Abstract
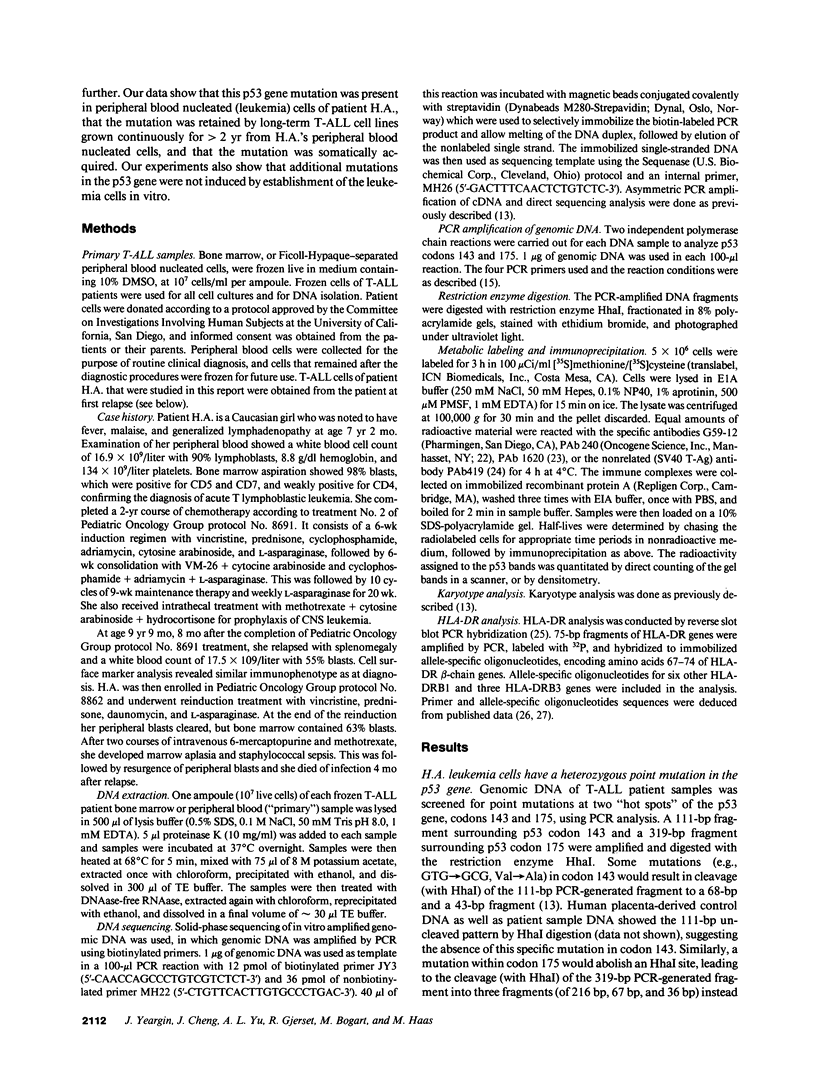
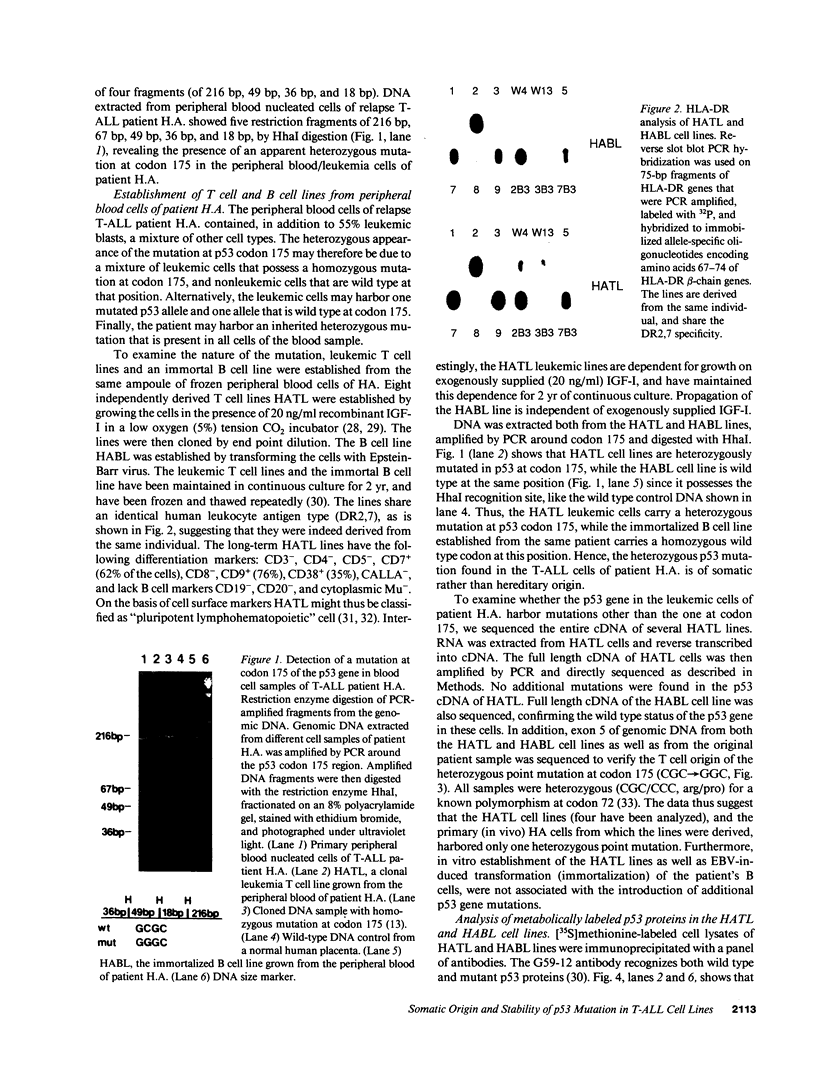
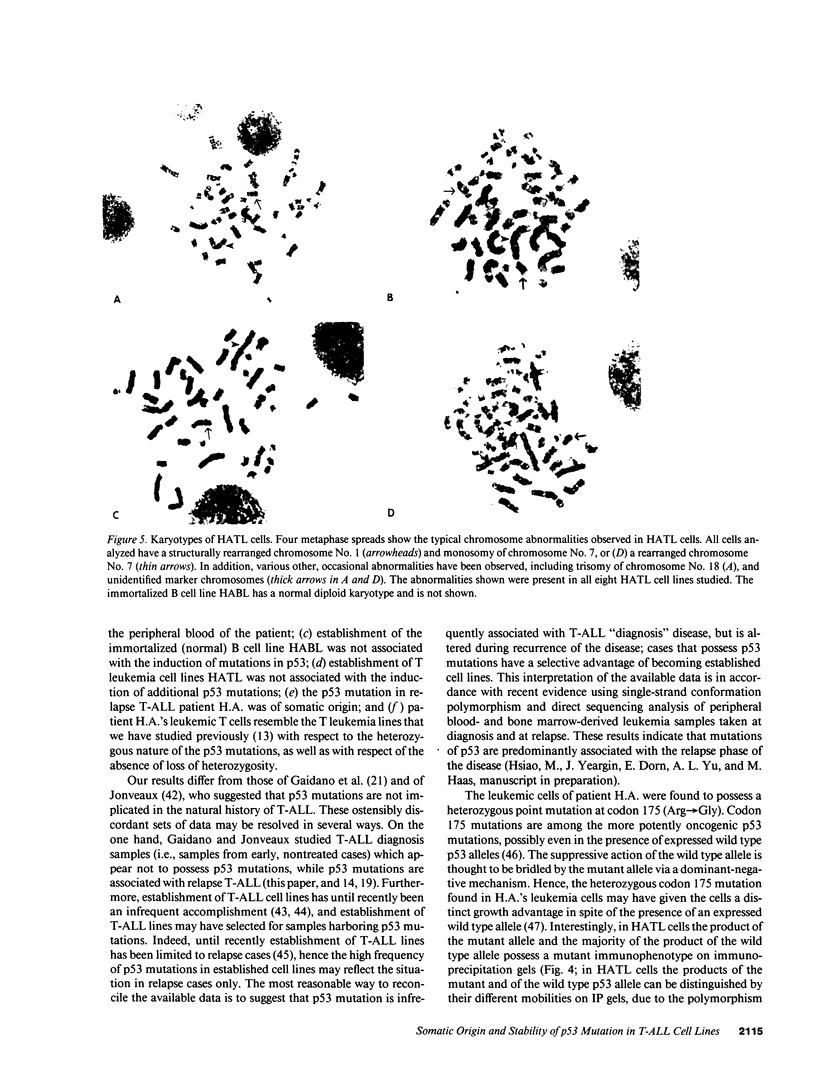
Samples donated by patients with T cell acute lymphoblastic leukemia (T-ALL) were screened for mutations of the p53 tumor suppressor gene. Peripheral blood cells of T-ALL relapse patient H.A. were found to possess a heterozygous point mutation at codon 175 of the p53 gene. To determine whether this was an inherited mutation, a B cell line (HABL) was established. Leukemic T cell lines (HATL) were concurrently established by growing peripheral blood leukemic T cells at low oxygen tension in medium supplemented with IGF-I. Previously we had shown that > 60% of leukemic T cell lines possessed mutations in the p53 gene (Cheng, J., and M. Hass. 1990. Mol. Cell. Biol. 10:5502), mutations that might have originated with the donor's leukemic cells, or might have been induced during establishment of the cell lines. To answer whether establishment of the HATL lines was associated with the induction of p53 mutations, cDNAs of the HATL and HABL lines were sequenced. The HATL lines retained the same heterozygous p53 mutation that was present in the patient's leukemic cells. The HABL line lacked p53 mutations. Immunoprecipitation with specific anti-p53 antibodies showed that HATL cells produced p53 proteins of mutant and wild type immunophenotype, while the HABL line synthesized only wild-type p53 protein. The HATL cells had an abnormal karyotype, while the HABL cells possessed a normal diploid karyotype. These experiments suggest that (a) p53 mutation occurred in the leukemic cells of relapse T-ALL patient HA; (b) the mutation was of somatic rather than hereditary origin; (c) the mutation was leukemia associated; and (d) establishment of human leukemia cell lines needs not be associated with in vitro induction of p53 mutations. It may be significant that patient HA belonged to a category of relapse T-ALL patients in whom a second remission could not be induced.
Full text
PDF



Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ahuja H., Bar-Eli M., Advani S. H., Benchimol S., Cline M. J. Alterations in the p53 gene and the clonal evolution of the blast crisis of chronic myelocytic leukemia. Proc Natl Acad Sci U S A. 1989 Sep;86(17):6783–6787. doi: 10.1073/pnas.86.17.6783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker S. J., Fearon E. R., Nigro J. M., Hamilton S. R., Preisinger A. C., Jessup J. M., vanTuinen P., Ledbetter D. H., Barker D. F., Nakamura Y. Chromosome 17 deletions and p53 gene mutations in colorectal carcinomas. Science. 1989 Apr 14;244(4901):217–221. doi: 10.1126/science.2649981. [DOI] [PubMed] [Google Scholar]
