Abstract
Relapse rates for children and adolescents with major depressive disorder (MDD) range from 30% to 40% within 1 to 2 years after acute treatment. Although relapse rates are high, there have been relatively few studies on the prevention of relapse in youth. While acute phase pharmacotherapy has been shown to reduce symptoms rapidly in depressed youth, children and adolescents frequently report ongoing residual symptoms and often relapse following acute treatment. Recent adult trials have begun examining augmentation with psychosocial treatment after successful medication treatment to enhance medication response and prevent future relapse. This strategy has not yet been examined in youth with depression. Here we present initial efforts to develop a sequential, combination treatment strategy to promoting rapid remission and to prevent relapse in depressed youth. We describe efforts to adapt CBT to prevent relapse (RP-CBT) in youth who respond to pharmacotherapy. The goals of RP-CBT include: preventing relapse, increasing wellness, and developing skills to promote and sustain a healthy emotional lifestyle. We describe the rationale for, components of, and methods used to develop RP-CBT. The results from a small open series sample demonstrate feasibility and indicate that youth appear to tolerate RP-CBT well. A future test of the treatment in a randomized controlled trial is described.
Advances in the development of treatments for depressed youth include effective antidepressant medications (Emslie et al., 1997; Emslie et al., 2004; TADS Team, 2004) and psychosocial treatments such as interpersonal therapy (IPT) and cognitive behavioral therapy (CBT; Compton et al., 2004; Mufson, Weissman, Moreau, & Garfinkel, 1999; Weisz, McCarty, & Valeri, 2006). Most of the literature focuses on the acute phase of treatment, which is aimed at reducing depressive symptoms. Clinicians, youth, and parents need treatments that not only maintain the gains achieved in the early stages of treatment, but also prevent relapse. CBT appears to be effective in preventing relapse in adults (Fava, Rafanelli, Cazzaro, Conti, & Grandi, 1998) and may offer this promise in youth with depression as well. Here we describe Relapse Prevention CBT (RP-CBT; Kennard, 2006): its development, components, and feasibility outcomes. Our initial efforts focus on using RP-CBT to reduce residual symptoms and prevent relapse in youth with major depressive disorder (MDD) who have previously responded to acute phase pharmacotherapy.
What Are the Most Effective Treatment Strategies for Youth With Depression?
Efficacy in randomized clinical trials of pediatric depression has typically been defined as an adequate treatment response or clinical improvement. Typically, response is defined as improvement on a clinical rating scale. However, more recently, particularly in the treatment literature on adult depression, remission or symptom-free status is the desired outcome (Rush & Trivedi, 1995). These definitions are important, as evidenced by the Treatment for Adolescents With Depression Study (TADS), which had dramatically different outcomes, based on whether the outcome was defined as loss of MDD diagnosis, response, or remission (Kennard, Silva, et al., 2006; TADS Team, 2004). Although acute efficacy trials in youth have demonstrated positive response, particularly with fluoxetine, remission rates remain low, and many youth continue to experience residual symptoms of depression (Kennard, Silva, et al., 2006). Rates of sustained remission, or continuation phase recovery, have not been reported in pediatric depression to date. A recent ACNP task force recommended that recovery be defined as the achievement of remission that is sustained by a well period of at least 4 months (Rush et al., 2006).
Remission rates in antidepressant trials, based on achieving a Children’s Depression Rating Scale–Revised (CDRS-R; Poznanski & Mokros, 1996) ≤ 28, range from 31% to 41% for active treatments (Emslie et al., 1997, 2002; Wagner et al., 2004). While CBT treatment studies rarely report on remission rates, Brent and colleagues report a remission rate of 64.7%, defined as absence of MDD on the Schedule for Affective Disorders and Schizophrenia for School-Aged Children–Present and Lifetime Version (K-SADS-PL; Kaufman et al., 1997) and three consecutive weekly scores on the Beck Depression Inventory–II (BDI-II; Beck, Steer, and Brown, 1996) < 9 (Brent et al., 1997). More common in psychotherapy studies is the use of diagnostic criteria to measure treatment outcome. Half of the published randomized controlled trials evaluating the efficacy of CBT in child and adolescents report on the percentage of subjects who no longer meet criteria for MDD after treatment (Compton et al., 2004), ranging from 47.6% to 87% (Clarke, Rohde, Lewinsohn, Hops, & Seeley, 1999; Lewinsohn, Clarke, Hops, & Andrews, 1990; Vostanis, Feehan, Grattan, & Bickerton, 1996; Wood, Harrington, & Moore, 1996). Although some studies have shown high response rates in subjects, remission is a more stringent standard and thus more difficult to meet. Even the group receiving a combination of fluoxetine and CBT in the TADS study had a relatively low remission rate (37%; Kennard, Silva, et al., 2006).
While combination treatment (antidepressant treatment with fluoxetine and CBT delivered concurrently) is an effective strategy for acute phase treatment for adolescents with MDD (TADS Team, 2004), fluoxetine alone was also effective in achieving response. Furthermore, time to response is shorter for fluoxetine than for CBT, supporting this as a good acute phase strategy (Kratochvil et al., 2006). CBT alone is also effective, as efficacy studies of acute treatment with CBT suggest that it reduces depressive symptoms in both children and adolescents (Compton et al., 2004; Curry, 2001; Reinecke, Ryan, & DuBois, 1998; Sherrill & Kovacs, 2004). In fact, recent findings suggest that by 18 to 24 weeks of treatment, fluoxetine and CBT have similar positive outcomes (TADS Team, 2007). While both fluoxetine and CBT are effective treatments, the speed of response favors fluoxetine as an acute treatment strategy in adolescent depression.
What Is Known About Relapse in Youth With Depression?
Relapse rates for children and adolescents with MDD are significant. Estimates range from 34% to 75% within 1 to 5 years after the index episode (Kennard, Emslie, Mayes, & Hughes, 2006). Much of what is known about relapse in this population is based on naturalistic follow-up studies. The comparison of these studies is complicated by the variable follow-up intervals and types of treatments received during the naturalistic follow-up, resulting in relapse rates that are difficult to interpret. In addition, the terms relapse and recurrence are often used interchangeably and variably defined, contributing to the confusion in the literature. For this paper, relapse is defined as the return of the index episode within 2 months after remission (Frank et al., 1991). Typically the treatment of depression can be divided into three phases: acute (treatment that results in clinical response and remission of symptoms), continuation (treatment to prevent relapse of symptoms of the index episode), and maintenance (treatment to prevent new episodes, or recurrences; Frank et al., 1991; Kupfer, 1991; Rush et al., 2006). Our goal in continuation phase CBT is to prevent relapse and promote recovery.
Risk for Relapse
Early age of onset in adults with depression is associated with a greater vulnerability for future episodes (Jarrett et al., 2001). In addition, a significant risk factor for relapse in adults with depression is the presence of residual symptoms at the end of acute treatment (Cornwall & Scott, 1997; Keller, 2004; Judd et al., 1998; Paykel et al., 1995). This is true for both pharmacotherapy trials (Judd et al., 1998; Faravelli, Ambonetti, Pallanti, & Pazzagli, 1986; Fava, Grandi, Zielezny, Canestrari, & Morphy, 1994; Paykel et al., 1999) and CBT trials (Simons, Murphy, Levine, & Wetzel, 1986; Thase et al., 1992). While the relationship between residual symptoms and relapse has not been studied in child and adolescent populations, the presence of residual symptoms is common in adolescents who have been successfully treated for depression and may be related to poor treatment outcomes (Kennard, 2007; Kennard, Silva, et al., 2006).
Prevention of Relapse
In adults with depression, CBT was found to be an effective strategy to prevent relapse (Hollon et al., 2002; Vittengl, Clark, Dunn, & Jarrett, 2007). Furthermore, the use of continuation phase CBT as an augmentation strategy to pharmacotherapy was effective in reducing risk for relapse in adults treated for major depression (Fava et al., 1994; Fava, Fabbri, & Sonino, 2002; Fava, Grandi, Zielezny, Rafanelli, & Canestrari, 1996; Fava, Rafanelli, Grandi, Canestrari, & Morphy, 1998; Nierenberg, 2001; Paykel et al., 1999; Teasdale et al., 2000). Furthermore, Jarrett and colleagues developed a continuation phase CBT (Jarrett & Kraft, 1997; Jarrett, Vittengl, & Clark, in press) that lowered relapse rates in responders to acute phase CBT (Jarrett et al., 2001).
