Abstract
Background
Greater trochanteric pain syndrome can be severely debilitating. Ideal imaging modalities are not established, treatments are not reliably evaluated, and the underlying pathology is not well understood.
Questions/purposes
Using surgical and histopathology findings as a gold standard, we therefore determined the positive predictive value of preoperative ultrasound assessment for greater trochanteric pain syndrome recalcitrant to nonoperative management. In addition, we report the outcomes of gluteal tendon reconstructive surgery using validated clinical and functional outcome tools and evaluate the contribution of the tendon and bursa to greater trochanteric pain syndrome.
Patients and Methods
We reviewed 24 patients who had combined gluteal tendon reconstruction and bursectomy. Preoperative ultrasound imaging was compared with surgical findings. In the absence of a greater trochanteric pain syndrome specific outcome tool, surgical outcomes for pain and function were assessed via a 100-mm visual analog scale, the modified Harris hip score, and the Oswestry Disability Index. Strength also was measured. The tendon and bursa tissue collected at surgery was histopathologically reviewed.
Results
In our small study, ultrasound had a high positive predictive value for gluteal tendon tears (positive predictive value = 1.0). Patients reported high levels of pain relief and function after surgery; tendon and bursa showed pathologic changes.
Conclusions
Ultrasound appears to be clinically useful in greater trochanteric pain syndrome; reconstructive surgery seems to relieve pain and the histopathologic findings show tendinopathy and bursa pathology coexist in greater trochanteric pain syndrome.
Level of Evidence
Level IV, case series. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Greater trochanteric pain syndrome (GTPS) has been associated with trochanteric bursitis and gluteus medius tendon tears, being likened to the pathologic features associated with supraspinatus tendinopathy and subacromial bursitis [7, 18, 23, 30]. Various surgical options have been reported for patients who no longer respond to nonoperative treatment. These include bursectomy [2, 14, 15, 44], iliotibial band release [14, 16, 35, 40], and surgical reconstruction of the tendons [11, 23, 30, 43], frequently in combination [11, 30, 43]. Imaging [9, 26, 34] and surgical [10, 28, 30, 34] observations implicating the tendons and bursae in the clinical syndrome have been reported.
The histopathologic features of structures around the greater trochanteric region have not been thoroughly described. One study reported histopathologic evidence of tendinopathy in five gluteus medius tendon specimens retrieved at surgery for this condition [9]. Another study [39] presented the findings of four people having hip arthroplasties, two of whom were symptomatic for trochanteric bursitis (according to the criteria of Ege Rasmussen and Fanø [13]). That study reported no difference in the histopathology of the two groups. We are unaware of any reports describing the histopathologic findings for the tendon and bursa from patients who have had surgery for gluteal tendon reconstruction.
Definitive diagnostic criteria have not been established for GTPS. Authors report lateral thigh pain as the most common complaint [18, 24, 27, 29, 31, 32, 42], and pain on palpation of the greater trochanter [13, 18, 24, 27, 29, 31, 32, 42]. Inconsistent findings for passive ROM have been reported; for example, Anderson [1] reported pain was variable and present in one or more of end range internal rotation, external rotation, abduction, and adduction. Similarly, resisted muscle tests have been advocated; however, their value is questionable as pain may not be elicited at all [1]. In addition, the Faber test was advocated in two studies [13, 18] and the relocation test and single-leg stance test in another [31].
Ultrasound assessment is used increasingly to aid musculoskeletal diagnosis [16, 17, 22] but has yet to be fully validated in GTPS. Variation in echo texture and hypoechogenicity noted on ultrasound imaging had been interpreted as tendinosis and tears. Variation in tendon size, and calcification and fluid pooling in the bursa, also have been reported [9]. In that study, surgery confirmed the ultrasound tendon findings in 22 of 53 cases, but the authors do not report any surgical or histologic bursa findings [9].
Studies reporting gluteal tendon reconstruction suggest high percentages of participants have complete resolution of symptoms; however, these studies have small sample sizes (n = 7–10) and limited use of validated outcome tools in the assessment of these interventions [11, 23, 30, 43].
Therefore, our study had three aims: (1) to calculate the sensitivity and positive predictive value of preoperative ultrasound assessment for GTPS; (2) to report the outcomes of gluteal tendon reconstructive surgery using validated clinical and functional outcome tools; and (3) to describe the histopathologic features of tendon and bursa specimens collected at the time of reconstructive surgery.
