Abstract
Purpose:
We examined the benefits of younger cochlear implantation, longer cochlear implant use, and greater pre-implant aided hearing to spoken language at 3.5 and 4.5 years of age.
Method:
Language samples were obtained at age 3.5 and 4.5 years from 76 children implanted by their third birthday. Hierarchical Linear Modeling (HLM) was employed to identify characteristics associated with spoken language outcomes at the two test ages. The Preschool Language Scale was used to compare skills with those of hearing age-mates at age 4.5.
Results:
Expected language scores increased with younger age at implant and lower pre-implant thresholds, even when compared at the same duration of implant use. Expected Preschool Language Scale (PLS) scores of the children who received the implant at the youngest ages reached those of hearing age-mates by 4.5 years, but those implanted after 24 months of age did not “catch up” with hearing peers.
Conclusions:
Children who received a cochlear implant before a substantial delay in spoken language developed (i.e., between 12-16 months) were more likely to achieve age-appropriate spoken language. These results favor cochlear implantation before 24 months of age, especially for children with better ear aided pure tone average thresholds greater than 65 dB prior to surgery.
The past decade has proved an exciting time for those involved in efforts to facilitate the spoken language development of young children with severe-profound hearing loss. Implementation of universal newborn hearing screening programs and advances in the technology available to improve the hearing experience itself has led to an era of new possibilities. Cochlear implants, in particular, have become widely embraced as an aid to exposing the deaf child's auditory system to a quality of sound experience not available with hearing aids alone. Clinicians who provide services to children with hearing loss report that children who, in the past, struggled for years with the considerable challenges of acquiring spoken language are now finding this task has become much easier. This has been a helpful turn of events for the families of more than 90% of deaf children who have no previous experience of deafness in the family and whose native languages are expressed through speech. In this paper we will present results of a large-scale study designed to examine the relationship between early cochlear implantation and the development of age-appropriate spoken language. The findings have implications for young children who are preparing to enter the mainstream school setting. In the literature review that follows, issues that bear on decisions about the most beneficial age for cochlear implantation are presented.
Why Expect Implantation in Infancy to Be the Most Beneficial?
Underlying mechanisms
While it is widely assumed that neural organization and/or structure related to speech perception is affected by auditory deprivation, the extent and potential reversibility of changes in the neural architecture are topics of ongoing investigation. Initially, notable differences in speech perception and production were demonstrated for children who received a cochlear implant under the age of about 5-6 years as compared with implant surgery after that age and were attributed to the existence of a period of relative plasticity in the auditory system (Robinson, 1998; Manrique et al., 1999). More recent work has focused on a critical or sensitive period wholly within the infancy/preschool-age stage of life. Sharma and colleagues (Sharma et al., 2004) found changes in neural responding within central auditory pathways that occurred shortly after cochlear implantation in very young children that appeared to be closely related to early communicative behaviors that develop at the same time. In addition, Ryugo, Kretzmer, & Niparko (2005) reported the ability to restore abnormal synaptic structures in the auditory nerve endings of deaf cats to a normal state by stimulating their auditory nerves for 3 months with a 6-channel cochlear implant. These results lend credibility to the notion that special opportunities may exist for preservation or restoration of the auditory system of deaf infants and preschool-aged children that may not be available to those who are just a few years older at time of implant surgery.
Previous studies showing effects of age at implantation surgery on outcomes related to spoken language
Since the introduction of pediatric clinical trials of multi-channel cochlear implantation in 1986, the average age at implantation surgery has been decreasing, with generally positive results (e.g. Richter, Eissele, Laszig, and Lohle, 2002). Studies have shown that language growth rates of children who receive implants before 5 years of age are close to the growth rates of normally hearing children once the deaf child has received an implant (Kirk et al., 2002; Robbins, Koch, Osberger, Zimmerman-Phillips & Kishon-Rabin, 2004; Spencer, 2004; Svirsky, Robbins, Kirk, Pisoni & Miyamoto, 2000; Svirsky, Teoh & Neuberger, 2004). The differences in language performance between children with implants and their hearing age-mates, therefore, are purported to be due to the existing delay in performance at the time of implantation. From this viewpoint, implantation should ideally occur not only early enough for normal language progress to be achieved, but also before delays are present.
Five studies have been published recently that examine the relative rates of language growth (or levels of language outcome) of children who received a cochlear implant exclusively under the age of 5-6 years. In all cases the most rapid progress and/or highest language levels were achieved by children who received the implant at the youngest ages (Kirk et al., 2002; Geers, 2004; Svirsky et al., 2004; Tomblin, Barker, Spencer, Zhang & Gantz, 2005). In all of these studies the tests were administered and language credited for the child's preferred mode of communication, whether speech or sign, or both. Very few studies published to date examine language outcomes solely in the domain of spoken language, and this should be considered when comparing results of different studies and/or in developing expectations for language outcomes. Because children who use total communication and receive cochlear implants at very young ages are more likely to have families who also begin using signs when their child is very young, the language advantages observed in their signed/spoken productions (over those receiving an implant later) may result either from earlier exposure to sign or from earlier auditory input.
In contrast, Hammes et al. (2002) reported exclusively on the spoken language development of 10 children who underwent surgery by 18 months of age and compared their progress to 35 children who received their implant later, up to 48 months of age. Analyses revealed that 70% of those implanted by 18 months, 30% of those implanted between 19-30 months, < 10% of those implanted between 31-40 months, and < 5% of those implanted between 41-48 months had a spoken language age within 1 year of their chronologic age. Manrique et al. (2004) measured the spoken language of 36 children with cochlear implants via the General Oral Expression scale of the Reynell Developmental Language Scales III (Edwars, Fletcher, Garman et al., 1997). It was found that those receiving an implant by age two years had a normal rate of growth though were generally one year delayed whereas children receiving an implant between two and six years exhibited a slower growth rate and a lag of between two and three years below achievement levels for hearing age-mates.
What Complicates Research on This Issue?
Confound of effects of age at surgery, duration of use
A significant problem in the study of age at implantation effects is the confounding of the influence of age at implantation with the influence of the duration of implant use. In the studies cited above duration of implant use and chronologic age at test varied among the different age-at-implantation groups, requiring a cautious interpretation. As the age at implantation is lowered, the duration of use is lengthened, given a particular test age. Typically, the children are grouped according to a range of implant ages and slopes of language scores over time can then be contrasted or entered into statistical analysis. The outcomes of children with differing cochlear implant surgery ages are compared over the same duration of use, leaving test age to vary. Cognitive and language development do not proceed linearly with age. Therefore, rates of progress may be affected by developmental level at the time of testing. A critical age for the most effective auditory stimulation to occur that will promote age-appropriate spoken language acquisition has yet to be verified.
Changing cochlear implant technologies
The same rapid advances in cochlear implant technology that have led to the gains in speech perception discussed above create a problem for studies of age at implantation effects that include participants with different generations of implant devices. Recent advances in newborn hearing screening and implant age candidacy guidelines have resulted in a progressive reduction in the average age at implantation. Therefore, children who were implanted younger are likely to have newer technology. This factor may contribute to an apparent advantage for younger implant recipients in studies that do not control for generation of implant technology. Better outcomes from earlier implanted children may be influenced by their more advanced technology in addition to younger age at implantation (Connor, Hieber, Arts & Zwolan, 2000).
