Abstract
Background
Foot placement during walking is closely linked to the body position, yet it is typically quantified relative to the other foot. The purpose of this study was to quantify foot placement patterns relative to body post-stroke and investigate its relationship to hemiparetic walking performance.
Methods
Thirty-nine participants with hemiparesis walked on a split-belt treadmill at their self-selected speeds and twenty healthy participants walked at matched slow speeds. Anterior-posterior and medial-lateral foot placements (foot center-of-mass) relative to body (pelvis center-of-mass) quantified stepping in body reference frame. Walking performance was quantified using step length asymmetry ratio, percent of paretic propulsion and paretic weight support.
Findings
Participants with hemiparesis placed their paretic foot further anterior than posterior during walking compared to controls walking at matched slow speeds (p < .05). Participants also placed their paretic foot further lateral relative to pelvis than non-paretic (p < .05). Anterior-posterior asymmetry correlated with step length asymmetry and percent paretic propulsion but some persons revealed differing asymmetry patterns in the translating reference frame. Lateral foot placement asymmetry correlated with paretic weight support (r = .596; p < .001), whereas step widths showed no relation to paretic weight support.
Interpretation
Post-stroke gait is asymmetric when quantifying foot placement in a body reference frame and this asymmetry related to the hemiparetic walking performance and explained motor control mechanisms beyond those explained by step lengths and step widths alone. We suggest that biomechanical analyses quantifying stepping performance in impaired populations should investigate foot placement in a body reference frame.
INTRODUCTION
During walking, foot placement is typically quantified by spatial and temporal measures in a global reference frame (e.g., step length and step width). These measures quantify foot placement in relation to the other foot without accounting for body position. However, foot placement closely relates to movements of the body and can also be quantified in a body reference frame which in turn may prove physiologically more relevant (Redfern and Schumann, 1994; Townsend, 1985). For instance, in the stance phase, body center of mass is propelled within the limits related to foot placement. Similarly at the end of swing phase precise placement of the foot relative to the body establishes a new base of support at each step that determines the dynamic stability during walking.
In this study, we define foot placement in a body reference frame as the calculation of foot position relative to body position during walking (i.e., independent of the other foot). For instance, step length in a body reference frame was calculated as the anterior distance between the leading foot center-of-mass (reflecting foot position) and pelvis center-of-mass (reflecting body position) at initial-contact. Whereas, step length in a global reference frame would be calculated as the anterior distance between the leading and trailing foot without accounting for the body position. Previous work with healthy participants investigating foot placement relative to body have reported specific relationships between foot placement and motor control during walking (Townsend, 1981; Townsend, 1985; MacKinnon and Winter, 1993; Redfern and Schumann, 1994; Zijlstra and Hof, 1997). Redfern and Schuman (1994) postulated that foot placement requires symmetry of the limbs with respect to the pelvis at initial-contact such that the body center of mass is placed equidistant from both feet during double support creating a stable support base. Mackinnon and Winter (1993) and Townsend (1981) reported that the most important factor affecting frontal whole body balance is the mediolateral foot placement relative to the center of mass established at initial-contact.
Studies of healthy gait suggest that quantifying where the foot is placed relative to the body may provide a deeper understanding of the mechanisms of hemiparetic walking compared to analyzing foot kinematics alone (i.e., when foot placement is defined relative to other foot). For instance, it is commonly reported that persons with stroke walk with asymmetrical step lengths (Olney and Richards, 1996; Kim and Eng, 2003; Balasubramanian et al., 2007; Patterson et al., 2008). While these asymmetries are quantified relative to the other foot, it is unclear whether foot placements relative to pelvis (or trunk) would also be asymmetrical. It is possible that, in those persons who take longer paretic steps than non-paretic; relative to the pelvis both feet are placed symmetrically. Similarly, it is unclear whether there is any asymmetry in lateral foot placements relative to pelvis and whether it relates to step width post-stroke. Mediolateral foot placement relative to the body can also influence the weight shifted and supported by the legs since the farther one places their foot relative to the body at initial-contact determines the extent of their body displacement. Furthermore, since healthy gait studies suggest strong relationships of foot placement in a body reference frame and forward progression and balance during walking, we hypothesized that investigation of foot placement relative to body in anterior-posterior and medial-lateral planes will provide important insight into forward progression and weight support during walking.
In this study we quantified foot placement relative to the body during post-stroke hemiparetic walking in order to 1) investigate the relationships between foot placement in a body reference frame to foot placement in a global reference frame and 2) examine the relationships between foot placement in a body reference frame and walking performance (forward progression and weight support). We also analyzed healthy participants as a control group to compare the foot placement patterns in the hemiparetic gait to healthy gait patterns. We hypothesized that the measures of stepping performance (step lengths and step widths), forward progression, weight support and dynamic stability would relate to the asymmetry in foot placement relative to body such that investigation of foot placement in a body reference frame will provide insights into essential requirements of locomotion and help better evaluate asymmetric gait post-stroke.
METHODS
Participants
Data were collected from thirty-nine participants with chronic hemiparesis [Age = 60.21 yrs (SD=12.32 yrs), 20 men, 19 left-side hemiparesis, time since stroke = 4 yrs ± 5 mos (SD = 3 yrs ± 2 mos)] and twenty age-matched healthy participants [Age = 66.15 yrs (SD=10.03 yrs), 4 men] at the VA-UF Human Motor Performance Laboratory, VA Medical Center at Gainesville Florida. Inclusion criteria for the participants with hemiparesis were: hemiparesis secondary to a single onset unilateral stroke; ability to ambulate independently with or without an assistive device over 10 m on a level surface; ability to walk on a regular basis at least at home; absence of significant lower extremity joint pain and major sensory deficits; absence of significant lower limb contractures and no significant cardiovascular or respiratory symptoms contraindicative to walking. All participants in the study signed a written informed consent and Institutional Review Board of University of Florida approved the protocol.