Patients and Methods
We contacted all 24 patients who underwent combined gluteal tendon reconstruction and bursectomy between February 2004 and February 2007. Patients had surgical reconstruction if there was evidence of tendon tears on imaging (in 17 patients the diagnosis was made with ultrasound and eight patients had a confirmatory MRI), and when nonoperative methods of treatment (ultrasound-guided corticosteroid injection and physical therapy) no longer provided pain relief. All 24 patients were female. The mean duration of symptoms at surgery was 33.8 months (range, 3–120 months). Baseline demographics, imaging results, and surgical findings were available for all patients. The mean age of the patients at the time of surgery was 56 years (range, 38–76 years). Of the 24 patients recalled for followup, 19 were available for assessment: two patients had revision tendon reconstructive surgery having torn the previously reconstructed gluteal tendons, two patients were lost to followup having moved without a forwarding address, and one declined to participate in the study. The minimum postoperative followup was 12 months (mean, 22 months; range, 12–56 months). Ethics approval was given by The Australian National University, ACT Health, Calvary Health Care ACT, and Deakin University human research ethics committees.
Before surgery, ultrasound examination of the greater trochanteric region was performed in all patients by a specialist in the field (WC [20 patients], BF [three patients], ID [one patient]). All examinations were performed on a Philips 5000 machine (Philips Healthcare; Andover, MA) with a 7-MHz probe. Patients lay in the lateral position with their hips and knees extended. Gel was applied and the probe was moved over the gluteal muscles, tendons, and greater trochanter ensuring the ultrasound beam remained at 90° to the tissues being examined. Confirmation of anatomy was achieved by the patient performing appropriate resisted movements. Tears were confirmed by injecting a small amount of air between the tendon planes.
Surgery was performed with the patient in the lateral position, using a direct lateral approach. The gluteus maximus was retracted, and the trochanteric bursa was exposed, evaluated, and then removed. The muscle and tendon of the gluteus medius then were identified and any defect in the tendon noted. The tendon (at the site of the tear) then was dissected from the greater trochanter, exposing the gluteus minimus musculotendinous unit, which likewise was assessed for integrity. In the absence of a gluteus medius tear, the gluteus minimus was inspected via a split in the gluteus medius over the minimus insertion. Defects were débrided back to healthy tissue. When the defect was near the enthesis, the greater trochanter was decorticated back to bleeding bone. Bursal tissue was collected during dissection of the lateral structures. Tendon tissue was collected during débridement of the tear. Tissue specimens were immediately placed in 10% buffered formalin. From the 24 people who had surgery, 16 tendon and 18 bursa specimens were available for examination. The gluteal muscles were reattached in an anatomic fashion using Number 5 Ethibond® modified Kessler-type sutures (Ethicon, Inc, Somerville, NJ) via transosseous tunnels. The fascia lata was closed completely. The wound then was closed in layers.
Postoperative management included nonweightbearing on the affected leg using crutches or a wheelchair for 6 weeks; weightbearing then progressed by approximately 25% of body weight per week. Strength training commensurate with the level of weightbearing was initiated at this time. Weightbearing and exercise progression were subject to strength return and pain management. Patients were encouraged to continue using a gait aid until they could walk without a limp. Rehabilitation was supervised by a physical therapist.
Patients were reviewed by the surgeon (PS) at 6 weeks and 6 months postoperatively, unless there was an indication (eg, lack of progress or increasing pain) to see them sooner. All patients, excluding those who had retorn tendons as observed on ultrasound or MRI and confirmed at revision surgery, were invited to attend a review of their status done by an independent assessor not associated with the surgery (AF). A set protocol that covered preoperative and postoperative history, functional scores, and a physical examination was performed. The patient completed a 100-mm visual analog scale (VAS) for recalled preoperative worst pain levels and current worst pain levels [25]. We chose to use two outcome measures that have face validity for assessment of GTPS: the Oswestry Disability Index (ODI) [3, 37, 38, 45] and the modified Harris hip score (HHS) [3, 11, 35, 40]. Strength of abduction, adduction, and internal and external rotation for both hips was measured via a calibrated handheld dynamometer (HHD) (Chatillon® MSC series medical dynamometer; Chatillon Force Measurement Systems, Largo, FL). Abduction and adduction were measured with the patient supine with the HHD positioned immediately proximal to the lateral (abduction) and medial (adduction) femoral condyle. Internal rotation and external rotation were measured with the patient prone with the knee at 90° flexion. The HHD was positioned immediately proximal to the medial (external rotation) or lateral (internal rotation) malleolus. Three submaximal trial tests were performed to ensure the patient understood the test. After this, the results of the best of three tests were recorded [5]. Additionally, gluteal strength was assessed via the Trendelenburg sign using the protocol of Hardcastle and Nade [19]. The patient stood on the affected leg, the other leg lifted to 90° hip flexion and the pelvis held level, with shoulders aligned over the pelvis, and the position maintained for a maximum of 30 seconds. The contralateral leg was used as a control for all measures in this study. Pain, ODI, and HHS assessments were completed for all 19 patients included with the minimum followup; strength and Trendelenburg testing were completed for 18 of the 19 patients.
