Abstract
Objective
To compare the clinical characteristics of primarily and secondarily infertile men with varicocele.
Design
Cross-sectional analysis.
Setting
Male infertility clinic, tertiary health care center.
Patient(s)
Two hundred ninety-five infertile men with palpable varicoceles.
Intervention(s)
Clinical evaluation including patient reproductive history (including assessment of primary or secondary infertility), physical examination, hormonal assessment and at least two semen analyses.
Main Outcome Measure(s)
Differences in the characteristics of men with primary vs. secondary infertility.
Result(s)
Two hundred five subjects were identified with primary infertility and 90 with secondary infertility. Secondarily infertile men were older (39.6 years vs. 35.0 years), with older partners (35.4 years vs. 33.2 years), but had higher sperm densities (51.3 vs. 36.0 million/mL) and a greater percentage of morphologically normal sperm (30.6% vs. 24.1%). A lower proportion of secondarily infertile men had total motile sperm count (TMC) <20 million compared with primarily infertile men (31.1% vs. 46.5%). Groups did not differ regarding infertility duration, tobacco or alcohol use, varicocele grade or laterality, testis volumes, or hormonal parameters. In multivariate modeling, secondary infertility (vs. primary) was an independent predictor of TMC >20 million (odds ratio 1.9).
Conclusion(s)
Men with secondary infertility are older and have older partners than primarily infertile men, yet they have significantly better sperm concentrations. Infertility in this group may be influenced by maternal reproductive potential.
Keywords: Male infertility, varicocele, primary infertility, secondary infertility
A varicocele is an abnormal dilatation to the pampiniform plexus, the complex network of veins that drain the testis. Although the exact etiology of how varicocele alters spermatogenesis is unclear, it is the most commonly documented cause of male infertility (1). Whereas varicocele is observed in 35% to 50% of primarily infertile men, it has been reported in up to 80% of secondarily infertile men (2). This finding has led investigators to suggest that varicocele may be a progressive lesion that continues to assert a negative impact on fertility over a man’s lifetime (2–4). Given the notion that a varicocele may be a progressive lesion, prophylactic varicocelectomy has been recommended to preserve fertility potential (4).
If varicocele is a progressive lesion, then when patients present with secondary infertility, the semen analyses should be as bad as or worse than those with primary infertility and varicocele. Indeed, secondarily infertile men with varicocele have been reported to be older and have worse semen parameters than primarily infertile men with varicocele (4). Interestingly, these same secondarily infertile men also have older partners, suggesting that female factors may have a significant impact on couples’ fertility.
More recently, the progressive nature of varicoceles has been questioned by Jarow et. al. (3), who found that the prevalence of varicocele was nearly identical in two cohorts of men with primary and secondary infertility. Those authors proposed that earlier reports may have been confounded by a larger proportion of “other” causes of infertility in cases of primary infertility, so that the relative prevalence of varicocele is higher in men with secondary infertility, even if the absolute number of varicocele cases is similar.
Thus, the clinical picture of primary and secondary infertility with varicocele remains confusing, as does the impact of varicocele on semen parameters in these two populations. We evaluated a contemporary cohort of men with palpable varicoceles undergoing infertility evaluation and sought to identify the clinical differences between primarily and secondarily infertile men.
METHODS
Study Population
After receiving institutional review board approval, we conducted a cross-sectional analysis of 295 consecutive patients with varicocele presenting for infertility evaluation at a single academic center from 1998 to 2000. Only patients with palpable varicoceles, undergoing evaluation for infertility, with complete history, physical examination, and semen analyses were included. Those evaluated for pain, scrotal mass, or fertility prophylaxis were excluded from the analysis. Patients referred for evaluation of subclinical varicoceles found incidentally on scrotal ultrasound were also excluded. In general, couples in this study underwent simultaneous male and female factor evaluations at a single institution, so that the presence or absence of female factor infertility did not serve as a basis for excluding couples from study inclusion.
Patient Evaluation
All subjects were evaluated by the same clinician, and varicoceles were graded according to routine clinical criteria while standing is a warm room (5). Testicular exam included an assessment of consistency as well as volume (measured bilaterally using ellipsoid Prader orchidometry (ASSI Instruments, NY). Semen was collected by masturbation after 2–4 days of abstinence and processed within 1 h of ejaculation. All semen analyses were performed in the male reproductive laboratory according to World Health Organization (WHO) standards. Hormonal evaluation included plasma T and FSH and were performed only when sperm concentrations were <10 million/mL (6).
