Summary
We compared the effects of evidence-based disease management guidelines delivered to patients with heart failure and diabetes using three different modalities: in-person visits alone (Control), in-person visits and a telephone intervention (Telephone), and in-person visits and telemonitoring (Telemonitoring). Patients were randomized to the three groups. There were 112 patients in the Control group, 93 in the Telephone group and 98 in the Telemonitoring group. During the first 60 days, 10% of the Control group were rehospitalized, 17% of the Telephone group and 16% of the Telemonitoring group. Having heart failure and receiving more in-person visits were significantly related to readmission and time to readmission. However, after adjusting for diagnosis and visits, the differences between the three groups were non-significant. There was a trend for increased risk of readmission for the Telephone group compared to Control alone (P= 0.07, risk ratio 2.2, 95% CI: 0.9 to 5.2) and for readmission sooner (P=0.02, risk ratio 2.3, 95% CI: 1.2 to 4.6). Patient rehospitalization and emergency department visit rates were lower than the national average, making it difficult to detect a difference between groups. Previous rehospitalization was a consistent predictor of those who were rehospitalized, suggesting that it may be a useful indicator for identifying patients likely to need additional attention.
Introduction
In the USA, 36 million people are aged over 65 years and the number of older Americans is growing rapidly.1 At least 80% have at least one chronic condition and 50% have two or more.2 A disproportionate share of health-care costs, about 83%, is from people with chronic conditions.3 The cost of medical care for chronic conditions was $470 billion in 1995, and it is estimated that by 2040 the cost could rise to $864 billion.4 New ways to manage chronic illness are imperative, especially as the population ages, chronic illness increases and the nursing shortage continues.
Evidence-based disease management programmes are designed to help patients improve self care and provide better clinical information for clinicians. Interventions generally include assessing health status, teaching and guiding patients about their care. The goals of disease management programmes are to facilitate adherence to evidence-based guidelines that should improve health and cost outcomes.5 Disease management can be provided in-person or by telephone.
Disease management programmes delivered by telephone have achieved positive health outcomes for chronically ill patients, most commonly heart failure (HF).6–8 However, the cost-effectiveness of these programmes is still in question.9,10 A meta-analysis of 11 studies of disease management in HF showed a 13% reduction in rehospitalization, but sub-analyses of the two studies that used a telephone modality did not show significant reductions in rehospitalization.11
Telemonitoring has the potential to improve the management of chronic illness and decrease preventable rehospitalizations and associated costs.12,13 Acquiring physiological data regularly from monitoring devices may be a better method of disease management than using in-person or telephone delivery. However, few studies have directly measured the value of telemonitoring. One study (n = 148) reported no significant improvements in medication compliance, self-efficacy or satisfaction when comparing telephone to telemonitoring intervention.14 Another (n = 37) reported success over usual care when telemonitoring and telephone groups were combined. However, there was no reported incremental benefit from telemonitoring over telephone contact.15 Nonetheless, telemonitoring is experiencing rapid growth based on its potential to increase access to care, improve clinical outcomes and decrease costs.13,16
The aim of the present study was to compare the effects of evidence-based disease management guidelines delivered to patients with HF and diabetes using three different modalities: in-person visits alone (Control), in-person visits and telephone intervention (Telephone) and in-person visits and telemonitoring (Telemonitoring). Readmission at 60 days was the primary outcome.
Methods
We conducted a prospective, randomized, study comparing outcomes among chronically ill adults who were receiving home care. The study was conducted at four agencies in Pennsylvania ranging in size from 5000 to 16,000 patients/year, most being rural. Eligible patients were those aged 55 years and older, receiving home care with HF or diabetes as one of the two main diagnoses, cognitively intact, able to hear and see well enough to use the equipment, English speaking, and having a conventional (fixed) telephone. Patients followed by other programmes were excluded because they received a different follow-up protocol.
Based on pilot work and the literature,11,14 the rate of rehospitalization for the Telemonitoring group was expected to be 20%. Thus, a sample size of 90 per group gave a power of 0.80, alpha = 0.05. Assuming an attrition rate of 25%, the goal was to recruit 324 subjects.