Preoperative ultrasound reports were accessed. The presence or not of tendon tears and bursa pathology was rated dichotomously, and the result then was compared with surgical observations for the tendon and histopathology for the bursa. In 15 of the 24 patients, tendon and bursa tissue from the same patient was available for histologic examination. In five patients, only bursa tissue was available and in two patients only tendon tissue was available. Hematoxylin and eosin staining was done of all specimens. Histopathologic analysis of tendon and bursa tissue taken during surgery was provided by a pathologist (JT). Findings were reported as degenerative tendinosis, acute tendinitis, or normal for the tendons and as degenerative bursa pathology, acute bursitis, or normal for the bursa. These findings were rated as normal or abnormal based on the worst pathologic features viewed.
Descriptive statistics were used for demographic information. We computed sensitivity and positive predictive values for ultrasound (tendon tear present or absent) based on surgical reports of tears (tear present or absent). We then computed sensitivity and positive predictive values for ultrasound bursa findings (pathology present or absent) based on histology (pathology present or absent), using a two-by-two contingency table in each case. Recalled preoperative and recorded postoperative pain and side-to-side strength results were compared with the Wilcoxon signed-rank test. ODI scores were inverted so that higher scores reflected better outcome for comparison to the HHS.
Results
Based on surgical findings in this cohort of symptomatic patients in whom nonoperative management had failed, ultrasound had a sensitivity of 0.79 and a positive predictive value of 1 of diagnosing a tear of either tendon. Based on the histology and ultrasound findings (n = 15), ultrasound has a sensitivity of 0.61, a specificity of 1.0, a positive predictive value of 1.0, and a negative predictive value of 1.0 of diagnosing bursa pathology (Table 1). An isolated gluteus medius tear was reported on ultrasound in 15 of the 24 patients, an isolated gluteus minimus tear in no patients, and tears in both tendons in four patients. The remaining five patients were reported to have tendinopathy in the gluteus medius and gluteus minimus (two) or tendinopathy in the gluteus medius and normal in the gluteus minimus (three). Ultrasound examination of the bursa was reported in 20 of the 24 patients. Sixteen reportedly had increased fluid or thickening, four were reported as normal, and in four instances the report contained no comment on the bursa. At surgery, tendon tears were reported in all 24 patients, the majority of cases (n = 18) having a tear of the gluteus medius and minimus tendons. One patient had an isolated tear of the gluteus medius tendon and three patients had an isolated tear of the gluteus minimus tendon. In two patients, the status of the gluteus minimus tendon was not reported. Abnormality of the bursa was reported in 11 patients.
Table 1.
Preoperative ultrasound and surgical findings, the presence of tissue samples, and clinical review
| Patient | Ultrasound either tendon | Ultrasound bursa | Surgery Gmed | Surgery Gmin | Surgery bursa | Tissue specimens tendon | Tissue specimens bursa | Clinical review |
|---|---|---|---|---|---|---|---|---|
| 1 | Tr | Abn | Tr | Tr | Abn | NS | NS | ✓ |
| 2 | Tr | Abn | Tr | NR | Abn | ✓ | ✓ | ✓ |
| 3 | Tr | Abn | Tr | Tr | NR | ✓ | ✓ | ✓ |
| 4 | Tr | Abn | Tr | Tr | NR | ✓ | ✓ | ✓ |
| 5 | Tr | Abn | Tr | Tr | Abn | ✓ | ✓ | ✓ |
| 6 | Tr | Abn | Tr | Tr | NR | ✓ | ✓ | ✓ |
| 7 | Tr | NR | Tr | Tr | NR | ✓ | NS | ✓ |
| 8 | Tr | NR | Tr | Tr | Abn | ✓ | ✓ | ✓ |
| 9 | Tr | Abn | Tr | Tr | Abn | ✓ | ✓ | ✓ |
| 10 | Tn | NAD | NT | Tr | Abn | NS | ✓ | ✓ |
| 11 | Tn | NAD | Tr | Tr | NAD | NS | ✓ | ✓ |
| 12 | Tn | Abn | NT | Tr | NR | ✓ | ✓ | ✓ |
| 13 | Tn | Abn | Tr | Tr | NR | ✓ | ✓ | ✓ |
| 14 | Tr | Abn | Tr | NT | Abn | ✓ | ✓ | Lost |
| 15 | Tr | Abn | NT | Tr | Abn | NS | NS | ✓ |
| 16 | Tr | NR | Tr | Tr | Abn | ✓ | ✓ | ✓ |
| 17 | Tr | NR | Tr | Tr | NAD | ✓ | ✓ | ✓ |
| 18 | Tr | Abn | Tr | Tr | NR | NS | ✓ | Retear |
| 19 | Tr | Abn | Tr | Tr | NR | ✓ | ✓ | Retear |
| 20 | Tr | Abn | Tr | Tr | NR | NS | ✓ | ✓ |
| 21 | Tr | Abn | Tr | Tr | Abn | ✓ | NS | ✓ |
| 22 | Tr | Abn | Tr | Tr | NR | ✓ | ✓ | ✓ |
| 23 | Tn | NAD | Tr | Tr | NR | NS | ✓ | Lost |
| 24 | Tr | NAD | Tr | NR | Abn | ✓ | ✓ | Declined |
| No report | 0 | 4 | 0 | 2 | 11 | 5 | ||
| Any pathology | 24 | 16 | 21 | 21 | 11 | 16 | 18 | |
| Total | 24 | 24 | 24 | 24 | 24 | 16 | 18 | 19 |
Gmed = gluteus medius; Gmin = gluteus minimus; Tr = tear; Tn = tendinosis; NT = no tear; Abn = any abnormality; NR = not reported; NAD = no apparent deformity; NS = no specimen; ✓ = specimen or clinical review was collected or performed.
