Abstract
Background
Qualitative research studies regarding physical activity in patients undergoing total joint arthroplasty (TJA) unfortunately are sparse in the current literature.
Questions/Purposes
To provide a foundation for future investigations, we performed a systematic review to identify the different instruments used to quantify physical activity in patients undergoing TJA and to determine how active these patients really are.
Methods
We systematically reviewed the literature on the bibliographic databases Medline, Cochrane Library, and EMBASE published until September 2008, focusing on studies assessing total physical activity in patients after or undergoing TJA. Results of those studies quantifying physical activity using accelerometers and pedometers were combined using meta-analytic methods.
Results
In the 26 studies included (n = 2460 patients), motion sensors and recall questionnaires were most commonly used. The research aims and goals varied widely among the studies and the results mainly were descriptive. Studies quantifying physical activity using pedometers and accelerometers suggested a weighted mean of 6721 steps/day (95% confidence interval [CI], 5744–7698). Steps per day determined by accelerometers were 2.2 times the steps measured by pedometers. Metaregression showed that walking activity decreased by 90 steps/day (95% CI, −156 to −23) every year of patient age.
Conclusions
These results suggest patients undergoing TJA are less active than recommended to achieve health-enhancing activity levels (greater than 10,000 steps/day), but they appear more active than normally assumed in typical wear simulations. Future investigations have to evolve more standardization in the assessment and reporting of physical activity in TJA patients.
Introduction
Physical inactivity is a modifiable lifestyle-related risk factor considered one of the leading causes for the major noncommunicable chronic diseases such as cardiovascular disease, diabetes mellitus, colon and breast cancers, obesity, hypertension, osteoporosis, and depression [43–45, 56, 71, 76, 77]. Approximately 250,000 deaths per year in the United States are associated with physical inactivity [7]. There is overwhelming evidence that regular physical activity reduces overall mortality and morbidity and the incidence of chronic diseases [11, 22, 43–45, 53, 65].
Recognizing the major role of physical activity in primary and secondary prevention, the main national and international organizations (World Health Organization, Centers for Disease Control and Prevention, American College of Sports Medicine, American Heart Association, National Institutes of Health) have proposed recommendations for health-enhancing physical activity [32, 57, 71]. Current recommendations suggest 30 minutes of moderate aerobic activities for 5 or more days per week or vigorous aerobic activities for 20 minutes at least 3 days per week [1, 2, 32, 57]. Although there are numerous modes of aerobic physical activity in which individuals can engage [9, 10], walking is the most widely performed aerobic activity in the United States [31, 71]. With the advent of pedometers, it also has become economically and technically feasible to accurately assess physical activity, quantified as steps taken per day [68–70]. A value of 10,000 steps/day currently is promoted as a target for obtaining health benefits [37, 61, 69].
Facing the older population with osteoarthritis and treated by total joint arthroplasty (TJA), there is evidence that aging individuals are less physically active than younger individuals and that physical performance and cardiovascular capacity decline with increasing age, which also might result in increased mortality [12, 24, 49, 58, 78, 79]. Greater than 46% of older Americans can be classified as inactive [39] and greater than 60% of adults with arthritis do not meet physical activity recommendations [26]. Therefore, considering the evident health benefits of physical activity, a successful surgical procedure such as TJA should not only improve pain and function, but also allow patients to be physically active, preferably as active as needed to meet recommended activity levels. However, physical activity is not unrestrictedly warranted in these patients, taking the increased risk of wear production and implant loosening into account that might accompany increased activity levels. Qualitative research defining the type and amount of physical activity in patients undergoing TJA that improves health without disproportionally increasing wear and revision rates unfortunately does not exist in the literature. Although such evidence would be the most desirable result of any future research efforts, the determination of the current state of physical activity research in patients undergoing TJA regarding quality (how is it assessed?) and quantity (how much is performed?) represents the cornerstone for future investigations.
Our systematic review therefore addressed the following questions: (1) How is total physical activity quantified in patients undergoing arthroplasty? (2) How active are patients undergoing TJA?
Materials and Methods
We identified relevant publications (ie, studies related to physical activity in patients undergoing TJA) using a computer-aided search by the two authors (FDN, FMI). We systematically reviewed the literature on the bibliographic databases Medline (through PubMed), Cochrane Library, and EMBASE published until September 2008 using the following combinations of search terms: “physical activity” OR “activity levels” OR “habitual activity” OR “health enhancing activity” OR “pedometer” OR “accelerometer AND “arthroplasty” OR “joint replacement” OR “knee prosthesis” OR “hip prosthesis.” This search strategy yielded 1688 citations. To identify additional articles, the bibliographies of recent review articles were searched for any additional relevant works. We then screened all articles according to a recommended protocol [82]. For the current review, we focused on studies conducted on patients after THA or TKA or patients with osteoarthritis undergoing joint arthroplasty. Accordingly, we defined three initial inclusion criteria: (1) the article referred to patients with hip or knee osteoarthritis and scheduled for joint arthroplasty or to patients with hip or knee arthroplasties; (2) the study evaluated habitual physical activity levels or the total amount of physical activity; and (3) the article was published in English, German, French, or Italian. Exclusion criteria were as follows: (1) the study assessed physical activity by simple rating scales or by not validated qualitative or relative questions (eg, “how would you rate your level of physical activity compared with preoperatively?”); (2) the study used only physical performance tests (eg, get-up-and-go test) or determined parameters of gait; and (3) the article was published in another language than one of those previously mentioned.
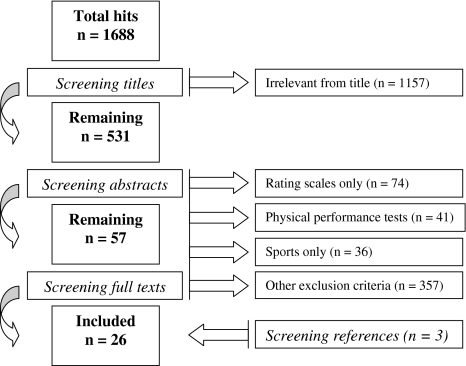
Of the 1688 identified citations, we excluded 1631 articles using the above criteria after screening titles and abstracts. The full texts of the remaining 57 articles were retrieved and further analyzed. After analyzing these full texts and screening recent review articles (Fig. 1), 26 separately published articles comprising 2460 patients met the inclusion and exclusion criteria (25 were in English, one in German) and were included in this review (Table 1) [3, 4, 8, 13, 16, 17, 23, 28, 29, 34, 35, 38, 47, 51, 54, 59, 60, 62–64, 72–75, 81, 84].
Fig. 1.
Of the 1688 identified citations, 26 separately published articles comprising 2460 patients met the inclusion and exclusion criteria (25 were in English, one was in German).
Table 1.
