Summary
Malignant tumours of the upper gum and hard palate account for 1-5% of malignant neoplasms of the oral cavity; two thirds of the lesions which involve these areas are squamous cell carcinomas. Most of these carcinomas are diagnosed late, when they invade the underlying bone. The procedures of choice for removal are: alveolectomy, palatectomy, maxillectomy, which may be total or partial. Surgical reconstruction of the defect may be carried out using a wide range of microvascularized flaps: osteomuscolocutaneous of the internal iliac crest, an osteocutaneous flap of the fibula or scapula, fascia, or osteocutaneous radial flap, or a pedicled flap of temporal muscle. These flaps are supported by single or multiple obturator prostheses. Rehabilitation via palatal obturators is preferred in patients with a poor prognosis or in weak condition. Rehabilitation aims to: restore the separation between the oral and nasal cavities, enable the patient to swallow, maintain or provide mastication, sufficient occlusion and mandibular support, support the soft facial tissues, re-establish speech and restore an aesthetically pleasing smile. Hence, it is crucial to work in close cooperation with the staff who makes the prosthesis and who evaluates the case when the surgery is planned and obtains the necessary gnatological, anatomical and functional information. Thereafter, during the surgical stage, for the immediate obturators, or in the successive days, for the temporary obturators, work is devoted to making the prostheses. In this regard, the Odonto-prostheses Service of the Stomatological Clinic does not follow a rigid protocol but materials and techniques are selected on a personal basis, according to the features of each individual clinical case. Mobile rehabilitative systems are the systems of choice, both of which related to the traditional concepts of retention and stability and systems of self-stabilizing prostheses according to J. Dichamp, albeit modified in materials, limiting, when possible the use of prostheses which are fixed on natural teeth, on appliances or combined.
Keywords: Oral cavity, Upper jawbone, Malignant tumours, Palatal resection, Obturator prostheses
Riassunto
I tumori maligni della gengiva superiore e del palato duro rappresentano l’1-5% delle neoplasie maligne del cavo orale ed i due terzi delle lesioni che coinvolgono tali aree sono carcinomi a cellule squamose. La maggior parte di questi carcinomi vengono diagnosticati tardivamente, quando invadono il tessuto osseo sottostante. Le procedure di scelta per l’asportazione sono: alveolectomia, palatectomia e maxillectomia, totale o parziale. La ricostruzione chirurgica del deficit può essere effettuata con una grande varietà di lembi microvascolarizzati: osteomuscolocutaneo di cresta iliaca interna, osteocutaneo di fibula o di scapola, fascio od osteocutaneo radiale; oppure con un lembo peduncolato di muscolo temporale. A questi si affianca la protesizzazione mediante otturatori palatali, in modo isolato o combinato. Nei pazienti defedati o con cattiva prognosi preferiamo la riabilitazione mediante otturatori palatali. Gli obiettivi che questa persegue sono: ripristinare la separazione tra cavità nasale e orale, permettere la deglutizione, mantenere o fornire masticazione, occlusione e sostegno mandibolare adeguati, sostenere i tessuti molli del volto, ristabilire la loquela ed una consona estetica del sorriso. È pertanto di assoluta importanza la stretta collaborazione con il protesista riabilitatore che valuta il caso durante la fase di programmazione chirurgica, raccogliendone le necessarie informazioni gnatologiche, anatomiche e funzionali. In seguito, durante la fase chirurgica per gli otturatori immediati o nei giorni successivi per gli otturatori temporanei, si procede all’allestimento dei manufatti. A questo proposito il Servizio di Odontoprotesi della U.O. di Clinica Stomatologica non segue rigidi protocolli, ma stanti le diversità che configurano ogni caso clinico, personalizza volta per volta materiali e tecniche. La scelta è di preferire sistemi riabilitativi mobili, siano essi legati ai concetti tradizionali di ritenzione e stabilità che a quelli della protesi autostabile secondo J. Dichamp, seppur modificata nei materiali, limitando quanto più possibile il ricorso a soluzioni protesiche fisse su denti naturali, su impianti o combinate.
