Abstract
Background
Since 1990, the National Breast and Cervical Cancer Early Detection Program (BCCEDP) has funded breast cancer screening and diagnostic services for low income, underinsured women. Case management was implemented in 2001 to address barriers to follow-up after an abnormal mammogram, and free treatment was introduced in 2004. However, the effect of these policies on timeliness of care has not been empirically evaluated.
Methods
Among 2,252 BCCEDP participants in Massachusetts during 1998 through 2007, we conducted a time-to-event analysis with pre-post comparisons to examine associations of case management and free treatment with diagnostic and treatment delays (>60 days and >90 days, respectively) following an abnormal mammogram.
Results
The proportion of women experiencing a diagnostic delay decreased from 33% to 23% after the introduction of case management (p<0.001), with a significant reduction in the adjusted risk of diagnostic delay (RR 0.65; 95% CI 0.53, 0.79) that did not differ by race/ethnicity. However, case management was not associated with changes in treatment delay (RR 0.93; 95% CI 0.80, 1.10). Free treatment was not associated with changes in the adjusted risk of diagnostic delay (RR 0.61; 95% CI 0.33, 1.14) or treatment delay (RR 0.77; 95% CI 0.43, 1.38), beyond improvements associated with case management.
Conclusion
Case management to assist women overcome logistical and psychosocial barriers to care may improve time to diagnosis among low-income women who receive free breast cancer screening and diagnostic services. Programs that provide services to coordinate care, in addition to free screening and diagnostic tests, may improve population health.
Introduction
The goal to expand health insurance coverage in the U.S. has placed new emphasis on the effectiveness of existing public health programs. With limited resources for health care financing, policymakers will have to decide which programs to cut or retain. To inform the current health reform debate, empirical evaluations are needed to determine whether established programs provide measurable benefits to population health, including the elimination of disparities.
Disparities in breast cancer outcomes exist by race/ethnicity, insurance status, and income level, and include more advanced stage at diagnosis, lower stage-specific survival rates, and higher death rates for low-income or uninsured women.1-5 To reduce the disproportionate burden of breast cancer among women with these characteristics1, 3 the U.S. Congress authorized the National Breast and Cervical Cancer Early Detection Program (BCCEDP) in 1990 (Public Law 101-354).6 This program serves a critical role in reducing barriers to breast cancer detection by funding breast cancer screening and diagnostic services for women who have historically been underserved by the medical system.6
However, improved access to health services alone does not necessarily translate into healthier populations.2, 7, 8 Two subsequent laws enacted by Congress recognized the need to facilitate timely diagnosis and initiation of treatment among National BCCEDP participants. In the Women's Health Research and Prevention Amendments of 1998 (Public Law 105-340), targeted funding was provided for case managers to assist National BCCEDP clients complete timely diagnostic testing after an abnormal mammogram, and enroll women in affordable treatment if breast cancer was diagnosed.6 In the Breast and Cervical Cancer Prevention and Treatment Act (Public Law 106-354), of 2000, states were given the option to use Medicaid to cover the cost of breast cancer treatment for eligible women.6
The BCCEDP case management process provides women with support to reduce anxiety, coordinates patient-doctor communications, and reduces health system barriers, similar to patient navigation programs reported in the literature. Studies of patient navigation suggest it can improve timely resolution after an abnormal mammogram.9-14 To our knowledge, no systematic study has been performed to evaluate change in diagnostic and treatment delays following implementation of the BCCEDP case management program and free treatment policy. To address this gap in knowledge, we used data from the Massachusetts BCCEDP to examine the following research questions: 1) Was implementation of the case management policy associated with lower risk of diagnostic and treatment delay after an abnormal mammogram?; 2) Was implementation of the free treatment policy associated with lower risk of diagnostic and treatment delay after an abnormal mammogram?; 3) Did associations between these policies and risk of delays in diagnosis and treatment of breast cancer, differ by race and ethnicity?
Methods
Data Source
Data were obtained from the Massachusetts BCCEDP, which was established in 1993, and administered by the Massachusetts Department of Public Health. Women eligible for the program have annual incomes ≤ 250% of the federal poverty level, are uninsured or under insured, and primarily 40-64 years of age. However, occasionally women younger than 40 years, or older than 64 years qualify for the program and are not turned-away due to age restrictions. Since the inception of the Massachusetts BCCEDP, 45 contractors (including community health centers, hospitals, and visiting nurse programs) have participated to provide outreach to eligible women, and health education, breast cancer screening, diagnostic tests, and case management to participants.
This research protocol used existing, de-identified data and was thus deemed exempt from review by the Harvard School of Public Health Human Subjects Committee. The study protocol was approved by the Massachusetts Department of Public Health Research and Data Access Review Committee.
