Summary
Identifying the site of obstruction and the pattern of airway change during sleep are the key points essential to guide surgical treatment decision making for Obstructive Sleep Apnoea-Hypopnoea Syndrome in adults. In this investigation, 250 cases were retrospectively analyzed in order to compare the pharyngolaryngeal endoscopic findings detected in the awake state, with those obtained in drug-induced sedation, by means of the Sleep Endoscopy technique. All endoscopic findings have been classified according to the semi-quantitative NOH staging. The awake and sedation NOH resulted identical in 25% of the cases only, while the discrepancies involved the oropharyngeal and hypopharyngeal sites, respectively in about 33% and 50% of the patients. The laryngeal obstructive role detected during sedation in almost 33% of the cases was both unforeseen and relevant, with all the consequent implications in the treatment choices particularly for the surgical cases.
Keywords: Snoring, OSAHS, Sleep endoscopy
Riassunto
Punti chiave essenziali per definire la programmazione chirurgica nell’adulto affetto da Sindrome delle Apnee-Ipopnee Ostruttive del Sonno sono l’identificazione del sito e del pattern di ostruzione che avvengono durante il sonno. Abbiamo analizzato retrospettivamente 250 casi allo scopo di confrontare i rilievi endoscopici faringolaringei ottenuti in veglia con quelli osservati in sedazione farmaco-indotta (Sleep Endoscopy). Ciascun riscontro endoscopico è stato classificato secondo il sistema semi-quantitativo NOH. Solamente nel 25% dei casi l’NOH in veglia ed in sedazione sono risultati identici, mentre le divergenze hanno riguardato i siti orofaringeo ed ipofaringeo rispettivamente nel 33% ed in circa il 50% dei pazienti. Imprevisto e rilevante il ruolo ostruttivo laringeo emerso durante la sedazione in quasi un terzo dei casi, con tutte le conseguenti implicazioni nelle scelte terapeutiche soprattutto se chirurgiche.
Introduction
Obstructive Sleep Apnoea Hypopnoea Syndrome (OSAHS) is an underestimated but impeding social and health problem 1 2. From the therapeutical point of view, Continuous Positive Airways Pressure (CPAP) ventilation is accepted worldwide as the gold standard approach 3. Alternative and well studied options are surgery, oral appliances and weight loss 4–6. In the management of severe cases, ventilation is universally regarded as the preferred option, but very recent surgery has proved to be a valuable alternative also in randomised prospective studies vs CPAP 7. On the other hand, effective surgical procedures need to be correctly selected and performed. Identifying the site of obstruction and the pattern of airway change during sleep are the key points essential to guide surgical treatment decision making 8. The traditional routine practice (ENT examination, Müller manoeuvre and X-ray cephalometry) has been found to be incomplete and thus unable to detect the hallmark of Sleep-Disordered Breathing (SDB): the increased muscle tone during the awake state may offer an erroneous set of information regarding airway obstruction 9–12. Indeed, the awake state findings may differ quite dramatically from the sleep-breathing situation 13, and inaccurate information may lead to inappropriate surgery 14 15. Several Authors have shown how incorrect selection criteria can, at least in part, explain the failure rate concerning OSAHS surgery 9 12 16. This methodological “bias” could be overcome by introducing nasendoscopy, carried out during sleep, indeed, called “Sleep-Endoscopy” (SE). Borowiecki et al., in 1978, and Rojewski et al., in 1982, were the first to perform endoscopy in patients under conditions of spontaneous sleep 17 18. In 1991, Croft and Pringle described, for the first time, endoscopic evaluation of the upper airway during pharmacologically induced sleep 13. We have retrospectively analyzed 250 cases in order to compare the pharyngolaryngeal endoscopic findings detected in the awake state while in a supine position, with those obtained under drug-induced sedation.
Patients and methods
The data reported refer to 250 SDB patients submitted to SE during the period November 2005 – July 2008. Features regarding the study population can be summarized as follows:
Male:Female = 9:1 (225 M, 25 F);
Mean age: 50 yrs (min: 10, max: 77; 55% from 40 to 60 yrs);
-
Mean Body Mass Index (BMI): 29 kg/m2 (min: 20.4, max: 49.1);
BMI < 25.1 kg/m2 = 13%;
BMI 25.1 ÷ 30.0 kg/m2 = 54%;
BMI > 30.0 kg/m2 = 33%;
-
Mean Epworth Sleepiness Scale (ESS): 11 (min: 1, max: 24);
ESS < 11 = 54% ;
ESS 11 ÷ 15 = 30%;
ESS > 15 = 16%.
