Abstract
Background
The high hip center technique used for a deficient acetabulum is reconstruction of the hip at a high center of rotation. In the literature, there is no consensus regarding the value of this technique.
Questions/purposes
We investigated whether the new-generation biconical threaded Zweymüller® cup fixed in a high nonanatomic position in patients with arthritis secondary to congenital hip disease experienced different rates of polyethylene wear and long-term survivorship when compared with anatomically positioned cups.
Patients and Methods
We studied the polyethylene wear rate and Kaplan-Meier survivorship of 104 titanium threaded Zweymüller® cups in 88 patients (81 females), placed in 70 hips at near-normal hip center and in 34 hips at a high hip center position at a distance of 31.1 to 60 mm (mean, 39.7 mm) from the interteardrop line. Minimum followup was 2 years (mean ± SD, 8.6 ± 3.5 years; range, 2–15 years).
Results
The mean linear polyethylene wear rates in the near-normal and high hip center groups were not different (0.110 ± 0.050 mm and 0.113 ± 0.057 mm, respectively). The Kaplan-Meier 15-year cup survivorship rates with revision for any reason as an event of interest in the near-normal and high hip center groups also were not different (97.2% [95% confidence interval, 88.5%–99.3%] and 97.1% [95% confidence interval, 73.8%–99.3%], respectively).
Conclusions
The high hip center technique using a biconical threaded Zweymüller® cup in patients with arthritis secondary to congenital hip disease results in a polyethylene wear rate and long-term cup survivorship comparable to those observed in anatomically positioned cups.
Level of Evidence
Level III, therapeutic study. See the Guidelines for Authors for a complete description of level of evidence.
Introduction
The high hip center (HHC) technique for a deficient acetabulum is defined as the reconstruction of the hip at a high center of rotation located at a distance greater than 35 mm from the interteardrop line (a method not analogous to the pelvis height of each patient [32]) or 15 mm higher than the approximate femoral head center (AFHC) [25, 28]. There is no consensus regarding the value of this technique. Previous experimental studies [8, 18, 37] suggest the HHC is a mechanically unacceptable hip position. Clinical studies [3, 9, 25] have shown high and especially lateral cup placement results in elevated rates of loosening and polyethylene (PE) wear. Nevertheless, the HHC technique in primary or revision arthroplasty for periacetabular bone deficiency has been proposed as a valuable alternative by many authors [1, 5, 7, 10, 13, 15, 21, 23, 32, 34, 35]. The HHC has the advantages of not requiring structural bone grafts, retention of adequate healthy bone stock for revision, and reducing anesthetic and surgical time [1, 10, 13, 15, 32, 34, 35].
By using longer neck/head length, adequate leg lengthening may be achieved, and sufficient strength and length of abductors to ensure hip stability [5, 7, 32]. Biconical threaded biologically fixed Zweymüller® (Aurau, Switzerland) cups also have had excellent results in normal hip reconstruction cases [2, 11, 22, 26, 27, 31, 33, 39, 40]. However, additional clarification of published studies is needed concerning linear PE wear rate and survivorship when these cups are placed in a high nonanatomic hip position.
In the current clinical study, we wished to show the utility of using HHC placement of Zweymüller® cups in patients with arthritis secondary to congenital hip disease. Specifically, we aimed to compare the rate of linear PE wear and the Kaplan Meier survivorship of total hip replacements performed for arthritis secondary to congenital hip disease placed with a high hip center versus a near normal position.
Patients and Methods
Between September 1993 and April 2007, we implanted 92 patients (112 hips) with osteoarthritis secondary to congenital hip disease with a titanium biologically fixed threaded biconical Zweymüller® cup in combination with a straight cementless stem with a double taper made of hot forged titanium alloy (BICON-PLUS® System; Plus Orthopaedics AG/Smith & Nephew, Aurau, Switzerland). Four patients died from causes unrelated to the hip surgery. We retrospectively reviewed 88 of these patients (104 hips), seven males (eight hips) and 81 females (96 hips), for mechanical cup loosening and mean linear PE wear at a minimum followup of 2 years (mean ± SD, 8.6 ± 3.5 years; range, 2–15 years). Seven patients (11 hips) unable to attend the followup in the office were evaluated by telephone and radiographs were sent for study and analysis. The mean age of the 88 patients was 52.3 years (range, 34–77.2 years) at the time of the first surgery. Fifty-one of the 104 reexamined hips (49%) were dysplastic at the time of surgery (36 of them [36 of 51, 70%] in patients with bilateral congenital hip disease); 39 of 104 (37.5%) were low dislocated (31 of them [31 of 39, 79.5%] in patients with bilateral congenital hip disease); and 14 of 104 (13.5%) were high dislocated according to the classification of Hartofilakidis et al. [14]. Eleven of the 14 high dislocations [78.6%] occurred in patients with bilateral congenital hip disease and seven of these patients had bilateral THAs. The mean Harris hip score was 36 (range, 16–67) preoperatively.