Considerably less is known about continuation and maintenance phase treatments in pediatric depression. A preliminary study of continuation phase treatment with fluoxetine found that 34% of those children and adolescents who continued on fluoxetine relapsed compared to 60% of those who were placed on placebo (Emslie et al., 2004). In the psychotherapy literature, there are only two reports investigating CBT continuation phase treatments in youth. In a pilot study, Kroll, Harrington, Jayson, Fraser, and Gowers (1996) found that 6 months of continuation phase CBT following acute phase CBT significantly lowered relapse rates compared to historical controls (6% vs. 50%). Clarke et al. (1999) reported that booster sessions did not reduce relapse rates, but did accelerate remission in patients with depression at the end of acute phase CBT. The relatively low number of booster sessions, along with poor attendance rates of these sessions, may account for the significant relapse rates.
TAILORING AND DEVELOPING CONTINUATION PHASE CBT TO PREVENT RELAPSE IN YOUTH
It is important to advance questions of which treatments are most effective (i.e., pharmacotherapy, psychosocial treatments, and combined treatments) for youth with depression and for specific subpopulations (Compton et al., 2004). It is also vital to investigate the timing of interventions to optimize their impact on depression (Weisz et al., 2006). When conceptualizing RP-CBT, we based our strategy on what has been found to be effective in the acute and continuation treatment phases in both the pediatric and adult literature to date. Acute phase pharmacotherapy (i.e., fluoxetine) is an efficacious intervention in treating pediatric depression (Emslie et al., 1997; Emslie et al., 2004; TADS Team, 2004). Additionally, fluoxetine demonstrates an accelerated time to response relative to CBT (Kratochvil et al., 2006). Continuation phase CBT has shown efficacy in reducing residual symptoms and preventing relapse in adults (Fava et al., 1996; Jarrett et al., 2001; Paykel et al., 1995; Teasdale et al., 2000). To date there have been no published reports of a CBT for depressed youth specifically developed to be delivered in the continuation phase of treatment. We hypothesized that using pharmacotherapy and CBT sequentially would effectively prevent relapse and promote recovery in children and adolescents with depression.
Rounsaville, Carroll, and Onken (2001) have suggested a stage model for the development and testing of novel behavioral interventions. In this framework, Stage I consists of manual writing, feasibility testing, and piloting of outcome measures. In Stage II, randomized clinical trials to test the efficacy of the manualized intervention are conducted. Finally, Stage III involves studies that evaluate the generalizability and transportability of treatments. In this manuscript we will present the process and preliminary findings in the Stage I of the treatment development of a relapse prevention treatment for depressed youth.
Stage Ia. Therapy Development/Manual Writing
Our goal was to develop a treatment manual for a CBT that targets relapse prevention in youth with depression. To this end, we began by reviewing available treatment literature and manuals of acute and continuation CBT interventions (Brent, Bridge, & Bonner, 2000; Brent & Poling, 1997; Clarke et al., 1999; Curry et al., 2000; Fava, Rafanelli, Cazzaro, et al., 1998; Jarrett & Kraft, 1997; Stark, 2005; Wilkes, Belsher, Rush, & Frank, 1994). We also explored more novel therapeutic approaches to relapse prevention, focusing on mindfulness and techniques from the positive psychology literature (Segal, Williams, & Teasdale, 2002; Seligman & Csikszentmihalyi, 2000; Snyder & Lopez, 2005). In adult populations, well-being therapy, which included positive psychology components, was found to be effective in reducing relapse rates (Fava, Rafanelli, Cazzaro, et al., 1998). We sought out and received consultation on our preliminary ideas from experts in childhood depression, CBT, and relapse prevention.
First and foremost we wanted the treatment to be both feasible to deliver and acceptable to patients and their families. To this end, we conducted focus interviews with current patients in clinical trials of pediatric depression. We asked the following questions: Would patients accept continuation phase CBT when pharmacotherapy had already provided relief from depressive symptoms? Would families and patients be reluctant to add another treatment modality and possibly more treatment visits after completing a 3-month trial of medication therapy? Was added CBT too burdensome or perceived as unnecessary? What expectations and requirements might patients and families have for a continuation treatment?
We conducted a short semistructured interview with six patients and families. All families were positive about the treatment and indicated that they would participate in such a program were it offered. Major concerns expressed included time commitment, or worry about missing school and work to participate in therapy sessions, and worry that the adolescent would have little incentive for further treatment. Parents stated they wanted to participate because of concern that the medication alone would not be enough to prevent relapse. As a result, the intervention was designed to be short in duration with more frequent sessions early in the treatment and more time between sessions as treatment progressed.
Following the focus interviews, the manual was revised to take into consideration the concerns of patients and families. Iterative revisions to the manual were planned based on experiences from open series cases and participants in the pilot study. In addition, several experts in child and adolescent CBT reviewed the manual and revisions were made based on their feedback and suggestions.
The Treatment: RP-CBT
RP-CBT is a brief (8 to 11 session), individual treatment that targets the prevention of relapse of depression after a response to pharmacotherapy. The RP-CBT is designed to be less intensive than acute phase CBT treatments for adolescents, which are typically 12 to 16 weekly sessions (Brent et al., 1997; Compton et al., 2004; TADS Team, 2004). In addition, it is comparable in length to continuation phase CBT used in remitted adults who were treated in the acute phase with antidepressant medication (10 sessions; Fava, Rafanelli, Cazzaro, et al., 1998). However, in Fava and colleague’s study, the sessions were only 30 minutes in duration and biweekly, which is more appropriate for an adult population. In treatment with youth, more time is needed for the teaching and practicing of skills and to include family sessions.
The treatment is designed to be flexibly delivered so that the therapist can tailor the treatment to the specific needs of the child. The RP-CBT skills target factors that have been found to be effective in the treatment of depression (Kazdin & Weisz, 1998). These skills, which include cognitive and behavioral components, were selected based on previous empirical research as well as the theoretical rationale that they would effectively address residual symptoms of depression.
The treatment was designed to address risk factors for relapse. While few studies have investigated relapse in youth, high expressed emotion and family conflict and disagreement have been found to be associated with relapse in children and adolescents (Asarnow, Goldstein, Tompson, & Guthrie, 1993; Birmaher et al., 2000). In addition, certain cognitive factors, such as negative attributional style and cognitive reactivity, have been linked to recurrence of depression (Hammen, 1992; Teasdale et al., 2001). Children who have had a depressive episode are at risk for reactivating negative schemas and negative attributions in the face of stress or change (positive or negative; Curry & Craighead, 1990). Therefore, the treatment is developed to counteract these negative schemas and attributions when the individual is faced both with positive outcomes as well as stress (Jaycox, Reivich, Gillham, & Seligman, 1994; Seligman, Schulman, DeRubeis, & Hollon, 1999;). Common residual symptoms in adolescents treated for depression include sleep and mood disturbance, fatigue, and concentration (Kennard, Silva, et al., 2006). Treatment components that address these residual symptoms are included in the manual as well as family interventions selected for the prevention of factors related to relapse (e.g., expressed emotion).
Structure of RP-CBT
RP-CBT includes eight scheduled sessions, with three optional booster sessions. The treatment is scheduled weekly for 4 weeks (four sessions), biweekly for 2 months (four sessions), and monthly for booster sessions (three possible sessions) for a total of 6 months of continuation phase treatment. Several components are common to each session. Parents are provided with a handout on the skills to be presented in the session. Early in each session, the therapist sets an agenda and elicits the patient’s concerns (i.e., items for the agenda). The therapist and patient review self-reports, content from the previous session, and homework and any adherence problems that occurred.
In each session, a skill is presented and related to the time line (see below). The therapist and patient identify attributions (explanatory style) for positive events, with the aim of building positive self-schema and an optimistic explanatory style (Curry & Craighead, 1990). As mood and activation improve with the reduction of depressive symptoms, it is hypothesized that teens will have more access to positive events. Questioning external and unstable attributions and promoting internal, stable explanations for such positive events may aid in relapse prevention. Finally, the therapist and patient collaborate on homework and an intersession reminder (e.g., “Make It Stick” Post-it note or postcard).
