Abstract
Aside from the well-established self-renewal and multipotent differentiation properties, mesenchymal stem cells exhibit both immunomodulatory and anti-inflammatory roles in several experimental autoimmune and inflammatory diseases. In this study, we isolated a new population of stem cells from human gingiva, a tissue source easily accessible from the oral cavity, namely, gingiva-derived mesenchymal stem cells (GMSCs), which exhibited clonogenicity, self-renewal, and multipotent differentiation capacities. Most importantly, GMSCs were capable of immunomodulatory functions, specifically suppressed peripheral blood lymphocyte proliferation, induced expression of a wide panel of immunosuppressive factors including IL-10, IDO, inducible NO synthase (iNOS), and cyclooxygenase 2 (COX-2) in response to the inflammatory cytokine, IFN-γ. Cell-based therapy using systemic infusion of GMSCs in experimental colitis significantly ameliorated both clinical and histopathological severity of the colonic inflammation, restored the injured gastrointestinal mucosal tissues, reversed diarrhea and weight loss, and suppressed the overall disease activity in mice. The therapeutic effect of GMSCs was mediated, in part, by the suppression of inflammatory infiltrates and inflammatory cytokines/mediators and the increased infiltration of regulatory T cells and the expression of anti-inflammatory cytokine IL-10 at the colonic sites. Taken together, GMSCs can function as an immunomodulatory and anti-inflammatory component of the immune system in vivo and is a promising cell source for cell-based treatment in experimental inflammatory diseases.
Mesenchymal stem cells (MSCs)3 have the capacity to self-renew and differentiate into different cell lineages, including mesodermal, endodermal, and ectodermal cells (1, 2). Originally isolated from bone marrow (3), similar subsets of multipotent MSCs have also been identified in skin (4, 5), adipose tissue (6), tendon (7), lung, heart, liver (8), placenta (9), amniotic fluid (10), and umbilical cord blood (11). In addition, several populations of MSCs have been identified in various dental tissues (12), including dental pulp stem cells (DPSC) (13, 14), stem cells of human exfoliated deciduous teeth (15), periodontal ligament stem cells (PDLSCs) (16), dental follicle precursor cells (17, 18), and stem cells from apical papilla (19). Aside from the abilities of self-renewal and multipotent differentiation, MSCs commonly express specific genes for embryonic stem cells, such as Octamer-4 (Oct-4) and stage-specific embryonic Ag 4 (SSEA-4) (20, 21), and share a similar expression profile of cell surface molecules, such as Stro-1, SH2 (CD105), SH4 (CD73), CD90, CD146, CD29, but typically lack hematopoietic stem cell markers, such as CD34 and CD45 (22). At the functional level, MSCs display chemotactic properties similar to immune cells in response to tissue insult and inflammation, thus exhibiting tropism for the sites of injury (23-25) via production of anti-inflammatory cytokines and antiapoptotic molecules. These unique characteristics of MSCs make them attractive candidates for the development of novel allogeneic cell-based therapeutic strategies in harnessing inflammation in the repair or regeneration of a variety of damaged tissues (26).
A growing body of evidence has demonstrated that bone marrow-derived MSCs (BMSCs) are nonimmunogenic and, more importantly, display profound immunomodulatory and anti-inflammatory capabilities (25, 27, 28). BMSCs exhibit immunomodulatory effects via inhibiting the proliferation and function of innate and adaptive immune cells such as NK, dendritic cells, and T and B lymphocytes, as well as promoting the expansion of CD4+CD25+FoxP3+ regulatory T cells (Tregs) via direct cell-cell contact or/and soluble factors (25, 27-29). To date, several soluble factors either produced constitutively by MSCs or as a result of cross-talk with target immune cells have been attributed to the immunomodulatory properties of MSCs, including TGF-β1, hepatocyte growth factor (HGF), IL-10, PG2, NO, and IDO (29-34). Interestingly, TNF-α and IFN-γ, two important proinflammatory cytokines secreted by activated T cells, have been demonstrated to stimulate PGE2, TGF-β1, HGF, NO, and IDO expression by MSCs (29-34). These findings suggest that TNF-α and IFN-γ serve as critical feedback signal molecules in the cross-talk between immune cells and MSCs with a potential role in MSC-mediated immunosuppressive activities. Furthermore, the immunomodulatory and anti-inflammatory effects of MSCs have been demonstrated in the treatment of several animal disease models, including graft-versushost disease (35, 36), diabetes (37), rheumatoid arthritis (38), autoimmune encephalomyelitis (39, 40), systemic lupus erythematosus (41), periodontitis (42), inflammatory bowel disease (IBD) (43), and sepsis (44). These studies have provided convincing evidence that BMSC-based therapy may offer potential anti-inflammatory and immunomodulating effects in the treatment of a variety of inflammatory and autoimmune diseases (45).
Until now, despite the discovery of several MSCs from a variety of tissue sources, most cell-based therapies were conducted using the well-characterized MSCs derived from bone marrow (35-41) and, recently, adipose tissue (43, 46). In this study, we explore whether a new population of MSCs derived from human gingiva (GMSCs), a tissue that is not only easily accessible from the oral cavity but can often be obtained as a discarded biological sample, possesses both stem cell-like and immunomodulatory properties. Gingiva is a unique oral tissue attached to the alveolar bone of tooth sockets, recognized as a biological mucosal barrier and a distinct component of the oral mucosal immunity. Wound healing within the gingiva and oral mucosa is characterized by markedly reduced inflammation, rapid re-epithelialization, and fetal-like scarless healing, contrary to the common scar formation present in skin (47, 48). Such differences in wound healing between gingival/oral mucosa and skin may be attributed to the unique tolerogenic properties of the oral mucosal/gingival immune network (49). Several studies have isolated and characterized progenitor cells in the dermis of skin (4, 5) and within the epithelium of oral mucosa (50), but to date there is a lack of evidence whether a population of progenitor or stem cells exists in the spinous layer of human gingiva. In the present study, we reported an abundant source of mesenchymal stem cells, GMSCs, with unique immunomodulatory functions, in addition to the well-documented self-renewal and multipotent differentiation properties. GMSCs are capable of eliciting a potent inhibitory effect on T cell proliferation in response to mitogen stimulation. Mechanistically, GMSCs exert their anti-inflammatory effect, partly via IFN-γ-induced stimulation of IDO expression. We will test the in vivo GMSC-based therapy using an established murine model of inflammatory disease, specifically human IBD.
Ulcerative colitis and Crohn’s disease are two major forms of chronic IBD characterized by dysfunction of the innate and adaptive immunity, resulting in colonic mucosal injuries to the distal small intestine (51, 52). Several well-established murine models of human IBD (53) have provided useful tools for preclinical studies of therapeutic strategies, particularly stem cell-based therapies (43, 46, 54). In our study, GMSC infusion attenuated dextran sulfate sodium (DSS)-induced colitis, restored normal digestive function, and stabilized body weight in mice. These findings provide first evidence to support GMSCs as a promising and easily accessible cell source for cell-based therapy in experimental inflammatory diseases.
Materials and Methods
Mice
C57BL/6J mice (male, 8–10 wk old; The Jackson Laboratory) and beige nude/nude Xid (III) (female, 8–10 wk old; Harlan) were group housed at the Animal Facility of the University of Southern California (USC, Los Angeles, CA) under temperature (72 ± 3°F) and air (50 ± 20% relative humidity)- controlled condition and allowed unrestricted access to standard diet and tap water. Mice were allowed to acclimate for up to 7 days before inclusion in all experiments. All animal care and experiments were performed under the institutional protocols approved by the Institutional Animal Care and Use Committee at USC (USC nos. 11327 and 10941).
Progenitor cell isolation and culture
Human tissue samples were collected from clinically healthy gingiva of subjects who had no history of periodontal disease and relatively healthy periodontium. The gingival tissues were obtained as remnant or discarded tissues following routine dental procedures at the School of Dentistry, USC and the Outpatient Dental Clinic at Los Angeles County-USC Medical Center under the approved Institutional Review Board protocol at USC.
Gingival tissues were treated aseptically and incubated overnight at 4°C with dispase (2 mg/ml; Sigma-Aldrich) to separate the epithelial and lower spinous layer. The tissues were minced into 1- to 3-mm2 fragments and digested at 37°C for 2 h in sterile PBS containing 4 mg/ml collagenase IV (Worthington Biochemical). The dissociated cell suspension was filtered through a 70-μm cell strainer (Falcon), plated on nontreated 10-cm petri dishes (VWR Scientific Products) with complete α-MEM (Invitrogen) containing 10% FBS (BD Clontech), 100 U/ml penicillin/100 μg/ml streptomycin (Invitrogen), 2 mM l-glutamine, 100 mM nonessential amino acid, and 550 μM 2-ME (Sigma-Aldrich), and cultured at 37°C in a humidified tissue culture incubator with 5% CO2 and 95% O2. After 72 h, the nonadherent cells were removed. The plastic-adherent confluent cells were passaged with 0.05% trypsin containing 1 mM EDTA and continuously subcultured and maintained in the complete growth medium. Cells from second to sixth passages were used in the experiments.
CFU fibroblasts (CFU-F) assay
The CFU-F assay was performed as previously described (55, 56). After isolation of the single-cell suspension from human gingival tissues, 2 × 104 cells/cm2 were seeded in 60-mm petri dishes containing complete α-MEM and incubated at 37°C and 5% CO2. After 2–3 days, nonadherent cells were washed off with PBS, and cells were fed twice a week with fresh medium. After 14 days, colonies were washed twice with PBS, fixed for 5 min with 100% methanol, stained with 1% aqueous crystal violet, and counted under a microscope. A CFU-F was defined as a group of at least 50 cells. The CFU-F assay was repeated in five independent experiments.
Single-cell cloning
A serial dilution method was used to generate single-cell clonogenic culture. For single-cell culture, 100 μl of the final diluted cell suspension (10 cells/ml) was seeded into each well of a noncoated 96-well tissue culture plate containing 100 μl of culture medium (200 μl/well, four plates per donor; Falcon). The plates were screened for the presence of single-cell colonies, while wells containing more than two colonies were excluded from further analysis. Wells containing a single cell were allowed to reach confluence, transferred to 24-well dishes, and further expanded in the complete growth medium (57).
Population doubling assay
Clonal gingival precursor cells at each passage (P2, P5, P10, and P20) were seeded at 1.0 × 103 cells in 35-mm dishes in complete growth medium as above for several intervals (0, 2, 4, 6, 8, and 10 days). Cells were treated with 0.05% trypsin-EDTA and cell number was determined by hemocytometer. Population doubling time was calculated with the formula, population doubling time = (t − t0)*lg2/lg(N/N0). N0 and N represent the cell numbers at time t0 and t, respectively. Meanwhile, the accumulated population doublings were determined and calculated according to the standard 3T3 protocol as described previously (58).
Human bone marrow MSC culture
Human bone marrow aspirates from healthy adult donors (20–35 years of age) were purchased from AllCells and cultured with α-MEM supplemented with 10% FBS, 100 μM l-ascorbic acid-2-phosphate, 2 mM l-glutamine, 100 U/ml penicillin, and 100 μg/ml streptomycin as reported previously (55, 56).