Descriptive results of the 26 included studies
| Study and location | Study aim | Subjects | Instruments/sampling time | Time from surgery | Main physical activity outcome |
|---|---|---|---|---|---|
| Bennett et al. [4], 2008* Northern Ireland |
To investigate wear paths and wear rates related to activity | N = 97, age 70.2 (SD 7.5) years 60% M, 40% F (THA) |
Pedometer (FitPro; Yamax, Tokyo, Japan) 14 days | 9.8 (range, 8.6–11.4) years | 4173 (SD 2329) steps/day |
| Bennett et al. [3], 2008* Northern Ireland |
To investigate the relation between walking activity and wear 10 years after THA | N = 26, age 70.9 (SD 2.9) years 50% M, 50% F (THA) N = 18, age 67.8 (SD 1.4) years 44% M, 56% F (THA) N = 29, age 72.5 (SD 1.5) years 72% M, 28% F (THA) N = 20, age 76.7 (SD 1.4) years 55% M, 45% F (THA) N = 7, age 82.9 (SD 2.1) years 43% M, 57% F (THA) |
Pedometer (FitPro) 14 days | 9.8 (SD 0.3) years 9.8 (SD 0.3) years 9.9 (SD 0.4) years 9.9 (SD 0.3) years 9.9 (SD 0.2) years |
4873 (SD 2810) steps/day 4892 (SD 3037) steps/day 3440 (SD 2023) steps/day 3428 (SD 1604) steps/day 2213 (SD 777) steps/day |
| Brandes et al. [8], 2008 Germany |
To assess the relation between quality of life and quality and quantity of gait parameters | N = 26, age 58.6 (SD 13.4) years BMI 27.6; 35% M, 65% F (KOA, HOA) |
Accelerometer (StepWatch Activity Monitor; Cyma Inc, Seattle, WA) 7 days Accelerometer (DynaPort; McRoberts, The Hague, The Netherlands) 1 day |
Preoperative | 9564 (SD 4232) steps/day 10.5% locomotion, 32.6% standing, 43.9% sitting, 12.5% lying |
| Cukras et al. [13], 2007 Poland |
To determine PA in patients undergoing THA compared with control subjects | N = 69, age 70.4 (SD 7.8) years 41% M, 59% F (THA) |
Questionnaire (PAR) | 27 months | F: 267.6 (SD 43.7) kcal/kg/week (total EE) M: 257.6 (SD 36.1) kcal/kg/week (total EE) |
| deGroot et al. [16], 2008 The Netherlands |
To determine actual PA in patients with osteoarthritis compared with control subjects | N = 36. age 61.5 (SD 12.8) years BMI 26.6; 46% M, 54% F (HOA/THA) N = 44, age 62.1 (SD 9.7) years BMI 32.1; 36% M, 64% F (KOA/TKA) |
Accelerometer (Activity Monitor; Temec Instr, Kerkrade, The Netherlands) 2 days Questionnaire (PASIPD) |
Preoperative, 3 and 6 months | Walking, cycling, and general movement in THA: 125 (SD 58) minutes/day (preoperative) 131 (SD 56) minutes/day (3 months) 132 (SD 53) minutes/day (6 months) Walking, cycling, and general movement in TKA: 117 (SD 55) minutes/day (preoperative) 129 (SD 59) minutes/day (3 months) 131 (SD 53) minutes/day (6 months) |
| deGroot et al. [17], 2008 The Netherlands |
To determine actual PA in patients with end-stage osteoarthritis compared with control subjects | N = 40, age 61.4 (SD 12.2) years BMI 26.6; 40% M, 60% F (HOA) N = 44, age 62.1 (SD 9.9) years BMI 32.1; 46% M, 54% F (KOA) |
Accelerometer (Activity Monitor) 2 days | Preoperative | Walking, cycling, and general movement in HOA: 127 (SD 60) minutes/day Walking, cycling, and general movement in KOA: 117 (SD 58) minutes/day |
| Feller et al. [23], 1994 United Kingdom |
To investigate the effect of PA on wear production | N = 79, age 56 (range, 20–75) years BMI 26.1; 40% M, 60% F (THA) |
Questionnaire (Activity questionnaire) | 10.3 (range, 8.3–16.3) years | 20,638 (R 984 to 67,408) meter/y (sliding distance) |
| Goldsmith et al. [29], 2001 United Kingdom |
To compare walking activity between THA and control subjects | N = 63, age 58.4 (range, 20–75) years 52% M, 48% F (THA) |
Pedometer (not specified) 14–28 days | 14.2 (range, 0.9–26.4) years | Steps = 12,863 – 89.4 x age (THA) |
| Goldsmith et al. [28], 2001 United Kingdom |
To investigate the relation between PA and cup penetration after THA | N = 54, age 57.7 (range, 17–73) years 46%F, 54% M (THA) |
Pedometer (not specified) | 13.1 (range, 1.3–26.4) years | 7815 (range, 1000–24,579) steps/day |
| Heisel et al. [34], 2004 California |
To determine the short-term in vivo wear of a moderately cross-linked polyethylene | N = 24, age 74 (SD 9.9) years BMI 27.3; 46% M, 54% F (THA-Enduron; DePuy) N = 34, age 60 (SD 14) years BMI 30.9; 32% M, 68% F (THA-Marathon; DePuy) |
Accelerometer (StepWatch Activity Monitor) | 23 months (Enduron) 33 months (Marathon) |
10,740 (SD 4602) steps/day (Enduron) 10,795 (SD 6575) steps/day (Marathon) |
| Heisel et al. [35], 2008 Germany |
To investigate running-in (ion concentrations) of metal-on-metal implants | N = 15, age 51 (range, 31–61) years BMI 28; 47% M, 53% F (THA) |
Accelerometer (not specified, probably StepWatch Activity Monitor) 10–14 days | 1 year | 11,945 (range, 5534–17,589) steps/day |
| Jones et al. [38], 2004 Pennsylvania |
To investigate if PA is a risk factor for THA revision | N = 52 (2 × 26), age 70.5 (SD 8.9) years BMI 30.3; 35% M, 65% F (TKA/TKA revision) |
Questionnaires (MAQ, Yale) | 6.4 years | 3792 (SD 3552) MET/minute/week (total historical EE) (TKA) 3048 (SD 2076) MET/minute/week (total historical EE) (TKA revision) |
| McClung et al. [47], 2000 California |
To investigate the relation between PA and BMI in patients undergoing TJA | N = 127, age 57.7 (SD 13.3) years BMI 25.7; 58% M, 42% F (THA) N = 24, age 62.1 (SD 11.8) years BMI 29.3; 33% M, 67% F (TKA) |
Pedometer (not specified, probably Sportline, Yonkers, NY) 7 days | Not specified | 5869 (SD 3564) steps/day (THA) 4597 (SD 2889) steps/day (TKA) |
| Naal et al. [51], 2009 Switzerland |
To assess the validity of different activity rating scales | N = 105, age 63.4 (SD 11.0) years BMI 26.3; 54% M, 46% F (HOA) N = 100, age 66.5 (SD 9.1) years BMI 28.1; 39% M, 61% F (KOA) |
Questionnaire (IPAQ) | Preoperative | 3690 (SD 5,68) MET/minute/week (HOA) 4623 (SD 6508) MET/minute/week (KOA) |
| Ono et al. [54], 2007 Japan |
To assess the reliability and validity of the Baecke Activity Questionnaire | N = 61, age 53.3 (SD 11.3) years BMI 22 (HOA) |
Accelerometer/Pedometer (Lifecorder; Suzuken Co, Nagoya, Japan) 3–7 days Questionnaire (Baecke) |
Preoperative | 6309 (SD 2392) steps/day |
| Schmalzried et al. [60], 1998 California |
To quantify walking activity in patients undergoing TJA | N = 111, age 59 (range, 23–82) years 51% M, 49% F (TJA) |
Pedometer (Sportline) 15 days | > 6 months | 4988 (SD 3040) steps/s |
| Schmalzried et al. [59], 2000 California |
To investigate the association between activity and wear | N = 31, age 72 (range, 46–85) years BMI 27.5; 45% M, 55% F (THA) |
Pedometer (Sportline) Accelerometer (StepWatch Activity Monitor) |
4.5 (range, 3–6.2) years | 6795 (SD 3762) steps/day (pedometer) 10,550 (SD 4416) steps/day (accelerometer) |
| Sechriest et al. [62], 2007* Minnesota |
To investigate the association between activity and wear | N = 34, age 50.3 (SD 6.5) years BMI 29.1; 50% M, 50% F (THA) |
Pedometer (Sportline) | 6.3 (SD 1.2) years | 6575 (SD 2192) steps/day |
| Silva et al. [64], 2002 California |
To compare pedometers and accelerometers in patients undergoing THA | N = 33, age 71.5 (SD 9.7) years BMI 27.5; 42% M, 58% F (THA) |
Pedometer (Sportline) 4 days Accelerometer (StepWatch Activity Monitor) 4 days |
> 2 years | 6878 (SD 3736) steps/day (pedometer) 10,438 (SD 4388) steps/day (accelerometer) |
| Silva et al. [63], 2005 California |
To compare 4-day and 7-day durations of pedometer sampling | N = 131, age 57.6 (SD 12.8) years 56% M, 44% F (TJA) |