Study Design
Men were classified as having primary or secondary infertility. A man was considered to have primary infertility if he had no history of prior paternity. A man was considered to have secondary infertility if he had previously fathered a child with his current partner or a previous partner. For each group, elements from the history (age, partner’s age, months attempting to conceive, medical comorbidities, smoking, and significant alcohol use), the physical examination (varicocele grade, laterality, testis volume, and testis consistency), hormonal analysis (FSH and T), and semen analysis (volume, concentration, motility, and morphology) were compared. In an attempt to isolate the male contribution to infertility, a subanalysis was performed after excluding couples in whom the female partner >35 years old.
For analysis, the total motile sperm count (TMC) was defined as the product of ejaculate volume, sperm concentration, and proportion of motile sperm. Mean TMCs were calculated from the multiple semen analyses obtained at each time point. Testicular hypotrophy was defined as a size discrepancy between testes of >3 mL or absolute testicular volumes ≤14 mL in cases of bilateral hypotrophy (7).
Continuous and categoric data were compared and tested for significance between groups using Wilcoxon rank sum and chi-squared tests, respectively. When continuous data was normally distributed, we used the Student t test (two-tailed). Unconditional multivariate logistic regression, controlling for age (continuous variable), female age (continuous variable), smoking (yes or no), alcohol use (yes [>2 drinks per day], or no), bilateral hypotrophy (yes or no), and systemic illnesses (yes or no), was used to determine whether secondary infertility could be used as a predictor for TMC.
RESULTS
Study Population
Of 301 patients with palpable varicoceles presenting for infertility evaluation, 295 (98%) were identified with: 1) complete histories and physical examinations; 2) clear documentation of primary or secondary infertility; and 3) complete semen analysis data. The mean patient age was 36.7 years and the mean partner age was 33.9 years. On average, couples had been trying to conceive for 27.6 months before presentation. A total of 205 (69%) subjects were identified with primary infertility and 90 (31%) with secondary infertility.
Characteristics of Primarily and Secondarily Infertile Men
Secondarily infertile men were older (mean age 39.6 vs. 35.0 years; P<.001), and had older partners (mean age 35.4 vs. 33.2 years; P<.001; Table 1). Secondarily infertile men had a higher mean sperm concentration compared with primarily infertile men (51.3 vs. 34.9 million/mL; P<.01) and a lower proportion with TMC <20 million (31.1% vs. 46.5%; P<.05). The distribution of sperm concentrations by fertility status (primary vs. secondary) is shown in Figure 1. Although secondarily infertile men also had a lower mean TMC than primarily infertile men, that finding was not statistically significant. Average sperm motility did not differ between the groups; however, those with secondary infertility had a greater mean percentage of normal forms by WHO criteria (30.6% vs. 24.1%; P<.05). The two groups did not differ by time attempting to conceive, tobacco or alcohol use, testicular hypotrophy, bilateral varicoceles, varicocele grade, FSH, or total T.
TABLE 1.
Comparison of primarily infertile and secondarily infertile men with varicocele.
| Primary infertility (n = 205) | Secondary infertility (n = 90) | P value | |
|---|---|---|---|
| Age (yrs) | 35.0 | 39.6 | <.001a |
| Partner age (yrs) | 33.2 | 35.4 | <.001a |
| Partner age <35 yrs (%) | 59.8 | 40.9 | <.01b |
| Time trying (months) | 26.0 | 28.9 | .5a |
| Smoking (%) | 11.8 | 10.0 | .6b |
| Alcohol use (%)d | 4.4 | 3.3 | .7b |
| Unilateral hypotrophy (%) | 15.6 | 11.4 | .3b |
| Bilateral hypotrophy (%) | 9.5 | 6.8 | .4b |
| Bilateral varicocele (%) | 25.6 | 26.7 | .8b |
| Grade I varicocele (%) | 8.4 | 5.6 | .4b |
| Grade II varicocele (%) | 61.1 | 72.2 | .07b |
| Grade III varicocele (%) | 30.5 | 22.2 | .1b |
| TMC (million) | 58.2 | 62.1 | .08c |
| TMC <20 million (%) | 46.5 | 31.1 | <.05b |
| Sperm motility (%) | 36.7 | 36.0 | .8b |
| Sperm concentration (million/mL) | 34.9 | 51.3 | <.01c |
| Morphology (% normal forms) | 24.1 | 30.6 | <.05b |
Note: TMC = total motile sperm count.
Student t test.
Chi-squared test.
