Abstract
Purpose
Stressful life events represent potent risk factors for the development of internalizing symptoms among adolescents. However the mechanisms linking stress to adolescent psychopathology remain inadequately understood. This study examined the role of emotion dysregulation as a mechanism linking stress to changes in internalizing symptoms among adolescents.
Methods
This study used a short-term longitudinal design. Stressful life events were assessed in a large diverse sample of adolescents (N = 1065), and emotion dysregulation and symptomatology outcomes were assessed at two subsequent time points. Structural equation modeling was used to examine the role of emotion dysregulation as a mediator of the association between stress and subsequent changes in internalizing symptoms.
Results
Emotion dysregulation mediated the relationship between stressful life events and changes in internalizing symptoms over time. Sobel’s test indicated a significant indirect effect of stressful life events on subsequent symptoms of depression (z = 5.05, p < .001) and anxiety (z = 4.95, p < .001) through emotion dysregulation.
Conclusions
Stressful life events appear to disrupt the adaptive processing of emotion among adolescents. Emotion dysregulation represents an intrapersonal mechanism linking stress to poor mental health outcomes. The implications for preventive interventions are discussed.
Keywords: Stress, Emotion regulation, Depression, Anxiety, Adolescence
Stress has long been recognized as a significant public health problem, given its association with morbidity and mortality across the life course [1–3]. Adolescence represents an especially important developmental period to understand the relationship between stress and mental health problems. Indeed, adolescence marks a substantial increase in both the number of stressors [4,5] and in the prevalence of psychopathology [6,7]. Although stress appears to be a unique determinant of adverse mental health among adolescents [8], there is a paucity of research addressing mediators of the stress–psychopathology relationship, despite repeated calls for such research [9]. Identifying mechanisms linking life stress to negative mental health outcomes among adolescents is essential for public health professionals to develop preventive interventions that reduce the prevalence of stress-related psychiatric morbidity.
To date, mediational studies have focused largely on the role of interpersonal processes, such as negative parenting [10]. Although this research is important, it is also necessary to identify intrapersonal mechanisms, especially those that may be modifiable through existing evidence-based preventive interventions. Previous research examining intrapersonal processes has examined the role of cognitive variables, such as negative attributional style and dysfunctional attitudes; but these constructs have been found to serve as moderators, as opposed to mediators, of the stress-psychopathology association [11]. The present study sought to address this gap in the literature by examining an intrapersonal mechanism that can explain how stressful life events “get under the skin” [12] to create mental health problems in adolescents. Specifically, this study examined the role of emotion regulation, which has been defined as “the extrinsic and intrinsic processes responsible for monitoring, evaluating, and modifying emotional reactions, to accomplish one’s goals” [13].
Emotion dysregulation has been hypothesized to be a potential mechanism linking chronic stress and poor health outcomes across the lifespan [14], although to date empirical studies examining this longitudinal association with specific mental health outcomes are lacking, particularly among adolescents. Emotion regulation deficits are increasingly understood as important predictors of internalizing symptoms among adolescents. Youth with anxiety disorders have poorer emotional understanding, experience negative emotions with greater intensity, have more difficulty managing negative emotions, and have lower confidence in their ability to manage their emotions than nonanxious youth [15,16]. Adolescent depression has also been linked to emotion dysregulation, particularly rumination, which involves a tendency to passively focus on the causes and consequences of depressed mood [17,18]. Importantly, although emotion dysregulation may increase in youth with depression and anxiety, poor emotion regulation is a distinct vulnerability factor for the subsequent development of internalizing problems [18].
Several lines of work suggest that emotion regulation may be a particularly likely mediator of the stress–psychopathology association. Exposure to chronic stress, such as maltreatment, leads to dysregulated emotions in youth [14,19]. This dysregulation of emotion has been identified as a mechanism linking maltreatment to behavior problems in young children and has been marginally associated with concurrent symptoms of depression and anxiety [20]. Moreover, both social exclusion [21] and stigma [22], two prevalent stressors during adolescence, have been shown to deplete self-regulation abilities that can be protective against mental health problems. Finally, stressful events become more closely linked to the emergence of negative affective states during adolescence [4]. This renders adolescents more emotionally vulnerable to the effects of stress, suggesting that the adaptive regulation of emotions in response to stressors is especially important during this developmental period. Taken together, this prior research suggests that the effort required to manage the increased arousal and negative affect associated with life stress may eventually diminish adolescents’ coping resources and therefore their ability to understand and adaptively regulate their emotions, leaving them more vulnerable to stress-related psychiatric morbidity.
The purpose of the current investigation was to examine the role of emotion dysregulation as a mediator of the association between stressful life events and subsequent changes in internalizing symptoms using prospective data from a large, diverse, community-based sample of adolescents. We hypothesized that stressful life events would lead to increases in emotion dysregulation (poor understanding of emotional reactions to stress, poor coping with anger and sadness, and ruminative responses to distress) and in symptoms of depression and anxiety. Furthermore we predicted that emotion dysregulation would mediate the association between stress and changes in symptomatology over time. Importantly, we were able to test causal mediation in this study using a longitudinal design with three separate assessments.