Preoperatively, we estimated Trendelenburg’s sign and functional leg length inequality by measuring the xiphisternum to medial malleolus distances and tried to determine the limb lengthening acceptable to the patient, keeping in mind all stiff pelvis or lumbar spine deformities and muscle contracture [29, 30]. Elevated shoes at different heights were used for all patients with unilateral congenital dislocation to determine preoperatively the approximate acceptable limits of leg lengthening.
The preoperative level of the greater trochanter in correlation with the interteardrop line (Fig. 1), another important parameter to estimate preoperatively the operative difficulties in lowering a congenital dislocated hip, was evaluated by one of the authors (KPD). In all high dislocated hips, the acetabular cranial or anterior column insufficiency and the most healthy osseous periacetabular region to fix the cup were evaluated by preoperative three-dimensional CT representations.
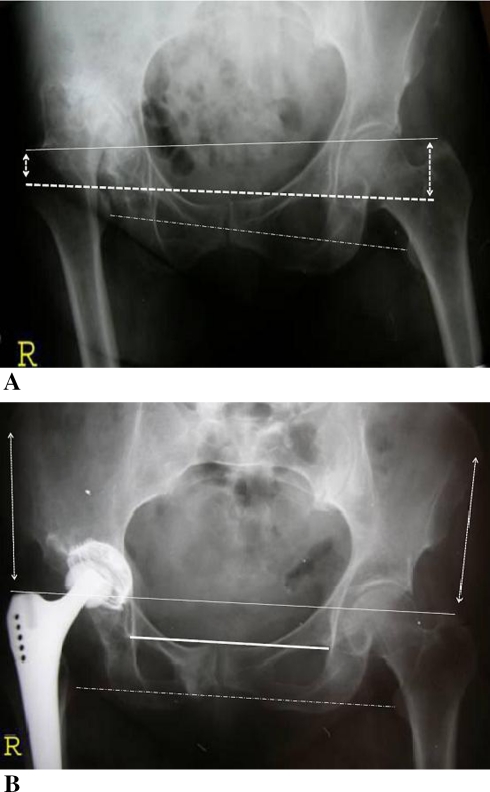
Fig. 1A–B.
The preoperative greater trochanter levels in high dislocated hips in correlation to the true acetabulum and interteardrop line position are shown in these illustrations. (A) The preoperative low position of the tip of the greater trochanter in a high dislocated hip in correlation to the opposite normal hip side and the interteardrop line position, and (B) the parallel position of the lesser trochanter line to interteardrop line postoperatively are shown. The equal distances between the tip of the greater trochanter and the anterior iliac spine on both sides also are illustrated.
The cup was placed in 70 hips at near-normal hip center (NHC) position and in 34 hips at a HHC position at a distance of 31.1 to 60 mm (mean, 39.7 mm) from the interteardrop line. In the latter group, the hip center was located at a vertical distance of greater than 15 mm from the AHFC [25]. In 22 of these hips (22 of 34, 64.7%), the hip center was located outside the Ranawat triangle [28] and at a vertical distance greater than 35 mm from the interteardrop line. In the remaining 12 hips (12 of 34, 35.3%), the hip center was located in the inner site of the Ranawat triangle, four at a vertical distance greater than 35 mm from the interteardrop line and eight at a vertical distance less than 35 mm from the interteardrop line but at a vertical distance greater than 15 mm from the AHFC, depending on the vertical diameter of the pelvis in each patient. In 14 of the HHC hips (14 of 34, 41%), the cup was placed in a superolateral position according to the classification of Pagnano et al. [25].
The articulating surfaces used in the cups placed at or near the NHC position were metal-on-metal in 20 of 70 (28.6%) hips, ceramic-on-PE in 38 of 70 (54.3%) hips, and metal-on-PE in 12 of 70 (17.1%) hips. In the HHC group, the articulating surfaces used were metal-on-metal in four of 34 (11.8%) hips, ceramic-on-PE in 21 of 34 (61.8%) hips, and metal-on-PE in nine of 34 (26.5%) hips. All heads had a diameter of 28 mm except three high dislocated hips in which metallic heads with a diameter of 22 mm were used. An UHMWPE liner was used in all metal- or ceramic-on-PE articulating surfaces (Plus Orthopedics AG/Smith & Nephew). The cup shell was of pure titanium with a surface roughened by grit blasting. The mean surface roughness was 5 μm, with no coating. The shells were designed as double cones [39, 40]. Internally, the cup had a system of three sectoral openings used to check the cup position intraoperatively and providing access for bone grafting. Once the cup was in its definitive position, the openings were closed, preventing direct contact between the PE liner and bony acetabular floor. Externally, the cup shell had sharply cutting teeth, providing threads in two types, shorter ones for normal to hard bone (standard type of cup) and longer ones for soft osteoporotic bone (porosis type of cup), and providing a surface area 46% larger than that of standard cup designs. There were no holes for screw fixation for added stability. Fifty-seven (54.8%) of the cups used were the standard version and the remaining cups were the porosis type. Cotyloplasty of the floor of the acetabulum using cancellous bone from the resected femoral head inserted through the apertures in the shell was made in four (0.38%) of the hips. No superior acetabular grafts were used. In three of 104 (0.28%) hips with anterior column insufficiency and deficient acetabular bone stock, special congenital hip dislocation Zweymüller® cups of 38 mm (one hip) and 40 mm (two hips) were used in combination with 22-mm metallic heads and elevated PE inserts. Elevated cup inserts were used in 12 (17.1%) NHC hips and in eight (23.5%) HHC hips.