Wilcoxon rank sum test.
Use of alcohol more than 2 drinks/day.
Walsh. Varicocele-related infertility. Fertil Steril 2009.
FIGURE 1.
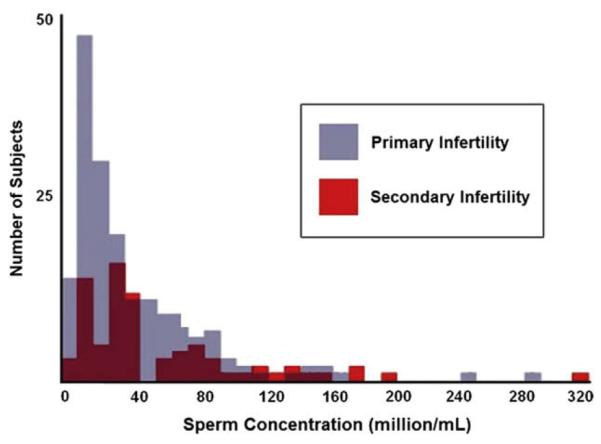
Distribution of sperm concentration by fertility status (primary vs. secondary).
Walsh. Varicocele-related infertility. Fertil Steril 2009.
Secondary Infertility as a Predictor of Normal Semen Analysis
Modeling the data using unconditional multivariate logistic regression, and controlling for age, female age, smoking, significant alcohol use, systemic illness, and bilateral hypotrophy, men with secondary infertility had nearly twice the odds of having a TMC >20 million compared with men with primary infertility (odds ratio 1.9, 95% confidence interval 1.0–3.6).
Exclusion of Couples in With Female Partner >35 Years Old
After excluding couples in whom the female partner was >35 years old, 107 men with primary remained for comparison with 36 with secondary infertility. Despite this exclusion, secondarily infertile men were significantly older than primarily infertile men (37.8 vs. 33.3 years; P<.001), as were their partners (31.4 vs. 29.9 years; P<.05). All semen parameters in secondarily infertile men trended toward being better than those in primarily infertile men, and morphology continued to be significantly better (concentration 41.7 vs. 32.6 million/ mL [P=.3], motility 37.2% vs. 35.6% [P=.7], morphology 30.9% vs. 20.1% normal forms [P<.05]).
DISCUSSION
Varicocele is the most common reversible cause of male infertility. Based on evidence that varicoceles are more common in secondarily infertile men, it has been proposed that varicocele may be a progressive lesion that increasingly impairs spermatogenesis with time and that should be prophylactically treated. Contrary to earlier studies, the present findings show that, compared with primarily infertile men, secondarily infertile men with varicocele have better semen analyses, are older, and have older partners. Furthermore, secondarily infertile men are more than twice as likely as primarily infertile men to have normal semen analyses.
Semen Quality in Secondarily Infertile Men
Secondarily infertile couples have been shown to be older in both general (2, 3) and varicocele populations (4). To our knowledge, this study is the first time that secondarily infertile men with varicocele have been shown to have better semen parameters than primarily infertile men with varicocele.
In comparing secondarily and primarily infertile men with varicocele, Gorelick and Goldstein (4) noted that the former group were older with older partners, but contrary to our findings they noted that secondarily infertile men had worse semen parameters. The difference between the two studies may be explained by differences in the study populations. Importantly, Gorelick and Goldstein attempted to exclude female factor by only including couples in which the woman was <40 years old and had previously undergone complete gynecologic infertility evaluation that ruled out identifiable female factors. Consequently, their population of men differed from ours in several ways (Table 2). In particular, the present population included older men with older partners in both secondarily and primarily infertile couples (primarily infertile male: 35.5 vs. 33.5 years; secondarily infertile male: 40.5 vs. 37.9 years; primarily infertile female: 33.4 vs. 31.7 years; secondarily infertile female: 36.1 vs. 33.8 years). Whereas Gorelick and Goldstein were able to investigate men who were potentially isolated from the influence of female factor infertility, in many clinical settings couples present before female factor issues are excluded and a parallel investigation of both partnersisperformed. Asa result, the present cohort may represent a different presentation of infertile couples with varicocele. However, after applying the stringent exclusion of couples in whom the female partners were older than 35 years, men with secondary infertility still appeared to have better semen parameters than men with primary infertility, suggesting that exclusion of female factors does not fully account for the differences in the studies’ findings.
TABLE 2.