Methods
Participants
The sample for this study was recruited from the total enrollment of two middle schools (grades 6–8) from a school district in central Connecticut that agreed to participate in the study. The community in which the schools are located is a small urban community (population ~ 71,500). The parents of all eligible children (N = 1567) in the middle schools were asked to provide active consent for their children to participate. Parents who did not return written consent forms to the school were contacted by telephone. Of the parents, 22% did not return consent forms and could not be reached to obtain consent, and 6% declined to provide consent for their child to participate. The overall participation rate in the study at baseline was 72%. Additional students who were not present at the baseline assessment period were added at Time 2 (71 students) and Time 3 (139 students). In all, 221 participants (20.8%) who were present at the baseline assessment did not participate at the Time 2 assessment, and 217 (20.4%) participants who were present at the baseline assessment did not participate at the Time 3 assessment. It is important to note the transience of student enrollment in this district. Data from the school district indicate that over the 4-year period from 2000–2004, 22.7% of students had left the district [23].
The baseline sample comprised 51.2% boys (n = 545) and 48.8% girls (n = 520), yielding 1065 participants, all of whom provided consent before participating in the study. Participants were evenly distributed across grade levels, with 31.8% (n = 337) of participants in the sixth, 33.9% (n = 360) in the seventh, and 34.3% (n = 364) in the eighth grade. Participants’ ages ranged from 11–14 years. The racical/ethnic composition of the sample was as follows: 13.2% (n = 141) white, 11.8% (n = 126) black, 56.9% (n = 610) Hispanic/Latino, 2.2%(n = 24) Asian/Pacific Islander, .2% (n = 2) Native American, .8% (n = 9) Middle Eastern, 9.3% (n = 100) biracial/multiracial, and 4.2% (n = 45) reported being members of other racial/ethnic groups. A few individuals 1.3% (n = 14), declined to provide this information. Of the participants, 27% (N = 293) reported living in single-parent house-holds. The community in which the participating schools reside is a uniformly lower-socioeconomic community than some, with a per-capita income of $18,404 [23]. School records indicated that 62.3% of students qualified for free or reduced lunches in the 2004–2005 school year. This project was approved by Yale University’s Human Subjects Committee.
Measures
Stress
The Life Events Scale for Children (LES) [24] is composed of 25 items that each represent a stressful life event (e.g.,“Your parents got divorced” and “You got suspended from school”). Participants are asked to indicate which events they have experienced in the prior 6 months. Life events checklists are the most commonly used instruments to assess adolescent stress [8], and the LES is one of the two most commonly used checklists in the adolescent stress literature [25].
Depressive symptoms
The Children’s Depression Inventory (CDI) [26] is the most widely used self-report measure of depressive symptoms in children and adolescents. The CDI is a self-report measure of depressive symptoms that has been standardized on children and adolescents aged 7–17 years. The CDI has sound psychometric properties, including internal consistency, test–retest reliability, and discriminant validity [26,27] and demonstrated good reliability in this sample (α = .82).
Anxiety symptoms
The Multidimensional Anxiety Scale for Children (MASC) [28] is the most widely used measure of anxiety in children. The MASC assesses physical symptoms of anxiety, harm avoidance, social anxiety, and separation anxiety, and is appropriate for youth ages 8–19 years. The MASC has high internal consistency and test–retest reliability across 3-month intervals, has good convergent and divergent validity [29], and has demonstrated good reliability in this sample(α = .88).
Emotion dysregulation measures
Poor emotional understanding
Emotional understanding was assessed using an eight-item subscale from the Emotion Expression Scale for Children (EESC) [30] that provides statements involving lack of emotional awareness and understanding. Higher scores on this subscale reflect lack of emotional understanding. A representative item from this scale is “I often do not know how I am feeling.” The EESC has high internal consistency and moderate test–retest reliability, and the construct validity of the measure has been established [30]. This subscale demonstrated good reliability in this sample (α = .82).
Dysregulated emotion expression
The Dysregulation scale from the Children’s Sadness Management Scale (CSMS)and Children’s Anger Management Scale (CAMS) was used to assess the extent to which children engage in culturally inappropriate expressions of emotion, such as excessive crying [31]. Higher scores on this scale reflect higher levels of emotion dysregulation. The scales have demonstrated adequate reliability, and their construct validity has been established [31]. Representative items include, “I attack whatever it is that is making me angry” (CAMS) and “I cry and carry on when I’m sad” (CSMS). The Dyregulation subscale of the CSMS (α = .60) and CAMS (α = .66) demonstrated adequate reliability in this sample.
