Abstract
Background
Sleeping sickness is spread over 36 Sub-Saharan African countries. In West and Central Africa, the disease is caused by Trypanosoma brucei gambiense, which produces a chronic clinical manifestation. The Luba focus (Bioko Island, Equatorial Guinea) has not reported autochthonous sleeping sickness cases since 1995, but given the complexity of the epidemiological cycle, the elimination of the parasite in the environment is difficult to categorically ensure.
Methodology/Principal Findings
The aim of this work is to assess, by a molecular approach (Polymerase Chain Reaction, PCR), the possible permanence of T. b. gambiense in the vector (Glossina spp.) and domestic fauna in order to improve our understanding of the epidemiological situation of the disease in an isolated focus considered to be under control.
The results obtained show the absence of the parasite in peridomestic livestock but its presence, although at very low rate, in the vector. On the other hand, interesting entomological data highlight that an elevated concentration of tsetse flies was observed in two out of the ten villages considered to be in the focus.
Conclusions
These findings demonstrate that even in conditions of apparent control, a complete parasite clearance is difficult to achieve. Further investigations must be focused on animal reservoirs which could allow the parasites to persist without leading to human cases. In Luba, where domestic livestock are scarcer than other foci in mainland Equatorial Guinea, the epidemiological significance of wild fauna should be assessed to establish their role in the maintenance of the infection.
Author Summary
Sleeping sickness is a neglected disease with an important impact on public health of many countries of Sub-Saharan Africa. It is transmitted by tsetse fly bites (the vector) and mainly affects remote and rural populations. The chronic form, caused by Trypanosoma brucei gambiense, includes almost 90% of reported cases, and it is often misdiagnosed or lately detected after months or years of infection. Many efforts have been carried out to control the disease and interesting advances have been achieved. Although elimination is considered possible, there is an urgent need to understand the disease dynamic, especially in foci with very low rate (or absent) of infection for a long time. We performed a parasite screening in tsetse flies and livestock from Luba focus (Equatorial Guinea), considered to be “controlled” since 1995 (no human cases for fifteen years). The obtained results demonstrate that T. b. gambiense still remains in the environment and entomological data reveal high population density of the vector in some localities. This finding suggests that other intervention ways focused on control of vector populations, combined with the detection of human cases, could be necessary to achieve the total elimination of the parasite in hypoendemic foci.
Introduction
Human African Trypanosomiasis (HAT), also known as sleeping sickness, is a parasitic disease endemic of the African continent. HAT is caused by two subspecies of the flagellate Trypanosoma brucei; T. b. gambiense, spread over West and Central Africa, which is responsible for the chronic form of the disease (more than 90% of total number of cases) and T. b. rhodesiense, which is present in East Africa and produces a few cases of acute infection per year. In addition, other members of Trypanosoma genus are able to infect a wide variety of animals producing diseases of veterinary importance such as nagana (T. b. brucei, T. vivax and T. congolense), surra (T. evansi) or dourine (T. equiperdum). T. brucei s.l. is mainly transmitted by tsetse flies (Diptera, Glossinidae) but other trypanosomes can be mechanically or sexually transmitted [1], [2].
In last years, control activities against sleeping sickness have been encouraged and significant advances were achieved to eliminate the disease [3]. The main strategy was to actively screen the human carriers in endemic foci [4], [5] since it is assumed that humans are the main reservoir of T. b. gambiense infection [6].
Luba focus, located on Bioko Island (Equatorial Guinea), is a good example of the success of control campaigns exclusively directed to humans. HAT was firstly declared in Luba in 1910 [7] and two decades later a successful control programme was implemented. At the end of 1960s, sleeping sickness was considered to be under control over the entire country and after the independence in 1968, HAT ceased to be a priority of public health for the new authority. In the middle of 1980s, Luba suffered a resurgence of the disease registering hundreds of cases leading to the establishment of the Sleeping Sickness National Control Programme (SSNCP) by Health Ministry and Social Welfare. This programme targeted the disease control combining active cases detection and passive surveillance using serological techniques. All parasitologically confirmed and serologically suspected cases were treated. This strategy led to a drastic reduction in the number of reported patients. The last autochthonous case was recorded in 1995 and no more surveys have been carried out since 2004 [5].