Case Management
Starting on July 1, 2001, all Massachusetts BCCEDP clients, with a mammogram result of Breast Imaging Reporting and Data System (BI-RADS) 4 (suspect abnormality) or 5 (highly suggestive malignant neoplasm)15 were offered case management. Further details of case management including client consent to participate, actual services provided, and additional revenues paid to contractors were not available in the data source used for this study, and have not been previously summarized. Minimum credentials for a case manager included a current licensure or national certificate in case management, and either a bachelor's degree in health and human services or registered nurse license in Massachusetts. Contractors were encouraged to hire case managers fluent in languages of the women served. Case managers assisted women to obtain timely subsequent diagnostic tests by educating patients, scheduling follow-up visits, communicating with providers, providing transportation vouchers, scheduling interpreter services and enrolling clients in treatment programs.16
Free Treatment
As of January 1, 2004, free treatment was made available through Medicaid for Massachusetts BCCEDP participants diagnosed with breast cancer. The free treatment program was not administered by the BCCEDP. However, case managers assisted women to apply for free treatment or enroll in alternative treatment programs if they were not eligible for free treatment. After women enrolled in a treatment program no further follow-up was provided by the BCCEDP case manager. Details of whether a woman enrolled in the free treatment program were not available in the data used for this study.
Study Population
Women with an abnormal mammogram (BI-RADS 4 or 5) during July 1, 1998 – March 31, 2007 were eligible for the study. Screening mammograms were defined by Current Procedural Terminology (CPT) code 76092 (bilateral) or Healthcare Common Procedure Coding System (HCPCS) code G0202 (direct digital image, bilateral). Diagnostic mammograms were identified by CPT codes 76090 (unilateral), 76091 (bilateral), or HCPCS codes G0204 (direct digital image, bilateral), G0206 (direct digital image, unilateral). For each woman, we selected the first abnormal mammogram in the study period for inclusion in the study. To ensure that changes in contractors did not account for changes in times to events, we limited inclusion to contractors engaged with the Women's Health Network during all three study periods (pre-case management, July 1, 1998-June 30, 2001; post-case management, July 1 2001-December 31, 2003; and post-treatment funding, January 1, 2004-March 31, 2007). Only women with self-reported race/ethnicity as non-Hispanic white, non-Hispanic black, non-Hispanic Asian, Hispanic, were included in the sample because other individual racial or ethnic groups did not have sufficient numbers to make meaningful contributions to the analysis.
Measures
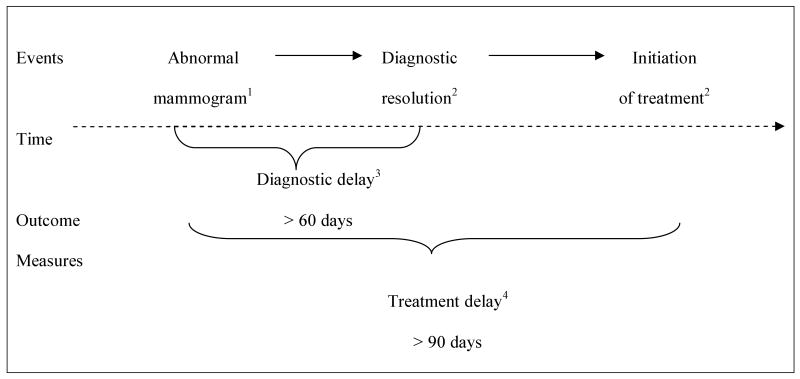
Two outcome measures of delay were assessed: diagnostic delay, and treatment delay (Figure 1). Diagnostic delay was based on the Centers for Disease Control and Prevention clinical guideline recommending resolution of a diagnostic evaluation within 60 days following an abnormal mammogram.17 Diagnostic resolution was defined as either a biopsy-confirmed diagnosis of breast cancer or a finding that breast cancer was ruled out through diagnostic ultrasound, biopsy, or diagnostic mammogram (BIRADS 1, 2, or 3).15 Treatment delay was computed only for women diagnosed with breast cancer and was based on literature suggesting that initiation of treatment greater than 90 days following an abnormal mammogram may be associated with decreased breast cancer survival.18
Figure 1. Outcome Measures of Delay.
1. Abnormal index mammograms occurred 7/1/1998-3/31/2007.
2. Follow-up events occurred 7/1/1998-6/30/2007.
3. Based on the Centers for Disease Control and Prevention recommendation for timely follow-up.17
4. Based on evidence suggesting treatment delays as short as 3 months may contribute to poorer survival.18
Demographic characteristics obtained for analyses included age at the time of the abnormal mammogram, education, and primary language. We also measured whether an abnormal clinical breast examination (CBE) occurred on the same date or within six months before the abnormal mammogram, and whether a woman completed a mammogram through the Massachusetts BCCEDP prior to the abnormal mammogram.
Statistical Analysis
The Cochran-Armitage test for trend and chi-square test were used, as appropriate, to examine bivariate associations between demographic and clinical variables, study periods, and outcome measures of delay. The unadjusted median number of days and interquartile range from the abnormal mammogram to diagnostic resolution and initiation of treatment were assessed with Kaplan-Meier survival estimates. We followed all women through June 30, 2007 to allow a minimum of 90 days for a follow-up event. Observations without a follow-up event were censored and June 30, 2007 was assigned as the event date.
