Summary
The diagnosis of lateral canalolithiasis is based on the typical finding of the horizontal paroxysmal positional nystagmus induced by the Pagnini-Mc Clure manoeuvre. This technique usually identifies also the affected side, namely, the side where the paroxysmal nystagmus is more intense in geotropic forms and the side where the paroxysmal nystagmus is less intense in apogeotropic forms. However, this method is not always applicable since, especially in apogeotropic forms, the intensity of the nystagmus is not so distinctly different between the two sides. Further useful signs to identify the affected side have been described in the Literature: Pseudo-spontaneous nystagmus in the sitting position; Leaning and Bowing nystagmus; Null-point in the vertical plane; Sitting to supine positioning nystagmus; Null-point in the horizontal plane. They are fully explained at pathophysiological level by the mechanism of canalolithiasis, as they are caused by otoliths moving in the ampullopetal direction in the non-ampullary segment (geotropic canalolithiasis) of the lateral canal or in ampullofugal direction in the ampullary segment (apogeotropic canalolithiasis) of the lateral canal. In other words, the movement of otoliths determines excitatory or inhibitory endolymphatic flow that generates specific nystagmic eye-movements. Authors analyse the characteristics of these signs, that they define as “Secondary signs of lateralization”, in 64 cases of apogeotropic lateral canalolithiasis. A decisive contribution of the “Secondary signs of lateralization” to diagnose the pathological side has been verified in 13 out of 64 cases, whereas, in all other cases, Pagnini-Mc Clure diagnostic manoeuvre proved successful in correctly identifying the affected side by itself. Among the “Secondary signs of lateralization”, the Pseudo-spontaneous nystagmus in the sitting position and the Sitting to the supine positioning nystagmus were particularly useful, due to both their frequency and their easy detection, as they do not require additional manoeuvres besides those usually performed during health examination of a patient affected by lateral canalolithiasis. In conclusion, the Authors propose a decision-making algorithm to diagnose and treat lateral canalolithiasis based on the attempt to obtain as much information as possible for a correct diagnosis, with the least trouble and inconvenience for patients.
Keywords: Benign paroxysmal positional vertigo, Lateral canalolithiasis, Paroxysmal nystagmus
Riassunto
La diagnosi di canalolitiasi laterale si basa sul tipico reperto del nistagmo parossistico da posizionamento evocato dalla manovra diagnostica di Pagnini-McClure. Mediante tale metodo, il lato affetto è quello in cui il nistagmo parossistico è più intenso nel caso delle forme geotrope ed il lato dove il nistagmo parossistico è meno intenso nelle forme apogeotrope. Tale criterio, però, non sempre è applicabile in quanto, specie nelle forme apogeotrope, l’intensità del nistagmo non è chiaramente diversa tra i due lati. Altri segni utili ad identificare il lato affetto sono stati descritti in Letteratura: nistagmo pseudospontaneo in posizione seduta; leaning e bowing nystagmus; null-point sul piano verticale; nistagmo da posizionamento dalla posizione seduta alla posizione supina; null-point sul piano orizzontale. Essi trovano una unica giustificazione fisiopatologica nel meccanismo della canalolitiasi, essendo generati dai movimenti ampullipeti o ampullifughi degli otoliti nel braccio ampollare (canalolitiasi apogeotropa) o nel braccio non ampollare (canalolitiasi geotropa) del canale laterale, che provocano correnti endolinfatiche eccitatorie od inibitorie dell’attività del canale interessato. Gli Autori analizzano il comportamento di tali segni, che essi definiscono “segni secondari di lateralità”, in una serie di 64 canalolitiasi laterali apogeotrope. Un contributo decisivo dei “segni secondari di lateralità” alla diagnosi di lato è stato riscontrato in 13/64 casi, laddove negli altri casi la manovra di Pagnini-McClure, che resta lo specifico mezzo diagnostico della canalolitiasi laterale, si è rivelata da sola sufficiente anche alla corretta identificazione del lato affetto. Nell’ambito di tali segni, il nistagmo pseudospontaneo in posizione seduta ed il nistagmo da posizionamento dalla posizione seduta alla posizione supina sono quelli che si sono rivelati particolarmente utili, sia per la loro frequenza, sia per la facilità di osservazione, in quanto non necessitano di alcuna manovra aggiuntiva rispetto a quelle che si compiono abitualmente nell’analisi clinica di un paziente affetto da canalolitiasi laterale. Gli Autori propongono infine un algoritmo decisionale per la diagnosi ed il trattamento delle canalolitiasi laterali, basato sul criterio di ottenere il massimo di informazione utile alla diagnosi con il minimo fastidio da arrecare al paziente.
Introduction
The lateral canal benign paroxysmal positional vertigo, which was first described in the Literature in 1985 1 2, is characterized by a horizontal bidirectional bipositional paroxysmal nystagmus induced by the Pagnini-Mc Clure manoeuvre (Head roll test in the supine position) 2 3.
Lateral canalolithiasis represents from 15% to 20% of all canalolithiases, and it can present a geotropic form with quick phases of the horizontal positioning paroxysmal nystagmus directed toward the lowermost ear, or an apogeotropic* form, with quick phases of the nystagmus directed toward the uppermost ear.