- Ball R. K., Siegl B., Quellhorst S., Brandner G., Braun D. G. Monoclonal antibodies against simian virus 40 nuclear large T tumour antigen: epitope mapping, papova virus cross-reaction and cell surface staining. EMBO J. 1984 Jul;3(7):1485–1491. doi: 10.1002/j.1460-2075.1984.tb02000.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell J. I., Denney D., Jr, Foster L., Belt T., Todd J. A., McDevitt H. O. Allelic variation in the DR subregion of the human major histocompatibility complex. Proc Natl Acad Sci U S A. 1987 Sep;84(17):6234–6238. doi: 10.1073/pnas.84.17.6234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bressac B., Kew M., Wands J., Ozturk M. Selective G to T mutations of p53 gene in hepatocellular carcinoma from southern Africa. Nature. 1991 Apr 4;350(6317):429–431. doi: 10.1038/350429a0. [DOI] [PubMed] [Google Scholar]
- Brodeur G. M., Saylors R. L., 3rd Neuroblastoma, retinoblastoma, and brain tumors in children. Curr Opin Oncol. 1991 Jun;3(3):485–496. doi: 10.1097/00001622-199106000-00007. [DOI] [PubMed] [Google Scholar]
- Cabanillas F., Pathak S., Grant G., Hagemeister F. B., McLaughlin P., Swan F., Rodriguez M. A., Trujillo J., Cork A., Butler J. J. Refractoriness to chemotherapy and poor survival related to abnormalities of chromosomes 17 and 7 in lymphoma. Am J Med. 1989 Aug;87(2):167–172. doi: 10.1016/s0002-9343(89)80692-8. [DOI] [PubMed] [Google Scholar]
- Chen P. L., Chen Y. M., Bookstein R., Lee W. H. Genetic mechanisms of tumor suppression by the human p53 gene. Science. 1990 Dec 14;250(4987):1576–1580. doi: 10.1126/science.2274789. [DOI] [PubMed] [Google Scholar]
- Cheng J., Haas M. Frequent mutations in the p53 tumor suppressor gene in human leukemia T-cell lines. Mol Cell Biol. 1990 Oct;10(10):5502–5509. doi: 10.1128/mcb.10.10.5502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng J., Yee J. K., Yeargin J., Friedmann T., Haas M. Suppression of acute lymphoblastic leukemia by the human wild-type p53 gene. Cancer Res. 1992 Jan 1;52(1):222–226. [PubMed] [Google Scholar]
