 subjects, depressive affect as measured by the CES-D remained stable for those over 70 years of age46. When comparing our results to this general aging literature, it is possible that our results (i.e., increasing depression with decreasing anxiety) may be unique to cancer. Despite the time since diagnosis in this sample of 4.5 years, issues of fear of recurrence, coping with side effects of treatment, and disease advancement may require continued treatment based on their psychological impact on this sample. This conclusion would only highlight the need for increased attention on depressive symptoms in older cancer patients. However, we cannot conclude this with certainty as our study does not include an age-matched comparison group without cancer. In addition, since prostate cancer is a disease of older men (70% diagnosed are over the age of 65) these data do not include younger adults. Despite this, the principal aim of this analysis is to help understand the primary psychological concerns of cancer patients within a sample of aging patients as opposed to determining if these results are unique to this population.
In view of these results, we specifically suggest oncologists focus on effective screening and diagnosis of depression in this population. Unfortunately, diagnosing depression in older cancer patients can be specifically challenging50. Depression and depressive symptoms are generally underdiagnosed in both cancer patients and older adults 41. One primary difficulty in recognizing depression in cancer patients is that many symptoms of cancer and side effects of treatment overlap with the symptoms of depression. For example, significant weight loss, sleep problems, fatigue/anergia, difficulty concentrating, and thoughts of suicide may be either symptoms of depression or symptoms of cancer and/or its accompanying treatment side effects. A challenge in diagnosing depression in older adults is that older adults tend to report fewer cognitive symptoms such as self-criticism, guilt, and sense of failure and more somatic symptoms of depression such as sleep problems and stomach aches than do younger adults. 51, 52, 53, 54 We suggest first assessing the gateway symptoms of depression (i.e. anhedonia and depressed mood), then attempting to differentiate symptoms of depression from the cancer itself, and lastly, focusing on novel symptoms that may be unique to depression and not cancer such as patients’ general malaise, diffuse somatic complaints, hopelessness, and mood variation (see Weinberger, Roth and Nelson, 2009 for a more thorough review). Thus, recognizing depression in older cancer patients combines the difficulty of diagnosing depression in both cancer and in the aging, which decreases the chance of proper recognition and treatment.
Of note for clinicians who work with men with prostate cancer, anxiety has always been a major concern for these men 28. In fact, our work has discussed how anxiety tends to be the most often experienced psychological symptom for men with prostate cancer, as estimates of anxiety in men with prostate cancer have hovered around 33%, while depression has been estimated between 12 and 15% 35. The data from this current study indicates that for men with prostate cancer over the age of 75, there may be a shift with a greater percentage of men reporting depressive symptoms as opposed to symptoms of anxiety.
This study is notwithstanding limitations. The current study was a cohort design. so even though age differences were found, longitudinal work will be necessary to further test these relationships. Since the sample for the current study was older prostate cancer patients, the results may not generalize to women, or younger patients with other types of cancers. Future research should aim to test age differences with both women and men. In addition, there was no formal assessment of cognition, and cognition has been found to correlate with depression in late life. However, all participants in the study were able to comprehend the informed consent and complete the packet of questions without any assistance. Thus, we believe there were no individuals with moderate to gross cognitive deficits.
Conclusion
The current study helps clarify the relationships between age and psychological variables such as distress, anxiety and depression within a sample of older prostate cancer patients. Results support a clear pattern of how overall distress and anxiety decreased with age, whereas depressive symptoms significantly and consistently increased with age. Continued research is needed to explore the association between age and psychological variables in a more varied sample and in a longitudinal fashion. In sum, clinicians should be aware that older cancer patients may display reduced distress and anxiety, yet still be struggling with depressive symptoms.