Introduction
The morphology of the jaw has a functional and aesthetic role. The palate separates the oral cavity from the nasal fossa and occlusion between the dental arches provides the mandible with the stability which enables the pharyngeal muscles to initiate the critically important act of swallowing. Aesthetically, the maxillary bone is responsible for the projection of the nose, cheeks and hemi-face. A maxillary-palatal defect may have serious consequences as far as concerns the relationship between form and function: inability to chew and swallow, disorders in phonation and important psychological implications 1. Malignant tumours of the upper gum and hard palate account for 1-5% of malignant neoplasms of the oral cavity; two thirds of the lesions which involve these areas are squamous cell carcinomas. Most of these carcinomas are diagnosed late, when they invade the underlying bone.
Today, treatment of malignant neoplasms of the hard palate comprises radical surgical resection having previously evaluated the location and extent of the lesion, histotype, patient’s age and general state of health. The preferred procedures for removal of carcinomas of limited size (T1N0) of the hard palate and upper maxillary are: alveolectomy and palatectomy which lead to a small deficit which can be reconstructed via simple repair surgery using a local pedicled flap. However, stage T2-T4 carcinomas require more demolitive surgery, such as: type I partial maxillectomy (resection of a single wall), type II subtotal maxillectomy (resection of ≤ 5 walls), type IIIA total maxillectomy (resection of all 6 walls with preservation of the orbital contents), type IIIB (resection of all 6 walls with orbital exenteration), type IV orbito-maxillectomy (resection of 5 walls, orbital exenteration and preservation of the hard palate). This results in an extensive maxillary-palatal deficit and the surgeon, already during clinical pre-surgery evaluation, is faced with a wide range of reconstructive surgical techniques. The defect can be repaired using free microvasularized flaps (osteo-musculocutaneous of the internal iliac crest, osteo-cutaneous flap of the fibula or scapula, fascia, or osteo-cutaneous radial flap) or pedicled flaps (temporalis muscle flap) 2 3 or by leaving a wide breach which will heal spontaneously, on which it is possible to place a stomatologic prosthesis which may be mobile (palatal obturators) or permanent (osteo-integrated implant).
In the literature, Rogers et al. have reported that there is no difference in the quality of life between the two types of treatment, however, if following palatectomy or total maxillectomy, insufficient bone tissue remains then osteointegrated implants cannot be placed 4.
Albeit, it is well established, among those involved in maxillo-facial rehabilitation, that the fewer the teeth remaining in the arch, the more complicated is the closure of the maxillary defects by means of flaps. In particular, the separation between the oral and nasal cavity with a muscular diaphragm which does not rest on hard tissue leads to a mobile support, for which it is impossible to carry out adequate impressions. Moreover, the support thus provided to the prosthesis gives way during mastication loads.
Materials and Methods
In our clinic, use of palatal obturators is generally preferred since they offer a safe oncological follow-up in patients at a high risk of local recurrences and a rapid, inexpensive restoration in terms of aesthetic appearance, phonation and mastication.
Palatal obturators may be used alone or in combination, integrating plastic reconstructive surgery. Various methods and techniques have been described for the preparation of obturator prostheses: it is possible to create an obturator with full or partial dentures on the basis of existing dentition.
One of the main problems of an obturator maxillary prosthesis is weight, the larger the defect the heavier the prosthesis, to the extent that for defects of over a certain size the force of gravity prevails over the capacity of retention of the substructures and residual elements. The approach we follow is to create, via our method, obturators the bulb of which is hollow, hence it is possible to maintain the weight within acceptable values, comparable to the weight of a normal complete upper prosthesis. This also offers a harmonic resonance box which enhances the patient’s phonation. The prosthesis, initially applied in a single block, is then milled to make it lighter and more comfortable. An impression is made of the opening, used to insert the milling cutter, and a resin surface is prepared which will close the opening.
The type of palatal obturator, we now use, is defined as "self-stabilizing" by J. Dichamp and has a silicon portion which adapts perfectly to the maxillectomy and a device on the opposite surface which anchors the dentures in acrylic resin 5. The layer of silicon closes the defect also in the absence of a prosthesis, thereby permitting the defect to be closed and sealed immediately. A grooved anchoring system gives maximum retention to the prosthesis even if there is no remaining dentition or underlying support. The obturator, in silicon, does not give rise to problems of deformation or growth of fungus on the surface for at least 3 years.
The present report refers to 3 cases treated at the Odonto-prosthesis Unit of the Odontriatric and Stomatological Clinic, University Hospital of Trieste.