The geotropic form is due to a canalolithiasis of the non-ampullary segment of the lateral canal, while the apogeotropic form is due either to a canalolithiasis of the ampullary segment of the lateral canal or to a lateral cupulolithiasis.
In order to understand the different intensity of the nystagmus induced by the diagnostic Pagnini-McClure manoeuvre, it is necessary to be aware that the excitatory nystagmus in the lateral canal is stronger than the inhibitory nystagmus, by Ewald’s second law.
In geotropic forms, when the patient lies on the affected side, otoliths fall in an ampullopetal direction, causing an excitatory stimulation, whereas in apogeotropic forms, ampullopetal flow and excitatory stimulation are present when the patient’s head is rotated towards the healthy side, namely, the side where the nystagmus will, therefore, be more violent.
Identification of the affected ear is fundamental in order to choose the side towards which a therapeutic manoeuvre should be performed.
In the geotropic form of lateral canalolithiasis, therapeutic manoeuvres are directed toward the healthy side; in the apogeotropic form, barbecue rotation manoeuvres are directed toward the healthy side 4, while the first step both of Gufoni’s manoeuvre 5 6 and of Vannucchi’s “Forced Prolonged Position” 7 is directed toward the affected ear and if they cause the transformation into a geotropic form, their second step is directed toward the healthy side.
However, the principle to assess the differential intensity of the nystagmus based on Ewald’s second law is not always relevant, as sometimes a clear difference between the two sides is not easily recognized: this occurs more frequently in apogeotropic forms.
In such cases, a search for other signs of laterality is essential to determine the affected side.
In the Literature, many signs are described: we call them “secondary signs of lateralization” (SSL).
In the sitting position, we have to search for: “pseudo-spontaneous” nystagmus 8 9, “null-point” in the pitch plane 9 10, “bowing and leaning” nystagmus 11, “bending nystagmus” 12, “head shaking induced nystagmus” (HSIN).
The pseudo-spontaneous nystagmus can be detected at rest and can be further highlighted or evoked by head turning to either side by a mild head shaking at about 0.5 Hz 9: in this case, however, our opinion is that we have to consider it as an evoked nystagmus.
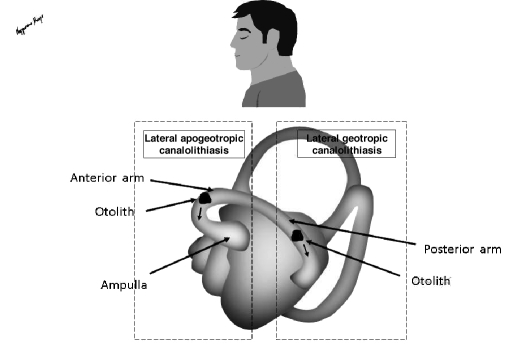
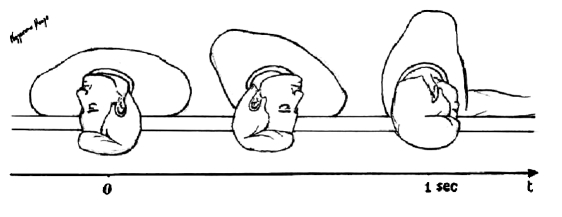
According to Asprella-Libonati 8 9, it is due to the slight movement of otoliths in the lateral semicircular canal (LSC), in an ampullofugal direction in geotropic forms and in an ampullopetal direction in apogeotropic forms, so that, in geotropic forms, the pseudo-spontaneous nystagmus beats towards the healthy side, while in apogeotropic forms it is directed towards the affected side (Fig. 1).
Fig. 1.
Mechanism of pseudospontaneous nystagmus in apogeotropic and geotropic canalolithiasis (left lateral canal: lateral view).
When present, the pseudo-spontaneous nystagmus can be blocked with an inclination of approximately 30° in the vertical plane (null-point on the pitch-plane), as observed by Bissdorff and Debatisse 10 and Asprella-Libonati 9 and it can be inverted by a maximal anterior flexion of the head 9.
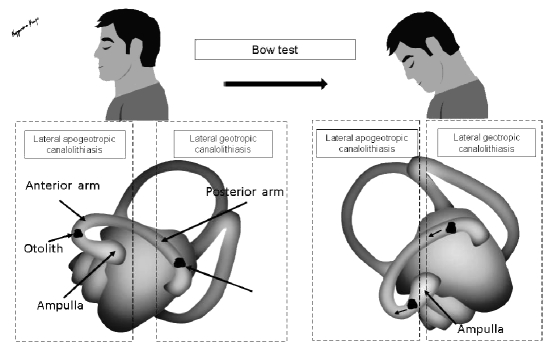
The bow and lean test (BLT) 11 consists of a manoeuvre of neck flexion and extension.
During the neck flexion, the test determines an ampullopetal endolymphatic flow in geotropic forms (“bowing” nystagmus directed toward the affected side) and an ampullofugal endolymphatic flow in apogeotropic forms (“bowing” nystagmus toward the healthy side) (Fig. 2).
Fig. 2.