Learning Objectives
Identify how aging affects anxiety, depression and quality of life
State two potential explanations for a tradeoff between anxiety and depression in older prostate cancer patients
Compare the literature on depression in general aging populations versus an aging cancer population
References
- 1.IOM. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington: The National Academies Press; 2007. [Google Scholar]
- 2.Lyness JM. Treatment of Depressive Conditions in Later Life: Real-World Light for Dark (or Dim) Tunnels. JAMA. 2004;291:1626–8. doi: 10.1001/jama.291.13.1626. [DOI] [PubMed] [Google Scholar]
- 3.Katon W, Lin E, Kroenke K. The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. General Hospital Psychiatry. 2007;29:147–55. doi: 10.1016/j.genhosppsych.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 4.Katon W, Unutzer J. Collaborative Care Models for Depression: Time to Move From Evidence to Practice. Arch Intern Med. 2006;166:2304–6. doi: 10.1001/archinte.166.21.2304. [DOI] [PubMed] [Google Scholar]
- 5.Katon W, Sullivan M. Depression and chronic medical illness. Journal of Clinical Psychiatry. 1990;51:3–34. [PubMed] [Google Scholar]
- 6.Katon WJ, Schoenbaum M, Fan M-Y, et al. Cost-effectiveness of Improving Primary Care Treatment of Late-Life Depression. Arch Gen Psychiatry. 2005;62:1313–20. doi: 10.1001/archpsyc.62.12.1313. [DOI] [PubMed] [Google Scholar]
- 7.Reynolds CF, III, Dew MA, Lenze EJ, Whyte EM. Preventing Depression in Medical Illness: A New Lead? Arch Gen Psychiatry. 2007;64:884–5. doi: 10.1001/archpsyc.64.8.884. [DOI] [PubMed] [Google Scholar]
- 8.Ullrich PM, Carson MR, Lutgendorf SK, Williams RD. Cancer fear and mood disturbance after radical prostatectomy: consequences of biochemical evidence of recurrence. J Urol. 2003;169:1449–52. doi: 10.1097/01.ju.0000053243.87457.60. [DOI] [PubMed] [Google Scholar]
- 9.Blank TO, Bellizzi KM. A gerontologic perspective on cancer and aging. Cancer. 2008;112:2569–76. doi: 10.1002/cncr.23444. [DOI] [PubMed] [Google Scholar]
- 10.Kurtz M, Kurtz J, Stommel M, Given C, Given B. Physical Functioning and Depression Among Older Persons with Cancer. Cancer Practice. 2001;9:11–8. doi: 10.1046/j.1523-5394.2001.91004.x. [DOI] [PubMed] [Google Scholar]
- 11.Blazer . Epidemiology of late life depression. In: Schneider LSRC, Lebowitz BE, et al., editors. Diagnosis and Treatment of Depression in Late Life. Washington: American Psychiatric Press; 1994. pp. 9–19. [Google Scholar]
- 12.Cassileth BR, Lusk EJ, Brown LL, Cross PA, Walsh WP, Hurwitz S. Factors associated with psychological distress in cancer patients. Med Pediatr Oncol. 1986;14:251–4. doi: 10.1002/mpo.2950140503. [DOI] [PubMed] [Google Scholar]
- 13.Given CW, Given B, Azzouz F, Stommel M, Kozachik S. Comparison of changes in physical functioning of elderly patients with new diagnoses of cancer. Med Care. 2000;38:482–93. doi: 10.1097/00005650-200005000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Burdette-Radoux S, Muss HB. Adjuvant chemotherapy in the elderly: whom to treat, what regimen? Oncologist. 2006;11:234–42. doi: 10.1634/theoncologist.11-3-234. [DOI] [PubMed] [Google Scholar]
- 15.Chen H, Cantor A, Meyer J, et al. Can older cancer patients tolerate chemotherapy? A prospective pilot study Cancer. 2003;97:1107–14. doi: 10.1002/cncr.11110. [DOI] [PubMed] [Google Scholar]
- 16.Norton TR, Manne SL, Rubin S, et al. Prevalence and predictors of psychological distress among women with ovarian cancer. J Clin Oncol. 2004;22:919–26. doi: 10.1200/JCO.2004.07.028. [DOI] [PubMed] [Google Scholar]
- 17.Eton DT, Lepore SJ. Prostate cancer and health-related quality of life: a review of the literature. Psychooncology. 2002;11:307–26. doi: 10.1002/pon.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bellizzi KM, Blank TO. Predicting posttraumatic growth in breast cancer survivors. Health Psychol. 2006;25:47–56. doi: 10.1037/0278-6133.25.1.47. [DOI] [PubMed] [Google Scholar]