Before fibre-optic evaluation (under sedation), all patients enrolled in the study underwent the following basic diagnostic work-up:
ENT examination;
Daytime sleepiness evaluation by means of the ESS 19;
X-ray cephalometry;
Polysomnographic study (PSG) according to the Associazione Italiana Medicina del Sonno-Associazione Italiana Pneumologi Ospedalieri (AIMS-AIPO) guidelines 20.
All endoscopic findings have been classified according to the Nose Oropharynx Hypopharynx (NOH) staging, that was first introduced, in clinical practice, by the Authors in 1999 21. Endoscopic observations have been classified according to the sites of collapse (nasopharyngeal; oropharyngeal; hypopharyngeal or laryngeal). The minimal sectional area (Müller manoeuvre) has been classified in 4 obstructing grades:
Grade I: < 25% collapse;
Grade II: between 25% and 50% collapse;
Grade III: between 51% and 75% collapse;
Grade IV: > 75% collapse.
Identification of the obstructing pattern was evaluated according to the shape of the dynamic collapse (antero-posterior, transversal or circular). The setting of all drug-induced Sleep-Endoscopies has been characterised by: operating room, supine position, oxygen saturation and cardiac rhythm monitoring, propofol infusion by means of the bolus technique, fiber-optic evaluation.
Results
The predictive value of the obstructive frameworks as detected in the awake vs sedation state has been shown to be extremely different: 76% (190/250) of overall dissonances (oropharyngeal and/or hypopharyngeal sites) (Fig. 1). On the other hand, endoscopic findings, in comparison with the two states of observation described, have been quite similar only in 24% (60/250) of cases.
Fig. 1.
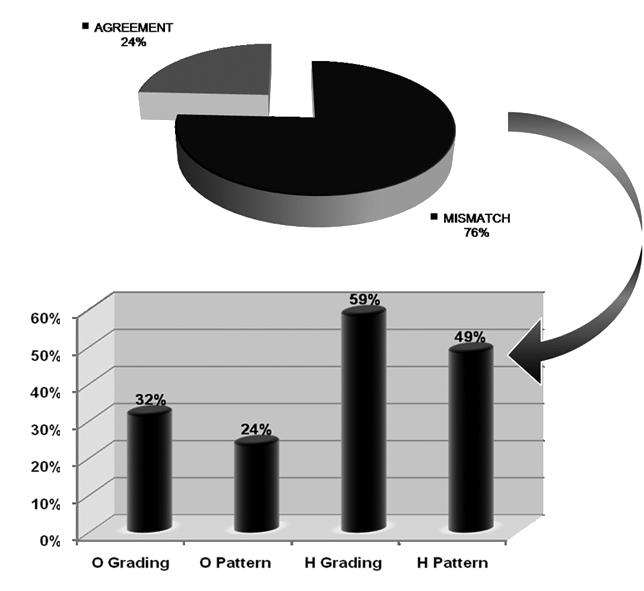
NOH Mismatch – discrepancy rates on Oropharyngeal (O) and Hypopharyngeal (H) findings.
Oropharyngeal site
Overall, 32% (80/250) disagreement, regarding obstructing grade has been identified, in particular:
27% (67/250) of increased collapsing grade during SE (> 25% and 50%, respectively, in 15% and 12% of cases);
3% (8/250) of lower collapsing grade during SE;
2% (5/250) in which SE was crucial to identify the grade of obstruction (patients unable to carry out Müller manoeuvre during awake endoscopy).
The analysis of the obstructing pattern has shown a 24% (60/250) dissonance frequently from a transversal (awake) to a circular (sedation) collapsing shape.
Hypopharyngeal site
Overall, 59% (148/250) disagreement, on obstructing grade, has been recorded, in particular:
51% (127/250) increased collapsing grade during SE (> 25% and 50%, respectively, in 43% and 8% of cases);
5% (13/250) of lower collapsing grade during SE;
3% (8/250) in which SE has been crucial in the identification of grade of obstruction (patients unable to carry out Müller manoeuvre during awake endoscopy).
The analysis of the obstructing pattern has shown 49% (123/250) discrepancy: during sedation, the most remarkable events concerned a change from a transversal to a circular (48/250 = 19%) or to an anteroposterior (33/250 = 13%) collapsing shape.
Laryngeal site
A total of 74 patients (30%) showed a laryngeal involvement during sedation, as representative of a significant change during sleep (Fig. 2):
Fig. 2.