Pedometer (Sportline) 7–123 days | > 4 months | 5737 (SD 1650) steps/day |
| Wagenmakers et al. [73], 2008 The Netherlands |
To assess habitual PA and compare with normative data | N = 273, age 62.7 (SD 13.7) years 39% M, 61% F (THA) |
Questionnaire (SQUASH) | > 39 (range, 17–78) months | 1003 minutes/week (light activity) 381 minutes/week (moderate activity) 218 minutes/week (vigorous activity) |
| Wagenmakers et al. [72], 2008 The Netherlands |
To investigate if the WOMAC can predict the amount of PA after THA | N = 364, age 64.4 (SD 13.7) years 38% M, 62% F (THA) |
Questionnaire (SQUASH) | > 1 year | 948 minutes/week (light activity) 341 minutes/week (moderate activity) 210 minutes/week (vigorous activity) |
| Walker et al. [74], 2002 United Kingdom |
To quantify the increase in ambulation after TKA | N = 19, age 69 years 47% M, 53% F (TKA) |
Accelerometer (Numact Activity Monitor; Newcastle University, Newcastle, UK) 1 day | Preoperative, 3 and 6 months | 10,738 steps/day 12,358 steps/day 15,641 steps/day |
| Wallbridge & Dowson [75], 1982 United Kingdom |
To assess the number of steps in patients undergoing TJA | N = 10, age 65.4 (SD 11) years (TJA) | Pedometer (not specified) | 3–5 years | 7950 (SD 1957) steps/day |
| Wollmerstedt et al. [81], 2006* Germany |
To develop and validate a PA questionnaire | N = 75, age 70 (SD 7) years 48% M, 52% F (THA) N = 59, age 58 (SD 9) years 50% M, 50% F (THA) N = 26, age 64 (SD 8) years 50% M, 50% F (HOA) |
Accelerometer (StepWatch Activity Monitor) Questionnaires (TWB, FFKA) |
10 years 5 years Preoperative |
10,420 (SD 1957) steps/day (10 years) 13,108 (SD 4824) steps/day (5 years) 9934 (SD 4308) steps/day (preoperative) |
| Zahiri et al. [84], 1998 California |
To validate the UCLA activity scale | N = 100, age 58.6 (R 23 to 82) years (THA) | Pedometer (Sportline) | > 6 months | 5,78 (range, 395–17,718) steps/day |
* Additional information supplied by the authors. Data reported in the original studies as number of cycles/year were transformed in steps/day; PA = physical activity; TJA = total joint arthroplasty (THA, TKA); HOA = hip osteoarthritis; KOA = knee osteoarthritis; BMI = body mass index (kg/m2); F = female; M = male; PAR = Physical Activity Recall; PASIPD = Physical Activity Scale for Individuals with Physical Disabilities; MAQ = Modifiable Activity Questionnaire; IPAQ = International Physical Activity Questionnaire; SQUASH = Short Questionnaire to Assess Health-Enhancing Physical Activity; TWB = Täglicher Würzburger Bewegungsaktivitätsfragebogen; FFKA = Freiburger Fragebogen zur körperlichen Aktivitiät; Yale = Yale Physical Activity Survey; EE = energy expenditure.
Both authors then independently abstracted the following data for each study: study location, study aim, subject characteristics (age, gender, body mass index), instrument (type, model, sampling duration), type of surgery (hip or knee), time to followup, and main physical activity outcome (Table 1). Consensus between both authors was achieved afterwards by discussing and resolving any discrepancies. When physical activity was measured with accelerometers, we converted the data from cycles to steps. For retrieving additional data not reported in the articles (sampling time, proportion of males and females, body mass index [BMI], standard deviations, and so on), the authors of the studies were contacted by e-mail or phone.
After data extraction, combining the results of the studies quantifying physical activity using accelerometers and pedometers seemed possible by using meta-analytic methods. To allow meta-analytic methods, the mean and standard deviation (or variance) of any measurement must be provided; reporting of patient demographics (ie, age, gender distribution, weight, height, BMI) and details on other variables of interest (eg, sampling time) are required for additional subgroup analyses. To obtain an overall weighted mean and the relative 95% confidence interval of the variable of interest, two methods can be used: fixed- and random-effect models [14, 15, 19–21, 80]. Not all the studies reported the variance or standard deviation. In those cases (ie, in which the standard deviation or variance was not reported or supplied by the authors), the standard deviation was estimated from the range value if available [36]. Both methods are intended to assign more weight to studies containing more information (eg, with larger sample size, higher quality of research designs). Fixed-effect models assume each study estimates the same true population value and, therefore, that the only source of error is the random error in the study [80]. To test this assumption, we checked homogeneity using Q statistics (ie, to examine if differences in studies are explained by sampling variation only). The Q statistics were significant (p < 0.0001) in all group and subgroup analyses, indicating a high degree of heterogeneity. To synthesize the results of the different studies and perform sensitivity analysis, we therefore used a random-effect model. This model assumes there is a distribution of population values and generates weighted means taking into account within- and between-study differences. Sensitivity analysis was performed stratifying data according to the instruments used for assessing physical activity (accelerometer versus pedometer). Other subgroup analyses were possible only for studies that used pedometers. Therefore, we divided and analyzed the pedometer data classifying them according to age categories (younger than 65 years versus 65 years or older) and time from joint arthroplasty (less than 5 years versus 5 years or longer). Although we attempted to retrieve additional data by contacting the authors of the studies, we were not able to retrieve enough data to do further analyses (eg, relation between physical activity and BMI). For the studies measuring physical activity using questionnaires, there were not enough data for meta-analysis and therefore no attempt for synthesizing these results was made. Data from these studies were presented and interpreted qualitatively. All statistical procedures were performed using the Comprehensive Meta-Analysis computer program (Version 2; Biostat, Englewood, NJ).
Results
The most common methods identified for quantifying physical activity in patients undergoing TJA were motion sensors (accelerometers and pedometers) and recall questionnaires. Ten studies assessed physical activity using pedometers [3, 4, 28, 29, 47, 60, 62, 63, 75, 84], six used accelerometers [8, 17, 34, 35, 74, 81], two used accelerometers and pedometers [59, 64], six used questionnaires [13, 23, 38, 51, 72, 73], two studies used accelerometers and questionnaires [16, 81], and one study used pedometers and questionnaires [54]. No study used one of the gold standard methods for assessment of total physical activity, ie, oxygen uptake or doubly labeled water. Several studies also determined activity levels using activity rating scales (eg, UCLA scale) or they assessed patient-reported outcomes using traditional measures (eg, WOMAC). Among the 26 included studies, physical activity mainly was assessed descriptively and the research goals were widespread and unfocused (Table 1).
