Abstract
Background
Primary or idiopathic osteoarthritis (OA) of the hip has increasingly been attributed to the presence of presumably minor femoral or acetabular deformities that are not routinely identified. The alpha angle reflects one such deformity of the femoral neck and reflects a risk for femoroacetabular impingement, which in turn reportedly is associated with OA. If impingement is in fact associated with OA, then one might expect the mean alpha angle to be greater in patients with presumed idiopathic hip OA.
Questions/purposes
We therefore compared the alpha angle among a group of elderly patients with idiopathic OA with that in a control group of elderly individuals without OA.
Patients and Methods
We measured the alpha angles in 50 individuals (72 hips) with a mean age of 70 years (range, 60–84 years) with apparently idiopathic OA and compared their angles with those from a control group of 56 individuals without OA. The alpha angle was measured by means of radiographs of their hips using the Dunn view at 45° flexion.
Results
The patients with OA had a greater percentage with abnormal alpha angles than did the normal subjects: 82% versus 30%, respectively. The mean alpha angle in the group with OA was larger than in the control subjects: 66.4º (range, 28°–108°) versus 48.1º (range, 34°–68°).
Conclusions
Hips with presumably idiopathic OA had more abnormalities at the femoral head-neck junction than did the control hips without OA and may relate to the risk of OA developing.
Level of Evidence
Level II, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
OA of the hip generally is considered primary (idiopathic) or secondary to known underlying disease such as inflammatory, metabolic, or vascular diseases; sequelae of infection or trauma in the hip, developmental dysplasia, Legg-Calvé-Perthes disease, or epiphysiolysis of the femoral head. More than four decades ago, Murray [14] suggested most cases of primary OA would be the result of minimal deformities of the hip. This thinking was shared by Solomon [17], Harris et al. [9], and Harris [8]. The latter stated primary OA, which had been described as accounting for as much as 65% of such cases, would in reality be an uncommon condition. Some studies suggest seemingly minor femoral or acetabular deformities cause femoroacetabular impingement which in turn reportedly causes OA [2, 5–7, 10, 15, 19–21].
The pistol grip deformity of the proximal femur [18] apparently relates to femoroacetabular impingement. This deformity is characterized as a diminution of the concavity of the head-neck junction, located mainly in the anterior portion.
The alpha angle described by Nötzli et al. [15] quantifies the concavity at the anterior head-neck junction and this reportedly reflects impingement. If impingement is in fact associated with OA, then one would anticipate the alpha angle would be greater in patients with presumed idiopathic OA. The presence of larger alpha angles in individuals with symptomatic femoroacetabular impingement was observed on MRI examinations by Nötzli et al. [15] and on radiographs by Allen et al. [1], and the relationship between an increased alpha angle and the presence of OA was confirmed on CT images by Ecker et al. [4].
We therefore evaluated conventional radiographs of the hip to determine whether patients with presumed idiopathic OA had a greater percentage of abnormal alpha angles than similarly aged subjects without OA.