As occurred in Luba, the neglect of control activities in the past has led to a resurgence of HAT foci considered to have been eliminated. Several hypotheses could explain the resurgence of the disease in apparently controlled foci and the heterogeneity of the disease prevalence in neighbouring foci: movement of carrier populations from active foci [8], changes of the tsetse flies host preference [9], [10], genetic variability of the parasite [11], [12], the existence of asymptomatic parasite-infected individuals [13], inherent limitations of surveillance systems [14] and maintenance of infection in animal reservoirs. The latter theory is supported by the capability of the parasite for surviving in some species of domestic and wild animals [15]–[24].
This study aims to analyse T. b. gambiense infection in tsetse flies and domestic livestock from localities of Luba focus, in order to determine the presence of the parasites apart from the human transmission cycle. Species-specific molecular tools (PCR) were employed for diagnosis. In addition, entomological data about tsetse fly populations in these localities are provided and discussed.
Materials and Methods
Study Area
Luba focus covers a surface of 700 Km2 in south-western of Bioko Island. There are two climatic seasons: the dry season, from December to May, and the rainy season, from June to November. Bioko's annual rainfall exceeds 2,000 mm and the relative humidity ranges from 70% to 100% throughout the year. The average temperature is 25°C, with the minimum ranging from 17°C to 21°C and the maximum from 29°C to 30°C, depending on the location and the season [25].
The majority of the inhabitants from Luba lived on smallholding, hunting and sea fishing. Rainforest and neglected cocoa plantations are widespread in Luba district, establishing suitable habitats for the tsetse flies [26], [27]. Nowadays, many people from rural areas have migrated to urban, mainly to the capital city (Malabo), due to the recent development of petroleum and building industry. Therefore, rural conditions have partially disappeared and, as a result, many risk factors have been removed. Nevertheless, some villages remain unchanged and human-vector contact is still common.
Sample Collection
In September 2007, blood samples of domestic animals (pigs, sheep and goats) were collected and tsetse flies were captured for further molecular analysis. Sampling procedures on Whatman filter paper for animal blood have been described elsewhere [28]. A previous census of livestock was elaborated in order to ensure a significant sample size. Ethical approval was obtained by Ministry of Health and Social Welfare and Veterinary Service from continental region (Ministry of Agriculture, Forestry and Environment). The study was conducted adhering to these institutions' guidelines for animal husbandry. Verbal informed consent was obtained from each owner of livestock prior to the extraction of blood samples by the field team.
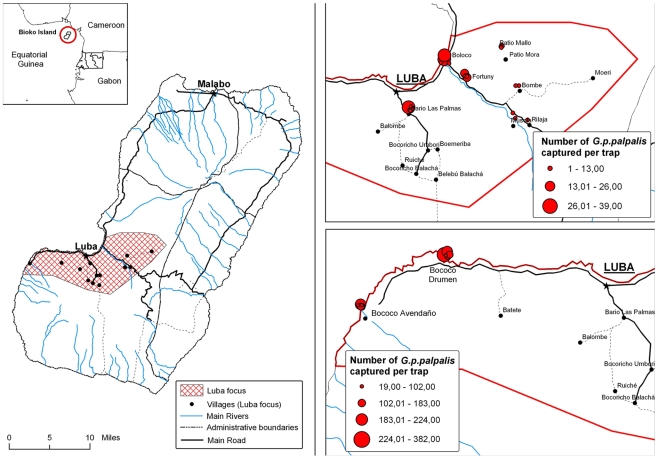
Monopyramidal traps were employed to catch tsetse flies [29]. This kind of trap has been successfully applied for vector control and entomological surveillance in Equatorial Guinea [26], [30], [31]. This device makes flies to fall in a collecting bottle containing conservation solution (formaldehyde 5%) and to be stored until the gathering. Fifty-five traps were spread over the 10 villages belonging to epicentre of Luba focus. They were located in places considered a priori as suitable habitats for tsetse flies. This criterion includes water sources, cocoa or coffee plantations and shady and humid ponds close to livestock [32]–[34]. Geographical coordinates of all traps were registered by GPS (Figure 1) and they remained two weeks in the field. Sampling was carried out twice, a week after the placing and when the traps were removed.
Figure 1. Map of Luba focus and distribution of tsetse fly captures over the villages.
Tsetse flies collected were stored in tubes with absolute ethanol in the field and separately processed in laboratory recording the trap number, an individual code, village, date, species, sex and age. The key of Brunhes et al. [35] was used for species identification and an age estimator, based on the degree of wear or fraying observed on the hind margin of the wing, was employed as previously described [36], [37]. In addition, apparent density (AD), estimated as AD = number of tsetse flies/trap/day, was calculated for each trap.