Following approval by the appropriate ethics committee, site coordinators or home care nurses obtained consent from the patients. The site coordinator randomized patients using sealed envelopes.
Usual care
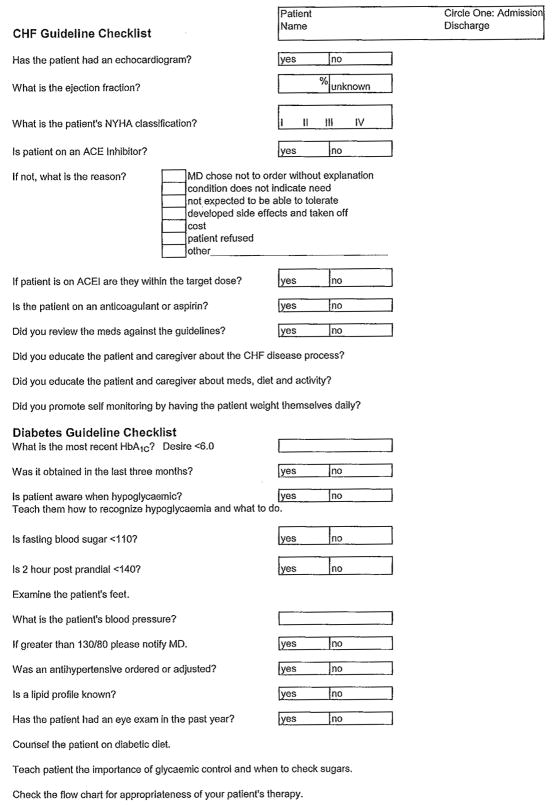
All patients, regardless of group assignment, received home nursing guided by the appropriate evidence-based disease-management protocol for HF, diabetes or both. The guidelines were developed and tested after extensive review of national guidelines by the Department of Health and Disease Management and, subsequently, by the Department of Clinical Effectiveness and Quality Improvement at the University of Pennsylvania Health System. The guidelines included the latest evidence for screening, monitoring, treating and teaching patients with HF or diabetes. Forty nurses were taught how to use the guidelines. They were instructed to compare the plan of care to the guidelines and complete the checklist elements that prompted and standardized the use of the disease-management guidelines (Figure 1). Nurses were encouraged to discuss discrepancies with the patients’ physician and request changes in the plan of care to increase concordance with the guidelines.
Figure 1.
Nurses’ guide to evidence-based practice
Telephone group
Nurses made at least four telephone contacts in addition to home visits. The nurses used a standard interview guide to ensure consistency (see Figure 2). The interview guide was developed and validated by physicians in the Department of Clinical Effectiveness and Quality Improvement as described above.
Figure 2.
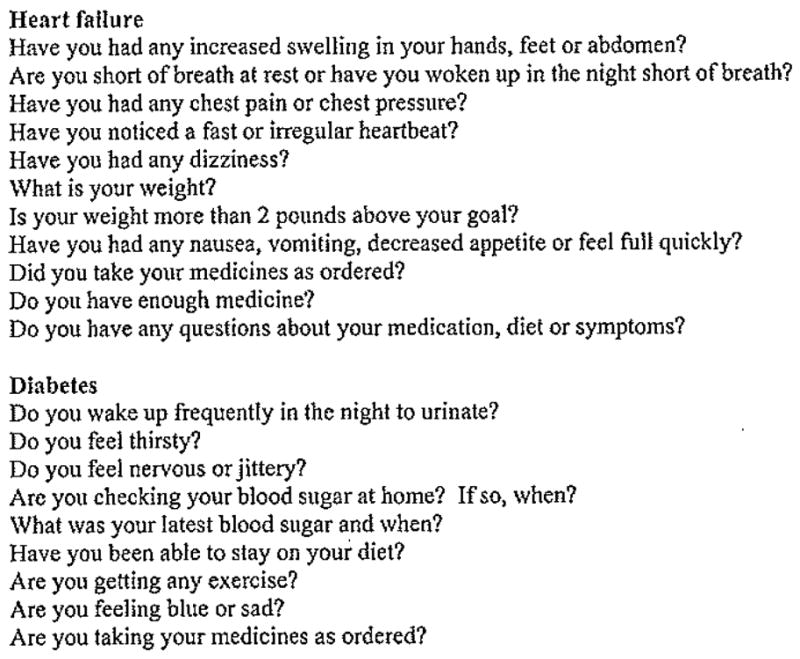
Phone call guide for heart failure or diabetes disease management
Telemonitoring group
Three different kinds of telehealth monitors were used. Two monitors provided physiological monitoring, with a blood pressure cuff, bodyweight scale, glucometer and pulse oximeter (Sentry III, Honeywell HomMed, Inc. and ViTelCare Turtle, Visual Telecommunications Network, Inc.). The third monitor (Aviva 1010, American TeleCare Inc.) provided this plus a digital stethoscope and videoconferencing. The telehealth information was transmitted to the agency where it was monitored daily by the nurses. Nurses assessed physical and emotional status, reviewed medications, and instructed the patients on self care and disease management. In those using video, nurses were instructed to make at least four video contacts. The monitoring equipment, used daily, was left in the patients’ homes until they were discharged.