Flow cytometric analysis
Approximately 5 × 105 cells at passage two or six were incubated with specific PE- or FITC-conjugated mouse mAbs for human CD45, CD29, CD73, CD90, CD105, CD146 (BD Biosciences), Stro-1, and SSEA-4 (R&D Systems) or isotype-matched control IgGs (Southern Biotechnology Associates) and subjected to flow cytometric analysis (55, 56) using a Beckman Coulter flow cytometer and FACScan program (BD Biosciences).
Multipotent differentiation of single colony-derived GMSCs
Osteogenic differentiation
GMSCs were plated at 5 × 105 cells/well in 6-well plates in MSC growth medium, allowed to adhere overnight, and replaced with Osteogenic Induction Medium (PT-3002; Cambrex) supplemented with dexamethasone, l-glutamine, ascorbic acid, and β-glycerophosphate. After 4–5 wk, the in vitro mineralization was assayed by Alizarin Red S (Sigma-Aldrich) staining and quantified by an acetic acid extraction method (59).
Adipogenic differentiation
As described above, GMSCs were plated in adipogenic induction medium supplemented with 10 μM human insulin, 1 μM dexamethasone, 200 μM indomethacin, and 0.5 mM 3-isobutyl-1-methylxanthine (Sigma-Aldrich). After 2 wk, Oil Red O staining was performed to detect intracellular lipid vacuoles characteristic of adipocytes, and the dye content was quantified by isopropanol elution (5-min shaking) and spectrophotometry at 510 nm (60).
Neuronal differentiation
GMSCs were plated at 1 × 104 cells/well in 8-well chamber slides (Nalge Nunc) coated with poly-d-lysine/laminin and cultured in DMEM/F12 (3/1; Invitrogen) supplemented with 10% FBS (Invitrogen), 1× N-2 supplement (Life Technologies), 100 U/ml penicillin and 100 μg/ml streptomycin, 10 ng/ml fibroblast growth factor 2, and 10 ng/ml epidermal growth factor (R&D Systems) and cultured for 14–21 days (61). In all experiments, medium was changed with 50% of fresh medium every 3–4 days.
Endothelial cell differentiation
GMSCs were plated at 1 × 104 cells/well in 8-well chamber slides (Nalge Nunc) precoated with fibronectin and cultivated in the presence or absence of endothelial growth medium 2 (Single-Quots; Lonza) for 7 days (62). Medium was changed every 2 days.
In vivo transplantation
Transplantation studies were conducted using single colony-derived GMSCs isolated from five different donors. Three well-characterized single colony-derived populations of GMSCs from separate donors were transplanted in triplicate (n = 3). Approximately 2.0 × 106 stem cells mixed with 40 mg of hydroxyapatite/tricalcium phosphate (HA/TCP) ceramic powder (Zimmer) were transplanted into the s.c. dorsal pouches of 8- to 10-wk-old female immunocompromised mice as previously described (55, 56).
RT-PCR
Total RNA was isolated from gingival tissues or cultured cells undergoing adipogenic and osteogenic differentiation using an RNeasy Mini kit (Qiagen). Adipocyte- and osteocyte-specific genes were amplified using the One-Step RT-PCR Kit (Qiagen. The specific primers were described as follows: Oct-4 forward primer, 5′-CGCACCACTGGCATTG TCAT-3′ and reverse primer, 5′- TTCTCCTTGATGTCACGCAC-3′; lipoprotein lipase (LPL) forward primer, 5′-CTGGTCGAAGCATTGGAAT-3′ and reverse primer, 5′-TGTAGGGCATCTGAGA ACGAG-3′; peroxisome proliferator-activated receptor γ2 (PPARγ2) forward primer, 5′-TCAGTGGAGACCGCCCA-3′ and reverse primer, 5′-TCTGAGGTCTGTCATTTTCTGGAG-3′; osteocalcin forward primer, 5′-TGAAGAGACCCAGGCGCTA-3′ and reverse primer, 5′-GATGTGGTCAGCCAACTCGTC-3′; and β-actin forward primer, 5′-TCAAGATCATTGCTCCTCCTG-3′ and reverse primer, 5′-CTGCTTGCTGATCCACATCTG-3′. All primers were synthesized at the Core Facility, Norris Comprehensive Cancer Center, at USC.
Immunofluorescence studies
Four percent paraformaldehyde-fixed cultured cells and paraffin-embedded or frozen sections of gingival tissue samples were immunolabeled with specific primary Abs followed by FITC- and/or rhodamine-conjugated secondary Abs (BD Biosciences). The primary Abs included mouse monoclonal IgG for human Oct-4 (C-10, sc-5279; Santa Cruz Biotechnology), SSEA-4 (R&D Systems), CD31 (BioLegend), β-tubulin III, and neurofilament (Sigma-Aldrich); mouse monoclonal IgM for human Stro-1 and human reverse telomerase transcriptase (hTERT; Novus); and rabbit polyclonal IgG for human glial fibrillary acidic protein (GFAP; Sigma-Aldrich). After the nuclei were counterstained with 4′,6-diamidino-2-phenylindole (DAPI), the samples were observed under a fluorescence microscope. Isotype-matched control Abs (Invitrogen) were used as negative controls. For semiquantification, positive signals in at least five random high-power fields were visualized, counted, and expressed as a percentage of total DAPI-positive cells (mean ± SD).
Histology and immunohistochemical studies
Gingival tissues or GMSC transplants were fixed with 10% formalin in PBS. For histological study, paraffin-embedded sections were stained with H&E. For immunohistochemical studies, the paraffin-embedded sections were incubated with specific primary Abs for human mitochondria, type I collagen, or Oct-4 and detected using the universal immunoperoxidase (HRP) ABC kit (Vector Laboratories). They were counterstained with hematoxylin. Isotype-matched control Abs (Invitrogen) were used as negative controls.
Western blot analysis
Cells were lysed with buffer containing 50 mM Tris-HCl (pH 7.5), 5 mM EDTA, 150 mM NaCl, 0.5% Triton X-100, 10 mM sodium fluoride, 20 mM 2-ME, 250 μM sodium orthovanadate, 1 mM PMSF, and complete protease inhibitor mixture (Sigma-Aldrich) and incubated at 4°C for 1 h. The lysates were ultrasonicated and centrifuged at 12,000 × g for 10 min. Protein concentrations were determined by bicinchoninic acid methods. Fifty to 100 μg of protein was separated on 8–10% polyacrylamide-SDS gels and electroblotted onto nitrocellulose membranes (Hybond ECL; Amersham Pharmacia). After blocking with TBS/5% nonfat dry milk for 2 h, the membrane was incubated overnight at 4°C with Abs against human IDO, cyclooxygenase 2 (COX-2), or inducible NO synthase (iNOS) followed by incubation with a HRP-conjugated secondary Ab (1/2000; Pierce) for 45 min at room temperature, and the signals were visualized by ECL detection. As a loading control, the blots were reprobed with a specific Ab against human β-actin (1/5000).
PBMC proliferation assay
Different numbers of human GMSCs or BMSCs (2 × 103, 4 × 103, 2 × 104) were plated in triplicates onto 96-well plates in 100 μl of complete medium (RPMI 1640 medium supplemented with 10% FBS, 2 mM l-glutamine, 50 U/ml penicillin, and 50 μg/ml streptomycin) and were allowed to adhere to the plates overnight. Human PBMCs (AllCells), resuspended at 2 × 105/ml, were added to wells (2 × 104 cells/well in a 100-μl volume) containing or lacking MSCs in the presence or absence of 5 μg/ml PHA (Sigma-Aldrich). Cocultures without PHA were used as controls. After 72 h, 100 μl of cells from each well was transferred to new 96-well plates with 10 μl of Cell Counting Kit-8 (Dojindo Laboratories). The absorbance at 450 nm was measured with a microplate reader.
Transwell experiments were performed in 24-well Transwell plates with 0.4-μm pore membranes (Corning Costar). A total of 2 × 105 PBMCs was seeded to the upper compartment of the chamber, whereby different numbers of GMSCs or BMSCs (2 × 104, 4 × 104, 2 × 105) were seeded to the lower compartment. Cells were cultured in the presence or absence of 5 μg/ml PHA (Sigma-Aldrich) for 72 h and analyzed as described above.
In other experiments, neutralizing Abs for human IL-10, TGF-β1, or an isotype-matched mAb (10 μg/ml; R&D Systems) and chemical antagonists for COX-2 (indomethacin, 20 μM; Sigma-Aldrich), iNOS (N-nitro-l-arginine methyl ester (l-NAME), 1 mM; Sigma-Aldrich), and IDO (1-methyl-l-tryptophan (1-MT), 500 μM; Sigma-Aldrich) were added into the coculture. All experiments were performed in triplicate and were repeated at least twice.
IDO activity/kynurenine assay
Kynurenine is the product of IDO-dependent catabolism of tryptophan. Therefore, the biological activity of IDO was evaluated by determining the level of kynurenine in GMSC culture in response to IFN-γ (PeproTech) or coculture with PBMCs in the presence or absence of 5 μg/ml PHA. One hundred microliters of conditioned culture supernatant was mixed with 50 μl of 30% TCA, vortexed, and centrifuged at 10,000 × g for 5 min. Afterward, 75 μl of the supernatant was added to an equal volume of Ehrlich reagent (100 mg of p–dimethylbenzaldehyde in 5 ml of glacial acetic acid) in a 96-well plate and incubated at room temperature for 10 min. The absorbance at 492 nm was determined. The concentration of kynurenine was quantified according to a standard curve of defined kynurenine (Sigma-Aldrich) concentration (0–150 μM).
DSS-induced murine colitis
C57BL/6 mice were randomly divided into the following groups (n = 6): 1) naive group without any treatment, 2) DSS, 3) DSS with human BMSC treatment, and 4) DSS with GMSC treatment. Acute colitis was induced by administering 3% (w/v) DSS (molecular mass 36,000–50,000 Da; MP Biochemicals) in drinking water, which was fed ad libitum for 7 days (46, 54). Two × 106 of GMSCs or BMSCs resuspended in 200 μl of PBS were i.p. injected into mice 1 day after initiation of DSS treatment. Colitis severity was scored (0–4) by evaluating the clinical disease activity through daily monitoring of weight loss, stool consistency/diarrhea, and presence of fecal bleeding (46, 54). At day 10 after colitis induction, mice were sacrificed by CO2 euthanasia, and the entire colon was quickly removed and gently cleared of feces with sterile PBS. For protein extraction and myeloperoxidase (MPO) activity assay, colon segments were rapidly frozen in liquid nitrogen. For histopathological analysis, colon segments were fixed in 10% buffered formalin phosphate and paraffin-embedded sections were prepared for H&E staining. Histological scores were blindly determined as previously described (54).
The infiltration of neutrophils in the colon was assessed by measuring MPO activity as described before (46, 54). Briefly, colon specimens were homogenized at 50 mg/ml in phosphate buffer (50 mM, pH 6.0) with 0.5% hexadecyltrimethylamonium bromide. The samples were centrifuged at 11,000 × g for 15 min at 4°C. The supernatants were diluted 1/30 with 50 mM phosphate buffer (pH 6.0) containing 0.167 mg/ml o-dianisidine (Sigma-Aldrich) and 0.0005% H2O2 (v/v). Changes in absorbance at 450 nm were recorded with a spectrophotometer every 30 s over 3 min. MPO activity was expressed in units per g of wet tissues, where 1 unit represents the enzyme activity required to degrade 1 μM H2O2/min/ml at 24°C.