All patients were operated on by the same surgeon (NAC). In three hips with high hip dislocation and fixed adduction deformity, an adductor tenotomy was performed before arthroplasty. The transgluteal approach of Thomine et al. [36] was used to prevent damage to the posterior strong part of the gluteus medius muscle and its nerve. Harding’s approach was used in high dislocated hips. Both approaches with the patient in a lateral decubitus position. Femoral shortening osteotomies or greater trochanter osteotomies were not performed in this series unless previous trochanteric varus osteotomies were performed, which was the case in seven (0.67%) hips.
The acetabulum was prepared in standard fashion for insertion of the threaded biconical Zweymüller® cup. Then the double-cone cup was put in place and screwed in, making sure its plane was parallel to the reamed bony acetabular floor without tilting. The cup initially was seated only halfway down and the seating instrument then was removed to check the implant position relative to the bony acetabular floor. The cup was stably fixed into the acetabular columns even in cranially uncovered cases and this was checked by the cup instrumentation during surgery. The sector shutters at the front end of the cup were closed to prevent direct contact of the bone with the PE liner. In cases of anterior column insufficiency, the metal shell was fixed into the columns at a position of greater flexion, but the flexion of the articulating cup surface was corrected by using an inclinated insert in the opposite direction. Once this was completed, we instrumented the femoral shaft, and by using trial stems at different depths in the femoral canal and by changing the usually 15° stem anteversion by a few degrees, stability of the hip was achieved under control of combined movements of extension, external rotation, and adduction, or full internal rotation, adduction, and flexion. Thus, in some cases, elevating or deepening the position of the stem in the femoral canal was used in combination with different head/neck lengths, resulting in what we estimated to be optimal for stability of the hip and producing the optimal length for gluteal muscle function (Fig. 2). The wound was closed in layers with two Redon drains in place. In the postoperative period, we advised the patient to load the surgically treated leg using two crutches for 6 weeks. All patients received antithrombotic prophylaxis using low-molecular-weight heparin.
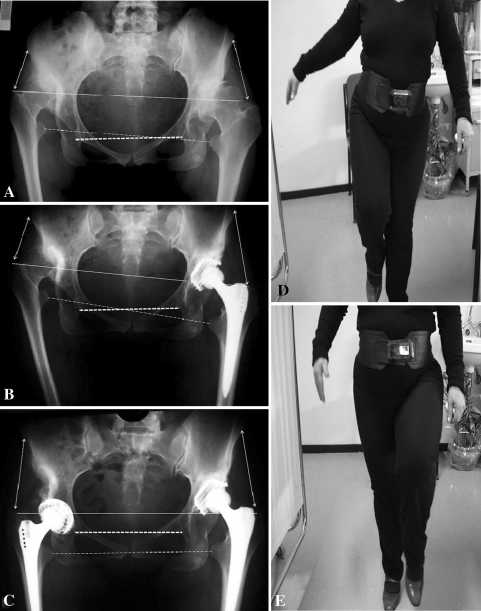
Fig. 2A–E.
The leg length equality in relation to the interteardrop line by normal cup placement position in the right high dislocated hip and a high cup placement in the left low dislocated hip in combination with equal traction of hip abductors are shown. (A) A preoperative radiograph of a 41-year-old woman shows osteoarthritis secondary to high hip dislocation at the right side and low hip dislocation at the left side according to the classification of Hartofilakidis et al. [14]. There are excessive leg length anatomic inequality and different distances between anterior iliac spines and tips of the greater trochanters. (B) An AP view of the pelvis taken 3 months postoperatively (left side) shows lowering of the greater trochanter and leg lengthening in combination with a high cup placement. (C) An AP view of the pelvis taken 9 years postoperatively from the first left arthroplasty and 8.3 years from the second right arthroplasty shows stable hip implants, leg length equality, and similar distances between anterior iliac spines and tips of the greater trochanters or periacetabular myoskeletal equilibrium of the pelvis and legs. The patient is shown in these (D) left and (E) right unilateral weightbearing standing positions, without Trendelenburg’s sign.
