Summary
Aim of the study was to investigate, in a randomized prospective trial, air-conducted vestibular evoked myogenic potentials (AC-VEMPs) and bone-conducted vestibular evoked myogenic potentials (BC-VEMPs) before and after successful stapedotomy. Enrolled in the study were 41 consecutive patients (32 female, 9 male; mean age 36 years) (42 ears) with otosclerosis. Audiological evaluations and diagnosis of otosclerosis were made according to the guidelines of the Committee on Hearing and Equilibrium. Successful stapedotomy was carried out in all otosclerotic ears. Air- and bone-conducted 4-frequency pure tone average (4-PTA), air-bone gap (ABG), AC- and BC-VEMPs were evaluated pre- and post-operatively. As far as concerns results, pre-operatively, AC- and BC-VEMPs could be recorded in 9 (21.4%) and 16 (38.1%) otosclerotic ears, respectively. Lower ABG was detected in patients with AC-VEMPs in comparison to those in whom air-conducted potentials (p = 0.032) could not be elicited. At 12-month post-operative follow-up, AC-VEMPs were present in 11 (26.2%) ears, while BC-VEMPs could be elicited in 15 (35.7%) cases. Reduced bone-conduction 4-PTA was observed in patients with BC-VEMPs in comparison to those without recordable bone-conducted potentials pre- and post-operatively (p = 0.003 and p = 0.005, respectively). A significantly (p = 0.022) lower air-conducted 4-PTA was measured post-stapedotomy in patients with BC-VEMPs in comparison to those without elicitable bone-conducted potentials. In conclusion, VEMPs reduced elicitability, in otosclerosis, is likely due to conductive hearing loss and inner ear impairment.
Keywords: Otosclerosis, Stapes surgery, Hearing loss, Vestibular evoked myogenic potentials
Riassunto
L’obiettivo del presente lavoro è di studiare in un trial randomizzato prospettico l’evocabilità dei VEMPs per via aerea e per via ossea prima e dopo l’intervento di stapedotomia. Sono stati inclusi nello studio 41 pazienti (31F/9M; età media: 36 anni) operati per otosclerosi, di cui uno operato bilateralmente, per un totale di 42 orecchi valutati nel pre- e nel post-operatorio. La diagnosi di otosclerosi e le valutazioni audiologiche dei pazienti sono state eseguite seguendo le linee guida del "Committee on Hearing and Equilibrium". Ottimi esiti chirurgici ed audiologici dell’intervento di stapedotomia sono stati riscontrati in tutti i pazienti operati. Per ogni paziente sono stati valutati, nel pre- e nel post-operatorio, il 4-frequency pure tone average (4-PTA) per via aerea e per via ossea, l’air-bone gap (ABG) ed i potenziali evocati vestibolari miogenici per via aerea (AC-VEMPs) e per via ossea (BC-VEMPs). Nel preoperatorio gli AC-VEMPs e i BC-VEMPs sono risultati presenti rispettivamente in 9 (21,4%) ed in 16 (38,1%) degli orecchi valutati; inoltre nei pazienti con AC-VEMPs evocabili nell’orecchio candidato all’intervento sono stati riscontrati valori minori di ABG (p = 0,032) rispetto ai pazienti con AC-VEMPs non evocabili. A 12 mesi dall’intervento di stapedotomia gli AC-VEMPs sono risultati presenti in 11 (26,2%) degli orecchi operati, mentre i BC-VEMPs in 15 (35,7%) degli stessi. Sia nel pre- che nel post-operatorio si sono rilevati valori significativamente minori di 4-PTA per via ossea nei pazienti con BC-VEMPs presenti dopo l’intervento (p = 0,003 e p = 0,005 rispettivamente) rispetto a quelli con BC-VEMPs assenti nello stesso periodo. Infine il 4-PTA per via aerea misurato dopo l’intervento chirurgico è risultato essere minore nei pazienti con BC-VEMPs evocabili rispetto a quelli con gli stessi potenziali non evocabili. I risultati dello studio suggeriscono che la riduzione dell’evocabilità dei VEMPs, nei pazienti otosclerotici, è dovuta alle alterazioni del sistema di trasmissione del suono e ai danni a carico dell’orecchio interno che la malattia procura.