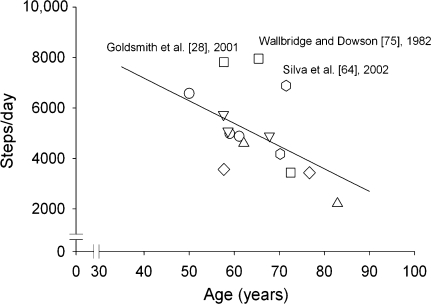
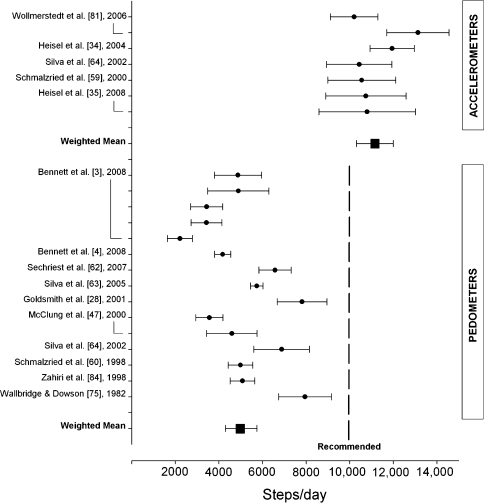
Meta-analysis was used for the studies that used accelerometers and pedometers. For group and subgroup analyses, Q tests showed a high degree of heterogeneity (p < 0.0001). The weighted mean of all studies quantifying physical activity using pedometers and accelerometers was 6721 (95% confidence interval [CI], 5744–7698; z = 13.477; p < 0.0001; n = 1169) steps/day. Subgroup analysis showed that steps assessed using accelerometers were 2.2 times the steps measured using pedometers (Table 2). Considering pedometer studies only, patients assessed less than 5 years after surgery took more steps/day than those assessed 5 or more years after surgery (6032 to 4251). Metaregression showed a relation (unrestricted maximum likelihood method; Q = 6.918, p = 0.008) between age and steps/day with physical activity decreasing by 90 steps/day (95% CI, −156 to −23) every year of age (Fig. 2). To better compare the number of steps/day of healthy people with those of patients undergoing TJA, we performed an additional subgroup analysis categorizing the studies in two age groups (younger than 65 years and 65 years or older) as reported by Bohannon in a recent meta-analysis on physical activity in adults [6].
Table 2.
Subgroup analysis of studies quantifying physical activity by pedometers or accelerometers
| Subgroup with number of studies | Number* | Mean | Standard error | Lower limit | Upper limit | Z-value | p Value |
|---|---|---|---|---|---|---|---|
| Measurement instrument | |||||||
| Pedometer (n = 10) | 877 | 5023 | 366 | 4305 | 5741 | 13.71 | < 0.001 |
| Accelerometer (n = 5) | 292 | 11,250 | 490 | 10,290 | 12,210 | 22.96 | < 0.001 |
| Age (studies using pedometers) | |||||||
| ≥ 65 years (n = 7)* | 270 | 4614 | 590 | 3457 | 5771 | 7.82 | < 0.001 |
| < 65 years (n = 8)* | 607 | 5372 | 370 | 4647 | 6098 | 14.51 | < 0.001 |
| Time to followup (studies using pedometers) | |||||||
| ≥ 5 years (n = 9)* | 458 | 4251 | 420 | 3427 | 5074 | 10.11 | < 0.001 |
| < 5 years (n = 6) | 419 | 6032 | 338 | 5369 | 6695 | 17.83 | < 0.001 |
* Number includes different age groups in the same study.
Fig. 2.
Metaregression showed walking activity decreased by 90 steps/day (95% confidence interval, −156 to −23) for every year of patient age.
The source of heterogeneity could not be identified with the sensitivity analysis. The latter was limited to few parameters because not enough data and studies were available, eg, we were not able to examine the relation between physical activity and BMI.
Discussion
Considering the evident health benefits of physical activity, a successful surgical procedure such as TJA should not only improve pain and function, but also allow patients to be physically active, preferably as active as needed to meet recommended health-enhancing activity levels. However, with increased physical activity levels in patients undergoing TJA, the production of wear and the risk of an early implant failure also might increase. Several published studies reported on the participation in sports and recreational activities after different joint arthroplasty interventions [33, 50–52, 83], but these studies do not allow for valid conclusions regarding health benefits, total physical activity levels, and the association between activity and wear or implant failure. Published qualitative research defining the type and amount of physical activity in these patients that improves health without disproportionally increasing wear and revision rates unfortunately does not exist. Consequently, the determination of the current state of physical activity research in patients undergoing TJA regarding quality (how is it assessed?) and quantity (how much is performed?) represents the cornerstone for future investigations. This systematic review therefore addressed the following questions: (1) How is total physical activity quantified in patients undergoing arthroplasty? (2) How active are patients undergoing TJA?
Before interpreting the current results, some limitations must be considered. The main limitation is related to the heterogeneity of the data so that the meta-analytic results have to be construed with some caution. Also, not all information required for an additional meta-analytic data interpretation (eg, sampling time, proportion of males and females, BMI or weights and heights, standard deviations, ranges, and so on) was reported in the studies and was not supplied by authors we contacted by e-mail or phone. Second, we did not screen all available databases, therefore some articles that would have met the inclusion and exclusion criteria might have been missed. We decided to focus on physical activity related to health enhancement because this issue is underrepresented in the orthopaedic literature despite the fact that people are aging, and today’s lifestyle factors increase the prevalence of cardiovascular disease and associated risk factors such as hypertension, diabetes, and obesity. We did not systematically review the topic of wear rates or implant loosening related to physical activity in this study. Such an investigation would be of great importance in patients undergoing TJA considering that physical activity levels required to obtain health benefits should not substantially compromise the implant durability. Our results nevertheless showed that the literature examining physical activity in patients undergoing TJA is very heterogeneous in terms of instruments and methodology used. Therefore, such an investigation seems to require additional quality investigations before being able to draw valid conclusions.
Several methods can be used for direct or indirect measurement of physical activity (oxygen uptake, heart rate, body temperature, doubly labeled water, motion sensors, physical activity records and questionnaires, and so on) [40]. Simple rating scales such as the UCLA, Tegner, or Devane scales provide an approximate overview over current and past activity levels, but they are only qualitative and we believe should not be used to make judgments regarding means to enhance health [51]. For this reason, we excluded studies that only used such rating scales. The most common methods for quantifying total physical activity in TJA currently are motion sensors (accelerometers and pedometers) and recall questionnaires. Our analysis, however, showed steps measured by pedometers were less than half the steps measured by accelerometers. Although there is a report indicating that pedometers record approximately 2000 steps/day less than accelerometers [68], the discrepancy we found is remarkable. An obvious difference between both types of motion sensors was reported by Silva et al. [63]; however, excluding that study from our meta-analysis, the differences remain similar (4904 versus 11,408 steps/day). The reason for this large discrepancy may be related to various factors that have influence on motion sensor readings such as walking velocity, altered gait biomechanics, and the amount of soft tissues [68]. Patients undergoing TJA may have altered gait biomechanics [46, 66], may walk at a slower speed than healthy subjects [46], and are more likely to be overweight or obese (BMI 25–31 kg/m2 in the current study). In addition, not all pedometer models have the same accuracy, particularly at slower walking speeds (less than 60 m/minute) [41, 42]. The pedometer model most often used in the studies reviewed was the Sportline (Yonkers, NY). Two models of the Sportline pedometer (Models 330 and 345) underestimate steps taken in the range of 20% to 40% compared with actual steps measured on a motorized treadmill at a walking speed of 54 m/minute [42]. Furthermore, pedometers usually start recording after four consecutive steps. In healthy people, Orendurff et al. [55] showed the most common walking period is 4 ± 1 steps (17% of total step counts). No studies have examined this in clinical populations, but it is possible that this observation is even more evident in patients undergoing TJA (ie, high frequency of periods of short walking). Underestimation of the slower and short periods of walking is not a concern when examining physical activity from a health-enhancing perspective, because for health enhancement, periods of 10 minutes are considered necessary. On the contrary, this is a problem when step counts are used in studies examining the relation between wear and physical activity where any and every step counts. Overall, the aforementioned factors may at least partly explain the difference between pedometers and accelerometers. Another reason could be related to the heterogeneity of the data, therefore, the differences between pedometer and accelerometer readings might not be as large as found here. Nevertheless, based on the aforementioned considerations and also taking biasing effects of the data heterogeneity into account, accelerometers appear to be the more appropriate instruments to objectively assess physical activity in individuals undergoing TJA. Furthermore, contrary to pedometers, accelerometers can give an estimation of the activity intensity, which is an important factor in fitness and wear production or implant loosening contexts. Wear production and implant loosening are not simply correlated with walking cycles, but also are dependent on body weight, muscle balancing, performed activities with shear and shock forces, and the intensity exerted during these activities [18].