The clinical course of each patient was evaluated preoperatively, at 6 to 8 weeks, at 1 year, and at 2-year intervals thereafter. We clinically assessed each patient with the Harris hip score, leg length inequality, Trendelenburg’s sign, and lumbar back pain. The anatomic or structural leg lengthening was estimated radiographically by measuring the distances between the tip of the lesser trochanters and the interteardrop line preoperatively and postoperatively. The apparent or functional leg equalization was estimated by measuring the distances between the xiphisternum and medial malleolus in both legs.
The first postoperative radiographs were obtained approximately 3 to 5 days after surgery. The implant position was first evaluated on the postoperative radiographs. Abduction of 40° to 50° was defined as the standard cup position. We also estimated the new hip center in correlation to the AFHC on the basis of the Ranawat triangle model [28].
Radiolucent lines were classified as described by DeLee and Charnley [6]. We also evaluated periimplant bony reactions and periacetabular gaps on postoperative radiographs.
The mean linear wear rate of UHMWPE was determined with the Roman software program [12] (Roman free to share software version V1.70; Robert Jones and Agnes Hunt Orthopaedic Hospital, Oswestry, UK; http://www.Keele.ac.uk/depts./rjah/). Intraobserver variability was determined for each method by determining the correlation coefficient of two measurements performed by one observer at 1-week intervals. Interobserver variability was determined by estimating the correlation coefficient of two measurements performed by two different observers (KPD, ANC). Using the same coordinate system as described above, the coordinates of the cup center, the head center, and the pelvic height were measured. PE wear was defined as the difference in the head center in each radiograph.
The continuous variables are expressed as mean ± SD. Distributions of the measured variables were assessed for normality by the Shapiro-Wilk test. Differences in mean parameter values between groups (NHC versus HHC) were assessed by Student’s t test. Homogeneity of parameter variance between the two groups was evaluated by Levene’s test. Kaplan-Meier [19] analysis was performed to assess the cup survivorship with revision for any reason as an event of interest at the time of followup. The equality of the survival distributions between NHC and HHC was compared by long-rank test. A two-tailed p value less than 0.05 was considered statistically significant. Statistical analysis was performed with SPSS® Version 15 (SPSS Inc, Chicago, IL).
Results
The mean Harris hip score was 88.6 (range, 56–100) at the time of followup, 91.2 (range, 54–100) for patients with NHC and 84.2 (range, 47–100) for patients with HHC. Trendelenburg gait was ameliorated in all hips except two with the HHC technique. The mean leg anatomic lengthening was 1.51 cm (range, 0.6–3.8 cm), 1.23 cm (range, 0.6–2.3 cm) for patients with NHC and 2.35 (range, 1.6–3.8 cm) for patients with HHC. The mean leg length anatomic inequality for all patients was corrected from 2.82 cm (range, 0–6.4 cm) preoperatively to 1.17 cm (range, 0–2.9 cm) postoperatively. The mean functional leg length inequality for all patients was corrected from 1.99 cm (range, 0–4.2 cm) preoperatively to 1.02 cm (range, 0–2.5 cm) postoperatively. One periprosthetic femoral shaft fracture, one superficial hematoma, one dislocation with cup displacement on the first postoperative day, and two dislocations 1 month postoperatively occurred in the HHC group (Table 1). No impingement problems or neurologic complications were observed in the HHC group. Triangular cranial gaps were present postoperatively in 16 (47%) HHC hips. In three of them, the cup was cranially totally uncovered. Also, partial gaps between the metal shell and acetabular floor, 1 to 4 mm wide, were present in 17 (24.3%) NHC hips and in nine (26.5%) HHC hips. In 51 (72.9%) NHC hips and in 23 (67.6%) HHC hips, there was evidence of periprosthetic new bone formation (Fig. 3).
Table 1.
Complications in near-normal and high hip center hips
| Complication | NHC (n = 70) | HHC (n = 34) |
|---|---|---|
| Intraoperative | ||
| Femoral shaft fracture | 1 (1.4%) | 1 (2.9%) |
| Early postoperative | ||
| Nerve paresis | 3 (4.3%) | 0 |
| Dislocation with cup displacement | 0 | 1 (2.9%) |
| Superficial hematoma | 2 (2.9%) | 1 (2.9%) |
| Superficial infection | 1 (1.4%) | 0 |
| Pulmonary embolism to death | 1 (1.4%) | 0 |
| Late postoperative | ||
| Dislocation | 2 (2.9%) | 2 (5.9%) |
| Ossification Brooker III | 1 (1.4%) | 0 |
| Osteolysis (metal-on-metal) without cup migration | 1 (1.4%) | 0 |
| Osteolysis (metal-on-metal) with cup migration | 0 | 1 (2.9%) |
| Stem loosening | 0 | 0 |
| Cup revision | 2 (2.9%) | 1 (2.9%) |
NHC = near-normal hip center; HHC = high hip center.
