Abstract
Background
One strategy that has had the greatest effect on improving blood pressure (BP) includes team-based care. The purpose of this systematic review was to determine the potency of interventions for BP involving nurses or pharmacists.
Methods
A Medline search for controlled clinical trials that involved a nurse or pharmacist intervention was conducted. Mean reductions in systolic (S) and diastolic (D) BP were determined by two reviewers who independently abstracted data and classified the different intervention components.
Results
Thirty-seven papers met the inclusion criteria. Education on BP medications was significantly associated with improved BP (−8.75/−3.60 mm Hg). Other strategies that had large effect sizes on SBP included: pharmacist made treatment recommendation (−9.30 mm Hg), nurse did the intervention (−4.80 mm Hg), and a treatment algorithm was used (−4.00 mm Hg). The odds ratio (OR) and 95% confidence interval (CI) for controlled BP were: nurses OR=1.69 (CI = 1.48, 1.93), pharmacists within primary care clinics OR=2.17 (CI = 1.75, 2.68) and community pharmacists OR=2.89 (CI = 1.83, 4.55), Mean reductions in SBP were: nursing studies = 5.84 ± 8.05 mm Hg, pharmacists in clinics = 7.76 ± 7.81 mm Hg and community pharmacists = 9.31 ± 5.00 mm Hg but there was no significant differences between the nursing and pharmacy studies (p≥0.19).
Conclusion
Team-based care was associated with improved BP control and individual components of the intervention appeared to predict potency. Implementation of new hypertension guidelines should consider changes in the health-care organizational structure to include important components of team-based care.
Keywords: hypertension management, quality improvement, team care, blood pressure, hypertension guidelines, pharmacist, nurse
Introduction
Blood pressure (BP) is poorly controlled in the US.1-5 The 8th Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC-8) is currently considering strategies to improve the implementation of the guidelines and achieve higher BP control rates. Investigators from the Stanford-UCSF Evidence-based Practice Center conducted an analysis of controlled clinical trials of quality improvement strategies and found that the only strategy that significantly improved BP involved interdisciplinary team-based care.6 Most of the quality improvement interventions utilized multiple components. These different strategies or the potency of the intervention may explain why there appears to be differences in effect sizes.7
One strategy to improve guideline adherence is to use team-based care involving pharmacists or nurses.8-13 The purpose of the present study was to conduct a systematic review of the research literature and to evaluate the potency of team-based care involving pharmacists or nurses. We theorized that the effect size would be greater for nurses or pharmacists working in the physician’s office or more independently by protocol than with more distant interventions such as recommendations from a community pharmacist.
Methods
We followed the same process as Walsh et al6 by including quasi-randomized trials, controlled before-after studies, interrupted time-series studies, patient-randomized trials and cluster-randomized trials. Quasi-randomized trials were defined as those that included at least two cohorts of patients identified prospectively using an arbitrary, but nonrandom allocation procedure.6 Controlled, before-after studies were defined as those with a contemporaneous observation for cohorts that differed primarily with respect to the exposure of the intervention.6 Interrupted time series required that the study report outcomes from at least three time points in the pre- and post-intervention periods.6
Search Strategy
Walsh et al. performed their search of the MEDLINE database from January 1980 through July 2003 and we extended the search to include papers published from January 1970 through February 2009. The search was conducted by a research librarian. Titles and abstracts were then screened to determine if the article included team-based care of hypertension involving pharmacists or nurses. Next, we searched the reference list of included papers and the reviews by Walsh6 to identify additional citations. Once the full text articles were selected, two reviewers (one Pharm.D. clinical pharmacist and one Ph.D. nurse) independently determined if each paper met the study criteria and, if so, the reviewers independently abstracted critical information including study design, setting, type of intervention, components of the intervention and degree of SBP and DBP change. The intervention components included: supplying free medications, education concerning BP medications, counseling on lifestyle modifications, assessing medication compliance, algorithm for treatment, home visits, intervention provider (nurse or pharmacist) could prescribe medications, intervention provider could order laboratory, length of the study, completion of a drug profile/medication history, physical examination was conducted, nurse provided intervention, pharmacist provided intervention and/or whether medication recommendations were made to a physician (as opposed to independent changes). Because every study used different combinations of these components, the two reviewers independently assigned a “potency score” for their predicted potency that the combination of interventions in a study would have on outcomes ranging from 0 (brings about no result) to 10 (brings about best result). Disagreements between the reviewers were resolved by an open dialog to develop consensus. Confirmation of the two reviewers’ findings was adjudicated by a biostatistician.
Evaluation of the Intervention Effect Size
We calculated effect size by determining the change in SBP (or DBP) attributable to the intervention (int) for each study defined as:6
and
BP control was defined as a BP < 140/90 for patients with uncomplicated BP and <130/80 mm Hg for those with diabetes or chronic kidney disease.14 The net change in BP control rates attributable to the intervention for each study was defined as:
The odds ratio and 95% confidence interval for controlled BP was calculated (22 studies) and weighted by the sample size of the study.8, 15-35 Odds ratios could not be calculated for 15 studies.36-50 We divided the studies into three groups to evaluate potency: 1) nursing interventions, 2) pharmacist interventions delivered in community pharmacies, and 3) interventions by clinical pharmacists working within a primary care office. We performed a sensitivity analyses to determine the effect of assigning studies to different categories when they had multiple strategies (e.g. involved both community pharmacists and nurses).
Analysis
Stepwise regression analyses and non-parametric analyses were performed using the Mann-Whitney test to evaluate the post-intervention difference between the intervention and control groups for mean SBP and DBP while controlling for study sample size using SPSS 17.0.0 statistical software (SPSS, Inc., Chicago, IL, Aug 23, 2008).