Case conceptualization in RP-CBT
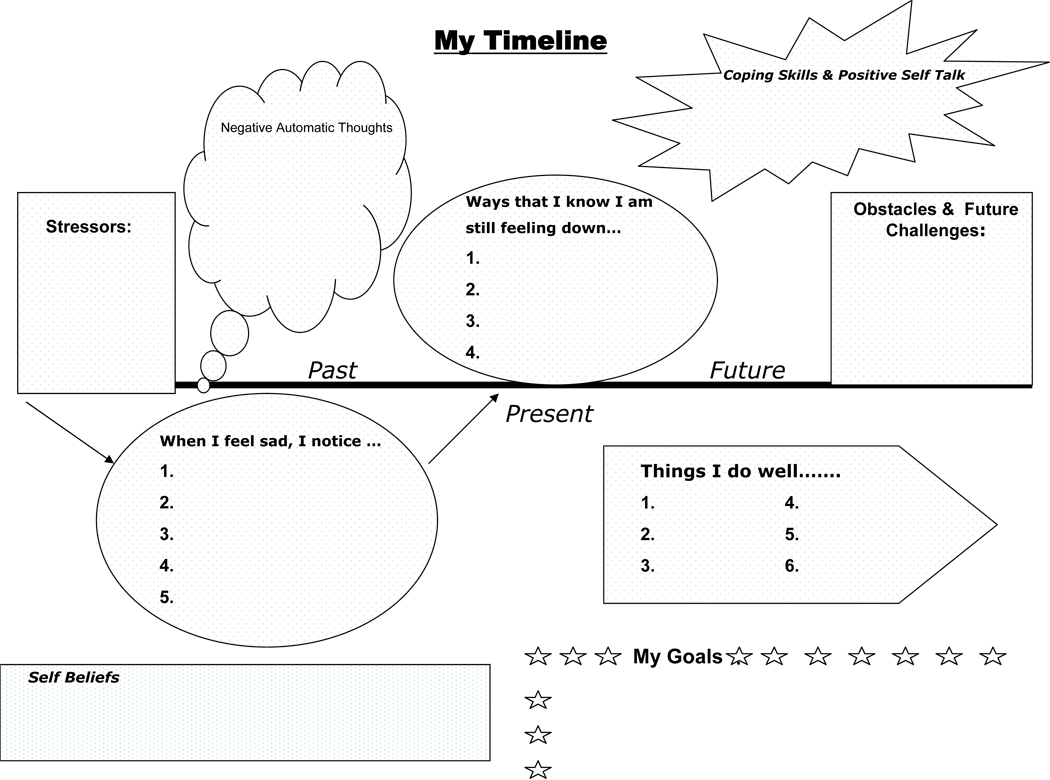
The time line worksheet for RP-CBT provides a collaboratively determined representation of the patient’s “story” of his/her depression. The time line (see Figure 1) serves as the basis for treatment planning. The components of the timeline include past symptoms, present or residual symptoms, and future obstacles. These factors, along with positive and negative thoughts, patient strengths, and goals, provide the therapist with targets for intervention as well as areas to increase or build on. The time line worksheet is typically used and referenced in each session. The therapist and patient add to the time line what is learned in treatment. As skills are identified that are useful in managing residual symptoms or increasing wellness, they are added to the time line. The patient and therapist add new skills, strengths, and thoughts identified (either positive or negative) in each session.
Figure 1.
Core CBT skills
As these patients are naïve to CBT, the first session of RP-CBT focuses on rapport building, understanding the child’s past depression and current residual symptoms (building the time line), and their goals for treatment. In addition, psychoeducation about relapse and the CBT model is completed. An introduction on mood monitoring occurs in the first session. In the subsequent early sessions (Sessions 2–4), core skills are introduced and tailored to the patient’s residual symptoms, clinical issues, and goals. These core skills include behavioral coping skills (Stark, Reynolds, & Kaslow, 1987), negative automatic thoughts and cognitive restructuring (Brent et al., 1997), and problem solving (Butler, Meitzitis, Friedman, & Cole, 1980; Stark et al., 1987). The treatment emphasizes the practice of core skills and application of these skills to individual issues in order to reinforce the skills and to increase their relevance to the patient. Additional skill modules, including emotional regulation, social skills, assertiveness training, and relaxation training, are included to assist the therapist in applying the core skills to these common issues encountered by patients. Finally, there is a section for the therapist on supplemental applications, with suggested strategies for addressing common residual symptoms including boredom, anxiety, self-esteem issues, impulsivity, irritability, hopelessness, interpersonal conflict, and adherence. Guidelines for managing suicidality are included in the treatment manual.
Brief family component
The first two sessions of RP-CBT include a conjoint component (patient and parents) for psychoeducation on relapse and the CBT model and a program overview. Each session includes a parent check-in, where the therapist may elicit input on the patient’s progress. All families also participate in a conjoint session on expressed emotion, which was found to be related to relapse in adults (Asarnow et al., 1993). Families also take part in a session on family wellness. In addition, a conjoint session on family attributions may be offered as needed.
Wellness component of RP-CBT
Ryff and Singer (1996) provide a model for defining dimensions of wellness in adults, which was later adapted to intervention strategies for relapse prevention in adults remitted for depression (Fava, Rafanelli, Cazzaro, et al., 1998). Seligman and the movement of positive psychology emphasize the need for practitioners to focus more attention on amplifying strengths and building positive traits (e.g., optimism) as a means of preventing illness (Seligman & Csikszentmihalyi, 2000; Seligman et al., 1999). In the treatment, the therapist introduces wellness as a continuum, or a range where degrees of wellness can fluctuate over time. The idea is that an individual can be “more well” or “less well,” and that it is not an all-or-nothing concept. The wellness aspect of the RP treatment was adapted from the work of Ryff and Singer (1996) and focuses on six general areas of wellness: self-acceptance, social, success, self-goals, spiritual, and soothing. The area of self-acceptance includes a focus on positive self-schemas and a helpful explanatory style. Social wellness includes social skills and social problem solving. The domain of success includes autonomy and mastery, while the self-goals component includes a sense of purpose. The idea of spiritual wellness encompasses optimism, gratitude, and altruism. Finally, the soothing area includes relaxation activities. Earlier in treatment, patients are encouraged to collect data on their own wellness skills, using a wellness log designed for RP-CBT. The therapist can use this information to assess for existing strengths, as well as for an idea of areas to improve. The wellness aspect of the treatment results in the development of an individualized wellness plan for the patient.
Relapse prevention and wellness plan
The culmination of RP-CBT is the development of a relapse prevention and wellness plan. At this point, the therapist and patient have completed the time line, and this time line includes several skills that the patient has learned to use. The major goal is to consolidate the relapse prevention plan that has been developed throughout the therapy with the wellness plan, which aims to help the patient maintain continued optimal quality of life.
End of treatment
The three booster sessions are optional at the end of RP-CBT. These may be used based on clinical need, with the central goal of assessing the effectiveness of the relapse prevention and wellness plan. Prior to the end of treatment, the therapist consults with the patient and family about the use of these boosters, including a collaborative discussion regarding the signs and symptoms of relapse for the patient. The therapist, patient, and family work together to identify when to seek additional support and the appropriate level of care.
Stage Ib. Piloting the Intervention
Six patients (ages 11 to 18, average age = 14.5; 3 males and 3 females) participated in the open series of RP-CBT. All patients were referred by local psychiatrists, who were asked to refer treatment responders to antidepressant medication, for participation in a feasibility test of the initial draft of RP-CBT. Patients were selected based on clinical determination of an adequate response to outpatient treatment. Other considerations in patient selection included age and gender, as the authors wanted to test the manual with a varied patient population. The therapists kept records of each patient’s course of therapy, including weekly session content (i.e., agenda items and skills taught) and number of sessions. The RP-CBT group met weekly in treatment development meetings to discuss our experiences with these patients. This group consisted of senior doctoral-level clinical psychologists (BDK and SMS), a postdoctoral fellow, a master’s-level therapist, and three graduate students (JLH). These treatment development meetings served both to coordinate the clinical care of these patients and to document and integrate the therapists’ experiences using the treatment.
In the open treatment series, all but one patient was on antidepressant medication (one patient had been prescribed medication but was not longer taking it). Patients were not receiving other psychosocial treatments outside of the study treatment. The average number of sessions utilized was 8.6 (ranging from 6 to 14). The CBT strategies used most frequently included cognitive restructuring, behavioral activation, and problem solving. An early concern of investigators was whether patients would be willing to increase visit frequency after remission of symptoms. However, session attendance and participation was not problematic in the open series cases. A second major concern of investigators was whether patients would develop sufficient rapport with the therapist, given the short duration of treatment. Patients and families reported satisfaction with both the therapist and the level of intervention. Our preliminary outcomes include a decrease in patient self-reported depressive symptoms (pretreatment BDI average = 10.83; posttreatment BDI average = 2.0). In addition, we found high ratings of consumer satisfaction on the Client Satisfaction Questionnaire–8 (CSQ-8; Nguyen, Attkisson, & Stegner, 1983), which has a range of 1 to 4, with 4 representing high satisfaction (posttreatment Client Satisfaction Questionnaire—child average = 3.5; posttreatment Client Satisfaction Questionnaire—parent average = 3.8).