Mechanism of bowing nystagmus in apogeotropic and geotropic canalolithiasis (left lateral canal: lateral view).
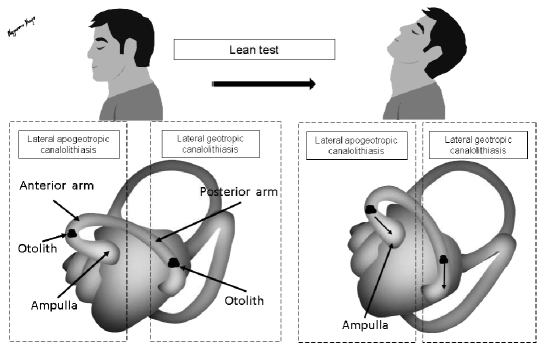
During the neck extension, the test determines opposite endolymphatic flow and then a horizontal nystagmus towards the healthy side in geotropic forms and towards the affected side in apogeotropic forms (“leaning” nystagmus) (Fig. 3).
Fig. 3.
Mechanism of leaning nystagmus in apogeotropic and geotropic canalolithiasis (left lateral canal: lateral view).
The bending test 12 consists in searching for nystagmus induced only by a forward neck flexion. The “bending” nystagmus is identical to the bowing nystagmus induced by BLT: the only difference is the word used by the Authors who described these tests 11 12.
Leaning and bowing/bending nystagmus are often only changes of the pseudo-spontaneous nystagmus, induced by the different positioning of the head, but sometimes they are observed even if the pseudo-spontaneous nystagmus is absent: in these cases, they have been considered as positioning evoked nystagmus.
After the head shaking test at about 2 Hz, HSIN with quick phases directed toward the healthy side can be recognized; its direction toward the healthy side is stable even after an eventual reversal from an apogeotropic into a geotropic form of the lateral canalolithiasis.
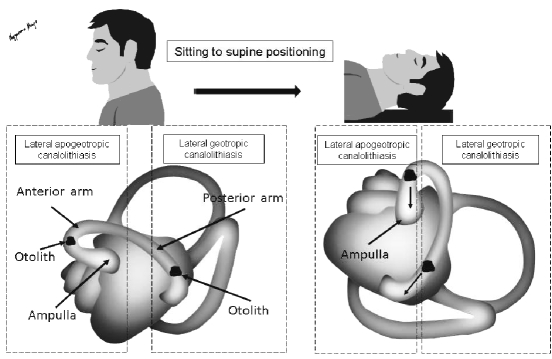
When the patient is brought from the sitting to the supine position, a flow of otoliths in the LSC may occur in an ampullofugal direction in geotropic forms and in an ampullopetal direction in apogeotropic forms (Fig. 4): a nystagmus (sitting to supine positioning nystagmus) directed toward the healthy side in geotropic forms and toward the affected side in apogeotropic forms can thus be detected. It was described by Nuti et al. 13 14 and then resumed by Han et al. 15 and Koo et al. 16.
Fig. 4.
Mechanism of sitting to supine positioning nystagmus in apogeotropic and geotropic canalolithiasis (left lateral canal: lateral view).
During the Pagnini-Mc Clure manoeuvre it is mandatory to observe both the direction and the different intensity of the horizontal bipositional paroxysmal nystagmus, the eventual second phase (spontaneous reversal) of the paroxysmal nystagmus, the null-point in the yaw plane, as described by Bissdorff and Debatisse in apogeotropic forms 10 and by Hiroaki 17 in geotropic forms.
The second nystagmic phase is usually observed on the side where the nystagmus has a greater intensity: namely, the affected side in geotropic forms and the healthy side in apogeotropic forms, where, however, this sign is less frequent.
The reversal of paroxysmal nystagmus from an apogeotropic to a geotropic form can be achieved with repeated lateral head rotations to either side, slowly towards the healthy side and quickly towards the affected side 14.
The conversion into a geotropic canalolithiasis makes the therapeutic manoeuvre easier, even though, in our opinion, the repeated positioning that is sometimes necessary when trying to achieve it, may result in unpleasant complaints for the patient.
Moreover, the subjective sensation reported by the patient must be taken into consideration, as it often gives a correct indication as to the side that mainly aches.
After a therapeutic manoeuvre, the resolution of the pathology is observed, as well as the transformation from an apogeotropic into a geotropic form, with change of direction of SSL, also (except of HSIN), the transformation from lateral into posterior canalolithiasis, the persistence of the pathological condition.
These observations offer the possibility to determine whether the choice of the affected side was right or wrong.
In the present survey, both the methods were applied in detecting the affected side of the apogeotropic lateral canalolithiasis: the differential intensity of the nystagmus evoked by the Pagnini-McClure manoeuvre and the direction of SSL, when present.
Other reports have referred to the application of just a sign 8–12 14–16.
All the reported signs were applied to verify the efficiency of the two methods in the correct diagnosis of the affected side and verify which is the simplest and more specific way to identify the affected side of apogeotropic lateral canalolithiasis.
Patients and methods
From May 2008 to August 2009, 824 cases of canalolithiasis were observed: 664 posterior canalolithiasis (80.6%) and 160 lateral canalolithiasis (19.4%).