Introduction
Otosclerosis is a primary osteodystrophy of the otic capsule and the middle ear ossicles. It only affects human temporal bones and its prevalence is 1-2% in Caucasians. It is more common in the female sex and shows a familiarity in more than 50% of patients. Clinical onset occurs between 20 and 40 years of age with a slow progressive hearing loss, frequently associated with tinnitus and, more rarely, with vestibular symptoms 1. The histopathological incidence of otosclerosis is 10 times higher than the clinical presentation of the disease 2. Histologically, the disorder is characterised by alternating phases of bone resorption and formation in the temporal bone with a primary localisation of otosclerotic foci around the otic capsule, between the cochlea and the vestibule just anterior to the stapes footplate (fissula ante-fenestram) 3. This close anatomical relationship between the stapes footplate and the vestibule (and the saccule of the otolith organs, in particular) is thought to be responsible for the vestibular symptoms in otosclerosis 4. However, whether vestibular functional tests correlate with the progression of otosclerosis remains to be fully investigated.
Vestibular-evoked myogenic potentials (VEMPs) have recently been added to the traditional audiological and vestibular investigations in otosclerosis. VEMPs are used clinically to record the motor response of the vestibulocollic reflex (VCR) from various muscles in the neck (e.g. sternocleidomastoid or trapezoid muscles). These were first described by Colebatch and Halmagyi and proposed as a clinical test of vestibular function 5. They are short-latency myogenic potentials produced by a sacculocollic reflex evoked by high-level acoustic stimuli, such as short tone burst (STB), click, and logon. VEMPs are generated through a disynaptic reflex, beginning in the saccule and proceeding along vestibular afferent fibres to the vestibular nuclei, then through rapidly conducting projections that synapse with the sternocleidomastoid muscle 6 7, where surface electrodes record the post-stimulatory tonical contraction of the muscle. Only two studies have been published recently to report the influence of otosclerosis on VEMPs responses. Singbartl et al. recorded pre- and post-operative tone bone-conducted VEMPs (BC-VEMPs) in patients with otosclerosis and did not observe any influence of stapedotomy surgery on BC-VEMPs 8. Yang and Young recorded air-conducted VEMPs (AC-VEMPs) and BC-VEMPs in otosclerotic ears not submitted to surgery. In their study, they observed a progressive disappearance of AC-VEMPs first, and then BC-VEMPs, according to the progressive worsening of hearing thresholds 9. However, so far, no studies have ever investigated AC- and BC-VEMPs in otosclerotic ears, before and after stapedotomy.
Aim of this study was to investigate AC- and BC-VEMP responses using air- and bone-conducted logon stimulation before and after stapes surgery. Possible clinical consequences of our findings are reported.
Materials and Methods
Prospectively examined were 41 consecutive caucasian patients (32 female, 9 male), candidate to stapedotomy for otosclerosis at the Area of Otolaryngology, "Campus Bio-Medico University" of Rome (mean age 36 years, range 22-47).
All patients underwent stapedotomy performed by the same surgeon (F.S.). One patient underwent bilateral stapedotomy, while in the others, unilateral stapedotomy was carried out. Overall, 42 otosclerotic ears were considered (Table I). No patient had a positive history for ear discharge, skull trauma, previous ear surgery, or superior dehiscence canal syndrome. Tinnitus was present in 3 (7.1%) subjects. No patient reported vertigo or dizziness.
Table I. Clinical information on 42 ears with otosclerosis.