However, pedometers and accelerometers may be unsuitable instruments for routine clinical practice considering their costs (especially for accelerometers) and burden (various visits for data downloading). For this reason, for routine assessment of physical activity in view of health enhancement and of potential adverse effects on replaced joints, recall questionnaires potentially are more useful instruments. Despite the inordinate number of habitual physical activity questionnaires that have been developed and described in the literature, only a few such measures have been used in patients undergoing TJA, and to our knowledge, none of these questionnaires has yet been criterion validated in this group of patients. A prerequisite for recommendation of any habitual physical activity questionnaire for routine use would be that it reports results in internationally comparable values such as the metabolic equivalent of task (MET) in addition to a criterion validation in the target patient group. Therefore, there is much room for future research of physical activity in patients undergoing TJA, for which we propose several important aspects concerning standardization and reporting that should be considered (Appendix).
Appendix.
Suggestions for future research projects and proposal regarding how data should be assessed and reported
| Investigation | Reason | How to assess | How to report |
|---|---|---|---|
| Compare pedometer and accelerometer readings in patients undergoing TJA | To prove that accelerometers may be more accurate because they assess each step taken and allow calculation of intensity | Data sampling with pedometers and accelerometers in the same patient; comparison with actual steps taken; tests at different walking speeds | Steps/day Sampling time Separately for patients undergoing THA and those undergoing TKA Numbers of females and males, age, weight, and height Mean, SD, and range for each subgroup |
| Compare the accuracy of different pedometer and accelerometer models in patients undergoing TJA | Large differences between models have been shown before; to determine the most appropriate models for patients undergoing TJA | Data sampling with pedometers and accelerometers in the same patient; comparison with actual steps taken; tests at different walking speeds | Steps/day Sampling time Separately for patients undergoing THA and those undergoing TKA Numbers of females and males, age, weight, and height Mean, SD, and range for each subgroup |
| Identification of potentially useful habitual physical activity questionnaires for patients undergoing TJA | Administration of questionnaires is more feasible in the daily routine; they may allow for additional assessment of activities not suited for pedometer or accelerometer use (eg, swimming) | Literature review of habitual physical activity questionnaires | Suitable questionnaires should allow quantification of physical activity in internationally comparable units such as kcal or METs They also should allow calculating the proportion of patients meeting or not meeting current physical activity recommendations |
| Assessment of usefulness of different habitual physical activity measures in patients undergoing TJA; criterion validation in the target group | Questionnaires differ in length and administrative burden; under- or overreporting might be present; criterion validation in the target group (ie, patients undergoing TJA) is necessary to prove that any questionnaire really measures what it intends to measure | Administration of different questionnaires together with traditionally used outcome measures such as the WOMAC or Oxford scores; calculation of response rates and assessment of patient judging; correlation with objective measures such as doubly labeled water, oxygen uptake, or accelerometers | Sampling time Separately for patients undergoing THA and those undergoing TKA Numbers of females and males, age, weight, and height Mean, SD, and range for each subgroup Questionnaire results in kcal or METs Proportion of patients meeting current physical activity recommendations Correlation coefficients between questionnaires and objective measures |
TJA = total joint arthroplasty; kcal = kilocalories; MET = metabolic equivalent of task (1 MET corresponds to the energy expenditure of sitting quietly for 1 minute; 3.5 mL O2).
Among the 26 studies included in this review, the research goals for the physical activity assessment were widespread and unfocused. Most studies reported their data more or less descriptively and the importance of physical activity for health maintenance or enhancement has been mostly neglected. Only two reports accounted habitual physical activity from a health perspective [51, 73]. Although we identified eight studies that tried to find associations between physical activity and wear rate or implant failure, the methods used in these studies varied considerably, prohibiting any attempt to summarize the data. The different modalities and often insufficient methods used to quantify physical activity in patients undergoing TJA may be the main reason for the discordance in the literature regarding the association of physical activity and wear or implant failure. Schmalzried et al., for example, highlighted that wear is a function of use, not time [59]. Sechriest et al., in contrast, found no correlation between linear wear rates and physical activity assessed by pedometers and the UCLA activity scale [62]. In a large patient sample (n = 1535), Flugsrud et al. found that male patients with intermediate to intense physical activity during leisure time had a fourfold increased risk of aseptic cup loosening after THA compared with their sedentary counterparts [25]. On the contrary, Gschwend and associates observed lower revision rates in patients active in sports 5 to 10 years after THA, although linear wear rates were higher in the active group [30]. In their case-control study, Jones et al. also concluded physical activity seems not to be a risk factor for the revision of TKA [38]. It might be undisputed that a joint implant is a mechanical device, and wear is increased in each mechanical device the more it is used, and also in dependency of the implant materials, bearing surfaces, and implant positions. However, the border between unacceptably increased failure risk and health benefits gained from physical activity has not yet been approximately estimated. Therefore, there is much room for future research, also considering our responsibility as treating surgeons to face the increasing patient expectations regarding sports and an active lifestyle.
A comparison between physical activity levels in patients undergoing TJA and recommended physical activity levels was not possible with data obtained using physical activity recall questionnaires. This was the result of the use of different questionnaires, the lack of sufficient information for transforming the reported physical activity in values with similar units (eg, METs), and untraditional ways to report physical activity compared with the specific literature. Therefore, future studies should try to standardize how physical activity results from questionnaires and motion sensors are reported, possibly following more common procedures so comparisons with the literature will be easier (Appendix) [5, 48, 67]. The only possible comparisons were with the amount of steps determined using pedometers (10,000 steps target) and with the data recently reported in a meta-analysis performed on studies examining physical activity in healthy people. Even taking into account any potential error of pedometers, it is clear that the amount of steps/day of patients undergoing TJA is well below the recommended 10,000 steps/day and walking activity reported for healthy people [6] (Fig. 3). Bohannon showed that healthy people older than 65 years take 6565 steps/day, whereas those younger than 65 years take 9800 steps/day. Our data are below these values and confirm that there is a relation between age and physical activity with steps decreasing with increasing age (Fig. 2). Extrapolating the mean of 6721 steps/day calculated in our review, patients undergoing TJA perform 1.22 million gait cycles per year. Considering the more accurate measurement using accelerometers, the value of 11,250 steps/day corresponds to 2.05 million cycles per year. These values are approximately 20% to 100% higher than the one million cycles that wear simulations normally assume to correspond to 1 year in vivo. Thus, these simulations correspond to an in vivo period of only 6 to 10 months and such results therefore must be interpreted cautiously even when performed several million times as these simulations would not reflect many years of use.
Fig. 3.
Patients undergoing total joint arthroplasty take obviously less than the recommended 10,000 steps/day for health enhancement (assessed by pedometers).