Both tsetse flies and blood samples were sent to National Centre of Tropical Medicine, Institute of Health Carlos III (Spain) for molecular processing.
DNA Extraction and Molecular Analysis
DNA extraction from blood samples was performed employing a slightly modified protocol with Chelex 100® ionic resin (Bio-Rad Laboratories, Madrid, Spain) as previously described [28], [38].
Prior to DNA extraction, wings and legs of tsetse flies were removed using a sterile surgical blade. This step was carried out in order to minimize the amount of exoskeleton compounds included in the sample, which are known to inhibit subsequent enzymatic reactions [39]. Flies were then washed in 70% ethanol and in double distilled water (DDW). For dried samples, each fly was put in a sterile 1.5 ml tube and DNA extraction was performed employing the SpeedTools Tissue DNA Kit (Biotools, B & M Labs, S.A., Madrid, Spain) following the manufacturer instructions. All extraction instruments were sterilized after processing each fly by ethanol submersion and flaming. Finally, a negative control (clean 1.5 ml tube with no sample) was included in all procedures of the extraction (one negative each seventeen samples).
Ten µl of DNA template from blood samples were subjected to species-specific PCR for T. brucei s.l. and, when positive, for T. b. gambiense. For T. brucei s.l. analysis, TBR1/2 primers were used [40] with the following conditions: 1× PCR Reaction Buffer (10 mM Tris-HCl, 1.5 mM MgCl2, 50 mM KCl, pH 8.3), 200 µM of each deoxynucleotide (dNTP), primers at 0.5 µM and 1.25 U of Taq DNA Polymerase (Roche Diagnostics, S.L. Barcelona, Spain) in a final volume of 50 µl. Positive samples for this test were diagnosed for T. b. gambiense employing a nested-PCR with a first reaction using TgsGP1/2 primers [41] and a second one with TgsGP sense2/antisense2 primers described by Morrison et al. [42]. In both reactions 50 µl of final volume were reached and conditions were identical to T. brucei s.l. test with the exception of the amount of polymerase employed (2.5 U). The amplification programme for T. brucei s.l. was set as follows: a first step at 85°C (5 min) for hot starting, 3 min at 95°C for initial DNA denaturation, 40 cycles of 95°C (1 min), 55°C (1 min) and 72°C (1 min) and a final extension step at 72°C (5 min). For the first reaction of T. b. gambiense the fixed programme was: initial denaturation step at 95°C (5 min), 45 cycles of 94°C (1 min), 63°C (1 min) and 72°C (1 min) with a final extension step at 72°C for 5 min. The programme for the second reaction was identical but only 25 cycles were performed.
The quality of DNA templates from tsetse samples were tested by amplification of specific tubulin gene following the protocols described by Hao Z et al. (2003) [43] and Ferreira F et al. (2008) [44]. This step was considered because of the known PCR inhibition with samples of arthropods [39]. DNA samples that displayed a positive amplification signal for the tsetse tubulin gene were further tested to detect T. brucei s.l. and T. b. gambiense with the same primers and similar conditions as above: 1× PCR reaction buffer (10 mM Tris-HCl, 50 mM KCl, pH 8.3), 2 mM MgCl2, primers at 0.5 µM, 200 µM of each dNTP, 1 µl of DNA template and 1 U of AmpliTaq® Gold DNA Polymerase (Applied Biosystems, Branchburg, New Jersey, USA) reaching a final volume of 25 µl. The amplification programmes were modified increasing the time for the first denaturation step up to 10 minutes for polymerase activation as recommended by manufacturer and excluding the manual hot start step performed previously for T. brucei s.l. reactions.
In all PCR assays two negative controls (with DDW as template) and one positive control (1 ng DNA from T. brucei s.l. 328.114 or 1 ng from T. b. gambiense ELIANE) were included.