After completing the open series cases, we finished the first full version of the RP-CBT manual. Specific early challenges in conceptualizing this treatment included differentiating the treatment from acute phase treatments including acute phase CBT, engaging the “well” patient, using a short-term intervention model in CBT naïve patients, moving from a model of psychopathology to a health and wellness model, adapting the treatment for a wide range of developmental levels, and finding appropriate outcome measures to utilize with treatment responders.
Specific Challenges in Designing RP-CBT
Engaging the young treatment responder
As with any treatment of depressed youth, the challenge of engagement and rapport is common. As we designed RP-CBT to be used as sequential treatment strategy with responders, we anticipated that the patient would be less motivated for continuation treatment. In addition, we wondered if some patients and families would be reluctant to engage in a psychosocial treatment given a positive response to medication. It is possible that patients would have difficulty switching from a medical explanatory model to one in which the focus is on behavioral and cognitive strategies to manage mood.
To address this, we present a comprehensive rationale for the continuation treatment to the patient, including specifically that CBT has shown to be effective in relapse prevention. This rationale included education about relapse and an introduction of the skills that manage mood and promote wellness. In addition, we designed the treatment to focus on the patient’s residual symptoms, goals, and any current issues causing distress. The treatment included developmentally appealing worksheets, visual aids and graphs, and acronyms to facilitate engagement and participation. Finally, the therapists encouraged relevant practice of skills in each session.
Generalizing the skills from a brief intervention
It was important to limit the number of sessions due to patients’ and families’ concerns about the burden of additional visits. The challenge in developing the treatment was to introduce the CBT treatment model and to teach basic skills of managing mood in a brief, short-term treatment. To address this issue, the treatment stressed a considerable emphasis on practice between sessions. Additionally, we relied on the use of reminders (e.g., weekly postcards), which included session content, homework assignments, and weekly goals. Finally, we provided parents with handouts, which presented the skills that the child was learning in each session. Our goal was to facilitate the parents’ participation in the treatment. The handouts also aided in the generalization of these skills to real-life situations for the child and family outside of the session, as the parent can act as a “coach.”
Adopting a wellness approach
In the RP-CBT treatment, we decided to use a model that was not solely focused on psychopathology, but also on wellness and interventions from the positive psychology literature. We hypothesized that strategies from positive psychology that improve mood above the neutral level might serve a protective function against relapse. Thus, in this treatment we conceptualized the patient’s level of functioning not just from a deficit model (i.e., decreasing negative mood and cognitions), but also from a positive approach (enhancement of strengths, positive experiences, mood and cognitions).
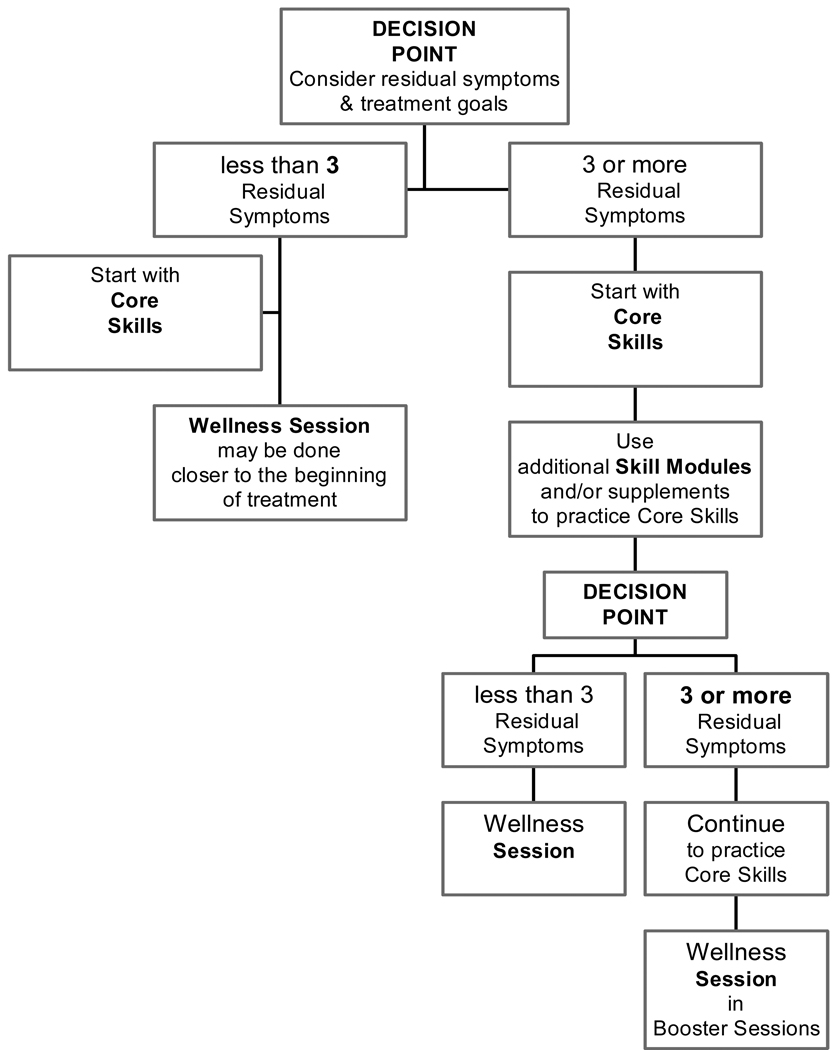
In the treatment manual, we included an algorithm to help the therapist decide when to introduce wellness skills versus skills that address residual depressive symptoms (see Figure 2). The algorithm is based on the number of residual symptoms at the beginning of RP-CBT. All patients begin the treatment with the introduction and application of core skills to target residual symptoms. In those with fewer residual symptoms, wellness and healthy lifestyle strategies are introduced earlier in treatment. In summary, the treatment is driven by the goal to achieve the absence of illness and also the presence of wellness.
Figure 2.
Decision Tree for RP-CBT Treatment Planning
Developmental considerations
Any treatment for youth must take into account the wide range of developmental levels represented. In RP-CBT, strategies were included that could be adapted for different age and developmental ranges (e.g., younger vs. older). For example, in introducing mood management to the younger child we use a more behavioral approach, such as measuring mood before and after doing a fun activity in the session. With an older child, we might practice mood management by recalling a recent event and the associated thoughts and feelings. The child practices different ways to think about the event, while attending to the relationship between thoughts and mood. Thus, for each intervention we identified techniques for both older and younger children that would facilitate skill assimilation.
Outcome measurement
Measuring outcomes for maintenance of gains from earlier treatment and continued improvement after response proved to be problematic. Patients entering the open series already had low self-reported depressive symptom ratings, making significant changes in these measures less likely at the end of treatment. This led to the investigation of better instruments to document residual symptoms, clinical issues not documented on depressive symptom scales (e.g., conflict with family members, interpersonal issues, homework problems), and wellness gains.
Therefore, in the ongoing RCT study we capture residual symptoms and clinical issues through measures such as the time line (see below) and the Children’s Hassles Scale (CHS; Varni et al., 1996). The CHS is a 43-item questionnaire that assesses the occurrence and severity of daily hassles. Four scores can be computed: (1) total number of events that occurred; (2) number of neutral events that occurred (i.e., event occurred but did not bother child); (3) number of negative events that occurred; and (4) sum of the negative events' rating of bother (possible range = 1 to 86, with higher scores indicating greater number and severity of hassles). The CHS has demonstrated acceptable construct and convergent validity and internal consistency reliability (Varni, Rubenfeld, Talbot, & Setoguchi, 1989; Varni, Setoguchi, Rappaport, & Talbot, 1991; Zuckerman, Oliver, Hollingsworth, & Austrin, 1986). The CHS would allow us to track the child’s ability to cope with the daily challenges, as research has shown that psychosocial stressors are associated with relapse and poorer outcomes (Lewinsohn, Rhode, Seeley, Klein, & Gotlib, 2000). In addition, more measures relating to positive psychology have been included, such as the Multidimensional Students’ Life Satisfaction Scale (Huebner, 1994). The MSLSS (Huebner, 1994) is a 40-item self-report scale designed to measure life satisfaction in youth. Life satisfaction is related to wellness. The MSLSS test-retest reliability is reported in the .70 to .90 ranges, and it has demonstrated acceptably validity, with moderate correlations with other measures of self-concept and life satisfaction (Gilman, Huebner, & Laughlin, 2000; Huebner, 2001).