- Diller L., Kassel J., Nelson C. E., Gryka M. A., Litwak G., Gebhardt M., Bressac B., Ozturk M., Baker S. J., Vogelstein B. p53 functions as a cell cycle control protein in osteosarcomas. Mol Cell Biol. 1990 Nov;10(11):5772–5781. doi: 10.1128/mcb.10.11.5772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinstein E., Cimino G., Gale R. P., Alimena G., Berthier R., Kishi K., Goldman J., Zaccaria A., Berrebi A., Canaani E. p53 in chronic myelogenous leukemia in acute phase. Proc Natl Acad Sci U S A. 1991 Jul 15;88(14):6293–6297. doi: 10.1073/pnas.88.14.6293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felix C. A., D'Amico D., Mitsudomi T., Nau M. M., Li F. P., Fraumeni J. F., Jr, Cole D. E., McCalla J., Reaman G. H., Whang-Peng J. Absence of hereditary p53 mutations in 10 familial leukemia pedigrees. J Clin Invest. 1992 Aug;90(2):653–658. doi: 10.1172/JCI115907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felix C. A., Nau M. M., Takahashi T., Mitsudomi T., Chiba I., Poplack D. G., Reaman G. H., Cole D. E., Letterio J. J., Whang-Peng J. Hereditary and acquired p53 gene mutations in childhood acute lymphoblastic leukemia. J Clin Invest. 1992 Feb;89(2):640–647. doi: 10.1172/JCI115630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlay C. A., Hinds P. W., Levine A. J. The p53 proto-oncogene can act as a suppressor of transformation. Cell. 1989 Jun 30;57(7):1083–1093. doi: 10.1016/0092-8674(89)90045-7. [DOI] [PubMed] [Google Scholar]
- Gaidano G., Ballerini P., Gong J. Z., Inghirami G., Neri A., Newcomb E. W., Magrath I. T., Knowles D. M., Dalla-Favera R. p53 mutations in human lymphoid malignancies: association with Burkitt lymphoma and chronic lymphocytic leukemia. Proc Natl Acad Sci U S A. 1991 Jun 15;88(12):5413–5417. doi: 10.1073/pnas.88.12.5413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gannon J. V., Greaves R., Iggo R., Lane D. P. Activating mutations in p53 produce a common conformational effect. A monoclonal antibody specific for the mutant form. EMBO J. 1990 May;9(5):1595–1602. doi: 10.1002/j.1460-2075.1990.tb08279.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gjerset R. A., Yeargin J., Volkman S. K., Vila V., Arya J., Haas M. Insulin-like growth factor-I supports proliferation of autocrine thymic lymphoma cells with a pre-T cell phenotype. J Immunol. 1990 Nov 15;145(10):3497–3501. [PubMed] [Google Scholar]
- Gregersen P. K., Shen M., Song Q. L., Merryman P., Degar S., Seki T., Maccari J., Goldberg D., Murphy H., Schwenzer J. Molecular diversity of HLA-DR4 haplotypes. Proc Natl Acad Sci U S A. 1986 Apr;83(8):2642–2646. doi: 10.1073/pnas.83.8.2642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas M., Yu A., Gjerset R. Characteristics of the leukemic cell in childhood acute lymphoblastic T cell leukemia at diagnosis. Leukemia. 1990 Mar;4(3):230–234. [PubMed] [Google Scholar]