One study had a large number of informed dropouts and found no significant difference between nurse management versus the physician.15 A stepwise regression analysis was conducted without this study (n=36) to predict the effect of individual intervention components on BP.
Unadjusted odds ratio for controlled BP were calculated so studies could be compared. Odds ratios were compared using a simple logistics regression model using one variable, unadjusted for any other item. We created a funnel plot of the log of the odds ratio plotted against the standard error for each study to assess the possibility that publication bias might exist.
Results
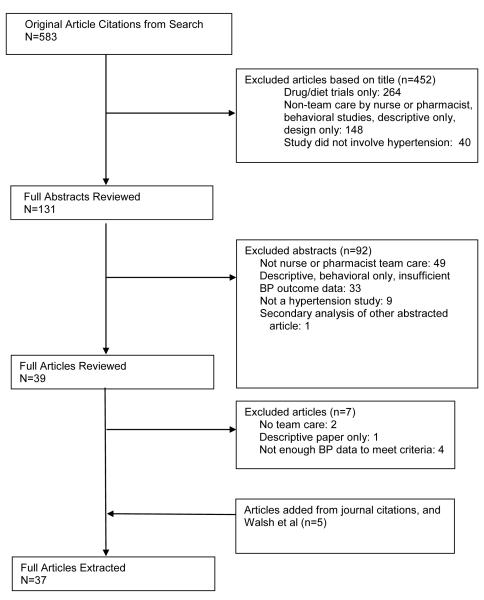
The literature review identified 583 citations and 37 articles that met the inclusion criteria (Figure 1). There was good reliability between the two abstractors for their evaluations of these studies (Pearson correlation coefficient = 0.74, p<0.001).
Figure 1.
Flow diagram for reasons trials were excluded.
Each study involved unique provider qualifications and training. For instance, studies involving community pharmacists may have included bachelor of science (B.S.) trained pharmacists8, 22, 51 or those with Doctor of Pharmacy (PharmD) degrees.20, 21 Studies that involved “pharmacists in clinics” nearly all involved clinical pharmacists (with Pharm.D. or MS degrees) who had completed postdoctoral residency training in primary care whose duties involved direct patient management,24, 26, 28, 30, 34, 36, 48 though several studies did not provide these details.25, 27, 35, 46 Most of the studies involving nurses did not specify their qualifications,17, 19, 33, 38-41, 44, 45, 47 but some noted that they were registered nurses (RN)42, 49 or nurse practitioners.16, 18 Training of the intervention nurses or pharmacists typically involved educational training sessions on hypertension guidelines given by an expert,8, 17, 19-25, 30, 32, 33, 35, 41, 42, 47, 49 but again, many did not specify the training program.16, 18, 26-29, 34, 36-40, 44-46, 48, 50 Only a few studies described patient empowerment or strategies such as home BP monitoring to assist with the intervention.23, 34, 35, 40 One finding is that nearly all studies involving nurses or pharmacists in clinics provided for consistent and dedicated case management activities distinct from traditional nursing or pharmacist duties. Pharmacists in community pharmacies, however, usually had to incorporate the intervention around traditional medication dispensing functions.
The stepwise regression compared the studies that included a given intervention strategy, with those studies that did not. Several individual components of the interventions were associated with significant reductions in SBP including “pharmacist recommended medication to physician” (−27.2 mm Hg, p=0.002), “counseling on lifestyle modification (−12.6 mm Hg, p=0.033), “pharmacist performed the intervention” (−11.7 mm Hg, p=0.028), “an algorithm was used” (−8.46 mm Hg, p<0.001), “a drug profile was completed” (−8.28 mm Hg, p=0.001) and the overall intervention potency score assigned by the study reviewers (p<0.001) (Table 1). For example, the regression coefficient for “used algorithm” was significant (9.37, p<0.001) which indicated that given all other factors in the model, the average reduction in SBP of the nine studies using an algorithm was 9.37 less than the change in SBP in the 27 studies not using an algorithm. Assuming that a study used an algorithm and no other intervention, the predicted reduction in SBP was 8.46 mm Hg (Table 1).
Table 1.
Stepwise meta-regression analysis of the effect on blood pressure (n=36 studies)*
| Outcome variable: Change of systolic blood pressure |
Regression Coefficient |
Predicted Change in SBP (mm Hg) |
p |
| Constant | −1.31 | NA | 0.664 |
| Pharmacist recommended medication to physician |
−9.68 | −27.21 | 0.002 |
| Counseling on lifestyle modification | 5.20 | −12.63 | 0.033 |
| Pharmacist performed the intervention | 6.13 | −11.70 | 0.028 |
| Algorithm used | 9.37 | −8.46 | 0.000 |
| Drug profile was completed | 9.55 | −8.28 | 0.001 |
| Overall intervention potency score** | −2.76 | NA | <0.001 |
| Outcome variable: Change of diastolic blood pressure |
Regression Coefficient |
Predicted Change DBP (mm Hg) |
P |
| Constant | −11.90 | NA | 0.010 |
| Referral was made to specialist | −7.71 | −19.61 | 0.039 |
| Physical Exam was conducted | −6.65 | −18.55 | 0.080 |
| Education on medications | −5.70 | −17.60 | 0.003 |
| Length of intervention | 0.04 | −10.13 | 0.060 |
| Algorithm was used | 3.12 | −8.78 | 0.051 |
| Drug profile was completed | 4.63 | −7.27 | 0.006 |
| Pharmacist performed the intervention | 7.87 | −4.03 | 0.044 |
| Nurse performed the intervention | 7.96 | −3.94 | 0.041 |
analysis when McClellan et al is excluded.15
controlled in the analyses and only significant for SBP.