Pre-implant residual hearing
Measuring the effects of earlier age at implantation is also complicated by the fact that children with more pre-implant residual hearing are typically implanted at somewhat older ages. This is due partly to the FDA guidelines that set stricter standards for implant candidacy between 12 and 23 months of age and partly to the challenges of fitting hearing aids in infants. Better pre-implant residual hearing is associated with superior speech recognition with a cochlear implant (Gantz et al., 2000; Dolan-Ash, Hodges, Butts & Balkany, 2000; Zwolan et al., 1997). In addition, very early use of hearing aids in children with residual hearing may act as a bridge to provide auditory access to language until the child receives an implant. Therefore, their experience with hearing aids before implantation may provide them with more advantages of early auditory stimulation than more profoundly deaf hearing aid users with similar age at implantation. Children with more aided residual hearing before implantation exhibited significantly better post-implant spoken language skills, independent of age at implantation (Nicholas & Geers, 2006; Szagun, 2001). Implanting children with the greatest degrees of hearing loss at the youngest ages may mask the true benefits of earlier implantation. These children may be predisposed to slower development of speech perception skills both prior to and following cochlear implantation than children with more residual hearing who are implanted somewhat later. Evidence for the interaction between degree of hearing loss, age at implant and spoken language was provided by Nicholas & Geers (2006). Not only were the children with the greatest degree of hearing loss implanted at the youngest ages, but also duration of hearing aid use prior to implantation was not significantly related to spoken language outcome. This suggests that children without sufficient aided hearing lost important language acquisition time without early use of an implant.
Purposes of the Present Study
It is already known that cochlear implantation under the age of three years, a longer duration of cochlear implant use, and better pre-implant aided hearing contribute to language development. In this study, we will examine the separate contributions of each of these factors to spoken language scores at 3.5 and 4.5 years of age. The analysis will focus on predicting expected language scores from age at surgery and pre-implant residual hearing at the same duration of implant use. It is hypothesized that children implanted at the youngest ages will exhibit a language advantage over children implanted somewhat later, even when they are compared at the same duration of implant use.
Another purpose of this study is to determine whether it is realistic for children with severe to profound hearing loss who receive both a cochlear implant and an oral-language method of education to achieve age-appropriate spoken language abilities during the preschool years. If the answer is yes, how long might we expect this to take? It is hypothesized that some children with severe to profound hearing loss enrolled in oral programs will achieve age-appropriate spoken language by the typical kindergarten entrance age. It is further hypothesized that the probability of achieving this level of spoken language success will be increased with better pre-implant hearing with hearing aids and younger age at implantation.
There are several unique aspects to this study. In this paper we focus on dependent variables that are derived from conversational language samples collected at play sessions in which the child is interacting with his or her parent. This provides a means of extending and/or corroborating language scores from formal tests and imparts a degree of “real-life” generalizability to the conclusions. Second, we focus exclusively on spoken language outcomes, which are of interest to a large percentage of parents and clinicians who provide cochlear implant devices. We measure these outcomes in a relatively large sample of children from a relatively large number of oral or auditory-verbal programs located across the U.S. and Canada. All of the children in the present study received their cochlear implant between their first and third birthdays (± 2 months), which represents the most common age of pediatric cochlear implant surgery at the present time. Finally, comparison data from one group of normal-hearing children at 3.5 years of age and another at 4.5 years of age from a previous study of spoken language development (Nicholas, 2000) will be included as reference points for some of the language measures that will be reported. The children experienced identical data collection procedures as those in the present study.
METHOD
Participants
Data from two groups of children will be included in this paper: children with severe-profound hearing loss who had received a cochlear implant who were tested in the present study and a reference group of normally hearing children from a previous study who underwent the same protocol. Background information on the normally hearing comparison group will be presented first, followed by a complete description of the sample of children with cochlear implants.
Children in the Normal-Hearing reference group
Background information for the normal-hearing children is as follows: 3.5 group mean age = 3 years, 5 months, and 25 days (SD = 11.06 days; N = 12) and 4.5 group mean age = 4 years, 5 months, and 20 days (SD = 15.41 days; N = 12). All children had been recruited through local birth records and had been administered a hearing screening at 500, 1000, and 2000 Hz and were found to have hearing within normal limits. All children had been administered the Communication Scale of the Vineland Adaptive Behavior Scales (Sparrow et al., 1984) and the Peabody Picture Vocabulary Test – 3rd Edition (Dunn & Dunn, 1997) and were found to score within the normal range for their chronologic age.
Participants in the Present Study
Participants in this study were 76 children who had received a cochlear implant between their first and third birthday (± 2 months) and who were enrolled in an oral educational program since receiving a cochlear implant. No participants had developmental or medical conditions other than their hearing loss that would be expected to interfere with speech and language development. All children scored within the average range on either a nonverbal intelligence test (e.g. Leiter International Performance Scale- Revised: Roid & Miller, 1997; Wechsler Preschool and Primary Scale of Intelligence: Wechsler, 2002) or the Daily Living Skills and Motor domains of the Vineland Adaptive Behavior Scales (Sparrow, Balla & Cicchetti, 1984). All children came from families in which English was the primary language or the only language spoken to the child.
Pre-implant history
Summary statistics of pre- and post-implant histories are presented in Table 1. The sample of 76 children was presumed deaf from birth and children were excluded from the study if there was any evidence that the child had once had normal hearing or a progressive hearing loss. Significant associations among the pre-implant participant characteristics were as follows: Age at diagnosis of hearing loss correlated positively with age at amplification (r = .982; p < 0.01) and negatively with duration of hearing aid use (r = −.422; p < 0.01) indicating that those diagnosed at the earliest ages received hearing aids at the youngest ages and had a longer period of hearing aid trial before receiving a cochlear implant. Duration of hearing aid use was negatively correlated with pre-implant aided threshold (r = −.340; p < 0.01) indicating that children with more aided residual hearing had longer periods of hearing aid trial before cochlear implant surgery.
Table 1.
Pre- and post-implant audiological history
| PRE-IMPLANT | |||
|---|---|---|---|
| Mean | Standard Deviation |
Range | |
| Age at diagnosis (mos) | 11.17 | 8.13 | 1-30 |
|
| |||
| First aided (mos) | 12.33 | 7.96 | 1-31 |
|
| |||
| Unaided better ear PTA at 500, 1K, 2K Hz |
107.36 | 10.84 | 77-120 |
|
| |||
| Better ear aided threshold |
64.62 | 14.57 | 32-80 |
|
| |||
| Length of HA use before CI |
10.83 | 5.96 | 0-30 |
|
| |||
| POST-IMPLANT | |||
| Age at Surgery | 23.16 | 7.75 | 12-38 |
|
| |||
| Average CI threshold | 30.21 | 5.20 | 20-43 |
Post-implant history
Age at implant surgery was positively correlated with age at diagnosis of deafness (r = .687; p < 0.01), age at hearing aid amplification (r = .714; p < 0.01), and duration of hearing aid use (r = .345; p <0.05); and negatively correlated with pre-implant unaided threshold (r = −.279; p < 0.05) and pre-implant aided threshold (r = −.380; p < 0.01). These results indicate that children implanted at the youngest ages were those who had the benefit of early identification and amplification and shorter hearing aid trials prior to cochlear implantation. However, they had more profound deafness and received less benefit from hearing aids than children implanted at somewhat older ages. All children received a cochlear implant between 1998 and 2003. Details of device use for the sample of children may be found in Table 2. One child received a second (bilateral) implant during the course of the study.
Table 2.
Post-Implant Device Use
| Percent of sample |
N | |
|---|---|---|
| Device | ||
| Med-El | 1 % | 1 |
| Cochlear Corp | 62 % | 47 |
| Advanced Bionics | 37 % | 28 |
| Full insertion of electrode array | 100 % | 76 |
| No interruption of CI for >30 days | 100 % | 76 |
| Wore HA on contralateral ear | 9 % | 7 |
| Pre-surgery, one ear with clear hearing advantage | 71 % | 54 |
| Of those, implant placed in better ear | (44%) | 24 / 54 |
| If no clear ear better, CI in R ear | 86 % | 19 / 22 |
Procedure
Participants were recruited from 23 different U.S. states as well as 1 Canadian province. Host sites were 14 schools for the deaf, 4 hospitals, 3 county child development centers, 4 public schools, and 7 auditory-verbal therapy practices. Administrators at each of these locations were asked to review their rosters for all children who met the criteria listed above. The parents of all children who met the criteria were given a letter describing the study and a release of information form to sign if they were interested in participating. A research team member then traveled to the child's school or therapy location and completed the data collection in that setting. The study was approved by the first author's Institutional Review Board.