Study population differences between Gorelick and Goldstein (4) and the current study.
| Gorelick and Goldstein |
Current study |
|||
|---|---|---|---|---|
| Primary infertility |
Secondary infertility |
Primary infertility |
Secondary infertility |
|
| Male Age (yrs) | 33.5 | 37.9 | 35.0 | 39.6 |
| Female age (years) | 31.7 | 33.8 | 33.2 | 35.4 |
| Grade I varicocele (%) | 43 | 36 | 8.4 | 5.6 |
| Grade II varicocele (%) | 32 | 43 | 61.1 | 72.2 |
| Grade III varicocele (%) | 25 | 21 | 30.5 | 22.2 |
| Bilateral varicocele (%) | 42 | 38 | 25.6 | 26.7 |
| Left varicocele (%) | 55 | 58 | 73 | 70 |
| Right varicocele (%) | 3 | 4 | 2 | 2 |
| Sperm concentration (million/mL) | 46.1 | 30.2 | 34.9 | 51.3 |
Walsh. Varicocele-related infertility. Fertil Steril 2009.
Influence of Female Age and Other Factors
Age plays a major role in the fertility potential of both men and women (8–10). Natural conception and IVF success are known to decline precipitously during a woman’s fourth decade of life. Although 35 years is commonly cited as the age at which female infertility becomes problematic, one study has noted that the chance of conception per IVF cycle fell by approximately 12% each year after the age of 31 years (8). This suggests that the 3-year age difference of women in our secondarily infertile population compared with the primary infertile cohort might be significant. Furthermore, this may also account for differences in couple fertility potential between Gorelick and Goldstein’s study population and ours, given the younger average age of female partners in the earlier study.
Age also affects male fertility, with studies showing worsening semen parameters with increasing age. A recent review noted that when comparing 30-year-old men with 50-year-old men, although sperm concentrations did not differ significantly, there was a decrease in sperm motility of 3% –37%, and a decrease in the proportion of normal morphological sperm of 4%–18% (11). However, unlike the biology of female age and infertility, there is no defined age after which men are considered to be infertile (12). Thus, the influence of female age on the fertility potential of couples with varicoceles may, in fact, be quite significant and account for much of the decline in fertility potential when men with primary and secondary infertility are compared.
Varicocele as a Progressive Lesion
The present study found that secondarily infertile men with varicocele had better semen parameters than men with primary infertility. This finding does not support the theory of varicocele as a progressive lesion. In fact, this observation is more consistent with studies that show no evidence of deteriorating semen quality in asymptomatic men with varicocele followed over an 8-year period compared with men without varicocele (13). Although there is strong evidence that varicocele has a progressive effect in adolescence, evidenced by both declining semen parameters and hypotrophy, a similar strong relationship may not exist in adults (14, 15).
Study Limitations
Our conclusions must be considered along with several limitations to this study. By design, the present study cannot conclusively determine whether or not varicocele is a progressive lesion. For that determination, controlled prospective longitudinal studies are necessary (13, 16). Indeed, longitudinal studies with small numbers of men have suggested that semen parameters do deteriorate with time in healthy men with varicoceles. Whether this trend would be maintained in larger populations of men followed longitudinally has yet to be determined. The present study does, however, add credence to the notion that varicocele is not a progressive lesion in adult men.
Whether or not female factor figures highly in the cohort of secondarily infertile couples is difficult to determine. This is because a prior female factor evaluation was not necessary for inclusion and this study used the semen analyses as a marker of fertility. Despite the fact that secondarily infertile men had relatively normal semen parameters, more subtle male factors than those uncovered by a standard semen analysis may be present (17).
CONCLUSIONS
We observed that secondarily infertile men with varicocele are older, have older partners, and yet have better semen parameters than primarily infertile men with varicocele. Because age is a significant risk factor for female infertility, it may be that female factor issues play a large role in these couples’ infertility. The present data also support the notion that varicocele is not a progressive lesion. Clinically, in secondarily infertile couples with a varicocele, if female factors have not been examined they should be pursued before varicocelectomy.
Acknowledgments
Dr. Walsh is a Men’s Reproductive Health Research K12 Scholar supported by National Institute of Child Health and Human Development K12 grant HD053943012 (TW), San Francisco, California.
Footnotes
T.J.W. has nothing to disclose. A.K.W. has nothing to disclose. M.S.C. has nothing to disclose. P.J.T. has nothing to disclose.