We identified the different instruments used up to now to quantify physical activity in patients undergoing an arthroplasty. The impact of surgical treatments on physical activity levels from a health-enhancing perspective is more or less neglected in the orthopaedic literature. Gartland criticized the narrow perspective of much orthopaedic research because clinical researchers often described the technical aspects of operative interventions and their impact on the function of a specific joint rather than on the overall physical and economic status of the patient [27]. The summarized results we found indicate, on average, patients undergoing TJA are less active than recommended to achieve health-enhancing activity levels, but they are more active than assumed in wear simulations. Therefore, simulation results or statements supplied by industrial concerns should be interpreted cautiously given an assumed one million cycles do not correspond to 1 year in vivo, but only to approximately 6 to 10 months and given most wear simulations do not even replicate many years of use. Future investigations should evolve more standardization in terms of physical activity assessment and reporting and this review can serve as the basis for such research.
Appendix
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
This work was performed at the Schulthess Clinic, Zurich, Switzerland.
References
- 1.ACSM. American College of Sports Medicine Position Stand The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc. 1998;30:975–991. doi: 10.1097/00005768-199806000-00032. [DOI] [PubMed] [Google Scholar]
- 2.ACSM’s Guidelines for Exercise Testing and Prescription. PPhiladelphia, PA: Lea & Febiger; 1995. [Google Scholar]
- 3.Bennett D, Humphreys L, O’Brien S, Kelly C, Orr J, Beverland DE. Activity levels and polyethylene wear of patients 10 years post hip replacement. Clin Biomech (Bristol, Avon) 2008;23:571–576. doi: 10.1016/j.clinbiomech.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 4.Bennett D, Humphreys L, O’Brien S, Kelly C, Orr J, Beverland DE. The influence of wear paths produced by hip replacement patients during normal walking on wear rates. J Orthop Res. 2008;26:1210–1217. doi: 10.1002/jor.20583. [DOI] [PubMed] [Google Scholar]
- 5.Blair SN, LaMonte MJ, Nichaman MZ. The evolution of physical activity recommendations: how much is enough? Am J Clin Nutr. 2004;79:913S–920S. doi: 10.1093/ajcn/79.5.913S. [DOI] [PubMed] [Google Scholar]
- 6.Bohannon RW. Number of pedometer-assessed steps taken per day by adults: a descriptive meta-analysis. Phys Ther. 2007;87:1642–1650. doi: 10.2522/ptj.20060037. [DOI] [PubMed] [Google Scholar]
- 7.Booth FW, Gordon SE, Carlson CJ, Hamilton MT. Waging war on modern chronic diseases: primary prevention through exercise biology. J Appl Physiol. 2000;88:774–787. doi: 10.1152/jappl.2000.88.2.774. [DOI] [PubMed] [Google Scholar]
- 8.Brandes M, Schomaker R, Mollenhoff G, Rosenbaum D. Quantity versus quality of gait and quality of life in patients with osteoarthritis. Gait Posture. 2008;28:74–79. doi: 10.1016/j.gaitpost.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 9.Caspersen CJ. Physical activity epidemiology: concepts, methods, and applications to exercise science. Exerc Sport Sci Rev. 1989;17:423–473. [PubMed] [Google Scholar]
- 10.Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100:126–131. [PMC free article] [PubMed] [Google Scholar]
- 11.Cavill N, Kahlmeier S, Racioppi F. Physical Activity and Health in Europe: Evidence for Action. Geneva, Switzerland: World Health Organization; 2006. [Google Scholar]
- 12.Church TS, Earnest CP, Skinner JS, Blair SN. Effects of different doses of physical activity on cardiorespiratory fitness among sedentary, overweight or obese postmenopausal women with elevated blood pressure: a randomized controlled trial. JAMA. 2007;297:2081–2091. doi: 10.1001/jama.297.19.2081. [DOI] [PubMed] [Google Scholar]
- 13.Cukras Z, Praczko K, Kostka T, Jegier A. Physical activity of elderly patients after total hip arthroplasty. Orthop Traumatol Rehabil. 2007;9:286–296. [PubMed] [Google Scholar]
- 14.Davey Smith G, Egger M. Meta-analysis: unresolved issues and future developments. BMJ. 1998;316:221–225. doi: 10.1136/bmj.316.7126.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davey Smith G, Egger M, Phillips AN. Meta-analysis: beyond the grand mean? BMJ. 1997;315:1610–1614. doi: 10.1136/bmj.315.7122.1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Groot IB, Bussmann HJ, Stam HJ, Verhaar JA. Small increase of actual physical activity 6 months after total hip or knee arthroplasty. Clin Orthop Relat Res. 2008;466:2201–2208. doi: 10.1007/s11999-008-0315-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Groot IB, Bussmann JB, Stam HJ, Verhaar JAN. Actual everyday physical activity in patients with end-stage hip or knee osteoarthritis compared with healthy controls. Osteoarthritis Cartilage. 2008;16:436–442. doi: 10.1016/j.joca.2007.08.010. [DOI] [PubMed] [Google Scholar]
- 18.Dorey FJ, Amstutz HC. The need to account for patient activity when evaluating the results of total hip arthroplasty with survivorship analysis. J Bone Joint Surg Am. 2002;84:709–710. doi: 10.2106/00004623-200205000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Egger M, Schneider M, Davey Smith G. Spurious precision? Meta-analysis of observational studies. BMJ. 1998;316:140–144. doi: 10.1136/bmj.316.7125.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Egger M, Smith GD. Meta-analysis: potentials and promise. BMJ. 1997;315:1371–1374. doi: 10.1136/bmj.315.7119.1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Egger M, Smith GD. Bias in location and selection of studies. BMJ. 1998;316:61–66. doi: 10.1136/bmj.316.7124.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fagard RH, Cornelissen VA. Effect of exercise on blood pressure control in hypertensive patients. Eur J Cardiovasc Prev Rehabil. 2007;14:12–17. doi: 10.1097/HJR.0b013e3280128bbb. [DOI] [PubMed] [Google Scholar]
- 23.Feller JA, Kay PR, Hodgkinson JP, Wroblewski BM. Activity and socket wear in the Charnley low-friction arthroplasty. J Arthroplasty. 1994;9:341–345. doi: 10.1016/0883-5403(94)90042-6. [DOI] [PubMed] [Google Scholar]
- 24.Fleg JL, Morrell CH, Bos AG, Brant LJ, Talbot LA, Wright JG, Lakatta EG. Accelerated longitudinal decline of aerobic capacity in healthy older adults. Circulation. 2005;112:674–682. doi: 10.1161/CIRCULATIONAHA.105.545459. [DOI] [PubMed] [Google Scholar]
- 25.Flugsrud GB, Nordsletten L, Espehaug B, Havelin LI, Meyer HE. The effect of middle-age body weight and physical activity on the risk of early revision hip arthroplasty: a cohort study of 1535 individuals. Acta Orthop. 2007;78:99–107. doi: 10.1080/17453670610013493. [DOI] [PubMed] [Google Scholar]