ELISA
The level of IFN-γ, IL-6, and IL-17 in colon tissue lysates was detected using mice ELISA Ready-SET-Go (eBioscience) according to the manufacturer’s instructions.
Statistical analysis
All data are expressed as mean ± SD from at least three independent experiments. Differences between experimental and control groups were analyzed by a two-tailed unpaired Student’s t test using SPSS. Values of p < 0.05 were considered statistically significant.
Results
Isolation and characterization of MSCs from human gingival tissues
A variety of postnatal or adult stem cells and/or precursor cells have been reported in several complex human tissues or organs (8, 22), including the dental tissues (63); however, to date, no study has confirmed whether such a population of precursor cells exists in human gingiva. Histologically, gingiva is composed of an epithelial layer, a basal layer, and a lower spinous layer that is similar to the dermis of the skin. In this study, we demonstrated that human gingival tissues display Oct-4-, SSEA-4-, and Stro-1- positive signals that were clustered in the subepithelial connective tissue proper (the lower spinous layer) (Fig. 1, A and B). Meanwhile, dual-color immunofluorescence studies showed the coexpression of Oct-4/SSEA-4 or Oct-4/Stro-1 by a proportion of cells in gingival tissues (supplemental Fig. S1A).4 In addition, the expression of Oct-4 mRNA in gingival tissues was further confirmed by RT-PCR (supplemental Fig. S1B). These results suggest the presence of a putative population of stem cells in human gingiva (20, 21).
FIGURE 1.
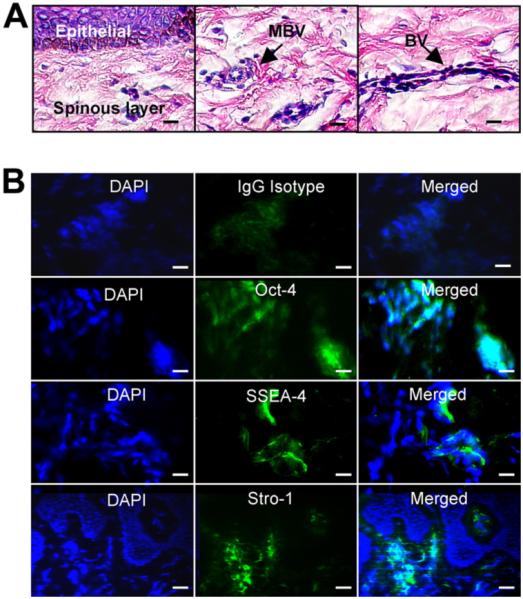
Expression of stem cell markers in human gingival tissues. A, H&E staining of paraffin sections of human gingival tissues. MBV, Microvascular blood vessel; BV, blood vessel. B, Frozen sections were immunostained with mouse mAbs specific for human Oct-4, SSEA-4, and Stro-1 or an isotype-matched mouse IgG, followed by incubation with FITC-conjugated secondary Abs. Images were observed under a fluorescence microscope. Scale bar, 100 μm. The results are representative of at least five independent experiments.
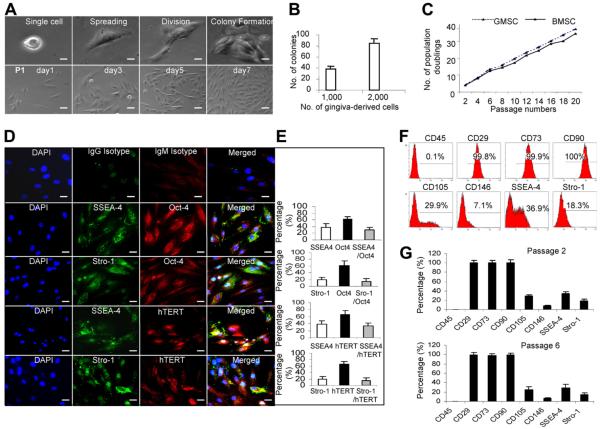
Using normal gingival tissues obtained from five healthy donors, we isolated a population of nonepithelial progenitor cells, namely, human GMSCs, and characterized their stem cell-like properties. Similar to BMSCs, human GMSCs adhered to culture dishes and organized as single CFUs (Fig. 2A). Colony formation was observed in ~4–6% of GMSCs (Fig. 2B). Like other dental-derived stem cells such as PDLSCs and stem cells of exfoliated deciduous teeth (15, 16), GMSCs showed a relatively higher proliferation rate and number of population doublings as compared with BMSCs (Fig. 2C). Adherent cells isolated from a small piece of gingival tissue (~2 × 2 mm2) usually reached confluence (~1–2 × 106 cells) after culture for 10~14 days (data not shown). Immunocytochemical studies showed that ~60% of single colony-derived GMSCs expressed Oct-4 and hTERT, respectively, while 18–20% of cells expressed Stro-1 (Fig. 2, D and E). Dual-color immunostaining revealed ~30% of GMSCs coexpressed SSEA-4/Oct-4 while ~15% of cells coexpressed Stro-1/Oct-4 or Stro-1/hTERT (Fig. 2, D and E), confirming the presence of an early mesenchymal progenitor cell phenotype. To further verify the stem cell phenotypic markers of GMSCs using flow cytometry, we observed that ~100% of GMSCs were negative for CD45, a hematopoietic cell surface marker, but consistently expressed CD29, CD73, and CD90/Thy-1 at passages two and six, while 36.9, 29.9, and 18.3% of GMSCs were consistently positive for SSEA-4, CD105, and Stro-1, respectively (Fig. 2, F and G). Most recently, a study reported that BMSCs could be expanded in monolayer up to passage five without altering their undifferentiated phenotype (64). Similarly, our results suggested that GMSCs could be steadily expanded in vitro and still maintained their early phenotypes at passage six. In addition to these stem cell markers, MSCs derived from various human tissues including bone marrow (22), adipose (65), and dermis (5, 65) have also been reported to express extracellular matrix components characteristic of mesenchymal stromal cells, such as vimentin, fibronectin, and type I collagen. Consistent with these findings, our in vitro-cultured GMSCs also expressed type I collagen as determined by Western blot analysis (supplemental Fig. S1C).
FIGURE 2.
Isolation and subcloning of MSCs from human gingival tissues. A, Subcloning and culture of MSCs from gingival tissues in α-MEM supplemented with 10% FBS, 1× nonessential amino acids and antibiotics. Scale bar, 100 μm. B, Capability of colony formation of gingiva-derived cells. C, Population doublings of GMSCs. D, Expression of stem cell markers in GMSCs. Cells cultured in an 8-well slide chamber were fixed and immunostained with specific Abs for human Stro-1, SSEA-4, Oct-4, or hTERT. Cells were incubated with rhodamine- or FITC-conjugated secondary Abs and then observed under a fluorescence microscope. Scale bar, 100 μm. E, Semiquantification of positive signals in at least five random high-power fields and expressed as the percentage of total DAPI-positive cells (mean ± SD). F, Expression of cell surface markers on GMSCs as determined by flow cytometry. G, Quantification of percentage of cells expressing respective surface markers from independent experiments from flow cytometry data (mean ± SD). The results are representative of at least five independent experiments.
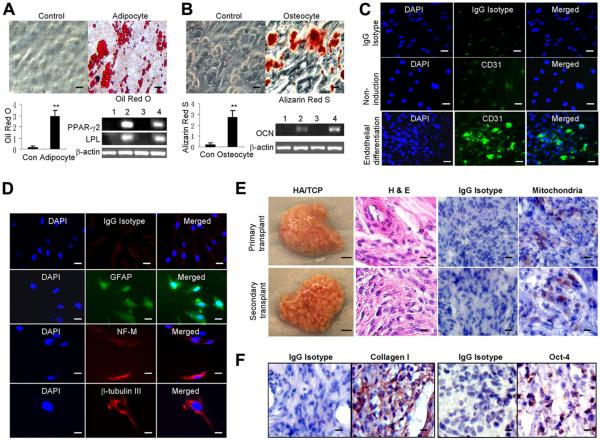
GMSCs are capable of multiple differentiation
We next examined the multidifferentiation potential of GMSCs. Under adipogenic and osteogenic induction conditions, single colony-derived GMSCs could differentiate into adipocytes and osteoblasts as determined by Oil Red O (Fig. 3A) and by Alizarin Red S staining (Fig. 3B), respectively. Adipogenic differentiation was further confirmed by the increased expression of specific adipogenic markers, including PPARγ2, LPL, as determined by RT-PCR (Fig. 3A). Likewise, the osteogenic differentiation of GMSCs was further confirmed by the increased expression of osteocalcin, an osteogenic marker (Fig. 3B). When cultured on fibronectin-coated slides in endothelial cell growth medium for 1 wk, ~36.7 ± 8.7% of GMSCs expressed the endothelial cell marker CD31, whereas no CD31-positive cells were observed under normal noninduction conditions (Fig. 3C and supplemental Fig. S2A). Under neural differentiation conditions, ~34.8 ± 9.4%, 22.27 ± 6.5%, and 16.8 ± 5.1% of the cells were positive for GFAP, neurofilament 160/200 (NF-M), and β-tubulin III, respectively (Fig. 3D and supplemental Fig. S2B), whereas no cells positive for these neural markers were detected in normal noninduction medium (supplemental Fig. S2, B and C). These findings, consistent with mesenchymal stem cell properties described in other tissues, indicate that single colony-derived human gingiva stem cells represent a putative MSC population with clonogenic renewal and multipotent differentiation capacities.
FIGURE 3.
Multipotent differentiation of GMSCs. A, Adipogenic differentiation of GMSCs. After culture under normal growth conditions (control, lanes 1 and 3) or adipogenic differentiation (lanes 2 and 4) conditions for 2 wk, adipocyte differentiation was determined by Oil Red O staining and RT-PCR analysis of specific genes. The graph shows the quantification of the Oil Red O dye content in differentiated adipocytes from independent experiments (mean ± SD). B, Osteogenic differentiation of GMSCs. After culture under normal growth conditions (control, lanes 1 and 3) or osteogenic differentiation conditions (lanes 2 and 4) for 4–5 wk, osteogenic differentiation was determined by Alizarin Red S staining and RT-PCR analysis of specific genes. The graph shows the quantification of the Alizarin Red S dye content in differentiated osteocytes from independent experiments (mean ± SD). OCN, Osteocalcin. Scale bar, 50 μm. C, Endothelial differentiation of GMSCs after culture in endothelial cell culture conditions for 7 days. Cells were immunostained with a mouse monoclonal IgG for human CD31, followed by incubation with FITC-conjugated secondary Ab, and then observed under a fluorescence microscope. Scale bar, 100 μm. D, Neural differentiation of GMSCs after culture in neural cell culture conditions for 14 days. Cells were immunostained with different primary Abs for neural markers, including GFAP, neurofilament M (NF-M), and β-tubulin III, followed by incubation with rhodamine- or FITC-conjugated secondary Abs and then observed under a fluorescence microscope. Scale bar, 100 μm. E, In vivo transplantation of GMSCs. Approximately 2.0 × 106 stem cells mixed with 40 mg of HA/TCP ceramic powder were s.c. transplanted into the dorsal surface of 8- to 10-wk-old female immunocompromised mice. Four weeks later, the transplants were harvested and cells were recovered for secondary transplantation. H&E staining was performed for histological examination. The cells of human origin were confirmed by immunostaining with a specific Ab for human mitochondria. Scale bar, 50 μm. F, Immunohistochemical studies of the expression of human type I collagen and Oct-4 in GMSC-derived transplants. The results are representative of at least three independent experiments.