The factors associated with a reduction in DBP were: “referral was made to a specialist” (−19.6 mm Hg, p=0.039), “providing patient education about BP medications” (−17.6 mm Hg, p=0.003), “a drug profile was completed” (−7.3 mm Hg, p=0.006), “a pharmacist did the intervention” (−4.0 mm Hg, p=0.044) or “a nurse did the intervention” (−3.9 mm Hg, p=0.041). Next, a nonparametric analysis was performed because the data were not normally distributed. The only individual component that had a significant reduction in BP was education on BP medications (−8.75/−3.60 mm Hg). However, several other intervention components had a large effect size on SBP (−11.0 to −4.8 mm Hg) including: 1) free medications (−10.80 mm Hg), 2) pharmacist made treatment recommendation to the physician (−9.30 mm Hg), 3) pharmacist did the intervention (−8.44 mm Hg), 4) a drug profile was compiled (−8.19 mm Hg), 5) medication compliance was assessed (−7.90 mm Hg), 6) counseling on lifestyle modification was performed (−7.59 mm Hg), 7) provider of the intervention could order laboratory tests (−7.00), and 8) nurse did the intervention (−4.8 mm Hg) (Table 2).
Table 2.
Effect of Quality Improvement Strategies on Blood Pressure Outcomes
| Type of Quality Improvement |
Median Reduction in Systolic Blood Pressure (mm Hg) [Interquartile range]# n = number of studies |
Median Reduction in Diastolic Blood Pressure (mm Hg) [Interquartile range]# n = number of studies |
|---|---|---|
| Free medications | −10.8 [−14.9, −9.10] n = 318, 39, 50 |
−6.4 [−8.70, −3.90] n = 318, 39, 50 |
| Pharmacist recommended medication to physician |
−9.30 *[−13.00, −5.00] n = 158, 20-24, 26, 27, 29, 30, 35, 37, 43, 46, 48 |
−3.60 [−7.03, −1.00] n = 158, 20-24, 26, 27, 29, 30, 35, 37, 43, 46, 48 |
| Education on BP medications |
−8.75**[−11.90, −4.25] n = 288, 17-23, 26-30, 32, 34, 35, 37, 39-44, 46-50 |
−3.60**[−7.03, −1.00] n = 278, 17, 18, 20-23, 26-30, 32, 34, 35, 37, 39-44, 46-50 |
| Pharmacist did intervention |
−8.44 [−12.25, −4.00] n = 228, 19-22, 24-30, 34-37, 41, 43, 46, 48, 50, 51 |
−3.30 [−6.87, −0.90] n = 218, 19-22, 24-30, 34-37, 41, 43, 46, 48, 50, 51 |
| Drug profile was completed |
−8.19 [−11.45, −2.93] n = 168, 17, 20, 21, 23, 25-27, 29, 30, 32, 35, 40, 42-44, 46, 48 |
−3.25 [−4.67, −1.00] n = 168, 17, 20, 21, 23, 25-27, 29, 30, 32, 35, 40, 42-44, 46, 48 |
| Assessed medication compliance |
−7.90 [−11.90, −3.48] n = 248, 17, 20, 21, 23, 25-30, 34-37, 39-44, 46, 47, 50 |
−3.25 [−8.65, −0.85] n = 248, 17, 20, 21, 23, 25-30, 34-37, 39-44, 46, 47, 50 |
| Counseling on lifestyle modification |
−7.59 [−11.45, −2.40] n = 288, 16, 17, 19-23, 26-32, 34, 35, 37, 38, 40-42, 45-50 |
−3.30 [−6.70, −1.00] n = 278, 16, 17, 20-23, 26-32, 34, 35, 37, 38, 40-42, 45-50 |
| Provider in intervention could order laboratory |
−7.00 [−8.94, −1.30] n = 916, 22, 25, 31, 33, 44, 48-50 |
−3.68 [−5.40,−0.15] n = 916, 22, 25, 31, 33, 44, 48-50 |
| Nurse did intervention | −4.80* [−9.63, −0.43] n =1616-19, 31-33, 38-42, 44, 45, 47, 49 |
−3.10 [−6.00, −0.10] n =1516-18, 31-33, 38-42, 44, 45, 47, 49 |
| Used algorithm for treatment |
−4.00* [−8.15, −0.90] n = 916, 23, 25, 32, 33, 35, 37, 44, 49 |
−1.00* [−4.20, −0.15] n = 916, 23, 25, 32, 33, 35, 37, 44, 49 |
| Made a home visit | −4.00 [−9.95, 0.15] n = 517, 18, 38, 41, 44 |
−1.00 [−4.95, 0.60] n = 517, 18, 38, 41, 44 |
| Provider of intervention could prescribe medication |
−2.40 [−11.28, 4.75] n = 416, 25, 28, 32 |
−0.65 [−11.35, −0.08] n = 416, 25, 28, 32 |
| Physical examination was conducted |
2.10* [−2.80, 7.00] n = 216, 25 # |
−0.15* [−0.30, 0.00] n = 216, 25 # |
When n = 2, brackets show the actual results of each study rather than interpolated interquartile range.
p < 0.10
p < 0.05 for Mann-Whitney analysis of reduction in systolic blood pressure and diastolic blood pressure comparing studies with the quality improvement strategy with those without it.