| No. | Sex | Age (yrs) | Side | Air 4-PTA (dBHL) | Bone 4-PTA (dBHL) | Air-Bone Gap (dBHL) | AC-VEMPs | BC-VEMPs |
| 1 | M | 47 | L | 37.5 | 22.5 | 16 | + | + |
| 2 | F | 35 | L | 57.5 | 31.25 | 32 | - | - |
| 3 | M | 45 | R | 50 | 32.5 | 21 | - | + |
| 4 | F | 22 | R | 66.25 | 38.75 | 32 | - | - |
| 5 | M | 27 | R | 47.5 | 22.5 | 27 | - | - |
| 6 | F | 30 | L | 76.25 | 53.75 | 26 | - | - |
| 7 | F | 39 | L | 28.75 | 8.75 | 21 | + | + |
| 8 | F | 41 | R | 33.75 | 23.75 | 13 | - | + |
| 9 | F | 36 | R | 33.75 | 23.75 | 14 | - | + |
| 10 | F | 33 | R | 70 | 28.75 | 25 | - | + |
| 11 | F | 40 | L | 70 | 47.5 | 26 | - | - |
| 12 | M | 38 | L | 51.25 | 31.25 | 22 | - | - |
| 13 | F | 37 | L | 80 | 42.5 | 42 | - | - |
| 14 | F | 32 | L | 53.75 | 35 | 23 | + | + |
| 15 | M | 35 | L | 36.25 | 22.5 | 15 | + | + |
| 16 | F | 41 | R | 60 | 6.25 | 55 | - | - |
| 17 | M | 34 | L | 66.25 | 32.5 | 34 | - | + |
| 18 | F | 39 | R | 83.75 | 51.25 | 35 | - | - |
| 19 | F | 38 | L | 52.5 | 7.5 | 46 | - | + |
| 20 | F | 37 | R | 50 | 26.25 | 28 | - | + |
| 21 | F | 43 | L | 58.75 | 36.25 | 25 | - | - |
| 22 | F | 42 | L | 35 | 17.5 | 21 | - | - |
| 23 | M | 41 | L | 61.25 | 35 | 28 | - | - |
| 24 | F | 35 | L | 63.75 | 43.75 | 24 | - | - |
| 25 | F | 32 | R | 48.75 | 18.75 | 35 | - | - |
| 26 | F | 30 | R | 27.5 | 10 | 17 | - | - |
| 27 | F | 36 | R | 47.5 | 31.25 | 20 | - | - |
| 28 | F | 37 | L | 81.25 | 47.5 | 40 | - | - |
| 29 | M | 45 | L | 55 | 37.5 | 20 | - | - |
| 30 | F | 40 | R | 47.5 | 18.75 | 33 | - | - |
| 31 | F | 27 | R | 80 | 48.75 | 34 | - | - |
| 32 | F | 37 | R | 55 | 27.5 | 30 | - | - |
| 33 | F | 28 | L | 43.75 | 26.25 | 18 | + | + |
| 34 | F | 22 | L | 77.5 | 57.5 | 19 | - | - |
| 35 | F | 36 | L | 41.25 | 28.75 | 17 | + | + |
| 36 | F | 38 | L | 106.25 | 55 | 54 | - | - |
| 37 | F | 39 | R | 71.25 | 48.75 | 29 | - | - |
| 38 | F | 43 | L | 82.5 | 50 | 35 | - | - |
| 39 | M | 46 | R | 58.75 | 36.25 | 26 | + | + |
| 40 | F | 32 | L | 25 | 11.25 | 14 | + | + |
| 41 | F | 31 | L | 38.75 | 30 | 9 | + | + |
| 42 | F | 37 | R | 87.5 | 52.5 | 40 | - | - |
AC-VEMPs: air-conducted vestibular-evoked myogenic potentials; BC-VEMPs: bone-conducted vestibular-evoked myogenic potentials; PTA: pure tone average; M: male; F: female; R: right; L: left; +: response present; -: response absent.
All the patients enrolled in this study were submitted, pre- and post-operatively, to local check-up on ear, nose, and throat fields, audiological assessment (consisting in pure tone audiometry, tympanometry and stapedial reflexes), and VEMPs test. Of these patients, 12 underwent high-resolution computed tomography (HRCT) for further evaluation of the disease. The audiological evaluation was made according to the guidelines of the Committee on Hearing and Equilibrium of the American Academy of Otolaryngology-Head and Neck Surgery Foundation, Inc. 10. In all patients, 4-frequency pure tone average (4-PTA) was measured for both air- and bone-conduction. Air-bone gap [(air-conducted threshold) - (bone-conducted threshold)] was calculated at 500, 1000, 2000, and 3000 Hz.