Because our interest was to evaluate the reduction in delay associated with case management and free treatment policies based on a clinically relevant number of days,6, 18 we estimated the adjusted relative risk (RR) of diagnostic and treatment delay by Poisson regression instead of survival analysis. Adjusted models controlled for race, ethnicity, education, primary language, age centered around the mean for the sample, abnormal CBE, completion of prior mammogram, type of index mammogram (screening or diagnostic), and the effect of the other study period, because these characteristics changed over time in our study, and/or the literature suggests they are associated with timely follow-up. Models that examined adjusted RR of diagnostic delay also included a dummy variable for each contractor to control for differences in program implementation or changes in contractor characteristics associated with the outcomes. The small number of cancer cases precluded us from including the contractor dummy variables in the model that examined adjusted relative risk of treatment delay. We also assessed whether the policies had a differential effect on outcomes by race/ethnicity by including interaction terms for “race/ethnicity by study period” in the adjusted Poisson regression models. To account for the clustering of women within contractors, we used generalized estimating equations in these adjusted models.19
All p-values were two-tailed with p < 0.05 as the threshold for statistical significance. We used SAS software, version 9.1 (Cary, North Carolina) for all analyses.
Results
Study Cohort
A total of 2,821 women, from 45 contracting organizations, were eligible for case management from July 1, 1998-March 31, 2007. We excluded 186 owing to race or ethnicity other than White, Black Asian, Hispanic (7%); 12 owing to missing date of birth or age greater than 100 years (<1%); and 371 because the abnormal mammogram came from a contractor that had a gap in program participation (13%). The final sample consisted of 2,252 women, age 19-84 years, from 26 contracting organizations. We censored 197 observations because a diagnostic resolution (n = 180, 8%), or initiation of treatment (n = 17, < 1%), did not occur within the observation period. The percentage of censored observation did not vary over time by diagnostic resolution (p = 0.93) or initiation of treatment (p = 0.50).
The distribution of several characteristics changed over the study periods. Racial and ethnic diversity of women was greater in the case management and free treatment periods compared to before these policies were implemented. Index abnormal mammograms were more likely to be diagnostic studies and associated with an abnormal CBE, prior mammogram, or diagnosis of breast cancer during the case management and free treatment periods, relative to the period before case management was implemented (Table 1).
Table 1. Massachusetts BCCEDP1 Participants Assessed with Abnormal Mammograms2.
| Characteristics | Pre Case Management 7/1/1998-6/30/2001 | Post Case Management 7/1/2001-12/31/2003 | Post Free Treatment 1/1/2004-3/31/2007 | p-value3 |
|---|---|---|---|---|
| n = 832 | n = 536 | n = 884 | ||
| # (%) | # (%) | # (%) | ||
| Age | ||||
| < 40 years | 86 (10%) | 61 (11%) | 105 (12%) | 0.496 |
| 40-49 years | 352 (42%) | 244 (46%) | 386 (44%) | |
| 50-64 years | 361 (43%) | 219 (41%) | 366 (41%) | |
| 65 years or older | 33 (4%) | 12 (2%) | 27 (3%) | |
| Race/Ethnicity | ||||
| Non-Hispanic White | 544 (65%) | 305 (57%) | 509 (58%) | <0.001 |
| Non-Hispanic Black | 85 (10%) | 56 (10%) | 73 (8%) | |
| Hispanic | 192 (23%) | 166 (31%) | 272 (31%) | |
| Non-Hispanic Asian | 11 (1%) | 9 (2%) | 30 (3%) | |
| Education | ||||
| Less than High School | 230 (28%) | 149 (28%) | 195 (22%) | <0.001 |
| High School or Equivalent | 286 (34%) | 168 (31%) | 324 (37%) | |
| Some Col./Associates Degree | 161 (19%) | 117 (22%) | 155 (18%) | |
| Bachelor's Degree or higher | 120 (14%) | 58 (11%) | 121 (14%) | |
| Unknown | 35 (4%) | 44 (8%) | 89 (10%) | |
| Primary language | ||||
| English | 552 (66%) | 298 (56%) | 488 (55%) | <0.001 |
| Spanish | 140 (17%) | 116 (22%) | 175 (20%) | |
| Portuguese | 75 (9%) | 62 (12%) | 113 (13%) | |
| Other | 60 (7%) | 52 (10%) | 79 (9%) | |
| Unknown | 5 (1%) | 8 (1%) | 29 (3%) | |
| Index abnormal mammogram | ||||
| Screening | 436 (52%) | 114 (21%) | 65 (7%) | <0.001 |
| Diagnostic | 396 (48%) | 422 (79%) | 819 (93%) | |
| Abnormal clinical breast exam | ||||
| Yes | 121 (15%) | 117 (22%) | 209 (24%) | <0.001 |
| No | 711 (85%) | 419 (78%) | 675 (76%) | |
| Prior mammogram | ||||
| Yes | 292 (35%) | 292 (54%) | 521 (59%) | <0.001 |
| No | 540 (65%) | 244 (46%) | 363 (41%) | |
| Breast cancer | ||||
| Diagnosed | 139 (17%) | 105 (20%) | 198 (22%) | 0.051 |
| Ruled out | 628 (75%) | 389 (73%) | 613 (69%) | |
| No resolution | 65 (8%) | 42 (8%) | 73 (8%) | |
BCCEDP: Breast and Cervical Cancer Early Detection Program.
Mammograms associated with BI-RADS results 4 (suspicious abnormality) or 5 (highly suggestive of malignancy).
Chi-square test.