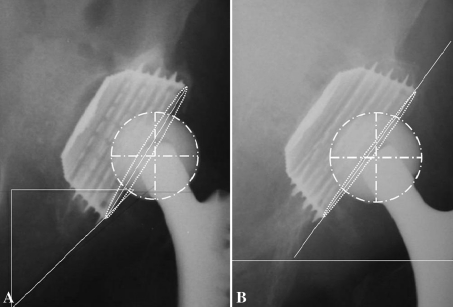
Fig. 3A–B.
The radiographic view of a cup placed at an extremely superolateral position and radiographic schedules of Roman software program for measurement of mean linear PE wear rate are shown. (A) An AP radiographic view of a ceramic-on-PE cup taken 1 month postoperatively shows the cup placed at a superior and lateral position out of the Ranawat triangle with a partial cranial gap and gap between the front end of the implant and the acetabular floor as a result of the surgical technique. (B) An AP radiographic view of the cup taken 9 years postoperatively shows a stable metal cup shell, periprosthetic osseointegration, and no measurable PE wear.
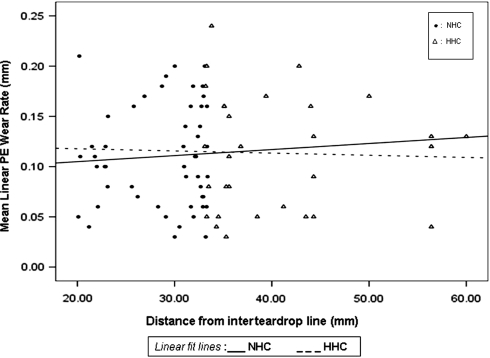
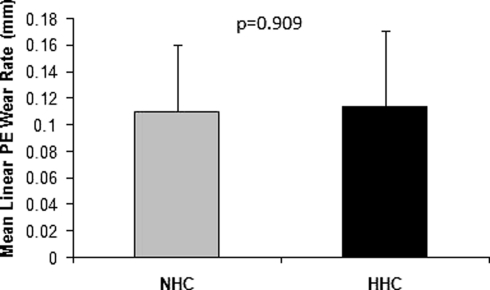
The mean linear PE wear rates in the NHC and HHC groups were similar (p = 0.909) (0.110 ± 0.050 mm and 0.113 ± 0.057 mm, respectively) (Fig. 4). The variance of the mean linear PE wear rates did not differ (Levene’s test, p = 0.309) between the two groups. Wide distribution of PE wear values occurred in the NHC and HHC groups (Fig. 5).
Fig. 4.
The mean linear PE wear rates of cups placed at different positions (NHC versus HHC) are shown.
Fig. 5.
The variance of the mean linear PE wear rate, which does not differ (Levene’s test, p = 0.309) between the NHC and HHC group, and the wide distribution of PE wear values in the NHC and HHC groups are shown. The error bars represent the SD of the mean.
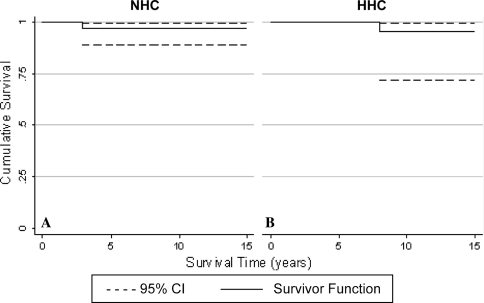
The Kaplan-Meier cup survivorship rates with revision for any reason as an event of interest were similar (p = 0.979) in the NHC and HHC groups (97.2% [95% confidence interval, 88.5%–99.3%] and 97.1% [95% confidence interval, 73.8%–99.3%], respectively) (Fig. 6). Migration of the cup from the postoperative position occurred in two hips: one in a patient with high hip dislocation in which the cup was placed in a NHC position and the metal-on PE cup migrated by 3 years postoperatively; and the other in a patient with hip dysplasia that was accompanied by excessive varus femoral neck deformity with the HHC position in which the metal-on-metal cup was loosened by 8 years postoperatively. This patient had an ipsilateral thigh allergic skin reaction, and severe periacetabulum osteolysis was seen on radiographs. In another patient with a NHC metal-on-metal cup, progressive periprosthetic osteolysis was not accompanied by cup or stem migration. The cup was changed to ceramic-on-PE with an insert and metallic head change and the patient’s hip remains stable 7 years postoperatively after periprosthetic new bone formation.
Fig. 6A–B.
The Kaplan-Meier cup survivorship rates with revision for any reason as an event of interest for the NHC and HHC groups are shown. CI = confidence interval.
Discussion
There is no consensus regarding the value of the HHC technique in cases of deficient acetabulum. In this study, we assessed and compared the PE wear rates and survivorship of cups placed in a HHC with those placed at a more anatomic hip center in patients with arthritis secondary to congenital hip disease.