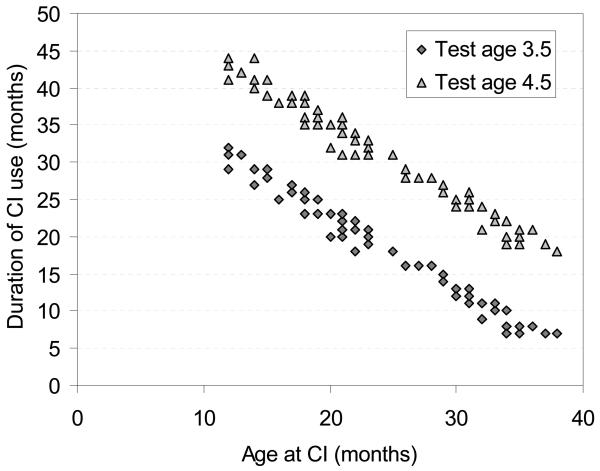
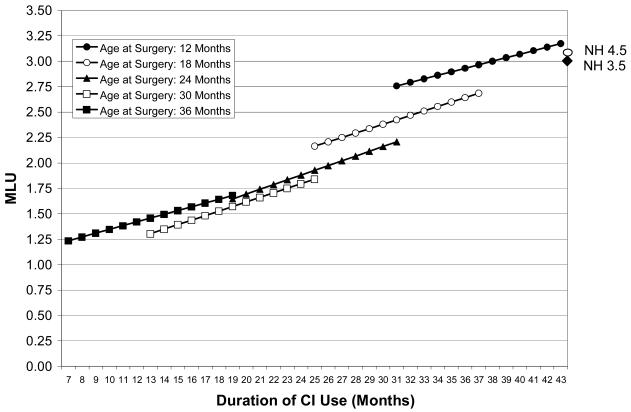
Language sampling
Each participant was videotaped in a 30-minute play session with his or her own parent in a quiet room. The session was a semi-structured time in which the parent was instructed to communicate with the child in a manner that was consistent with their everyday interactions. Parents were specifically asked not to treat the session as a “teaching” session but rather to simply play with their child. Four sets of toys, one set introduced every 7-8 minutes, were provided to the child-parent dyad for purposes of stimulating conversation. The toy boxes each contained a set of toys that were chosen to be age-appropriate as well as being likely to elicit interest and conversation. For example, a storybook with no printed words was included, as well as various sets of human figures and accessories that encourage imaginative play. Language sampling sessions were conducted twice with each child, once when they were 3.5 years old (± 2 months) and again one year later at 4.5 years of age (± 2 months). Duration of implant use across the two test sessions ranged from 7 months to 45 months. The relation between age at implant and duration of implant experience at each test session is plotted in Figure 1. The sample contains children with the same age at cochlear implant surgery but different durations of use and children with the same duration of use but differing ages at implant surgery.
Figure 1.
The relation between age at implant and duration of implant experience at each test session.
Measures derived from the language sample
An experienced teacher of deaf children transcribed from videotape all intelligible spoken words produced by children and parents. When a transcriber questioned whether an utterance was an intelligible representation of a potential target word, the following criteria were applied: same number of syllables, match on at least one vowel, and match on at least one consonant. A second teacher of the deaf reviewed each of the videotapes with its transcript and made any necessary corrections due to omission or error. The transcription procedures follow the CHAT format of the Child Language Data Exchange System (CHILDES; MacWhinney, 2000).
A number of spoken language variables were derived from the language sample and are referred to as “language sample variables”. They were counted utilizing the CLAN software programs provided by the CHILDES (MacWhinney, 2000). Total Number of Words, Number of Different Word Roots, Mean Length of Utterance, Number of Bound Morphemes and Number of Different Bound Morphemes were counted from the transcripts of the 30-minute play session. All of the children were learning spoken language exclusively; only spoken language was included in the dependent variable counts and all references in this paper to a “word” refer to a spoken word.
The five language sample variables provide for a description of several important aspects of a young child's emerging language skill. The Total Number of Words (TNW) provides a measure of the amount of intelligible speech generated by the child within the confines of the 30-minute play session. The Number of Different Word (NDW) Roots is a measure of the breadth of the child's vocabulary. In the calculation of this variable, words that contain a single free (root) morpheme such as “look” (root of look-s, look-ed, look-ing) are counted as a single vocabulary word, thereby decreasing the possibility of over-or under-estimating the breadth of the child's base lexicon based on high or low usage of bound morphemes. The Mean Length of Utterance (in Words) (MLU-W) was included as a simple measure of syntactic development and, consistent with other researchers, it is our practice to exclude repetitions, false starts, and abandoned utterances in the calculation of this measure. A bound morpheme was defined as any grammatical tag or marker that cannot function independently and is attached to a free morpheme or other bound morpheme. This definition includes inflectional suffixes such as –s, -es, -'s, -ing, -ed, -er (“bigger”), derivational suffixes such as –ly, -ist, -er (“painter”), -ness, -ment, as well as contractions such as –'s (is), -'nt (not), -ll (will), -'re (are), -'m (am), and –'us (us). The Number of Bound Morphemes per Word (NBM) provides a sense of how often a child is using bound morphemes and Number of Different Bound Morphemes (DBM) indicates the breadth of the child's mastery of bound morpheme types.
These measures (or subsets thereof) are used with some regularity in the analysis of language samples in the field of language disorders and the analysis of spoken language samples of children with hearing loss (e.g., Paul, 2001; Klee, 1992; Pan, 1994; Bellaire, Plante, Swisher, 1994; Nicholas & Geers, 2006; Geers, Nicholas & Sedey, 2003).
Transcription reliability
For the purposes of examining transcriber reliability, fifteen 30-minute language samples were independently transcribed in their entirety by the two transcribers. Mean values for each of the language variables produced by the two transcribers were as follows: TNW (564,567), NDW (47,51), TBM (42,45), NDBM (6.2, 6.0), and MLU-W (.82, .85). Correlations were calculated to determine the degree of correspondence between the two transcribers for each dependent variable. The mean correspondence between transcribers was .97 and the range of correlations was .93 (for Number of Different Bound Morphemes) to .99 (for Total Number of Words).
Standardized language testing
Formal language testing with the Preschool Language Scale – 3rd Edition (PLS-3; Zimmerman, Steiner, & Pond, 1992) was conducted only at test age 4.5 years. Only spoken responses were credited in the scoring of the test. Expressive language quotient scores were used to represent the rate of language progress in relation to hearing age-mates. A quotient score of 100 reflects language that is on par with hearing children of the same chronological age. Quotient scores below 85 reflect development that is more than one standard deviation behind that of hearing age-mates.
RESULTS
General Language Levels Observed
In order to illustrate the magnitude of language outcomes, average spoken language variable counts from the two language samples are presented in Table 3 for the 76 children with cochlear implants (CI) and the 12 hearing children tested at 3.5 years and the 12 hearing children tested at 4.5 years. Results for the sample of children with CIs represents change in the same individuals over the one-year intra test interval. Because different hearing children were tested at 3.5 and at 4.5 years of age, no comparisons are made between the cochlear implant and normal hearing groups in terms of growth rates. Rather, mean scores for each age group are provided for the normal hearing children simply as a frame of reference for the CI group's scores.
Table 3.