In lateral canalolithiasis, geotropic forms accounted for 96 cases (60%), apogeotropic forms for 64 (40%): this analysis concerns the 64 cases of apogeotropic lateral canalolithiasis.
The diagnosis of apogeotropic lateral canalolithiasis was carried out if the Pagnini-McClure manoeuvre evoked the typical horizontal bilateral bidirectional paroxysmal apogeotropic nystagmus (primary diagnostic sign); using this method, the side where the paroxysmal nystagmus was less intense was considered the side affected.
A search was also made for the SSL, using the above-mentioned procedure to identify the affected side.
Then, a comparison was made of the indication of the affected side using the classic method (differential intensity of the paroxysmal nystagmus induced by the Pagnini-McClure manoeuvre) and the directions of nystagmus in SSL.
Observations were carried out by video-nystagmoscopic examination and videonystagmography recording (VNG Ulmer, Marseille, France).
Patients group
Patients comprised 38 females and 26 males (mean age 51.3 ± 10.67 years, range 19-82).
Once the diagnosis of the affected side was made, patients were treated by Gufoni’s manoeuvre (GM).
The first step of GM was performed on the affected side, while a second step on the healthy side was performed if the first step transformed the apogeotropic canalolithiasis into a geotropic form.
When apogeotropic canalolithiasis was converted into the geotropic form by repeated head roll manoeuvres in the horizontal plane, GM was performed towards the healthy side.
All the patients were controlled after one day, searching again for horizontal bilateral bidirectional paroxysmal nystagmus evoked by the Pagnini-McClure manoeuvre and for the torsional paroxysmal nystagmus evoked by the Dix-Hallpike positioning, because of the possible conversion into a posterior canalolithiasis.
If GM transformed lateral canalolithiasis into posterior canalolithiasis, it was treated by the “Quick Liberatory Rotation” manoeuvre (QLR) 18: two minutes after the paroxysmal torsional nystagmus disappears, the patient is turned from the affected to the contralateral side by a quick rotation (less than one second) of the head of about 180° in the horizontal plane. In the final lying position, the head is about 45° downward (Fig. 5). In this position, it is possible to observe a secondary nystagmus similar, in direction, to that evoked by the Dix-Hallpike positioning (“liberatory” nystagmus). The patient remains in this position for two minutes after the secondary nystagmus disappears or four minutes, if the secondary nystagmus is not detected. Finally, the patient returns to the sitting position.
Fig. 5.
The “quick liberatory rotation” manoeuvre.
If the lateral canalolithiasis persisted, further attempts were made to search for SSL.
The project used herein foresaw a “final step”: if after three therapeutic attempts, the first choice was not successful, the side was changed, based on the other method, namely, SSL if the classic method was used first to define the affected ear, or vice versa, if SSL was used first.
Finally, the results of GM were compared when using either the classic method or SSL in indicating the affected side.
Control group
30 healthy subjects (mean age 46.4 ± 8.67 years, range 18-72 years) with no symptoms or personal history of vestibular diseases and 20 subjects affected by unilateral loss of the vestibular function (compensated vestibular neuritis) (mean age 43.5 ± 9.76 years, range 17-70 years) were observed for horizontal bilateral bidirectional paroxysmal nystagmus evoked by the Pagnini-McClure manoeuvre and for SSL.
Statistical analysis
Statistical analysis was performed using the SPSS© (SPSS Inc., Chicago, IL, USA) statistical package (version 11.5) according to criteria proposed by Jeckel et al. 19. The results are expressed as mean ± standard deviation (SD) for continuous variables and as absolute (percent values) for discrete variables. Data were analysed by sensitivity and specificity derived from the receiver operating characteristic (ROC) curve and the area under the ROC curve. This latter parameter is expressed as an area (lower bound-upper bound) (95% confidence interval).
The efficiency of the Pagnini-McClure manoeuvre and of SSL in correctly detecting the affected side was confirmed by the positive results of the treatment by GM in the management of lateral canalolithiasis.
Results
Control group
The horizontal bilateral bidirectional paroxysmal nystagmus evoked by the Pagnini-McClure manoeuvre was not observed either in healthy subjects or in patients affected by unilateral loss of the vestibular function.
SSL were never observed in healthy subjects, while in the patients affected by unilateral loss of the vestibular function, a paretic HSIN (quick phases toward the healthy side) was observed, as a sign of the vestibular loss of function, in 16/20 cases (80%).
Patients group
The Pagnini-McClure manoeuvre was always positive in evoking a horizontal bipositional paroxysmal apogeotropic nystagmus and the sensitivity and specificity, in detecting lateral canalolithiasis, were 100% when compared to the “control group”.
In 52/64 cases (81.2%), a different intensity of the nystagmus induced by the Pagnini-McClure manoeuvre on the two sides was clearly evident and the side where the less intense nystagmus was induced was considered to be the affected side.
Data referring to SSL in the “patients group” are outlined in Table I.