Rumination
The rumination subscale from the Children’s Response Styles Questionnaire (CRSQ) [18] assesses the extent to which children respond to sad feelings with rumination (self-focused thought concerning the causes and consequences of depressed mood, e.g., “[I] think, why can’t I handle things better?”). The reliability and validity of the CRSQ have been demonstrated [18]. The rumination subscale demonstrated good reliability in this study (α = .86).
Procedure
Participants completed study questionnaires during their homeroom period. Symptom measures were assessed at Time 1 and Time 3, and mediators were assessed at Time 2. Four months elapsed between the Time 1 (November 2005) and Time 2 (March 2006) assessments, and 3 months elapsed between Time 2 and Time 3 (June 2006) assessments. This time frame was chosen to allow the maximum time between assessments while ensuring that all assessments occurred within the same academic year to avoid high attrition.
Data analysis
Structural equation modeling was used to test the mediation analyses using AMOS 6.0 software (SPSS, Inc., Chicago, IL). Analyses were conducted using the full information maximum likelihood estimation method, which estimates means and intercepts to handle missing data.
Procedures outlined by Baron and Kenny [32] were modified to evaluate the hypothesis that emotion dysregulation mediated the relationship between stress and symptomatology over time. The mediation analyses proceeded as follows: (1) Time 1 stress was examined as a predictor of Time 3 symptoms, controlling for baseline symptom levels; (2) Time 1 stress was examined as a predictor of Time 2 emotion dysregulation represented by a latent variable comprised of poor emotional awareness, dysregulated expression of anger and of sadness, and rumination; (3) emotion regulation deficits at Time 2 were evaluated as predictors of symptoms at Time 3 after controlling for baseline symptom levels; (4) the full mediation model was tested to evaluate the hypothesis that emotion dysregulation mediated the relationship between stress and internalizing symptoms. Mediation effects were examined regardless of the statistical significance of the longitudinal association between stressful life events and symptom changes, as requiring a significant association between exposure and outcome has been found to reduce the power of mediation analyses and to lead to high rates of type II error [33]. Moreover, identifying mechanisms linking exposures and health outcomes represents an important public health goal, even if the association between exposure and outcome is not statistically significant over short time intervals. Sobel’s z test [34] was performed to determine whether there were significant mediation effects. Mediation analyses were performed separately for symptoms of depression and anxiety. Finally, we conducted multigroup analyses to examine whether our mediation models were moderated by sociodemographic variables including gender, race/ethnicity, and grade level.
Results
Attrition
Analyses were first conducted to determine whether participants who did not complete all three assessments differed from those who completed the baseline and two follow-up assessments. These analyses revealed that participants who completed the baseline but not both follow-up assessments were more likely to be female (χ2 = 6.85, p < .01) but did not differ in grade level, race/ethnicity, being from a single-parent household, Time 1 depression or anxiety symptoms, or Time 2 emotional awareness, dysregulated sadness, dysregulated anger, or rumination (all p > .10).
Descriptive statistics
Depressive symptoms increased significantly over time, F(1,850) = 9.03, p = .003, η2 = .01, whereas anxiety symptoms decreased across the two assessments, F(1,854) = 109.59, p < .001, η2 = .11. Table 1 displays the means and standard deviations of stress, symptom, and emotion dysregulation variables, along with the zero-order correlations.
Table 1.
Correlations, means, and standard deviation of stress, symptoms, and emotion dysregulation variables
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| Stress T1 | — | ||||||||
| CDI Depression T1 | .29** | — | |||||||
| MASC Anxiety T1 | .10** | .28** | — | ||||||
| EESC Poor Emotional Awareness |
.20** | .35** | .33** | — | |||||
| CSMS Dysregulated Sadness | .06 | .15** | .17** | .30** | — | ||||
| CAMS Dysregulated Anger | .07 | .18** | .09* | .23** | .19** | — | |||
| CRSQ Rumination | .18** | .39* | .43** | .51** | .34** | .24** | — | ||
| CDI Depression T3 | .20** | .54** | .13** | .30** | .17** | .24** | .33** | — | |
| MASC Anxiety T3 | .14** | .24** | .53** | .36** | .28** | .10* | .44** | .33** | — |
| Mean (SD) | 5.10 (3.33) | 9.67 (6.44) | 40.20 (15.39) | 19.81 (6.79) | 4.66 (1.45) | 5.53 (1.64) | 10.84 (7.65) | 10.63 (8.15) | 34.80 (18.05) |
Emotion dysregulation measures were assessed at Time 2.
CDI = Children’s Depression Inventory; CAMS = Children’s Anger Management Scale; CRSQ = Children’s Response Styles Questionnaire; CSMS = Children’s Sadness Management Scale; EESC = Emotion Expression Scale for Children; MASC = Multidimensional Anxiety Scale for Children.
p < .05,
p < .01.