RP-CBT Case Illustration
Jason was a 14-year-old Caucasian male who presented with his first episode of MDD to the research clinic. Jason, a freshman in high school, lived with his mother, father, and 11-year-old sister. His depressive symptoms at baseline (assessed by the K-SADS-PL; Kaufman et al., 1997) included depressed mood, irritability and anger, anhedonia, lack of interest in activities, sleep disturbance (hypersomnia), fatigue, tiredness, psychomotor disturbance (retardation), and feelings of guilt/worthlessness. In addition, he reported conflict with his father, academic problems (incomplete homework, poor grades), and high levels of family conflict at home. His baseline depression severity, as assessed by a clinician rating scale (CDRS-R; Poznanski & Mokros, 1996), was 69, indicating severe depressed mood. In addition, his self-reported depression severity score was 21, suggesting moderate depressive symptomatology (BDI; Beck et al., 1996).
In the acute phase of treatment (12 weeks), Jason received open treatment with fluoxetine (30 mg/day). He entered the continuation phase of treatment in remission (CDRS-R= 17; BDI = 2). Jason was randomized to medication management and RP-CBT. His residual symptoms at randomization were reassessed, with only weight and appetite problems remaining on the K-SADS-PL. However, when completing the CHS and the time line with the therapist, Jason also reported struggling with interpersonal issues and parent conflict (feeling criticized by parents).
Sessions 1–4
Treatment began by discussing Jason’s ideas and concerns about beginning a continuation phase treatment, especially given his low level of residual symptoms. Jason was very receptive to the treatment as he was eager to work on relationship issues at home and at school. The completion of the time line was helpful in identifying past symptoms of concern, explained as important to monitor to prevent relapse, as well as current issues that were continuing to cause distress. Future obstacles were identified as well as goals for treatment. Psychoeducation on relapse prevention and the CBT model (relationship between mood and thoughts and behaviors) was provided to Jason and his family. The family was given a handout to further educate them about relapse prevention and CBT. Jason was asked to monitor his mood, thinking, and behaviors between the first and second sessions.
Over the next three sessions, the therapist introduced the core skills: behavioral coping skills (behavioral activation), automatic thoughts and cognitive distortions, and problem solving. These skills were linked to the session agenda items in order to focus on practical application of strategies to real-life situations. Specifically, Jason was able to identify several recurring negative automatic thoughts (e.g., “She’d rather be with friends than with me” in response to his girlfriend’s frequent social activities). Jason learned to be alert to overpersonalizing in social situations and to use more adaptive thinking. One metaphor that resonated with Jason was that of “replacing the tape,” that is using the more adaptive thought of “This is not about me; my girlfriend is very social.” The time line was also helpful in identifying Jason’s past symptoms and associated cognitions (“When I feel sad, I assume the worst”). Upon identifying this pattern of thinking, Jason was able to plan ahead for this distortion. His strategies included the use of more adaptive thoughts and behavioral skills, such as getting support or using exercise as a coping skill.
In addition, Jason identified potential stressors such as “arguments with parents” and frequent criticism by his father. Early in the treatment, Jason and the therapist devised specific behavioral coping skills, such as playing music or calling a friend, which Jason could utilize to stabilize his mood after family conflict. Jason and the therapist agreed to have family sessions with the goal of reducing conflict and negative emotion in the home. Jason’s family was seen for three family sessions within the first few weeks of treatment. These family sessions were conducted in conjunction with the individual sessions, so that session length for the individual visit was 45 minutes followed by a 45-minute conjoint session. Initially the family was provided with psychoeducation on the connection between family conflict and negative emotion and the risk for relapse. Jason, his family, and the therapist collaboratively determined ways to give Jason support to maintain remission. The family and Jason worked to negotiate minimal expectations for him at home and consequences for meeting these goals. The therapist met with Jason’s parents briefly at each visit to obtain input about Jason’s progress and to answer questions about the skills handouts provided to the parents at each session.
As individual and family skills were identified as effective for specific problems, these skills were added to the timeline. Post-it notes (to “Make it Stick”) were collaboratively completed to include summarized key points from the sessions, identified practice tasks, and homework assignments. The therapist sent postcards to Jason between sessions for encouragement. These postcards also often reviewed key points and served as homework reminders.
Sessions 5–8
Jason and the therapist met biweekly for 8 weeks. Once Jason’s residual symptoms decreased and his target areas showed improvement, the focus of the treatment shifted to wellness skills. The therapist introduced the concept of a wellness continuum, using sports metaphors of conditioning and strengthening to prevent future injury. Jason completed a wellness log of current activities that reflected wellness behavior as well as positive strengths and abilities.
Jason and the therapist identified two wellness areas to build on: success activities and spiritual activities. In the area of success or mastery, Jason identified that he wanted to expand his musical activities. Jason had played the guitar primarily by himself at home. Jason and the therapist devised a list of possible ways that Jason could increase opportunities for success in music, including adding guitar lessons and joining a band. In addition, he wanted to strengthen his spiritual wellness and indicated a desire to increase his participation in altruistic activities. Jason began to help out family members more at home, particularly his mother. This also resulted in improved relationships at home. He also identified a goal of increasing community service at school.
In Session 8, Jason completed a relapse prevention and wellness plan. He identified potential stressors, including depressive cognitions and behaviors associated with relapse. Jason and the therapist paired these risk factors with skills to use to manage his mood. In addition, he listed several wellness activities to increase with a plan for monitoring them on a weekly basis.
Sessions 9–11, Optional Booster Sessions
Jason met monthly with the therapist for booster sessions. The focus of these sessions was (a) to monitor his relapse risk factors, (b) to continue to apply RP-CBT strategies in the management of his mood, and (c) to continue to identify activities to maintain wellness. Jason continued to work on managing his thinking in relationship to perceived criticism from others. Jason reported to the therapist that he had joined a band and was volunteering at a local recreation center. Termination included a review of treatment progress and a review of the relapse prevention and wellness plan. Jason was presented with a binder that contained copies of his worksheets, “Make It Stick” Post-it notes, and the postcards. Emphasis was placed on Jason’s own competence in his ability to manage his mood and maintain his wellness activities. In addition, the family was included in a final review of the relapse prevention and wellness plan to clarify their role in helping Jason maintain the gains made in continuation treatment. At both 9 and 12 months after the start of acute treatment, Jason remained in remission.
Moving From Stage I to Stage II: Design of the RCT of RP-CBT
We are currently conducting a small, randomized controlled trial, funded through a NIMH R34 treatment development mechanism, to provide pilot data for a larger RCT to test the efficacy of the above treatment. The two main goals of the ongoing project: (1) to test the acceptability and feasibility of randomizing youth to a continuation phase treatment after successful acute treatment, and (2) to provide pilot data on the efficacy of the RP-CBT intervention and the appropriateness and utility of the chosen outcome measures.