Mean Outcome Scores at 3.5 and 4.5 Years of Age
| Children with a Cochlear implant | Hearing Children | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| N = 76 | N = 12 @ 3.5 & 4.5 yrs | ||||||||
| CA | Mean | SD | Min | Max | Mean | SD | Min | Max | |
| Total Words | 3.5 | 421 | 273 | 33 | 1316 | 762 | 164 | 539 | 1035 |
| 4.5 | 588 | 293 | 65 | 1477 | 850 | 237 | 405 | 1256 | |
|
| |||||||||
| Root Words | 3.5 | 111 | 53 | 9 | 251 | 199 | 28 | 166 | 245 |
| 4.5 | 151 | 55 | 30 | 287 | 225 | 40 | 159 | 287 | |
|
| |||||||||
| Total Bound Morphemes |
3.5 | 26.98 | 29 | 0 | 127 | 91 | 29 | 43 | 135 |
| 4.5 | 52.96 | 37 | 0 | 153 | 104 | 34 | 44 | 163 | |
|
| |||||||||
| Different Bound Morphemes |
3.5 | 4.88 | 3.3 | 0 | 12 | 10.75 | 1.71 | 8 | 13 |
| 4.5 | 7.18 | 3.2 | 0 | 12 | 10.67 | 1.50 | 7 | 13 | |
|
| |||||||||
| MLU | 3.5 | 1.82 | 0.67 | 1.00 | 3.83 | 3.02 | 0.36 | 2.48 | 3.77 |
| 4.5 | 2.34 | 0.75 | 1.06 | 3.88 | 3.06 | 0.35 | 2.64 | 3.89 | |
Separate Contributions of Pre-CI Aided Hearing, Duration of CI use, and Age at Surgery
Hypothesis 1: Better language outcomes and faster language growth are associated with younger age at implant, better pre-implant aided thresholds and longer duration of implant use
Hierarchical Linear Modeling (HLM) was used to examine this hypothesis at 2 levels. The first level examined the extent to which language scores achieved by children with implants were predicted by age at surgery and pre-implant residual hearing. HLM was used to examine the linear relation between language outcome and duration of implant use and to establish whether children implanted at younger ages exhibited a language advantage beyond that achieved with increased implant experience. Next, the growth functions between 3.5 and 4.5 years of age were examined for children implanted at different ages. This step examined whether children implanted younger exhibited a steeper growth of language scores over the one-year test interval than children implanted somewhat older.
Each HLM analysis viewed the data at two levels: growth over time at the level of the individual (Level 1) and between-individual moderators of the growth parameters (Level 2). Level 1 effects are those involving the intercept and the slope for each individual. At Level 1, the duration of implant use at the time of each test is the within-individual predictor and each of the five language measures is the outcome, for example, Mean Length of Utterance (MLU):
where πoi is the intercept or level of the outcome when duration is centered at 24 months and π1i is the linear growth parameter. At Level 1 (the individual), growth rate is the difference in scores between Test Age 1 and Test Age 2. These are averaged across participants and the overall effects are represented at Level 2. Level 2 coefficients indicate if either the Level 1 intercept or Level 1 slope are related to participant characteristics (e.g. age at implant, pre implant hearing). They are between-participants effects.
In the second analysis, the degrees to which the growth parameters depend on Level 2 characteristics of the participants are modeled. Together, these analyses tested the extent to which the overall level of each language outcome measure, and the linear component of growth due to duration of cochlear implant use, were influenced by the pre-implant aided threshold and the age at which the children were implanted
ß00 is the level of the language outcome measure when all other variables are centered as follows: Aided HA Threshold = 64 dB (grand mean); Age at Implant = 21 Mos; Duration of CI use = 24 Mos). ß10 indicates the linear effect of Duration of CI Use on outcome score with each of the other variables centered as indicated.
It is important to consider both Level 1 and Level 2 effects in each of the analyses. If Level 1 was all that mattered, then only the first term to the right of the equality (Pre-CI aided thresholds) in the above equations would matter – these are Level 2 intercepts and represent the overall level and slope – essentially the average over participants of their individual Level 1 parameters. The other terms to the right of the equality reveal whether individual level parameters depend on participant characteristics (pre-CI aided thresholds, age at surgery). If they do, then that indicates that the intercepts alone cannot tell the whole story. For example, in Table 5, a significant β12 would indicate that the Level 1 slopes depend on age at surgery in a linear fashion. In this case, Level 1 slope increases as age at implant surgery increases. A significant β13 would mean that the Level 1 slopes change with age at surgery in a quadratic fashion. This means that the amount of change in the dependent variable predicted by an increase in the predictor variable(s) varies as a function of location on the curve. For example, Level 1 slopes increase faster as age at implantation surgery decreases.
Table 5.
Hierarchical Linear Modeling Analysis of Level 1 Growth as a function of Subject Characteristics
| Outcome | Fixed Effect | Coefficient | SE | t |
|---|---|---|---|---|
| Total Words | Intercept (β10) | 12.18 | 2.66 | 4.57*** |
| Pre CI Aided PTA (β11) | −0.08 | 0.12 | −0.68 | |
| Age at implant (β12) | 0.22 | 0.33 | 0.67 | |
| AOI2 (β13) | 0.01 | 0.33 | 0.22 | |
| Root Words | Intercept | 2.95 | 0.43 | 6.85*** |
| Pre CI Aided PTA | 0.00 | 0.02 | 0.12 | |
| Age at implant | 0.02 | 0.05 | 0.34 | |
| AOI2 | 0.00 | 0.00 | 0.78 | |
| MLU | Intercept | 0.05 | 0.00 | 8.23*** |
| Pre CI Aided PTA | 0.00 | 0.00 | −1.95* | |
| Age at implant | 0.00 | 0.00 | 0.81 | |
| AOI2 | −0.00 | 0.00 | −1.07 | |
| Bound Morphs. | Intercept | 2.52 | 0.30 | 8.42*** |
| Pre CI Aided PTA | −0.06 | 0.01 | −4.02*** | |
| Age at implant | 0.02 | 0.04 | 0.59 | |
| AOI2 | −0.01 | 0.00 | −2.10* | |
| Diff. Morphs. | Intercept | 0.20 | 0.02 | 7.60*** |
| Pre CI Aided PTA | −0.00 | 0.00 | −0.13 | |
| Age at implant | 0.01 | 0.00 | 2.44** | |
| AOI2 | −0.00 | 0.00 | −1.12 |
p < .05
p < .01
p < .001, df = 72
Table 4 presents results for the overall level of language outcome, showing the influence of subject characteristics. (Note that the intercepts must be different from zero because they are the mean performance levels when predictors are at their means.) The mean language scores were influenced significantly by two subject characteristics: pre-implant residual hearing and age at implant. These characteristics had a significant negative effect, indicating that a higher language outcome was associated with a lower PTA threshold (i.e., greater pre-implant residual hearing) and a lower age at implant (i.e., younger implantation) when duration of CI use was centered at 24 months. No significant curvilinear trends were noted (AOI2).
Table 4.