Measurement model
The measurement model of emotion dysregulation was constructed using four indicator variables reflecting three distinct types of emotion dysregulation: poor emotional awareness, dysregulated expression of anger and sadness, and ruminative responses to distress. Values of the normed fit index (NFI) and comparative fit index (CFI) >.95 indicate adequate fit, and the root-mean-square error of approximation (RMSEA) should be <.06 [35]. For the hypothesized model, NFI = .99, RFI = .98, CFI = .99, and RMSEA = .01. The χ2 test of independence indicated no significant difference between the observed and reproduced covariance matrices (χ2 = 1.21, p = .299). All fit indices indicated that the measurement model of emotion dysregulation fit the data very well.
Mediation analyses
Depression
The study data supported the first three criteria demonstrating mediation. Time 1 stress was marginally associated with Time 3 depressive symptoms, controlling for Time 1 depression (β = .05, p = .086). Time 1 stress predicted emotion dysregulation at Time 2, controlling for baseline emotion regulation (β = .25, p < .001). Finally, Time 2 emotion dysregulation was associated with Time 3 depressive symptoms, controlling for Time 1 depression (β = .20, p < .001). Time 1 depressive symptoms were significantly associated with all Time 2 emotion dysregulation indicator variables in bivariate analyses (Table 1); as such, a path from Time 1 depressive symptoms to Time 2 emotion dysregulation was added to this model.
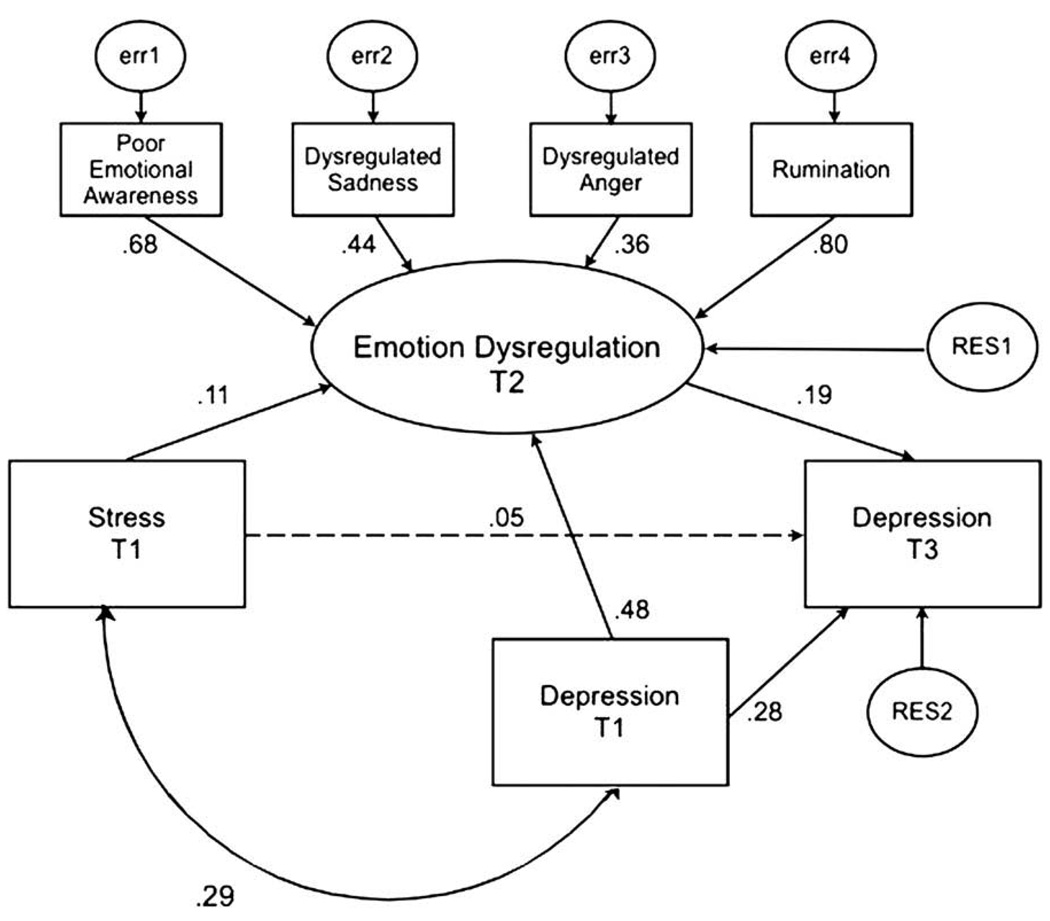
In the full mediation model, Time 1 stress was no longer associated with Time 3 depressive symptoms, controlling for Time 1 symptoms, when emotion dysregulation was added to the model (β = .05, p = .173). In the final model, the covariation between Time 1 depressive symptoms and stress was also modeled (Figure 1). All fit indices indicated that the model fit the data very well: NFI = .98, RFI = .95, CFI = .99, and RMSEA < .03. The χ2 test of independence indicated no significant difference between the observed and reproduced covariance matrices (χ2 = 1.67, p = .074). Sobel’s z test revealed a significant indirect effect of stress on depressive symptoms through emotion dysregulation (z = 5.05, p < .001).
Figure 1.