All patients were submitted to stapedotomy with success (closure of the air-bone gap within 10 dBHL). Post-stapedotomy audiological and VEMPs testing was carried out one, six, and twelve months after surgery. VEMPs were recorded with an Amplaid MK12 (Amplaid, Milan, Italy), as described in the medical literature 7 11. The electromyographic activity of the sternocleidomastoid (SCM) muscle was recorded while patients were lying supine on a bed and asked to raise their head off the bed in order to activate their neck flexors bilaterally and the saccular receptor were acoustically stimulated. The recording electrodes were placed at the middle third of the SCM and referenced to electrodes placed on the medial clavicle, bilaterally. The ground electrode was placed on the upper edge of the sternum. Attention was paid to place bilateral electrodes on the symmetrical site. The resulting impedance of the recording electrodes were maintained below 3 kΩ by cleaning the skin with a peeling gel. VEMPs were recorded after stimulation with logon. The eliciting stimuli were delivered via earphones (Telephonics THD49), for elicitation of VEMPs evoked by air-conducted signal, and via bone conductor (RadioEar B71) placed at the mastoid directly behind the auricle for evocation of responses evoked by bone-conducted stimuli. Therefore, air and bone conducted stimuli were applied in this study.
Logon is a pure tone, with amplitude modulated by a Gaussian function; it can be considered as the best compromise between a rectangular wave and a continuous pure tone 12. As suggested by Valli et al., logon of 500 Hz frequency was delivered at an intensity of 130 dB SPL and 70 dB SPL for air- and bone-conducted stimuli respectively. Logon rate was 4/s, while stimuli duration was 10 milliseconds 13. Stimuli (air- and bone-conducted click and logon) intensity was chosen by selecting the maximum output acoustic power of the machine used (Amplaid MK12). The Authors of the present study already experienced the eliciting capacity of VEMPs without acoustic trauma of such stimulation (data accepted for publication but not yet published).
Analysis time was 100 ms. Potentials were amplified and band pass filtered (10-1500 Hz). Recordings were obtained averaging 200 stimuli and two traces from each test were obtained in order to assess reproducibility. In each trace, the latency and amplitude of the positive-negative waves P1/N1 were considered. The study protocol was approved by our Institutional Review Board. Patients gave their written, informed consent to participate in the study.
Statistical analyses were performed using the Statistical Package for Social Sciences Software (SPSS 10.0 for Windows, SPSS Inc., Chicago, IL, USA) and STATA 7 (Stata Corporation, College Station, TX, USA; http://www.stata.com). Data are shown as mean and standard deviation or as median and inter-quartile range. Parametric (Student’s t-test) and non-parametric (Wilcoxon test for paired data and Mann-Whitney U-test for non-paired data) tests were used to compare different values. The criteria for statistical significance was set at a P-value of ≤ 0.05 (two-tailed).
Results
Pre-operatively, mean air-conducted 4-PTA was 57.11 (±18.66), while mean bone-conducted 4-PTA was 32.32 (±13.95). Mean ABG in our otosclerotic ears was 27.16 (±9.30) dBHL; AC-VEMPs were present in 9 (21.4%) ears while BC-VEMPs were recordable in 16 (38.1%) cases on the side candidate to surgery. All the patients with AC-VEMPs presented also BC-VEMPs on the otosclerotic ear (Table I).
After stapedotomy, all patients showed the closure of ABG within 10 dBHL (mean post-operative ABG = 9.8 dBHL). Mean air-conducted 4-PTA was 37.55 (±14.46), while mean bone-conducted 4-PTA was 28.36 (±13.42). AC-VEMPs were present in 11 (26.2%) ears (9 of which already presented VEMPs before surgery). BC-VEMPs were recordable in 15 (35.7%) cases. All subjects with elicitable AC-VEMPs presented also BC-VEMPs on the operated side. No difference in audiological and VEMPs results were observed during the 12-month follow-up. No relationship was found between patients’ age and VEMPs elicitability, either pre- or post-operatively. Five patients experienced transient vertigo after surgery, which recovered within 24 hours. No correlation was found between the clinical occurrence of vertigo and the elicitability of VEMPs.
As far as concerns the correlation between audiological test results and VEMPs, pre-operatively, a statistically significant reduction of ABG (p = 0.032) and bone-conducted 4-PTA (p = 0.027) were observed in patients with AC-VEMPs in comparison to those in whom vestibular evoked myogenic potentials were not elicitable. Furthermore, reduced bone-conducted 4-PTA was detected in subjects with elicitable BC-VEMPs in comparison to those without recordable potentials, both pre-operatively (p = 0.003) and 12 months after surgery (p = 0.005).
At the post-operative follow-up, the patients with recordable BC-VEMPs showed significantly (p = 0.022) lower air-conducted 4-PTA with respect to those without elicitable vestibular-evoked myogenic potentials (Table II).