Procedures
Retro-reflective markers were attached to the participant to collect bilateral 3D kinematics using a 12 camera VICON motion analysis system. Markers were attached to the head, trunk, upper extremity, lower extremity and feet. Clusters of reflective markers attached to rigid bodies were also located on the pelvis, bilateral thighs, shanks and feet. A fixed laboratory coordinate reference frame was created within the VICON system that was placed at the left corner of the laboratory. Marker placement was typically performed or overseen by a small number of research physical therapists who were all trained similarly. Since the study was completed we performed post-hoc analyses with three such persons using this marker configuration. This revealed excellent reliability.
At the beginning of the test session, controls and participants with hemiparesis walked for 2–3 trials across a 12 ft long instrumented mat (GaitRite) at their self-selected walking speeds to collect overground spatiotemporal parameters of steps and estimate their overground walking speeds. Gaitrite is a valid instrument to measure spatiotemporal parameters during walking (Bilney et al., 2003).
Subsequently, controls and participants with hemiparesis walked on an instrumented split-belt treadmill (TECMACHINE) for three trials at their self-selected treadmill walking speed. The treadmill self-selected speeds were 10 – 30% slower than the overground self-selected speeds for participants with hemiparesis. For healthy participants, treadmill speeds closely approximated their over ground speeds. Participants with hemiparesis completed three 30-second walking trials without use of an assistive device or ankle-foot orthosis. A safety harness mounted to the laboratory ceiling was worn across the shoulders and chest to protect the participants in the event that they lose balance. No bodyweight was offloaded by the harness. Additionally, a physical therapist closely guarded the participants as they walked over the treadmill (although no manual support was provided). Healthy participants also walked on the treadmill at 0.3 m/s, 0.6 m/s, and 0.9 m/s to provide matched control data for the hemiparetic participants.
To optimize capture of steady-state data on the treadmill, each subject walked for 10 s prior to each of the 30 s of data collection. Bilateral three-dimensional GRFs were simultaneously collected at 200 Hz.
Data analyses
Kinematic data was low-pass filtered using a fourth-order zero-lag Butterworth filter with a 10 Hz cutoff frequency. The marker trajectories were fitted to an eight-segment musculoskeletal model generated using SIMM (MusculoGraphics, Inc.) consisting of a trunk (including the mass of the torso, head and arms), pelvis and legs for each subject. Each lower extremity consisted of a thigh, shank and foot. The anthropometrics and inertial properties were based on that of de Leva (de Leva, 1996). Segmental center-of-mass (COM) calculations were used to calculate the whole body COM. In this study, the pelvis COM was used to represent the body centered reference frame.
Ground reaction force (GRF) data were low-pass filtered using a fourth-order zero-lag Butterworth filter with a 20 Hz cutoff frequency. The GRFs were normalized to participant body weight and time normalized to 100% of the paretic leg gait cycle (paretic initial-contact to paretic initial-contact).
Calculation of study variables
All variables were calculated by averaging across all complete gait cycles of each of the three trials. The number of steps that are used to calculate the averages varied across subjects since they walked at different speeds and cadences.
Foot Placement in a body reference frame
Anterior-Posterior (AP) and medial-lateral (ML) foot placement and position variables relative to pelvis were calculated for individual legs. The body was referenced at the pelvis COM (Figure 1). Initial foot placement (calculated at initial-contact in the 1st double support phase) and terminal foot position (calculated at foot-off in the 2nd double support phase) in AP and ML direction is presented in Table 1. The terminology foot-off was chosen instead of toe-off to account for the variance in foot patterns shown by hemiparetic participants. The term foot position was used to distinguish the posterior foot position from anterior foot placement relative to the body.
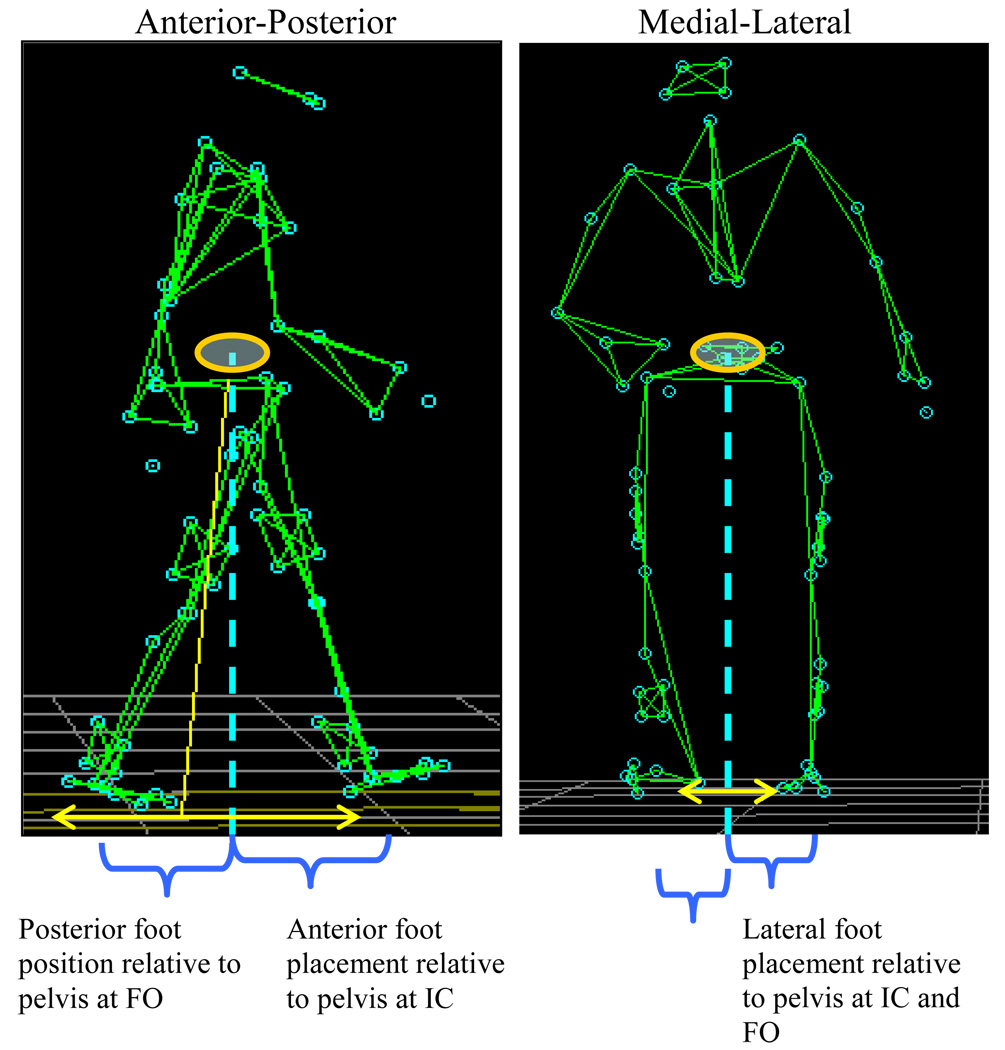
Figure 1. Calculation of Anterior-Posterior and Medial-Lateral foot placements relative to the pelvis.