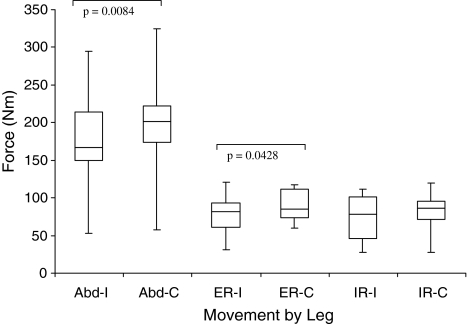
Nineteen patients reported less pain after surgery and good to excellent levels of function (Soderman and Malchau [41]) (Table 2). Pain decreased from a median recalled preoperative worst pain of 85 mm (interquartile range [IQR], 75–100 mm) to 9 mm (IQR, 0–25 mm) postoperatively, resulting in a median improvement in pain of 71 mm (IQR, 50–92) (p = 0.0002). The median HHS postoperatively was 74 (IQR, 59–85) and the median ODI was 82 (IQR, 74–92). The dynamometry measures (n = 18) showed abduction and external rotation for the ipsilateral leg were weaker than for the contralateral leg (p = 0.0084 and p = 0.0428, respectively; Wilcoxon signed-rank test) (Fig. 1). Based on the Trendelenburg sign patients were able to stand on the surgically treated leg for a shorter time (p = 0.009) than on the contralateral leg (median, 15 seconds [IQR, 7.0–30.0 seconds] versus median, 30 seconds [IQR, 15–30 seconds], respectively).
Table 2.
Outcomes of surgery for reconstruction of greater trochanter pain syndrome were recorded at review (n = 19)
| Patient rank | Pain difference* | Satisfaction | HHS | ODI |
|---|---|---|---|---|
| 1 | −100 | 100 | 82 | 86 |
| 2 | −100 | 100 | 82 | 96 |
| 3 | −99 | 100 | 85 | 86 |
| 4 | −92 | 83 | 74 | 80 |
| 5 | −92 | 76 | 75 | 92 |
| 6 | −80 | 90 | 62 | 74 |
| 7 | −77 | 85 | 59 | 78 |
| 8 | −76 | 100 | 88 | 70 |
| 9 | −71 | 100 | 85 | 82 |
| 10 | −68 | 68 | 67 | 78 |
| 11 | −65 | 69 | 65 | 84 |
| 12 | −65 | 90 | 85 | 92 |
| 13 | −60 | 78 | 57 | 68 |
| 14 | −50 | 50 | 56 | 72 |
| 15 | −50 | 100 | 84 | 98 |
| 16 | −47 | 61 | 73 | 86 |
| 17 | −10 | 70 | 40 | 60 |
| 19 | 16 | 74 | 58 | 76 |
* Patients were ranked by the difference between recalled preoperative and postoperative pain; all but two patients had a clinically significant improvement in pain levels (p = 0.0002) [6]; HHS = Harris hip score; ODI = Oswestry Disability Index.
Fig. 1.
Hip abduction and external rotation strength are weaker (p = 0.0084 and p = 0.0428, respectively) on the ipsilateral compared with the contralateral leg at a minimum of 12 months postoperatively. Abd-I = hip abduction ipsilateral; Abd-C = hip abduction contralateral; ER-I = hip external rotation ipsilateral; ER-C = hip external rotation contralateral; IR-I = hip internal rotation ipsilateral; IR-C = hip internal rotation contralateral. The box represents the interquartile (middle 50%) of the range, the horizontal line across the box represents the median score, and the whiskers represent the upper and lower quartiles.
Degenerative changes were reported in all tendons. There was no report of normal tendon or acute tendinitis. Degenerative changes were reported for all 18 bursa specimens. There was no report of normal bursa or acute bursitis.