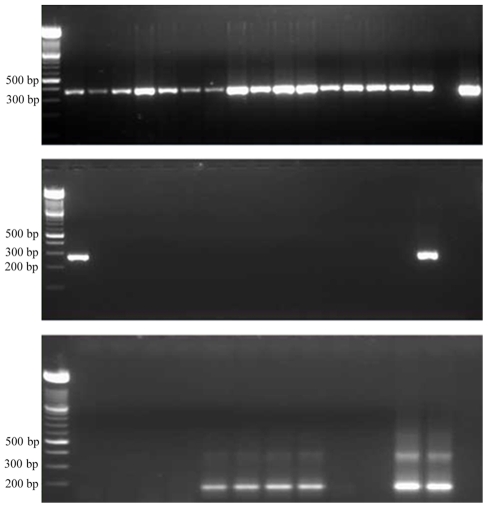
All amplification products were separated by electrophoresis in a 2% agarose gel stained with ethidium bromide (1 µg/ml) and photographed under UV light. Any sample displaying a visible band of the expected length in the gel was considered as positive (Figure 2).
Figure 2. Revealed results of PCR in 2% agarose gel stained with ethidium bromide under UV.
Above: Samples from sixteen tsetse flies submitted to PCR using GmTub primers as DNA quality control. Expected band size ∼380 bp. Middle: Molecular diagnosis of samples from fifteen tsetse flies for T. b. gambiense. First sample corresponds to the one positive tsetse fly. The band at right is the positive control. Expected band size 270 bp. Below: Detection of T. brucei s.l. in animal samples. 5–8 and 11 are positives, 12 is the positive control. Expected band size 177 bp.
Statistical Analysis
SPSS software (version 16.0.1, SPSS Inc., Chicago, IL, USA) was employed for statistical analysis and randomization of samples. Chi-square analysis was applied in order to compare significance of differences between variables (CI 95%). Given the low number of animals sampled in each village and subsequently positives for T. brucei s.l., no variables were statistically compared. Regarding tsetse flies, statistical associations between sex, age, sampling week, village and T. brucei infection were analysed, considering statistically significant p-value<0.05.
Results
Entomological Field Data
Overall 1,839 flies were collected. Almost all of them (1,830) were identified as G. palpalis palpalis as expected by previous entomological data in the country [5], [30], [31]. Eight flies were registered as Glossina caliginea and one individual could not be classified. Only two villages (Bococo Drumen and Bococo Avendaño) concentrated 89.7% of overall captures (1,650/1,839) (Table 1) and those localities showed a mean AD higher than 1 (14.9 in B. Drumen and 8.7 in B. Avendaño). The overall sex ratio was 1.59 (1,128 females/711 males) and no significant difference was observed between the sampling weeks (χ2 = 0.005, p = 0.942). However, sex ratio varies among the villages, from 1.01 in the lowest sampling localities to 1.33 in B. Avendaño and 2.2 in B. Drumen (χ2 = 19.2, p<0.001). Distribution of flies by age groups shows that during second sampling week collected individuals were significantly younger than in the first one (χ2 = 62.16, p<0.001).
Table 1. Distribution of tsetse fly captures and infection amongst villages.
| Village | Total Captures 1st week | Total Captures 2nd week | Positives for T. brucei s.l./Total analysed | Positives for T. b. gambiense | AD* |
| B. Las Palmas | 27 | 20 | 9/47 | 0/9 | 0.67 |
| Fortuny (Boloco)** | 57 | 27 | 20/81 | 0/20 | 0.88 |
| Fortuny | 22 | 17 | 7/38 | 0/7 | |
| Musola | 1 | 2 | 1/3 | 0/1 | 0.04 |
| Rilaja | 0 | 1 | 1/1 | 0/1 | 0.01 |
| Bombe | 1 | 1 | 1/2 | 0/1 | 0.03 |
| Patio Mallo | 9 | 5 | 3/12 | 0/3 | 0.2 |
| B. Drumen | 550 | 493 | 143/531 | 1/143 | 14.9 |
| B. Avendaño | 270 | 336 | 74/190 | 0/74 | 8.67 |
| Total | 937 | 902 | 259/905 | 1/259 | 2.39 |
No flies were trapped in Moeri or Patio Mora.
*AD = Apparent density calculated as number of flies/trap/day.
**Boloco belongs to Fortuny village but a set of five traps were located there due to its relative geographical distance.