Table I. The overall incidence of “secondary signs of lateralization”.
| Signs | Present (%) | Absent |
| Pseudo-spontaneous nystagmus | 36 (56.2) | 28 |
| Bending nystagmus | 38 (59.3) | 26 |
| Bowing and leaning nystagmus | 24 (37.5) | 40 |
| HSIN | 40 (62.5) | 24 |
| Nystagmus from sitting to supine position | 48 (75) | 16 |
| Null-point in the yaw plane | 34/36 (94.4) | 2 |
| Conversion to a geotropic form by HR | 8 (12.5) | 56 |
| Conversion to a lateral geotropic form after GM | 28/56 (50) | 28 |
| Conversion to a posterior canalolithiasis after GM | 4 (6.2) | 60 |
HSIN: head shaking-induced nystagmus; HR: head roll in the supine position; GM: Gufoni’s manoeuvre
In 26 cases, the pseudo-spontaneous nystagmus was observed in still patients, while in another 10 cases it was evoked by a mild Head shaking.
It was inhibited at the null-point, in the pitch plane, in 34/36 cases (94.4%).
HSIN always beat towards the healthy side, as indicated by the Pagnini-McClure manoeuvre and/or by other SSL.
Interestingly, when both kinds of nystagmus were present, HSIN was opposed to the pseudo-spontaneous nystagmus induced by a mild head shaking.
BLT was considered positive when it evoked both leaning and bowing nystagmus.
The bowing/bending positioning always reversed the Pseudo-spontaneous nystagmus, when it was present.
The sitting to supine positioning nystagmus was the most frequently observed secondary sign of laterality (48/64 cases: 75%).
During the diagnostic phase, reversal from the apogeotropic to geotropic form was rarely requested since this phase can be considerably unpleasant for the patient. It was nonetheless detected in 8 patients.
When recording the patients’ medical history, a greater uncomfortable sensation, on one side, was reported in 36/64 cases and only two patients gave an incorrect reference, when it was referred to the clinical findings.
Two groups of patients were distinguished.
First group
The Pagnini-McClure manoeuvre evoked asymmetrical nystagmic responses between the two sides (52 cases: 81.8%).
The indications of SSL agreed with the results of the Pagnini-McClure manoeuvre, except in two cases.
In fact, the side indicated by the less intense horizontal paroxysmal nystagmus (affected side) was the same as that indicated by the direction of the pseudo-spontaneous nystagmus, of the leaning nystagmus, of the sitting to supine positioning nystagmus and by the side of the null-point on the yaw plane in 50 cases.
In one case, HSIN, the bowing and leaning nystagmus and the sitting to supine positioning nystagmus were in opposition to the indications of the Pagnini-McClure manoeuvre; in another case, the sitting to supine positioning nystagmus was in opposition both with the indication of the Pagnini-McClure manoeuvre and the indication of the bending nystagmus.
Second group
The Pagnini-McClure manoeuvre did not show a clear difference between the two sides in evoking asymmetrical nystagmic responses (12 cases: 18.2%).
In these patients, considered as affected was the side indicated by the pseudo-spontaneous nystagmus, the leaning nystagmus, the sitting to supine positioning nystagmus and the side where the null point on the yaw plane was observed.
On the contrary, the healthy side was indicated by the bowing/bending nystagmus and by the quick phases of HSIN.
These data agreed with the conversion into a geotropic canalolithiasis during the diagnostic phase (2 cases), the conversion into a geotropic lateral canalolithiasis (4 cases) or into a posterior canalolithiasis (2 cases) after GM.
These cases are reported in Table II.
Table II. “Secondary signs of lateralization” in cases of uncertain diagnosis of affected side.
| PS | HSIN | B&L | Be | SiToSu | NP | Diag Tran | Ther Tran | Diagnosis | |
| 1 | – | R | B R L Le | R | – | Le | – | – | Le Apo |
| 2 | R | Le | – | Le | R | – | – | Post R | R Apo |
| 3 | – | – | – | – | Le | Le | – | – | Le Apo |
| 4 | Le | R | B R L Le | R | – | – | – | Geo Le | Le Apo |
| 5 | Le | – | – | – | Le | – | Geo Le | – | Le Apo |
| 6 | – | Le | B Le L R | Le | R | R | – | – | R Apo |
| 7 | – | – | B Le L R | Le | R | R | – | – | R Apo |
| 8 | R | Le | – | – | R | – | – | Post R | R Apo |
| 9 | – | R | – | – | – | Le | – | – | Le Apo |
| 10 | R | Le | B Le L R | Le | – | – | – | Geo R | R Apo |
| 11 | – | – | – | – | Le | – | Geo Le | – | Le Apo |
| 12 | R | Le | B Le L R | Le | R | R | – | Geo R | R Apo |
PS: pseudo-spontaneous nystagmus; HSIN: head shaking-induced nystagmus; B: bowing nystagmus; L: leaning nystagmus; Be: bending nystagmus; SiToSu: nystagmus from the sitting to the supine position; NP: null point on the yaw plane; Diag Tran: transformation into a geotropic form by repeated head-roll test; Ther Tran: transformation into a lateral geotropic form or a posterior canalolithiasis by the Gufoni’s manoeuvre; Geo: geotropic lateral canalolithiasis; Post: posterior canalolithiasis; Le: left; R: right; Apo: apogeotropic lateral canalolithiasis.
The therapeutic phase
All the patients underwent GM as reported in Patients and methods.