Case 1
A 62-year-old female suffering from squamous carcinoma stage T4aN0M0 involving the left hard palate, the left inferior nasal fossa with the initial invasion of the floor of the left maxillary sinus who, in February 2007, underwent inferior-anterior maxillectomy and rehabilitation with a mobile, partially hollow palatal prosthesis with dentures (Fig. 1a, b).
Fig. 1a.

Intra-oral view between oral cavity and left nasal fossa following left anterior maxillectomy.
Fig. 1b.

Completed hollow obturator prosthesis, initially used by the patient, later substituted with a self-stabilizing prosthesis.
Later, the patient was fitted with a partially hollow palatal obturator of a self-stabilising type, comprising three reciprocally stable parts, allowing separation of the oral and nasal cavities also in the absence of a prosthesis with dentures (Fig. 2).
Fig. 2.

Silicon layer, on resin structure with part with dentures.
Case 2
A 77-year-old male with squamous cell carcinoma (SCC) of verrucoid pattern of the hard palate (T2N0M0) located in the right median-paramedian who underwent, in July 2007, an inferior-lateral maxillectomy and functional dissection of the right lateral-cervical lymph node (Fig. 3 a – c).
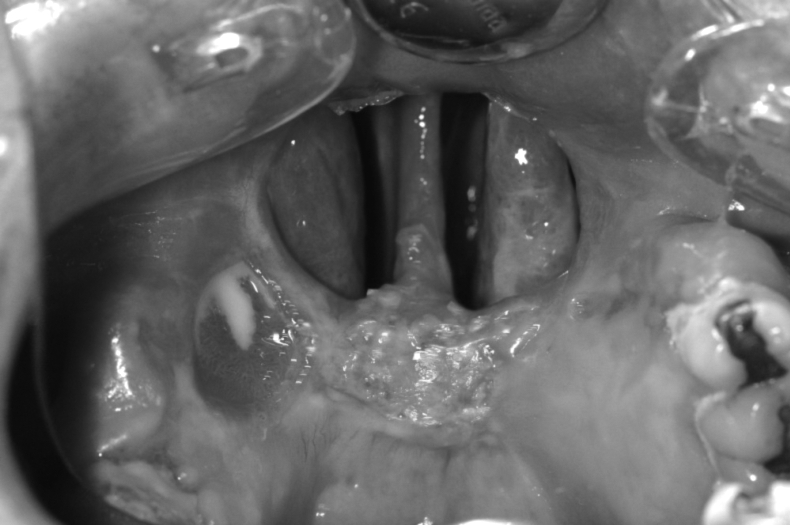
Fig. 3a.
Intra-oral view of the lateral post-maxillectomy defect.
Fig. 3c.

Front view of the lower hemi-face with complete prosthesis.
Case 3
A 68-year-old male with SCC (T3N0M0) involving the hard palate on the median line and infiltration of the floor of the nasal fossa, the third anterior-inferior of the nasal septum and the columella.
Prior to surgery, a stomatological evaluation was carried out to prepare the obturator prosthesis.
In January 2007, a paralateronasal approach was taken for inferior median maxillectomy, resection of the nasal septum involved and the area of the columella, opening up the area between the oral cavity and the floor of the nasal fossas. Plastic surgery of the soft pericolumella tissues was carried out with a graft of cartilage from the third median and posterior of the nasal septum. During surgery, a stomatological re-evaluation was made in order to obtain an impression of the defect to be treated (Fig. 4a – c).
Fig. 4a.
Intra-oral view of the posterior post-maxillectomy defect.
Fig. 4c.

Side view of the profile of the inferior hemi-face with prosthesis.
Discussion
Rehabilitation of the deficit, in the oral cavity and dentition following midface-palatal-maxillectomy, can be achieved by using an obturator prosthesis or a vascularised free-flap containing a bone segment.
Generally, the palatal obturator is used as a simple reconstruction solution for minor palatal defects, whilst larger maxillary-palatal defects represent a challenge for functional and aesthetic reconstruction in both solutions 6.
The obturator prosthesis offers several advantages, which include the possibility to immediately restore dentition without need of further surgery and enables the residual cavity to be kept under control in case of recurrences of the disease. On the other hand, the flap composed of vascularised bone provides permanent closure of the oral-nasal passage with an osteo-integrated implant, but as reported by Cordeiro et al. there are systemic complications in 11.7% of the patients and in 9.1% re-exploration is necessary because the vessels of the free flap are compromised with partial necrosis in 1.8% 2.