Data collection
Two trained, blinded, research assistants collected baseline data within one week of admission by telephone. The information included sociodemographics; self-rated health; depression; hospitalizations in the last year; and knowledge, behaviour, and severity of symptoms related to diet and medications. Follow-up data were collected at 60 days and included the same outcomes plus emergency department (ED) and hospital use. At 90 days, self-rated health status, ED use and rehospitalization dates and reasons were collected.
Instruments
Age, ethnicity, gender, marital status, educational level and income data were collected using an investigator-developed form.
Prediction of rehospitalization (Pra). The Pra instrument is an eight-item questionnaire that measures risk of readmission.17,18 The Pra score is a value between 0 and 1, with higher values indicating higher probability of readmission. In previous studies, patients with Pra scores >0.50 were rehospitalized at twice the rate of subjects scoring <0.50.18,19 A high test-retest reliability (kappa = 0.78) has been reported.20
Self-rated health was measured using a single question, ‘How would you rate your overall health at the present time?’ with responses on a five-point scale (1 = excellent to 5 = poor). Highly significant correlations have been oberved between self-reports and physician ratings.21
Knowledge, behaviour and severity of symptoms related to diet and medication. The Omaha System Problem Rating Scale for Outcomes22 was used to assess patient knowledge of and adherence behaviours regarding diet and medication regimens, and severity of symptoms. Finn’s r reliabilities are 0.73, 0.74 and 0.79, respectively, for the items.23 This tool is usually administered by a home care nurse. In the present study, the research assistants used probe questions by telephone. For example, to assess dietary knowledge, patients were asked to name two foods high in sodium. The instrument provides a 5-point Likert scale with higher scores being better. During training, the inter-rater reliability was 82–86% for 10 cases.
Depression was measured with the Patient Health Questionnaire (PHQ-9).24 Patients scoring 10 or more or with thoughts of suicide prompted immediate physician notification.
Rehospitalizations and ED visits and time to first event were counted if it was for an unplanned reason related to HF or diabetes. The reason was judged as related or not by two observers who were blinded to the study group assignment. Sixty-day rehospitalization and ED use were verified using the Outcomes Assessment Data Set items M0080 and M00840 for ED use and M0855 and M0895 for hospitalizations.25 Utilization at 90 days was collected from the patient and caregivers via telephone.
Data analysis
Descriptive comparisons were performed at baseline using t-tests, one-way ANOVA and Wilcoxon rank sum tests for interval variables; and chi-square, Fisher’s exact tests, or generalized Fisher’s exact tests for categorical variables using SAS version 8.0.
Outcomes analysis
A mixed model MANOVA26,27 was used to assess the fixed effect of intervention group on each continuous dependent measure over time (e.g. depression, knowledge, behaviour, severity). The Initial model included terms for group, site, time and group by time interaction. Subsequent models assessed the effect of group controlling for either HF diagnosis and number of visits, along with the interaction by group (covariates were tested one-at-a-time because of correlation between HF diagnosis and number of visits). For discrete measures (subjective health), non-parametric analogues to ANOVA were used. A logistic regression was used to compare the groups on any related rehospitalization or ED use during the first 60 days post discharge. A final model using SAS PROC.LIFETES28 was used to assess group differences separately for HF and non-HF patients. Finally, a Cox proportional hazards model was used to compare the groups for time to first related hospital readmission and ED use.29,30 The data analysis was a modified intention to treat. Data from patients were included if they received at least one home visit, telephone call or telemonitoring contact, and at least one follow-up assessment.