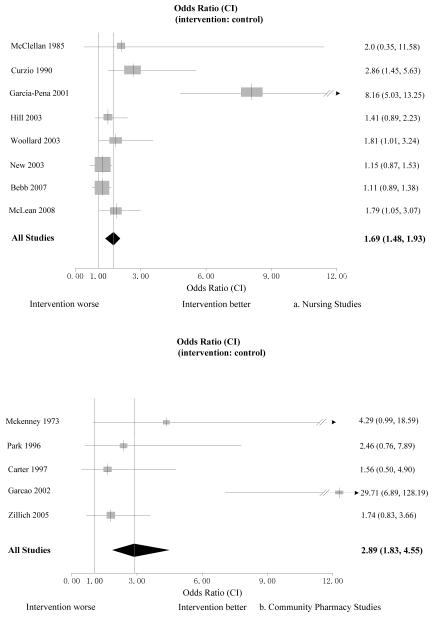
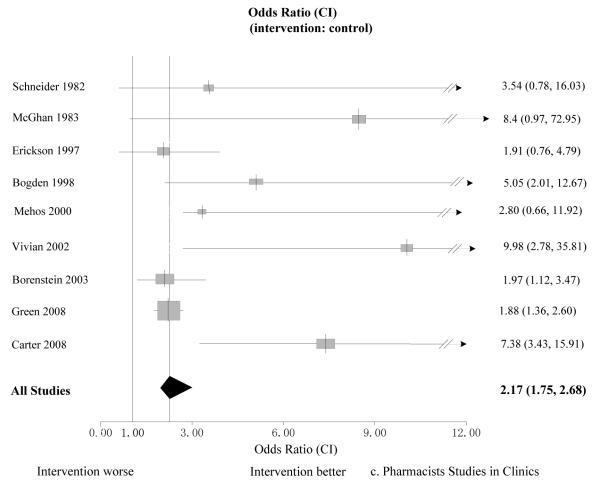
The estimated odds ratio and 95% confidence interval (CI) for controlled BP for nursing studies was OR=1.69 (CI = 1.48, 1.93) (Figure 2a), studies involving community pharmacists was OR=2.89 (CI = 1.83, 4.55) (Figure 2b), and studies involving pharmacists within primary care clinics was OR=2.17 (CI = 1.75, 2.68) (Figure 2c).
Figure 2.
The Odds Ratio (confidence interval) that systolic blood pressure is controlled in the intervention group compared to the control group. Figure 2a displays 8 studies involving nurses, Figure 2b displays 5 studies conducted in community pharmacies and Figure 2c figure displays 9 studies involving pharmacists in primary care clinics.
In the non-parametric analyses of the 36 studies, the mean reduction in SBP was 5.84 ± 8.05 mm Hg for nursing studies (n=16) compared to 7.76 ± 7.81 mm Hg in the studies involving pharmacists in clinics (n=7) and 9.31 ± 5.00 mm Hg for studies by community pharmacists (n=13). Reductions in diastolic BP were 3.46 ± 4.15 mm Hg for nursing studies, 4.18 ± 4.25 mm Hg for pharmacists in clinics and 4.59 ± 4.64 mm Hg for community pharmacists (SBP and DBP were not significantly different between any group).
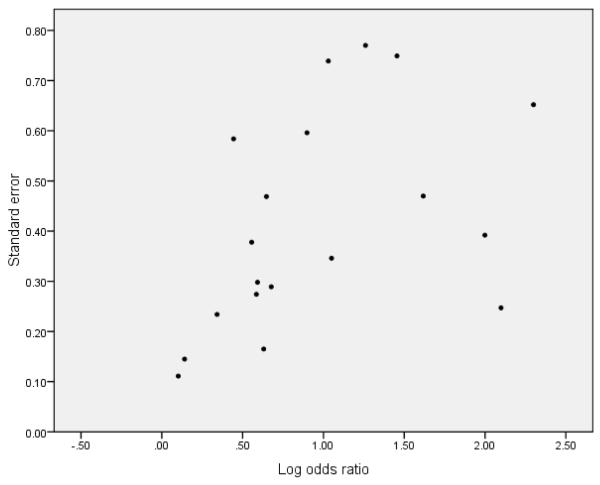
We constructed a funnel plot to evaluate whether there may have been publication bias (Figure 3). Three of four studies with the largest log odds ratios had moderate to low standard error suggesting the absence of publication bias. However, publication bias cannot be ruled out since there are few studies with high log odds ratios and low standard error.
Figure 3.
Funnel plot for all studies included in Figure 2
Discussion
This study found that interventions involving pharmacists or nurses were associated with significantly improved BP control. These findings extended the previous report that found involving pharmacists or nurses was the most potent quality improvement strategy to improve BP control.6 We also wanted to determine if specific aspects of team care were more potent. Our analysis found that studies involving pharmacists resulted in not only lower BP but a greater OR of achieving BP control compared to studies involving nurses. However, the reductions in systolic BP and confidence intervals for controlled BP (Figure 2) overlap for the different providers.
We had hypothesized that studies involving community pharmacists would be less potent than those involving nurses or pharmacists within primary care clinics. Interestingly, studies involving community pharmacists had the highest OR (2.89). These findings may be based on how the reviewers categorized the studies. First, one study conducted in community pharmacies in Portugal had an extremely high OR (29.71).22 Another study in community pharmacy had an OR of 4.29 but this pharmacist worked closely with two physicians and reviewed medical records of study patients in the physicians’ office.20 Instead, we could have classified this as a “pharmacist in the clinic” which would have reduced the OR for community pharmacy studies and increased the OR for “pharmacists in clinics.” Second, we classified one study as a nursing intervention for the OR calculations but the intervention involved both a nurse and community pharmacist (OR=1.79).19 Excluding the first two studies and adding the third study to the analysis of community pharmacy studies would have resulted in an OR closer to 1.8 for the “community pharmacy” group.