To explore the in vivo differentiation capability, the expanded subclonal GMSCs (2 × 106) were s.c. transplanted using HA/TCP as a carrier in immunocompromised mice. Similar transplants were conducted using human BMSCs as another source of stem cells. Unlike BMSC transplants, which showed formation of bone nodules in vivo, GMSCs from several donors consistently regenerated connective tissue-like transplants (five of five mice), with the histological features of the early connective tissue phenotype, including the presence of collagen fibers (Fig. 3E). The human origin of cellular components of the transplants was confirmed by immunostaining with specific Abs to human mitochondria (Fig. 3E). Therefore, under our experimental conditions using HA/TCP as carrier, we did not observe osteogenic differentiation in s.c. transplants with GMSCs. The fate of in vivo lineage commitment of MSCs depends on multiple factors such as different tissue origins, the hierarchy of lineage commitment, cell culture conditions, local growth factors, and transplantation conditions (carriers and recipients) (13, 16). Then further studies are warranted to determine whether in vivo osteogenic differentiation of GMSCs can be induced by modifying the transplant carrier and niche components.
To further confirm the renewal and differentiation capability of GMSCs, we performed serial s.c. transplantation using the HA/TCP carrier and 2 × 106 GMSCs in immunocompromised mice. At 4 wk after primary transplantation, the transplants were harvested and digested single cells were retransplanted s.c. into immunocompromised mice to generate the secondary transplant (Fig. 3E). Our results indicated that GMSCs recovered from primary transplants maintained the expression of Oct-4 and the in vivo ability to self-renew and formed connective-like tissues expressing type I collagen (Fig. 3F). Together, these results indicated that GMSCs represent a new population of stem cells derived from human gingiva with self-renewal and unique differentiation capabilities.
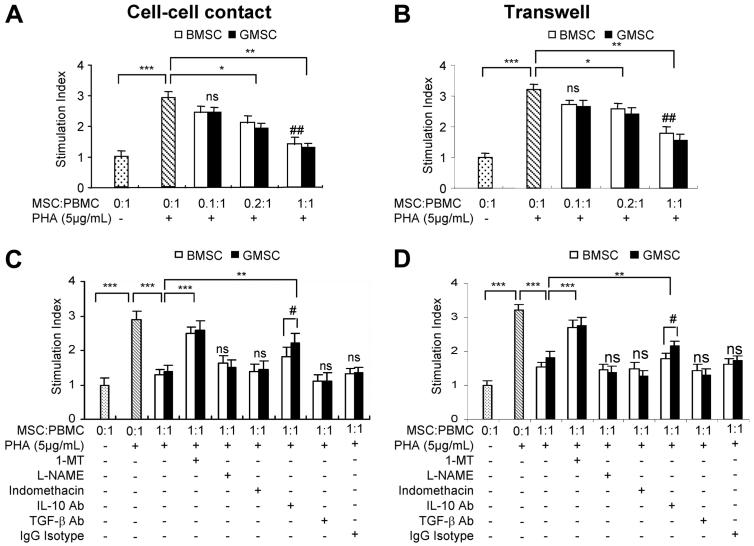
GMSCs are capable of suppressing PBMC proliferation
Next, we sought to determine whether GMSCs had immunosuppressive effects on the proliferation of T lymphocytes in response to mitogenic stimulation in vitro. To this end, GMSCs or BMSCs were cocultured under cell-cell contact or Transwell systems with increasing numbers of human PBMCs in the presence of PHA for 72 h. Our results showed that GMSCs, similar to BMSCs, inhibited mitogen-stimulated PBMC proliferation in a cell density-dependent manner under both cell-cell contact and Transwell cultures (Fig. 4, A and B). Meanwhile, our data also indicated that GMSC-mediated inhibition of PBMC proliferation was more severe under cell-cell contact conditions than in Transwells (p < 0.05; Fig. 4, A and B). In addition, the viability of PBMCs cocultured with GMSCs under both cell-cell contact and Transwell conditions was >95% as determined by trypan blue exclusion (data not shown). These results suggest that direct cell-cell contact contributes, at least in part, to the mechanisms of GMSC-mediated immunosuppression via suppression of PBMC proliferation.
FIGURE 4.
Inhibitory effects of GMSCs on PHA-stimulated PBMC proliferation. A and B, 2 × 105 PBMCs were cultured alone or cocultured with increasing numbers of GMSCs or BMSCs under both cell-cell contact (A) and Transwell (B) conditions in the presence or absence of 5 μg/ml PHA for 72 h. Afterward, cell numbers were counted using a Cell Counting Kit-8. *, p < 0.05; **, p < 0.01; ***, p < 0.001; ns, no significant difference; ##, p < 0.05 compared with Transwell. C and D, GMSCs or BMSCs were pretreated for 2 h wit h 1-MT (1 mM), l-NAME (500 μM), indomethacin (10 μM), or neutralizing Abs for IL-10 or TGF-β1 (10 μg/ml), followed by coculturing with the same number of PBMCs (1/1) under both cell-cell contact (C) and Transwell (D) conditions in the presence or absence of 5 μg/ml PHA for 72 h. Afterward, cell numbers were counted using a Cell Counting Kit-8. *, p < 0.05; **, p < 0.01; ***, p < 0.001; #, p < 0.05; ns, no significant difference (mean ± SD). The results are representative of at least three independent experiments.
Soluble mediators involved in GMSC-mediated inhibition of PBMCs
We next determined the role of soluble mediators in GMSC-mediated suppression of PBMC proliferation. To this purpose, GMSCs or BMSCs were pretreated with neutralizing Abs for human IL-10, TGF-β1, or an isotype-matched mAb or with chemical antagonists for COX-2 (indomethacin), iNOS (l-NAME), or IDO (1-MT) for at least 2 h, followed by coculture with PBMCs in the presence of PHA stimulation for 72 h. Our results showed that pretreatment with 1-MT, a specific inhibitor of IDO, significantly reversed GMSC- and BMSC-mediated inhibition of PBMC proliferation under both cell-cell contact and Transwell conditions (p < 0.001; Fig. 4, C and D). In addition, treatment with IL-10-neutralizing Ab could reverse the inhibitory effect of PBMC proliferation exerted by GMSCs to a better extent than that mediated by BMSCs (p < 0.05; Fig. 4, C and D). However, treatment with neutralizing Ab for TGF-β1, antagonists for COX-2 and iNOS, or an isotype-matched control IgG could not reverse the inhibitory effects of GMSCs on PBMC proliferation (Fig. 4, C and D). These results suggest that IDO and IL-10, not TGF-β1 or COX-2 or iNOS, may contribute, in part, to GMSC-mediated suppression of PBMCs.
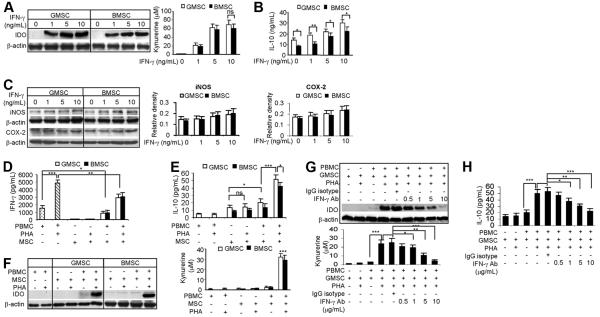
Up-regulation of IFN-γ-induced IDO and IL-10 contributes to GMSC-mediated suppression of PBMCs
Previous studies have shown that the inflammatory cytokine IFN-γ is capable of regulating the immunomodulatory functions of MSCs via up-regulation of a variety of immunosuppressive factors, including IDO and IL-10 (29-34). MSCs have been reported to inhibit the secretion of IFN-γ by PHA-activated immune cells (11, 31, 32). We examined whether IFN-γ could up-regulate IDO and IL-10 expression in GMSCs. In this study, we demonstrated that IFN-γ induced IDO protein expression in GMSCs in a dose-dependent manner, albeit to a similar extent as in BMSCs (Fig. 5A). Meanwhile, functional assays confirmed that the concentration of kynurenine, a metabolic product of IDO, increased in supernatants of both GMSCs and BMSCs in response to IFN-γ stimulation (Fig. 5A), suggesting that the MSC-induced IDO molecule was active. Moreover, IFN-γ also stimulated IL-10 secretion by GMSCs in a dose-dependent manner, an effect stronger than that observed in BMSCs (p < 0.05; Fig. 5B). However, only a mild increase in the expression of iNOS and COX-2 was detected in both GMSCs and BMSCs in response to IFN-γ (Fig. 5C).
FIGURE 5.
IFN-γ-induced IDO expression and IL-10 secretion by GMSCs. A–C, GMSCs or BMSCs were stimulated with increasing concentrations of IFN-γ for 24 h. Then the expression of IDO protein was determined by Western blot, while the IDO activity was analyzed by measuring the concentration of kynurenine in the conditioned medium (A). IFN-γ-induced IL-10 secretion in the supernatants was determined by using ELISA (B), whereas the expression of iNOS and COX-2 in MSCs in response to IFN-γ was determined by Western blot (C). D–F, Two × 105 PBMCs were cultured alone or cocultured with the same number of GMSCs or BMSCs under cell-cell contact conditions in the presence or absence of 5 μg/ml PHA for 72 h. Afterward, the concentrations of IFN-γ (D) and IL-10 (E) in the supernatants were determined by using ELISA, whereas IDO protein expression and activity were determined by Western blot and kynurenine assay, respectively (F). G and H, PBMCs were pretreated for 2 h with different concentrations of specific neutralizing Ab for human IFN-γ (0.5–10 μg/ml) or an isotype-matched mouse IgG (10 μg/ml), followed by coculturing with the same number of GMSCs (1/1) under cell-cell contact conditions in the presence or absence of 5 μg/ml PHA for 72 h. Then IDO protein expression and activity were determined by Western blot and kynurenine assay, respectively (G), whereas the concentration of IL-10 in the supernatants was determined by using ELISA (H). *, p < 0.05; **, p < 0.01; ***, p < 0.001; ns, no significant difference (mean ± SD). The results are representative of at least three independent experiments.
We next determined whether immunosuppressive factors such as IFN-γ, IL-10, and IDO were expressed by PBMCs cultured alone or cocultured with MSCs in the presence or absence of PHA stimulation. As expected, mitogen stimulation robustly triggered IFN-γ production by PBMCs (p < 0.001); however, this burst of IFN-γ was abrogated by coculture with GMSCs, both at the basal level and in the presence of PHA stimulation (Fig. 5D). We confirmed that PBMCs secreted very low levels of IL-10 either in the absence or presence of PHA, and PHA only had a slight effect on IL-10 production in both GMSCs and BMSCs (p > 0.05; Fig. 5E). However, the secretion of IL-10 by GMSCs was moderately induced in the presence of PBMCs (p < 0.05), an effect that was more augmented when cocultured with PHA-stimulated PBMCs (p < 0.001; Fig. 5E), albeit to a greater response than in BMSCs (p < 0.05; Fig. 5E). In addition, we determined the expression and activity of IDO under similar conditions. As shown in Fig. 5F, PHA stimulation had no effects on IDO protein expression and activity in both PBMCs and BMSCs. However, in the presence of PHA-stimulated, not the unstimulated PBMCs, a substantial upregulation of IDO expression and activity was observed in both GMSCs and BMSCs (Fig. 5F). Taken together, these results suggest that GMSCs upon activation by PHA-stimulated PBMCs are capable of enhanced IL-10 secretion and IDO activity.