Mediational model for depressive symptoms. Numbers represent standardized path coefficients (β). All paths shown are significant (p < .05) except those with broken lines.
Anxiety
The data supported the first three criteria demonstrating mediation. Time 1 stress was significantly associated with Time 3anxiety symptoms, controlling for Time 1 anxiety (β = .53, p < .001). Time 1 stress predicted emotion dysregulation at Time 2, controlling for baseline emotion regulation (β = .25, p < .001). Finally, Time 2 emotion dysregulation was associated with Time 3anxiety symptoms, controlling for Time 1 anxiety (β = .37, p < .001). A path from Time 1 anxiety to Time 2 emotion dysregulation was included in this model.
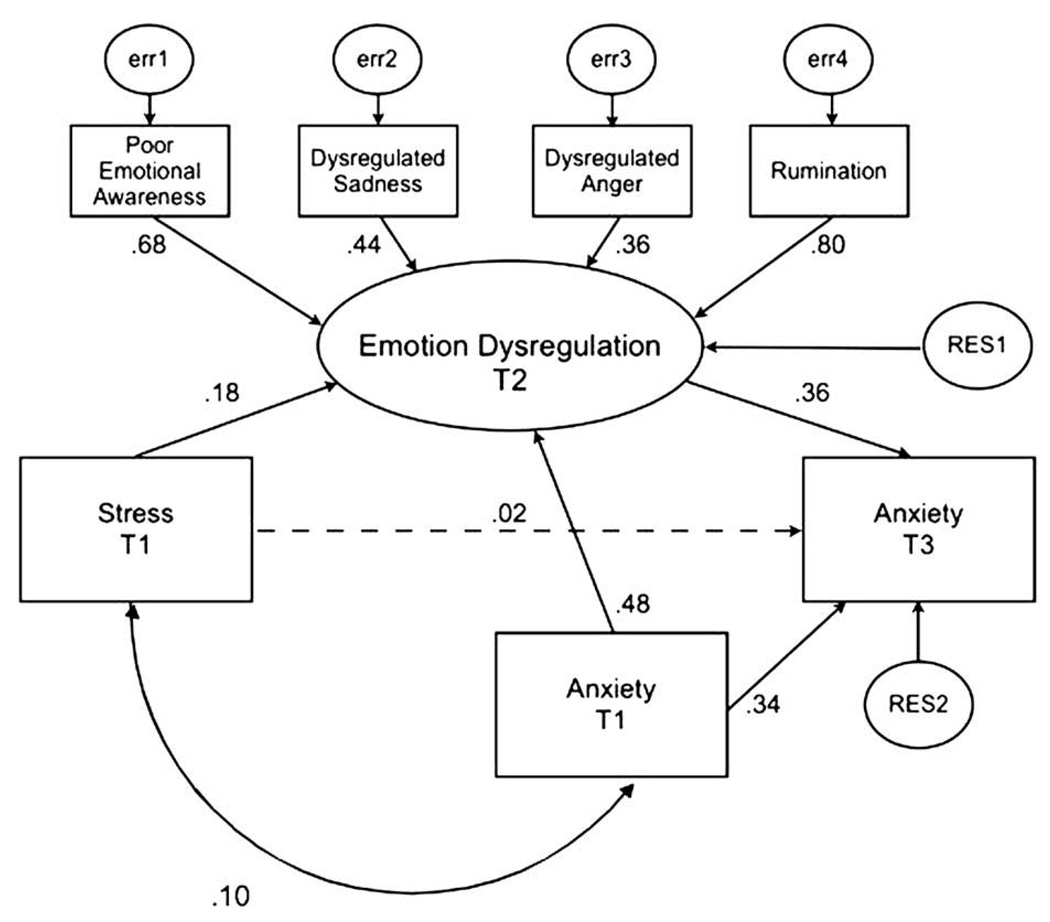
Stress was no longer a significant predictor of Time 3 anxiety symptoms, controlling for Time 1 symptoms, when emotion dysregulation was added to the model (β = .06, p = .100). In the final model, the covariation between Time 1 anxiety symptoms and Time 1 stress was also modeled (Figure 2). All fit indices indicated that the model fit the data very well (NFI = .97, CFI = .98, and RMSEA = .05). However, the χ2 test of independence indicated a significant difference between the observed and reproduced covariance matrices (χ2 = 2.27, p = .009). In large samples, even small differences between the observed and reproduced matrices can lead to significant χ2 test results. The large sample size of the current study may be driving the significant χ2 value. Sobel’s z test revealed a significant indirect effect of stress on anxiety symptoms through emotion dysregulation (z = 4.95, p < .001).
Figure 2.
Mediational model for anxiety symptoms. Numbers represent standardized path coefficients (β). All paths shown are significant (p < .05) except those with broken lines.