Results
A total of 338 patients were enrolled of whom 303 were eligible for the modified intention to treat analysis. Of 35 patients who did not meet the modified intention to treat threshold, the reasons were: refused phone calls (n = 4), the telemonitoring unit (n = 11) or home visits (n = 3); died before intervention (n = 3); unable to reach (n = 3); too busy (n = 5); moved (n = 3); house unsuitable for telemonitoring (n = 1); and physicians wanted telemonitoring (n = 2). These subjects were not different at baseline from the study patients.
Of the 303 patients, 63% were female, the average age was 75 years and 65% had heart failure alone or heart failure with diabetes. There were 112 patients in the Control group, 93 in the Telephone group and 98 in the Telemonitoring group. Thirty-seven percent rated their health as fair and 29% as poor at baseline. The Pra scores indicated low to moderate risk for readmission (mean 0.37). Despite randomization, there were significantly more HF patients in the Telemonitoring group (84%) compared to the Control (59%) or Telephone group (54%), P < 0.001. Patients in the Control group received an average of 9 visits (range 1–35); the Telephone patients received 9 visits (range 1–36) and 4 calls (range 1–14); and the Telemonitoring patients received 11 visits (range 1–36) and provided an average of 34 data transmissions (range 1–123) (P= 0.06 for visits). At baseline, the Telemonitoring group had better ratings than the other groups for diet behaviour, and the Telephone group had better diet severity ratings than the Control or Telemonitoring groups. These differences were controlled for in the outcomes analyses.
Rehospitalization
During the first 60 days, 10% of the Control group were rehospitalized, 17% of the Telephone group and 16% of the Telemonitoring group. Both HF and the increased number of nursing visits were significantly related to having a rehospitalization during the first 60 days post discharge (P = 0.002 and P = 0.006). After adjusting for HF and number of nursing visits, the difference between the three groups was not significant (P= 0.15). The contrast comparing Telemonitoring to Control was not significant (P = 0.69), whereas the contrast for Telephone to Control showed a trend (P = 0.07), with an increased risk of rehospitalization during the first 60 days, risk ratio = 2.2 (95% CI: 0.9 to 5.2). It was not possible to test differences for non-HF patients, because there was only one failure among non-HF telemonitoring patients.
Emergency department use
During the first 60 days, 10% of the Control group used an ED, 17% of the Telephone group and 17% of the Telemonitoring group. HF was not significantly related to using the ED (P = 0.16) and nursing visits were marginally related (P = 0.09). The overall P value for differences among the three groups was not significant (P = 0.25). The contrast comparing Telemonitoring to Control was not significant (P = 0.32) and nor was Telephone to Control (P = 0.10).
Time to rehospitalization
Both HF and number of nursing visits were significantly related to time to first rehospitalization (P = 0.001 and P = 0.003, respectively). After adjusting for HF (P = 0.002) and number of nursing visits (P = 0.01), the differences between the three groups was significant (P = 0.01). The comparison of Telemonitoring to Control was not significant (P = 0.66), whereas Telephone to Control was significant (P= 0.02), with an increased risk of rehospitalization, risk ratio = 2.3 (95% CI: 1.2 to 4.6). The P value for the non-HF patients was not a reliable estimate because there was only one event in the non-HF group.
Patients with any hospitalization in the prior 12 months had a 60% increased risk of rehospitalization post discharge (P = 0.02, hazard ratio = 1.6, 95% CI: 1.1 to 2.4). However, the Cox Proportional Hazards model was not significant (P = 0.11) after adjusting for previous hospitalizations.
Time to emergency department use
The Cox Proportional Hazards model was not significant (P = 0.24) for time to ED use. The hazard ratio comparing the Telephone group to the Control group was 1.4 (95% CI: 0.7 to 2.9) with P = 0.38. Similarly, the hazard ratio comparing the Telemonitoring group to the Control group was 1.2 (95% CI 0.6 to 2.5) with P = 0.66.