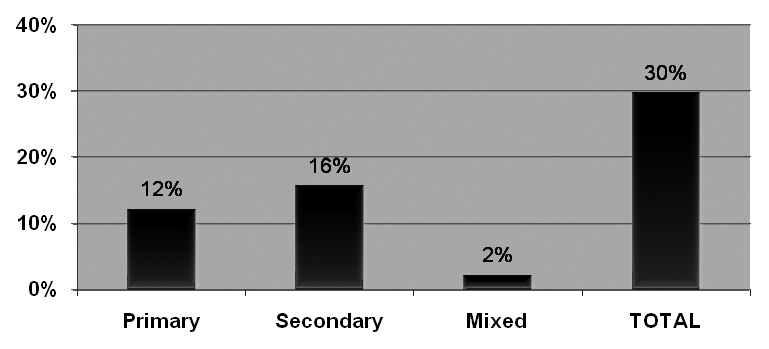
Laryngeal involvement during sedation – obstruction frameworks.
12% primary role (30 out of 250), when the laryngeal obstruction is not due to external causes. A glottic occlusion has rarely been observed (1/30), more likely (29/30) a sovraglottic obstruction (epiglottic in 16/29; arytenoid in 6/29 or both in 7/29);
-
16% secondary role (39/250), when the laryngeal obstruction is due to compression or displacement of nearby areas, in particular:
epiglottic back position secondary to tongue base hypertrophy or verticalization of the hyoid-tongue complex;
“transversal epiglottic closure” (V-shaped), more frequently due to giant tonsil hypertrophy;
2% mixed role (both primary and secondary obstructing mechanisms): 5/250.
Discussion
Upper airways are collapsible in order to accommodate three essential physiologic functions: breathing, swallowing and speech 22.
During wakefulness, collapse of the upper airways can be prevented by a high pharyngeal neuromuscular tone. Due to a reduction of this neurophysiologic phenomenon, sleep onset results in a progressive upper airways muscular hypotonia, that is greater in OSAHS patients than in normal subjects. The described process contributes to a partial or complete airways obstruction in SDB patients 23. An anatomic-based methodological approach during sleep may be crucial to guide surgical treatment decision making 8. In 1977 and 1978, respectively, Weitzman et al. 24, and Hill et al. 25 were the first to report the use of fiber-optic endoscopy in awake state in order to investigate pharyngeal collapse in patients with sleep apnoea. While not underestimating the relevance of Müller manoeuvre (the importance of which is still worthwhile), we would suggest sleep endoscopy as a useful additional method to reveal site/s of obstruction not likely detectable otherwise. Endoscopy combined with Müller manoeuvre which is simple to carry out, is a functional examination that leads to complete visualisation of the upper airway, also allowing the possibility to exclude any other lesion. Albeit, results depend not only on a subjective visual estimation of the airway collapse, but are related – and, indeed, limited – to a variable cooperation, coordination and effort on the part of the patient 26–29. Several Authors have shown that erroneous selection criteria can account for at least part of the failure rate related to OSAHS surgery 9 12 16. Sher et al. 30 used the Müller manoeuvre to select OSAHS patients and submit them to uvulopalatopharyngoplasty (UPPP). Results of the study revealed that not in all patients presenting ideal responses to the Müller manoeuvre was surgery successful 30. Later, Pringle and Croft showed that results of the Müller manoeuvre alone should not be considered reliable due to the fact that the findings are not always representative of what really occurs during sleep: misleading positive results may occur 31. Camilleri et al. have demonstrated the reliable predictive value of pre-operative sleep endoscopy for the successful outcome of UPPP 32 and Lin et al. reported that endoscopic pharyngeal sedated evaluation, in patients with OSAHS, had clinical power to improve the UPPP results 33. Likewise, Hessel and de Vries concluded that, after diagnostic work-up by sleep registration and SE, the success rate of UPPP increases compared to historical controls 34. Unfortunately, no standard references exist to determine the real site and pattern of obstruction during sleep. In our experience, on 250 cases retrospectively analysed between November 2005 and July 2008, the predictive value of the obstructive frameworks, as detected in the awake state or in sedation, was shown to be extremely misleading: 76% of the dissonance rate on the oropharyngeal and/or hypopharyngeal site (Fig. 1). In particular, SE versus awake endoscopy supplied remarkably dissonance rates on hypopharyngeal grading and pattern of obstruction (59% and 49%, respectively). The most relevant differences have emerged from a sub-evaluation of the collapsing grade during wakefulness. Laryngeal involvement, during sedation, has been representative of a crucial notable changing throughout sleep (Fig. 2). In the awake findings, the laryngeal obstruction may be just hypothesized as due to the deformed epiglottic shape 35, while direct visualization of laryngeal collapse has been possible only during the sedated state 36. In our experience, according to and in agreement with the literature 9 11 12 31 37, tongue base hypertrophy, as well as commonly associated sovraglottic tissue collapse, proved to be considered a non-exceptional sleep-related obstructive condition.