Finally, one large study was conducted within a managed care organization that involved education by a pharmacist via the web.35 We classified this study as one within primary care but this study did not have as great of an effect (OR=1.88) compared to studies in which the pharmacist adjusted therapy either alone or in collaboration with physicians (OR=7.38-9.98). Without that study, the OR would have been 3.27 for “pharmacist in clinics”. It may be possible to explain our findings based on the dose, duration and potency of the intervention. For instance, Carter conducted three studies in community pharmacies, where the pharmacists had no prior established relationship with the physicians and the interventions were only 4 and 5 months in length.8, 21, 23 These studies had modest OR for controlled BP (1.56, 1.74 and 2.46). Carter recently completed a randomized controlled effectiveness (pragmatic) study of a 6-month pharmacist intervention in 402 patients from six family medicine clinics that was not included in this systematic review because it was unpublished at the time of our evaluation.52 In that study, SBP was reduced 12.0 mm Hg more in the intervention group than the control group and the OR for controlled BP was OR= 3.2 (95% CI 2.0, 5.1). Finally, these investigators conducted an efficacy study in which BP was controlled in 54% of patients in the control group and 89% in the intervention group (OR 7.38, CI 3.43, 15.91).30 The main reason for high BP control in this latter study was attributed to assertive and frequent medication intensification recommended by the pharmacist. Thus, the OR for the 5 studies by these investigators were: community pharmacy studies (B.S. trained pharmacists) between 1.56-2.46; the pragmatic trial of clinical pharmacists (Pharm.D. with residency or fellowship) 3.2 and the efficacy trial (ideal intervention delivery) with clinical pharmacists (Pharm.D. with residency) of 7.38.
Therefore, when the literature involving team care is evaluated, it is critical to assess the duration of the intervention, the type of organization in which the intervention is performed (home, worksite, community pharmacy or primary care clinic) and whether the study is an efficacy or effectiveness trial. These factors, as well as the activities of the intervention, predict the potency of the intervention.
Studies involving community pharmacists largely involved making recommendations to physicians by telephone or facsimile. Studies involving pharmacists in clinics typically involved pharmacists employed in the clinic and who worked collaboratively with physician colleagues and/or provided more autonomous care. Pharmacists within primary care clinics work closely with physicians and the expected levels of trust and cooperation might be higher than with community pharmacists where interaction is usually not in person and occurs from distant locations.23, 51, 53 In fact, recommendations to change BP medications were accepted 95% of the time from pharmacists within the same clinic30 but only 45-50% when recommendations were made by community pharmacists.8, 21, 23 Therefore, lower acceptance for community pharmacists’ recommendations could be due to lower levels of trust and cooperation by physicians.51, 53
Many of the nursing studies did not describe the types of nurses, their educational background or training but four studies used either registered nurses or nurse practitioners.15, 16, 18, 42, 49 Nursing interventions seemed more likely to involve home visits, use an algorithm and patient engagement than pharmacy studies. It is likely that many of the interventions involving nurses or pharmacists increased patient empowerment but few studies specifically provided such descriptions. Only 5 nursing studies described a patient-led process17, 47, 49 or home BP monitoring41, 42 and 3 pharmacy studies used home BP monitoring.23, 34, 35 We suspect that nurse practitioners would have more autonomy than registered nurses and in some cases, nurse practitioners can prescribe medications. We could not detect whether nursing degree or training influenced the results. However, using an algorithm or making a home visit both had a predicted reduction in SBP of4 mm Hg.
Each intervention, or combination of intervention components, is/are unique. It is not possible to state that either nurses or pharmacists can improve BP control without first determining the patient population, organizational structure involved and the type of autonomy the interventionist has to change therapy. Strategies that provided medication education were the most effective but this strategy is impossible to evaluate alone since it was usually provided with additional strategies by the nurse or pharmacist who may have recommended therapy changes or personally changed therapy within a primary care office. Any incremental addition of components from Table 2 that a physician office or health system can implement should improve BP control rates but this requires additional research. We believe that nurses possess unique skills in patient management and non-medication counseling techniques that pharmacists usually do not. Likewise, pharmacists receive four years of concentrated education in medication pharmacology, pharmacokinetics, pharmacodyamics, therapeutics and chronic disease drug-therapy guidelines. Including both nurses and pharmacists in an integrated hypertension management program should be even more effective than either alone and should be more cost effective. Consistent with our findings, the pharmacists could adjust medications until BP is controlled while the nurse provides continuity and counseling on lifestyle and social support.9, 10 The nurse would continue to serve as a case manager between physician visits when BP is controlled. The pharmacist would then only be re-activated if BP control is lost. Such an approach can not only improve BP control rates but markedly improve the efficiency and productivity of the physician.54, 55 Including many of the components of these interventions into hypertension management programs could improve the implementation of the JNC-8 or other chronic disease guidelines.
Strengths and Limitations of the publications
The vast majority of the studies (89%) were randomized controlled trials (Appendix 1). The quality of the studies support the findings that these interventions are likely to be effective. There were, however, large differences in the duration of the intervention (4-24 months), sample size (26-1,534) and subject (patient) dropout (2-62%). Nearly all of the studies adequately described the most important characteristics of the patients but many did not adequately describe the number, education and training of the intervention pharmacists or nurses. Our analysis could not determine if there is a preferred level of qualifications such as a PharmD degree with residency or a MS nurse practitioner degree. Likewise, many studies did not describe the training but those that did typically noted ½ to 2 day training programs on the hypertension guidelines and BP measurement. It is possible that RN nurses or B.S. pharmacists may have required more intense or longer training than nurse practitioners or pharmacists with PharmD degrees with residencies, but this could not be determined from these studies. Future interventional studies of this type should specify the educational background, postgraduate training and specific training programs for the study that were used to implement the intervention.
Only one study performed a cost-effectiveness analysis.48 Clinic visit costs were significantly higher in the pharmacist-managed clinic ($131 per patient) than the physician clinic ($74) (p<0.001), but the costs for emergency room visits was significantly lower in the pharmacist-managed clinic than the physician clinic ($0 vs $10.84 per patient, p<0.04). The cost of decreasing SBP/mm Hg was $27 for the pharmacist-managed clinic and $193 for the physician clinic. The cost of decreasing DBP/mm Hg was $48 in the pharmacist-managed clinic and $151 in the physician clinic.