Molecular Analysis
A total of 951 tsetse flies gathered (761 randomly selected from B. Drumen and B. Avendaño and 190 flies collected from the other villages) were submitted to DNA extraction and specific tubulin amplification. From them, 905 (95.2%) yielded a positive result for tubulin amplification and then were considered to have enough DNA quality to be included in further diagnostic analysis. Overall, 28.6% (259) of these flies were positive for specific T. brucei s.l. PCR and only one (a young male fly from Bococo Drumen) showed a positive amplification for TgsGP being considered as carrier of T. b. gambiense. No significant difference in T. brucei s.l. prevalence was observed regarding the sex (χ2 = 0.708, p = 0.401), age (χ2 = 9.368, p = 0.095) or week of sampling (χ2 = 0.000, p = 1.00) but infection rate was significantly higher in B. Drumen than the others localities (χ2 = 42.43, p<0.001). Among the G. caliginea individuals (6) included in the analysis neither T. brucei s.l. nor T. b. gambiense were detected.
A previous census showed that there were 161 animals in villages belonging to the epicentre of Luba focus. Only 84 (52.2%) could be sampled since livestock were not kept in sheds and moved freely around the dwellings. Nine animals (eight pigs and one goat) (10.7%) yielded a positive result for T. brucei s.l. and none of them resulted positive for T. b. gambiense (Table 2).
Table 2. Distribution of animal sampling and infection amongst villages.
| Number of animals sampled/censed | Number of animals positive for T. brucei s.l. | |||||
| Village | Pigs | Goats | Total | Pigs | Goats | Total |
| B. Las Palmas | 7/11 | 10/15 | 17/26 | 0/7 | 0/10 | 0/17 |
| Fortuny (Boloco) | 7/36 | 4/7 | 11/43 | 0/7 | 0/4 | 0/11 |
| Fortuny | 0/0 | 3/3 | 3/6 | 0/0 | 0/3 | 0/3 |
| Patio Mallo | 9/14 | 0/0 | 9/14 | 1/9 | 0/0 | 1/9 |
| B. Drumen | 24/40 | 4/4 | 28/44 | 4/24 | 1/4 | 5/28 |
| B Avendaño | 16/28 | 0/0 | 16/28 | 3/16 | 0/0 | 3/16 |
| Total | 63/129 | 21/29 | 84/161 | 8/63 | 1/21 | 9/84 |
Although three sheep were censed none of them could be sampled. In Musola, Rilaja, Bombe, Moeri and Patio Mora, no animals were present.
Discussion
In order to investigate the presence of Trypanosoma brucei gambiense in Luba focus and its possible maintenance in a non-human transmission cycle, molecular diagnosis was performed on tsetse flies and peridomestic fauna. Our study has revealed the occurrence of one tsetse fly carrier of T. b. gambiense, demonstrating that parasite has not completely disappeared from the environment. Although only one individual was considered positive (prevalence ∼0.1%) this result is consistent with the typical low infection rate reached in the vector even in active foci [45], [46]. Regarding the domestic livestock no T. b. gambiense was detected, contrary to occur in other continental foci [28].
Prevalence of T. brucei s.l. was also determined in order to obtain an estimation of transmission activity in the focus. In tsetse flies, an overall high rate of infection was shown, although variations were observed regarding the village. A significantly higher tsetse flies infection rate was observed in Bococo Drumen from where it was gathered the majority of specimens collected in the focus during the study. In contrast, a relatively low prevalence of T. brucei s.l. in livestock was noticed, especially when compared with those previously described in continental foci [28]. Taking both data together it could be suggested that there is a high transmission activity, mainly in Bococo Drumen, but domestic fauna do not seem to act as the main feeding source for G. p. palpalis populations as in the other mainland foci.
A wild transmission cycle could explain all these epidemiological features: G. p. palpalis would mainly feed over wild fauna, which could lead to a high trypanosome infection rate of the vector and the maintenance of T. b. gambiense in the focus. Wild fauna would have a role as reservoir of T. b. gambiense, absent in peridomestic cycle, and it would be expected to show a higher prevalence for T. brucei s.l. than observed in livestock. In contrast with this situation, in Mbini focus (mainland Equatorial Guinea) domestic animals (sheeps and goats) have shown to be carriers of T. b. gambiense [28]. It should be pointed out that livestock breeding is more common in continental foci, where almost all villages have some kind of farming. In Mbini, around five hundred animals were censed in a previous study [28], whereas Luba only registered 161. A less availability of livestock could be other factor which favours the feeding preference of G. p. palpalis for wild fauna. Tsetse fly host preferences should be thoroughly studied in order to clarify this issue but the opportunistic feeding behaviour of this species described in several studies allows to hypothesize about a wild transmission cycle [47], [48]. Also, further research should be carried out in Luba to determine the role of wild animals in the maintenance of T. b. gambiense which has been previously described and discussed in neighbouring countries [15]–[17], [20], [22]–[24].