Percentages may not total 100% due to rounding.
Timing of Clinical Care
The median time from an abnormal mammogram to diagnostic resolution decreased by 8 days from the pre- to post-case management period, and by an additional 4 days from the post-case management to post-free treatment period. We also observed improvements in time to initiation of treatment across study periods. The median time from an abnormal mammogram to initiation of treatment decreased by 12 days from the pre to post-case management period, and by 3 additional days from the post-case management to post-free treatment period (Table 2).
Table 2. Timing of Clinical Care Following an Abnormal Mammogram1 for Massachusetts BCCEDP2 Participants.
| All Participants (n = 2,252) | n | Median Days to Diagnostic Resolution3 | Interquartile Range3 | p-value4 |
|---|---|---|---|---|
| Study Period of Follow-up | ||||
| Pre-Case Management 7/1/1998-6/30/2001 | 832 | 40 | 21- 84 | p < 0.001 |
| Post-Case Management 7/1/2001-12/31/2003 | 536 | 32 | 17 - 57 | |
| Post-Free Treatment 1/1/2004-6/30/2007 | 884 | 28 | 15 - 54 | |
| Race/Ethnicity | ||||
| Non-Hispanic White | 1,358 | 29 | 15 - 57 | < 0.001 |
| Non-Hispanic Black | 214 | 37 | 21 - 67 | |
| Hispanic | 630 | 38 | 22 - 71 | |
| Non-Hispanic Asian | 50 | 30 | 12 - 159 | |
| Breast Cancer Cases (n = 442) | n | Median Days to Initiation of Treatment3 | Interquartile Range3 | p-value4 |
| Study Periods | ||||
| Pre-Case Management 7/1/1998-6/30/2001 | 139 | 57 | 34 - 90 | p = 0.001 |
| Post-Case Management 7/1/2001-12/31/2003 | 105 | 45 | 28 - 70 | |
| Post-Free Treatment 1/1/2004-6/30/2007 | 198 | 42 | 30 - 60 | |
| Race/Ethnicity | ||||
| Non-Hispanic White | 320 | 45 | 30 - 74 | 0.2146 |
| Non-Hispanic Black | 37 | 36 | 28 - 66 | |
| Hispanic | 79 | 51 | 35 - 79 | |
| Non-Hispanic Asian | 6 | 40 | 17 - 54 | |
Mammograms associated with BI-RADS results 4 (suspicious abnormality) or 5 (highly suggestive of malignancy) that occurred 7/1/1998 – 3/31/2007.
BCCEDP: Breast and Cervical Cancer Early Detection Program.
Kaplan-Meier estimates.
Wilcoxon Test of Equality over Strata.
Among all study subjects, white and Asian women had the shortest median number of days to diagnostic resolution (29 days and 30 days, respectively). Among women diagnosed with breast cancer, black women had the shortest median number of days to initiation of treatment (36 days), and Hispanic women had the longest median time to treatment (51 days) (Table 2).
Unadjusted Trends in the Delay of Clinical Care
The proportion of women with diagnostic delay decreased by 10 percentage points following implementation of case management, and by an additional 3 percentage points following implementation of free treatment (p<0.001). There was also a decreasing trend in the proportion of women who experienced treatment delay across study periods (p=0.001), with a decrease of 10 percentage points after implementation of case management, and an additional decrease of 3 percentage points after implementation of free treatment (Table 3).
Table 3. Unadjusted Delays in Clinical Care Following an Abnormal Mammogram1 for Massachusetts BCCEDP2 Participants.
| Measures | Pre Case Management 7/1/1998-6/30/2001 | Post Case Management 7/1/2001-12/31/2003 | Post Free Treatment 1/1/2004-6/30/2007 | p-value5 |
|---|---|---|---|---|
| All Participants (n = 2,252) | ||||
| Diagnostic Delay3 | n = 832 | n = 536 | n = 884 | |
| 274 (33%) | 121 (23%) | 180 (20%) | p < 0.001 | |
| Women Diagnosed with Breast Cancer (n = 442) | ||||
| Treatment Delay4 | n = 139 | n = 105 | n = 198 | |
| 34 (24%) | 15 (14%) | 22 (11%) | p = 0.001 | |
Mammograms associated with BI-RADS results 4 (suspicious abnormality) or 5 (highly suggestive of malignancy) that occurred 7/1/1998 – 3/31/2007.
BCCEDP: Breast and Cervical Cancer Early Detection Program.
Diagnostic delay: > 60 days from the index abnormal mammogram to diagnostic resolution.
Treatment delay: > 90 days from the index abnormal mammogram to initiation of treatment.
Cochran-Armitage test.
Adjusted Relative Risk of Clinical Delays
We observed a 35% reduction in the adjusted risk of diagnostic delay during the case management period. An additional 7% decrease in the adjusted risk of diagnostic delay followed the implementation of free treatment but was not statistically significant. Similarly, the decreases in the adjusted risk of treatment delay after the implementation of case management and free treatment (39% and 23% respectively) were not statistically significant (Table 4).