Based on these findings, we postulate that the increased IL-10 secretion and IDO expression by GMSCs may be attributed to an increased IFN-γ production by PHA-stimulated PBMCs. We pretreated PBMCs with increasing concentrations of IFN-γ-neutralizing Ab followed by coculture with GMSCs in the presence or absence of PHA for 24 h. Our results showed that treatment with IFN-γ-neutralizing Ab led to a dose-dependent inhibition of IDO expression/activity and IL-10 secretion by GMSCs upon coculture with PHA-stimulated PBMCs (Fig. 5, G and H). Similar results were observed in BMSCs, whereas no inhibitory effects were seen in the control group treated with an isotype-matched control Ab (Fig. 5, G and H). Altogether, these findings support the notion that IFN-γ directly contributes to GMSC-mediated suppression of PBMCs through the up-regulation of IL-10 and IDO expression.
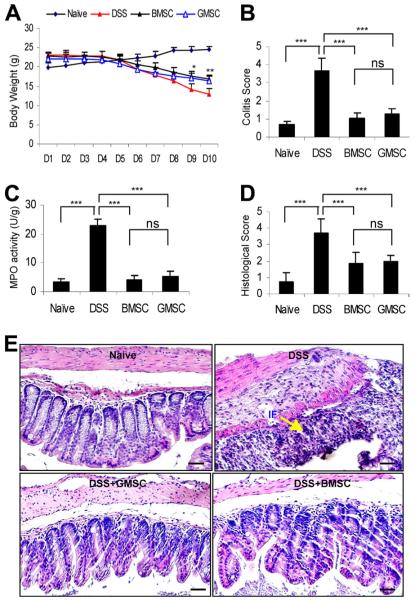
GMSC-based therapy ameliorates DSS-induced colitis in mice
Based on the unique immunomodulatory properties of GMSCs, we next explored the potential therapeutic effects of GMSC infusion in harnessing inflammation and reversing inflammatory-related tissue injuries using an established murine model of colitis induced by oral administration of DSS (54). Similar to previous reports (46, 54), we confirmed that oral administration of 3% DSS for 7 days induced acute colitis in C57BL/6 mice characterized by an overall elevation of colitis scores based on the presence of sustained weight loss and bloody diarrhea/loose feces (Fig. 6, A and B). Histological studies revealed severe colonic transmural inflammation with increased wall thickness and localized inflammatory cell infiltration, epithelial ulceration with degeneration of crypt architecture, and loss of goblet cells (Fig. 6, D and E). The histopathological disease activity of induced colitis was assessed by measuring MPO activity released from local neutrophil infiltration (Fig. 6C). Importantly, our results showed that systemic infusion with GMSCs, similar to BMSCs, protected mice against colitis-related tissue injuries and reduced the overall disease severity, shown here as a decrease in disease score, reversing and stabilizing of body weight (p < 0.05 or p < 0.01, compared with treatment with DSS alone at day 9 or day 10), suppressing of colonic inflammation (p < 0.001; Fig. 6, A and B), and MPO activities (p < 0.001; Fig. 6C). Histologically, GMSCs significantly ameliorated colonic transmural inflammation and decreased wall thickness, restored goblet cells, and suppressed mucosal ulceration and focal loss of crypts, thus restoring normal intestinal architecture and resulting in a reduced histological colitis score (p < 0.001; Fig. 6, D and E). These compelling findings suggest that cell-based therapy using GMSCs can alleviate DSS-induced experimental colitis in mice.
FIGURE 6.
Treatment with GMSCs ameliorates DSS-induced experimental colitis in C57BL/6 mice. Colitis was induced by oral administration of 3% DSS in drinking water for 7 days. Two × 106 of GMSCs or BMSCs in 200 μl of PBS were i.p. injected into mice 1 day after initiation of DSS treatment. Mice without any treatment (naive mice) or mice that received 200 μl of PBS served as controls. At day 10, mice were sacrificed. A and B, Clinical progression of the disease was monitored by body weight changes (A) and colitis score evaluation (B), whereas in A, *, p < 0.05 and **, p < 0.01 compared with DSS alone. C, Colonic MPO activity assays. D and E, Histopathological analysis of colitis. IF, Inflammation. Scale bar, 200 μm. *, p < 0.05; **, p < 0.01; ***, p < 0.001; ns, no significant difference (mean ± SD). The results are representative of at least three independent experiments.
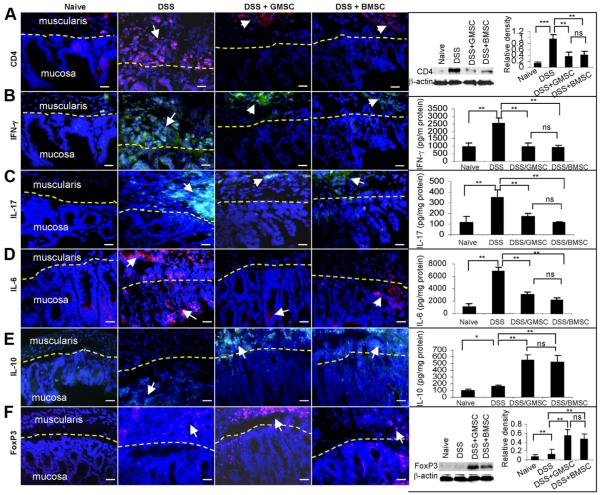
We next investigated the in vivo effects of GMSCs on inflammatory cell response and production of local inflammatory cytokines mechanistically linked to inflammatory-related colonic injuries in DSS-induced colitis (43, 46, 54). We observed an increased infiltration of CD4+ T lymphocytes in the mucosal and muscularis layers of the inflamed colons of colitic mice as determined by immunofluorescence studies and semiquantified Western blot analysis (p < 0.001; Fig. 7A). Meanwhile, immunohistochemical studies showed abundant expression of proinflammatory cytokines (IL-6 and IFN-γ) in the mucosal and muscularis layers of the inflamed colons of colitic mice (Fig. 7, B and D), whereas IL-17 signals were restricted only in the muscularis layer (Fig. 7C). The increased expression of these inflammatory cytokines in inflamed colons was further confirmed and quantified by ELISA (p < 0.01; Fig. 7, B–D).
FIGURE 7.
GMSC treatment attenuates colonic inflammatory responses but induces Treg responses in DSS-induced experimental colitis in C57BL/6 mice. Colitis was induced by oral administration of 3% DSS in drinking water for 7 days. Two × 106 of GMSCs or BMSCs in 200 μl of PBS were i.p. injected into mice 1 day after initiation of DSS treatment. Mice without any treatment (naive mice) or mice that received 200 μl of PBS served as controls. At day 10, mice were sacrificed. A, Immunofluorescence staining and Western blot analysis of the infiltrated CD4+ T lymphocytes in inflamed colons. B–E, Immunofluorescence staining and ELISA of IFN-γ, IL-17, IL-6, and IL-10 in inflamed colons. F, Immunofluorescence staining and Western blot analysis of FoxP3 in inflamed colon tissues. Scale bars, 100 μm. *, p < 0.05; **, p < 0.01; ***, p < 0.001; ns, no significant difference (means ± SD). The results are representative of at least three independent experiments.
Systemic infusion with GMSCs, similar to BMSCs, significantly attenuated the local recruitment of CD4+ T lymphocytes at the colonic sites (p < 0.01; Fig. 7A). The suppression of CD4+ T lymphocyte infiltration elicited by treatment with GMSCs or BMSCs was accompanied by down-regulated levels of inflammatory cytokines, specifically at the intestinal mucosa, with minimal basal activities in the deeper layers (p < 0.01; Fig. 7, B–D). Interestingly, systemic infusion of GMSCs, similar to BMSCs, also significantly increased the level of anti-inflammatory cytokine IL-10 and promoted the infiltration of regulatory T cells (Tregs) demonstrated as the expression of the specific transcriptional factor FoxP3 or by immunostaining, ELISA and semiquantitative Western blot analyses (p < 0.01; Fig. 7, E and F). These compelling findings suggest that GMSC treatment confers significant protection against inflammatory-related colonic injuries in experimental colitis by suppressing inflammatory cell infiltration and proinflammatory cytokine secretion as well as by increasing the accumulation of Tregs and IL-10 expression at the local intestinal sites.
Discussion
In the present study, we have isolated and characterized a new population of precursor cells from human gingival tissues, termed GMSC, which exhibit several unique stem cell-like properties as MSCs derived from bone marrow and other postnatal tissues (8, 22). These characteristics include in vitro proliferation as plastic-adherent cells with fibroblast-like morphology, colony-forming ability, multipotent differentiation into different cell lineages, including mesodermal (adipocytes, osteocytes), endodermal, and neuroectodermal progenies, and expression of mesenchymal cell surface markers and stem cell-specific genes (1-3, 20, 21). More importantly, we have demonstrated that single colony-derived GMSCs possess in vivo self-renewal and differentiation capacities, further supporting their stem cell-like properties. In addition, compared with MSCs derived from several other adult dental tissues such as DPSCs (13, 14) and PDLSCs (16, 18), GMSCs express a similar profile of cell surface molecules, a high proliferative rate, and an increased population doubling, and thus can be easily expanded ex vivo for several cell-based clinical applications. However, s.c. transplantation of GMSCs could form connective tissue-like structures, whereas transplantation of DPSCs and PDLSCs could generate dentin-like and cementum/PDL-like structures (13, 14, 16). These findings have provided evidence that human gingiva, an easily accessible tissue from the oral cavity or a discarded tissue sample following some dental procedures, might serve as a unique source of postnatal stem cells with potential therapeutic functions in tissue regeneration and repair (1-3, 12).
In recent years, a major breakthrough was the discovery that MSCs are immune privileged and, more importantly, possess profound immunosuppressive and anti-inflammatory effects both in vitro and in vivo via inhibiting the proliferation and function of several major types of innate and adaptive immune cells such as NK cells, dendritic cells, and T and B lymphocytes (25, 27-29). However, to date, the underlying mechanisms of MSC-mediated suppression of lymphocyte proliferation remain largely unknown (28, 30, 31, 33, 66, 67). In one study, the suppressive activity of human bone marrow MSCs was shown to be independent of cell-cell contact (31); however, several other studies have reported that cell-cell contact contributed, at least in part, to the immunosuppression mediated by MSCs derived from human bone marrow, adipose, or umbilical cord blood (32, 68, 69). In this study, we showed that GMSCs when cocultured with PBMCs under cell-cell contact conditions exhibited a slightly stronger inhibition on PBMC proliferation than GMSCs when cocultured with PBMCs separately in Transwells, thus supporting the notion that the cell-cell contact mechanism may partly contribute to GMSC-mediated suppression of PBMC proliferation.