- 19.Erikson EH. In: Identity and the life cycle: Selected Papers. Monograph PI, editor. Vol. 1. 1959. pp. 1–177. [Google Scholar]
- 20.Erikson EH. Childhood and Society. 2. New York: WW Norton; 1963. [Google Scholar]
- 21.Brandtstadter J, Rothermund K. Self-percepts of control in middle and later adulthood: buffering losses by rescaling goals. Psychol Aging. 1994;9:265–73. doi: 10.1037//0882-7974.9.2.265. [DOI] [PubMed] [Google Scholar]
- 22.Carstensen LL. The influence of a sense of time on human development. Science. 2006;312:1913–5. doi: 10.1126/science.1127488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carstensen LL, Lockenhoff CE. Aging, emotion, and evolution: the bigger picture. Ann N Y Acad Sci. 2003;1000:152–79. doi: 10.1196/annals.1280.008. [DOI] [PubMed] [Google Scholar]
- 24.Forstmeier S, Maercker A. Motivational reserve: lifetime motivational abilities contribute to cognitive and emotional health in old age. Psychol Aging. 2008;23:886–99. doi: 10.1037/a0013602. [DOI] [PubMed] [Google Scholar]
- 25.Jacobsen PB. Screening for psychological distress in cancer patients: challenges and opportunities. J Clin Oncol. 2007;25:4526–7. doi: 10.1200/JCO.2007.13.1367. [DOI] [PubMed] [Google Scholar]
- 26.Esper P, Mo F, Chodak G, Sinner M, Cella D, Pienta KJ. Measuring quality of life in men with prostate cancer using the functional assessment of cancer therapy-prostate instrument. Urology. 1997;50:920–8. doi: 10.1016/S0090-4295(97)00459-7. [DOI] [PubMed] [Google Scholar]
- 27.ACS. In; 2008.
- 28.Roth AJ, Rosenfeld B, Kornblith AB, et al. The memorial anxiety scale for prostate cancer: validation of a new scale to measure anxiety in men with with prostate cancer. Cancer. 2003;97:2910–8. doi: 10.1002/cncr.11386. [DOI] [PubMed] [Google Scholar]
- 29.Roth A, Nelson CJ, Rosenfeld B, et al. Assessing anxiety in men with prostate cancer: further data on the reliability and validity of the Memorial Anxiety Scale for Prostate Cancer (MAX-PC) Psychosomatics. 2006;47:340–7. doi: 10.1176/appi.psy.47.4.340. [DOI] [PubMed] [Google Scholar]
- 30.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta psychiatrica Scandinavica. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 31.Cella DF, Tulsky DS, Gray G, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. Journal of clinical oncology. 1993;11:570–9. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- 32.Cella DF. Manual of The Functional Assessment of Chronic Illness Therapy Scales, Version 4. Chicago: Center on Outcomes, Research and Education (CORE), Evanston Northwestern Healthcare and Northwestern University; 1997. [Google Scholar]
- 33.Massie MJ. Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr. 2004:57–71. doi: 10.1093/jncimonographs/lgh014. [DOI] [PubMed] [Google Scholar]
- 34.van’t Spijker A, Trijsburg RW, Duivenvoorden HJ. Psychological sequelae of cancer diagnosis: a meta-analytical review of 58 studies after 1980. Psychosom Med. 1997;59:280–93. doi: 10.1097/00006842-199705000-00011. [DOI] [PubMed] [Google Scholar]
- 35.Roth AJ, Kornblith AB, Batel-Copel L, Peabody E, Scher HI, Holland JC. Rapid screening for psychologic distress in men with prostate carcinoma: a pilot study. Cancer. 1998;82:1904–8. doi: 10.1002/(sici)1097-0142(19980515)82:10<1904::aid-cncr13>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 36.Pirl WF, Siegel GI, Goode MJ, Smith MR. Depression in men receiving androgen deprivation therapy for prostate cancer: a pilot study. Psychooncology. 2002;11:518–23. doi: 10.1002/pon.592. [DOI] [PubMed] [Google Scholar]
- 37.Carroll BT, Kathol RG, Noyes R, Jr, Wald TG, Clamon GH. Screening for depression and anxiety in cancer patients using the Hospital Anxiety and Depression Scale. Gen Hosp Psychiatry. 1993;15:69–74. doi: 10.1016/0163-8343(93)90099-a. [DOI] [PubMed] [Google Scholar]