Abbreviations: IC – Initial-contact at 1st double-support (initial foot placement), FO – Foot-off at 2nd double-support (terminal foot position).
This figure presents the foot placement variables calculated in a body reference frame. Body is referenced at the pelvis COM and foot is referenced at the foot COM. Variables were calculated as the AP and ML distance between foot COM and pelvis COM. Note, the arrows present the step length and step width calculated relative to other foot.
Table 1.
Definition of Study variables
| Foot placement in a body reference frame |
|---|
| Anterior-Posterior |
|
Anterior Foot placement relative to pelvis: Distance in AP direction from foot COM to pelvis COM at the initial foot placement (initial-contact in the 1st double-support). |
|
Posterior Foot position relative to pelvis: Distance in AP direction from foot COM to pelvis COM at the terminal foot position (foot-off in the 2nd double-support phase). |
| Medial-Lateral |
|
Lateral Foot placement relative to pelvis: Distance in ML direction from foot COM to pelvis COM at the initial foot placement (initial-contact in the 1st double-support). |
|
Lateral Foot position relative to pelvis: Distance in AP direction from foot COM to pelvis COM at the terminal foot position (foot-off in the 2nd double-support phase). |
| Foot placement in a global reference frame |
|
Step length: Distance in AP direction from leading mid-foot to trailing mid-foot at the the initial foot placement (initial-contact in the 1st double-support). |
|
Step width: Distance in ML direction from leading mid-foot to trailing mid-foot at the the initial foot placement (initial-contact in the 1st double-support). |
| Walking performance measures |
|
Step length asymmetry: calculated as a Paretic Step Ratio (PSR = paretic step length / (paretic + non- paretic step length) and expressed as a percentage. |
| Paretic propulsion: Paretic propulsive impulse / (Paretic + Non-paretic propulsive impulse). |
|
Percent weight supported on the paretic leg: Paretic average vertical force / (Paretic + Non-paretic average vertical force) expressed as a percentage. |
Foot placement in a global reference frame
Step lengths and widths were also calculated for individual legs in the global reference frame (Table 1).
Walking performance measures
Hemiparetic walking performance was quantified using step asymmetry patterns, forward progression and weight support. Step length asymmetry was quantified using a Paretic Step Ratio (Balasubramanian et al., 2007; Balasubramanian et al., 2009), (Table 1). Asymmetry in the hemiparetic participants was characterized based on symmetry ranges calculated from similarly-aged healthy participants walking on the treadmill, as follows: ‘longer paretic step’ than non-paretic (PSR > 55), ‘shorter paretic step’ than non-paretic (PSR < 45) and ‘symmetric step lengths’ (45 ≤ PSR ≤ 55). Forward progression was quantified using paretic propulsion (Bowden et al., 2006), (Table 1). Weight support was quantified by the average vertical force supported on individual legs during the stance phases (Table 1).
Statistical analyses
For control participants, right-left foot placements and positions relative to body were similar at all speeds, in anterior-posterior and medial-lateral planes (p > .05). Therefore, the left leg was used as the control leg in the comparisons with participants post-stroke. Foot placement patterns in participants with hemiparesis were quantified and compared to controls. For these comparisons, a 3 (leg: paretic, non-paretic, control) × 2 (phase: initial-contact, foot-off) Mixed ANOVA was used. Median foot placement of the control participants at speeds of 0.3, 0.6 and 0.9 m/s were compared to participants with hemiparesis walking at their self-selected treadmill speeds. Most participants with hemiparesis walked close to the matched-control speeds of (0.3, 0.6 and 0.9). However, since the participants with hemiparesis did not walk at these exact speeds, persons walking less than equal to each of the matched-control speeds were grouped together. For example, a hemiparetic participant walking at 0.7 m/s would fall in the third group of speeds 0.9 m/s and would be compared with controls walking at 0.9 m/s. speed ranges. Note that each speed group consisted of different hemiparetic participants walking at their self-selected speeds. Pearson correlations were conducted to evaluate the relationships between foot placements and walking performance measures. Quadratic relations were additionally explored for each of the relationships but it did not improve the explanatory power significantly in any relationship, therefore linear relationships are presented.
RESULTS
Two types of asymmetry are reported: asymmetry in the body reference frame and asymmetry in the global reference frame. Asymmetry in the body reference frame includes: anterior-posterior asymmetry, anterior foot placement asymmetry and lateral foot placement asymmetry (defined below). Asymmetry in the global reference frame includes step length asymmetry (as presented in the methods section).
Quantification of foot placement in a body reference frame
Anterior-Posterior
In control participants, foot placement was anterior at initial-contact (IC) and posterior at foot-off (FO) relative to the pelvis, with the anterior placement showing greater excursion than posterior at all speeds (40 – 80 mm, p < .001) (Figure 2a). This asymmetry in foot placement is termed as ‘anterior-posterior’ (AP) asymmetry (asymmetric foot placements for the same foot at two different instances of IC and FO). Similar to controls, participants with hemiparesis had AP asymmetry relative to pelvis. However, the pattern of AP asymmetry differed with self-selected speed (see data below).