Patients and Methods
We reviewed the radiographs of hips of 106 individuals older than 60 years from two hospitals. Their mean age was 70 years (range, 60–84 years), and 82 (77%) were female. Their mean body mass index (BMI) was 28 kg/m2 (Table 1). The patients comprised two groups. The first group (Group A) was composed of 50 patients (72 hips with 22 being bilateral) with presumably idiopathic hip OA; their mean age was 69.6 years (range, 60–84 years) and 33 (66%) were women. The second group (Group C) was composed of 56 healthy individuals (112 hips) who were willing to voluntarily undergo the same clinical-radiographic evaluation as the patients in Group A; their mean age was 70.5 years (range, 60–82 years) and 49 (88%) were women. For Group A, we included patients older than 60 years with an indication for THA. These patients presented with disabling pain and reduced hip ROM. Radiographs on these patients showed OA Grade III or IV according to the classification of Kellgren and Lawrence [11]. These patients were included provided an outline of the femoral head and neck was seen that could be distinguished from degenerative alterations (which present outlines that are more irregular). We also included the hip contralateral to the one with the indication for THA if it was OA Grade II or III [11]. All of the patients needed to have sufficient hip mobility to make it possible to obtain the radiographic views (standing AP view of the pelvic girdle, Lequesne false profile view, and Dunn at 45° flexion). We excluded all patients with possible secondary OA such as that related to inflammatory arthritis, trauma, sepsis, development dysplasia of the hip, metabolic diseases, Paget’s disease, osteonecrosis, or proximal femoral epiphysiolysis and patients with other musculoskeletal diseases affecting the lower limbs. We recruited the asymptomatic control elderly participants (control subjects) from among active or retired employees of a public hospital. We excluded patients with a history of lumbar or lower limb musculoskeletal complaints or a history of pain in the hip region (which could be lumbar pain with radiation to the trochanteric region or real hip pain) or radiographic signs of OA such as osteophytes, subchondral cysts, or diminished joint space (superolateral less than 3 mm, apical less than 2 mm, and superomedial less than 2 mm [12]). All of the participants received explanations about the project from the researcher who conducted the examinations (HJMB). They were enrolled in the study only after they agreed with the informed consent statement by signing it. This study had been approved by the ethics committee for research project assessment.
Table 1.
Demographic distribution of Group A (arthritis) and Group C (control)
| Parameter | Arthritis | Control | p Value |
|---|---|---|---|
| Gender | |||
| Male | 17 (34%) | 7 (12.5%) | 0.008 |
| Female | 33 (66%) | 49 (87.5%) | |
| Age (years) | 69.6 ± 5.7 (range, 60–84) | 70.5 ± 5.9 (range, 60–82) | 0.438 |
| Body mass index (kg/m2) | 28 ± 5.2 (range, 18–43) | 26.6 ± 3.9 (range, 17–38) | 0.133 |
Most of the subjects were mixed race, and therefore it was not possible to distinguish groups according to race or ethnicity. Considering the difference in alpha angle that was found between the groups, the sample power was greater than 99%. Women accounted for 87% of Group C (CI of 79 to 96%) and 66% of Group A (CI of 54 to 79%) Therefore, we included gender as a covariable in the statistical analysis.
To document appropriateness for entry in either group we evaluated the clinical history of all the individuals in both groups with emphasis on the presence of symptoms in the hip region and any clinical history; we did not use any standardized method of clinical assessment as the primary inclusion criteria were radiographic. We recorded each patient’s height and weight from which the BMI was calculated. We evaluated ROM to determine whether it would be possible to produce the radiographic views proposed. The name, gender, age, and BMI data for these individuals were recorded in a table in Microsoft Office Excel 2007 (Microsoft Inc, Redmond, WA), and each individual received an identification number.
All subjects in both groups underwent radiographic examination of both hips, including a standing AP view of the pelvic girdle, the Lequesne false profile view [3], and the Dunn view at 45° flexion [19]. All views were obtained in a standardized manner and under supervision by the investigator (HJMB). All radiographs were produced by the same radiology service using the same xray equipment (Duo Diagnost 800 mA telecommand equipment; Phillips Medical Systems, Hamburg, Germany) by a technical team formed by three radiology technicians who were trained and supervised by the same radiologist (MBR).