Twelve studies (9 nursing, 2 in community pharmacies, 1 pharmacist in clinics) were conducted in countries other than the U.S.16, 17, 19, 22, 31-33, 39, 43-45, 47 It is not know what effects the unique characteristics of the health care system in these countries might have had on the interventions. Likewise, some studies were conducted in integrated managed care settings29, 35 or the Department of Defense or Veterans Administration.28, 50 Future research should clarify the functional components of a team and how best to utilize the strengths of members of this team as they fit into the chronic care model.56, 57 Also, the larger impact of the health care delivery system on the potency of these interventions should be assessed, specifically if incentives might be aligned to optimize performance. Finally, we cannot rule out publication bias in our analyses since only 3 studies had high odds ratios and low standard error.
Conclusion
This evaluation of team-based care in hypertension found that interventions involving nurses or pharmacists are effective strategies to improve BP control. Several individual components were associated with improvements in BP. Research involving team-based care must be carefully designed, reported and interpreted to include the organizational structure in which the intervention is performed, the education and training of the intervention providers and the individual components of the intervention so that similar interventions can be implemented within a given health system.
Supplementary Material
Acknowledgments
Supported, in part from National Heart, Lung, and Blood Institute grant HL070740 and the Agency for Healthcare Research and Quality (AHRQ) Centers for Education and Research on Therapeutics Cooperative Agreement #5U18HSO16094. Dr. Carter is also supported by the Center for Research in Implementation in Innovative Strategies in Practice (CRIISP), Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service (HFP 04-149). The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans
References
- 1.Garg JP, Elliott WJ, Folker A, Izhar M, Black HR. Resistant hypertension revisited: a comparison of two university-based cohorts. Am J Hypertens. 2005;18:619–626. doi: 10.1016/j.amjhyper.2004.11.021. [DOI] [PubMed] [Google Scholar]
- 2.Berlowitz DR, Ash AS, Hickey EC, et al. Inadequate management of blood pressure in a hypertensive population. N Engl J Med. 1998;339:1957–1963. doi: 10.1056/NEJM199812313392701. [DOI] [PubMed] [Google Scholar]
- 3.Oliveria SA, Lapuerta P, McCarthy BD, L’Italien GJ, Berlowitz DR, Asch SM. Physician-related barriers to the effective management of uncontrolled hypertension. Arch Intern Med. 2002;162:413–420. doi: 10.1001/archinte.162.4.413. [DOI] [PubMed] [Google Scholar]
- 4.Hyman DJ, Pavlik VN. Characteristics of patients with uncontrolled hypertension in the United States. N Engl J Med. 2001;345:479–486. doi: 10.1056/NEJMoa010273. [DOI] [PubMed] [Google Scholar]
- 5.Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999-2004. Hypertension. 2007;49:69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- 6.Walsh JM, McDonald KM, Shojania KG, et al. Quality improvement strategies for hypertension management: a systematic review. Med Care. 2006;44:646–657. doi: 10.1097/01.mlr.0000220260.30768.32. [DOI] [PubMed] [Google Scholar]
- 7.Weinberger M, Oddone EZ, Henderson WG, et al. Multisite randomized controlled trials in health services research: scientific challenges and operational issues. Med Care. 2001;39:627–634. doi: 10.1097/00005650-200106000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Carter BL, Barnette DJ, Chrischilles E, Mazzotti GJ, Asali ZJ. Evaluation of hypertensive patients after care provided by community pharmacists in a rural setting. Pharmacotherapy. 1997;17:1274–1285. [PubMed] [Google Scholar]
- 9.Carter BL. Hypertension Disease Management Services. In: Black HR, Elliott WJ, editors. Hypertension, A Companion to Braunwald’s Heart Disease. Elsevier; Philadelphia, Pennsylvania: 2007. pp. 527–534. [Google Scholar]
- 10.Carter BL. Nonphysician providers and the management of hypertension. In: Izzo JL, Sica DA, Black HR, editors. Hypertension Primer. 4th edition American Heart Association; 2008. pp. 424–427. [Google Scholar]
- 11.Bosworth HB, Olsen MK, Dudley T, et al. The Take Control of Your Blood pressure (TCYB) study: study design and methodology. Contemp Clin Trials. 2007;28:33–47. doi: 10.1016/j.cct.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 12.Bosworth HB, Olsen MK, Gentry P, et al. Nurse administered telephone intervention for blood pressure control: a patient-tailored multifactorial intervention. Patient Educ Couns. 2005;57:5–14. doi: 10.1016/j.pec.2004.03.011. [DOI] [PubMed] [Google Scholar]
- 13.Bosworth HB, Olsen MK, Goldstein MK, et al. The veterans’ study to improve the control of hypertension (V-STITCH): design and methodology. Contemp Clin Trials. 2005;26:155–168. doi: 10.1016/j.cct.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 14.Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 15.McClellan WM, Craxton LC. Improved follow-up care of hypertensive patients by a nurse practitioner in a rural clinic. J Rural Health. 1985;1:34–41. doi: 10.1111/j.1748-0361.1985.tb00125.x. [DOI] [PubMed] [Google Scholar]