Moderation analyses
When we constrained the mediation paths of interest to be equivalent across groups, the model fit did not significantly worsen for gender or race/ethnicity, indicating that the process of mediation is the same for boys and girls, and for individuals of black, white, and Latino ethnicity. Significant moderation by grade was found for depression, χ2(3) = 20.53, p < .01, but not for anxiety. Examination of the estimates for individual structural paths indicated that the pathway from emotion dysregulation to Time 3 depression was stronger for older adolescents.
Discussion
Prior research has documented that stressors such as negative life events represent potent determinants of mental health problems among adolescents [8]. However, with the exception of a handful of studies on interpersonal mechanisms [9], there remains a gap in the literature regarding the mechanisms by which stress ultimately “gets under the skin” [12] and leads to psychiatric morbidity. The purpose of the present study was to determine whether an intrapersonal mechanism—namely, emotion dysregulation—could account for the link between stressful life events and adolescent psychopathology. Identifying such mechanisms represents an important public health priority because intrapersonal processes are particularly amenable to modification through existing evidence-based mental health preventive interventions.
To our knowledge, the results of the present study provide the first longitudinal evidence that emotion dysregulation mediates the association between stressful life events and internalizing symptoms among adolescents. Emotion dysregulation mediated the association between stress and both depression and anxiety, although the mediation results were stronger for anxiety. Mediation effects were similar across gender and race/ethnicity and were stronger among older adolescents who are at greater risk for depressive symptoms [6]. These results suggest that specific intrapersonal mechanisms, in addition to contextual and family factors [10], account for the stress–psychopathology association in adolescents. The conceptualization of emotion dysregulation as a pathway linking stressful life events to psychiatric symptoms is consistent with prior research suggesting that the chronic stress associated with adverse rearing environments disrupts the adaptive processing of emotion [19,36], and that emotion dysregulation resulting from chronic stress represents a mechanism linking maltreatment and behavior problems among young children [20].
The identification of intrapersonal mechanisms linking stressful life events to poor mental health outcomes represents an important step towards developing preventive interventions targeting stress-related psychopathology. Chronic stress may contribute more to negative mental health outcomes during adolescence than at earlier points in development given the increased emotional vulnerability to stress [4] and increased risk of psychopathology [6,7] that accompany this period. As such, adolescents who face chronic stressful life events, particularly economically disadvantaged youth such as the participants in this study, represent important targets for interventions aimed at preventing the negative mental health sequelae of stressful life experiences. Our results suggest that emotion regulation skills represent an important target for preventive interventions that seek to reduce the prevalence of psychopathologic outcomes among youth experiencing chronic stress. This might be done through several existing evidence-based protocols that have shown promise in facilitating more adaptive regulation of emotions, including behavioral activation interventions [37] and newly developed emotion regulation intervention approaches [38]. In addition, interventions that foster effective coping after major stressors such as parental divorce [39] could be adapted to target stress more generally for youth experiencing chronic stress. Importantly, intrapersonal mechanisms are easier to target with preventive interventions than the family-level factors that have been identified as mechanisms linking stress and psychopathology in prior research [10], as intrapersonal mechanisms can be targeted by school-based interventions that do not involve the logistical difficulties associated with family-level interventions.
Although our results contribute substantially to understanding how stressful life events lead to adolescent psychopatholic conditions, limitations of the study warrant consideration. The first is our use of self-reported symptomatology and emotion regulation abilities. Although administration of a structured interview to establish DSM-IV clinical diagnoses would represent a methodologic improvement, the validity of the self-report symptom measures used in this study is well established [26,27]. Although there are methods for assessing emotion regulation other than self-report [40], the size of the sample and the longitudinal nature of the current investigation made use of self-report measures the only reasonable option for assessing emotion regulation. Importantly, numerous prior studies examining emotion regulation and youth psychopathology have also relied on self-report measures of emotion regulation [15,16]. Our use of a self-report checklist of stressful life events represents an additional limitation. Importantly, the questionnaire in our study is among the most widely used self-report measures of stressful life events in adolescence [25]. In addition, the stressors measured are predominantly external, environmental changes or conditions and consequently are not confounded with subjective appraisals of the stressor [9]. Furthermore, stress checklists represent the most reliable methodology for assessing stress in large community samples in which stressor interviews are prohibitive in time and cost [8]. Nevertheless, stressor interviews, which capture more “objective” indices of stressors and the level of threat associated with these stressors, would represent a methodologic improvement and should therefore be used in future studies [25]. This study also did not assess stressful life events at subsequent time points and therefore could not test for reciprocal relationships between stress, emotion dysregulation, and symptomatology, an important direction for future inquiry. Finally, the depression results warrant replication over longer time intervals, given that the association between stress and increases in depressive symptoms was only marginally significant.