- 38.Nelson CJ, Holland J, Roth AJ. Assessing depression in geriatric cancer patients: Do we have appropriate measures?. Abstract to be Presented at the Annual Conference of the American Psych-Oncology Society; Irvine, CA. 2008. [Google Scholar]
- 39.Beekman AT, de Beurs E, van Balkom AJ, Deeg DJ, van Dyck R, van Tilburg W. Anxiety and depression in later life: Co-occurrence and communality of risk factors. Am J Psychiatry. 2000;157:89–95. doi: 10.1176/ajp.157.1.89. [DOI] [PubMed] [Google Scholar]
- 40.Carstensen LL. Motivation for social contact across the > life span:A theory of socioemotional selectivity. In: Jacobs J, editor. Nebraska Symposium on motivation. Lincoln: University of Nebraska Press; 1993. pp. 209–54. [PubMed] [Google Scholar]
- 41.Blazer DG. Depression in late life: review and commentary. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2003;58:249–65. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- 42.Morley JE. The top 10 hot topics in aging. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2004;59:24–33. doi: 10.1093/gerona/59.1.m24. [DOI] [PubMed] [Google Scholar]
- 43.Scott KM, Von Korff M, Alonso J, et al. Age patterns in the prevalence of DSM-IV depressive/anxiety disorders with and without physical co-morbidity. Psychol Med. 2008;38:1659–69. doi: 10.1017/S0033291708003413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jorm AF. Does old age reduce the risk of anxiety and depression? A review of epidemiological studies across the adult life span. Psychol Med. 2000;30:11–22. doi: 10.1017/s0033291799001452. [DOI] [PubMed] [Google Scholar]
- 45.Jorm AF, Windsor TD, Dear KB, Anstey KJ, Christensen H, Rodgers B. Age group differences in psychological distress: the role of psychosocial risk factors that vary with age. Psychol Med. 2005;35:1253–63. doi: 10.1017/S0033291705004976. [DOI] [PubMed] [Google Scholar]
- 46.Nguyen HT, Zonderman AB. Relationship between age and aspects of depression: consistency and reliability across two longitudinal studies. Psychol Aging. 2006;21:119–26. doi: 10.1037/0882-7974.21.1.119. [DOI] [PubMed] [Google Scholar]
- 47.Stordal E, Mykletun A, Dahl AA. The association between age and depression in the general population: a multivariate examination. Acta Psychiatr Scand. 2003;107:132–41. doi: 10.1034/j.1600-0447.2003.02056.x. [DOI] [PubMed] [Google Scholar]
- 48.Snowdon J. Is depression more prevalent in old age? Aust N Z J Psychiatry. 2001;35:782–7. doi: 10.1046/j.1440-1614.2001.00968.x. [DOI] [PubMed] [Google Scholar]
- 49.Palsson SP, Ostling S, Skoog I. The incidence of first-onset depression in a population followed from the age of 70 to 85. Psychol Med. 2001;31:1159–68. doi: 10.1017/s0033291701004524. [DOI] [PubMed] [Google Scholar]
- 50.Weinberger MI, Roth AJ, Nelson CJ. Untangling the Complexities of Depression Diagnosis in Older Cancer Patients. Oncologist. 2009 doi: 10.1634/theoncologist.2008-0147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Brodaty H, Cullen B, Thompson C, et al. Age and gender in the phenomenology of depression. Am J Geriatr Psychiatry. 2005;13:589–96. doi: 10.1176/appi.ajgp.13.7.589. [DOI] [PubMed] [Google Scholar]
- 52.Christensen H, Jorm AF, Mackinnon AJ, et al. Age differences in depression and anxiety symptoms: a structural equation modelling analysis of data from a general population sample. Psychol Med. 1999;29:325–39. doi: 10.1017/s0033291798008150. [DOI] [PubMed] [Google Scholar]
- 53.Husain MM, Rush AJ, Sackeim HA, et al. Age-related characteristics of depression: a preliminary STAR*D report. Am J Geriatr Psychiatry. 2005;13:852–60. doi: 10.1176/appi.ajgp.13.10.852. [DOI] [PubMed] [Google Scholar]
- 54.Kim Y, Pilkonis PA, Frank E, Thase ME, Reynolds CF. Differential functioning of the Beck depression inventory in late-life patients: use of item response theory. Psychol Aging. 2002;17:379–91. doi: 10.1037//0882-7974.17.3.379. [DOI] [PubMed] [Google Scholar]