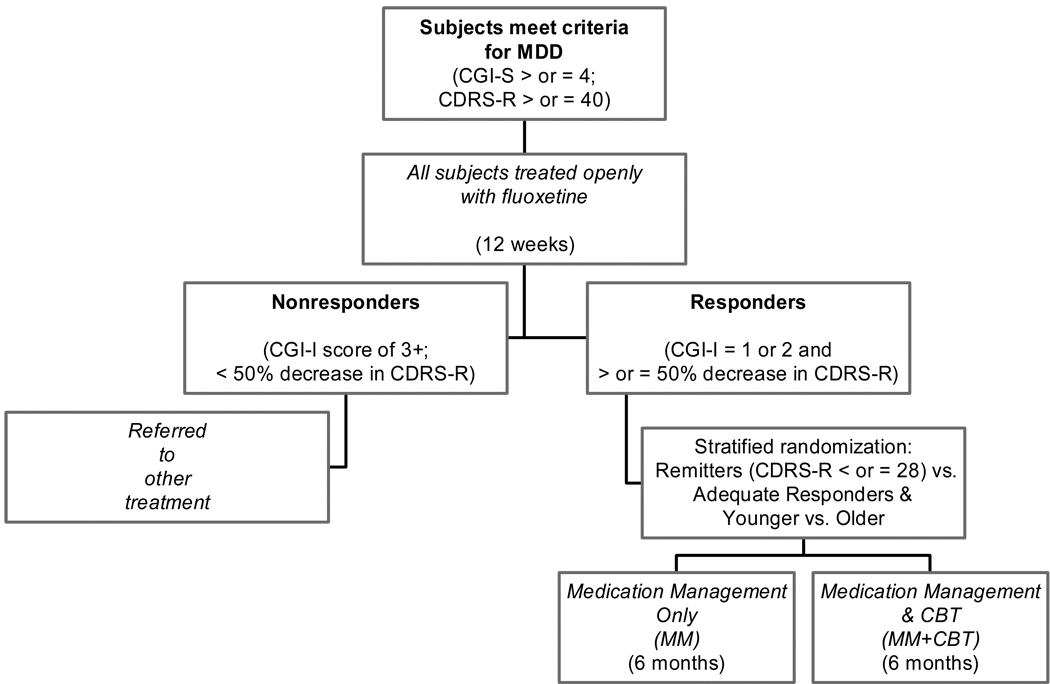
The ongoing trial tests a sequential treatment strategy, with acute open treatment (12 weeks) and randomized continuation phase treatment (24 weeks). Sixty child and adolescent outpatients who meet DSM-IV criteria for MDD and complete a 2-week (three visit) diagnostic evaluation will be treated openly during acute phase treatment with fluoxetine (10 to 40 mg) for 12 weeks. The acute phase duration of 12 weeks was chosen, as remission rates are low at 8 weeks of treatment and we wanted to allow adequate time to for response and remission to occur (Cheung, Emslie, & Mayes, 2005). Responders (estimated n = 40), defined as those participants with a Clinical Global Impression–Improvement (CGI-I; Guy, 1976) score of 1 or 2 and a greater than or equal to 50% reduction in symptoms on the CDRS-R (Poznanski & Mokros, 1996), are randomized to continued Medication Management (MM) or continued MM plus CBT (MM+CBT). The randomization is stratified according to the subject level of response: remitters (CGI-I of 1 or 2 and CDRS-R ≤ 28) and adequate responders (CGI-I of 1 or 2 and ≥ 50% decrease in CDRS-R from baseline; but > 28). In addition, groups are stratified by age (younger, 11 to 14, vs. older, 15 and above). The rationale for stratification by subject level of response is that there is some evidence that continuation CBT is more effective for those with residual symptoms than for those in full remission (without residual symptoms; Perlis et al., 2002). Furthermore, Clarke et al. (1999) reported that booster sessions (quarterly) led to further improvement of residual symptoms, which we will also be measuring for pilot data. Finally, there is some recent evidence that younger and older patients respond differently to treatments for depression (Curry et al., 2006).
See Figure 3 for the ongoing RCT study design. Participants in both MM and MM+CBT continue on the same dose of fluoxetine for 12 additional weeks. During this time, participants in the MM+CBT cell receive RP-CBT. At 24 weeks, participants in both cells are discontinued off of medication. Participants in the MM+CBT arm then receive 12 additional weeks of RP-CBT (monthly optional booster sessions). All participants have monthly assessments after week 24 for 3 months and a final assessment 1 year post-baseline (week 52). At this time the pilot study is still ongoing, with scheduled completion in January 2008.
Figure 3.
RP-CBT Pilot Study Design
Conclusions
There are successful acute treatments for pediatric depression in children and adolescents. Due to high rates of relapse, however, maintaining treatment gains is difficult. There is a need to develop continuation phase treatments that focus on the prevention of relapse in this age group. The RP-CBT treatment is designed to reduce residual symptoms of depression and increase wellness and lifelong strategies that promote emotional health after acute treatment for depression. While this treatment strategy is currently being pilot tested in a randomized controlled trial, our experiences to date indicate that this treatment is feasible, well tolerated, and acceptable to patients and families.
Acknowledgments
This research is funded by two National Institute of Mental Health Grants: R34 MH072737 awarded to Dr. Kennard and K24 MH001571 awarded to Dr. Jarrett. We would like to thank Avery Hoenig, Jessica Jones, and Puja Patel for their valuable contributions to the development of the treatment manual. In addition, we also greatly appreciate the careful review and suggestions from David Brent, Greg Clarke, John Curry, Kim Poling, Kevin Stark and his graduate students.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Asarnow JR, Goldstein MJ, Tompson M, Guthrie D. One-year outcomes of depressive disorders in child psychiatric in-patients. Evaluation of the prognostic power of a brief measure of expressed emotion. Journal of Child Psychology and Psychiatry. 1993;34:129–137. doi: 10.1111/j.1469-7610.1993.tb00975.x. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory – II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Birmaher B, Brent DA, Kolko D, Baugher M, Bridge J, Holder D, et al. Clinical outcome after short-term psychotherapy for adolescents with major depressive disorder. Archives of General Psychiatry. 2000;57:29–36. doi: 10.1001/archpsyc.57.1.29. [DOI] [PubMed] [Google Scholar]
- Brent D, Bridge M, Bonner C. Cognitive behavior therapy manual for TORDIA. 2000 Unpublished manuscript. [Google Scholar]
- Brent DA, Holder D, Kolko D, Birmaher B, Baugher M, Roth C, et al. A clinical psychotherapy trial for adolescent depression comparing cognitive, family, and supportive therapy. Archives of General Psychiatry. 1997;54:877–885. doi: 10.1001/archpsyc.1997.01830210125017. [DOI] [PubMed] [Google Scholar]
- Brent D, Poling K. Cognitive therapy treatment manual for depressed and suicidal youth. 1997 Unpublished manuscript. [Google Scholar]
- Butler L, Mietzitis S, Friedman R, Cole E. The effect of two school-based intervention programs on depressive symptoms in preadolescents. American Educational Research Journal. 1980;17:111–119. [Google Scholar]
- Cheung AH, Emslie GJ, Mayes TL. Review of the efficacy and safety of antidepressants in youth. Journal of Child Psychology and Psychiatry. 2005;46:735–754. doi: 10.1111/j.1469-7610.2005.01467.x. [DOI] [PubMed] [Google Scholar]
- Clarke GN, Rohde P, Lewinsohn PM, Hops H, Seeley JR. Cognitive-behavioral treatment of adolescent depression: Efficacy of acute group treatment and booster sessions. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:272–279. doi: 10.1097/00004583-199903000-00014. [DOI] [PubMed] [Google Scholar]
- Compton SN, March JS, Brent D, Albano AM, Weersing R, Curry J. Cognitive-behavioral psychotherapy for anxiety and depressive disorders in children and adolescents: An evidence-based medicine review. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43:930–959. doi: 10.1097/01.chi.0000127589.57468.bf. [DOI] [PubMed] [Google Scholar]
- Cornwall PL, Scott J. Partial remission in depressive disorders. Acta Psychiatrica Scandinavica. 1997;95:265–271. doi: 10.1111/j.1600-0447.1997.tb09630.x. [DOI] [PubMed] [Google Scholar]
- Curry JF. Specific psychotherapies for childhood and adolescent depression. Biological Psychiatry. 2001;49:1091–1100. doi: 10.1016/s0006-3223(01)01130-1. [DOI] [PubMed] [Google Scholar]
- Curry JF, Craighead WE. Attributional style in clinically depressed and conduct disordered adolescents. Journal of Consulting and Clinical Psychology. 1990;58:109–115. doi: 10.1037//0022-006x.58.1.109. [DOI] [PubMed] [Google Scholar]
- Curry J, Rohde P, Simons A, Silva S, Vitiello B, Kratochvil C, et al. Predictors and moderators of acute outcome in the Treatment for Adolescents with Depression Study (TADS) Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45:1427–1439. doi: 10.1097/01.chi.0000240838.78984.e2. [DOI] [PubMed] [Google Scholar]
- Curry J, Wells K, Brent D, Clarke G, Rodhe P, Albano AM, et al. Cognitive behavior therapy manual for TADS. 2000 Unpublished manuscript. [Google Scholar]
- Emslie GJ, Heiligenstein JH, Hoog SL, Wagner KD, Findling RL, McCracken JT, et al. Fluoxetine treatment for prevention of relapse of depression in children and adolescents: a double-blind, placebo-controlled study. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43:1397–1405. doi: 10.1097/01.chi.0000140453.89323.57. [DOI] [PubMed] [Google Scholar]
- Emslie GJ, Heiligenstein J, Wagner K, Hoog S, Ernest D, Brown E, et al. Fluoxetine for acute treatment of depression in children and adolescents: A placebo-controlled, randomized clinical trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:1205–1215. doi: 10.1097/00004583-200210000-00010. [DOI] [PubMed] [Google Scholar]