Table 4. Adjusted1 Relative Risk of Delay in Clinical Care Following an Abnormal Mammogram2 for Massachusetts BCCEDP3 Participants.
| Measures | Post Case Management 7/1/2001-12/31/2003 | Post Free Treatment 1/1/2004-6/30/2007 | ||
|---|---|---|---|---|
| Adjusted RR4 (95% CI) | Adjusted RR5 (95% CI) | |||
| All Participants (n = 2,252) | ||||
| Diagnostic Delay6 | 0.65 (0.53, 0.79) | 0.93 (0.80, 1.10) | ||
| Women Diagnosed with Breast Cancer (n = 442) | ||||
| Treatment Delay7 | 0.61 (0.33, 1.14) | 0.77 (0.43, 1.38) | ||
Adjusted for age, education, primary language, race/ethnicity, abnormal clinical breast exam, mammogram history, type of index mammogram, and effect of other study period. The effect of contractors was held constant for estimates of relative risk of diagnostic delay.
Mammograms associated with BI-RADS results 4 (suspicious abnormality) or 5 (highly suggestive of malignancy) that occurred 7/1/1998 – 3/31/2007.
BCCEDP: Breast and Cervical Cancer Early Detection Program.
Relative to Pre-Case Management 7/1/1998-6/30/2001.
Relative to Post-Case Management 7/1/2001-12/31/2003.
Diagnostic delay: > 60 days from the index abnormal mammogram to diagnostic resolution.
Treatment delay: > 90 days from the index abnormal mammogram to initiation of treatment.
The risk of diagnostic delay was greater among Asian women, relative to white women (RR 1.61; 95% CI 1.17, 2.20), and lower among women with an abnormal CBE, relative to those with no abnormality (RR 0.73; 95% CI 0.59, 0.89). The risk of treatment delay was also lower among women who had a diagnostic mammogram as an index event, compared to a screening mammogram, (RR 0.54; 95% CI 0.38, 0.79), and was greater among women who completed an earlier mammogram through the program, relative to those who did not (RR 1.62; 95% CI 1.13, 2.33). The associations of case management with diagnostic delay did not differ for non-Hispanic Black (p=0.32), Hispanic (p=0.48), or Asian women (p=0.86), compared to non-Hispanic White women.
Discussion
To our knowledge this is the first time-to-event analysis with before-after comparisons to examine associations between implementation of case management and free treatment for BCCEDP participants, and diagnostic and treatment delays. In this empirical evaluation of Massachusetts BCCEDP data, we found that implementation of case management was associated with improved timely diagnostic resolution following an abnormal mammogram. Notably, the association between case management and diagnostic delay did not differ by race or ethnicity. Case management was not associated with changes in time to treatment in our study. We also found no association between the implementation of free treatment and delays in diagnosis or treatment beyond improvements associated with case management.
Our finding that case management improved time to diagnosis is consistent with evidence from smaller observational studies and randomized trials that demonstrated patient navigation services successfully improved timely diagnosis for low income, minority women.9-14 Randomized trials found that women who received patient navigation experienced a lower mean time to diagnostic resolution relative to those who received usual care (25 days vs. 43 days)12, and were more likely to receive a timely diagnosis (77% vs. 57%).11 We attribute similarities between our findings and earlier research to comparable activities performed by the Massachusetts BCCEDP case managers and patient navigators. These services likely removed barriers to diagnosis through psychosocial support and navigation of the health system. Unfortunately, we are not able to compare the level of delay or change in delay in our study to earlier research due to differences in criteria for inclusion of BI-RADS categories, definitions of timely follow-up, methods for censoring missing events, and choice of statistics.
We found only one study of patient navigation that examined time to treatment.11 This trial showed a greater percentage of the patient navigation group initiated treatment within 90 days of an abnormal mammogram (80%, n = 5), compared to usual care (50%, n = 10).11 The low number of women diagnosed with breast cancer precluded statistical testing of this difference. We experienced similar power issues in our adjusted analysis of treatment delay. With approximately 550 women in the pre-case management and post-case management periods, we had only 45% power to detect the 10% change in treatment delay, at an alpha-level of 0.05. However, when testing for unadjusted trends across all three study periods, we found a significant decrease in treatment delay.
The free treatment policy was not associated with timeliness of diagnostic resolution or initiation of treatment, beyond improvements observed after implementation of case management. We attribute this finding to two factors. First, barriers to timely resolution of an abnormal mammogram are primarily due to health system factors,20-24 and patient factors20-22 that were addressed through case management. Second, given the size of our sample, the probability of a false-negative finding was high at an alpha-level of 0.05. We had only 22% power to detect the 3% change in diagnostic delay, and 10% power to detect the 3% change in treatment delay following implementation of free treatment. Moreover, the greatest benefits of free treatment may be found in outcomes not measured in this study, such as improved receipt of treatment sessions, reduced anxiety, and mitigation of the financial burden of cancer treatment.3
The greater RR of diagnostic delay among Asian women should be interpreted carefully, as this estimate is strongly influenced by outlier values for time to resolution. Median days to diagnosis, a measure insensitive to outliers, showed that 50% of Asian women received diagnostic resolution within the same number of days as White women, 30 days versus 29 days, respectively. We found no other associations by race/ethnicity, and the relationship between case management and relative risk of diagnostic delay did not differ by race or ethnicity. This result implies that policies enacted to address barriers to care for low-income women, in addition to providing coverage for services, may improve the quality of care for all women served.