These limitations notwithstanding, this study had a number of important methodologic strengths. In particular, the use of a longitudinal design allowed us to examine intrapersonal mechanisms responsible for the association between stressful life events and increases in depressive and anxious symptoms over time. A large sample with substantial racial/ethnic diversity participated. In addition to these methodologic strengths, the study provides an important theoretical contribution to the literature on the relationship between stress and adverse mental health outcomes. The results documented that the emotion dysregulation generated by stressful life events accounted for the relationship between stress and psychopathology, suggesting novel avenues for intervention research targeting adolescents suffering from stress-related psychiatric morbidity. Given the prevalence of adolescent stressors and the increase in psychopathology during this developmental period, the findings have implications for addressing a significant public health issue.
Acknowledgments
This work was supported by a National Institute of Health Individual National Research Service Award (NRSA) and by the Yale Institute for Social and Policy Studies, Field Experiment Initiative.
References
- 1.Brown G. Life events and affective disorder: Replications and limitations. Psychosom Med. 1993;55:248–259. doi: 10.1097/00006842-199305000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC. The effects of stressful life events on depression. Annu Rev Psychol. 1997;48:191–214. doi: 10.1146/annurev.psych.48.1.191. [DOI] [PubMed] [Google Scholar]
- 3.Dohrenwend BP. Adversity, stress, and psychopathology. New York: Oxford University Press; 1998. [Google Scholar]
- 4.Larson R, Ham M. Stress and “storm and stress” in early adolescence: The relationship of negative events with dysphoric affect. Devel Psychol. 1993;29:130–140. [Google Scholar]
- 5.Seidman E, Allen L, Aber JL, et al. The impact of school transitions in early adolescence on the self-system and perceived social context of poor urban youth. Child Dev. 1994;65:507–522. [PubMed] [Google Scholar]
- 6.Hankin BL, Abramson LY, Moffitt TE, et al. Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal study. J Abnorm Psychol. 1998;107:128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- 7.Lewinsohn PM, Striegel-Moore RH, Seeley JR. Epidemiology and natural course of eating disorders in youngwomen fromadolescence to young adulthood. J Am Acad Child Adolesc Psychiatry. 2000;39:1284–1292. doi: 10.1097/00004583-200010000-00016. [DOI] [PubMed] [Google Scholar]
- 8.Grant KE, Compas BE, Thurm AE, et al. Stressors and child and adolescent psychopathology: Measurement issues and prospective effects. J Clin Child Adolesc Psychol. 2004;33:412–425. doi: 10.1207/s15374424jccp3302_23. [DOI] [PubMed] [Google Scholar]
- 9.Grant KE, Compas BE, Stuhlmacher AF, et al. Stressors and child and adolescent psychopathology: Moving from markers to mechanisms of risk. Psychol Bull. 2003;129:447–466. doi: 10.1037/0033-2909.129.3.447. [DOI] [PubMed] [Google Scholar]
- 10.Grant KE, Compas BE, Thurm AE, et al. Stressors and child and adolescent psychopathology: Evidence of moderating and mediating effects. Clin Psychol Rev. 2006;26:257–283. doi: 10.1016/j.cpr.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 11.Hankin BL, Abramson LY, Miller N, et al. Cognitive vulnerability-stress theories depression: Examining affective specifity in the prediction of depression versus anxiety in three prospective studies. Cogn Ther Res. 2004;28:309–345. [Google Scholar]
- 12.Taylor SE, Repetti RL, Seeman TE. Health psychology: What is an unhealthy environment and how does it get under the skin? Annu Rev Psychol. 1997;48:411–447. doi: 10.1146/annurev.psych.48.1.411. [DOI] [PubMed] [Google Scholar]
- 13.Thompson RA. Emotion regulation: A theme in search of definition. Monogr Soc Res Child Dev. 1994;59:25–52. [PubMed] [Google Scholar]
- 14.Repetti RL, Taylor SE, Seeman TE. Risky families: Family social environments and the mental and physical health of offspring. Psychol Bull. 2002;128:330–336. [PubMed] [Google Scholar]
- 15.Southam-Gerow MA, Kendall PC. A preliminary study of the emotional understanding of youth referred for treatment of anxiety disorders. J Clin Child Psychol. 2000;29:319–327. doi: 10.1207/S15374424JCCP2903_3. [DOI] [PubMed] [Google Scholar]
- 16.Suveg C, Zeman J. Emotion regulation in children with anxiety disorders. Journal of Clinical Child and Adolesc Psychol. 2004;33:750–759. doi: 10.1207/s15374424jccp3304_10. [DOI] [PubMed] [Google Scholar]
- 17.Silk JS, Steinberg L, Morris AS. Adolescents’ emotion regulation in daily life: Links to depressive symptoms and problem behaviors. Child Dev. 2003;74:1869–1880. doi: 10.1046/j.1467-8624.2003.00643.x. [DOI] [PubMed] [Google Scholar]