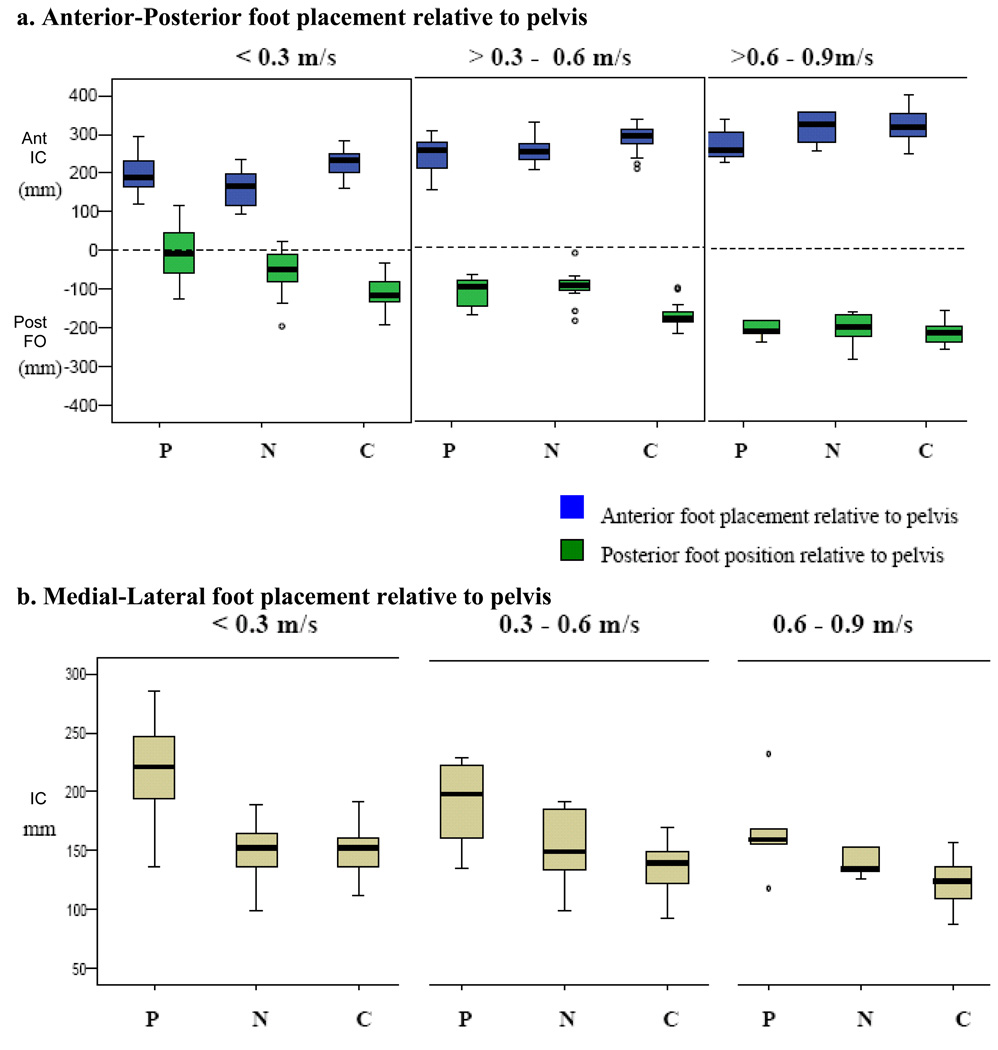
Figure 2. Foot Placement relative to pelvis during hemiparetic and healthy gait.
Abbreviations: IC – Initial-contact at 1st double-support (initial foot placement), FO – Foot-off at 2nd double-support (terminal foot position), P- Paretic foot, N-Non-paretic foot, C-Control foot.
The box plots indicate the range in the data. The central horizontal line is the median of the sample. The length of the box indicates the inter-quartile range with the upper and lower boundaries of the box indicating the upper and lower quartile, respectively. Circles represent sample values that statistically indicate outlier or extreme values (by SPSS software).
Foot placement in slow walkers (≤0.3 m/s, n = 22) and controls walking at matched-speeds
Median foot placements were anterior at IC and posterior at FO relative to pelvis. The paretic foot was more anterior and less posterior than the non-paretic foot (p =.003). There was increased inter-subject variability in posterior paretic foot position at FO such that at least half the participants in this group never positioned their foot posterior relative to pelvis (Figure 2a). The control participants showed greater excursions in anterior and posterior planes relative to the pelvis compared to the paretic and non-paretic patterns of hemiparetic participants at matched slow speed (p < .001). However, the difference in anterior foot placement between control and paretic feet was small (~30 mm).
Foot placement in Moderate (> 0.3m/s – 0.6 m/s, n = 12) and Fast walkers (> 0.6 m/s – 0.9m/s, n = 5) and controls walking at matched-speeds
For participants walking at moderate (0.3 – 0.6 m/s) and fast (0.6 – 0.9 m/s) speeds there were no differences between foot placement and position relative to the pelvis between the paretic and non-paretic legs. However, both feet were placed more anterior than posterior relative to pelvis (IC – FO relative to pelvis = 6 – 10 cm), (p < .01), Figure 2a. For fast walkers, foot placement excursions were similar to that of the Controls (p < .001), except in paretic anterior foot placement that was reduced.
Medial-lateral
Foot placements at IC and FO were equal for controls and hemiparetic participants (i.e., same lateral distance at IC and FO). Therefore, only lateral foot placement at IC is presented. In hemiparetic participants walking at slow and moderate speeds, the paretic foot was placed more lateral to the pelvis compared to both non-paretic (difference range = 30 – 70 mm) and speed-matched control (difference range = 49 – 74 mm) foot placement (p < .001) (Figure 2b). The wider paretic foot placement relative to the pelvis than non-paretic at initial-contact is defined as ‘Lateral foot placement asymmetry’. Slow walkers (< 0.3 m/s) showed the most lateral paretic foot placement. In the fast walkers (speed 0.6 – 0.9 m/s), the paretic foot was significantly lateral to the body only relative to speed-matched control foot placement and not non-paretic foot placement (p < .01) (Figure 2b).