- 26.Fontaine KR, Heo M, Bathon J. Are US adults with arthritis meeting public health recommendations for physical activity? Arthritis Rheum. 2004;50:624–628. doi: 10.1002/art.20057. [DOI] [PubMed] [Google Scholar]
- 27.Gartland JJ. Orthopaedic clinical research: Deficiencies in experimental design and determinations of outcome. J Bone Joint Surg Am. 1988;70:1357–1364. [PubMed] [Google Scholar]
- 28.Goldsmith AA, Dowson D, Wroblewski BM, Siney PD, Fleming physical activity. Lane JM. The effect of activity levels of total hip arthroplasty patients on socket penetration. J Arthroplasty. 2001;16:620–627. doi: 10.1054/arth.2001.23566. [DOI] [PubMed] [Google Scholar]
- 29.Goldsmith AA, Dowson D, Wroblewski BM, Siney PD, Fleming physical activity. Lane JM, Stone MH, Walker R. Comparative study of the activity of total hip arthroplasty patients and normal subjects. J Arthroplasty. 2001;16:613–619. doi: 10.1054/arth.2001.23568. [DOI] [PubMed] [Google Scholar]
- 30.Gschwend N, Frei T, Morscher E, Nigg B, Loehr J. Alpine and cross-country skiing after total hip replacement: 2 cohorts of 50 patients each, one active, the other inactive in skiing, followed for 5–10 years. Acta Orthop Scand. 2000;71:243–249. doi: 10.1080/000164700317411825. [DOI] [PubMed] [Google Scholar]
- 31.Hamer M, Chida Y. Walking and primary prevention: a meta-analysis of prospective cohort studies. Br J Sports Med. 2008;42:238–243. doi: 10.1136/bjsm.2007.039974. [DOI] [PubMed] [Google Scholar]
- 32.Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1423–1434. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 33.Healy WL, Sharma S, Schwartz B, Iorio R. Athletic activity after total joint arthroplasty. J Bone Joint Surg Am. 2008;90:2245–2252. doi: 10.2106/JBJS.H.00274. [DOI] [PubMed] [Google Scholar]
- 34.Heisel C, Silva M, dela Rosa MA, Schmalzried TP. Short-term in vivo wear of cross-linked polyethylene. J Bone Joint Surg Am. 2004;86:748–751. doi: 10.2106/00004623-200404000-00012. [DOI] [PubMed] [Google Scholar]
- 35.Heisel C, Streich N, Krachler M, Jakubowitz E, Kretzer JP. Characterization of the running-in period in total hip resurfacing arthroplasty: an in vivo and in vitro metal ion analysis. J Bone Joint Surg Am. 2008;90(suppl 3):125–133. doi: 10.2106/JBJS.H.00437. [DOI] [PubMed] [Google Scholar]
- 36.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Iwane M, Arita M, Tomimoto S, Satani O, Matsumoto M, Miyashita K, Nishio I. Walking 10,000 steps/day or more reduces blood pressure and sympathetic nerve activity in mild essential hypertension. Hypertens Res. 2000;23:573–580. doi: 10.1291/hypres.23.573. [DOI] [PubMed] [Google Scholar]
- 38.Jones DL, Cauley JA, Kriska AM, Wisniewski SR, Irrgang JJ, Heck DA, Kwoh CK, Crossett LS. Physical activity and risk of revision total knee arthroplasty in individuals with knee osteoarthritis: a matched case-control study. J Rheumatol. 2004;31:1384–1390. [PubMed] [Google Scholar]
- 39.Kruger J, Carlson SA, Buchner D. How active are older Americans? Prev Chronic Dis. 2007;4:A53. [PMC free article] [PubMed] [Google Scholar]
- 40.Lamonte MJ, Ainsworth BE. Quantifying energy expenditure and physical activity in the context of dose response. Med Sci Sports Exerc. 2001;33(suppl):S370–S378; discussion S419–S420. [DOI] [PubMed]
- 41.Le Masurier GC, Lee SM, Tudor-Locke C. Motion sensor accuracy under controlled and free-living conditions. Med Sci Sports Exerc. 2004;36:905–910. doi: 10.1249/01.mss.0000126777.50188.73. [DOI] [PubMed] [Google Scholar]
- 42.Le Masurier GC, Tudor-Locke C. Comparison of pedometer and accelerometer accuracy under controlled conditions. Med Sci Sports Exerc. 2003;35:867–871. doi: 10.1249/01.MSS.0000064996.63632.10. [DOI] [PubMed] [Google Scholar]
- 43.Lee IM, Skerrett PJ. Physical activity and all-cause mortality: what is the dose-response relation? Med Sci Sports Exerc. 2001;33(suppl):S459–S471; discussion S493–S494. [DOI] [PubMed]
- 44.Leon AS, Connett J, Jacobs DR, Jr, Rauramaa R. Leisure-time physical activity levels and risk of coronary heart disease and death. The Multiple Risk Factor Intervention Trial. JAMA. 1987;258:2388–2395. [PubMed] [Google Scholar]
- 45.Macera CA, Ham SA, Yore MM, Jones DA, Ainsworth BE, Kimsey CD, Kohl HW., III Prevalence of physical activity in the United States: Behavioral Risk Factor Surveillance System, 2001. Prev Chronic Dis. 2005;2:A17. [PMC free article] [PubMed] [Google Scholar]
- 46.Madsen MS, Ritter MA, Morris HH, Meding JB, Berend ME, Faris PM, Vardaxis VG. The effect of total hip arthroplasty surgical approach on gait. J Orthop Res. 2004;22:44–50. doi: 10.1016/S0736-0266(03)00151-7. [DOI] [PubMed] [Google Scholar]
- 47.McClung CD, Zahiri CA, Higa JK, Amstutz HC, Schmalzried TP. Relationship between body mass index and activity in hip or knee arthroplasty patients. J Orthop Res. 2000;18:35–39. doi: 10.1002/jor.1100180106. [DOI] [PubMed] [Google Scholar]
- 48.Mudd LM, Rafferty AP, Reeves MJ, Pivarnik JM. Physical activity recommendations: an alternative approach using energy expenditure. Med Sci Sports Exerc. 2008;40:1757–1763. doi: 10.1249/MSS.0b013e31817bb8a2. [DOI] [PubMed] [Google Scholar]
- 49.Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346:793–801. doi: 10.1056/NEJMoa011858. [DOI] [PubMed] [Google Scholar]
- 50.Naal FD, Fischer M, Preuss A, Goldhahn J, Knoch F, Preiss S, Munzinger U, Drobny T. Return to sports and recreational activity after unicompartmental knee arthroplasty. Am J Sports Med. 2007;35:1688–1695. doi: 10.1177/0363546507303562. [DOI] [PubMed] [Google Scholar]
- 51.Naal FD, Impellizzeri FM, Leunig M. Which is the best activity rating scale for patients undergoing total joint arthroplasty? Clin Orthop Relat Res. 2009;467:958–965. doi: 10.1007/s11999-008-0358-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Naal FD, Maffiuletti NA, Munzinger U, Hersche O. Sports after hip resurfacing arthroplasty. Am J Sports Med. 2007;35:705–711. doi: 10.1177/0363546506296606. [DOI] [PubMed] [Google Scholar]
- 53.Nocon M, Hiemann T, Muller-Riemenschneider F, Thalau F, Roll S, Willich SN. Association of physical activity with all-cause and cardiovascular mortality: a systematic review and meta-analysis. Eur J Cardiovasc Prev Rehabil. 2008;15:239–246. doi: 10.1097/HJR.0b013e3282f55e09. [DOI] [PubMed] [Google Scholar]
- 54.Ono R, Hirata S, Yamada M, Nishiyama T, Kurosaka M, Tamura Y. Reliability and validity of the Baecke physical activity questionnaire in adult women with hip disorders. BMC Musculoskelet Disord. 2007;8:61. doi: 10.1186/1471-2474-8-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Orendurff MS, Schoen JA, Bernatz GC, Segal AD, Klute GK. How humans walk: bout duration, steps per bout, and rest duration. J Rehabil Res Dev. 2008;45:1077–1089. doi: 10.1682/jrrd.2007.11.0197. [DOI] [PubMed] [Google Scholar]