Table II. Correlations between audiological test results with air- and bone-conducted vestibular evoked myogenic potentials before and after stapedotomy.
| AC-VEMPs (+)/11 Ears | AC-VEMPs (-)/31 Ears | p value | BC-VEMPs (+)/15 Ears | BC-VEMPs (-)/27 Ears | p value | |
| Pre-operative | ||||||
| Mean Air 4-PTA | 39.20 | 63.46 | NS | 44.41 | 64.02 | NS |
| Mean Bone 4-PTA | 24.43 | 35.12 | 0.027* | 24.25 | 36.80 | 0.003* |
| Mean Air-Bone Gap | 16.90 | 30.80 | 0.032* | 21.26 | 30.44 | NS |
| Post-operative | ||||||
| Mean Air 4-PTA | 30.56 | 40.04 | NS | 30.83 | 41.29 | 0.022* |
| Mean Bone 4-PTA | 22.15 | 30.56 | NS | 20.83 | 32.54 | 0.005* |
| Mean Air-Bone Gap | 8.63 | 10.22 | NS | 10.40 | 9.48 | NS |
AC-VEMPs: air-conducted vestibular evoked myogenic potentials; BC-VEMPs: bone-conducted vestibular evoked myogenic potentials; PTA: pure tone average; NS: non-significant difference; * p < 0.05.
Discussion
Otosclerosis is among the most common causes of progressive hearing loss in Caucasians 1. Although vertigo or dizziness is known to occur in about 20% of cases 14, the possible saccular origin of such symptoms has not been investigated in detail as yet. Only two papers have been published reporting evaluation of VEMPs in otosclerotic ears 8 9, but no Author has ever analyzed both AC-VEMPs and BC-VEMPs before and after stapedotomy in patients affected by otosclerosis.
The results of the present study confirm the reduction of both AC- and BC-VEMPs elicitability in otosclerotic patients in comparison to healthy subjects 15, as already reported in the literature. In particular, pre-operatively, AC-VEMPs were recordable in 9/42 (21.4%) of the ears under study in the present investigation, while BC-VEMPs were elicitable in 16/42 (38.1%) of them. Although the cause of the present findings is not completely clear, it is likely due to two causes: first of all, the air-bone gap, which is considered to be responsible for the pre-operative difference in elicitability between AC- and BC-VEMPs. This hypothesis is confirmed by the significantly lower pre-operative ABG in patients with AC-VEMPs in comparison to those with non-recordable air-conducted vestibular-evoked myogenic potentials (16.90 vs. 30.80 dBHL), and by the partial increase of AC-VEMPs elicitability (26.2%) after ABG closure post-operatively. Secondly, an inner ear impairment, which is likely responsible for the low elicitability of BC-VEMPs both pre- and post-operatively, and the high frequency (73.8%) of absence of AC-VEMPs despite the ABG closure after stapedotomy. Although the cause of inner ear damage is not clear, it is possible that otosclerosis can influence the generation of VEMPs due to an ototoxic effect of substances produced by otosclerotic foci on saccular receptors 16.
Our results also show that even if all patients presented an ABG closure, after stapes surgery, a not statistically significant number of new patients had recordable AC-VEMPS after surgery (only 3 new patients compared to those with recordable AC-VEMPS already pre-operatively). None with no-recordable BC-VEMPS pre-operatively presented BC-VEMPS after surgical treatment. These data suggest that even if the operation restores transmission of sound, it does not influence the elicitability of both AC-VEMPS and BC-VEMPS, in agreement with the literature 8.