“First group”: 6 cases were transformed into the geotropic form by repeated head roll manoeuvres in the yaw plane and were cured by GM following a one-step treatment.
Persistent apogeotropic canalolithiasis was cured by the first step of GM in 19/46 cases (41.3%).
In 24 cases, apogeotropic lateral canalolithiasis was transformed by the first step of GM into geotropic forms, which were treated by a second step of GM toward the healthy side.
In 2 cases, GM transformed lateral canalolithiasis into posterior canalolithiasis, treated and cured by QLR.
When the indication of the affected side between the Pagnini-McClure manoeuvre and SSL was different, one case was cured by GM, based on the indication of the Pagnini-McClure manoeuvre, while the second case did not respond to the treatment.
In the “First group”, the treatment (GM plus where necessary QLR) was effective in curing lateral canalolithiasis in 51/52 cases (98.1%).
The patient who failed to respond to the treatment was treated changing the choice of the affected side, based now on the indications of the SSL (“final step”): GM performed towards the “new” affected side cured the lateral canalolithiasis, by a two-step treatment.
Finally, all 52 cases in the “First group” were cured.
In the “Second group”, 2 cases were transformed into the geotropic form by the head roll manoeuvre in the yaw plane and they were cured by GM on the healthy side.
GM cured apogeotropic lateral canalolithiasis by a one-step treatment towards the affected ear in 4/10 cases, while in 4 cases a two-step treatment was necessary.
In 2 cases, GM converted lateral into posterior canalolithiasis, cured by QLR.
Finally, the treatment (GM plus eventually QLR) was effective in curing lateral canalolithiasis in all 12 cases.
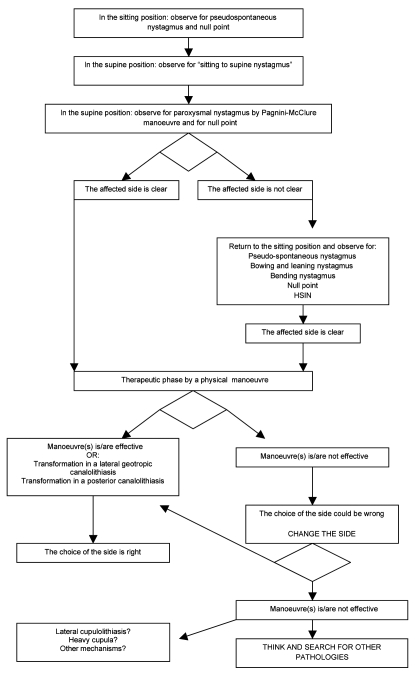
ROC curve (Fig. 6) illustrates the sensitivity and specificity of the Pagnini-McClure manoeuvre and of other signs of lateralization in correctly detecting the side of lateral canalolithiasis.
Fig. 6.
ROC curves for the signs of lateralization.
The area under the ROC curve was 0.958 (0.891-0.999) for Pagnini-McClure manoeuvre; 0.708 (0.512-0.905) for null point; 0.521 (0.318-724) for pseudospontaneuos nystagmus; 0.604 (0.401-0.808) for bending nystagmus; 0.500 (0.297-0.703) for bowing and leaning nystagmus; 0.458 (0.257-0.660) for HSIN; 0.542 (0.337-0.746) for sitting to supine positioning nystagmus; 0.500 (0.297-0.703) for diagnostic transition from apogeotropic to geotropic canalolithiasis and 0.646 (0.449-0.842) for therapeutic transition from an apogeotropic to a geotropic form or from a lateral canalolithiasis to a posterior canalolithiasis. The latter did not differ significantly from the reference line. Only Pagnini-Mc Clure diagnostic manoeuvre (p < 0.001) and null point (p = 0.044) showed an area under the ROC curve significantly different form the reference line.
Discussion
The primary diagnostic criterion of lateral canalolithiasis is the horizontal bipositional bidirectional paroxysmal nystagmus evoked by the Pagnini-McClure manoeuvre.
The nystagmus is stronger on the affected side in geotropic canalolithiasis, stronger on the healthy side in apogeotropic canalolithiasis, according to Ewald’s second law: therefore, the diagnosis of the affected side by the Pagnini-McClure manoeuvre is based upon the different intensity of the nystagmus evoked on the two sides.
The analysis of our data highlights that the Pagnini-Mc Clure manoeuvre is the specific diagnostic technique in diagnosing lateral canalolithiasis.
It also allows a correct diagnosis of the affected side in most cases: it proved to be effective in detecting asymmetrical nystagmic responses between the two sides in 52 out of 64 cases (81.2%) and, in 51/52 cases (98.1%), it correctly identified the affected side, based upon the results of the GM.
In a minority of 13 patients (12 patients in the Second Group and 1 patient in the First Group), SSL was needed to determine the affected side, observing the direction of the nystagmus.
In our opinion, the nystagmus observed in the sitting position (pseudo-spontaneous nystagmus; leaning nystagmus; bowing/bending nystagmus), their inhibition at the null point, the sitting to supine positioning nystagmus, as well as the nystagmus evoked by the Pagnini-McClure manoeuvre, are signs of a single phenomenon: the ampullopetal or ampullofugal movement of otoliths in the LSC, caused by their position either in the anterior or in the posterior arm, and by the position of the head in the pitch or in the yaw plane.