Relationship between foot placement in a body reference frame and foot placement in a global reference frame
Anterior-Posterior
Anterior foot placement asymmetry (defined as asymmetric foot placements for the two legs at the same instance of initial-contact in the gait cycle) was associated with step length asymmetry (r = .756, p < .001), suggesting that persons taking asymmetrical step lengths also place their feet asymmetrically relative to pelvis (Figure 3). Nonetheless, asymmetry ranges in the two reference frames differed. Note that persons severely asymmetric in the global reference frame (PSR > 90%) showed similar patterns in both reference frames, however persons showing mild to moderate step length asymmetry (PSR = 60 – 80%) placed their paretic and non-paretic feet more symmetrically with respect to the pelvis (asymmetry range in body reference frame = 55 – 60%) (Figure 3).
Figure 3. Relationship between anterior foot placement asymmetry relative to pelvis and step length asymmetry in participants with hemiparesis.
This figure shows the relationship between asymmetry in foot placements relative to pelvis (body reference frame) and step length asymmetry (relative to the other foot). The vertical dashed lines indicate the step length symmetry ranges (45 ≤ PSR ≤ 55) and the horizontal dashed lines indicate symmetry ranges in the body reference frame (46 ≤ PSR ≤ 54) calculated similarly from healthy controls. Persons above the range take ‘Longer paretic’ steps than non-paretic and those below the range take ‘Shorter paretic’ steps than non-paretic. Note that, four persons (bold arrow) taking longer paretic than non-paretic step lengths placed their paretic and non-paretic feet symmetric with respect to the pelvis. On the other hand, three persons (dashed arrow) who were taking symmetric step lengths place their paretic foot closer to pelvis than non-paretic (i.e. shorter paretic steps in the body reference frame).
Medial-lateral
The relationship between step width and lateral foot placement relative to pelvis was not significant (r = .235, p = .150). In addition, there was no difference in paretic and non-paretic step widths in the global reference frame during hemiparetic walking (p = .732).
Relationship between foot placement in a body reference frame and walking performance measures
Anterior-posterior foot placement relative to pelvis and step length asymmetry
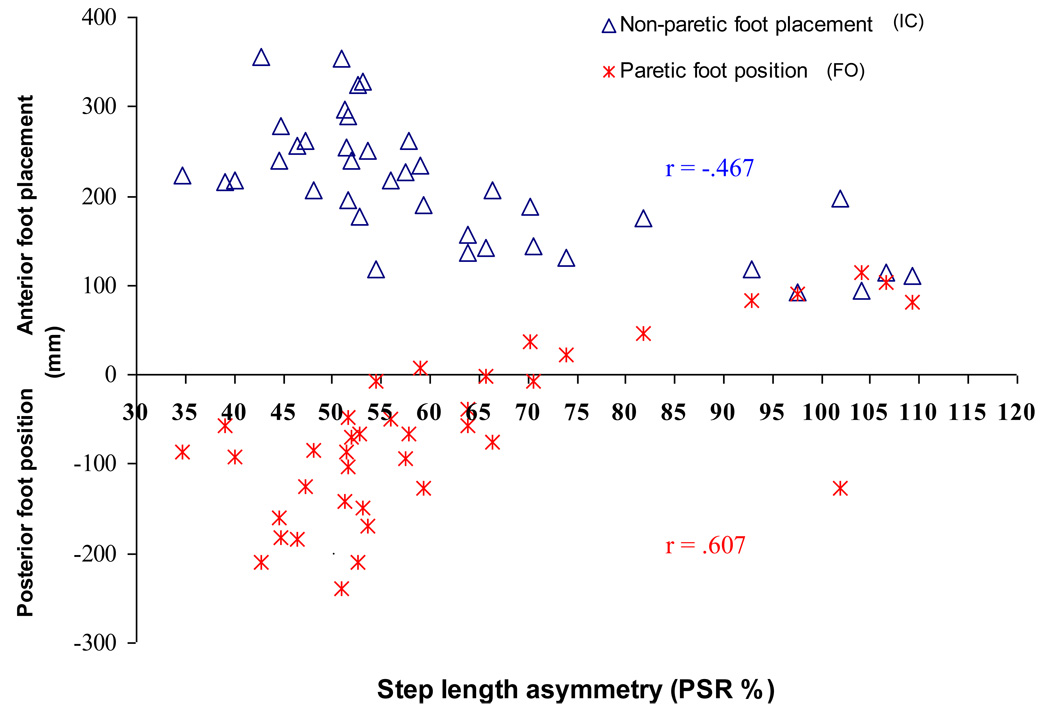
Paretic foot position at FO and non-paretic foot placement at IC strongly correlated with step length asymmetry (PSR) even after controlling for walking speed (Figure 4). Note in Figure 4, participants taking relatively long paretic steps (PSR > 70%) positioned their paretic foot anterior (opposite to the expected pattern) at FO. Similarly, participants’ taking relatively shorter paretic steps (PSR ≤ 40%) positioned their paretic foot much less posteriorly at FO relative to the symmetric group.
Figure 4. Relationship between step length asymmetry and anterior-posterior foot placement relative to pelvis in participants with hemiparesis.
Abbreviations: IC – Initial-contact at 1st double-support (initial foot placement), FO – Foot-off at 2nd double-support (terminal foot position). This figure shows the relationship between step length asymmetry and between-phase asymmetry in foot placements relative to pelvis at IC and FO. The step length symmetry ranges (45 ≤ PSR ≤ 55) were calculated similarly from healthy controls. Note the posterior paretic foot position in persons taking ‘Longer paretic’ steps (PSR > 55). Some persons with severe step length asymmetry (PSR > 70%) never position their paretic foot posterior to the pelvis in this phase of their gait cycle (2nd double support). Similarly, severely asymmetric persons taking ‘Shorter paretic’ steps (PSR < 40%) place paretic foot much anterior to pelvis than posterior at foot-off. Also, compare the paretic posterior and non-paretic anterior placement relative to pelvis between the symmetric and asymmetric persons.