- Harlow E., Crawford L. V., Pim D. C., Williamson N. M. Monoclonal antibodies specific for simian virus 40 tumor antigens. J Virol. 1981 Sep;39(3):861–869. doi: 10.1128/jvi.39.3.861-869.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris N., Brill E., Shohat O., Prokocimer M., Wolf D., Arai N., Rotter V. Molecular basis for heterogeneity of the human p53 protein. Mol Cell Biol. 1986 Dec;6(12):4650–4656. doi: 10.1128/mcb.6.12.4650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey D. M., Levine A. J. p53 alteration is a common event in the spontaneous immortalization of primary BALB/c murine embryo fibroblasts. Genes Dev. 1991 Dec;5(12B):2375–2385. doi: 10.1101/gad.5.12b.2375. [DOI] [PubMed] [Google Scholar]
- Hinds P. W., Finlay C. A., Quartin R. S., Baker S. J., Fearon E. R., Vogelstein B., Levine A. J. Mutant p53 DNA clones from human colon carcinomas cooperate with ras in transforming primary rat cells: a comparison of the "hot spot" mutant phenotypes. Cell Growth Differ. 1990 Dec;1(12):571–580. [PubMed] [Google Scholar]
- Hirose M., Minato K., Tobinai K., Shimoyama M., Watanabe S., Abe T., Deura K. Two novel cultured cell lines, A3/Kawakami and A4/Fukuda, derived from malignant lymphoma of B(non-T)-cell nature of the gastrointestinal tract. Gan. 1983 Feb;74(1):106–115. [PubMed] [Google Scholar]
- Hsu I. C., Metcalf R. A., Sun T., Welsh J. A., Wang N. J., Harris C. C. Mutational hotspot in the p53 gene in human hepatocellular carcinomas. Nature. 1991 Apr 4;350(6317):427–428. doi: 10.1038/350427a0. [DOI] [PubMed] [Google Scholar]
- Huang C. C., Hou Y., Woods L. K., Moore G. E., Minowada J. Cytogenetic study of human lymphoid T-cell lines derived from lymphocytic leukemia. J Natl Cancer Inst. 1974 Sep;53(3):655–660. doi: 10.1093/jnci/53.3.655. [DOI] [PubMed] [Google Scholar]
- Iggo R., Gatter K., Bartek J., Lane D., Harris A. L. Increased expression of mutant forms of p53 oncogene in primary lung cancer. Lancet. 1990 Mar 24;335(8691):675–679. doi: 10.1016/0140-6736(90)90801-b. [DOI] [PubMed] [Google Scholar]
- Jonveaux P., Berger R. Infrequent mutations in the P53 gene in primary human T-cell acute lymphoblastic leukemia. Leukemia. 1991 Oct;5(10):839–840. [PubMed] [Google Scholar]
- Kelman Z., Prokocimer M., Peller S., Kahn Y., Rechavi G., Manor Y., Cohen A., Rotter V. Rearrangements in the p53 gene in Philadelphia chromosome positive chronic myelogenous leukemia. Blood. 1989 Nov 15;74(7):2318–2324. [PubMed] [Google Scholar]