Various studies have indicated that soluble factors such as TGF-β1, HGF, IL-10, HLA-G5, PGE2, NO, and IDO play an important role in MSC-mediated immunosuppression (27-35, 66-69). However, it is noteworthy that the relative contribution of these soluble factors to the immunosuppressive effects of MSCs varies under different experimental conditions, and neutralizing these soluble factors does not completely abrogate the immunosuppressive activity of MSCs (32). For example, IL-10, HGF, and TGF-β1 have been shown to contribute to BMSC-mediated immunosuppression (33, 66), but in other studies, these three factors appeared not to be related to immunosuppression mediated by BMSCs and human adipose-derived stem cells (hASCs) (30, 31, 67). In addition, controversies about the role of PGE2 in MSC-mediated immunosuppression have also been reported. In some studies, blocking PGE2 production by COX-2 resulted in partial abrogation of immunosuppression by BMSCs and hASCs (29, 30, 32, 33); however, Cui et al. (67) have recently reported that PGE2 is the major soluble factor in the in vitro inhibition of allogeneic lymphocyte reaction. In the present study, we observed that blocking TGF-β1, PGE2, or NO by using specific neutralizing Abs or antagonists for synthetic enzymes showed no obvious effects on GMSC-mediated suppression of PBMC proliferation. However, blocking IL-10 led to moderate abrogation of GMSC-mediated suppression of PBMC proliferation, albeit to a greater extent than in BMSCs. These findings suggest that IL-10 might partially contribute to GMSC-mediated immunosuppression.
IDO is an enzyme that catabolizes tryptophan, an essential amino acid. A growing body of evidence has indicated that IDO plays a critical role in immunosuppression mediated by MSCs of various tissue origins, whereas 1-MT, a specific antagonist of IDO, can abrogate the immunosuppressive effects (30, 31, 32, 33, 70). The immunomodulatory effects of IDO are attributed to tryptophan depletion and/or accumulation of the downstream metabolites such as kynurenine, 3-hydroxykynurenine, and 3-hydroxyanthranilic acid (30, 31, 32, 33, 70). Most recently, studies have shown that IDO activity is involved in PDLSCs and gingival fibroblast-mediated immunosuppression (70, 71). Consistently, we have demonstrated that the addition of 1-MT also significantly ablated GMSC-mediated suppression of PBMC proliferation in response to mitogen stimulation under both cell-cell contact and Transwell conditions, suggesting that IDO might play a major role in GMSC-mediated immunosuppression.
Generally, IDO is not constitutively expressed by mesenchymal stromal cells, but can be significantly induced by a variety of inflammatory mediators (30, 32, 71). Accumulating evidence has shown that IFN-γ plays a critical role in the cross-talk between MSCs and immune cells. Upon activation, immune cells secrete a high amount of inflammatory cytokines, especially IFN-γ, which may subsequently stimulate MSCs to express various immunosuppressive molecules, such as IDO, resulting in a negative feedback inhibition of inflammatory cell responses in terms of proliferation and cytokine secretion (11, 29, 31, 32). In agreement with previous reports (29, 30, 32, 70, 71), GMSCs do not constitutively express IDO, but in response to IFN-γ stimulation, harbored a significantly increased level of functional IDO. Coculture with GMSCs led to moderate suppression of mitogen-stimulated PBMC proliferation and IFN-γ secretion; however, the presence of stimulated PBMCs enhanced IL-10 secretion and IDO expression by GMSCs. Furthermore, the addition of IFN-γ-neutralizing Ab significantly blocked the secretion of IL-10 and the expression of functional IDO in GMSCs. These findings suggest that the up-regulated inflammatory signals dominated by IFN-γ in the coculture of GMSCs and stimulated PBMCs can induce GMSC-mediated immunosuppression, mediated in part, via the up-regulation of IL-10 and functional IDO expression. However, further studies are required to determine whether other inflammatory cytokines such as TNF-α and IL-1β are involved in priming GMSC-mediated immunosuppression.
Recently, several studies have reported that treatment with human bone marrow- or adipose-derived MSCs exhibits early efficacy in attenuating the progression of several experimental inflammatory diseases in murine models, including experimental arthritis (38), colitis (43, 46), and autoimmune encephalomyelitis (39). The apparent lack of graft rejection and positive treatment effects of human MSCs on these murine disease models could be due to their inherent capabilities to harness inflammatory cell infiltration, suppress inflammatory mediator production, and/or regulate immune tolerance by increasing the production of anti-inflammatory cytokines (e.g., IL-10) and inducing the generation/activation of Tregs (38, 39, 43, 46). Most recently, a study by Gonzalez et al. (38) suggested that the viability of human adipose-derived MSCs was not required for their long-term immunosuppressive activities since these cells were only detectable in the recipient for ~1 wk after injection. Similar to recent studies using hASCs to treat experimental colitis (43, 46), the present study has demonstrated that infusion of GMSCs could ameliorate the severity of inflammatory-related colonic tissue injuries in experimental colitis, possibly by reducing colonic infiltrates of inflammatory cells, down-regulating the production of inflammatory cytokines, and by promoting the generation/activation of Tregs. However, it remains unclear why infusion of human MSCs, including GMSCs, into immunocompetent mice in our murine models can attenuate disease progression in the absence of an apparent graft-versus- host disease response. Further studies are warranted to address this important issue.
Despite the potential benefits of MSCs in clinical applications, several questions remain unanswered, especially regarding the identity and biological properties of MSCs as compared with other stromal cells such as fibroblasts (72). Accumulating evidence has shown that MSCs share many common features with fibroblasts, including a spindle-like cell morphology, plastic adherence, expression profile of certain cell surface markers, multipotent differentiation, and even immunomodulatory functions (72-74). Previous analysis of human bone marrow MSC subclones revealed that the lineage commitment was hierarchical in nature (75) and may differ among MSC subpopulations derived from different tissues (75, 76). As such, the so-called fibroblast population may represent a more differentiated subpopulation of MSCs (22, 76). Up to date, there is still a lack of evidence whether such hierarchy exists in relevance to several biological functions, specifically the immunomodulatory properties of MSCs, and should be further addressed.
In conclusion, the unique immunomodulatory and anti-inflammatory properties of GMSCs as well as their ease of isolation, abundant tissue source, and rapid ex vivo expansion render these postnatal stem cells an ideal source for stem cell-based therapeutic approaches in clinical applications, including inflammatory diseases.
Supplementary Material
Footnotes
This work was supported in part by National Institutes of Health Research Grant R01DE 019932 (to A.D.L., Songtao Shi, and Y.S.), Oral and Maxillofacial Surgery Foundation Research Support Grant OMSF 002894 (to Q.Z.), the California Institute for Regenerative Medicine (RN1-00572 for Songtao Shi), and the University of Southern California institutional fundings, Clinical Translational Science Institute, and Zumberge (to A.D.L. and Songtao Shi).
- MSC
- mesenchymal stem cell
- GMSC
- gingiva-derived mesenchymal stem cell
- BMSC
- bone marrow-derived mesenchymal stem cell
- Oct-4
- octamer-4
- SSEA-4
- stage-specific embryonic Ag 4
- hTERT
- human reverse telomerase transcriptase
- DAPI
- 4′,6-diamidino-2-phenylindole
- LPL
- lipoprotein lipase
- PPARγ2
- peroxisome proliferator-activated receptor γ-2
- 1-MT
- 1-methyl-l-tryptophan
- iNOS
- inducible NO synthase
- l-NAME
- N-nitro-l-arginine methyl ester
- COX-2
- cyclooxygenase 2
- DSS
- dextran sulfate sodium
- IBD
- inflammatory bowel disease
- MPO
- myeloperoxidase
- DPSC
- dental pulp stem cell
- PDLSC
- periodontal ligament stem cell
- HGF
- hepatocyte growth factor
- CFU-F
- CFU fibroblast
- HA/TCP
- hydroxypatite/tricalcium phosphate
- GFAP
- glial fibrillary acidic protein
- Treg
- regulatory T cell
- hASC
- human adipose-derived stem cell
The online version of this article contains supplemental material.
Disclosures
The authors have no financial conflict of interest.