The observed lower risk of diagnostic delay among women with an abnormal CBE and among women with an index diagnostic mammogram are consistent with earlier research that suggests women with the greatest clinical need receive more timely follow-up.25 The observed association between mammogram use and treatment delay is similar to an earlier study that found women who completed previous mammograms had longer time from abnormal mammogram to initiation of treatment.26 Research is needed to inform our understanding of how earlier experiences with mammography may influence timely follow-up for subsequent tests.
Our ability to describe client participation in the Massachusetts BCCEDP case management and free treatment was limited by lack of data on the type and frequency of services provided to women. More detailed information on program participation is kept in local records by contractors but is not summarized in a data source at the Massachusetts BCCEDP. Our study also did not have measures for history of breast cancer, use of hormone replacement therapy, or prior screening outside the program, which may have influenced timely follow-up if these characteristics changed over time. However, we did control for patient and clinical characteristics most likely to be associated with diagnostic and treatment delays, to account for temporal changes in the race/ethnicity, education level, primary language, type of index mammogram, breast symptoms, and prior mammogram use of program participants. Temporal change in activities not related to the program under study but associated with the outcome is of greatest concern in before-after intervention studies that lack a comparison group. However, we are not aware of broader regional or statewide initiatives to improve follow-up of abnormal mammograms during the period when case management was implemented.
Several studies have demonstrated improved time to diagnostic resolution following implementation of patient navigation. However, gaps remain in knowledge on why this service is effective and whether the benefits outweigh the cost of maintaining the service. Future research can assess more detailed information on the costs and types of services and interactions between patients and navigators. Also, measuring more proximal outcomes of patient navigation may guide our ability to design effective programs by determining whether greater satisfaction with care or reduced anxiety over abnormal test results12, 16 improves timely follow-up.
Our analysis was limited to one potential outcome of the free treatment policy. A more comprehensive evaluation is needed to examine the impact of free treatment on out-of-pocket costs and standards of care given that income level, insurance status, and race are associated with these factors. Out-of-pocket costs for cancer care can force patients to incur debt, even when they are covered by private insurance.27 In addition, standards of care for breast cancer are less likely to be followed for women who reside in impoverished areas, are uninsured, enrolled in Medicaid, or of black race.5, 28-32
The rate of timely follow-up after abnormal mammograms in this study was within the range reported in other studies. Earlier reports of diagnostic delays greater than 60 days have ranged from 18%-29% (Massachusetts BCCEDP 20%), and treatment delays greater than 90 days ranged from 5% - 22% (Massachusetts BCCEDP 11%).26, 33-35 Results from our study may not be generalizable to other BCCEDP programs because the structure and implementation of case management services varies across sites. Nonetheless, our methods could readily be applied by other investigators to guide policy makers about the impact of BCCEDP programs in other states.
While improvement in rates of successful follow-up after abnormal findings are impressive for this public program, a reduction in disparities will also require a shift in social determinants of disease burden.36 All women need insurance coverage for breast cancer screening and diagnostic services, particularly low-income women who are not able to pay for medical services out-of-pocket. However, limited funding for the BCCEDP means that services reach approximately 13% of eligible women37, and breast cancer screening remains inaccessible for many low-income women.
Our study demonstrated that most women who participated in the Massachusetts BCCEDP received follow-up after an abnormal mammogram within the time recommended by clinical guidelines. Implementation of a case management policy through the Massachusetts BCCEDP was associated with improved time to resolution following an abnormal mammogram and the benefits of this policy did not differ by race/ethnicity.
Acknowledgments
This work was supported by the National Cancer Institute Cancer Prevention and Control Fellowship [5 R25 CA057711-15]; National Cancer Institute, MassCONECT [5 U01 CA114644], and K05CA124415. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Cancer Institute's Center to Reduce Cancer Health Disparities. Dr. Ayanian was supported by the Health Disparities Research Program of the Harvard Catalyst/The Harvard Clinical and Translational Science Center [NIH Grant # 1 UL1 RR 025758-01 and financial contributions from participating institutions].
Dr. Lobb had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The authors wish to thank Mary Lou Woodford, RN, BSN, MBA, CCM, Director of the Women's Health Network, Massachusetts Department of Public Health, for sharing her knowledge of the Massachusetts BCCEDP with us. We also are grateful for assistance from New England Research Institutes' Anne Stoddard, ScD who offered guidance with the study design, and Meena Doshi's, MS, MPH who provided advice on statistical programming. We also acknowledge the critical revisions suggested by Howard K. Koh, MD MPH, former Director of the Division of Public Health Practice, Harvard School of Public Health, prior to his appointment as the Assistant Secretary of Health in the U.S. Department of Health and Human Services (HHS).