From the radiographs produced in the standing AP view of the pelvic girdle, one of us (HJMB) made all radiographic measurements: the center-edge (Wiberg) angle [3], Tönnis angle [3], acetabular depth/diameter index [3], percentage coverage of the femoral head [3], and neck-diaphysis angle [3] (Table 2). We also determined the presence or absence of a crossover sign (a reflection of retroversion) [19], coxa profunda, and acetabular protrusion. The crossover sign was present in 7.1% of the patients with OA versus 8.1% of the control subjects. Neither a protruding nor a deep acetabulum was observed on any of the radiographs. From radiographs produced in the Lequesne view, we measured the center-anterior edge angle [3] (Table 2), and from the Dunn view at 45°, we measured the femoral head-neck offset [19] (Table 2) and the alpha angle [19]. To measure the alpha angle we used the Dunn radiographic view at 45° flexion of the hip, which we obtained by positioning the patient in dorsal decubitus with the hip to be evaluated at 45° flexion and at neutral rotation and 20° abduction, with the center beam directed to the inguinal fold at 90° at a source-to-film distance of 100 cm (Fig. 1). We measured the alpha angle measurement by first obtaining the intersection between two lines: the first line was the long axis of the femoral neck and the second connected the center of the femoral head to the point where the anterior cortical surface of the junction between the head and the femoral neck diverged from where the ideal circumference of the femoral head would be (Fig. 2). To make these measurements, we used compasses and an aluminum goniometer with double angulation and an elongated arm. We considered an angle greater than 50° as abnormal [19]. The radiographs were marked using an ordinary pencil. To evaluate the reliability of these measures, the same investigator reevaluated a random sample of 100 hips 6 months after the first assessment. The intraclass correlation coefficient was 0.887 with a 95% confidence interval ranging from 0.836 to 0.992; Nötzli et al. [15] reported an intraobserver variation of approximately 3% and interobserver variation of approximately 5%.
Table 2.
Other radiographic parameters evaluated in Group A (arthritis) and Group C (control)
| Parameter | Group | Mean | SD | Median | Minimum | Maximum | Range | 95% confidence interval related to the mean | |
|---|---|---|---|---|---|---|---|---|---|
| Center-edge angle p = 0.892 | Arthritis | 38.8 | 10.1 | 38.0 | 20 | 74 | 54 | 36.5 | 41.1 |
| Control | 39.1 | 6.7 | 38.0 | 20 | 56 | 36 | 37.9 | 40.3 | |
| Total | 39.0 | 8.2 | 38.0 | 20 | 74 | 54 | 37.8 | 40.2 | |
| HTE p = 0.299 | Arthritis | 4.9 | 6.4 | 6.0 | −18 | 16 | 34 | 3.4 | 6.4 |
| Control | 3.5 | 5.1 | 4.0 | −12 | 15 | 27 | 2.6 | 4.4 | |
| Total | 4.1 | 5.6 | 4.0 | −18 | 16 | 34 | 3.3 | 4.9 | |
| Acetabular depth/diameter index p = 0.002 | Arthritis | 53.3 | 9.7 | 51.5 | 35.7 | 84.4 | 48 | 51.1 | 55.5 |
| Control | 58.2 | 6.8 | 58.2 | 44.3 | 81.8 | 37.5 | 56.9 | 59.5 | |
| Total | 56.3 | 8.4 | 56.0 | 35.7 | 84.4 | 48.7 | 55.1 | 57.5 | |
| Percent coverage of femoral head p = 0.006 | Arthritis | 84.2 | 9.4 | 83.2 | 55.6 | 120.0 | 64.4 | 82 | 86.4 |
| Control | 88.9 | 7.3 | 88.2 | 66.7 | 115.9 | 49.2 | 87.5 | 90.3 | |
| Total | 87.1 | 8.5 | 86.3 | 55.6 | 120.0 | 64.4 | 85.9 | 88.3 | |
| Neck-diaphysis angle p = 0.003 | Arthritis | 134.2 | 7.5 | 133.0 | 118 | 150 | 32 | 132.5 | 135.9 |
| Control | 130.5 | 5.6 | 130.0 | 120 | 144 | 24 | 129.5 | 131.5 | |
| Total | 132.0 | 6.6 | 131.0 | 118 | 150 | 32 | 131.0 | 133.0 | |
| VCA angle p = 0.106 | Arthritis | 48.8 | 14.7 | 47.0 | −20 | 80 | 100 | 45.4 | 52.2 |
| Control | 46.1 | 6.9 | 46.0 | 22 | 60 | 38 | 44.8 | 47.4 | |
| Total | 47.2 | 10.7 | 46.0 | −20 | 80 | 100 | 45.7 | 48.7 | |
| Femoral head/neck offset p = 0.294 | Arthritis | 6.9 | 3.5 | 7.0 | 0 | 15 | 15 | 6.1 | 7.7 |
| Control | 7.5 | 2.5 | 8.0 | 1 | 14 | 13 | 7 | 8.0 | |
| Total | 7.3 | 2.9 | 7.0 | 0 | 15 | 15 | 6.9 | 7.7 | |
HTE = horizontal toit externe (Tönnis angle); VCA = vertical central anterior.