Hierarchical Linear Modeling of Level 1 Intercepts as a Function of Subject Characteristics
| Outcome | Fixed Effect | Coefficient | SE | t |
|---|---|---|---|---|
| Total Words | Intercept (β00) | 497.30 | 32.41 | 15.34*** |
| Pre CI Aided PTA (β01) | −7.82 | 1.71 | 1.71*** | |
| Age at implant (β02) | −11.93 | 4.86 | 4.87** | |
| (Age at implant)2 (β03) | 0.42 | 0.50 | 0.84 | |
| Root Words | Intercept | 125.56 | 5.62 | 22.34*** |
| Pre CI Aided PTA | −1.80 | 0.29 | −6.10*** | |
| Age at implant | −2.07 | 0.83 | −2.50*** | |
| (Age at implant)2 | 0.10 | 0.09 | 1.20 | |
| MLU | Intercept | 1.98 | 0.07 | 26.83*** |
| Pre CI Aided PTA | −0.02 | 0.00 | −3.75*** | |
| Age at implant | −0.04 | 0.01 | −3.75*** | |
| (Age at implant)2 | 0.00 | 0.00 | 1.92 | |
| Bound Morphemes |
Intercept | 34.55 | 3.72 | 9.29*** |
| Pre CI Aided PTA | −0.98 | 0.20 | −4.81*** | |
| Age at implant | −1.58 | 0.52 | −3.03** | |
| (Age at implant)2 | 0.09 | 0.05 | 1.62 | |
| Different Morphemes |
Intercept | 5.89 | 0.34 | 17.46*** |
| Pre CI Aided PTA | −0.11 | 0.02 | −6.13*** | |
| Age at implant | −0.19 | 0.05 | −3.76*** | |
| (Age at implant)2 | 0.01 | 0.00 | 1.68 |
p < .01
p < .001 df = 72
Note: The t-values for the intercept reflect the expected outcome that means will be different from zero.
Table 5 presents results relating duration of CI use to language growth between the age 3.5 and 4.5 test sessions. This analysis indicates the degree to which the growth function was significant overall (intercept does not equal zero) and the degree to which growth was influenced by subject characteristics. The intercepts in this table indicate the overall rate of growth when the subject characteristics are at their centered values. All of these intercepts show the expected overall increase in language scores as duration of CI use increases. In addition, the linear increase in two language outcomes (MLU and Number of Bound Morphemes) with duration of implant use was negatively influenced by pre-implant threshold. Children with better pre-implant residual hearing exhibited steeper growth of language with greater implant experience than children with less pre-implant aided hearing. For most of these language outcomes, growth rates did not differ for children implanted at different ages. An exception was growth rate in different bound morphemes used. The linear increase in number of different bound morphemes with greater CI use was negatively influenced by age at implant, indicating that children implanted at younger ages showed slower growth in variety of bound morphemes used with greater implant experience. This finding resulted from children implanted at 12 months of age approaching a ceiling on this measure. The variable Total Bound Morphemes revealed a significant quadratic trend, with the latest implanted showing a slower growth rate.
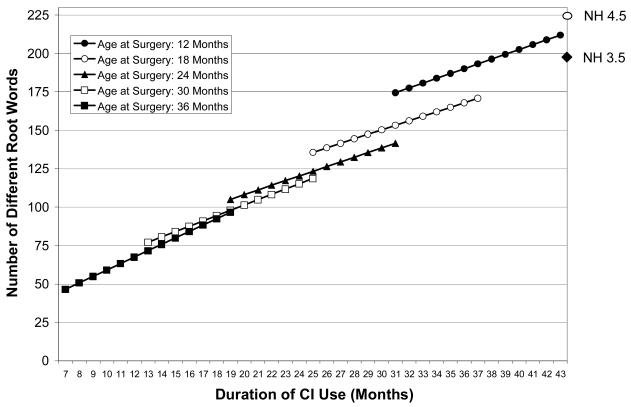
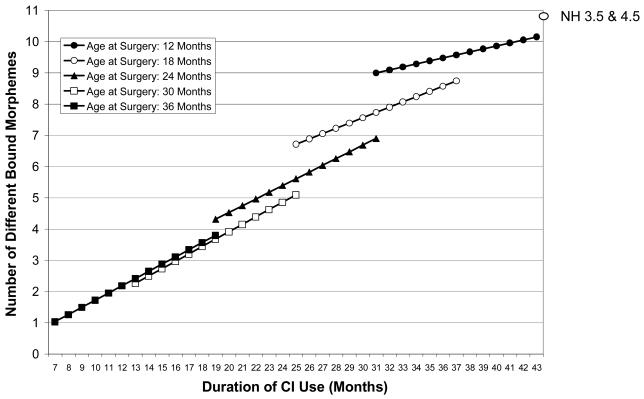
Language level by age at implant surgery
Results of the HLM analyses were used to calculate expected outcome scores for children at five different ages of implant surgery (12, 18, 24, 30 & 36 mos) with pre-implant hearing threshold held constant at the mean. These expected values for five different ages at implant surgery are plotted by duration of implant use for three of the outcome measures in Figures 2-4: Number of different root words, mean length of utterance and number of different bound morphemes. The mean levels achieved by the two groups of subjects with normal hearing at age 3.5 and 4.5 are indicated on the far right ordinate of each graph for purposes of comparison. (Recall that the values for normal hearing children are actual test scores.) These graphs illustrate expected language outcomes for different ages at implant at similar durations of use. The significant advantage for earlier age at implant is apparent across all three language measures (and was observed for the other two measures as well). In all cases, the outcome level achieved at the same duration of implant use is higher for children implanted under two years of age. For example, at approximately 31 months of device use, children implanted at 12 months of age achieved an expected average of 175 different words while the comparable expected value for those implanted at 24 months was 140 words. Similarly, the expected number of different bound morphemes at 31 months of implant use is nine for children implanted at 12 months of age, but less than seven for children implanted at 24 months. Across the language measures, children implanted at 12 months of age exhibited language outcomes at 3.5 years of age that were not achieved by those implanted at 18 months until 4.5 years of age. Below an implant age of 24 months, a consistent advantage is illustrated for younger cochlear implantation at any given duration of implant use. Follow-up tests of significance between expected means at any given duration of use is not provided within the HLM analysis as it is with a standard regression approach. However, visual inspection of the graphs suggests that children who received their implants after about 24 months of age do not show the same advantage in language level achieved with earlier implantation for the same duration of use.
Figure 2. Number of Different Words.
Each figure shows, for selected surgery ages, the relationship between duration of implant use and an outcome variable. These figures were derived in the following way. For a given surgery age and assuming the grand mean for pre-implant aided threshold, a duration slope and intercept were calculated from the HLM equations (see Tables 4 and 5). These were obtained by multiplying the appropriate Level 2 coefficients by the particular surgery age (as a deviation from the group mean of 21 months) or its square (pre-implant aided threshold was centered at its grand mean and so assumed a value of 0 in these calculations). The duration centering constant is 24 months, representing two years of use. By using these centering constants, the Level 1 constant and slope coefficients are the expected values for a subject with a median surgery age. The constant is further the expected outcome for a participant with a median surgery age and two years of implant use. The resulting surgery-age-specific slope and intercept coefficients were then used to generate the predicted outcomes for different values of duration (a range of duration values were selected that were typical for the particular surgery age). The resulting figures thus show the expected outcome values given different surgery ages and durations of implant use.
Figure 4. Number of Different Bound Morphemes.
Each figure shows, for selected surgery ages, the relationship between duration of implant use and an outcome variable. These figures were derived in the following way. For a given surgery age and assuming the grand mean for pre-implant aided threshold, a duration slope and intercept were calculated from the HLM equations (see Tables 4 and 5). These were obtained by multiplying the appropriate Level 2 coefficients by the particular surgery age (as a deviation from the group mean of 21 months) or its square (pre-implant aided threshold was centered at its grand mean and so assumed a value of 0 in these calculations). The duration centering constant is 24 months, representing two years of use. By using these centering constants, the Level 1 constant and slope coefficients are the expected values for a subject with a median surgery age. The constant is further the expected outcome for a participant with a median surgery age and two years of implant use. The resulting surgery-age-specific slope and intercept coefficients were then used to generate the predicted outcomes for different values of duration (a range of duration values were selected that were typical for the particular surgery age). The resulting figures thus show the expected outcome values given different surgery ages and durations of implant use.