Patients with a hospitalization in the prior 12 months had a 62% increased risk of ED use post discharge (p= 0.02, hazard ratio of 1.6, 95% CI: 1.1 to 2.4). However, the Cox Proportional Hazards model was not significant (P = 0.90) after adjusting for previous hospitalizations.
Subjective health status rating
There were no significant differences in health ratings between the groups from baseline to 60 or 90 days (P = 0.76). The group x time interaction was not significant (P = 0.66). There were no significant differences in health status after adjusting for site (P = 0.08), number of visits (P = 0.28) or HF diagnosis (P = 0.60).
Diet knowledge, behaviour and severity of symptoms
There was a significant interaction between diet knowledge, behaviour, severity of symptoms, nursing visits and group (P = 0.04) but post hoc contrast tests showed no significant difference among groups for low, medium or high numbers of nursing visits.
Medication knowledge, behaviour and severity of symptoms
There was a significant interaction between medication knowledge and the number of nursing visits (P = 0.02). In post hoc analyses, for patients who received 12 or more visits, there was a significant increase in knowledge for the Telemonitoring patients compared to the Telephone patients (P = 0.03). There was also a significant interaction between nursing visits and medication behaviour (P = 0.01). While the behaviour scores declined in the Control and Telephone groups, they declined significantly more in the Telephone group. Post hoc analysis showed significantly lower behaviour scores in the Telephone versus the Control group when the number of nursing visits was 12 or more (P= 0.02). There was a non-significant trend for lower scores in Telemonitoring versus Telephone when the number of nursing visits was 12 or more (P= 0.06). There were no significant effects on medication severity of symptoms.
Depression
At baseline 24% of all subjects had moderate to severe depression. There were no significant differences in depression scores between the groups at baseline or at 60 days after adjustments for HF and number of nursing visits.
Discussion
The study showed that there was no difference between the groups in the primary outcome (rehospitalization), although there was a trend toward increased hospital readmissions in the Telephone patients versus Control only. Patients were in home care for only 30–60 days so perhaps a longer intervention and monitoring period would have yielded more effect. The trend to more and earlier readmissions in the Telephone group might be explained by the additional verbal contact afforded through telephone contact. Perhaps patients reported worrying symptoms by telephone and nurses had to act on information that they would have been able to confirm (or dispute) had the contact been in person or had they had telemonitoring information available. Further study is needed to explore this phenomenon.
Given the low proportion of patients who used the ED or were rehospitalized it was not possible to detect a significant difference between disease management modalities.
In response to national quality improvement efforts, agencies have instituted many interventions to decrease readmissions making it difficult to show a difference when these events are already low due to other successful interventions such as front loading visits.31 (This means that the nurse visits most often early on in the episode when the patient is most unstable.) The national average for rehospitalization from home care is currently 29% by 60 days.32 All of the study agencies performed better than the national average. The proportion of events in the present study are also lower than the average reported by these agencies for all types of patients (24%) suggesting that the use of the disease-management protocols for patients with diabetes or H F, who generally have the highest rates, may have helped. However, confirming this would require an additional study group that did not receive the disease management protocol. The sample was also low to moderate risk for readmission based on the average Pra score of 0.37. Perhaps in a higher risk cohort the results would have been different. The study findings suggest that patients with HF are much more likely to be rehospitalized than patients with diabetes.
There were improvements in medication knowledge in the Telemonitoring group compared to Telephone as the number of visits increased. Medication knowledge may have increased in the Telemonitoring group because of the reinforcement of medical effectiveness that the patients obtained from their telehealth data. Reviewing blood pressure and bodyweight may help patients to learn the purpose and actions of their medications. However, we do not know why we did not observe the same difference between Telemonitoring and Control alone. Nurses should employ strategies to assess how much patients know by asking them to ‘teach back’ what they have been told.33 Perhaps there is a role for technology to make this teaching more interactive and memorable. There appear to be no studies of the relationship between medication knowledge and telemonitoring to date.