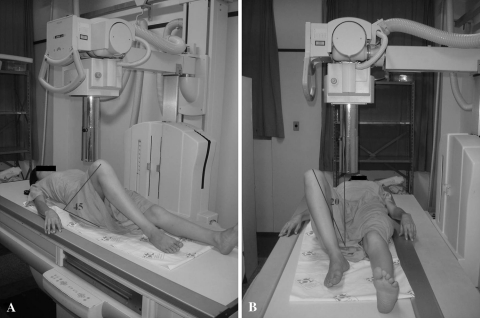
Fig. 1A–B.
Dunn radiographic views at 45° flexion produced by positioning the patient in dorsal decubitus with (A) 45° flexion of the hip that is to be evaluated, and with (B) neutral rotation and 20° abduction are shown; the center beam is regulated at 90° centered on the hip. The source-to-film distance should be 1 m.
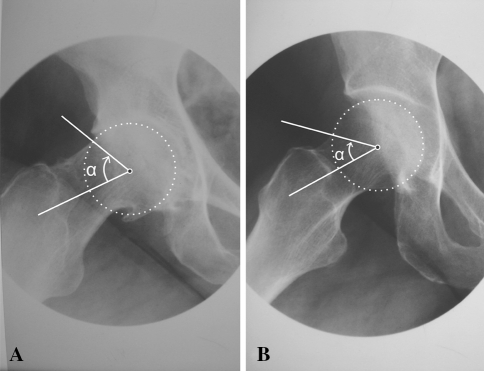
Fig. 2A–B.
The alpha angle was defined as the acute angle between the neck axis and the line connecting the center of the femoral head with the point where the cortical surface of the head-neck junction first exited a perfect circle drawn around an ideally spherical femoral head. (A) A right hip with severe osteoarthritis (OA), with an increased alpha angle, and (B) a right hip without OA, with a normal alpha angle are shown.
Measurements made on the two hips of the same individual could not be considered independent. For this reason, we compared the means in Groups A and C using ANOVA with repeated measurements on the hips of the same individual in an unstructured covariance matrix [16], which is a parametric test with suppositions of normality and equality of variance except for independence of the data. We included gender as a covariate in the ANOVA. The intraobserver reliability was evaluated based on the intraclass correlation coefficient.
Results
The group with OA had a greater (p < 0.001) percentage of patients with abnormal alpha angles than did the healthy control subjects: 82% versus 30%. Group A had a greater (p < 0.001) mean alpha angle than did Group C with and without gender as a covariant: 66.4º versus 48.1º, respectively (Table 3).
Table 3.
Alpha angle in Group A (arthritis) and Group C (control)
| Parameter | Group | Mean (degrees) | SD | Median | Minimum | Maximum | Range | 95% confidence interval related to the mean | |
|---|---|---|---|---|---|---|---|---|---|
| Alpha angle p < 0.001 | Arthrosis | 66.4 | 13.3 | 68.0 | 28 | 108 | 80 | 63.3 | 69.5 |
| Control | 48.1 | 6.8 | 48.0 | 34 | 68 | 34 | 46.8 | 49.4 | |
| Total | 55.3 | 13.3 | 51.0 | 28 | 108 | 80 | 53.4 | 57.2 | |
Discussion
Among the anatomic abnormalities of the hip that have been discussed as predisposing factors for the development of OA, the pistol grip deformity [18], located in the femoral portion of the hip, is a major risk factor [7]. It may occur alone or, often, in association with acetabular deformities. This deformity, which generally occurs at the anterior femoral head-neck junction, can be quantified by measuring the alpha angle. To confirm these suggestions, we evaluated conventional radiographs of the hip to determine whether patients with presumed idiopathic OA had a greater percentage of abnormal alpha angles than did similarly aged subjects without OA.