- 16.Curzio JL, Rubin PC, Kennedy SS, Reid JL. A comparison of the management of hypertensive patients by nurse practitioners compared with conventional hospital care. J Hum Hypertens. 1990;4:665–670. [PubMed] [Google Scholar]
- 17.Garcia-Pena C, Thorogood M, Armstrong B, Reyes-Frausto S, Munoz O. Pragmatic randomized trial of home visits by a nurse to elderly people with hypertension in Mexico. Int J Epidemiol. 2001;30:1485–1491. doi: 10.1093/ije/30.6.1485. [DOI] [PubMed] [Google Scholar]
- 18.Hill MN, Han HR, Dennison CR, et al. Hypertension care and control in underserved urban African American men: behavioral and physiologic outcomes at 36 months. Am J Hypertens. 2003;16:906–913. doi: 10.1016/s0895-7061(03)01034-3. [DOI] [PubMed] [Google Scholar]
- 19.McLean DL, McAlister FA, Johnson JA, et al. A randomized trial of the effect of community pharmacist and nurse care on improving blood pressure management in patients with diabetes mellitus: study of cardiovascular risk intervention by pharmacists-hypertension (SCRIP-HTN) Arch Intern Med. 2008;168:2355–2361. doi: 10.1001/archinte.168.21.2355. [DOI] [PubMed] [Google Scholar]
- 20.McKenney JM, Slining JM, Henderson HR, Devins D, Barr M. The effect of clinical pharmacy services on patients with essential hypertension. Circulation. 1973;48:1104–1111. doi: 10.1161/01.cir.48.5.1104. [DOI] [PubMed] [Google Scholar]
- 21.Park JJ, Kelly P, Carter BL, Burgess PP. Comprehensive pharmaceutical care in the chain (pharmacy) setting. J Am Pharm Assoc. 1996;NS36:443–451. doi: 10.1016/s1086-5802(16)30099-7. [DOI] [PubMed] [Google Scholar]
- 22.Garcao JA, Cabrita J. Evaluation of a pharmaceutical care program for hypertensive patients in rural Portugal. J Am Pharm Assoc. 2002;42:858–864. doi: 10.1331/108658002762063691. [DOI] [PubMed] [Google Scholar]
- 23.Zillich AJ, Sutherland JM, Kumbera PA, Carter BL. Hypertension outcomes through blood pressure monitoring and evaluation by pharmacists (HOME study) J Gen Intern Med. 2005;20:1091–1096. doi: 10.1111/j.1525-1497.2005.0226.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schneider PJ, Larrimer JN, Visconti JA, Miller WA. Role effectiveness of a pharmacist in the maintenance of patients with hypertension and congestive heart failure. Contemp Pharm Pract. 1982;5:74–79. [PubMed] [Google Scholar]
- 25.McGhan WF, Stimmel GL, Hall TG, Gilman TM. A comparison of pharmacists and physicians on the quality of prescribing for ambulatory hypertensive patients. Med Care. 1983;21:435–444. doi: 10.1097/00005650-198304000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Erickson SR, Slaughter R, Halapy H. Pharmacists’ ability to influence outcomes of hypertension therapy. Pharmacotherapy. 1997;17:140–147. [PubMed] [Google Scholar]
- 27.Bogden PE, Abbott RD, Williamson P, Onopa JK, Koontz LM. Comparing standard care with a physician and pharmacist team approach for uncontrolled hypertension. J Gen Intern Med. 1998;13:740–745. doi: 10.1046/j.1525-1497.1998.00225.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vivian EM. Improving blood pressure control in a pharmacist-managed hypertension clinic. Pharmacotherapy. 2002;22:1533–1540. doi: 10.1592/phco.22.17.1533.34127. [DOI] [PubMed] [Google Scholar]
- 29.Borenstein JE, Graber G, Saltiel E, et al. Physician-pharmacist comanagement of hypertension: a randomized, comparative trial. Pharmacotherapy. 2003;23:209–216. doi: 10.1592/phco.23.2.209.32096. [DOI] [PubMed] [Google Scholar]
- 30.Carter BL, Bergus GR, Dawson JD, et al. A Cluster Randomized Trial to Evaluate Physician/Pharmacist Collaboration to Improve Blood Pressure Control. J Clin Hypertens. 2008;10:260–271. doi: 10.1111/j.1751-7176.2008.07434.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Woollard J, Burke V, Beilin LJ. Effects of general practice-based nurse-counselling on ambulatory blood pressure and antihypertensive drug prescription in patients at increased risk of cardiovascular disease. J Hum Hypertens. 2003;17:689–695. doi: 10.1038/sj.jhh.1001593. [DOI] [PubMed] [Google Scholar]
- 32.New JP, Mason JM, Freemantle N, et al. Specialist nurse-led intervention to treat and control hypertension and hyperlipidemia in diabetes (SPLINT): a randomized controlled trial. Diabetes Care. 2003;26:2250–2255. doi: 10.2337/diacare.26.8.2250. [DOI] [PubMed] [Google Scholar]
- 33.Bebb C, Kendrick D, Coupland C, et al. A cluster randomised controlled trial of the effect of a treatment algorithm for hypertension in patients with type 2 diabetes. Br J Gen Pract. 2007;57:136–143. [PMC free article] [PubMed] [Google Scholar]
- 34.Mehos BM, Saseen JJ, MacLaughlin EJ. Effect of pharmacist intervention and initiation of home blood pressure monitoring in patients with uncontrolled hypertension. Pharmacotherapy. 2000;20:1384–1389. doi: 10.1592/phco.20.17.1384.34891. [DOI] [PubMed] [Google Scholar]
- 35.Green BB, Cook AJ, Ralston JD, et al. Effectiveness of home blood pressure monitoring, Web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA. 2008;299:2857–2867. doi: 10.1001/jama.299.24.2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hawkins DW, Fiedler FP, Douglas HL, Eschbach RC. Evaluation of a clinical pharmacist in caring for hypertensive and diabetic patients. Am J Hosp Pharm. 1979;36:1321–1325. [PubMed] [Google Scholar]
- 37.Solomon DK, Portner TS, Bass GE, et al. Clinical and economic outcomes in the hypertension and COPD arms of a multicenter outcomes study. Journal of the American Pharmaceutical Association. 1998;38:574–585. doi: 10.1016/s1086-5802(16)30371-0. [DOI] [PubMed] [Google Scholar]