In the different positions of the head in the spatial planes, free-floating otoliths move in the LSC as on an inclined plane and this determines specific endolymphatic flow: the ampullopetal flow provokes excitatory nystagmic responses, the ampullofugal flow inhibitory nystagmic responses.
This agrees perfectly with the theory of canalolithiasis, both in geotropic forms and in apogeotropic forms.
In our opinion, a real “cupulolithiasis” of the lateral canal (otoliths closely adhering to the cupula) is uncommon and its diagnosis requires criteria other than only the paroxysmal horizontal apogeotropic nystagmus: but this feature was not within the aims of this study.
In the apogeotropic form of lateral canalolithiasis, both in the sitting position, when the head is upright or in the leaning position, and in the positioning from the sitting to the supine position, otoliths can move towards the ampulla, causing a nystagmus directed towards the affected side (Figs. 1, 3, 4).
On the contrary, in the bowing/bending position, otoliths can move away from the ampulla, causing a nystagmus directed towards the healthy side (Fig. 2).
When these pathophysiological data are applied to a clinical setting, in apogeotropic lateral canalolithiasis, the pseudo-spontaneous nystagmus, the leaning nystagmus and the sitting to supine positioning nystagmus, beat towards the affected side, while the bowing/bending nystagmus beats towards the healthy side.
Null points on the pitch plane and on the yaw plane are the neutral positions of otoliths in the lateral canal, where they are not affected by gravitational forces and cause no endolymphatic flow.
Instead, HSIN is based upon a relative loss of function of the lithiasic canal.
In fact, HSIN is always a deficitary nystagmus with quick phases directed towards the healthy side, both in apogeotropic and in geotropic lateral canalolithiasis, and it is stable in its direction even after the possible conversion from an apogeotropic to a geotropic form.
SSL were perfectly in agreement with each other and analysis of these usually led to a correct diagnosis of the affected side, both in the group of the patients where the Pagnini-McClure manoeuvre was enough to diagnose the side (First group) and in the group where the Pagnini-McClure manoeuvre was not (Second group).
Only in one patient in the “First group”, was the side indicated by SSL found to be wrong and in contrast with the indication of the Pagnini-McClure manoeuvre, which correctly guided the first step of GM.
The pseudo-spontaneous nystagmus in the sitting position and the sitting to supine positioning nystagmus were revealed to be particularly useful, because of their high frequency and of an extremely easy and tolerable position of observation.
Our results (analysis both of the control group and patients group) showed that the Pagnini-McClure manoeuvre is the specific diagnostic criterion for lateral canalolithiasis and that, in most of cases, it is enough to correctly diagnose also the affected side.
Furthermore, in our opinion, it is not necessary to always search for all the “secondary signs of lateralization”: we can initially observe only the pseudo-spontaneous nystagmus, the Sitting to supine positioning nystagmus and the null points on the pitch and yaw planes, because our aim should be to make a correct diagnosis of the pathological condition and of the affected side, in the easiest way, with least trouble and inconvenience for the patient.
It is necessary to research the other SSL only when the results of the Pagnini-McClure manoeuvre are nor clear or when therapeutic manoeuvres failed to resolve the paroxysmal positional vertigo.
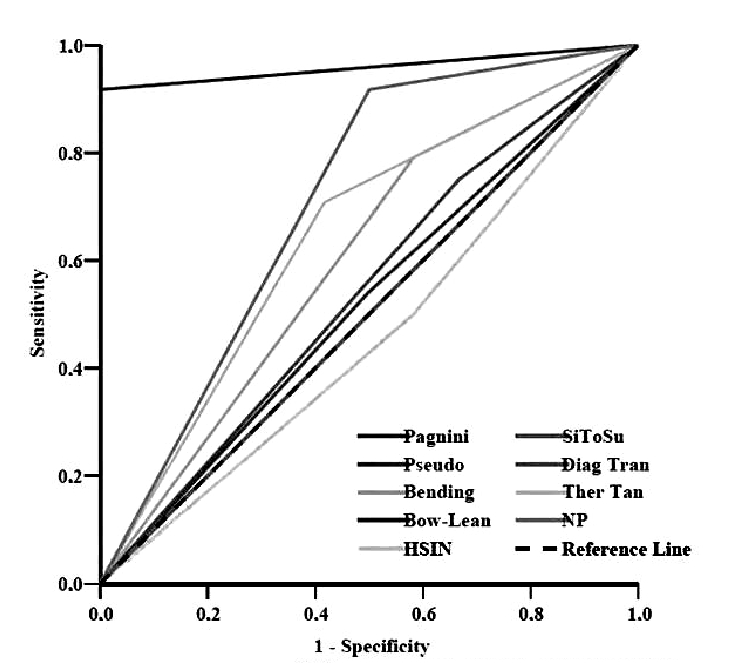
Based on these remarks, we suggest the following diagnostic algorithm (Table III).
Table III. Decision-making algorithm in the diagnosis and treatment of lateral apogeotropic canalolithiasis.