- Koeffler H. P., Miller C., Nicolson M. A., Ranyard J., Bosselman R. A. Increased expression of p53 protein in human leukemia cells. Proc Natl Acad Sci U S A. 1986 Jun;83(11):4035–4039. doi: 10.1073/pnas.83.11.4035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurtzberg J., Bigner S. H., Hershfield M. S. Establishment of the DU.528 human lymphohemopoietic stem cell line. J Exp Med. 1985 Nov 1;162(5):1561–1578. doi: 10.1084/jem.162.5.1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurtzberg J., Waldmann T. A., Davey M. P., Bigner S. H., Moore J. O., Hershfield M. S., Haynes B. F. CD7+, CD4-, CD8- acute leukemia: a syndrome of malignant pluripotent lymphohematopoietic cells. Blood. 1989 Feb;73(2):381–390. [PubMed] [Google Scholar]
- Lane D. P., Crawford L. V. T antigen is bound to a host protein in SV40-transformed cells. Nature. 1979 Mar 15;278(5701):261–263. doi: 10.1038/278261a0. [DOI] [PubMed] [Google Scholar]
- Malkin D., Li F. P., Strong L. C., Fraumeni J. F., Jr, Nelson C. E., Kim D. H., Kassel J., Gryka M. A., Bischoff F. Z., Tainsky M. A. Germ line p53 mutations in a familial syndrome of breast cancer, sarcomas, and other neoplasms. Science. 1990 Nov 30;250(4985):1233–1238. doi: 10.1126/science.1978757. [DOI] [PubMed] [Google Scholar]
- Marks J. R., Davidoff A. M., Kerns B. J., Humphrey P. A., Pence J. C., Dodge R. K., Clarke-Pearson D. L., Iglehart J. D., Bast R. C., Jr, Berchuck A. Overexpression and mutation of p53 in epithelial ovarian cancer. Cancer Res. 1991 Jun 1;51(11):2979–2984. [PubMed] [Google Scholar]
- Mashal R., Shtalrid M., Talpaz M., Kantarjian H., Smith L., Beran M., Cork A., Trujillo J., Gutterman J., Deisseroth A. Rearrangement and expression of p53 in the chronic phase and blast crisis of chronic myelogenous leukemia. Blood. 1990 Jan 1;75(1):180–189. [PubMed] [Google Scholar]
- Masuda H., Miller C., Koeffler H. P., Battifora H., Cline M. J. Rearrangement of the p53 gene in human osteogenic sarcomas. Proc Natl Acad Sci U S A. 1987 Nov;84(21):7716–7719. doi: 10.1073/pnas.84.21.7716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercer W. E., Shields M. T., Amin M., Sauve G. J., Appella E., Romano J. W., Ullrich S. J. Negative growth regulation in a glioblastoma tumor cell line that conditionally expresses human wild-type p53. Proc Natl Acad Sci U S A. 1990 Aug;87(16):6166–6170. doi: 10.1073/pnas.87.16.6166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milner J., Medcalf E. A. Cotranslation of activated mutant p53 with wild type drives the wild-type p53 protein into the mutant conformation. Cell. 1991 May 31;65(5):765–774. doi: 10.1016/0092-8674(91)90384-b. [DOI] [PubMed] [Google Scholar]