Some points about data must be added to this discussion. Firstly, the relative low sensitivity of the diagnostic technique employed for T. b. gambiense detection was previously reported since it targets TgsGP gene, only present once per haploid genome [49]. The low sensitivity of the test should not be a priori a serious drawback for tsetse flies samples since a great number of Trypanozoon subgenus parasites are usually found in infected midgut (around a maximum of 106) [50] but it should be taken into account when data from animal blood samples are analysed. On the other hand, not all domestic animals were sampled and, as a result, it cannot be categorically ruled out the presence of the parasite in these hosts. These considerations should lead to weigh up the alternative hypothesis of the maintenance of infection in domestic livestock even in the absent of positive samples. In favour of this theory, it is noteworthy that Bococo Drumen and Bococo Avendaño, the villages where the tsetse fly density was higher, show the majority of domestic animals too. However, the low T. brucei s.l. infection rate found in livestock contradicts this apparent correlation. Future studies narrowly focused in feeding preferences of tsetse flies in Luba could clarify this issue.
Entomological data were also gathered in order to better understand the epidemiological dynamic of the focus. Surprisingly, it was shown that only two out of ten villages sampled in the epicentre of Luba exhibited a high density of vector population. Almost 90% of collected flies belonged to B. Drumen and B. Avendaño. These villages registered a significantly higher AD levels than the others which showed AD values according to the data observed in mainland foci [30], [31]. Factors such as rural condition, a more isolated location, a suitable environmental for resting and breeding (cocoa and coffee plantations) and the absence of vector control activities may have contributed to the spreading of tsetse fly populations in these villages. Moreover, the presence of wild and domestic animal hosts in this remote area of the southern Luba district could be the most conditioning factor in the vector densities. A higher sex ratio (female/male) of tsetse flies was also noticed in B. Drumen and B. Avendaño while this rate was near 50% in the other villages sampled. In previous studies carried out in mainland foci, a seasonal variation of sex ratio was observed, being higher after a peak of G. p. palpalis density typically reached at the end of rainy seasons [30], [31]. The sampling of this study was carried out during that period in order to collect as many flies as possible for a more accurate analysis and then, a high female/male ratio was expected. This pattern is more noticeable in the two villages with a higher density of vector where population seems to be well established and follow the natural dynamic. On the other hand, the individuals caught in the second week were younger, suggesting that the removal of flies during the first week had an impact over population dynamic. This phenomenon was also noticed in previous studies in this focus [26], [27]. It is consistent with the known low reproductive rate of Glossina genus and its relatively small population sizes [34], [51], [52].
Vector control was performed in Luba during a few months in order to assess its utility for reducing the human – vector contact. It was later given up and control activities were focused in active screening of human cases and passive detection in the district hospital [5], [27]. The high cost and maintained efforts needed for vector control strategies make it unsuitable in conditions of very low human infection rate. Nevertheless, strategies such as active screening, chemoprophylaxis with drugs, treatment of infection or spraying animals with insecticides to prevent bites of tsetse flies would not be viable in a wild cycle and hence, vector control would be the only option for an indirect intervention at this level. A vector control campaign focused in the areas surrounding villages with higher density of tsetse fly could reduce the vector - fauna contact, enabling a permanent elimination of the parasite in the epidemiological cycle.
In the last two decades, successful control campaigns have been carried out in Luba. Its insular situation gives a degree of isolation which makes more difficult the reintroduction of new cases or infected vectors from neighbouring countries, condition which allowed the tsetse fly elimination in others islands such as Zanzibar and Principe [53]–[55]. Other foci in the mainland Equatorial Guinea, where the same control activities were undertaken, have showed a fall of reported patients but T. b. gambiense infection was never completely cleared and a constant drop of cases per year is currently being described [3]. Other factors, such as economical changes (mainly petroleum exploitation) and the subsequent abandon of rural activities such livestock breeding and agriculture, could have contributed to the exceptional success of these control campaigns in Luba.