- Emslie GJ, Rush AJ, Weinberg WA, Kowatch RA, Hughes CW, Carmody T, et al. A double-blind, randomized, placebo-controlled trial of fluoxetine in children and adolescents with depression. Archives of General Psychiatry. 1997;54:1031–1037. doi: 10.1001/archpsyc.1997.01830230069010. [DOI] [PubMed] [Google Scholar]
- Faravelli C, Ambonetti A, Pallanti S, Pazzagli A. Depressive relapses and incomplete recovery from index episode. American Journal of Psychiatry. 1986;143:888–891. doi: 10.1176/ajp.143.7.888. [DOI] [PubMed] [Google Scholar]
- Fava GA, Fabbri S, Sonino N. Residual symptoms in depression: An emerging therapeutic target. Progress in Neuro-Psychopharmacology & Biological Psychiatry. 2002;26:1019–1027. doi: 10.1016/s0278-5846(02)00226-9. [DOI] [PubMed] [Google Scholar]
- Fava GA, Grandi S, Zielezny M, Canestrari R, Morphy MA. Cognitive behavioral treatment of residual symptoms in primary major depressive disorder. American Journal of Psychiatry. 1994;151:1295–1299. doi: 10.1176/ajp.151.9.1295. [DOI] [PubMed] [Google Scholar]
- Fava GA, Grandi S, Zielezny M, Rafanelli C, Canestrari R. Four-year outcome for cognitive behavioral treatment of residual symptoms in major depression. American Journal of Psychiatry. 1996;153:945–947. doi: 10.1176/ajp.153.7.945. [DOI] [PubMed] [Google Scholar]
- Fava GA, Rafanelli C, Cazzaro M, Conti S, Grandi S. Well-being therapy: A novel psychotherapeutic approach for residual symptoms of affective disorders. Psychological Medicine. 1998;28:475–480. doi: 10.1017/s0033291797006363. [DOI] [PubMed] [Google Scholar]
- Fava GA, Rafanelli C, Grandi S, Canestrari R, Morphy MA. Six-year outcome for cognitive behavioral treatment of residual symptoms in major depression. American Journal of Psychiatry. 1998;155:1443–1445. doi: 10.1176/ajp.155.10.1443. [DOI] [PubMed] [Google Scholar]
- Frank E, Prien RF, Jarrett RB, Keller MB, Kupfer DJ, Lavori PW, et al. Conceptualization and rationale for consensus definitions of terms in major depressive disorder: Remission, recovery, relapse, and recurrence. Archives of General Psychiatry. 1991;48:851–855. doi: 10.1001/archpsyc.1991.01810330075011. [DOI] [PubMed] [Google Scholar]
- Gilman R, Huebner EW, Laughlin JE. A first study of the Multidimensional Student Life Satisfaction Scale with adolescents. Social Indicators Research. 2000;52:135–160. [Google Scholar]
- Guy W. Washington, DC: US Government Printing Office; ECDEU Assessment Manual for Psychopharmacology, 2nd ed. (DHEW Publication ABM 76–388) 1976
- Hammen C. Life events and depression: The plot thickens. American Journal of Community Psychology. 1992;20:179–193. doi: 10.1007/BF00940835. [DOI] [PubMed] [Google Scholar]
- Hollon SD, Munoz RF, Barlow DH, Beardslee WR, Bell CC, Bernal G, et al. Psychosocial intervention development for the prevention and treatment of depression: Promoting innovation and increasing access. Biological Psychiatry. 2002;52:610–630. doi: 10.1016/s0006-3223(02)01384-7. [DOI] [PubMed] [Google Scholar]
- Huebner ES. Preliminary development and validation of a multidimensional life satisfaction scale for children. Psychological Assessment. 1994;6:149–158. [Google Scholar]
- Huebner ES. Manual for the Multidimensional Students’ Life Satisfaction Scale. 2001 Unpublished manuscript. [Google Scholar]
- Jarrett RB, Kraft D. Prophylactic cognitive therapy for major depressive disorder. In Session. 1997;3:55–67. [Google Scholar]
- Jarrett RB, Kraft D, Doyle J, Foster BM, Eaves GG, Silver PC. Preventing recurrent depression using cognitive therapy with and without a continuation phase: A randomized clinical trial. Archives of General Psychiatry. 2001;58:381–388. doi: 10.1001/archpsyc.58.4.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarrett RB, Vittengl J, Clark LA. Cognitive therapy for recurrent major depressive disorder: Relapse prevention. In: Whisman MA, editor. Cognitive therapy for complex and comorbid depression: Assessment and treatment. New York: Guilford Press; (in press). [Google Scholar]
- Jaycox LH, Reivich KJ, Gillham J, Seligman ME. Prevention of depressive symptoms in school children. Behavior Research and Therapy. 1994;32:801–816. doi: 10.1016/0005-7967(94)90160-0. [DOI] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS, Maser JD, Zeller PJ, Endicott J, Coryell W, et al. Major depressive disorder: A prospective study of residual subthreshold depressive symptoms as predictor of rapid relapse. Journal of Affective Disorders. 1998;50:97–108. doi: 10.1016/s0165-0327(98)00138-4. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children – Present and Lifetime Version (K-SADS-PL): Initial reliability and validity date. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Weisz JR. Identifying and developing empirically supported child and adolescent treatments. Journal of Consulting and Clinical Psychology. 1998;66:19–36. doi: 10.1037//0022-006x.66.1.19. [DOI] [PubMed] [Google Scholar]
- Keller MB. Remission versus response: The new gold standard of antidepressant care. Journal of Clinical Psychiatry. 2004;65 Suppl. 4:53–59. [PubMed] [Google Scholar]
- Kennard BD. Relapse Prevention CBT: Reducing residual symptoms and increasing emotional wellness in youth with MDD. 2006 Unpublished Manuscript. [Google Scholar]
- Kennard BD, Emslie GJ, Mayes TL, Hughes JL. Relapse and recurrence in pediatric depression. Child and Adolescent Psychiatric Clinics of North America. 2006;15:1057–1079. doi: 10.1016/j.chc.2006.05.003. [DOI] [PubMed] [Google Scholar]
- Kennard B, Silva S, Vitiello B, Curry J, Kratochvil C, Simons A, et al. Remission and residual symptoms after short-term treatment in the Treatment of Adolescents with Depression Study (TADS) Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45:1404–1411. doi: 10.1097/01.chi.0000242228.75516.21. [DOI] [PubMed] [Google Scholar]
- Kennard BD. Remission and recovery in the TADS; Presented at the 54th Annual Meeting of the American Academy of Child and Adolescent Psychiatry; Boston, MA. 2007. Oct, [Google Scholar]
- Kratochvil C, Emslie G, Silva S, McNulty S, Walkup J, Curry J, et al. Acute time to response in the Treatment for Adolescents with Depression Study (TADS) Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:1412–1418. doi: 10.1097/01.chi.0000237710.73755.14. [DOI] [PubMed] [Google Scholar]
- Kroll L, Harrington R, Jayson D, Fraser J, Gowers S. Pilot study of continuation cognitive-behavioral therapy for major depression in adolescent psychiatric patients. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35:1156–1161. doi: 10.1097/00004583-199609000-00013. [DOI] [PubMed] [Google Scholar]
- Kupfer DJ. Long-term treatment of depression. Journal of Clinical Psychiatry. 1991;52 Suppl.:28–34. [PubMed] [Google Scholar]
- Lewinsohn PM, Clarke GN, Hops H, Andrews JA. Cognitive-behavioral treatment for depressed adolescents. Behavior Therapy. 1990;21:385–401. [Google Scholar]
- Lewinsohn PM, Rhode P, Seeley JR, Klein DN, Gotlib IH. Natural course of adolescent major depressive disorder in a community sample: Predictors of recurrence in young adults. American Journal of Psychiatry. 2000;157:1584–1591. doi: 10.1176/appi.ajp.157.10.1584. [DOI] [PubMed] [Google Scholar]
- Mufson L, Weissman MM, Moreau D, Garfinkel R. Efficacy of interpersonal psychotherapy for depressed adolescents. Archives of General Psychiatry. 1999;56:573–579. doi: 10.1001/archpsyc.56.6.573. [DOI] [PubMed] [Google Scholar]