We must note several limitations to our study design. We have an insufficient number of patients with a high congenital hip dislocation in the study. Another problem, one that exists in all similar studies, is that periacetabular chronic myoskeletal abnormalities between patients sometimes were completely different, especially in patients with a unilateral high dislocation, which presented a different degree of pelvis tilting, lumbar spine deformity, and muscle contracture for each patient. Another limitation to our study is that we used two different lateral approaches: Harding’s more extended approach for high congenital dislocation and the not extended to vastus lateralis approach of Thomine et al. [36] for hips with low dislocation or dysplasia.
Our Zweymüller® threaded cups placed superiorly or superolaterally did not show higher rates of PE wear or mechanical loosening than cups placed at the near-true acetabulum at a mean followup of 8.6 ± 3.5 years (range, 2–15 years).
In the majority of the HHC hips, the cup insert, inclinated or not, was placed at normal abduction and flexion even in hips without full osseous cranial coverage of the metal shell. The low rates of mechanical cup failure in our HHC hips are in accordance with the clinical results of the HHC technique reported by others [1, 5, 7, 10, 13, 15, 21, 23, 32, 34, 35]. In contrast, Chougle et al. [4], estimated cup survival for hips with high congenital dislocation reconstructed at the NHC position was only 12% at 20 years.
The lack of difference in linear PE wear rate and variance between the NHC and HHC groups and the wide distribution of PE wear values in both groups are in accordance with the results of studies that found not only the hip center is responsible for PE wear in a hip arthroplasty but also numerous other factors, such as cup inclination, articulating surfaces, femoral head size, and patient age or body weight [16, 17, 20, 23, 24, 38].
The low rates of mechanical cup failure in our series using the HHC technique and Zweymüller® cups placed at a high nonanatomic position are in accordance with the results reported by others concerning good stability and minimal osteolysis of these cups in series including cranial cup uncovered cases [2, 11, 22, 26, 27, 31, 33, 39, 40]. It seems, using this technique, successful acetabular reconstruction with a hip center that is functional and adaptable to all chronic peripelvic myoskeletal deformities, even at a higher than normal position, can be obtained in hips with osteoarthritis secondary to congenital hip disease. The HHC technique including stable Zweymüller® cup fixation in a healthy osseous region without femoral shortening osteotomies, bone grafts, or soft tissue injuries, in combination with suitable head/neck length, suitable stem position, and adequate gluteus medius tensioning, gives results similar to those of the near-true acetabular reconstruction concerning PE wear rates, mechanical cup survival, hip stability, Trendelenburg gait, and leg length restoration without excessive traction, muscle injuries, or neurologic complications. By using longer head/neck lengths, impingement also can be avoided. The HHC technique using a Zweymüller® threaded cup seems to be a valuable alternative solution in some difficult cases of osteoarthritis secondary to congenital hip disease with minimal complications and excellent clinical results.
Acknowledgments
We thank Ageliki Stavrianou, MD, Thomas Georgas, MD, Theodoros Papaioannou, PhD, Christos Sdrenias, MD, Georgios Salagiannis, MD, for help in preparing this manuscript.
Footnotes
Each author certifies that he has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Department of Orthopaedics, Karpenissi General Hospital.
References
- 1.Bozic KL, Freiberg AA, Harris WH. The high hip center. Clin Orthop Relat Res. 2004;420:101–105. doi: 10.1097/00003086-200403000-00014. [DOI] [PubMed] [Google Scholar]
- 2.Büttner-Janz K, Jessen N, Hommel H. [Acetabular component implantation in coxarthrosis due to dysplasia after high congenital hip dislocation] [in German] Chirurg. 2000;71:1374–1379. doi: 10.1007/s001040051229. [DOI] [PubMed] [Google Scholar]
- 3.Carls J, Wirth CJ, Börner C, Pape A. [Changes of biomechanical parameters in dysplasia of the hip by total hip replacement] [in German] Z Orthop Ihre Grenzgeb. 2002;140:527–532. doi: 10.1055/s-2002-33999. [DOI] [PubMed] [Google Scholar]