- Nigro J. M., Baker S. J., Preisinger A. C., Jessup J. M., Hostetter R., Cleary K., Bigner S. H., Davidson N., Baylin S., Devilee P. Mutations in the p53 gene occur in diverse human tumour types. Nature. 1989 Dec 7;342(6250):705–708. doi: 10.1038/342705a0. [DOI] [PubMed] [Google Scholar]
- Prokocimer M., Shaklai M., Bassat H. B., Wolf D., Goldfinger N., Rotter V. Expression of p53 in human leukemia and lymphoma. Blood. 1986 Jul;68(1):113–118. [PubMed] [Google Scholar]
- Saiki R. K., Walsh P. S., Levenson C. H., Erlich H. A. Genetic analysis of amplified DNA with immobilized sequence-specific oligonucleotide probes. Proc Natl Acad Sci U S A. 1989 Aug;86(16):6230–6234. doi: 10.1073/pnas.86.16.6230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirasawa S., Urabe K., Yanagawa Y., Toshitani K., Iwama T., Sasazuki T. p53 gene mutations in colorectal tumors from patients with familial polyposis coli. Cancer Res. 1991 Jun 1;51(11):2874–2878. [PubMed] [Google Scholar]
- Sidransky D., Von Eschenbach A., Tsai Y. C., Jones P., Summerhayes I., Marshall F., Paul M., Green P., Hamilton S. R., Frost P. Identification of p53 gene mutations in bladder cancers and urine samples. Science. 1991 May 3;252(5006):706–709. doi: 10.1126/science.2024123. [DOI] [PubMed] [Google Scholar]
- Smith S. D., McFall P., Morgan R., Link M., Hecht F., Cleary M., Sklar J. Long-term growth of malignant thymocytes in vitro. Blood. 1989 Jun;73(8):2182–2187. [PubMed] [Google Scholar]
- Srivastava S., Zou Z. Q., Pirollo K., Blattner W., Chang E. H. Germ-line transmission of a mutated p53 gene in a cancer-prone family with Li-Fraumeni syndrome. Nature. 1990 Dec 20;348(6303):747–749. doi: 10.1038/348747a0. [DOI] [PubMed] [Google Scholar]
- Takahashi T., Nau M. M., Chiba I., Birrer M. J., Rosenberg R. K., Vinocour M., Levitt M., Pass H., Gazdar A. F., Minna J. D. p53: a frequent target for genetic abnormalities in lung cancer. Science. 1989 Oct 27;246(4929):491–494. doi: 10.1126/science.2554494. [DOI] [PubMed] [Google Scholar]
- Varley J. M., Brammar W. J., Lane D. P., Swallow J. E., Dolan C., Walker R. A. Loss of chromosome 17p13 sequences and mutation of p53 in human breast carcinomas. Oncogene. 1991 Mar;6(3):413–421. [PubMed] [Google Scholar]
- Yeargin J., Cheng J., Haas M. Role of the p53 tumor suppressor gene in the pathogenesis and in the suppression of acute lymphoblastic T-cell leukemia. Leukemia. 1992;6 (Suppl 3):85S–91S. [PubMed] [Google Scholar]













