Summary
Personal experience is presented concerning a case in which reconstruction of the anterior floor of the mouth was carried out using a fascio-cutaneous free flap harvested from the lateral part of the leg; the flap pedicle is represented by perforating vessels originating from the peroneal vascular axis.
Keywords: Head and neck tumours, Floor of the mouth, Surgical treatment, Reconstructive surgery, Perforator flap, Peroneal vessels
Riassunto
Gli Autori presentano la loro esperienza relativa ad un caso in cui la ricostruzione del pavimento orale anteriore è stata eseguita mediante un lembo libero fascio-cutaneo prelevato dalla faccia laterale della gamba; il peduncolo del lembo è rappresentato da vasi perforanti provenienti dall’asse vascolare peroniero.
Introduction
Vascularization of perforator flaps is based on small calibre cutaneous blood vessels, which, originating from a deep main pedicle, reach and cross the superficial fascia after passing through the muscles or the fibrous septa which separate them.
Use of these flaps has achieved popularity only in recent years and its application in the intra-oral region is even more recent. The Authors present their experience concerning a case in which reconstruction of the anterior floor of the mouth was carried out using a fascio-cutaneous free flap harvested from the lateral part of the leg; the flap pedicle is represented by perforating vessels originating from the peroneal vascular axis.
Clinical case
This case concerns a 65-year-old male patient suffering from anterior floor of the mouth squamous cell carcinoma, studied as T2N0M0 (Figs. 1, 2). The patient, under general anaesthetic, underwent a subisthmic tracheotomy, selective bilateral dissection of the latero-cervical lymph glands, extended to levels I-II-III (saving the facial vessels), and removal of the anterior floor of the mouth (Fig. 3). The surgical deficit was corrected by the preparation and transposition of a peroneal perforator flap harvested from the right leg. The use of a Doppler probe helped to identify the position of the pedicle, in order to rationalize access into the lower limb. A 3 × 7 cm flap was tailored from the middle third of the leg (Fig. 4).
Fig. 1.
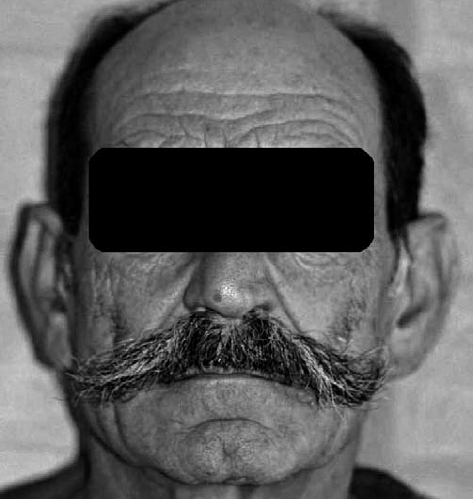
Pre-operative frontal view.
Fig. 2.

Oral floor squamous cell carcinoma.
Fig. 3.
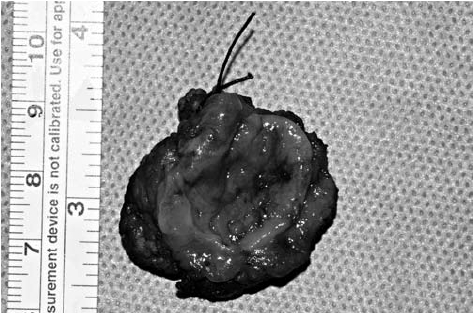
Tumour resected.
Fig. 4.

Pre-operative design of the donor region.
The perforating vessels were seen to have an intra-muscular passage leading to the peroneal axis; meticulous dissection, enhanced by using a 4x loop, made it possible to obtain a pedicle measuring 5 cm in length (Fig. 5). Anastomoses were carried out using a 10.0 nylon thread between the flap artery and the left submental artery, and between the pedicle vein and the left submental vein (Fig. 6). The flap was successfully transferred (Figs. 7, 8). In the immediate post-operative period, the patient developed an oro-cervical fistula; this problem was overcome by the application of a naso-gastric tube and frequent cleansing.
Fig. 5.

Pedicle dissection.
Fig. 6.

Arterial flow in submental artery.
Fig. 7.
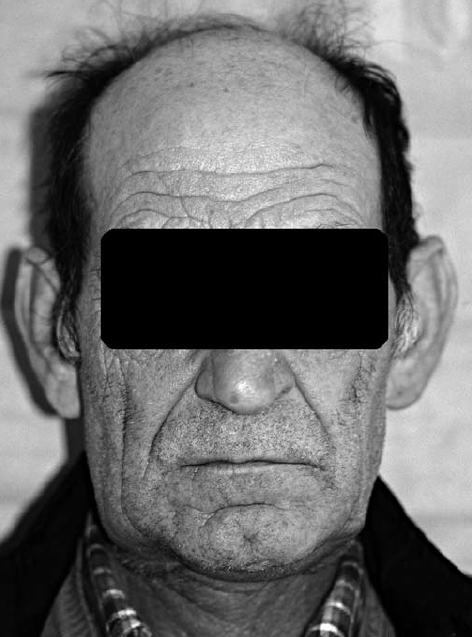
Post-operative frontal view.
Fig. 8.