The results of this study suggest interesting features about trypanosomiasis epidemiology in Luba focus. Several differences have been noticed with regards to the other foci of Equatorial Guinea. T. brucei s.l. prevalence in domestic animals is much lower in Luba and no positive T. b. gambiense samples were found. By contrast, T. brucei s.l. infection rate in tsetse flies was high which could be a signal of an intense transmission. Taking into account both data, the hypothesis of the wild fauna as an important feeding source of Glossina spp. and T. brucei s.l reservoir should be considered. Although the prevalence rate is very low, T. b. gambiense infection in tsetse fly also confirms the theory of the permanence of this parasite in Luba focus. It could be concluded that controlling HAT in a given focus is a complex aim and different approaches must be addressed; conventional active human screening is an efficient strategy to decrease the number of cases but other interventions (such as vectorial control and management of other reservoirs) could be assessed in order to ensure the elimination of the parasite.
In the past, Luba suffered the effects of the neglect of successful control activities leading to a resurgence beginning the 1980s after more than 20 years of apparent absence of the parasite [26]. Nowadays, with the improved epidemiological knowledge achieved by decades of experience fighting the sleeping sickness, resurgences of this disease could be avoidable.
Acknowledgments
We would like to thank the National Sleeping Sickness Control Programme, Ministry of Health and Social Welfare of the Republic of Equatorial Guinea, for its technical support during the study. We are particularly grateful to Dr. P. Anda and M. Rodríguez Vargas for technical advices and Dr. J. M. Bart for his helpful revision of the manuscript.
Footnotes
The authors have declared that no competing interests exist.
This study was funded by the Spanish International Cooperation Agency for Development (AECID) and the Institute of Health Carlos III (Ministry of Science and Innovation) within the Network of Tropical Diseases Research Centers (RICET R06/0021/0000). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Hoare CA. The trypanosomes of mammals. Oxford: Blackwell Scientific Publications; 1972. 749 [Google Scholar]
- 2.Gibson W. Resolution of the species problem in African trypanosomes. Int J Parasitol. 2007;37:829–38. doi: 10.1016/j.ijpara.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 3.WHO. Human African Trypanosomiasis (sleeping sickness): epidemiological update. Weekly Epidemiological Record. 2006:69–80. [PubMed] [Google Scholar]
- 4.Lutumba P, Robays J, Miaka mia BC, Mesu VK, Molisho D, et al. Trypanosomiasis control, Democratic Republic of Congo, 1993–2003. Emerg Infect Dis. 2005;11:1382–8. doi: 10.3201/eid1109.041020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Simarro PP, Franco JR, Ndongo P, Nguema E, Louis FJ, et al. The elimination of Trypanosoma brucei gambiense sleeping sickness in the focus of Luba, Bioko Island, Equatorial Guinea. Trop Med Int Health. 2006;11:636–46. doi: 10.1111/j.1365-3156.2006.01624.x. [DOI] [PubMed] [Google Scholar]
- 6.WHO. Control and Surveillance of African Trypanosomiasis. 1998. WHO Technical Report Series No. 881, Geneva.
- 7.Pittaluga G. 1910. [Report of the Mission of the Instituto Nacional de Higiene Alfonso XIII sent to Spanish territories in the Gulf of Guinea to study Sleeping Sickness]. Imprenta artística J. Bass y Cía, Madrid.
- 8.Courtin F, Jamonneau V, Duvallet G, Garcia A, Coulibaly B, et al. Sleeping sickness in West Africa (1906–2006): changes in spatial repartition and lessons from the past. Trop Med Int Health. 2008;13:334–44. doi: 10.1111/j.1365-3156.2008.02007.x. [DOI] [PubMed] [Google Scholar]
- 9.Laveissiere C, Courret D, Staak C, Hervouet JP. Glossina palpalis palpalis et ses hôtes en secteur forestier de Côte d'Ivoire. Relation avec l'épidémiologie de la tripanosomiase humaine. Cah ORSTOM, Sér Ent Med Parasitol. 1985;23:297–303. [Google Scholar]
- 10.Simo G, Mbida Mbida JA, Herder S, Njitchouang GR, Njiokou F. Feeding preferences of Tsetse flies from human african trypanosomosis foci of southern Cameroon. 2005. 28th Meeting ISCTRC Addis Ababa, Ethiopia.