Conclusion
In our experience, SE is a useful additional method to reveal site/s of collapse unlikely to be detectable otherwise (in particular, hypopharyngeal and laryngeal involvement). Indeed, SE is not the only instrument available for investigation, but should be regarded as an additional specific tool in the hands of SDB medicine.
Acknowledgments
Authors express their gratitude to all medical members of ENT Staff, and Anaesthesiological Staff for valuable assistance.
References
- 1.Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med 2002;165:1217-39. [DOI] [PubMed] [Google Scholar]
- 2.De Benedetto M, Cuda D, Leante M. Diurnal hypersomnolence and chronic snoring: an epidemiological study. Acta Otorhinolaryngol Ital 1991;11:579-86. [PubMed] [Google Scholar]
- 3.Giles TL, Lasserson TJ, Smith BH, et al. Continuous positive airways pressure for obstructive sleep apnoea in adults. Cochrane Database Syst Rev 2006;19:CD001106. [DOI] [PubMed] [Google Scholar]
- 4.Lim J, Lasserson TJ, Fleetham J, et al. Oral appliances for obstructive sleep apnoea. Cochrane Database Syst Rev 2006;25:CD004435. [DOI] [PubMed] [Google Scholar]
- 5.Sundaram S, Bridgman SA, Lim J, et al. Surgery for obstructive sleep apnoea. Cochrane Database Syst Rev 2005;19:CD001004. [DOI] [PubMed] [Google Scholar]
- 6.Shneerson J, Wright J. Lifestyle modification for obstructive sleep apnoea. Cochrane Database Syst Rev 2001;1:CD002875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vicini C, Dallan I, Campanini A, et al. Surgery vs ventilation in adult severe obstructive sleep apnea syndrome. Am J Otolaryngol 2010;31:14-20. [DOI] [PubMed] [Google Scholar]
- 8.Abdullah VJ, Wing YK, van Hasselt CA. Video sleep nasendoscopy: the Hong Kong experience. Otolaryngol Clin North Am 2003;36:461-71. [DOI] [PubMed] [Google Scholar]
- 9.Den Herder C, Van Tinteren H, de Vries N. Sleep endoscopy versus modified Mallampati score in sleep apnea and snoring. Laryngoscope 2005;115:735-9. [DOI] [PubMed] [Google Scholar]
- 10.Kezirian EJ. Drug-induced sleep endoscopy. Oper Tech Otolaryngol 2006;17:230-2. [Google Scholar]
- 11.Kotecha BT, Hannan SA, Khalil HMB, et al. Sleep nasendoscopy: a 10-year retrospective audit study. Eur Arch Otorhinolaryngol 2007;264:1361-7. [DOI] [PubMed] [Google Scholar]
- 12.Bachar G, Feinmesser R, Shpitzer T, et al. Laryngeal and hypopharyngeal obstruction in sleep disordered breathing patients, evaluated by sleep endoscopy. Eur Arch Otorhinolaryngol 2008;265:1397-402. [DOI] [PubMed] [Google Scholar]
- 13.Croft CB, Pringle M. Sleep nasendoscopy: a technique of assessment in snoring and obstructive sleep apnoea. Clin Otolaryngol 1991;16:504-9. [DOI] [PubMed] [Google Scholar]
- 14.Skatvedt O. Localization of site of obstruction in snorers and patients with obstructive sleep apnea syndrome: a comparison of fiberoptic nasopharyngoscopy and pressure measurements. Acta Otolaryngol 1993;113:206-9. [DOI] [PubMed] [Google Scholar]
- 15.De Benedetto M, Leante M, Graziuso M. La chirurgia nella roncopatia cronica. In: De Benedetto M, editor. La roncopatia cronica. Official Report of XVI A.O.O.I. Convention. Pisa: Pacini 1992. p. 129-49. [Google Scholar]
- 16.Rodriguez-Bruno K, Goldberg AN, Mc Culloch CE, et al. Test-retest reliability of drug-induced sleep endoscopy. Otolaryngol Head Neck Surg 2009;140:646-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Borowiecki B, Pollak CP, Weitzman ED, et al. Fibro-optic study of pharyngeal airway during sleep in patients with hypersomnia obstructive sleep-apnea syndrome. Laryngoscope 1978;88:1310-3. [DOI] [PubMed] [Google Scholar]
- 18.Rojewski TE, Schuller DE, Clark RW, et al. Synchronous video recording of the pharyngeal airway and polysomno-graphy in patients with obstructive sleep apnea. Laryngoscope 1982;92:246-50. [DOI] [PubMed] [Google Scholar]