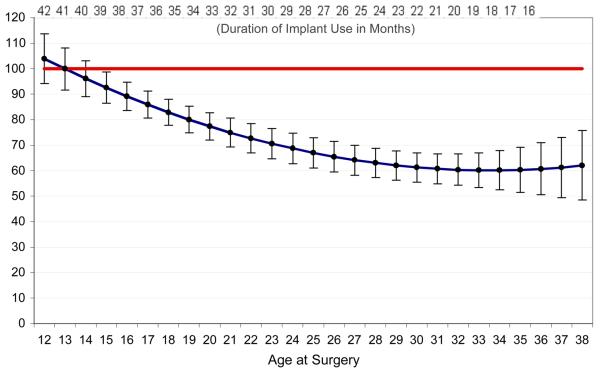
Is It Realistic to Expect Age Appropriate Spoken Language By Age 4.5 Years?
Hypothesis 2: Children who receive a cochlear implant before their second birthday can be expected to achieve age-appropriate spoken language by 4.5 years of age
While Figures 2-4 indicate that by age 4.5, some children (those implanted at 12 months of age) would be expected to achieve values that approached those observed in hearing age mates, the measures may not fully reflect normal language development. The levels achieved by hearing children on some measures, for example mean length of utterance and number of different bound morphemes, show very little change between the 3.5 and 4.5 years groups, so may not be sensitive to language growth at these ages. Therefore, a standardized language test, the Preschool Language Scale, was administered at the 4.5 test session so that the performance of children with cochlear implants could be compared with a large normative sample of age-matched hearing children. Expressive quotient scores on the Preschool Language Scale were examined using regression analysis to establish the surgery age and amount of auditory experience needed to achieve age-appropriate growth rates in spoken language.
A mean quotient of 100 indicates that language acquisition is proceeding at the expected rate for hearing age-mates. Quotient scores within 15 points of this mean indicate growth rates within the average range. The regression function for quotient scores as a function of age at implant is plotted in Figure 5, with the 95% confidence intervals indicated with error bars. Regression results are summarized in Table 6, indicating significant effects of both age at implant and pre-implant aided threshold on language quotient scores. Both linear and quadratic trends were significant for age at implantation. Below an implant surgery age of 30 months there was a linear increase in PLS quotient scores with younger cochlear implantation. This means a language quotient score closer to age-appropriate level for each month's decrease in surgery age from 30 to 12 months. The 95% confidence limits surrounding each value indicate that the expected mean score of children implanted between 12 and 16 months of age was within one standard deviation of the normative sample of hearing age mates (i.e., a score of > 85). A quadratic trend was evident between 30 and 38 months age at implant where the estimated quotient score remained close to 65 across the 8-month interval. For children implanted later than 30 months of age, the existing language delay, combined with a slower rate of language development suggests that they may not catch up with hearing age-mates, even with longer duration of implant use.
Figure 5.
PLS Expressive Standard Scores at Test Session 2 by Age at Implant
Table 6.
Regression coefficients predicting PLS Expressive standardized scores
| Source | Unstandardized Regression Coefficient (β) |
t-ratio | p-value | Partial η2 |
|---|---|---|---|---|
| Aided PTA | −0.498 | −3.406 | .001 | .139 |
| Age CI | −6.326 | −3.400 | .001 | .138 |
| Age CI2 | .094 | 2.462 | .016 | .078 |
Consideration of Alternative Explanations
Possible effect of imitation on child language outcomes
Self-repetitions and imitations were included in the language sample transcriptions. More frequent use of these behaviors by children of particular description (e.g., children with better pre-implant aided hearing) could potentially change the interpretation of our findings. Therefore, these events were identified for the purpose of examining their impact on the dependent variables. At Test Age 3.5, the children with implants used Repetition/Imitation in 14% (SD = .12) of their utterances, as compared to 5% (SD = 2.0) for normal-hearing children of the same age. At Test Age 4.5, the percentage of same was 6 % (SD = .06) for the children with implants versus 2% (SD = 2) for the normal-hearing reference group. Correlations of Repetition/Imitation with each of the language sample outcome variables were as follows: Total Number of Words - .44, Number of Different Words -.50, MLU-Words -.51, Total Bound Morphemes -.43, and Different Bound Morphemes -.49. These results suggest that children with lower level language skills tended to produce more repetitions and imitations in their conversational speech. Additionally, the correlation between age at surgery and percent of utterances that were Repetitions/Imitations was .30, suggesting that children who received the implant early were less likely to be imitating and therefore less likely to have language scores that had been influenced in this way.
Possible effect of volume of parent talk on child language outcomes
It is conceivable that the amount of talk produced by the parent could influence the child language outcome variables. For example, if some parents tended to dominate the conversation, they might leave less time for the child to talk, thereby artificially depressing the child's scores on many of the outcome variables. Further, if the amount of parent talk was also related to the child's pre-implant hearing status then this might affect the interpretation of the influence of pre-CI hearing on the outcome variables. We found these alternative explanations to have little support in our data. The correlation between the volume of parent talk and the child's pre-implant aided hearing was -.15. Further, an exploration of the possible relationship between parent talk and child language sample measures revealed correlations ranging from .11 to .24, none of which were significant at the p < .05 level. Therefore, it does not appear that the children's measured language level was affected by parent output.
DISCUSSION
What predicts overall language level and growth?
One purpose of the present study was to evaluate the role of implantation age, duration of implant use, and aided pre-implant hearing in predicting language growth rate and overall language levels achieved. As expected, on average the predicted scores on linguistic measures increased with longer duration of cochlear implant experience. Moreover, the age of the child at the time of cochlear implant surgery was shown to have a significant effect on expected overall language level over and above the effect of duration of implant use. Expected scores of children who received an implant at 12 to 18 months of age, were consistently higher than those of children implanted at older ages, even with the same duration of use. However, almost identical expected language performance was predicted for any given duration of use when children were implanted at 24 months of age or later.
On the other hand, few notable differences were observed in rate of predicted language growth as a function of age at cochlear implantation. The two exceptions to this general finding involve growth in the use of bound morphemes. The children who received the implant at about 36 months of age showed a slower expected rate of growth in the Total Number of Bound Morphemes used – perhaps indicating that this aspect of language growth does not improve much in the near post-implantation period. In addition, the growth rate of the children implanted at around 12 months of age was not as steep for the variable Number of Different Bound Morphemes which may reflect the fact that their use of morphemes was nearly on par with their hearing age mates at this point in time.
For most of the language sample measures, the hypothesized effect of age at implantation on outcome level was confirmed (i.e., younger age at implant resulted in significantly higher predicted scores). On the other hand, the hypothesized difference in rate of language growth was not confirmed (i.e., predicted rate of growth was the same regardless of the age at implantation). The observed higher level of language functioning in children who received the implant at a younger age was most likely the result of steeper growth rates experienced prior to their participation in this study. This result is in concert with the Tomblin et al. (2005) conclusion that cochlear implantation early in the second year of life likely results in an early burst of language growth. Tomblin reports that this rapid rate of initial language growth is a phenomenon that is not evident in the language scores of children implanted after the age of about 18 months, a finding confirmed by these data.
One unique aspect of this approach to analysis of age-of-implantation data was to control for the effect of pre-implant hearing thresholds. In earlier cochlear implant studies, in which children with implants had uniformly profound hearing losses prior to surgery, age at implantation effects could be more readily observed because of smaller amounts of variability. More recently, children with greater residual hearing have been receiving a cochlear implant, and the resulting benefit from early amplification may contribute independently to spoken language development. When this increase in variability is taken into account the beneficial effects of early cochlear implantation are even more apparent. Pre-implant data from this sample indicated that children implanted at younger ages had poorer aided residual hearing than those implanted somewhat later. Higher pre-implant aided thresholds were also associated with lower language scores at 3.5 and 4.5 years of age and in some cases slower growth rates. Removing the variance due to differences in aided thresholds and equalizing expected outcomes at the mean PTA value of 65 dB serves to enhance the predicted outcomes of those implanted at the youngest ages.