Discussion
Ultrasound imaging, although commonly used clinically for many conditions, has limited evidence to support its use in GTPS [9]. Surgical reconstruction of the gluteal tendons has been reported as being effective for pain relief in patients who no longer respond to nonoperative treatment; however, the inconsistent use of, and in some cases complete lack of validated outcome tools, means the results are difficult to interpret [11, 30, 43]. Finally, the underlying comparative pathologic features of the tendons and bursa about the greater trochanter, to our knowledge, have not been reported for GTPS, limiting the understanding of the pathology. We therefore (1) calculated the sensitivity and positive predictive value of preoperative ultrasound assessment for GTPS, (2) reported the outcomes of gluteal tendon reconstructive surgery using validated clinical and functional outcome tools, and (3) reported the histopathologic features of tendon and bursa specimens collected at the time of reconstructive surgery.
This retrospective study has several limitations. First, the lack of a control group prevented calculation of meaningful ultrasound sensitivity and specificity. The false-positive aspect of this calculation was underrepresented, and the prevalence of GTPS overrepresented. This study does not provide information regarding the number of patients who may have tendon or bursa pathology that is not observed by ultrasound, as patients had to have a positive ultrasound for tendon tear to be included for surgery.
Second, the lack of a control group prevented a comparison with normal tendon and bursa histology; however, normal morphologic features of tendon and bursa are well known. Although one experienced musculoskeletal pathologist examined all of our histologic specimens, we did not perform intrarater reliability testing for assessment of the histopathology. Third, the lack of preoperative data limits comparison with postoperative status. We used recalled pain and strength in the contralateral leg for comparison instead. Reporting recalled pain may be inaccurate, as pain can be difficult to describe and assess, and recalled pain may be influenced by worst pain experience [21, 36]. However, two short-term studies suggest recalled pain reliably reflects previous pain [6, 20]; additionally, our cohort reported pain levels similar to reported levels [11, 30]. The Trendelenburg sign is widely used clinically and in research to assess hip function. However, pain and poor balance have been identified as confounders of this test [19]; we used dynamometry to confirm the results of the Trendelenburg test.
We found ultrasound had a high positive predictive value for gluteal tendon tears documented at surgery in select patients, which is comparable to that reported for shoulder rotator cuff injury [12, 33]. The only other study of ultrasound imaging for GTPS did not report the positive predicative value and was not able to report the sensitivity, because like us, they did not have a surgical control group. They did not report on bursa findings at surgery or on histopathology [9]. In studies that have used MRI or ultrasound to differentiate between gluteus medius and minimus pathology, including ours, imaging gluteus minimus pathology has been underreported when compared with the surgical findings [4, 8, 9, 23, 26, 30, 34].
We found the surgical reconstructive procedure resulted in a reduction of pain and good function (based on the HHS results). Surgical outcomes from our patients are similar to those in the four other studies reporting outcomes: one retrospective case series [23] and three prospective series [11, 30, 43]. These papers reported remission of pain and return to function but with inconsistent use of standardized tools for patient assessment. Improvements in the HHS of 46 to 82 have been reported [11]. In five of eight cases, “complete remission” was reported by Lequesne et al. [30] and in 10 of 10 cases by Voos et al. [43]. Surgical outcomes are affected by inclusion and exclusion criteria and surgical technique. All studies included patients who were nonresponsive to nonoperative treatment for GTPS. Exclusion criteria were not reported for three studies [11, 23, 43]. Our study and that of Lequesne et al. [30] used similar surgical techniques; a description was not provided by Kagan [23]. One study reported on iliotibial band “Z” lengthening and repair of torn tendons when found; however, the authors did not report the incidence of these tears [11]. The same study reported an incidence of revision surgery similar to that in our patients. We reoperated on two patients: one was receiving long-term oral steroids, and the other was a long-term smoker who was noncompliant with postoperative rehabilitation. The fourth study reports repairs of the tendons in combination with multiple procedures to the hip [43].
We found, based on the gold standard of histopathology, the tendon and the bursa were affected in this select group of patients with GTPS. To our knowledge, previous published histopathology data are limited to one series of five tendon specimens [9] and one series of bursa specimens from two symptomatic and two control patients [39]. We were able to compare tendon and bursa from the same patients.
To assess the effectiveness of an intervention, tools designed and validated for the disease provide the most reliable results. In the absence of a disease-specific tool, we used the HHS, validated for hip arthritis, and the ODI, validated for low back and leg pain. We also used the Trendelenburg test, which has limitations as mentioned above [19]. The functional tests developed and used by Lequesne et al. [31] included a pain-dependent single-leg stance test (not the Trendelenburg test), providing a sensitivity and specificity of 100% and 97.3%, respectively, for tendon tear confirmed at surgery. This promising assessment tool would benefit from independent validation.