Medication behaviour declined in all groups but more so in the Telephone and Telemonitoring groups compared to Control, particularly in those who had more in-person visits. This may suggest a relationship between personal contact (either via telephone or in person) and behaviour related to taking medications. Perhaps having a nurse checking medication adherence either by telephone or in person has a greater effect than using telehealth monitoring devices. However, Wakefield and colleagues14 reported no difference between Telephone and Telemonitoring on medication adherence.
Although not significantly affected by the interventions, the other clinical outcomes are of interest. Two thirds of the subjects rated their health as fair or poor. Poor health ratings serve as an indicator of severity of illness and a predictor of poor outcomes.34–36 If measured routinely, subjective health rating might serve as one indication of high risk patients.
Nearly one-quarter of the study sample had moderate to severe depression. Studies in primary care have reported 4–10%.37–39 Use of the PHQ-9 with elderly people in home care revealed a rate of 10%.40 However, this rate is not directly comparable to our findings because they counted a score of 8 or more plus one of two symptoms present as major depression. Our rate was derived from those scoring 10 or more as suggested by the instrument developers.24 Rates in other home care populations were reported as 14–26% depending on the measure.41,42 Depression assessment may be an important addition to the home care database and indicate another use for telemonitoring.
The present study was limited to Medicare or Medicare/Managed Care patients with HF and/or diabetes at home care agencies with a mainly Caucasian, rural population. Forty nurses were trained to conduct the intervention and there may have been variability in the application of the Control protocols. While we monitored the number of encounters, the nurses admitted to inconsistencies in interacting with physicians to institute changes in the plan of care as directed by the protocol. It was also difficult to complete the minimum number of telephone calls or telemonitoring contacts prior to discharge. These problems affected the final sample size, the intervention exposure and the quantity of missing data.
Nurses in our study reported communication and collaboration barriers with physicians, creating difficulty in using the disease-management guidelines. They suggested that future attempts at home disease management should partner with physician groups to assure better collaboration. Jerant and colleagues assisted nurses with physician communication by sending letters for non-urgent requests or calling directly for urgent ones.15 The physicians agreed to make changes in 44% of instances. This communication barrier warrants further study to develop interventions that improve communication and collaboration.
The low hospitalization rates achieved in these agencies indicate the need to carefully target telehealth interventions to those who need it most. This study did not target high risk patients, making it more difficult to show an effect on readmission. Studies are needed that match the intensity of disease management and telemonitoring with severity of illness to produce the most effective outcomes.
Acknowledgments
We thank the nurses and administrators of the four home care agencies and the Pennsylvania Home Care Association who made the study possible. The work was supported by grant number RO1 DP000215-01 from the Centers for Disease Control and Prevention (this paper does not necessarily represent the official views of the CDC).
References
- 1.Centers for Disease Control and Prevention. Health, United States. 2007 See http://www.cdc.gov/nchs/data/hus/hus07.pdf (last checked 11 May 2009)
- 2.Merck Institute of Aging and Health. The Slate of Aging and Health in America. 2004 See http://www.cdc.gov/aging/pdf/State_of_Aging_and_Health_In_America_2004.pdf (last checked 11 May 2009)