We caution readers about several limitations. First, because of the limitation of motion among the patients with OA, we had difficulty obtaining some of the lateral views of the femoral neck. We chose to use only the Dunn view at 45°, because this view is considered superior for evaluating abnormalities of the femoral head-neck outline that are located anterosuperiorly [13]. Second, the sample size initially was based on the literature rather than a previous calculation or pilot study. However, the sample was sufficient after calculating the power analysis. Third, the sample had a greater number of females. However, the statistical analysis using gender as a covariable showed this factor did not influence the results. Fourth, it is possible the degenerative alterations in the hip consequent to OA, such as the presence of osteophytes, could influence measurement of the alpha angle. However, while measuring the angles, we judged it was possible to distinguish these abnormalities, because the osteophytes were characterized by presenting outlines of greater irregularity, whereas the pistol grip deformity that we sought to evaluate was, in turn, characterized by a continuous, slightly convex line between the femoral head and the anterior cortex of the femoral neck. Fifth, we measured the alpha angle from conventional lateral-view radiographs of the femoral neck rather than using CT or MRI. However, our data were similar to those from other studies that used CT [4] or MRI [15], but at lower cost and with less exposure to ionizing radiation than with CT. Finally, various anatomic deformities frequently are associated with OA that is considered primary [1]. In particular, there are acetabular deformities that also cause femoroacetabular impingement [1]. These may be present alone or in association with femoral deformities [1]. Although we studied only a femoral deformity, we do not presume this is the only or even a main cause of hip OA, but rather as one important predictive factor of OA among others.
The mean alpha angle of 48.1° we found for the control group of healthy individuals was very close to findings described in the literature (Table 4) as normal values for the alpha angle. Nötzli et al. [15] obtained a mean value of 42º and Allen et al. [1] observed a mean of 63°, whereas Toogood et al. [20] reported a mean of 49º among individuals older than 50 years. From our analysis of the difference between the alpha angle measurements in the group with symptomatic hips (Table 4), our results (66.4°) also were close to those presented in the literature (74° [15] versus 69.9° [1]).
Table 4.
Comparison of published alpha angle results between normal and diseased groups
The relationship between deformities at the femoral head-neck junction and evolution to OA, which was emphasized by others [2, 5–7], could be described through the alpha angle results reported by Ecker et al. [4] and in our study. In a study using alpha angle measurements obtained from CT images, Ecker et al. [4] reported mean alpha angles among elderly people without OA of 51.2º and 65.6º in a group with OA. These values are similar to ours. Likewise, the frequency of individuals with an alpha angle greater than 50º that we observed (83% for the group with OA versus 30% in the control group) was similar to that reported by Ecker et al. [4] (83% versus 40%).