The correct term is “apogeotropic”, not “ageotropic”, as often reported. “A-” is derived from Greek and Latin “Depriving alpha” (without, … less): then “Ageotropic nystagmus” means “Nystagmus without geotropism”. “Apo” is derived from Greek “άπο” (apo) that means: “in opposition to, away from”. Apogeotropic nystagmus means: “Nystagmus whose fast phases “go away from” the gravitational field”: this is the case of the apogeotropic variant of lateral canal BPPV! “Apogeotropic” respects the correct etymology of the term in its proper sense: then, it is the adjective we must use in these cases.
References
- 1.Cipparrone L, Corridi G, Pagnini P. Cupulolitiasi. In: V Giornata Italiana di Nistagmografia Clinica. Nistagmografia e patologia vestibolare periferica. Milano: CSS Boots-Formenti; 1985. p. 36-53. [Google Scholar]
- 2.McClure A. Lateral canal BPV. J Otolaryngol 1985;14:30-5. [PubMed] [Google Scholar]
- 3.Pagnini P, Nuti D, Vannucchi P. Benign paroxysmal vertigo of the horizontal canal. ORL J Otorhinolaryngol Relat Spec 1989; 51:161-70. [DOI] [PubMed] [Google Scholar]
- 4.Lempert T, Tiel-Wilck K. A positional maneuver for treatment of horizontal-canal benign positional vertigo. Laryngoscope 1996;106:476-8. [DOI] [PubMed] [Google Scholar]
- 5.Gufoni M, Mastrosimone L. Trattamento con manovra di riposizionamento per la canalolitiasi orizzontale. Acta Otorhinolaryngol Ital 1998;18:363-7. [PubMed] [Google Scholar]
- 6.Gufoni M. Treatment of lithiasis of the lateral semicircular canal. In: Guidetti G, Pagnini P. editors. Labyrintholithiasis-related paroxysmal positional vertigo. S. Donato Milanese: Excerpta Medica 2002; p. 103-12. [Google Scholar]
- 7.Vannucchi P, Giannoni B, Giuffreda P, et al. The therapy of benign paroxysmal positional vertigo of the lateral semicircular canal. In: Versino M, Zambardieri D. Editors. International workshop on eye movements. Pavia: 1994; p. 321-4. [Google Scholar]
- 8.Asprella-Libonati G. Diagnostic and treatment strategy of lateral semicircular canal canalolithiasis. Acta Otorhinolaryngol Ital 2005;25:277-83. [PMC free article] [PubMed] [Google Scholar]
- 9.Asprella-Libonati G. Pseudo-Spontaneous Nystagmus: a new sign to diagnose the affected side in Lateral Semicircular Canal Benign Paroxysmal Positional Vertigo. Acta Otorhinolaryngol Ital 2008;28:73-8. [PMC free article] [PubMed] [Google Scholar]
- 10.Bissdorff AR, Debatisse D. Localizing signs in positional vertigo due to lateral cupulolithiasis. Neurology 2001;57:1085-8. [DOI] [PubMed] [Google Scholar]
- 11.Choung Y-H, Shin YR, Kahng H, et al. “Bow and Lean test” to determine the affected ear of horizontal canal benign paroxysmal positional vertigo. Laryngoscope 2006;116:1776-81. [DOI] [PubMed] [Google Scholar]
- 12.Lee S-H, Choi K-D, Jeong S-H, et al. Nystagmus during neck flexion in the pitch plane in benign paroxysmal positional vertigo involving the horizontal canal. J Neurol Sci 2007;256:75-80. [DOI] [PubMed] [Google Scholar]
- 13.Nuti D, Vannucchi P, Pagnini P. Benign paroxysmal positional vertigo of the horizontal canal: a form of canalolithiasis with variable clinical features. J Vest Res 1996;6:173-84. [PubMed] [Google Scholar]
- 14.Nuti D,Vannucchi P, Pagnini P. Lateral canal BPPV: which is the affected side? Audiol Med 2005;3:16-20. [Google Scholar]
- 15.Han BI, Oh HJ, Kim JS. Nystagmus while recumbent in horizontal canal benign paroxysmal positional vertigo. Neurology 2006;66:706-10. [DOI] [PubMed] [Google Scholar]
- 16.Koo JW, Moon IJ, Shim WS, et al. Value of lying-down nystagmus in the lateralization of horizontal semicircular canal benign paroxysmal positional vertigo. Otol Neurotol 2006;27:367-71. [DOI] [PubMed] [Google Scholar]
- 17.Hiroaki I. Light cupula theory in persistent type of geotropic direction-changing positional nystagmus. http://homepage1.nifty.com/ichijoent/sakusaku/6_1.htm
- 18.Califano L, Capparuccia PG, Di Maria D, et al. Treatment of benign paroxysmal positional vertigo of posterior semicircular canal by “Quick Liberatory Rotation Manoeuvre”. Acta Otorhinolaryngol Ital 2003;23:161-7. [PubMed] [Google Scholar]
- 19.Jekel JF, Elmore JG, Katz DL. Epidemiologia, biostatistica e medicina preventiva. Napoli: EdiSES 2005. [Google Scholar]