- 38.Hill MN, Bone LR, Hilton SC, Roary MC, Kelen GD, Levine DM. A clinical trial to improve high blood pressure care in young urban black men: recruitment, follow-up, and outcomes. Am J Hypertens. 1999;12:548–554. doi: 10.1016/s0895-7061(99)00007-2. [DOI] [PubMed] [Google Scholar]
- 39.Guerra-Riccio GM, Giorgi DM Artigas, Consolin-Colombo FM, et al. Frequent nurse visits decrease white coat effect in stage III hypertension. Am J Hypertens. 2004;17:523–528. doi: 10.1016/j.amjhyper.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 40.Rudd P, Miller NH, Kaufman J, et al. Nurse management for hypertension. A systems approach. Am J Hypertens. 2004;17:921–927. doi: 10.1016/j.amjhyper.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 41.Artinian NT, Flack JM, Nordstrom CK, et al. Effects of nurse-managed telemonitoring on blood pressure at 12-month follow-up among urban African Americans. Nurs Res. 2007;56:312–322. doi: 10.1097/01.NNR.0000289501.45284.6e. [DOI] [PubMed] [Google Scholar]
- 42.Artinian NT, Washington OG, Templin TN. Effects of home telemonitoring and community-based monitoring on blood pressure control in urban African Americans: a pilot study. Heart Lung. 2001;30:191–199. doi: 10.1067/mhl.2001.112684. [DOI] [PubMed] [Google Scholar]
- 43.de Castro MS, Fuchs FD, Santos MC, et al. Pharmaceutical care program for patients with uncontrolled hypertension. Report of a double-blind clinical trial with ambulatory blood pressure monitoring. Am J Hypertens. 2006;19:528–533. doi: 10.1016/j.amjhyper.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 44.Tobe SW, Pylypchuk G, Wentworth J, et al. Effect of nurse-directed hypertension treatment among First Nations people with existing hypertension and diabetes mellitus: the Diabetes Risk Evaluation and Microalbuminuria (DREAM 3) randomized controlled trial. CMAJ. 2006;174:1267–1271. doi: 10.1503/cmaj.050030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tonstad S, Alm CS, Sandvik E. Effect of nurse counselling on metabolic risk factors in patients with mild hypertension: a randomised controlled trial. Eur J Cardiovasc Nurs. 2007;6:160–164. doi: 10.1016/j.ejcnurse.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 46.Murray MD, Harris LE, Overhage JM, et al. Failure of computerized treatment suggestions to improve health outcomes of outpatients with uncomplicated hypertension: results of a randomized controlled trial. Pharmacotherapy. 2004;24:324–337. doi: 10.1592/phco.24.4.324.33173. [DOI] [PubMed] [Google Scholar]
- 47.Schroeder K, Fahey T, Hollinghurst S, Peters TJ. Nurse-led adherence support in hypertension: a randomized controlled trial. Fam Pract. 2005;22:144–151. doi: 10.1093/fampra/cmh717. [DOI] [PubMed] [Google Scholar]
- 48.Okamoto MP, Nakahiro RK. Pharmacoeconomic evaluation of a pharmacist-managed hypertension clinic. Pharmacotherapy. 2001;21:1337–1344. doi: 10.1592/phco.21.17.1337.34424. [DOI] [PubMed] [Google Scholar]
- 49.Gabbay RA, Lendel I, Saleem TM, et al. Nurse case management improves blood pressure, emotional distress and diabetes complication screening. Diabetes Res Clin Pract. 2006;71:28–35. doi: 10.1016/j.diabres.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 50.Lee JK, Grace KA, Taylor AJ. Effect of a pharmacy care program on medication adherence and persistence, blood pressure, and low-density lipoprotein cholesterol: a randomized controlled trial. JAMA. 2006;296:2563–2571. doi: 10.1001/jama.296.21.joc60162. [DOI] [PubMed] [Google Scholar]
- 51.Zillich AJ, Doucette WR, Carter BL, Kreiter CD. Development and initial validation of an instrument to measure physician-pharmacist collaboration from the physician perspective. Value Health. 2005;8:59–66. doi: 10.1111/j.1524-4733.2005.03093.x. [DOI] [PubMed] [Google Scholar]
- 52.Carter BL, Ardery G, Dawson JD, James PA, Bergus GR, Doucette WR, Chrischilles EA. A Randomized-Controlled Effectiveness Trial of Physician/Pharmacist Collaboration to Improve Blood Pressure Control. Arch Intern Med. 2009 doi: 10.1001/archinternmed.2009.358. (in 2nd review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zillich AJ, McDonough RP, Carter BL, Doucette WR. Influential characteristics of physician/pharmacist collaborative relationships. Ann Pharmacother. 2004;38:764–770. doi: 10.1345/aph.1D419. [DOI] [PubMed] [Google Scholar]
- 54.Conrad D, Fishman P, Grembowski D, et al. Access intervention in an integrated, prepaid group practice: effects on primary care physician productivity. Health Serv Res. 2008;43:1888–1905. doi: 10.1111/j.1475-6773.2008.00880.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dorr DA, Wilcox A, McConnell KJ, Burns L, Brunker CP. Productivity enhancement for primary care providers using multicondition care management. Am J Manag Care. 2007;13:22–28. [PubMed] [Google Scholar]
- 56.Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1998;1:2–4. [PubMed] [Google Scholar]
- 57.Wagner EH. The role of patient care teams in chronic disease management. BMJ. 2000;320:569–572. doi: 10.1136/bmj.320.7234.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gourley DR, Gourley GA, Solomon DK, et al. Development, implementation, and evaluation of a multicenter pharmaceutical care outcomes study. J Am Pharm Assoc. 1998;38:567–573. doi: 10.1016/s1086-5802(16)30370-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.