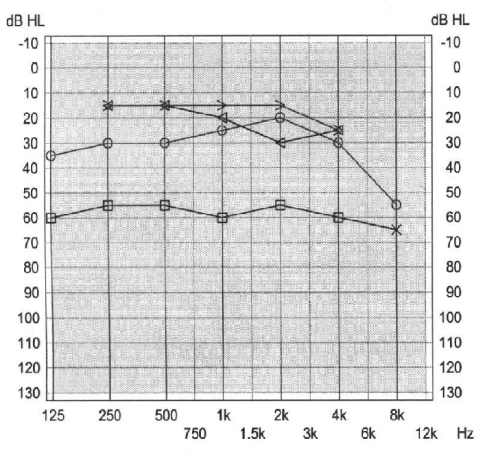
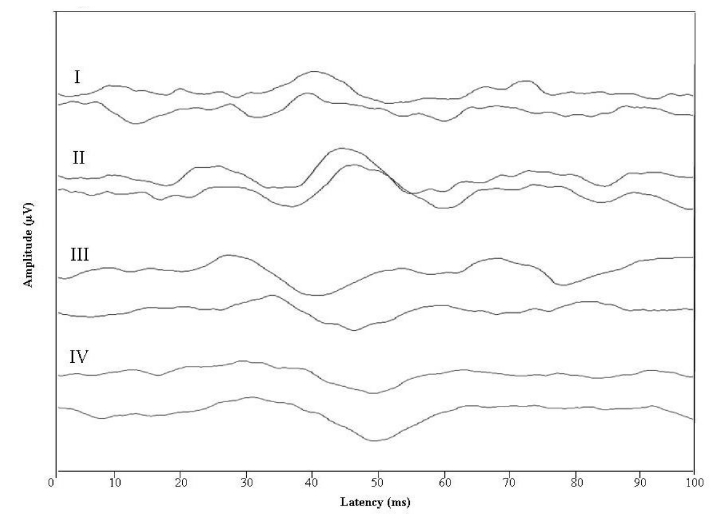
As shown in Figures 1 and 2, a 47-year-old male, submitted to successful right stapedotomy 2 years earlier, candidate to left stapedotomy for otosclerosis, revealed absence of AC- and BC-VEMPs on both ears. HRCT showed otosclerotic foci extending to the circumferential footplate and the adjacent area around the vestibule (Fig. 3) and possibly responsible for inner ear impairment. This hypothesis seems to be confirmed by the statistically significant lower bone 4-PTA in patients with BC-VEMPs in comparison to those with non-recordable bone-conducted vestibular-evoked myogenic potentials both pre- and post-operatively (24.25 vs. 36.80 dBHL pre-operatively and 20.83 vs. 32.54 dBHL post-operatively). Therefore, the development of otosclerotic foci in the otic capsule seems to be associated not only with a progressive worsening of bone-conduction hearing thresholds, but also with an impairment of the vestibule responsible for BC-VEMPs non-elicitability in those patients.
Fig. 1.
47-year-old male, otosclerosis, bilaterally, submitted to right stapedotomy two years earlier (case no. 1). Audiometry reveals moderate mixed-type hearing loss for all frequencies on left ear and mild mixed-type hearing impairment on right ear.
Fig. 2.
Vestibular evoked myogenic potentials elicited by air-conducted (I = right ear; III = left ear) and bone-conducted (II = right ear; IV = left ear) logon stimulation showing absent responses, bilaterally.
Fig. 3.
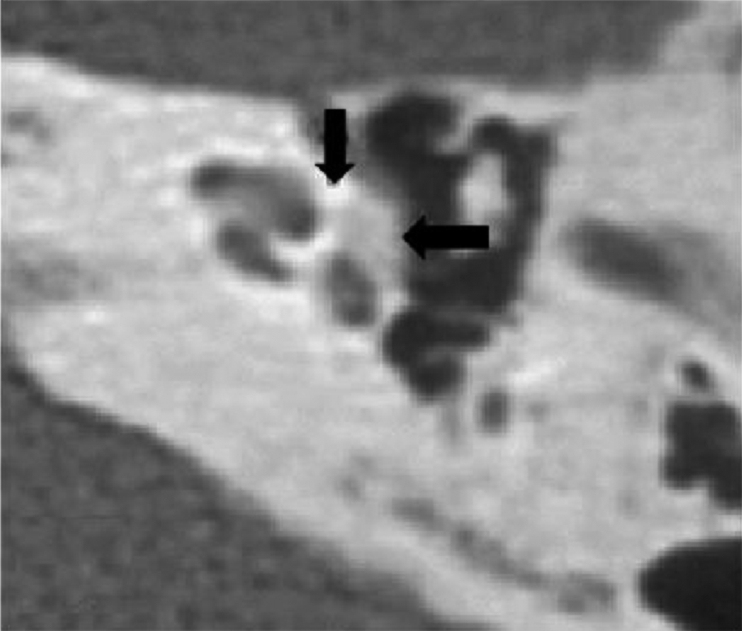
High resolution computed tomography of left ear, axial scan, showing otosclerotic foci (arrows) extending to oval window and vestibule
Further studies are needed to completely elucidate the pathogenesis of VEMPs impairment in otosclerosis and understand the possible usefulness of VEMPs for the differential diagnosis of cochlear otosclerosis from some other causes of sensorineural hearing loss in which VEMPs are usually recordable 17.