Optimal reconstruction of the post-maxillectomy defect is still controversial according to Rogers et al. who compared the repair via obturator or free flap in relation to the function and the quality of life recovery-dependent 3. Reconstructive surgery has various options: non-vascularised grafts, local-regional flaps, free flaps or obturator prostheses. Each technique has its advantages and disadvantages; however, the obturator prosthesis permits a satisfactory reconstruction and the success is partly correlated to the entity of the extension of the resection of the vertical and horizontal components, i.e., to a quarter or less of the hard palate and to a third or less of the soft palate. The subjective outcomes reached are similar and generally the evaluation via Health-related Quality of Life questionnaires reveals that the patients who have undergone rehabilitation with obturator prostheses are satisfied. Furthermore, there are no statistically significant differences between the groups treated with free flaps or palatal obturators with regard to language, swallowing, appetite and correlated depression 4.
The maxillary-facial prosthesis is often correlated with properties of retention, which prevent nasal speech and the passage of liquids into the nasal cavity. Etienne et al. maintain that retention is easier to obtain in the clinical management of patients with maxillectomy with dentition compared to those without. The structure of the prosthesis obturator in patients with partial dentition usually comprises clasp components. Furthermore, the use of precise clasps in patients with maxillectomy with dentition may lead to a significant functional improvement guaranteeing aesthetic advantages 7.
In certain difficult post-operative situations, such as a jaw without dentition and/or extensive resection, Aydin et al. maintain that a fixed prosthesis might be considered similar to a traditional prosthesis. The Authors report, moreover, cases of osteonecrosis of the upper mandibular in patients with osteointegrated implants following radiotherapy. Indeed, one of the problems in the use of implants for maxillary obturators is the location of irradiation and recently most authorities hold that irradiation of the jaw is a contraindication for the placement of an implant 8.
According to Blair et al. maxillary resection has a high level of morbidity with significant functional and psychological implications for the patient. To re-establish functionality adequate closure of the defect is essential to prevent the passage of air, liquid and food between the nasal and oral cavity. Moreover, in wide resections, the obturator supports the facial tissues 9.
Weir et al. hold that for an extensive, composite defect of the oral-mandibular area, in the surgical treatment of T3 and T4 carcinomas, the best procedure for an aesthetic and functional result is a combined reconstruction with an osteomusculocutaneous free flap of fibula and an anterior-lateral of thigh. This operation, however, requires an otolaryngological team and two teams of micro-surgeons. They report complete survival of the flap in 90.9% of cases, partial necrosis in 6.8% and complete loss of the flap in 2.3% of cases 10.
Jones et al. report, in patients with carcinoma of the oral cavity who underwent resection and immediate jaw reconstruction with an osteocutaneous flap, local recurrences or a second tumour in the aero-digestive tract of 15% in synchronous lesions and 4% in metachronous; this requires the use of a second microvascular flap the function of which is merely palliative 11.
A retrospective analysis of oral-mandibular carcinomas carried out from 1997 to 2000 at the Chang Chang Memorial Hospital reported that 70% of tumours were diagnosed at stage IV while the remaining 30% had recurrences of carcinoma. Of these patients, 30.8% needed a salvage secondary reconstruction using a fibula osteoseptocutaneous flap, with a success rate of 90%. The main complications occurred at a rate of 69.2%, and the most common was the extrusion of plaque which occurred in 46.15% of patients. Other complications included the deficit of soft tissues with deformation of the lateral mandibular outline of the face, intra-oral retraction with loss of the gingivobuccal sulcus, oral incontinence, lockjaw, osteoradionecrosis 12.
According to Chiapasco et al., the exclusion criteria for treatment with implants are: a) patients with very poor prognosis or whose health is systemically compromised; b) patients who have undergone resection of the posterior part of the maxillary or the mandibular with sufficient remaining dentition to guarantee acceptable mastication; c) patients with recurrences of oral carcinoma but who continue to use alcohol or tobacco; or d) non compliant patients. The only limitation of the fibula free flap may be the height of the step of over 14 mm. This can create aesthetic problems, in particular in patients who have residual dentition on the healthy side 3.
The success of a total or subtotal bilateral obturator depends on the volume of the defect and on the remaining soft and hard palate, essential for retention, stabilisation and support to the prosthesis.
The weight of the obturator can act as a dislocating force, hence the prosthesis should be as light as possible.