Anterior-posterior foot placement relative to pelvis and paretic propulsion
Anterior foot placement asymmetry relative to pelvis and step length asymmetry were negatively associated to paretic propulsion (r = −.584 and r = −.520, respectively), suggesting that both anterior foot placement asymmetry in body reference frame and step length asymmetry in the global reference frame related to percent propulsion generated the paretic leg.
Relationship between lateral foot placements relative to body and paretic weight support
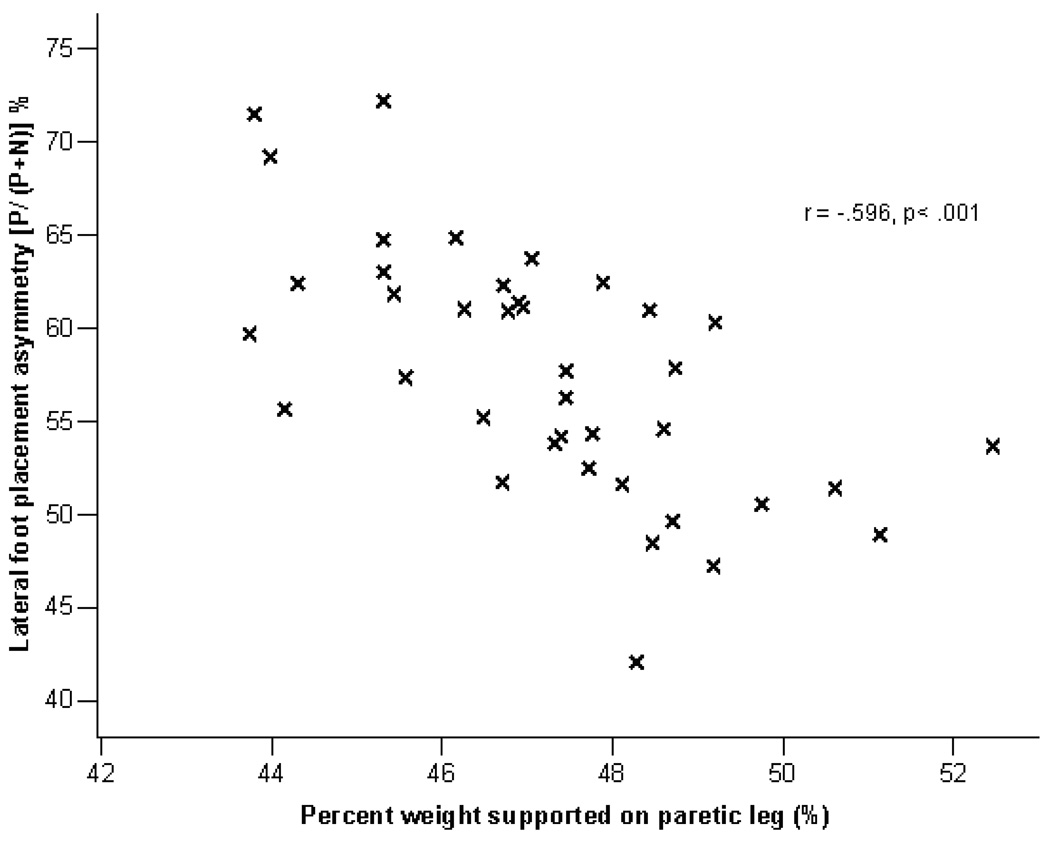
The lateral foot placement asymmetry (wider paretic foot placement at IC compared to non-paretic at IC) was negatively associated to the percent weight supported by the paretic leg (r = −.596, p < .001). However, the relationship between step width and percent weight borne by the paretic leg was not significant (r = .244, p = .135) (Figure 5).
Figure 5. Relationship between paretic and non-paretic lateral foot placemen asymmetry relative to pelvis and percent weight supported on the paretic leg.
This figure shows the relationship between lateral foot placement asymmetry and paretic leg weight supported. The greater lateral foot placement asymmetry (i.e., paretic foot placed wider relative to pelvis than non-paretic foot placement relative to pelvis) lesser the weight supported on the paretic leg during the stance phase.
DISCUSSION
Anterior-posterior foot placement relative to pelvis
Foot placement is further anterior at Initial-contact than posterior at Foot-off relative to pelvis during walking (anterior-posterior asymmetry)
Relative to the pelvis the foot was placed more anterior at IC and less posterior at FO in the controls and participants with hemiparesis at all speeds. Post-stroke participants showed greater AP asymmetry in the paretic leg than non-paretic legs and controls walking at matched slow speeds. While AP asymmetry was largest for paretic foot placements, overall foot excursions were greatest for controls even at the matched slow speeds indicating that slower walking speeds alone cannot explain the AP asymmetry in the hemiparetic participants. Specifically, posterior paretic foot position at FO showed increased inter-subject variability (See Figure 2a, speeds ≤ 0.3 m/s), which suggests that there were persons who never positioned their paretic foot posterior to the pelvis and others who positioned it posterior and yet these two groups were walking at similarly slow walking speeds.
Anterior-posterior foot placement patterns relative to pelvis suggest reduced leg extension in persons with hemiparesis taking ‘Longer paretic steps’ and compensatory trunk lean in those taking ‘Shorter paretic steps’
In persons taking ‘longer paretic’ steps than non-paretic (PSR > 55%), the paretic posterior foot position was either reduced or anterior relative to the pelvis suggesting that paretic leg orientation at pre-swing phase was opposite than expected (posterior positioning) in this phase. Therefore, while persons with ‘longer paretic’ steps had good stepping ability evidenced by the greater paretic anterior foot placement relative to the pelvis than the non-paretic placement (see Figure 4), an inability to achieve a more posterior paretic foot position at FO suggests impaired paretic leg extension in the ‘longer paretic’ group. Reduced posterior position of the foot relative to the body at foot-off can impair trunk propulsion during this phase since the ground reaction force through the foot would be directed less anteriorly ( Turns et al., 2007; Balasubramanian et al., 2007). Therefore, foot position relative to the body in the pre-swing phase can mechanically influence trunk forward progression during walking.