We confirm the findings of Connell et al. [9] that gluteal tendon tears are observed by ultrasound examination in this population; additionally, we found bursa pathology is seen on ultrasound. We confirm previous findings, using validated tools, that reconstructive surgery for GTPS is likely to reduce pain and provide patients with a good level of function. The histopathology of tissue specimens associated with GTPS strongly suggests there was gluteal tendinopathy with associated bursa degeneration. There was no evidence of ongoing acute bursitis. Therefore, we believe treatment should address the tendinopathy as a primary goal. Future research should include a randomized controlled trial assessing the long-term benefits of nonoperative treatments (corticosteroid injection and physical therapy) compared with surgical treatment and a randomized controlled trial comparing surgical methods using standardized and validated assessment tools.
Acknowledgments
We thank Sarah Tobin, Wes Cormick, Teresa Neeman, Keith Dear, Jane Twin, Simon Gallant, Barry Flynn, Ian Duncan, and the patients.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
The surgery was performed at the Calvary John James Memorial Hospital, Deakin, ACT. The clinical assessments were performed at Canberra Hospital, Woden, ACT. The pathology was performed at Capital Pathology, Deakin, ACT. The imaging was performed by Canberra Imaging Group, ACT.
References
- 1.Anderson TP. Trochanteric bursitis: diagnostic criteria and clinical significance. Arch Phys Med Rehabil. 1958;39:617–622. [PubMed] [Google Scholar]
- 2.Baker CL, Jr, Massie RV, Hurt WG, Savory CG. Arthroscopic bursectomy for recalcitrant trochanteric bursitis. Arthroscopy. 2007;23:827–832. doi: 10.1016/j.arthro.2007.02.015. [DOI] [PubMed] [Google Scholar]
- 3.Ben-Galim P, Ben-Galim T, Rand N, Haim A, Hipp J, Dekel S, Floman Y. Hip-spine syndrome: the effect of total hip replacement surgery on low back pain in severe osteoarthritis of the hip. Spine (Phila Pa 1976). 2007;32:2099–2102. doi: 10.1097/BRS.0b013e318145a3c5. [DOI] [PubMed] [Google Scholar]
- 4.Bird PA, Oakley SP, Shnier R, Kirkham BW. Prospective evaluation of magnetic resonance imaging and physical examination findings in patients with greater trochanteric pain syndrome. Arthritis Rheum. 2001;44:2138–2145. doi: 10.1002/1529-0131(200109)44:9<2138::AID-ART367>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 5.Bohannon RW. Make tests and break tests of elbow flexor muscle strength. Phys Ther. 1988;68:193–194. doi: 10.1093/ptj/68.2.193. [DOI] [PubMed] [Google Scholar]
- 6.Bolton JE. Accuracy of recall of usual pain intensity in back pain patients. Pain. 1999;83:533–539. doi: 10.1016/S0304-3959(99)00161-X. [DOI] [PubMed] [Google Scholar]
- 7.Bunker TD, Esler CN, Leach WJ. Rotator-cuff tear of the hip. J Bone Joint Surg Br. 1997;79:618–620. doi: 10.1302/0301-620X.79B4.7033. [DOI] [PubMed] [Google Scholar]
- 8.Chung CB, Robertson JE, Cho GJ, Vaughan LM, Copp SN, Resnick D. Gluteus medius tendon tears and avulsive injuries in elderly women: imaging findings in six patients. AJR Am J Roentgenol. 1999;173:351–353. doi: 10.2214/ajr.173.2.10430134. [DOI] [PubMed] [Google Scholar]
- 9.Connell DA, Bass C, Sykes CA, Young D, Edwards E. Sonographic evaluation of gluteus medius and minimus tendinopathy. Eur Radiol. 2003;13:1339–1347. doi: 10.1007/s00330-002-1740-4. [DOI] [PubMed] [Google Scholar]
- 10.Cormier G, Berthelot JM, Maugars Y, SRO (Société de Rhumatologie de l’Ouest) Gluteus tendon rupture is underrecognized by French orthopedic surgeons: results of a mail survey. Joint Bone Spine. 2006;73:411–413. doi: 10.1016/j.jbspin.2006.01.021. [DOI] [PubMed] [Google Scholar]
- 11.Craig RA, Jones DP, Oakley AP, Dunbar JD. Iliotibial band Z-lengthening for refractory trochanteric bursitis (greater trochanteric pain syndrome) ANZ J Surg. 2007;77:996–998. doi: 10.1111/j.1445-2197.2007.04298.x. [DOI] [PubMed] [Google Scholar]