The design of the obturator for partial or total post-maxillectomy provides for the use of obturators which are open or hollow inside, with air internally or hollow obturators comprising two parts. A multi-disciplinary treatment plan is essential to achieve adequate retention and functioning of the prosthesis.
Ortegon et al. described an original anchoring technique of the anterior nasal opening to increase the anterior retention of a hollow obturator in a bilateral subtotal defect post-maxillectomy. The method is simple to carry out and can be used for immediate, temporary and/or definitive closure. Ten days after surgery a temporary obturator is prepared in hydrocolloid, the impression of which is set up on a stock tray in plaster. During follow-up, a custom tray in acrylic light polymer resin is used to prepare a functional impression in silicon. The mould is coated in wax, while the palatal outline is formed by a polymerised acrylic resin. A "handle" is added to the palatal surface and remodelled to facilitate the correct intra-oral position, then a posterior extension is attached above the remaining third of the soft palate with a coating in resistant material, which is positioned to close the lateral and posterior wall of the pharynx so as to ensure an excellent functional result. The Author mentions various methods for the retention of a bilateral complete obturator, which can be supported: 1) using the remaining mouth structures, as the third posterior of the soft palate; 2) supporting the obturator with a lateral healing band; 3) extending the prosthesis extra-orally within the nasal fossa; 4) fixing it to osteointegrated implants 13.
Management of the patient, in our clinic, takes place in three basic stages: the pre-surgery stage, when the stomatologist gathers gnatological, anatomical and functional information; immediate post-operative period, if it is not possible during surgery, to permit the stomatologist to set up temporary prostheses which are personalised in terms of technique and materials. Since the extent of the surgical defect stabilises approximately one year after surgery and the oral cavity of the patient may possibly undergo chemo-radiotherapy there may be further structural remodelling and several palatal obturators may be required post-surgery. Late post-operative period, after 12 months, when clinical recovery is complete and there are no recurrences of the disease, the positioning of a definitive obturator is planned, as described in the literature 7.
At the end of the demolitive operation of inferior maxillectomy, a breach is created at a level of the floor of the nasal fossa or maxillary sinus, which is filled with Vaseline-impregnated gauze fixed to the surrounding structures by stitches. Nutrition is temporarily (7-14 days) enteral via nasal-gastric tube with good compliance in patients.
In the period immediately after surgery, patients undergo an initial speech therapy cycle which evaluates the oral-pharyngeal phases of swallowing, nasal resonance and quality of speech; discharge is planned with oral nutrition on the 10th-12th day.
It is important that the clinician does not neglect the modifications to the prosthesis in order to prevent nasal emission during speech and regurgitation of food 13.
Crucial to good results is the cooperation between the stomatologist and the otolaryngologist already prior to surgery in order to set up immediately after surgery a temporary obturator, which can be modelled on the basis of the structural evolution of the oral cavity until complete recovery from surgery when a definitive mobile obturator can be made.
Conclusions
"No single flap or technique is sufficient to reconstruct all midfacial defects. The choice of free tissue transfer should be tailored to the needs of the individual defect and the desires of the individual patient. Loss of mid-facial structures secondary to tumour extirpation has significant functional (speech, mastication and swallowing) and aesthetic consequences. The variable loss of soft tissue and/or bone leading to collapse of the lip, cheek and peri-orbital soft tissues as well as palatal competence present a challenging dilemma for reconstructive surgeons. Common reconstructive goals include the need to obtain a healed wound, separate the oral and sino-nasal cavities, support the orbit, and restore facial contours. In addition, restoration of a functional maxillary dentition is essential. No single reconstructive technique has been described to achieve all of these goals. Placement of a maxillary prosthesis has been a traditional and reliable method for the obturator of maxillary defects. Although adequate in many patients, the prosthesis must be in place for speech and swallowing. It must be removed and cleaned on a regular basis, and the patient must maintain meticulous hygiene of the maxillary cavity" 14.
The most common issues in prosthesis treatment of patients who have undergone maxillectomy are: lack of support, retention and stability.
The palatal obturator restores: mastication, swallowing, articulation and intelligibility of speech and the contour of the midface.
Rehabilitation with an obturator prosthesis is functional, reliable/safe, easy to build and has a low level of invasiveness. Three-dimensional reconstruction, on the other hand, is complex as it requires longer operations given the invasive nature of reconstruction methods with lower patient tolerance, a high risk of systemic complications or very poor prognosis of the donor site 15. Further features which have been reported in favour of palatal obturators are the rapidity of their use immediately following surgery at 30 days, the absence of complications, such as osteonecrosis, reported in our clinic (20%) of osteointegrated implants and the fact that they are much cheaper than implants.