- Nguyen TD, Attkisson CC, Stegner BL. Assessment of patient satisfaction: Development and refinement of a service evaluation questionnaire. Evaluation and Program Planning. 1983;6:299–314. doi: 10.1016/0149-7189(83)90010-1. [DOI] [PubMed] [Google Scholar]
- Nierenberg AA. Long-term management of chronic depression. Journal of Clinical Psychiatry. 2001;62:17–21. [PubMed] [Google Scholar]
- Paykel ES, Ramana R, Cooper Z, Hayhurst H, Kerr J, Barocka A. Residual symptoms after partial remission: An important outcome in depression. Psychological Medicine. 1995;25:1171–1180. doi: 10.1017/s0033291700033146. [DOI] [PubMed] [Google Scholar]
- Paykel ES, Scott J, Teasdale JD, Johnson AL, Garland A, Moore R, et al. Prevention of relapse in residual depression by cognitive therapy: A controlled trial. Archives of General Psychiatry. 1999;56:829–835. doi: 10.1001/archpsyc.56.9.829. [DOI] [PubMed] [Google Scholar]
- Perlis R, Nierenberg A, Alpert J, Pava J, Matthews J, Buchin J, et al. The effects of adding cognitive therapy to fluoxetine dose increase on risk of relapse and residual depressive symptoms in continuation treatment of major depressive disorder. Journal of Clinical Psychopharmacology. 2002;22:474–480. doi: 10.1097/00004714-200210000-00006. [DOI] [PubMed] [Google Scholar]
- Poznanski E, Mokros H. Children’s Depression Rating Scale-Revised (CDRS-R) Los Angeles: WPS; 1996. [Google Scholar]
- Reinecke MA, Ryan NE, DuBois DL. Cognitive-behavioral therapy of depression and depressive symptoms during adolescence: A review and meta-analysis. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:26–34. doi: 10.1097/00004583-199801000-00013. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Carroll KM, Onken LS. A stage model of behavioral therapies research: Getting started and moving on from stage I. Clinical Psychology: Science and Practice. 2001;8:133–142. [Google Scholar]
- Rush AJ, Kraemer HC, Sackeim HA, Fava M, Trivedi MH, Frank E, et al. Report by the ACNP Task Force on response and remission in major depressive disorder. Neuropsychopharmacology. 2006;31:1841–1853. doi: 10.1038/sj.npp.1301131. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH. Treating depression to remission. Psychiatric Annals. 1995;25:704–709. [Google Scholar]
- Ryff CD, Singer B. Psychological well-being: Meaning, measurement, and implications for psychotherapy research. Psychotherapy and Psychosomatics. 1996;65:14–23. doi: 10.1159/000289026. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression. New York: Guilford Press; 2002. [Google Scholar]
- Seligman M, Csikszentmihalyi M. Positive psychology: An introduction. American Psychologist. 2000;55:5–14. doi: 10.1037//0003-066x.55.1.5. [DOI] [PubMed] [Google Scholar]
- Seligman MEP, Schulman P, DeRubeis RJ, Hollon SD. The prevention of depression and anxiety. Prevention and Treatment. 1999;2 Article 8. Available on the World Wide Web: http://journals.apa.org/prevention/volume2/pre0020008a.html.
- Sherrill JT, Kovacs M. Treatment of mood disorders in children and adolescents: Nonsomatic treatment of depression. Psychiatric Clinics of North America. 2004;27:139–154. doi: 10.1016/S0193-953X(03)00115-1. [DOI] [PubMed] [Google Scholar]
- Simons AD, Murphy GE, Levine JL, Wetzel RD. Cognitive therapy and pharmacotherapy for depression: Sustained improvement over one year. Archives of General Psychiatry. 1986;43:43–48. doi: 10.1001/archpsyc.1986.01800010045006. [DOI] [PubMed] [Google Scholar]
- Snyder CR, Lopez SJ, editors. Handbook of positive psychology. New York: Oxford University Press; 2005. [Google Scholar]
- Stark K. Treating depressed girls: Counselor manual for ACTION. 2005 Unpublished manuscript. [Google Scholar]
- Stark KD, Reynolds WM, Kaslow NJ. A comparison of the relative efficacy of self-control therapy and behavioral problem-solving therapy for depression in children. Journal of Abnormal Child Psychology. 1987;15:91–113. doi: 10.1007/BF00916468. [DOI] [PubMed] [Google Scholar]
- TADS Team. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents with Depression Study (TADS) randomized controlled trial. JAMA. 2004;292:807–820. doi: 10.1001/jama.292.7.807. [DOI] [PubMed] [Google Scholar]
- TADS Team. The Treatment for Adolescents with Depression Study (TADS): Long-term effectiveness and safety outcomes. Archives of General Psychiatry. 2007;64:1132–1143. doi: 10.1001/archpsyc.64.10.1132. [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Scott J, Moore RG, Hayhurst H, Pope M, Paykel ES. How does cognitive therapy prevent relapse in residual depression? Evidence from a controlled trial. Journal of Consulting and Clinical Psychology. 2001;69:347–357. doi: 10.1037//0022-006x.69.3.347. [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Segal ZV, Williams JM, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting & Clinical Psychology. 2000;68:615–623. doi: 10.1037//0022-006x.68.4.615. [DOI] [PubMed] [Google Scholar]
- Thase ME, Simons AD, McGeary J, Cahalane JF, Hughes C, Harden T, et al. Relapse after cognitive behavior therapy of depression: Potential implications for longer courses of treatment. American Journal of Psychiatry. 1992;149:1046–1052. doi: 10.1176/ajp.149.8.1046. [DOI] [PubMed] [Google Scholar]
- Varni JW, Rapoff MA, Waldron SA, Gragg RA, Bernstein BH, Lindsley CB. Effects of perceived stress on pediatric chronic pain. Journal of Behavioral Medicine. 1996;19:515–528. doi: 10.1007/BF01904901. [DOI] [PubMed] [Google Scholar]
- Varni JW, Rubenfeld LA, Talbot D, Setoguchi Y. Determinants of self-esteem in children and adolescents with congenital/acquired limb deficiencies. Journal of Developmental and Behavioral Pediatrics. 1989;10:13–16. [PubMed] [Google Scholar]
- Varni JW, Setoguchi Y, Rappaport LT, Talbot D. Effects of stress, social support, and self-esteem on depression in children with limb deficiencies. Archives of Physical Medicine and Rehabilitation. 1991;72:1053–1058. [PubMed] [Google Scholar]
- Vittengl JR, Clark LA, Dunn TW, Jarrett RB. Reducing relapse and recurrence in unipolar depression: A comparative meta-analysis of cognitive therapy’s effects. Journal of Consulting and Clinical Psychology. 2007;75:475–488. doi: 10.1037/0022-006X.75.3.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vostanis P, Feehan C, Grattan E, Bickerton W. A randomised controlled outpatient trial of cognitive-behavioural treatment for children and adolescents with depression: 9-month follow-up. Journal of Affective Disorders. 1996;40:105–116. doi: 10.1016/0165-0327(96)00054-7. [DOI] [PubMed] [Google Scholar]
- Wagner KD, Robb AS, Findling RL, Jin J, Gutierrez MM, Heydorn WE. A randomized, placebo-controlled trial of citalopram for the treatment of major depression in children and adolescents. American Journal of Psychiatry. 2004;161:1079–1083. doi: 10.1176/appi.ajp.161.6.1079. [DOI] [PubMed] [Google Scholar]
- Weisz JR, McCarty CA, Valeri SM. Effects of psychotherapy for depression in children and adolescents: A meta-analysis. Psychological Bulletin. 2006;132:132–149. doi: 10.1037/0033-2909.132.1.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkes TCR, Belsher G, Rush AJ, Frank E. Cognitive therapy for depressed adolescents. New York: Guilford Press; 1994. [Google Scholar]
- Wood A, Harrington R, Moore A. Controlled trial of a brief cognitive-behavioural intervention in adolescent patients with depressive disorders. Journal of Child Psychology and Psychiatry. 1996;37:737–746. doi: 10.1111/j.1469-7610.1996.tb01466.x. [DOI] [PubMed] [Google Scholar]
- Zuckerman LA, Oliver JM, Hollingsworth HH, Austrin H. A comparison of life events scoring methods as predictors of psychological symptomatology. Journal of Human Stress. 1986;12:64–70. doi: 10.1080/0097840X.1986.9936769. [DOI] [PubMed] [Google Scholar]