- 12.Cullen DM, Breidahl WH, Janes GC. Diagnostic accuracy of shoulder ultrasound performed by a single operator. Australas Radiol. 2007;51:226–229. doi: 10.1111/j.1440-1673.2007.01685.x. [DOI] [PubMed] [Google Scholar]
- 13.Ege Rasmussen KJ, Fanø N. Trochanteric bursitis: treatment by corticosteroid injection. Scand J Rheumatol. 1985;14:417–420. doi: 10.3109/03009748509102047. [DOI] [PubMed] [Google Scholar]
- 14.Farr D, Selesnick H, Janecki C, Cordas D. Arthroscopic bursectomy with concomitant iliotibial band release for the treatment of recalcitrant trochanteric bursitis. Arthroscopy. 2007;23:905.e1–e5. [DOI] [PubMed]
- 15.Fox JL. The role of arthroscopic bursectomy in the treatment of trochanteric bursitis. Arthroscopy. 2002;18:E34. doi: 10.1053/jars.2002.35143. [DOI] [PubMed] [Google Scholar]
- 16.Fredberg U, Bolvig L, Pfeiffer-Jensen M, Clemmensen D, Jakobsen BW, Stengaard-Pedersen K. Ultrasonography as a tool for diagnosis, guidance of local steroid injection and, together with pressure algometry, monitoring of the treatment of athletes with chronic jumper’s knee and Achilles tendinitis: a randomized, double-blind, placebo-controlled study. Scand J Rheumatol. 2004;33:94–101. doi: 10.1080/03009740310004126. [DOI] [PubMed] [Google Scholar]
- 17.Girish G, Finlay K, Landry D, O’Neill J, Popowich T, Jacobson J, Friedman L, Jurriaans E. Musculoskeletal disorders of the lower limb: ultrasound and magnetic resonance imaging correlation. Can Assoc Radiol J. 2007;58:152–166. [PubMed] [Google Scholar]
- 18.Gordon EJ. Trochanteric bursitis and tendinitis. Clin Orthop. 1961;20:193–202. [PubMed] [Google Scholar]
- 19.Hardcastle P, Nade S. The significance of the Trendelenburg test. J Bone Joint Surg Br. 1985;67:741–746. doi: 10.1302/0301-620X.67B5.4055873. [DOI] [PubMed] [Google Scholar]
- 20.Jamison RN, Raymond SA, Slawsby EA, McHugo GJ, Baird JC. Pain assessment in patients with low back pain: comparison of weekly recall and momentary electronic data. J Pain. 2006;7:192–199. doi: 10.1016/j.jpain.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 21.Jensen MP, Mardekian J, Lakshminarayanan M, Boye ME. Validity of 24-h recall ratings of pain severity: biasing effects of “Peak” and “End” pain. Pain. 2008;137:422–427. doi: 10.1016/j.pain.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 22.Joines MM, Motamedi K, Seeger LL, DiFiori JP. Musculoskeletal interventional ultrasound. Semin Musculoskelet Radiol. 2007;11:192–198. doi: 10.1055/s-2007-1001883. [DOI] [PubMed] [Google Scholar]
- 23.Kagan A., II Rotator cuff tears of the hip. Clin Orthop Relat Res. 1999;368:135–140. doi: 10.1097/00003086-199911000-00016. [DOI] [PubMed] [Google Scholar]
- 24.Karpinski M, Piggott H. Greater trochanteric pain syndrome: a report of 15 cases. J Bone Joint Surg Br. 1985;67:762–763. doi: 10.1302/0301-620X.67B5.4055877. [DOI] [PubMed] [Google Scholar]
- 25.Katz J, Melzack R. Measurement of pain. Surg Clin North Am. 1999;79:231–251. doi: 10.1016/S0039-6109(05)70381-9. [DOI] [PubMed] [Google Scholar]
- 26.Kingzett-Taylor A, Tirman PF, Feller J, McGann W, Prieto V, Wischer T, Cameron JA, Cvitanic O, Genant HK. Tendinosis and tears of gluteus medius and minimus muscles as a cause of hip pain: MR imaging findings. AJR Am J Roentgenol. 1999;173:1123–1126. doi: 10.2214/ajr.173.4.10511191. [DOI] [PubMed] [Google Scholar]
- 27.Krout RM, Anderson TP. Trochanteric bursitis: management. Arch Phys Med Rehabil. 1959;40:8–14. [PubMed] [Google Scholar]
- 28.LaBan MM, Weir SK, Taylor RS. “Bald trochanter” spontaneous rupture of the conjoined tendons of the gluteus medius and minimus presenting as a trochanteric bursitis. Am J Phys Med Rehabil. 2004;83:806–809. doi: 10.1097/01.PHM.0000140792.48248.49. [DOI] [PubMed] [Google Scholar]
- 29.Leonard MH. Trochanteric syndrome; calcareous and noncalcareous tendonitis and bursitis about the trochanter major. J Am Med Assoc. 1958;168:175–177. doi: 10.1001/jama.1958.63000020003007a. [DOI] [PubMed] [Google Scholar]