We would expect that in the ‘shorter paretic’ group the posterior paretic foot position would be relatively greater compared to the ‘longer paretic’ group since these persons show good paretic propulsion. While all participants in the shorter paretic group positioned their paretic foot posterior to the pelvis (Figure 4) in the severely asymmetric (PSR < 40%), the posterior foot position relative to the pelvis was much reduced similar to some persons in the ‘longer paretic’ group. Therefore, we additionally investigated their foot position relative to the trunk COM to evaluate if compensatory trunk lean might be the mechanism utilized to propel the body forward. Relative to the trunk, paretic foot position was much more posterior at FO (showing similar excursion as anterior non-paretic foot placement at IC). Since the foot placement relative to the trunk depends not only on where the foot is placed but where the trunk is positioned, it is possible that at least some of these persons in the ‘shorter paretic’ group generate good body forward progression during the paretic pre-swing phase by flexing the trunk forward and thereby creating a mechanically advantageous position for the propulsive ground reaction forces generated from the paretic leg to propel the body forward. Therefore, by investigating the foot placement relative to the trunk (in addition to pelvis), we are able to report compensatory strategies such as trunk lean.
For some participants with hemiparesis, foot placement patterns differed between the global and body reference frames
Overall, anterior stepping asymmetry in the two reference frames were correlated (for example, persons taking longer paretic steps relative to non-paretic steps were also placing their paretic foot more anterior relative to pelvis). However, the symmetry range in the body reference frame was narrower than step length symmetry range and some persons who were asymmetric taking longer paretic step lengths than non-paretic steps (PSR = 55 –65%) were symmetric in the body reference frame (Figure 3). Interestingly, others who were taking symmetrical step lengths were actually asymmetric relative to pelvis taking shorter paretic steps than non-paretic steps. The ability to place the foot further anterior to the pelvis suggests good stepping ability and the observation that the borderline symmetric persons actually took shorter paretic steps relative to the pelvis suggests their impaired paretic stepping ability. Therefore, we suggest that since some person’s [mildly asymmetric (longer paretic) and symmetric] step lengths changed their asymmetry in a translating body reference frame, additional investigation of foot placement pattern relative to pelvis might be necessary to classify them as symmetric or asymmetric.
Medial-lateral foot placement relative to pelvis
In participants with hemiparesis, paretic foot was placed more lateral to the pelvis than non-paretic (lateral foot placement asymmetry)
There was no difference in ML foot placement at initial-contact and foot-off. However, the paretic foot was placed wider relative to the pelvis compared to the non-paretic foot (lateral foot placement asymmetry) in hemiparetic participants walking at slow and moderate speeds. The lateral foot placement asymmetry between-leg was less in those hemiparetic subjects who walked faster (Figure 2b). There was no lateral foot placement asymmetry in control participants at any speed, suggesting that the pattern of lateral foot placement was not merely due to the mechanical effects of the slower walking speed.
Wider paretic foot placement relative to pelvis than the non-paretic foot relates to the decreased weight supported by the paretic leg than the non-paretic leg
We found that the lateral foot placement asymmetry (paretic step wider than non-paretic step) was strongly correlated with weight support (r = −.596, p < .001). The other variables associated to the lateral foot placement asymmetry might be the paretic lower extremity strength limiting the paretic limb loading. Overall paretic leg supported less weight compared to the non-paretic leg evidenced by the percentages less than 50 (Figure 5). This weight-bearing asymmetry is consistently reported in the post-stroke population (De Bujanda et al., 2003; Kim and Eng, 2003). However, the relationship between lateral foot placement and weight supported by the legs has not yet been reported in this population. While we expected that weight supported by the legs would be related to lateral foot placement, our results specifically show that the asymmetry in lateral foot placement relative to the pelvis (i.e., wider paretic steps relative to the pelvis than non-paretic steps) related to the weight supported by the paretic leg during stance. On the other hand, step widths were unrelated to the paretic weight support suggesting that investigation of lateral foot placement asymmetry relative to the pelvis specifically revealed the impaired paretic leg weight support in persons taking wider paretic steps relative to body. Therefore, we suggest that close observation of the lateral paretic foot placement relative to the body in comparison to lateral non-paretic foot placement can provide useful insight for clinicians regarding the amount of weight supported by the paretic leg.
Limitations
The current study was conducted on a treadmill and foot placement relative to body might differ overground. One of the advantages of our approach is that in the future our foot placement measures could be calculated with inertial and insole baropodometric sensors at the pelvis and foot and thereby allow walking overground. Nonetheless, it is expected that while absolute foot placement (in isolation) might be altered (i.e., longer versus shorter step lengths) while walking overground, its relation to the body movements would remain consistent suggesting the functional relevance of foot placement relative to body. This hypothesis could be tested in future studies by exploring the step-by-step variability in foot placement relative to body and whether this changes from treadmill to overground walking. Further, the treadmill self-selected speed was 10–30% slower than the overground. Hip and knee kinematics were not explored in the current study. Since the foot is under multi-segmental and end-point control, it is expected that the foot kinematics relative to the body will be the end result of different combinations of hip and knee kinematics such that investigation of foot kinematics relative to body might be a relatively easy method to understand post-stroke walking from a control model viewpoint.