Will They Catch Up?
Another purpose of the study was to determine whether it is realistic to expect that children who both receive a cochlear implant and enroll in a spoken-language based program at a young age will be able to achieve age-appropriate spoken language abilities by they end of the preschool period. We also wanted to identify those factors that maximize the likelihood of that accomplishment. Although some school-aged children with a cochlear implant received prior to the age of five years have been reported to be “closing the gap” with their hearing peers in terms of spoken language production, verbal IQ, and academic achievement (Stacey, Fortnum, Barton & Summerfield, 2006; Moog, 2002; Geers, Nicholas, & Sedey, 2003; Geers, 2004), many of these children continue to exhibit delays for many years. Geers (2004) reported that only 43% of a nation-wide sample of eight- to nine- year-old deaf children who received a cochlear implant between 24 and 35 months of age achieved combined speech and language skills within the average range for hearing children of that chronological age. Results of the current study indicate that children who receive a cochlear implant and oral education before 24 months of age can be expected to exhibit levels of spoken language that are on par with hearing age mates before they enter kindergarten. The likelihood of achieving normal language in preschool decreases as age at implantation increases, so that children implanted as late as three years of age may experience great difficulty catching up with hearing age-mates. These results suggest that (a) it is appropriate for expectations of spoken language competence to be raised for children receiving cochlear implants before 24 months of age and (b) the children who receive the implant at the earliest ages will likely be able to make a successful transition to the mainstream educational system in time for kindergarten.
In sum, the total amount of language produced, the breadth of vocabulary, complexity of sentences, and use of varied morphology seems to be directly affected by both the amount of hearing available to the child before the implant as well as the age at which the cochlear implant surgery was performed. Previous work (Nicholas & Geers, 2006) has shown that the age at diagnosis of the hearing loss and the length of time that a hearing aid was used are not significant predictors of later spoken language outcomes unless they lead to a child receiving a cochlear implant within this time period. The results of the present study clearly show that at 4.5 years of age, when these children were approaching kindergarten, the expected language quotient scores of the very young cochlear implant recipients were well within the range documented for hearing age-mates. If the goal for a congenitally profoundly deaf child is to achieve age-appropriate spoken language in the shortest possible timeframe, then younger cochlear implantation is clearly justified. The added benefit to spoken language of receiving an equivalent amount of implant experience at a very young age (e.g., 12-18 months) compared to even a few months later (e.g., 24 months) argues strongly in support of a critical period for auditory stimulation. These results favor early diagnosis of profound hearing loss, early initiation of a hearing aid trial, and cochlear implantation by 18 months of age, especially for children with better ear aided pure tone average thresholds greater than 65 dB. Future research should focus on documenting the extent to which the advantages of very early auditory stimulation persist into elementary school and whether children implanted below 12 months of age are able to achieve age-appropriate expected spoken language skills even earlier than 4.5 years of age.
Figure 3. Mean Length of Utterance.
Each figure shows, for selected surgery ages, the relationship between duration of implant use and an outcome variable. These figures were derived in the following way. For a given surgery age and assuming the grand mean for pre-implant aided threshold, a duration slope and intercept were calculated from the HLM equations (see Tables 4 and 5). These were obtained by multiplying the appropriate Level 2 coefficients by the particular surgery age (as a deviation from the group mean of 21 months) or its square (pre-implant aided threshold was centered at its grand mean and so assumed a value of 0 in these calculations). The duration centering constant is 24 months, representing two years of use. By using these centering constants, the Level 1 constant and slope coefficients are the expected values for a subject with a median surgery age. The constant is further the expected outcome for a participant with a median surgery age and two years of implant use. The resulting surgery-age-specific slope and intercept coefficients were then used to generate the predicted outcomes for different values of duration (a range of duration values were selected that were typical for the particular surgery age). The resulting figures thus show the expected outcome values given different surgery ages and durations of implant use.
Acknowledgements
This study was supported by Grant # R1DC04168 from the National Institute on Deafness and Other Communication Disorders to Central Institute for the Deaf and Washington University School of Medicine. The authors wish to thank the following people for their assistance: Michael Strube for statistical consultation, , Sallie Shiel Vanderhoof, Sarah Fessenden, Heidi Geers, Heather L. Hayes, and Christine Brenner for data collection, transcription, and technical assistance. We also thank the many families and school/hospital/therapy programs that generously agreed to participate.
Contributor Information
Johanna Grant Nicholas, Central Institute for the Deaf Research Department of Otolaryngology Washington University School of Medicine St. Louis, MO.
Ann E. Geers, Southwestern Medical Center University of Texas at Dallas Dallas, TX
REFERENCES
- Battmer RD, Gupta SP, Allum-Mecklenburg DJ, Lenarz T. Factors influencing cochlear implant perceptual performance in 132 adults. Annals of Otology, Rhinology & Laryngology. 1995;166:S185–S187. [PubMed] [Google Scholar]
- Bellaire S, Plante E, Swisher L. Bound morpheme skills in the oral language of school-age, language-impaired children. Journal of Communication Disorders. 1994;27:265–279. doi: 10.1016/0021-9924(94)90017-5. [DOI] [PubMed] [Google Scholar]
- Connor CM, Hieber S, Arts HA, Zwolan TA. Speech, vocabulary, and the education of children using cochlear implants: Oral or total communication? Journal of Speech, Language, and Hearing Research. 2000;43:1185–1204. doi: 10.1044/jslhr.4305.1185. [DOI] [PubMed] [Google Scholar]
- Dolan-Ash S, Hodges AV, Butts SL, Balkany TJ. Borderline pediatric cochlear implant candidates: Preoperative and postoperative results. Annals of Otology, Rhinology & Laryngology. 2000;109:36–38. doi: 10.1177/0003489400109s1215. [DOI] [PubMed] [Google Scholar]
- Dunn LM, Dunn LM. The Peabody Picture Vocabulary Test. 3rd ed. American Guidance Service; Circle Pines, MN: 1997. [Google Scholar]
- Edwars S, Flethcher P, Garman M. The Reynell Developmental Language Scales III. Nfer-Nelson Publishing Company Ltd; Windsor, UK: 1997. [Google Scholar]
- Gantz BJ, Rubinstein JT, Tyler RS, Teagle HF, Cohen NL, Waltzman SB. Long-term results of cochlear implants in children with residual hearing. Annals of Otology, Rhinology, & Laryngology. 2000;109:33–36. doi: 10.1177/0003489400109s1214. [DOI] [PubMed] [Google Scholar]
- Geers A. Speech, language, and reading skills after early cochlear implantation. Archives of Otolaryngology – Head and Neck Surgery. 2004;130:634–638. doi: 10.1001/archotol.130.5.634. [DOI] [PubMed] [Google Scholar]