References
- 1.Prockop DJ. Marrow stromal cells as stem cells for nonhematopoietic tissues. Science. 1997;276:71–74. doi: 10.1126/science.276.5309.71. [DOI] [PubMed] [Google Scholar]
- 2.Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284:143–147. doi: 10.1126/science.284.5411.143. [DOI] [PubMed] [Google Scholar]
- 3.Friedenstein AJ, Chailakhjan RK, Lalykina KS. The development of fibroblast colonies in monolayer cultures of guinea-pig bone marrow and spleen cells. Cell Tissue Kinet. 1970;3:393–403. doi: 10.1111/j.1365-2184.1970.tb00347.x. [DOI] [PubMed] [Google Scholar]
- 4.Fernandes KJ, McKenzie IA, Mill P, Smith KM, Akhavan M, Barnabé-Heider F, Biernaskie J, Junek A, Kobayashi NR, Toma JG, et al. A dermal niche for multipotent adult skin-derived precursor cells. Nat. Cell Biol. 2004;6:1082–1093. doi: 10.1038/ncb1181. [DOI] [PubMed] [Google Scholar]
- 5.Toma JG, McKenzie IA, Bagli D, Miller FD. Isolation and characterization of multipotent skin-derived precursors from human skin. Stem Cells. 2005;23:727–737. doi: 10.1634/stemcells.2004-0134. [DOI] [PubMed] [Google Scholar]
- 6.Kim JM, Lee ST, Chu K, Jung KH, Song EC, Kim SJ, Sinn DI, Kim JH, Park DK, Kang KM, et al. Systemic transplantation of human adipose stem cells attenuated cerebral inflammation and degeneration in a hemorrhage stroke model. Brain Res. 2007;1183:43–50. doi: 10.1016/j.brainres.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 7.Bi YM, Ehirchiou D, Kilts TM, Inkson CA, Embree MC, Sonoyama W, Li L, Leet AI, Seo BM, Zhang L, et al. Identification of tendon stem/progenitor cells and the role of the extracellular matrix in their niche. Nat. Med. 2007;13:1219–1227. doi: 10.1038/nm1630. [DOI] [PubMed] [Google Scholar]
- 8.Beltrami AP, Cesselli D, Bergamin N, Marcon P, Rigo S, Puppato E, D’Aurizio F, Verardo R, Piazza S, Pignatelli A, et al. Multipotent cells can be generated in vitro from several adult human organs (heart, liver, and bone marrow) Blood. 2007;110:3438–3446. doi: 10.1182/blood-2006-11-055566. [DOI] [PubMed] [Google Scholar]
- 9.Chang CJ, Yen ML, Chen YC, Chien CC, Huang HI, Bai CH, Yen BL. Placenta-derived multipotent cells exhibit immunosuppressive properties that are enhanced in the presence of interferon-γ. Stem Cells. 2006;24:2466–2477. doi: 10.1634/stemcells.2006-0071. [DOI] [PubMed] [Google Scholar]
- 10.In’t Anker PS, Scherjon SA, Kleijiburg-van der Keur C, Noort WA, Claas FH, Willemze R, Fibbe WE, Kanhai HH. Amniotic fluid as a novel source of mesenchymal stem cells for therapeutic transplantation. Blood. 2003;102:1548–1549. doi: 10.1182/blood-2003-04-1291. [DOI] [PubMed] [Google Scholar]
- 11.Oh W, Kim DS, Yang YS, Lee JK. Immunological properties of umbilical cord blood-derived mesenchymal stromal cells. Cell Immunol. 2008;251:116–123. doi: 10.1016/j.cellimm.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 12.Morsczeck C, Schmalz G, Reichert TE, Völlner F, Galler K, Driemel O. Somatic stem cells for regenerative dentistry. Clin. Oral Invest. 2008;12:113–118. doi: 10.1007/s00784-007-0170-8. [DOI] [PubMed] [Google Scholar]
- 13.Gronthos S, Mankani M, Brahim J, Robey PG, Shi S. Postnatal human dental pulp stem cells (DPSCs) in vitro and in vivo. Proc. Natl. Acad. Sci. USA. 2000;97:13625–13630. doi: 10.1073/pnas.240309797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gronthos S, Brahim J, Li W, Fisher LW, Cherman N, Boyde A, DenBesten P, Robey PG, Shi S. Stem cell properties of human dental pulp stem cells. J. Dent. Res. 2002;81:531–535. doi: 10.1177/154405910208100806. [DOI] [PubMed] [Google Scholar]
- 15.Miura M, Gronthos S, Zhao M, Lu B, Fisher LW, Robey PG, Shi S. SHED: stem cells from human exfoliated deciduous teeth. Proc. Natl. Acad. Sci. USA. 2003;100:5807–5812. doi: 10.1073/pnas.0937635100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Seo BM, Miura M, Gronthos S, Bartold PM, Batouli S, Brahim J, Young M, Robey PG, Wang CY, Shi S. Investigation of multipotent postnatal stem cells from human periodontal ligament. Lancet. 2004;364:149–155. doi: 10.1016/S0140-6736(04)16627-0. [DOI] [PubMed] [Google Scholar]
- 17.Morsczeck C, Gotz W, Schierholz J, Zeilhofer F, Kühn U, Möhl C, Sippel C, Hoffmann KH. Isolation of precursor cells (PCs) from human dental follicle of wisdom teeth. Matrix Biol. 2005;24:155–165. doi: 10.1016/j.matbio.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 18.Lindroos B, Mäenpää K, Ylikomi T, Oja H, Suuronen R, Miettinen S. Characterisation of human dental stem cells and buccal mucosa fibroblasts. Biochem. Biophys. Res. Commun. 2009;368:329–335. doi: 10.1016/j.bbrc.2008.01.081. [DOI] [PubMed] [Google Scholar]
- 19.Jo YY, Lee HJ, Kook SY, Choung HW, Park JY, Chung JH, Choung YH, Kim ES, Yang HC, Choung PH. Isolation and characterization of postnatal stem cells from human dental tissues. Tissue Eng. 2007;13:767–773. doi: 10.1089/ten.2006.0192. [DOI] [PubMed] [Google Scholar]
- 20.Gang EJ, Bosnakovski D, Figueiredo CA, Visser JW, Perlingeiro RC. SSEA-4 identifies mesenchymal stem cells from bone marrow. Blood. 2007;109:1743–1751. doi: 10.1182/blood-2005-11-010504. [DOI] [PubMed] [Google Scholar]
- 21.Greco SJ, Liu K, Rameshwar P. Functional similarities among genes regulated by OCT4 in human mesenchymal and embryonic stem cells. Stem Cells. 2007;25:3143–3154. doi: 10.1634/stemcells.2007-0351. [DOI] [PubMed] [Google Scholar]
- 22.Covas DT, Panepucci RA, Fontes AM, Silva WA, Jr., Orellana MD, Freitas MC, Neder L, Santos AR, Peres LC, Jamur MC, Zago MA. Multipotent mesenchymal stromal cells obtained from diverse human tissues share functional properties and gene–expression profiles with CD146+ perivascular cells and fibroblasts. Exp. Hematol. 2008;36:642–654. doi: 10.1016/j.exphem.2007.12.015. [DOI] [PubMed] [Google Scholar]
- 23.Spaeth E, Klopp A, Dembinski J, Andreeff M, Marini F. Inflammation and tumor microenvironments: defining the migratory itinerary of mesenchymal stem cells. Gene Ther. 2008;15:730–738. doi: 10.1038/gt.2008.39. [DOI] [PubMed] [Google Scholar]
- 24.Karp JM, Leng Teo GS. Mesenchymal stem cell homing: the devil is in the details. Cell Stem Cell. 2009;4:206–216. doi: 10.1016/j.stem.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 25.Nauta AJ, Fibbe WE. Immunomodulatory properties of mesenchymal stromal cells. Blood. 2007;110:3499–3506. doi: 10.1182/blood-2007-02-069716. [DOI] [PubMed] [Google Scholar]
- 26.Abdallah BM, Kassem M. The use of mesenchymal (skeletal) stem cells for treatment of degenerative diseases: current status and future perspectives. J. Cell Physiol. 2009;218:9–12. doi: 10.1002/jcp.21572. [DOI] [PubMed] [Google Scholar]
- 27.Uccelli A, Moretta L, Pistoia V. Mesenchymal stem cells in health and disease. Nat. Rev. Immunol. 2008;8:726–736. doi: 10.1038/nri2395. [DOI] [PubMed] [Google Scholar]
- 28.Selmani Z, Naji A, Zidi I, Favier B, Gaiffe E, Obert L, Borg C, Saas P, Tiberghien P, Rouas-Freiss N, et al. Human leukocyte antigen-G5 secretion by human mesenchymal stem cells is required to suppress T lymphocyte and natural killer function and to induce CD4+CD25highFoxP3+ regulatory T cells. Stem Cells. 2008;26:212–222. doi: 10.1634/stemcells.2007-0554. [DOI] [PubMed] [Google Scholar]
- 29.Aggarwal S, Pittenger MF. Human mesenchymal stem cells modulate allogeneic immune cell responses. Blood. 2005;105:1815–1822. doi: 10.1182/blood-2004-04-1559. [DOI] [PubMed] [Google Scholar]
- 30.Ryan JM, Barry F, Murphy JM, Mahon BP. Interferon-γ does not break, but promotes the immunosuppressive capacity of adult human mesenchymal stem cells. Clin. Exp. Immunol. 2007;149:353–363. doi: 10.1111/j.1365-2249.2007.03422.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Krampera M, Cosmi L, Angeli R, Pasini A, Liotta F, Andreini A, Santarlasci V, Mazzinghi B, Pizzolo G, Vinante F, et al. Role for interferon-γ in the immunomodulatory activity of human bone marrow mesenchymal stem cells. Stem Cells. 2006;24:386–398. doi: 10.1634/stemcells.2005-0008. [DOI] [PubMed] [Google Scholar]
- 32.Delarosa O, Lombardo E, Beraza A, Mancheño P, Ramírez C, Menta R, Rico L, Camarillo E, García L, Abad JL, Trigueros C, Delgado M, Büscher D. Requirement of IFN-γ-mediated indoleamine 2,3-dioxygenase expression in the modulation of lymphocyte proliferation by human adipose-derived stem cells. Tissue Eng. Part A. 2009;15:2795–2806. doi: 10.1089/ten.TEA.2008.0630. [DOI] [PubMed] [Google Scholar]
- 33.Spaggiari GM, Capobianco A, Abdelrazik H, Becchetti F, Mingari MC, Moretta L. Mesenchymal stem cells inhibit natural killer-cell proliferation, cytotoxicity, and cytokine production: role of indoleamine 2,3-dioxygenase and prostaglandin E2. Blood. 2008;111:1327–1333. doi: 10.1182/blood-2007-02-074997. [DOI] [PubMed] [Google Scholar]
- 34.Sato K, Ozaki K, Oh I, Meguro A, Hatanaka K, Nagai T, Muroi K, Ozawa K. Nitric oxide plays a critical role in suppression of T-cell proliferation by mesenchymal stem cells. Blood. 2007;109:228–234. doi: 10.1182/blood-2006-02-002246. [DOI] [PubMed] [Google Scholar]
- 35.Polchert D, Sobinsky J, Douglas GW, Kidd M, Moadsiri A, Reina E, Genrich K, Mehrotra S, Setty S, Smith B, Bartholomew A. IFN-γ activation of mesenchymal stem cells for treatment and prevention of graft versus host disease. Eur. J. Immunol. 2008;38:1745–1755. doi: 10.1002/eji.200738129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Le Blanc K, Rasmusson I, Sundberg B, Götherström C, Hassan M, Uzunel M, Ringdén O. Treatment of severe acute graft-versus-host disease with third party haploidentical mesenchymal stem cells. Lancet. 2004;363:1439–1441. doi: 10.1016/S0140-6736(04)16104-7. [DOI] [PubMed] [Google Scholar]
- 37.Lee RH, Seo MJ, Reger RL, Spees JL, Pulin AA, Olson SD, Prockop DJ. Multipotent stromal cells from human marrow home to and promote repair of pancreatic islets and renal glomeruli in diabetic NOD/scid mice. Proc. Natl. Acad. Sci. USA. 2006;103:17438–17443. doi: 10.1073/pnas.0608249103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.González MA, Gonzalez-Rey E, Rico L, Büscher D, Delgado M. Treatment of experimental arthritis by inducing immune tolerance with human adipose-derived mesenchymal stem cells. Arthritis Rheum. 2009;60:1006–1019. doi: 10.1002/art.24405. [DOI] [PubMed] [Google Scholar]
- 39.Zhang J, Li Y, Chen J, Cui Y, Lu M, Elias SB, Mitchell JB, Hammill L, Vanguri P, Chopp M. Human bone marrow stromal cell treatment improves neurological functional recovery in EAE mice. Exp. Neurol. 2005;195:16–26. doi: 10.1016/j.expneurol.2005.03.018. [DOI] [PubMed] [Google Scholar]