- 4.Chougle Α, Hemmady MV, Hodgkinson JP. Severity of hip dysplasia and loosening of the socket in cemented total hip replacement: a long-term follow-up. J Bone Joint Surg Br. 2005;87:16–20. [PubMed] [Google Scholar]
- 5.Dearborn JT, Harris WH. High placement of an acetabular component inserted without cement in a revision hip arthroplasty: results after a mean of ten years. J Bone Joint Surg Am. 1999;81:469–480. doi: 10.2106/00004623-199904000-00004. [DOI] [PubMed] [Google Scholar]
- 6.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 7.Delp SL, Wixson RL, Komattu AV, Kocmond JH. How superior placement of the joint center in hip arthroplasty affects the abductor muscles. Clin Orthop Relat Res. 1996;328:137–146. doi: 10.1097/00003086-199607000-00022. [DOI] [PubMed] [Google Scholar]
- 8.Doehring TC, Rubash HE, Shelley FJ, Schwendeman LJ, Donaldson TK, Navalgund YA. Effect of superior and superolateral relations of the hip center on hip joint forces: an experimental and analytical analysis. J Arthroplasty. 1996;11:693–703. doi: 10.1016/S0883-5403(96)80008-8. [DOI] [PubMed] [Google Scholar]
- 9.Flecher X, Parratte S, Brassart N, Aubaniac JM, Argenson JN. Evaluation of the hip center in total hip arthroplasty for old developmental dysplasia. J Arthroplasty. 2008;23:1189–1196. doi: 10.1016/j.arth.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 10.Fousek J, Indrakova P. [Total hip arthroplasty in post-dysplastic hip arthritis: can type and position of the acetabular component influence longevity of the prosthesis?] [in Czech] Acta Chir Orthop Traumatol Cech. 2007;74:47–54. [PubMed] [Google Scholar]
- 11.Garcia-Cimbrelo E, Cruz-Pardos A, Madero R, Ortega-Andreu M. Total hip arthroplasty with use of the cementless Zweymüller Alloclassic system: a ten to thirteen-year follow-up study. J Bone Joint Surg Am. 2003;85:296–303. doi: 10.2106/00004623-200302000-00017. [DOI] [PubMed] [Google Scholar]
- 12.Geerdink CH, Grimm B, Vencken W, Heyligers IC, Tonino AJ. The determination of linear and angular penetration of the femoral head into the acetabular component as an assessment of wear in total hip replacement: a comparison of four computer-assisted methods. J Bone Joint Surg Br. 2008;90:839–846. doi: 10.1302/0301-620X.90B7.20305. [DOI] [PubMed] [Google Scholar]
- 13.Gustke ΚA. Jumbo cup or high hip center: is bigger better? J Arthroplasty. 2004;19:120–123. doi: 10.1016/j.arth.2004.02.012. [DOI] [PubMed] [Google Scholar]
- 14.Hartofilakidis G, Stamos K, Karachalios T, Ioannidis TT, Zacharakis N. Congenital hip disease in adults: classification of acetabular deficiencies and operative treatment with acetabuloplasty combined with total hip arthroplasty. J Bone Joint Surg Am. 1996;78:683–692. doi: 10.2106/00004623-199605000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Hendricks KJ, Harris WH. High placement of noncemented acetabular components in revision total hip arthroplasty: a concise follow-up, at a minimum of fifteen years, of a previous report. J Bone Joint Surg Am. 2006;88:2231–2236. doi: 10.2106/JBJS.E.00247. [DOI] [PubMed] [Google Scholar]
- 16.Hirakawa K, Mitsugi N, Koshino T, Saito T, Hirasawa Y, Kubo T. Effect of acetabular cup position and orientation in cemented total hip arthroplasty. Clin Orthop Relat Res. 2001;388:135–142. doi: 10.1097/00003086-200107000-00020. [DOI] [PubMed] [Google Scholar]
- 17.Ito M, Tokunaga K, Endo N, Takano Y, Yuasa N. The effect of cup placement in cementless total hip arthroplasty on the wear rate of polyethylene. Orthopedics. 2008;31:225. doi: 10.3928/01477447-20080301-19. [DOI] [PubMed] [Google Scholar]
- 18.Johnston RC, Brand RA, Crowninshield RD. Reconstruction of the hip: a mathematical approach to determine optimum geometric relationships. J Bone Joint Surg Am. 1979;61:639–652. [PubMed] [Google Scholar]
- 19.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. doi: 10.2307/2281868. [DOI] [Google Scholar]
- 20.Kligman M, Michael H, Roffman M. The effect of abduction differences between cup and contralateral acetabular angle on polyethylene component wear. Orthopedics. 2002;25:65–67. doi: 10.3928/0147-7447-20020101-18. [DOI] [PubMed] [Google Scholar]
- 21.Kobayashi S, Saito N, Nawata M, Horiuchi H, Iorio R, Takaoka K. Total hip arthroplasty with bulk femoral head autograft for acetabular reconstruction in developmental dysplasia of the hip. J Bone Joint Surg Am. 2003;85:615–621. doi: 10.2106/00004623-200304000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Kou B, Perner K, Yuan Y. [Primary Zweymuller total hip arthroplasty for osteoarthritis secondary to congenital acetabular dysplasia] [in Chinese] Zhonghua Wai Ke Za Zhi. 2001;39:623–625. [PubMed] [Google Scholar]