Post-operative intra-oral view.
No complications occurred at the donor site, sutured by first intention (Fig. 9). The intra-osseous vessels were not damaged.
Fig. 9.
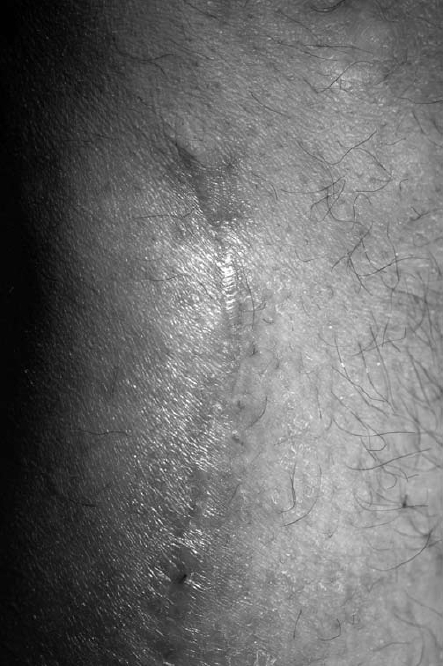
Donor site scar.
Discussion
The progressive increase in indications to use free flaps has provided an excellent boost to the development of this reconstructive technique over the last 25 years. Further innovative impetus has appeared over the last few years following the increase in popularity of the free flaps, known as perforator flaps. The term "perforator flap", used for the first time by Koshima in 1989 1, was specifically provided by Wei, in 2001 2, although the description of a technique being carried out to prepare a flap answering to this definition appeared in the literature about a decade earlier, followed by a number of other experiences 3–7. In a recent article, Hallock 8 proposes a more detailed terminology, referring to indirect perforator flaps, to indicate blood vessels which require intra-muscular dissection, and direct perforator flaps to indicate vessels which pass through the intramuscular septa or a more direct path to the skin.
An outline of the common characteristics of each perforator flap can be summarized as follows: thinness of the cutaneous segment of the flap compared to myocutaneous flaps, short pedicle length, modest vessel calibre, minimum donor site morbidity.
In the field of reconstructive surgery of the head region, good results have now been achieved using a coded series of revascularized flaps which can be defined as traditional flaps. One of the areas in which it finally appears that improvements can be made concerns the results regarding donor site morbidity; on this subject, there has been an exciting boom in documentation aimed at developing and refining existing techniques as well as conceiving new flaps.
Taking a closer look at the case presented herein, it is worthwhile briefly analyzing the characteristics of the reconstructive method, stating first of all that attention was drawn to the leg region on account of the excellent knowledge on the distribution pattern of the perforating blood vessels, as documented in a number of studies 9–12.
The extreme thinness of the cutaneous segment makes this surgical option particularly suited for closing intra-oral tissue loss. When comparing the applicability of the peroneal flap with other fascio-cutaneous free flaps, only the forearm flap or the dorsalis pedis flap offer a similar thinness but at the expense of a far greater risk of donor site morbidity 13–16.
In contrast to the considerations concerning the pedicle; rather than the limits of vessel calibre, it is the shortness of the vessels which can create some slight difficulty when performing anastomosis. For this reason, reports in the literature have recommended the use, on the receiving bed end, of the lingual artery and its venae comitantes due to their close positioning to the surgical gap 17; should this prove unfeasible, use of the thyroid superior artery is highly recommended as this can be mobilized and rotated upwards for a reasonable length. In our modest experience, we have taken advantage of the same characteristics offered by the facial artery. Should oncological requirements entail sacrificing the internal jugular vein together with the relative venous tree, the shortness of the pedicle means the use of the peroneal perforator flap cannot be recommended.
Depending on the availability of tissue, flaps measuring up to 22 × 8 cm have been described, a size which covers even large demolitions 18.
A last comparison with the antero-lateral thigh seems appropriate, characterized by negligible donor site morbidity, it provides an excellent pedicle though it may be subject to anatomic variations 19–22. Its abundant mass is, at times, excessive adding the relative risk of cutaneous devascularization caused by the procedures needed to reduce the thickness.
To conclude, despite the difficulties, which concern vascular suturing more than dissection, the peroneal perforator flap can be considered a valid alternative to the forearm flap in the reconstruction of intra-oral defects for those cases in which use of the antero-lateral thigh flap cannot satisfy reconstructive needs due to its excessive volume.