- 18.Abela JR, Brozina K, Haigh EP. An examination of the response styles theory of depression in third- and seventh-grade children: A short-term longitudinal study. J Abnorm Child Psychol. 2002;30:515–527. doi: 10.1023/a:1019873015594. [DOI] [PubMed] [Google Scholar]
- 19.Cicchetti D, Toth TL. Child maltreatment. Annu Rev Clin Psychol. 2005;1:409–438. doi: 10.1146/annurev.clinpsy.1.102803.144029. [DOI] [PubMed] [Google Scholar]
- 20.Maughan A, Cicchetti D. Impact of child maltreatment and interadult violence on children’s emotion regulation abilities and socioemotional adjustment. Child Dev. 2002;73:1525–1542. doi: 10.1111/1467-8624.00488. [DOI] [PubMed] [Google Scholar]
- 21.Baumeister RF, DeWall CN, Ciarocco NJ, et al. Social exclusion impairs self-regulation. J Personal Soc Psychol. 2005;88:589–604. doi: 10.1037/0022-3514.88.4.589. [DOI] [PubMed] [Google Scholar]
- 22.Inzlicht M, McKay L, Aronson J. Stigma as ego depletion: How being the target of prejudice affects self-control. Psychol Sci. 2006;17:262–269. doi: 10.1111/j.1467-9280.2006.01695.x. [DOI] [PubMed] [Google Scholar]
- 23.Connecticut Department of Education. Strategic School Profile 2005–2006: New Britain Public Schools. Hartford: Connecticut Department of Education; 2006. [Google Scholar]
- 24.Coddington DR. The significance of life events as etiologic factors in the diseases of children: A study of normal population. Psychosom Res. 1972;16:205–213. doi: 10.1016/0022-3999(72)90045-1. [DOI] [PubMed] [Google Scholar]
- 25.Hammen C. Stress exposure and stress generation in adolescent depression. In: Nolen-Hoeksema S, Hilt LM, editors. Handbook of Depression in Adolescents. New York: Lawrence Erlabaum; In press. [Google Scholar]
- 26.Kovacs M. Children’s Depression Inventory manual. North Tonawanda, NY: Multi-Health Systems; 1992. [Google Scholar]
- 27.Reynolds WM. Assessment of depression in children and adolescents by self-report measures. In: Reynolds WM, Johnston HF, editors. Handbook of depression in children and adolescents. New York: Plenum Press; 1994. pp. 209–234. [Google Scholar]
- 28.March JS, Parker JDA, Sullivan K, et al. The Multidimensional Anxiety Scale for Children (MASC): Factor structure, reliability, and validity. J Am Acad Child Adolesc Psychiatry. 1997;36:554–565. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- 29.Muris P, Merckelbach H, Ollendick T, et al. Three traditional and three new childhood anxiety questionnaires: Their reliability and validity in a normal adolescent sample. Behav Res Ther. 2002;40:753–772. doi: 10.1016/s0005-7967(01)00056-0. [DOI] [PubMed] [Google Scholar]
- 30.Penza-Clyve S, Zeman J. Initial validation of the emotion expression scale for children (EESC) J Clin Child Adolesc Psychol. 2002;31:540–547. doi: 10.1207/S15374424JCCP3104_12. [DOI] [PubMed] [Google Scholar]
- 31.Zeman J, Shipman K, Penza-Clyve S. Development and initial validation of the Children’s Sadness Management Scale. Journal of Nonverbal Behavior. 2001;25:187–205. [Google Scholar]
- 32.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 33.MacKinnon DP, Lockwood CM, Hoffman JM, et al. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation model. In: Leinhart S, editor. Sociological Methodology. San Francisco: Jossey-Bass; 1982. pp. 290–312. [Google Scholar]
- 35.Hu L, Bentler PM. Cutoff criteria for fit indices in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equat Model. 1999;6:1–55. [Google Scholar]
- 36.Camras LA, Ribordy S, Hill J, et al. Recognition and posing of emotional expressions by abused children and their mothers. Dev Psychol. 1988;24:776–781. [Google Scholar]
- 37.Jacobson NS, Dobson KS, Truax PA, et al. A component analysis of cognitive-behavioral treatment for depression. J Consult Clin Psychol. 1996;64:295–304. doi: 10.1037//0022-006x.64.2.295. [DOI] [PubMed] [Google Scholar]
- 38.Kovacs M, Sherrill J, George CJ, et al. Contextual emotion-regulation therapy for childhood depression: Description and pilot testing of a new intervention. J Am Acad Child Adolesc Psychiatry. 2006;45:892–903. doi: 10.1097/01.chi.0000222878.74162.5a. [DOI] [PubMed] [Google Scholar]
- 39.Wolchik SA, Sandler IN, Millsap RE, et al. Six-year follow-up of preventive interventions for children of divorce. A randomized controlled trial. JAMA. 2002;288:1874–1881. doi: 10.1001/jama.288.15.1874. [DOI] [PubMed] [Google Scholar]
- 40.Gross JJ. Antecedent-and response-focused emotion regulation: Divergent consequences for expression, experience, and physiology. J Personal Soc Psychol. 1998;24:224–237. doi: 10.1037//0022-3514.74.1.224. [DOI] [PubMed] [Google Scholar]