- 23.ΜacKenzie JR, Kelley SS, Johnston RC. Total hip replacement for coxarthrosis secondary to congenital dysplasia and dislocation of the hip: long-term results. J Bone Joint Surg Αm. 1996;78:55–61. doi: 10.2106/00004623-199601000-00008. [DOI] [PubMed] [Google Scholar]
- 24.Oki H, Ando M, Omori H, Okumura Y, Negoro K, Uchida K, Bada H. Relation between vertical orientation and stability of acetabular component in the dysplastic hip simulated by nonlinear three-dimensional finite element method. Artif Οrgans. 2004;28:1050–1054. doi: 10.1111/j.1525-1594.2004.00017.x. [DOI] [PubMed] [Google Scholar]
- 25.Pagnano W, Hanssen AD, Lewallen DG, Shaughnessy WJ. The effect of superior placement of the acetabular component on the rate of loosening after total hip arthroplasty. J Bone Joint Surg Am. 1996;78:1004–1014. doi: 10.2106/00004623-199607000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Perka C, Fischer U, Taylor WR, Matziolis G. Developmental hip dysplasia treated with total hip arthroplasty with a straight stem and a threaded cup. J Bone Joint Surg Am. 2004;86:312–319. doi: 10.2106/00004623-200402000-00014. [DOI] [PubMed] [Google Scholar]
- 27.Pospischill M, Knahr K. Cementless total hip arthroplasty using a threaded cup and a rectangular tapered stem: follow-up for ten to 17 years. J Bone Joint Surg Br. 2005;87:1210–1215. doi: 10.1302/0301-620X.87B9.16107. [DOI] [PubMed] [Google Scholar]
- 28.Ranawat CS, Dorr LD, Inglis AE. Total hip arthroplasty in protrusio acetabuli of rheumatoid arthritis. J Bone Joint Surg Am. 1980;62:1059–1065. [PubMed] [Google Scholar]
- 29.Ranawat CS, Rao RR, Rodriguez JA, Bhende HS. Correction of limb-length inequality during total hip arthroplasty. J Arthroplasty. 2001;16:715–720. doi: 10.1054/arth.2001.24442. [DOI] [PubMed] [Google Scholar]
- 30.Ranawat CS, Rodriguez JA. Functional leg-length inequality following total hip arthroplasty. J Arthroplasty. 1997;12:359–364. doi: 10.1016/S0883-5403(97)90190-X. [DOI] [PubMed] [Google Scholar]
- 31.Reigstad O, Siewers P, Røkkum M, Espehaug B. Excellent long-term survival of an uncemented press-fit stem and screw cup in young patients: follow-up of 75 hips for 15–18 years. Acta Orthop. 2008;79:194–202. doi: 10.1080/17453670710014978. [DOI] [PubMed] [Google Scholar]
- 32.Russotti GM, Harris WH. Proximal placement of the acetabular component in total hip arthroplasty: a long-term follow-up study. J Bone Joint Surg Am. 1991;73:587–592. [PubMed] [Google Scholar]
- 33.Schröder JH, Matziolis G, Tuischer J, Leutloff D, Duda GN, Perka C. The Zweymüller threaded cup: a choice in revision? Migration analysis and follow-up after 6 years. J Arthroplasty. 2006;21:497–502. doi: 10.1016/j.arth.2005.05.029. [DOI] [PubMed] [Google Scholar]
- 34.Sutherland CJ. Treatment of type III acetabular deficiencies in revision total hip arthroplasty without structural bone-graft. J Arthroplasty. 1996;11:91–98. doi: 10.1016/S0883-5403(96)80166-5. [DOI] [PubMed] [Google Scholar]
- 35.Tanzer M. Role and results of the high hip center. Orthop Clin North Am. 1998;29:241–247. doi: 10.1016/S0030-5898(05)70322-9. [DOI] [PubMed] [Google Scholar]
- 36.Thomine JM, Duparc F, Dujardin F, Biga N. [Transgluteal approach to the hip by anterior hemimyotomy of the gluteus medius] [in French] Rev Chir Orthop Reparatrice Appar Mot. 1999;85:520–525. [PubMed] [Google Scholar]
- 37.Vasavada AN, Delp SL, Maloney WJ, Schurman DJ, Zajac FE. Compensating for changes in muscle length in total hip arthroplasty: effects on the moment generating capacity of the muscles. Clin Orthop Relat Res. 1994;302:121–133. [PubMed] [Google Scholar]
- 38.Wan Z, Boutary M, Dorr LD. The influence of acetabular component position on wear in total hip arthroplasty. J Arthroplasty. 2008;23:51–56. doi: 10.1016/j.arth.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 39.Zweymüller KA, Lintner FK, Semlitsch MF. Biologic fixation of a press-fit titanium hip joint endoprosthesis. Clin Orthop Relat Res. 1988;235:195–206. [PubMed] [Google Scholar]
- 40.Zweymüller KA, Steindl M, Schwarzinger U. Good stability and minimal osteolysis with a biconical threaded cup at 10 years. Clin Orthop Relat Res. 2007;463:128–137. [PubMed] [Google Scholar]