- 56.Paffenbarger RS, Jr, Hyde RT, Wing AL, Hsieh CC. Physical activity, all-cause mortality, and longevity of college alumni. N Engl J Med. 1986;314:605–613. doi: 10.1056/NEJM198603063141003. [DOI] [PubMed] [Google Scholar]
- 57.Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, Bouchard C, Buchner D, Ettinger W, Heath GW, King AC, et al. Physical activity and public health: a recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273:402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 58.Pescatello LS, Blanchard BE, Heest JL, Maresh CM, Gordish-Dressman H, Thompson PD. The metabolic syndrome and the immediate antihypertensive effects of aerobic exercise: a randomized control design. BMC Cardiovasc Disord. 2008;8:12. doi: 10.1186/1471-2261-8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schmalzried TP, Shepherd EF, Dorey FJ, Jackson WO, dela Rosa M, Fa’vae F, McKellop HA, McClung CD, Martell J, Moreland JR, Amstutz HC. The John Charnley Award. Wear is a function of use, not time. Clin Orthop Relat Res. 2000;381:36–46. doi: 10.1097/00003086-200012000-00005. [DOI] [PubMed] [Google Scholar]
- 60.Schmalzried TP, Szuszczewicz ES, Northfield MR, Akizuki KH, Frankel RE, Belcher G, Amstutz HC. Quantitative assessment of walking activity after total hip or knee replacement. J Bone Joint Surg Am. 1998;80:54–59. [PubMed] [Google Scholar]
- 61.Schneider PL, Bassett DR, Jr, Thompson DL, Pronk NP, Bielak KM. Effects of a 10,000 steps per day goal in overweight adults. Am J Health Promot. 2006;21:85–89. doi: 10.4278/0890-1171-21.2.85. [DOI] [PubMed] [Google Scholar]
- 62.Sechriest VF, II, Kyle RF, Marek DJ, Spates JD, Saleh KJ, Kuskowski M. Activity level in young patients with primary total hip arthroplasty: a 5-year minimum follow-up. J Arthroplasty. 2007;22:39–47. doi: 10.1016/j.arth.2006.02.083. [DOI] [PubMed] [Google Scholar]
- 63.Silva M, McClung CD, Dela Rosa MA, Dorey FJ, Schmalzried TP. Activity sampling in the assessment of patients with total joint arthroplasty. J Arthroplasty. 2005;20:487–491. doi: 10.1016/j.arth.2004.08.013. [DOI] [PubMed] [Google Scholar]
- 64.Silva M, Shepherd EF, Jackson WO, Dorey FJ, Schmalzried TP. Average patient walking activity approaches 2 million cycles per year: pedometers under-record walking activity. J Arthroplasty. 2002;17:693–697. doi: 10.1054/arth.2002.32699. [DOI] [PubMed] [Google Scholar]
- 65.Sofi F, Capalbo A, Cesari F, Abbate R, Gensini GF. Physical activity during leisure time and primary prevention of coronary heart disease: an updated meta-analysis of cohort studies. Eur J Cardiovasc Prev Rehabil. 2008;15:247–257. doi: 10.1097/HJR.0b013e3282f232ac. [DOI] [PubMed] [Google Scholar]
- 66.Talis VL, Grishin AA, Solopova IA, Oskanyan TL, Belenky VE, Ivanenko YP. Asymmetric leg loading during sit-to-stand, walking and quiet standing in patients after unilateral total hip replacement surgery. Clin Biomech (Bristol, Avon). 2008;23:424–433. [DOI] [PubMed]
- 67.Thompson D, Batterham AM, Markovitch D, Dixon NC, Lund AJ, Walhin JP. Confusion and conflict in assessing the physical activity status of middle-aged men. PLoS ONE. 2009;4:e4337. doi: 10.1371/journal.pone.0004337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tudor-Locke C, Ainsworth BE, Thompson RW, Matthews CE. Comparison of pedometer and accelerometer measures of free-living physical activity. Med Sci Sports Exerc. 2002;34:2045–2051. doi: 10.1097/00005768-200212000-00027. [DOI] [PubMed] [Google Scholar]
- 69.Tudor-Locke C, Hatano Y, Pangrazi RP, Kang M. Revisiting ‘how many steps are enough?’ Med Sci Sports Exerc. 2008;40(suppl):S537–S543. [DOI] [PubMed]
- 70.Tudor-Locke C, Sisson SB, Lee SM, Craig CL, Plotnikoff RC, Bauman A. Evaluation of quality of commercial pedometers. Can J Public Health. 2006;97(suppl 1):S10–S16. doi: 10.1007/BF03405359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.US Department of Health and Human Services. Physical Activity and Health: A Report of the Surgeon General. Sudbury, MA: Jones and Bartlett Publishers; 1999.
- 72.Wagenmakers R, Stevens M, Akker-Scheek I, Zijlstra W, Groothoff JW. Predictive value of the Western Ontario and McMaster Universities Osteoarthritis Index for the amount of physical activity after total hip arthroplasty. Phys Ther. 2008;88:211–218. doi: 10.2522/ptj.20060321. [DOI] [PubMed] [Google Scholar]
- 73.Wagenmakers R, Stevens M, Zijlstra W, Jacobs ML, Akker-Scheek I, Groothoff JW, Bulstra SK. Habitual physical activity behavior of patients after primary total hip arthroplasty. Phys Ther. 2008;88:1039–1048. doi: 10.2522/ptj.20070375. [DOI] [PubMed] [Google Scholar]
- 74.Walker DJ, Heslop PS, Chandler C, Pinder IM. Measured ambulation and self-reported health status following total joint replacement for the osteoarthritic knee. Rheumatology. 2002;41:755–758. doi: 10.1093/rheumatology/41.7.755. [DOI] [PubMed] [Google Scholar]
- 75.Wallbridge N, Dowson D. The walking activity of patients with artificial hip joints. Eng Med. 1982;11:95–96. doi: 10.1243/emed_jour_1982_011_023_02. [DOI] [PubMed] [Google Scholar]
- 76.Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: the evidence. CMAJ. 2006;174:801–809. doi: 10.1503/cmaj.051351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Warburton DE, Nicol CW, Bredin SS. Prescribing exercise as preventive therapy. CMAJ. 2006;174:961–974. doi: 10.1503/cmaj.1040750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wei M, Gibbons LW, Kampert JB, Nichaman MZ, Blair SN. Low cardiorespiratory fitness and physical inactivity as predictors of mortality in men with type 2 diabetes. Ann Intern Med. 2000;132:605–611. doi: 10.7326/0003-4819-132-8-200004180-00002. [DOI] [PubMed] [Google Scholar]
- 79.Wei M, Kampert JB, Barlow CE, Nichaman MZ, Gibbons LW, Paffenbarger RS, Jr, Blair SN. Relationship between low cardiorespiratory fitness and mortality in normal-weight, overweight, and obese men. JAMA. 1999;282:1547–1553. doi: 10.1001/jama.282.16.1547. [DOI] [PubMed] [Google Scholar]
- 80.Whitehead A. Meta-analysis of Controlled Clinical Trials. Chichester, United Kingdom: Wiley & Sons; 2002. [Google Scholar]
- 81.Wollmerstedt N, Noth U, Mahlmeister F, Lotze A, Finn A, Eulert J, Hendrich C. [A novel questionnaire to assess activity in patients after hip arthroplasties] [in German] Orthopade. 2006;35:1237–1245. doi: 10.1007/s00132-006-1010-2. [DOI] [PubMed] [Google Scholar]
- 82.Wright RW, Brand RA, Dunn W, Spindler KP. How to write a systematic review. Clin Orthop Relat Res. 2007;455:23–29. doi: 10.1097/BLO.0b013e31802c9098. [DOI] [PubMed] [Google Scholar]
- 83.Wylde V, Blom A, Dieppe P, Hewlett S, Learmonth I. Return to sport after joint replacement. J Bone Joint Surg Br. 2008;90:920–923. doi: 10.1302/0301-620X.90B7.20614. [DOI] [PubMed] [Google Scholar]
- 84.Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13:890–895. doi: 10.1016/s0883-5403(98)90195-4. [DOI] [PubMed] [Google Scholar]