CONCLUSIONS
Post-stroke gait is asymmetric when quantifying foot placement relative to the pelvis in the anterior-posterior and medial-lateral planes. Participants with hemiparesis placed their paretic foot further anterior than posterior during walking and this asymmetry decreased in those walking at faster speeds. By quantifying foot placement relative to the pelvis we are able to propose some underlying motor control mechanisms in the sub-groups of the participants. We suggest impaired initial conditions and paretic leg extension in the ‘longer paretic’ group versus impaired stepping ability and potentially compensatory trunk lean in the ‘shorter paretic’ group as potential mechanisms. Since foot placement in a global and body reference frames were associated in the anterior-posterior plane, foot placement in a global reference frame (i.e., step length) is still appropriate to quantify asymmetrical performance and forward progression. Nonetheless, since some borderline asymmetrical (PSR = 55 – 65%) and other symmetrical persons show differing performance in the translating reference frame, it may be additionally useful to investigate foot placement relative to the pelvis in these persons. For the medial-lateral plane, we suggest foot placement relative to the pelvis as a better outcome to characterize hemiparetic performance. Lateral foot placement asymmetry correlated with the weight supported by the paretic leg. Therefore, lateral paretic foot placement relative to the body in comparison to lateral non-paretic foot placement can help in quantification of the paretic leg weight support during hemiparetic walking. Clinically, such a measure could be used by simply observing the paretic and non-paretic lateral foot placements relative to the pelvis. No such information is available from observing step widths.
Overall, we were able to attain additional insights on motor control mechanisms and asymmetrical performance during hemiparetic walking by investigating foot placement in a body reference frame. Therefore, we suggest that biomechanical analyses quantifying stepping performance in impaired populations should investigate foot placement in a body reference frame in addition to foot placement in a global reference frame to better understand motor control mechanisms during hemiparetic walking.
ACKNOWLEDGEMENTS
This work was funded by Center of Excellence grant # F2182C (Brain Rehabilitation Research Center) from the Rehabilitation Research and Development Service of the Department of Veterans Affairs and NIHR01 HD 46820 (Intramuscular coordination of Hemiparetic walking). This material is the result of work supported in part by the Office of Research and Development, Rehabilitation R&D Service, Department of Veterans Affairs and the Malcolm Randal VA Medical Center, Gainesville, FL. The authors would like to thank Shrinaresh Subramanian and Ryan Knight and for their help in data analysis and Mark Bowden and Erin Carr for their help in data collection in the Gainesville center. The authors would also like to thank Felix Zajac and Sylvie Nadeau for their insightful suggestions on this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Ayyappa E. Normal human locomotion, Part 1:Basic concepts and terminology. J Prosthet Orthot. 1997;9:10–17. [Google Scholar]
- Bilney B, Morris M, Webster K. Concurrent related validity of the GAITRite walkway system for quantification of the spatial and temporal parameters of gait. Gait Posture. 2003;17(1):68–74. doi: 10.1016/s0966-6362(02)00053-x. [DOI] [PubMed] [Google Scholar]
- Balasubramanian CK, Bowden MG, Neptune RR, Kautz SA. Relationship between step length asymmetry and walking performance in subjects with chronic hemiparesis. Arch Phys Med Rehabil. 2007;88(1):43–49. doi: 10.1016/j.apmr.2006.10.004. [DOI] [PubMed] [Google Scholar]
- Balasubramanian CK, Neptune RR, Kautz SA. Variability in spatiotemporal step characteristics and its relationship to walking performance post-stroke. Gait Posture. 2009;29(3):408–414. doi: 10.1016/j.gaitpost.2008.10.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowden MG, Balasubramanian CK, Neptune RR, Kautz SA. Anterior-posterior ground reaction forces as a measure of paretic leg contribution in hemiparetic walking. Stroke. 2006;37(3):872–876. doi: 10.1161/01.STR.0000204063.75779.8d. [DOI] [PubMed] [Google Scholar]
- de Leva P. Adjustments to Zatsiorsky-Seluyanov's segment inertia parameters. J Biomech. 1996;29(9):1223–1230. doi: 10.1016/0021-9290(95)00178-6. [DOI] [PubMed] [Google Scholar]
- De Bujanda E, Nadeau S, Bourbonnais D, Dickstein R. Associations between lower limb impairments, locomotor capacities and kinematic variables in the frontal plane during walking in adults with chronic stroke. J Rehabil Med. 2003;35(6):259–264. doi: 10.1080/16501970310012428. [DOI] [PubMed] [Google Scholar]
- Kim CM, Eng JJ. Symmetry in vertical ground reaction force is accompanied by symmetry in temporal but not distance variables of gait in persons with stroke. Gait Posture. 2003;18(1):23–28. doi: 10.1016/s0966-6362(02)00122-4. [DOI] [PubMed] [Google Scholar]
- MacKinnon CD, Winter DA. Control of whole body balance in the frontal plane during human walking. J Biomech. 1993;26(6):633–644. doi: 10.1016/0021-9290(93)90027-c. [DOI] [PubMed] [Google Scholar]
- Olney SJ, Richards C. Hemiparetic gait following stroke. Part I: Characteristics. Gait & Posture. 1996;4:136–148. [Google Scholar]
- Patterson KK, Parafianowicz I, Danells CJ, Closson V, Verrier MC, Staines WR, Black SE, McIlroy WE. Gait asymmetry in community-ambulating stroke survivors. Arch Phys Med Rehabil. 2008;89(2):304–310. doi: 10.1016/j.apmr.2007.08.142. [DOI] [PubMed] [Google Scholar]
- Redfern MS, Schumann T. A model of foot placement during gait. J Biomech. 1994;27(11):1339–1346. doi: 10.1016/0021-9290(94)90043-4. [DOI] [PubMed] [Google Scholar]
- Townsend MA. Dynamics and coordination of torso motions in human locomotion. J Biomech. 1981;14(11):727–738. doi: 10.1016/0021-9290(81)90029-4. [DOI] [PubMed] [Google Scholar]
- Townsend MA. Biped gait stabilization via foot placement. J Biomech. 1985;18(1):21–38. doi: 10.1016/0021-9290(85)90042-9. [DOI] [PubMed] [Google Scholar]
- Turns LJ, Neptune RR, Kautz SA. Relationships between muscle activity and anteroposterior ground reaction forces in hemiparetic walking. Arch Phys Med Rehabil. 2007 Sep;88(9):1127–1135. doi: 10.1016/j.apmr.2007.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zijlstra W, Hof AL. Displacement of the pelvis during human walking: experimental data and model predictions. Gait Posture. 1997;6:249–262. [Google Scholar]