- Geers AE, Nicholas JG, Sedey AL. Language skills of children with early cochlear implantation. Ear and Hearing. 2003;24:46S–58S. doi: 10.1097/01.AUD.0000051689.57380.1B. [DOI] [PubMed] [Google Scholar]
- Hammes DM, Novak MA, Rotz LA, Willis M, Edmondson DM, Thomas JF. Early identification and cochlear implantation: Critical factors for spoken language development. Annals of Otology, Rhinology, & Laryngology. 2002;111:74–78. doi: 10.1177/00034894021110s516. [DOI] [PubMed] [Google Scholar]
- Holt RF, Svirsky MA, Neuburger H, Miyamoto RT. Age at implantation and communicative outcome in pediatric cochlear implant users: Is younger always better? International Congress Series. 2004;1273:368–371. [Google Scholar]
- Kirk KI, Miyamoto RT, Lento CL, Ying E, O'Neill T, Fears B. Effects of age at implantation in young children. Annals of Otology, Rhinology, & Otolaryngology. 2002;111:69–73. doi: 10.1177/00034894021110s515. [DOI] [PubMed] [Google Scholar]
- Klee T. Developmental and diagnostic characteristics of quantitative measures of children's language production. Topics in Language Disorders. 1992;12:28–41. [Google Scholar]
- MacWhinney B. The CHILDES project: Tools for analyzing talk. Third Edition Lawrence Erlbaum Associates; Mahwah, NJ: 2000. [Google Scholar]
- Manrique M, Cervera-Paz FJ, Huarte A, Perez N, Molina M, Garcia-Tapia R. Cerebral auditory plasticity and cochlear implants. International Journal of Pediatric Otorhinolaryngology. 1999;49:S193–S197. doi: 10.1016/s0165-5876(99)00159-7. [DOI] [PubMed] [Google Scholar]
- Manrique M, Cervera-Paz FJ, Huarte A, Molina M. Advantages of cochlear implantation in prelingual deaf children before 2 years of age when compared with later implantation. Laryngoscope. 2004;114:1462–1469. doi: 10.1097/00005537-200408000-00027. [DOI] [PubMed] [Google Scholar]
- McConkey-Robbins A, Koch D, Osberger M, Zimmerman-Phillips S, Kishon-Rabin L. Effect of age at cochlear implantation on auditory skill development in infants and toddlers. Archives of Otolaryngology-Head and Neck Surgery. 2004;130:570–574. doi: 10.1001/archotol.130.5.570. [DOI] [PubMed] [Google Scholar]
- Moog JS. Changing expectations for children with cochlear implants. Annals of Otology, Rhinology, & Laryngology. 2002;111:138–142. doi: 10.1177/00034894021110s527. [DOI] [PubMed] [Google Scholar]
- Nicholas JG. Age differences in the use of informative/heuristic communicative functions in young children with and without hearing loss who are learning spoken language. Journal of Speech, Language, and Hearing Research. 2000;43:380–394. doi: 10.1044/jslhr.4302.380. [DOI] [PubMed] [Google Scholar]
- Nicholas JG, Geers AE. Effects of early auditory experience on the spoken language of deaf children at 3 years of age. Ear and Hearing. 2006;27:286–298. doi: 10.1097/01.aud.0000215973.76912.c6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan BA. Basic measures of child language. In: Sokolov JL, Snow CE, editors. Handbook of research in language development using CHILDES. Lawrence Erlbaum Associates; Hillsdale, NJ: 1994. [Google Scholar]
- Paul R. Language disorders: From infancy through adolescence. 2nd edition Mosby Publishing; St. Louis, MO: 2001. [Google Scholar]
- Richter B, Eissele S, Laszig R, Lohle E. Receptive and expressive language skills of 106 children with a minimum of 2 years' experience in hearing with a cochlear implant. International Journal of Pediatric Otorhinolaryngology. 2002;64:111–125. doi: 10.1016/s0165-5876(02)00037-x. [DOI] [PubMed] [Google Scholar]
- Robbins AM, Koch DB, Osberger MJ, Zimmerman-Phillips S, Kishon-Rabin L. Effect of age at cochlear implantation on auditory skill development in infants and toddlers. Archives of Otolaryngology, Head and Neck Surgery. 2004;130:570–574. doi: 10.1001/archotol.130.5.570. [DOI] [PubMed] [Google Scholar]
- Robinson K. Implications of developmental plasticity for the language acquisition of deaf children with cochlear implants. International Journal of Pediatric Otorhinolaryngology. 1998;46:71–80. doi: 10.1016/s0165-5876(98)00125-6. [DOI] [PubMed] [Google Scholar]
- Roid GH, Miller LJ. Leiter International Performance Scale – Revised. Stoelting Company; Wood Dale, IL: 1997. [Google Scholar]
- Ryugo DK, Kretzmer EA, Niparko JK. Restoration of auditory nerve synapses in cats by cochlear implants. Science. 2005;310:1490–1492. doi: 10.1126/science.1119419. [DOI] [PubMed] [Google Scholar]
- Sharma A, Tobey E, Dorman M, Bharadwaj S, Martin K, Gilley P, Kunkel F. Central auditory maturation and babbling development in infants with cochlear implants. Archives of Otolaryngology: Head and Neck Surgery. 2004;130:511–516. doi: 10.1001/archotol.130.5.511. [DOI] [PubMed] [Google Scholar]
- Sparrow S, Balla D, Cicchetti D. Vineland Adaptive Behavior Scales. American Guidance Service; Circle Pines, MN: 1984. [Google Scholar]
- Spencer PS. Individual differences in language performance after cochlear implantation at one to three years of age: Child, family, and linguistic factors. Journal of Deaf Studies and Deaf Education. 2004;9:395–412. doi: 10.1093/deafed/enh033. [DOI] [PubMed] [Google Scholar]
- Stacey PC, Fortnum HM, Barton GR, Summerfield AQ. Hearing-impaired children in the United Kingdom, I: Auditory performance, communication skills, educational achievements, quality of life, and cochlear implantation. Ear and Hearing. 2006;27:161–186. doi: 10.1097/01.aud.0000202353.37567.b4. [DOI] [PubMed] [Google Scholar]
- Svirsky MA, Robbins AM, Kirk KI, Pisoni DB, Miyamoto RT. Language development in profoundly deaf children with cochlear implants. Psychological Science. 2000;11:153–158. doi: 10.1111/1467-9280.00231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svirsky MA, Teoh S-W, Neuburger H. Development of language and speech perception in congenitally, profoundly deaf children as a function of age at cochlear implantation. Audiology and Neuro-Otology. 2004;9:224–233. doi: 10.1159/000078392. [DOI] [PubMed] [Google Scholar]
- Szagun G. Language acquisition in young German-speaking children with cochlear implants: Individual differences and implications for conceptions of a ‘sensitive phase’. Audiology and Neuro-Otology. 2001;6:288–297. doi: 10.1159/000046134. [DOI] [PubMed] [Google Scholar]
- Tomblin JB, Barker BA, Spencer LJ, Zhang X, Gantz BJ. The effect of age at cochlear implant initial stimulation on expressive language growth in infants and toddlers. Journal of Speech, Language, and Hearing Research. 2005;48:853–867. doi: 10.1044/1092-4388(2005/059). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyler RS, Teagle HF, Kelsay DM, Gantz BJ, Woodworth GG, Parkinson AJ. Speech perception by prelingually deaf children after six years of cochlear implant use: Effects of age at implant. International Journal of Language and Communication Disorders. 2001;36(Supp):82–84. doi: 10.1177/0003489400109s1235. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Preschool and Primary Scale of Intelligence. 3rd Ed. The Psychological Corp; San Antonio, TX: 2002. [Google Scholar]
- Zimmerman IL, Steiner VG, Pond RE. Preschool Language Scale. 3rd edition Psychological Corp; San Antonio, TX: 1992. [Google Scholar]
- Zwolan TA, Ashbaugh CM, Alarfaj A, Kileny PR, Arts HA, El-Kashlan HK, et al. Pediatric cochlear implant patient performance as a function of age at implantation. Otology & Neuro-Otology. 2004;25:112–120. doi: 10.1097/00129492-200403000-00006. [DOI] [PubMed] [Google Scholar]
- Zwolan TA, Zimmerman-Phillips S, Ashbaugh CJ, Hieber SJ, Kileny PR, Telian SA. Cochlear implantation of children with minimal open-set speech recognition skills. Ear and Hearing. 1997;18:240–251. doi: 10.1097/00003446-199706000-00007. [DOI] [PubMed] [Google Scholar]