The mean alpha angle is greater in elderly patients with idiopathic hip OA compared with individuals of the same age without disease in the hip, and femoral head-neck asphericity is more common in patients with hip OA. The recognition of this association may help with early detection of individuals at risk for having OA develop. Through this, preventive measures can be determined, such as recommendations for altering occupations or sports activities. For symptomatic patients with these recognized deformities there may be indications for early correction to relieve symptoms.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Allen D, Beaulé PE, Ramadan O, Doucette S. Prevalence of associated deformities and hip pain in patients with cam-type femoroacetabular impingement. J Bone Joint Surg Br. 2009;91:589–594. doi: 10.1302/0301-620X.91B5.22028. [DOI] [PubMed] [Google Scholar]
- 2.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 3.Delaunay S, Dussault RG, Kaplan PA, Alford BA. Radiographic measurements of dysplastic adult hips. Skeletal Radiol. 1997;26:75–81. doi: 10.1007/s002560050197. [DOI] [PubMed] [Google Scholar]
- 4.Ecker TM, Tannast M, Puls M, Siebenrock KA, Murphy SB. Pathomorphologic alterations predict presence or absence of hip osteoarthrosis. Clin Orthop Relat Res. 2007;465:46–52. doi: 10.1097/BLO.0b013e318159a998. [DOI] [PubMed] [Google Scholar]
- 5.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264–272. doi: 10.1007/s11999-007-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 7.Goodman DA, Feighan JE, Smith AD, Latimer B, Buly RL, Cooperman DR. Subclinical slipped capital femoral epiphysis: relationship to osteoarthrosis of the hip. J Bone Joint Surg Am. 1997;79:1489–1497. doi: 10.2106/00004623-199710000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Harris WH. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986;213:20–33. [PubMed] [Google Scholar]
- 9.Harris WH, Bourne RB, Oh I. Intra-articular acetabular labrum: a possible etiological factor in certain cases of osteoarthritis of the hip. J Bone Joint Surg Am. 1979;61:510–514. [PubMed] [Google Scholar]
- 10.Jager M, Wild A, Westhoff B, Krauspe R. Femoroacetabular impingement caused by a femoral osseous head-neck bump deformity: clinical, radiological, and experimental results. J Orthop Sci. 2004;9:256–263. doi: 10.1007/s00776-004-0770-y. [DOI] [PubMed] [Google Scholar]
- 11.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lequesne M, Malghem J, Dion E. The normal hip joint space: variations in width, shape, and architecture on 223 pelvic radiographs. Ann Rheum Dis. 2004;63:1145–1151. doi: 10.1136/ard.2003.018424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meyer DC, Beck M, Ellis T, Ganz R, Leunig M. Comparison of six radiographic projections to assess femoral head/neck asphericity. Clin Orthop Relat Res. 2006;445:181–185. doi: 10.1097/01.blo.0000201168.72388.24. [DOI] [PubMed] [Google Scholar]
- 14.Murray RO. The aetiology of primary osteoarthritis of the hip. Br J Radiol. 1965;38:810–824. doi: 10.1259/0007-1285-38-455-810. [DOI] [PubMed] [Google Scholar]
- 15.Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 16.Ranstam J. Problems in orthopedic research: dependent observations. Acta Orthop Scand. 2002;73:447–450. doi: 10.1080/00016470216327. [DOI] [PubMed] [Google Scholar]
- 17.Solomon L. Patterns of osteoarthritis of the hip. J Bone Joint Surg Br. 1976;58:176–183. doi: 10.1302/0301-620X.58B2.932079. [DOI] [PubMed] [Google Scholar]
- 18.Stulberg SD. Unrecognized childhood hip disease: a major cause of idiopathic osteoarthritis of the hip. In: Cordell LD, Harris WH, Ramsey PL, MacEwen GD, eds. The Hip: Proceedings of the Third Open Scientific Meeting of the Hip Society. St Louis, MO: CV Mosby; 1975:212–228.
- 19.Tannast M, Goricki D, Beck M, Murphy SB, Siebenrock KA. Hip damage occurs at the zone of femoroacetabular impingement. Clin Orthop Relat Res. 2008;466:273–280. doi: 10.1007/s11999-007-0061-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Toogood BS, Skalak A, Cooperman DR. Proximal femoral anatomy in the normal human population. Clin Orthop Relat Res. 2009;467:876–885. doi: 10.1007/s11999-008-0473-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wagner S, Hofstetter W, Chiquet M, Mainil-Varlet P, Stauffer E, Ganz R, Siebenrock KA. Early osteoarthritic changes of human femoral head cartilage subsequent to femoro-acetabular impingement. Osteoarthritis Cartilage. 2003;11:508–518. doi: 10.1016/S1063-4584(03)00075-X. [DOI] [PubMed] [Google Scholar]