REFERENCES
- 1.Meacham RB, Joyce GF, Wise M, Kparker A, Niederberger C. Male infertility. J Urol. 2007;177:2058–66. doi: 10.1016/j.juro.2007.01.131. [DOI] [PubMed] [Google Scholar]
- 2.Witt MA, Lipshultz LI. Varicocele: a progressive or static lesion? Urology. 1993;42:541–3. doi: 10.1016/0090-4295(93)90268-f. [DOI] [PubMed] [Google Scholar]
- 3.Jarow JP, Coburn M, Sigman M. Incidence of varicoceles in men with primary and secondary infertility. Urology. 1996;47:73–6. doi: 10.1016/s0090-4295(99)80385-9. [DOI] [PubMed] [Google Scholar]
- 4.Gorelick JI, Goldstein M. Loss of fertility in men with varicocele. Fertil Steril. 1993;59:613–6. [PubMed] [Google Scholar]
- 5.Dubin L, Amelar RD. Varicocele size and results of varicocelectomy in selected subfertile men with varicocele. Fertil Steril. 1970;21:606–9. doi: 10.1016/s0015-0282(16)37684-1. [DOI] [PubMed] [Google Scholar]
- 6.Sigman M, Jarow JP. Endocrine evaluation of infertile men. Urology. 1997;50:659–64. doi: 10.1016/S0090-4295(97)00340-3. [DOI] [PubMed] [Google Scholar]
- 7.Takihara H, Cosentino MJ, Sakatoku J, Cockett AT. Significance of testicular size measurement in andrology: II. Correlation of testicular size with testicular function. J Urol. 1987;137:416–9. doi: 10.1016/s0022-5347(17)44053-5. [DOI] [PubMed] [Google Scholar]
- 8.van Noord-Zaadstra BM, Looman CW, Alsbach H, Habbema JD, te Velde ER, Karbaat J. Delaying childbearing: effect of age on fecundity and outcome of pregnancy. BMJ. 1991;302:1361–5. doi: 10.1136/bmj.302.6789.1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dunson DB, Baird DD, Colombo B. Increased infertility with age in men and women. Obstet Gynecol. 2004;103:51–6. doi: 10.1097/01.AOG.0000100153.24061.45. [DOI] [PubMed] [Google Scholar]
- 10.Schwartz D, Mayaux MJ. Female fecundity as a function of age: results of artificial insemination in 2193 nulliparous women with azoospermic husbands. Federation CECOS. N Engl J Med. 1982;306:404–6. doi: 10.1056/NEJM198202183060706. [DOI] [PubMed] [Google Scholar]
- 11.Kidd SA, Eskenazi B, Wyrobek AJ. Effects of male age on semen quality and fertility: a review of the literature. Fertil Steril. 2001;75:237–48. doi: 10.1016/s0015-0282(00)01679-4. [DOI] [PubMed] [Google Scholar]
- 12.Adamson GD, Baker VL. Subfertility: causes, treatment and outcome. Best Pract Res Clin Obstet Gynaecol. 2003;17:169–85. doi: 10.1016/s1521-6934(02)00146-3. [DOI] [PubMed] [Google Scholar]
- 13.Lund L, Larsen SB. A follow-up study of semen quality and fertility in men with varicocele testis and in control subjects. Br J Urol. 1998;82:682–6. doi: 10.1046/j.1464-410x.1998.00850.x. [DOI] [PubMed] [Google Scholar]
- 14.Okuyama A, Nakamura M, Namiki M, Takeyama M, Utsunomiya M, Fujioka H, et al. Surgical repair of varicocele at puberty: preventive treatment for fertility improvement. J Urol. 1988;139:562–4. doi: 10.1016/s0022-5347(17)42525-0. [DOI] [PubMed] [Google Scholar]
- 15.Sayfan J, Siplovich L, Koltun L, Benyamin N. Varicocele treatment in pubertal boys prevents testicular growth arrest. J Urol. 1997;157:1456–7. [PubMed] [Google Scholar]
- 16.Chehval MJ, Purcell MH. Deterioration of semen parameters over time in men with untreated varicocele: evidence of progressive testicular damage. Fertil Steril. 1992;57:174–7. doi: 10.1016/s0015-0282(16)54796-7. [DOI] [PubMed] [Google Scholar]
- 17.Guzick DS, Overstreet JW, Factor-Litvak P, Brazil CK, Nakajima ST, Coutifaris C, et al. Sperm morphology, motility, and concentration in fertile and infertile men. N Engl J Med. 2001;345:1388–93. doi: 10.1056/NEJMoa003005. [DOI] [PubMed] [Google Scholar]