- 40.Parekkadan B, Tilles AW, Yarmush ML. Bone marrow-derived mesenchymal stem cells ameliorate autoimmune enteropathy independent of regulatory T cells. Stem Cells. 2008;26:1913–1919. doi: 10.1634/stemcells.2007-0790. [DOI] [PubMed] [Google Scholar]
- 41.Zhou K, Zhang H, Jin O, Feng X, Yao G, Hou Y, Sun L. Transplantation of human bone marrow mesenchymal stem cell ameliorates the autoimmune pathogenesis in MRL/lpr mice. Cell Mol. Immunol. 2008;5:417–424. doi: 10.1038/cmi.2008.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu Y, Zheng Y, Ding G, Fang D, Zhang C, Bartold PM, Gronthos S, Shi S, Wang S. Periodontal ligament stem cell-mediated treatment for periodontitis in miniature swine. Stem Cells. 2008;26:1065–1073. doi: 10.1634/stemcells.2007-0734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.González MA, Gonzalez-Rey E, Rico L, Büscher D, Delgado M. Adipose-derived mesenchymal stem cells alleviate experimental colitis by inhibiting inflammatory and autoimmune responses. Gastroenterology. 2009;136:978–989. doi: 10.1053/j.gastro.2008.11.041. [DOI] [PubMed] [Google Scholar]
- 44.Németh K, Leelahavanichkul A, Yuen PS, Mayer B, Parmelee A, Doi K, Robey PG, Leelahavanichkul K, Koller BH, Brown JM, et al. Bone marrow stromal cells attenuate sepsis via prostaglandin E2-dependent reprogramming of host macrophages to increase their interleukin-10 production. Nat. Med. 2009;15:42–49. doi: 10.1038/nm.1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Iyer SS, Rojas M. Anti-inflammatory effects of mesenchymal stem cells: novel concept for future therapies. Exp. Opin. Biol. Ther. 2008;8:569–581. doi: 10.1517/14712598.8.5.569. [DOI] [PubMed] [Google Scholar]
- 46.Gonzalez-Rey E, Anderson P, González MA, Rico L, Büscher D, Delgado M. Human adult stem cells derived from adipose tissue protect against experimental colitis and sepsis. Gut. 2009;58:929–939. doi: 10.1136/gut.2008.168534. [DOI] [PubMed] [Google Scholar]
- 47.Irwin CR, Picardo M, Ellis I, Sloan P, Grey A, McGurk M, Schor SL. Inter- and intra-site heterogeneity in the expression of fetal-like phenotypic characteristics by gingival fibroblasts: potential significance for wound healing. J. Cell Sci. 1994;107:1333–1346. doi: 10.1242/jcs.107.5.1333. [DOI] [PubMed] [Google Scholar]
- 48.Stephens P, Davies KJ, Occleston N, Pleass RD, Kon C, Daniels J, Khaw PT, Thomas DW. Skin and oral fibroblasts exhibit phenotypic differences in extracellular matrix reorganization and matrix metalloproteinase activity. Br. J. Dermatol. 2001;144:229–237. doi: 10.1046/j.1365-2133.2001.04006.x. [DOI] [PubMed] [Google Scholar]
- 49.Novak N, Haberstock J, Bieber T, Allam JP. The immune privilege of the oral mucosa. Trends Mol. Med. 2008;14:191–198. doi: 10.1016/j.molmed.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 50.Jones PH, Watt FM. Separation of human epidermal stem cells from transit amplifying cells on the basis of differences in integrin function and expression. Cell. 1993;73:713–724. doi: 10.1016/0092-8674(93)90251-k. [DOI] [PubMed] [Google Scholar]
- 51.Podolsky DK. Inflammatory bowel disease. N. Engl. J. Med. 2002;347:417–429. doi: 10.1056/NEJMra020831. [DOI] [PubMed] [Google Scholar]
- 52.Xavier RJ, Podolsky DK. Unravelling the pathogenesis of inflammatory bowel disease. Nature. 2007;448:427–434. doi: 10.1038/nature06005. [DOI] [PubMed] [Google Scholar]
- 53.Mizoguchi A, Mizoguchi E. Inflammatory bowel disease, past, present and future: lessons from animal models. J. Gastroenterol. 2008;43:1–17. doi: 10.1007/s00535-007-2111-3. [DOI] [PubMed] [Google Scholar]
- 54.Alex P, Zachos NC, Nguyen T, Gonzales L, Chen TE, Conklin LS, Centola M, Li X. Distinct cytokine patterns identified from multiplex profiles of murine DSS and TNBS-induced colitis. Inflamm. Bowel Dis. 2009;15:341–352. doi: 10.1002/ibd.20753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shi S, Gronthos S, Chen S, Reddi A, Counter CM, Robey PG, Wang CY. Bone formation by human postnatal bone marrow stromal stem cells is enhanced by telomerase expression. Nat. Biotech. 2002;20:587–591. doi: 10.1038/nbt0602-587. [DOI] [PubMed] [Google Scholar]
- 56.Yamaza T, Miura Y, Bi Y, Liu YZ, Akiyama K, Sonoyama W, Patel V, Gutkind S, Young M, Gronthos S, Le A, Wang C-Y, Chen WJ, Shi S. Pharmacologic stem cell based intervention as a new approach to osteoporosis treatment in rodents. PLoS One. 2008;3:e2615. doi: 10.1371/journal.pone.0002615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bartsch G, Yoo JJ, De Coppi P, Siddiqui MM, Schuch G, Pohl HG, Fuhr J, Perin L, Soke S, Atala A. Propagation, expansion, and multilineage differentiation of human somatic stem cells from dermal progenitors. Stem Cell Dev. 2005;14:337–348. doi: 10.1089/scd.2005.14.337. [DOI] [PubMed] [Google Scholar]
- 58.You S, Moon JH, Kim TK, Kim SC, Kim JW, Yoon DH, Kwak S, Hong KC, Choi YJ, Kim H. Cellular characteristics of primary and immortal canine embryonic fibroblast cells. Exp. Mol. Med. 2004;36:325–335. doi: 10.1038/emm.2004.43. [DOI] [PubMed] [Google Scholar]
- 59.Gregory CA, Gunn WG, Peister A, Prockop DJ. An Alizarin Red-based assay of mineralization by adherent cells in culture: comparison with cetylpyridinium chloride extraction. Anal. Biochem. 2004;329:77–84. doi: 10.1016/j.ab.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 60.Yu W, Chen Z, Zhang J, Zhang L, Ke H, Huang L, Peng Y, Zhang X, Li S, Lahn BT, Xiang AP. Critical role of phosphoinositide 3-kinase cascade in adipogenesis of human mesenchymal stem cells. Mol. Cell Biochem. 2007;310:11–18. doi: 10.1007/s11010-007-9661-9. [DOI] [PubMed] [Google Scholar]
- 61.Tao H, Rao R, Ma D. Cytokine-induced stable neuronal differentiation of human bone marrow mesenchymal stem cells in a serum/feeder cell-free condition. Dev. Growth Differ. 2005;47:423–433. doi: 10.1111/j.1440-169X.2005.00810.x. [DOI] [PubMed] [Google Scholar]
- 62.Cipriani P, Guiducci S, Miniati I, Cinelli M, Urbani S, Marrelli A, Dolo V, Pavan A, Saccardi R, Tyndall A, et al. Impairment of endothelial cell differentiation from bone marrow-derived mesenchymal stem cells: new insight into the pathogenesis of systemic sclerosis. Arthritis Rheum. 2007;56:1994–2004. doi: 10.1002/art.22698. [DOI] [PubMed] [Google Scholar]
- 63.Morsczeck C, Schmalz G, Reichert TE, Völlner F, Galler K, Driemel O. Somatic stem cells for regenerative dentistry. Clin. Oral Invest. 2008;12:113–118. doi: 10.1007/s00784-007-0170-8. [DOI] [PubMed] [Google Scholar]
- 64.Cournil-Henrionnet C, Huselstein C, Wang Y, Galois L, Mainard D, Decot V, Netter P, Stoltz JF, Muller S, Gillet P, Watrin-Pinzano A. Phenotypic analysis of cell surface markers and gene expression of human mesenchymal stem cells and chondrocytes during monolayer expansion. Biorheology. 2008;45:513–526. [PubMed] [Google Scholar]
- 65.Lorenz K, Sicker M, Schmelzer EE, Rupf T, Salvetter J, Schulz-Siegmund M, Bader A. Multilineage differentiation potential of human dermal skin-derived fibroblasts. Exp. Dermatol. 2008;17:925–932. doi: 10.1111/j.1600-0625.2008.00724.x. [DOI] [PubMed] [Google Scholar]
- 66.Di Nicola M, Carlo-Stella C, Magni M, Milanesi M, Longoni PD, Matteucci P, Grisanti S, Gianni AM. Human bone marrow stromal cells suppress T-lymphocyte proliferation induced by cellular or nonspecific mitogenic stimuli. Blood. 2002;99:3838–3843. doi: 10.1182/blood.v99.10.3838. [DOI] [PubMed] [Google Scholar]
- 67.Cui L, Yin S, Liu W, Li N, Zhang W, Cao Y. Expanded adipose-derived stem cells suppress mixed lymphocyte reaction by secretion of prostaglandin E2. Tissue Eng. 2007;13:1185–1195. doi: 10.1089/ten.2006.0315. [DOI] [PubMed] [Google Scholar]
- 68.Wang M, Yang Y, Yang D, Luo F, Liang W, Guo S, Xu J. The immunomodulatory activity of human umbilical cord blood-derived mesenchymal stem cells in vitro. Immunology. 2009;126:220–232. doi: 10.1111/j.1365-2567.2008.02891.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sheng H, Wang Y, Jin Y, Zhang Q, Zhang Y, Wang L, Shen B, Yin S, Liu W, Cui L, Li N. A critical role of IFNγ in priming MSC-mediated suppression of T cell proliferation through up-regulation of B7–H1. Cell Res. 2008;18:846–857. doi: 10.1038/cr.2008.80. [DOI] [PubMed] [Google Scholar]
- 70.Wada N, Menicanin D, Shi S, Bartold PM, Gronthos S. Immunomodulatory properties of human periodontal ligament stem cells. J. Cell Physiol. 2009;219:667–676. doi: 10.1002/jcp.21710. [DOI] [PubMed] [Google Scholar]
- 71.Mahanonda R, Sa-Ard-Iam N, Montreekachon P, Pimkhaokham A, Yongvanichit K, Fukuda MM, Pichyangkul S. IL-8 and IDO expression by human gingival fibroblasts via TLRs. J. Immunol. 2007;178:1151–1157. doi: 10.4049/jimmunol.178.2.1151. [DOI] [PubMed] [Google Scholar]
- 72.Haniffa MA, Collin MP, Buckley CD, Dazzi F. Mesenchymal stem cells: the fibroblasts’ new clothes? Haematologica. 2009;94:258–263. doi: 10.3324/haematol.13699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lysy PA, Smets F, Sibille C, Najimi M, Sokal EM. Human skin fibroblasts: from mesodermal to hepatocyte-like differentiation. Hepatology. 2007;46:1574–1585. doi: 10.1002/hep.21839. [DOI] [PubMed] [Google Scholar]
- 74.Haniffa MA, Wang XN, Holtick U, Rae M, Isaacs JD, Dickinson AM, Hilkens CM, Collin MP. Adult human fibroblasts are potent immunoregulatory cells and functionally equivalent to mesenchymal stem cells. J. Immunol. 2007;179:1595–1604. doi: 10.4049/jimmunol.179.3.1595. [DOI] [PubMed] [Google Scholar]
- 75.Muraglia A, Cancedda R, Quarto R. Clonal mesenchymal progenitors from human bone marrow differentiate in vitro according to a hierarchical model. J. Cell Sci. 2000;113:1161–1166. doi: 10.1242/jcs.113.7.1161. [DOI] [PubMed] [Google Scholar]
- 76.Sudo K, Kanno M, Miharada K, Ogawa S, Hiroyama T, Saijo K, Nakamura Y. Mesenchymal progenitors able to differentiate into osteogenic, chondrogenic, and/or adipogenic cells in vitro are present in most primary fibroblast-like cell populations. Stem Cells. 2007;25:1610–1617. doi: 10.1634/stemcells.2006-0504. [DOI] [PubMed] [Google Scholar]
- 77.Zhang Q, Shi S, Liu Y, Uyanne J, Shi Y, Shi S, Le AD. Mesenchymal stem cells derived from human gingiva are capable of immunomodulatory functions and ameliorate inflammation-related tissue destruction in experimental colitis. J. Immunol. 2009;183:7787–7798. doi: 10.4049/jimmunol.0902318. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.