References
- 1.American Cancer Society. Breast Cancer Facts & Figures 2009-2010. Atlanta, GA: American Cancer Society, Inc.; [Google Scholar]
- 2.Ayanian JZ, Kohler BA, Abe T, Epstein AM. The relation between health insurance coverage and clinical outcomes among women with breast cancer. N Engl J Med. 1993 Jul 29;329(5):326–331. doi: 10.1056/NEJM199307293290507. [DOI] [PubMed] [Google Scholar]
- 3.Ward E, Halpern M, Schrag N, et al. Association of insurance with cancer care utilization and outcomes. CA Cancer J Clin. 2008 Jan-Feb;58(1):9–31. doi: 10.3322/CA.2007.0011. [DOI] [PubMed] [Google Scholar]
- 4.Halpern MT, Ward EM, Pavluck AL, Schrag NM, Bian J, Chen AY. Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: a retrospective analysis. Lancet Oncol. 2008 Mar;9(3):222–231. doi: 10.1016/S1470-2045(08)70032-9. [DOI] [PubMed] [Google Scholar]
- 5.Byers TE, Wolf HJ, Bauer KR, et al. The impact of socioeconomic status on survival after cancer in the United States : findings from the National Program of Cancer Registries Patterns of Care Study. Cancer. 2008 Aug 1;113(3):582–591. doi: 10.1002/cncr.23567. [DOI] [PubMed] [Google Scholar]
- 6.National Breast and Cervical Cancer Early Detection Program: Summarizing the first 12 years of partnerships and progress against breast and cervical cancer: Centers for Disease Control and Prevention; 1991-2002 National Report.
- 7.Bradley CJ, Given CW, Roberts C. Race, socioeconomic status, and breast cancer treatment and survival. J Natl Cancer Inst. 2002 Apr 3;94(7):490–496. doi: 10.1093/jnci/94.7.490. [DOI] [PubMed] [Google Scholar]
- 8.Roetzheim RG, Pal N, Tennant C, et al. Effects of health insurance and race on early detection of cancer. J Natl Cancer Inst. 1999 Aug 18;91(16):1409–1415. doi: 10.1093/jnci/91.16.1409. [DOI] [PubMed] [Google Scholar]
- 9.Battaglia TA, Roloff K, Posner MA, Freund KM. Improving follow-up to abnormal breast cancer screening in an urban population. A patient navigation intervention. Cancer. 2007 Jan 15;109(2 Suppl):359–367. doi: 10.1002/cncr.22354. [DOI] [PubMed] [Google Scholar]
- 10.Clark CR, Baril N, Kunicki M, et al. Addressing social determinants of health to improve access to early breast cancer detection: results of the Boston REACH 2010 Breast and Cervical Cancer Coalition Women's Health Demonstration Project. J Womens Health (Larchmt) 2009 May;18(5):677–690. doi: 10.1089/jwh.2008.0972. [DOI] [PubMed] [Google Scholar]
- 11.Ell K, Vourlekis B, Lee PJ, Xie B. Patient navigation and case management following an abnormal mammogram: a randomized clinical trial. Prev Med. 2007 Jan;44(1):26–33. doi: 10.1016/j.ypmed.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 12.Ferrante JM, Chen PH, Kim S. The effect of patient navigation on time to diagnosis, anxiety, and satisfaction in urban minority women with abnormal mammograms: a randomized controlled trial. J Urban Health. 2008 Jan;85(1):114–124. doi: 10.1007/s11524-007-9228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Palmieri FM, DePeri ER, Mincey BA, et al. Comprehensive diagnostic program for medically underserved women with abnormal breast screening evaluations in an urban population. Mayo Clin Proc. 2009 Apr;84(4):317–322. doi: 10.1016/S0025-6196(11)60539-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Psooy BJ, Schreuer D, Borgaonkar J, Caines JS. Patient navigation: improving timeliness in the diagnosis of breast abnormalities. Can Assoc Radiol J. 2004 Jun;55(3):145–150. [PubMed] [Google Scholar]
- 15.Eberl MM, Fox CH, Edge SB, Carter CA, Mahoney MC. BI-RADS classification for management of abnormal mammograms. J Am Board Fam Med. 2006 Mar-Apr;19(2):161–164. doi: 10.3122/jabfm.19.2.161. [DOI] [PubMed] [Google Scholar]
- 16.Schutt RK, Cruz E, Woodford M. Client Satisfaction in a Breast and Cervical Cancer Early Detection Program: The Influence of Ethnicity and Language, Health, Resources, and Barriers. Women Health. 2008;48(3):283–302. doi: 10.1080/03630240802463475. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. National Breast and Cervical Cancer Early Detection Program Program Manual. Policy and Procedure Chapter. [November, 2009];2005 http://health.utah.gov/utahcancer/Healthcare_Provider/UCCP_policies/P&P_PDFs/NBCCEDP_policies_procedures.pdf.