- 3.Alliance for Aging Research. The Silver Book. See http://www.silverbook.org/fact/30 (last checked 11 May 2009)
- 4.Robert Wood Johnson Foundation. Chronic Care in America: A 21st Century Challenge. See http://www.rwjf.org/files/publications/other/ChronicCareinAmerica.pdf (Qast checked 11 May 2009)
- 5.Kapp MC. Overview: disease management. Health Care Financ Rev. 2008;30:1–3. [PMC free article] [PubMed] [Google Scholar]
- 6.Motheral BR. 2008: a tipping point for disease management? J Manag Care Pharm. 2008;14:643–9. doi: 10.18553/jmcp.2008.14.7.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mattke S, Seid M, Ma S. Evidence for the effect of disease management: is $1 billion a year a good investment? Am J Manag Care. 2007;13:670–6. [PubMed] [Google Scholar]
- 8.Hebert PL, Sisk JE, Wang JJ, et al. Cost-effectiveness of nurse-led disease management for heart failure in an ethnically diverse urban community. Ann Intern Med. 2008;149:540–8. doi: 10.7326/0003-4819-149-8-200810210-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Orr PM, Dimengo J. Outcomes from a comprehensive heart failure disease management program. J Card Fail. 2003;9 (Suppl 1):S86. [Google Scholar]
- 10.Gonseth J, Guallar-Castillón P, Banegas JR, Rodríguez-Artalejo F. The effectiveness of disease management programmes in reducing hospital re-admission in older patients with heart failure: a systematic review and meta-analysis of published reports. Eur Heart J. 2004;25:1570–95. doi: 10.1016/j.ehj.2004.04.022. [DOI] [PubMed] [Google Scholar]
- 11.Ahmed A. Quality and outcomes of heart failure care in older adults: role of multidisciplinary disease-management programs. J Am Geriatr Soc. 2002;50:1590–3. doi: 10.1046/j.1532-5415.2002.50418.x. [DOI] [PubMed] [Google Scholar]
- 12.DelliFraine JL, Dansky KH. Home-based telehealth: a review and meta-analysis. J Telemed Telecare. 2008;14:62–6. doi: 10.1258/jtt.2007.070709. [DOI] [PubMed] [Google Scholar]
- 13.Bowles KH, Baugh AC. Applying research evidence to optimize telehomecare. J Cardiovasc Nurs. 2007;22:5–15. doi: 10.1097/00005082-200701000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wakefield BJ, Holman JE, Ray A, et al. Outcomes of a home telehealth intervention for patients with heart failure. J Telemed Telecare. 2009;15:46–50. doi: 10.1258/jtt.2008.080701. [DOI] [PubMed] [Google Scholar]
- 15.Jerant AF, Azari R, Martinez C, Nesbitt TS. A randomized trial of telenursing to reduce hospitalization for heart failure: patient-centered outcomes and nursing indicators. Home Health Serv Q. 2003;22:1–20. doi: 10.1300/J027v22n01_01. [DOI] [PubMed] [Google Scholar]
- 16.Darkins A, Ryan P, Kobb R, et al. Care coordination/home telehealth: the systematic implementation of health informatics, home telehealth, and disease management to support the care of Veteran patients with chronic conditions. Telemed J E Health. 2008;14:1118–26. doi: 10.1089/tmj.2008.0021. [DOI] [PubMed] [Google Scholar]
- 17.Boult C, Dowd B, McCaffrey D, Boult L, Hernandez R, Krulewitch H. Screening elders for risk of hospital admission. J Am Geriatr Soc. 1993;41:811–7. doi: 10.1111/j.1532-5415.1993.tb06175.x. [DOI] [PubMed] [Google Scholar]
- 18.Pacala JT, Boult C, Boult L. Predictive validity of a questionnaire that identifies older persons at risk for hospital admission. J Am Geriatr Soc. 1995;43:374–7. doi: 10.1111/j.1532-5415.1995.tb05810.x. [DOI] [PubMed] [Google Scholar]
- 19.Pacala JT, Boult C, Reed RL, Aliberti E. Predictive validity of the Pra instrument among older recipients of managed care. J Am Geriatr Soc. 1997;45:614–7. doi: 10.1111/j.1532-5415.1997.tb03097.x. [DOI] [PubMed] [Google Scholar]
- 20.Boult L, Boult C, Pirie P, Pacala JT. Test-retest reliability of a questionnaire that identifies elders at risk for hospital admission. J Am Geriatr Soc. 1994;42:707–11. doi: 10.1111/j.1532-5415.1994.tb06528.x. [DOI] [PubMed] [Google Scholar]
- 21.Maddox GL, Douglass EB. Self-assessment of health: a longitudinal study of elderly subjects. J Health Soc Behav. 1973;14:87–93. [PubMed] [Google Scholar]