- 30.Lequesne M, Djian P, Vuillemin V, Mathieu P. Prospective study of refractory greater trochanter pain syndrome: MRI findings of gluteal tendon tears seen at surgery. Clinical and MRI results of tendon repair. Joint Bone Spine. 2008;75:458–464. doi: 10.1016/j.jbspin.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 31.Lequesne M, Mathieu P, Vuillemin-Bodaghi V, Bard H, Djian P. Gluteal tendinopathy in refractory greater trochanter pain syndrome: diagnostic value of two clinical tests. Arthritis Rheum. 2008;59:241–246. doi: 10.1002/art.23354. [DOI] [PubMed] [Google Scholar]
- 32.Little H. Trochanteric bursitis: a common cause of pelvic girdle pain. Can Med Assoc J. 1979;120:456–458. [PMC free article] [PubMed] [Google Scholar]
- 33.Milosavljevic J, Elvin A, Rahme H. Ultrasonography of the rotator cuff: a comparison with arthroscopy in one-hundred-and-ninety consecutive cases. Acta Radiol. 2005;46:858–865. doi: 10.1080/02841850500270506. [DOI] [PubMed] [Google Scholar]
- 34.Pfirrmann CW, Notzli HP, Dora C, Hodler J, Zanetti M. Abductor tendons and muscles assessed at MR imaging after total hip arthroplasty in asymptomatic and symptomatic patients. Radiology. 2005;235:969–976. doi: 10.1148/radiol.2353040403. [DOI] [PubMed] [Google Scholar]
- 35.Pretell J, Ortega J, Garcia-Rayo R, Resines C. Distal fascia lata lengthening: an alternative surgical technique for recalcitrant trochanteric bursitis. Int Orthop. 2009;33:1223–1227. doi: 10.1007/s00264-009-0727-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Redelmeier DA, Kahneman D. Patients’ memories of painful medical treatments: real-time and retrospective evaluations of two minimally invasive procedures. Pain. 1996;66:3–8. doi: 10.1016/0304-3959(96)02994-6. [DOI] [PubMed] [Google Scholar]
- 37.Sayana MK, Maffulli N. Eccentric calf muscle training in non-athletic patients with Achilles tendinopathy. J Sci Med Sport. 2007;10:52–58. doi: 10.1016/j.jsams.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 38.Segal NA, Felson DT, Torner JC, Zhu Y, Curtis JR, Niu J, Nevitt MC, Multicenter Osteoarthritis Study Group Greater trochanteric pain syndrome: epidemiological and associated factors. Arch Phys Med Rehabil. 2007;88:988–992. doi: 10.1016/j.apmr.2007.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Silva F, Adams T, Feinstein J, Arroyo RA. Trochanteric bursitis: refuting the myth of inflammation. J Clin Rheumatol. 2008;14:82–86. doi: 10.1097/RHU.0b013e31816b4471. [DOI] [PubMed] [Google Scholar]
- 40.Slawski DP, Howard RF. Surgical management of refractory trochanteric bursitis. Am J Sports Med. 1997;25:86–89. doi: 10.1177/036354659702500117. [DOI] [PubMed] [Google Scholar]
- 41.Soderman P, Malchau H. Is the Harris hip score system useful to study the outcome of total hip replacement? Clin Orthop Relat Res. 2001;384:189–197. doi: 10.1097/00003086-200103000-00022. [DOI] [PubMed] [Google Scholar]
- 42.Swezey RL. Pseudo-radiculopathy in subacute trochanteric bursitis of the subgluteus maximus bursa. Arch Phys Med Rehabil. 1976;57:387–390. [PubMed] [Google Scholar]
- 43.Voos JE, Shindle MK, Pruett A, Asnis PD, Kelly BT. Endoscopic repair of gluteus medius tendon tears of the hip. Am J Sports Med. 2009;37:743–747. doi: 10.1177/0363546508328412. [DOI] [PubMed] [Google Scholar]
- 44.Wiese M, Rubenthaler F, Willburger RE, Fennes S, Haaker R. Early results of endoscopic trochanter bursectomy. Int Orthop. 2004;28:218–221. doi: 10.1007/s00264-004-0569-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wittink H, Turk DC, Carr DB, Sukiennik A, Rogers W. Comparison of the redundancy, reliability, and responsiveness to change among SF-36, Oswestry Disability Index, and Multidimensional Pain Inventory. Clin J Pain. 2004;20:133–142. doi: 10.1097/00002508-200405000-00002. [DOI] [PubMed] [Google Scholar]