- 19.Oksenberg A, Arons E, Nasser K, et al. Severe obstructive sleep apnea: Sleepy versus non-sleepy patients. Laryngoscope 2009;25:643-8. [DOI] [PubMed] [Google Scholar]
- 20.Commissione paritetica AIPO-AIMS. Linee guida di procedura diagnostica nella sindrome delle apnee ostruttive dell’adulto. Rassegna di Patologia dell’Apparato Respiratorio 2001;16:278-80. [Google Scholar]
- 21.Frassineti S, Vicini C, Dallan I. Fibroscopia e sistema NOH. In: Vicini C, editor. Chirurgia della roncopatia. Lucca: Eureka S.r.l. 2007. p. 253-9. [Google Scholar]
- 22.Arens R, Marcus CL. Pathophysiology of upper airway obstruction: a developmental perspective. Sleep 2004;27:997-1019. [DOI] [PubMed] [Google Scholar]
- 23.Schwartz AR, Patil SP, Squier S, et al. Obesity and upper airway control during sleep. J Appl Physiol 2010;108:430-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weitzman ED, Pollak C, Borowiecki B, et al. The Hypersomnia Sleep-Apnea Syndrome: site and mechanism of upper airway obstruction. Trans Am Neurol Assoc 1977;102:150-3. [PubMed] [Google Scholar]
- 25.Hill MW, Guilleminault C, Simmons FB. Fiber-optic and EMG studies in hypersomnia-sleep apnea syndrome. In: Guilleminault C, Dement WC, editors. Sleep apnea syndromes. New York: Alan R. Liss Inc.; 1978. p. 249-58. [Google Scholar]
- 26.Woodson BT, Naganuma H. Comparison of methods of airway evaluation in obstructive sleep apnea syndrome. Otolaryngol Head Neck Surg 1999;120:460-3. [PubMed] [Google Scholar]
- 27.Terris DJ, Hanasono MM, Liu YC. Reliability of the Müller maneuver and its association with sleep-disordered breathing. Laryngoscope 2000;110:1819-23. [DOI] [PubMed] [Google Scholar]
- 28.Dreher A, de la Chaux R, Klemens C, et al. Correlation between otorhinolaryngologic evaluation and severity of obstructive sleep apnea syndrome in snorers. Arch Otolaryngol Head Neck Surg 2005;131:95-8. [DOI] [PubMed] [Google Scholar]
- 29.Herzog M, Metz T, Schmidt A, et al. The prognostic value of simulated snoring in awake patients with sleep-disordered breathing: introduction of a new technique examination. Sleep 2006;29:1456-62. [DOI] [PubMed] [Google Scholar]
- 30.Sher AE, Thorpy MJ, Shprintzen RJ, et al. Predictive value of Muller maneuver in selection of patients for uvulopalato-pharyngoplasty. Laryngoscope 1985;95:1483-7. [DOI] [PubMed] [Google Scholar]
- 31.Pringle MB, Croft CB. A comparison of sleep nasendoscopy and the Muller manoeuvre. Clin Otolaryngol 1991;16:559-62. [DOI] [PubMed] [Google Scholar]
- 32.Camilleri AE, Ramamurthy L, Jones P. Sleep nasendoscopy: what benefit to the management of snorers? J Laryngol Otol 1995;109:1163-5. [DOI] [PubMed] [Google Scholar]
- 33.Li W, Ni D, Jiang H, et al. Predictive value of sleep nasendoscopy and the Muller maneuver in uvulopalatopharyngoplasty for the obstructive sleep apnea syndrome. Lin Chuang Er Bi Yan Hou Ke Za Zhi 2003;17:145-6. [PubMed] [Google Scholar]
- 34.Hessel NS, de Vries N. Results of uvulopalatopharyngoplasty after diagnostic workup with polysomnography and sleep endoscopy: a report of 136 snoring patients. Eur Arch Otorhinolaryngol 2003;260:91-5. [DOI] [PubMed] [Google Scholar]
- 35.Gazayerli M, Bleibel W, Elhorr A, et al. A correlation between the shape of the epiglottis and obstructive sleep apnea. Surg Endosc 2006;20:836-7. [DOI] [PubMed] [Google Scholar]
- 36.Stuck BA, Maurer JT. Airway evaluation in obstructive sleep apnea. Sleep Med Rev 2008;12:411-36. [DOI] [PubMed] [Google Scholar]
- 37.Barkdull GC, Kohl CA, Patel M, et al. Computed tomography imaging of patients with obstructive sleep apnea. Laryngoscope 2008;118:1486-92. [DOI] [PubMed] [Google Scholar]