There is debate regarding the relative merits of surgical obturation or post-maxillectomy prosthesis due to the fact that few patients have been subject to longitudinal comparative studies.
Fig. 3b.

Hollow palatal obturator with dentures.
Fig. 4b.

Side view of palatal obturator which has partial dentures.
References
- 1.Genden EM, Okay D, Stepp MT, et al. Comparison of functional and quality-of-life outcomes in patients with and without palatomaxillary reconstruction. Arch Otolaryngol Head Neck Surg 2003;129:775-80. [DOI] [PubMed] [Google Scholar]
- 2.Cordeiro PG, Santamaria E. A classification system and algorithm for reconstruction of maxillectomy and midfacial defects. Plast Reconstr Surg 2000;105:2331-46. [DOI] [PubMed] [Google Scholar]
- 3.Chiapasco M, Biglioli F, Auteliano L, et al. Clinical outcome of dental implants placed in fibula-free flaps used for the reconstruction of maxillo-mandibular defects following ablation for tumors or osteoradionecrosis. Clin Oral Impl Res 2006;17:220-8. [DOI] [PubMed] [Google Scholar]
- 4.Rogers SN, Lowe D, McNally D, et al. Health-related quality of life after maxillectomy: a comparison between prosthetic obturation and free flap. J Oral Maxillofac Surg 2003;61:174-81. [DOI] [PubMed] [Google Scholar]
- 5.Dichamp J, Razouk O, Sidibe CA, et al. An obturator prosthesis in a patient with perfect dentition. Functional, esthetic approach. Rev Stomatol Chir Maxillofac 1994;95:195-6. [PubMed] [Google Scholar]
- 6.Genden EM, Wallace D, Buchbinder D, et al. Iliac crest internal oblique osteomusculocutaneous free flap reconstruction of the postablative palatomaxillary defect. Arch Otolaryngol Head Neck Surg 2001;127:854-61. [PubMed] [Google Scholar]
- 7.Etienne OMG, Taddei AMI. Case report. Use of bar-clip attachments to enhance the retention of a maxillofacial prosthetic obturator: a clinical report. J Oral Rehabil 2004;31:618-21. [DOI] [PubMed] [Google Scholar]
- 8.Aydin C, Delilbasi E, Yilmaz H, et al. Reconstruction of total maxillectomy defect with implant-retained obturator prosthesis - Case report. NY State Dent J 2007;73:38-41. [PubMed] [Google Scholar]
- 9.Blair FM, Hunter NR. The hollow box maxillary obturator. Br Dent J 1998;184:484-7. [DOI] [PubMed] [Google Scholar]
- 10.Wei F-C, Celick N, Chen H-C, et al. Combined anterolateral thigh flap and vascularized fibula osteoseptocutaneous flap in reconstruction of extensive composite mandibular defects. Plast Reconstr Surg 2002;109:45-52. [DOI] [PubMed] [Google Scholar]
- 11.Jones NF, Taub PJ. Sequential second free bone flap for reconstruction of metachronous mandibular defects. Plast Reconstr Surg 2005;116:939-45. [DOI] [PubMed] [Google Scholar]
- 12.Wei F-C, Celick N, Yang W-g, et al. Complication after reconstruction by plate and soft-tissue free flap in composite mandibular defects and secondary salvage reconstruction with osteocutaneous flap. Plast Reconstr Surg 2003;112:37-42. [DOI] [PubMed] [Google Scholar]
- 13.Ortegon SM, Martin JW, Lewin JS. A hollow delayed surgical obturator for a bilateral subtotal maxillectomy patient: a clinical report. J Prosthet Dent 2008;99:14-8. [DOI] [PubMed] [Google Scholar]
- 14.Futran ND. Retrospective case series of primary and secondary microvascular free tissue transfer reconstruction of midfacial defects. J Prosthet Dent 2001;86:369-76. [DOI] [PubMed] [Google Scholar]
- 15.Sakuraba M, Kimata Y, Ota Y, et al. Simple maxillary reconstruction using free tissue transfer and protheses. Plast Reconstr Surg 2003;111:594-8. [DOI] [PubMed] [Google Scholar]