- 22.Martin KS. The Omaha System: A Key to Practice, Documentation, and Information Management. St Louis, MO: Elsevier; 2005. [Google Scholar]
- 23.Finn RH. A note on estimating the reliability of categorical data. Educ Psychol Meas. 1970;30:71–6. [Google Scholar]
- 24.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Medicare and Medicaid Services. OASIS Data Set. See http://www.cms.hhs.gov/OASIS/046_DataSet.asp#TopOfPage (last checked 11 May 2009}
- 26.Westfall PH, Tobias RD. Multiple Comparisons and Multiple Tests Using the SAS System. Cary, NC: SAS Institute Inc; 1999. [Google Scholar]
- 27.Littell RC, Milliken GA, Stroup WW, Wolfinger RD. SAS System for Mixed Models. Cary, NC: SAS Institute Inc; 1996. [Google Scholar]
- 28.Singer JD. Using SAS PROC MIXED to fit multilevel models, hierarchical models, and individual growth models. Journal of Educational and Behavioral Statistics. 1998;23:323–55. [Google Scholar]
- 29.Cox DR. Regression models and life-tables. J Roy Stat Soc B. 1972;34:187–220. [Google Scholar]
- 30.Allison PD. Survival Analysis Using SAS: A Practical Guide. Cary, NC: SAS Institute Inc; 1995. [Google Scholar]
- 31.Rogers JM, Schott DK. Front loading visits: a best practice measure to decrease rehospitalization in heart failure patients. Home Health Care Management and Practice. 2008;20:147–53. [Google Scholar]
- 32.Centers for Medicare and Medicaid Services. Home Health Compare. See http://www.medicare.gov/HHCompare/Home.asp?version=default&browser=IE%7C6%7CWinXP&language=English&pagelist=Home&CookiesEnabledStatus=True&dest=NAV|Home|Searc (last checked 11 May 2009)
- 33.Schillinger D, Piette J, Grumbach K, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003;163:83–90. doi: 10.1001/archinte.163.1.83. [DOI] [PubMed] [Google Scholar]
- 34.Lyyra TM, Heikkinen E, Lyyra AL, Jylhä M. Self rated health and mortality: could clinical and performance-based measures of health and functioning explain the association? Arch Gerontol Geriat. 2006;42:277–88. doi: 10.1016/j.archger.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 35.Walker JD, Maxwell CJ, Hogan DB, Ebly EM. Does self-rated health predict survival in older persons with cognitive impairment? J Am Geriatr Soc. 2004;52:1895–900. doi: 10.1111/j.1532-5415.2004.52515.x. [DOI] [PubMed] [Google Scholar]
- 36.Ruo B, Bertenthal D, Sen S, Bittner V, Ireland CC, Hlatky MA. Self-rated health among women with coronary disease: depression is as important as recent cardiovascular health. Am Heart J. 2006;152:921.e1–e7. doi: 10.1016/j.ahj.2006.01.012. [DOI] [PubMed] [Google Scholar]
- 37.AHCPR Archived Clinical Practice Guidelines. Depression in Primary Care: Detection and Diagnosis. See http://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=hstat6.chapter.14485 (last checked 11 May 2009)
- 38.Katon W. The epidemiology of depression in medical care. Int J Psychiatry Med. 1987;17:93–112. doi: 10.2190/xe8w-glcj-kem6-39fh. [DOI] [PubMed] [Google Scholar]
- 39.Williams JW, Kerber CA, Mulrow CD, Medina A, Aguilar C. Depressive disorders in primary care: prevalence, functional disability and identification. J Gen Intern Med. 1995;10:7–12. doi: 10.1007/BF02599568. [DOI] [PubMed] [Google Scholar]
- 40.Ell K, Unützer J, Aranda M, Sanchez K, Lee PJ. Routine PHQ-9 depression screening in home health care: depression, prevalence, clinical and treatment characteristics and screening implementation. Home Health Care Serv Q. 2005;24:1–19. doi: 10.1300/J027v24n04_01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bruce ML, McAvay GJ, Raue PJ, et al. Major depression in elderly home health care patients. Am J Psychiatry. 2002;159:1367–74. doi: 10.1176/appi.ajp.159.8.1367. [DOI] [PubMed] [Google Scholar]
- 42.Banerjee S, Macdonald A. Mental disorder in an elderly home care population: associations with health and social service use. Brit J Psychiatry. 1996;168:750–6. doi: 10.1192/bjp.168.6.750. [DOI] [PubMed] [Google Scholar]