- 18.Richards MA, Westcombe AM, Love SB, Littlejohns P, Ramirez AJ. Influence of delay on survival in patients with breast cancer: a systematic review. Lancet. 1999 Apr 3;353(9159):1119–1126. doi: 10.1016/s0140-6736(99)02143-1. [DOI] [PubMed] [Google Scholar]
- 19.Allison P. Logistic Regression Using SAS: Theory and Application. Cary, NC: SAS Institute Inc.; 1999. [Google Scholar]
- 20.Allen JD, Shelton RC, Harden E, Goldman RE. Follow-up of abnormal screening mammograms among low-income ethnically diverse women: findings from a qualitative study. Patient Educ Couns. 2008 Aug;72(2):283–292. doi: 10.1016/j.pec.2008.03.024. [DOI] [PubMed] [Google Scholar]
- 21.Rojas M, Mandelblatt J, Cagney K, Kerner J, Freeman H. Barriers to follow-up of abnormal screening mammograms among low-income minority women. Cancer Control Center of Harlem. Ethn Health. 1996 Sep;1(3):221–228. doi: 10.1080/13557858.1996.9961790. [DOI] [PubMed] [Google Scholar]
- 22.Caplan LS, Helzlsouer KJ, Shapiro S, Wesley MN, Edwards BK. Reasons for delay in breast cancer diagnosis. Prev Med. 1996 Mar-Apr;25(2):218–224. doi: 10.1006/pmed.1996.0049. [DOI] [PubMed] [Google Scholar]
- 23.Poon EG, Haas JS, Louise Puopolo A, et al. Communication factors in the follow-up of abnormal mammograms. J Gen Intern Med. 2004 Apr;19(4):316–323. doi: 10.1111/j.1525-1497.2004.30357.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Karliner LS, Patricia Kaplan C, Juarbe T, Pasick R, Perez-Stable EJ. Poor patient comprehension of abnormal mammography results. J Gen Intern Med. 2005 May;20(5):432–437. doi: 10.1111/j.1525-1497.2005.40281.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Caplan LS, Helzlsouer KJ, Shapiro S, Freedman LS, Coates RJ, Edwards BK. System delay in breast cancer in whites and blacks. Am J Epidemiol. 1995 Oct 15;142(8):804–812. doi: 10.1093/oxfordjournals.aje.a117719. [DOI] [PubMed] [Google Scholar]
- 26.Gwyn K, Bondy ML, Cohen DS, et al. Racial differences in diagnosis, treatment, and clinical delays in a population-based study of patients with newly diagnosed breast carcinoma. Cancer. 2004 Apr 15;100(8):1595–1604. doi: 10.1002/cncr.20169. [DOI] [PubMed] [Google Scholar]
- 27.Spending to Survive: Cancer Patients Confront Holes in the Health Insurance System. Kaiser Family Foundation and the American Cancer Society. 2009 [Google Scholar]
- 28.Coburn N, Fulton J, Pearlman DN, Law C, DiPaolo B, Cady B. Treatment variation by insurance status for breast cancer patients. Breast J. 2008 Mar-Apr;14(2):128–134. doi: 10.1111/j.1524-4741.2007.00542.x. [DOI] [PubMed] [Google Scholar]
- 29.Liu MJ, Hawk H, Gershman ST, et al. The effects of a National Breast and Cervical Cancer Early Detection Program on social disparities in breast cancer diagnosis and treatment in Massachusetts. Cancer Causes Control. 2005 Feb;16(1):27–33. doi: 10.1007/s10552-004-1289-4. [DOI] [PubMed] [Google Scholar]
- 30.Hassett MJ, Griggs JJ. Disparities in breast cancer adjuvant chemotherapy: moving beyond yes or no. J Clin Oncol. 2009 May 1;27(13):2120–2121. doi: 10.1200/JCO.2008.21.1532. [DOI] [PubMed] [Google Scholar]
- 31.Kim SH, Ferrante J, Won BR, Hameed M. Barriers to adequate follow-up during adjuvant therapy may be important factors in the worse outcome for Black women after breast cancer treatment. World J Surg Oncol. 2008;6:26. doi: 10.1186/1477-7819-6-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hershman DL, Unger JM, Barlow WE, et al. Treatment quality and outcomes of African American versus white breast cancer patients: retrospective analysis of Southwest Oncology studies S8814/S8897. J Clin Oncol. 2009 May 1;27(13):2157–2162. doi: 10.1200/JCO.2008.19.1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gorin SS, Heck JE, Cheng B, Smith SJ. Delays in breast cancer diagnosis and treatment by racial/ethnic group. Arch Intern Med. 2006 Nov 13;166(20):2244–2252. doi: 10.1001/archinte.166.20.2244. [DOI] [PubMed] [Google Scholar]
- 34.Elmore JG, Nakano CY, Linden HM, Reisch LM, Ayanian JZ, Larson EB. Racial inequities in the timing of breast cancer detection, diagnosis, and initiation of treatment. Med Care. 2005 Feb;43(2):141–148. doi: 10.1097/00005650-200502000-00007. [DOI] [PubMed] [Google Scholar]
- 35.Caplan LS, May DS, Richardson LC. Time to diagnosis and treatment of breast cancer: results from the National Breast and Cervical Cancer Early Detection Program, 1991-1995. Am J Public Health. 2000 Jan;90(1):130–134. doi: 10.2105/ajph.90.1.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Graham H. Social determinants and their unequal distribution: clarifying policy understandings. Milbank Q. 2004;82(1):101–124. doi: 10.1111/j.0887-378X.2004.00303.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tangka FK, Dalaker J, Chattopadhyay SK, et al. Meeting the mammography screening needs of underserved women: the performance of the National Breast and Cervical Cancer Early Detection Program in 2002-2003 (United States) Cancer Causes Control. 2006 Nov;17(9):1145–1154. doi: 10.1007/s10552-006-0058-y. [DOI] [PMC free article] [PubMed] [Google Scholar]