However, it is not possible to compare donor site morbidity which is negligible in the leg region, but more evident in the forearm region, due to the dimensions of the scarring area, with relative recession, the need to harvest skin and the hyper-pigmentation of the afore-mentioned skin. All these effects, which are constant, remain particularly visible. Furthermore, there are the potential complications which range from the unpleasant, though relatively innocuous loss of cutaneous sensitivity in the fingers, to the far more serious, even if less frequent, ischaemic problems affecting the hand 13–16.
References
- 1.Koshima I, Soeda S. Inferior epigastric artery skin flaps without rectus abdominis muscle. Br J Plast Surg 1989;42:645-8. [DOI] [PubMed] [Google Scholar]
- 2.Wei FC, Jain V, Suominen S, et al. Confusion among perforator flaps: What is a true perforator flap? Plast Reconstr Surg 2001;107:874-6. [DOI] [PubMed] [Google Scholar]
- 3.Kroll SS, Rosenfield L. Perforator-based flaps for low posterior midline defects. Plast Reconstr Surg 1988;81:561-6. [DOI] [PubMed] [Google Scholar]
- 4.Koshima I, Moriguchi T, Ohta S, et al. The vasculature and clinical application of the posterior tibial perforator-based flap. Plast Reconstr Surg 1992;90:643-9. [DOI] [PubMed] [Google Scholar]
- 5.Wu WC, Chang YP, So YC, et al. The anatomic basis and clinical applications of flaps based on the posterior tibial vessels. Br J Plast Surg 1993;46:470-9. [DOI] [PubMed] [Google Scholar]
- 6.Koshima I, Hosoda M, Inagawa K, et al. Free medial thigh perforator-based flaps: New definition of the pedicle vessels and versatile application. Ann Plast Surg 1996;37:507-15. [DOI] [PubMed] [Google Scholar]
- 7.Blondeel PN, Van Lunduyt KH, Monstrey SJ, et al. The "Gent" consensus on perforator flap terminology: preliminary definitions. Plast Reconstr Surg 2003;112:1378-83. [DOI] [PubMed] [Google Scholar]
- 8.Hallock GG. Direct and indirect perforator flaps: The history and the controversy. Plast Reconstr Surg 2003;111:855-65. [DOI] [PubMed] [Google Scholar]
- 9.Ponten B. The fascio-cutaneous flap: Its use in soft tissue defects of the lower leg. Br J Plast Surg 1981;34:215-20. [DOI] [PubMed] [Google Scholar]
- 10.Yoshimura M, Shimada T, Hosokawa M. The vasculature of the peroneal tissue transfer. Plast Reconstr Surg 1990;85:917-21. [DOI] [PubMed] [Google Scholar]
- 11.Schusterman MA, Reece GP, Miller MJ, et al. The osteocutaneous free fibula flap: Is the skin paddle reliable? Plast Reconstr Surg 1992;90:787-93. [PubMed] [Google Scholar]
- 12.Wolff KD, Stellmach R. The osteoseptocutaneous or purely septocutaneous peroneal flap with a supramalleolar skin paddle. Int J Oral Maxillofac Surg 1995;24:38-43. [DOI] [PubMed] [Google Scholar]
- 13.Bardsley AF, Soutar DS, Elliot D, et al. Reducing morbidity in the radial forearm flap donor site. Plast Reconstr Surg 1990;86:287-92. [PubMed] [Google Scholar]
- 14.Timmons MJ, Missotten FEM, Poole MD, et al. Complications of radial forearm flap donor sites. Br J Plast Surg 1986;39:176-8. [DOI] [PubMed] [Google Scholar]
- 15.Boorman JG, Brown JA, Sykes PJ. Morbidity in the forearm flap donor arm. Br J Plast Surg 1987;40:207-12. [DOI] [PubMed] [Google Scholar]
- 16.Jones BM, O’Brien CJ. Acute ischemia of the hand resulting from elevation of a radial forearm flap. Br J Plast Surg 1985;38:396-7. [DOI] [PubMed] [Google Scholar]
- 17.Wolff KD, Holze F, Nolte D. Perforator flap from the lower leg for intraoral reconstruction. Plast Reconstr Surg 2004;113:107-13. [DOI] [PubMed] [Google Scholar]
- 18.Tsai FC, Yang JY, Chuang SS, et al. Combined method of free lateral leg perforator flap with cervicoplasty for reconstruction of anterior cervical scar contractures: A new flap. J Reconstr Microsurg 2002;18:185-90. [DOI] [PubMed] [Google Scholar]
- 19.Wei FC, Jain V, Celik N, et al. Have we found the ideal soft-tissue flap? An experience with 672 anterolateral thigh flaps. Plast Reconstr Surg 2002;109:2219-26. [DOI] [PubMed] [Google Scholar]
- 20.Celik N, Wei FC, Lin CH. Technique and strategy in anterolateral thigh perforator flap surgery, based on an analysis of 15 complete and partial failures in 439 cases. Plast Reconstr Surg 2002;109:2211-6. [DOI] [PubMed] [Google Scholar]
- 21.Luo S, Raffoul W, Luo J. Anterolateral thigh flap: a review of 168 cases. Microsurgery 1999;19:232-8. [DOI] [PubMed] [Google Scholar]
- 22.Kimata Y, Uchiyama K, Ebihara S. Anatomic variations and technical problems of the anterolateral thigh flap: a report of 74 cases. Plast Reconstr Surg 1998;102:1517-23. [DOI] [PubMed] [Google Scholar]