References
- 1.Salvinelli F, Casale M, Di Peco V, et al. Stapes surgery in relation to age. Clin Otolaryngol Allied Sci 2003;28:520-3. [DOI] [PubMed] [Google Scholar]
- 2.Menger DJ, Tange RA. The aetiology of otosclerosis: a review of the literature. Clin Otolaryngol Allied Sci 2003;28:112-20. [DOI] [PubMed] [Google Scholar]
- 3.Friedmann I, Arnold W. Pathology of the Ear. Edinburgh, UK: Churchill Livingstone; 1993. p. 369. [Google Scholar]
- 4.Yoon TH, Paparella MM, Schachern PA. Otosclerosis involving the vestibular aqueduct and Ménière’s disease. Otolaryngol Head Neck Surg 1990;103:107-12. [DOI] [PubMed] [Google Scholar]
- 5.Colebatch JG, Halmagyi GM. Vestibular evoked potentials in human neck muscles before and after unilateral vestibular deafferentation. Neurology 1992;42:1635-6. [DOI] [PubMed] [Google Scholar]
- 6.Murofushi T, Curthoys IS, Topple AN, et al. Responses of guinea pig primary vestibular neurons to clicks. Exp Brain Res 1995;103:174-8. [DOI] [PubMed] [Google Scholar]
- 7.Picciotti PM, Fiorita A, Di Nardo W, et al. Vestibular evoked myogenic potentials in children. Int J Pediatr Otorhinolaryngol 2007;71:29-33. [DOI] [PubMed] [Google Scholar]
- 8.Singbartl F, Basta D, Seidl RO, et al. Perioperative recordings of vestibular-evoked myogenic potentials in otosclerosis. Otol Neurotol 2006;27:1070-3. [DOI] [PubMed] [Google Scholar]
- 9.Yang TL, Young YH. Vestibular-evoked myogenic potentials in patients with otosclerosis using air- and bone-conducted tone-burst stimulation. Otol Neurotol 2007;28:1-6. [DOI] [PubMed] [Google Scholar]
- 10.Committee on Hearing and Equilibrium guidelines for the evaluation of results of treatment of conductive hearing loss. American Academy of Otolaryngology-Head and Neck Surgery Foundation, Inc. Otolaryngol Head Neck Surg 1995;113:186-7. [DOI] [PubMed] [Google Scholar]
- 11.Picciotti PM, Fiorita A, Di Nardo W, et al. VEMPs and dynamic posturography after intratympanic gentamycin in Ménière’s disease. J Vestib Res 2005;15:161-8. [PubMed] [Google Scholar]
- 12.Davis H. Principles of electric response audiometry. Ann Otol Rhinol Laryngol 1976;85(Suppl 28):1-96. [PubMed] [Google Scholar]
- 13.Valli P, Valli S, Vicini C. Our methodological contribution. In: Vestibular Evoked Myogenic Potentials. First International Course, Bertinoro (Italy) 2002. [Google Scholar]
- 14.Gros A, Vatovec J, Sereg-Bahar M. Histologic changes on stapedial footplate in otosclerosis. Correlations between histologic activity and clinical findings. Otol Neurotol 2003;24:43-7. [DOI] [PubMed] [Google Scholar]
- 15.Welgampola MS, Colebatch JG. Characteristics and clinical applications of vestibular-evoked myogenic potentials. Neurology 2005;64:1682-8. [DOI] [PubMed] [Google Scholar]
- 16.Linthicum FH Jr, Filipo R, Brody S. Sensorineural hearing loss due to cochlear otospongiosis: theoretical considerations of etiology. Ann Otol Rhinol Laryngol 1975;84:544-51. [DOI] [PubMed] [Google Scholar]
- 17.Chen CN, Young YH. Differentiating the cause of acute sensorineural hearing loss between Ménière’s disease and sudden deafness. Acta Otolaryngol 2006;126:25-31. [DOI] [PubMed] [Google Scholar]