- 11.Simo G, Cuny G, Demonchy R, Herder S. Trypanosoma brucei gambiense: Study of population genetic structure of Central African stocks using amplified fragment length polymorphism (AFLP). Exp Parasitol. 2008;118:172–80. doi: 10.1016/j.exppara.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 12.Truc P, Ravel S, Jamonneau V, N'Guessan P, Cuny G. Genetic variability within Trypanosoma brucei gambiense: evidence for the circulation of different genotypes in human African trypanosomiasis patients in Cote d'Ivoire. Trans R Soc Trop Med Hyg. 2002;96:52–5. doi: 10.1016/s0035-9203(02)90237-3. [DOI] [PubMed] [Google Scholar]
- 13.Koffi M, Solano P, Denizot M, Courtin D, Garcia A, et al. Aparasitemic serological suspects in Trypanosoma brucei gambiense human African trypanosomiasis: a potential human reservoir of parasites? Acta Trop. 2006;98:183–8. doi: 10.1016/j.actatropica.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 14.Louis FJ, Kohagne TL, Ebo'O EV, Simarro PP. [Organizing an active screening campaign for human african trypanosomiasis due to Trypanosoma brucei gambiense]. Med Trop (Mars ) 2008;68:11–6. [PubMed] [Google Scholar]
- 15.Herder S, Simo G, Nkinin S, Njiokou F. Identification of trypanosomes in wild animals from southern Cameroon using the polymerase chain reaction (PCR). Parasite. 2002;9:345–9. doi: 10.1051/parasite/2002094345. [DOI] [PubMed] [Google Scholar]
- 16.Njiokou F, Laveissiere C, Simo G, Nkinin S, Grebaut P, et al. Wild fauna as a probable animal reservoir for Trypanosoma brucei gambiense in Cameroon. Infect Genet Evol. 2006;6:147–53. doi: 10.1016/j.meegid.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 17.Njiokou F, Simo G, Nkinin SW, Laveissiere C, Herder S. Infection rate of Trypanosoma brucei s.l., T. vivax, T. congolense “forest type”, and T. simiae in small wild vertebrates in south Cameroon. Acta Trop. 2004;92:139–46. doi: 10.1016/j.actatropica.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 18.Njiokou F, Sima FO, Njitchouang GR, Nimpaye H, Cuny G, et al. Importance of domestic animal reservoir of Trypanosoma brucei gambiense in Cameroon. 2005. 28th Meeting ISCTRC Addis Ababa, Ethiopia.
- 19.Simo G, Asonganyi T, Nkinin SW, Njiokou F, Herder S. High prevalence of Trypanosoma brucei gambiense group 1 in pigs from the Fontem sleeping sickness focus in Cameroon. Vet Parasitol. 2006;139:57–66. doi: 10.1016/j.vetpar.2006.02.026. [DOI] [PubMed] [Google Scholar]
- 20.Guedegbe B, Verhulst A, Van MN, Pandey VS, Doko A. [Serological evidence of the existence of a wild reservoir of Trypanosoma brucei gambiense in the Pendjari biosphere reservation in the Republic of Benin]. Ann Soc Belg Med Trop. 1992;72:113–20. [PubMed] [Google Scholar]
- 21.Jamonneau V, Ravel S, Koffi M, Kaba D, Zeze DG, et al. Mixed infections of trypanosomes in tsetse and pigs and their epidemiological significance in a sleeping sickness focus of Cote d'Ivoire. Parasitology. 2004;129:693–702. doi: 10.1017/s0031182004005876. [DOI] [PubMed] [Google Scholar]
- 22.Makumyaviri A, Mehlitz D, Kageruka P, Kazyumba GL, Molisho D. [Animal reservoir hosts of Trypanosoma brucei gambiense in Zaire: trypanosome infections in two foci in Bas-Zaire]. Trop Med Parasitol. 1989;40:258–62. [PubMed] [Google Scholar]
- 23.Mehlitz D. Le reservoir Animal de la Maladie du Sommeil à Trypanosoma brucei gambiense. 1986. Etudes et Synthèses de L′I E M V T.
- 24.Noireau F, Paindavoine P, Lemesre JL, Toudic A, Pays E, et al. The epidemiological importance of the animal reservoir of Trypanosoma brucei gambiense in the Congo. 2. Characterization of the Trypanosoma brucei complex. Trop Med Parasitol. 1989;40:9–11. [PubMed] [Google Scholar]
- 25.Alvar J, Mas-Coma S, Carrasco M. Modern history and physical geography of Equatorial Guinea. Res Rev Parasitol. 1996;2–3:77–83. [Google Scholar]
- 26.Simarro PP, Mas J, Lancien J, Ona SF, Mateo MJ, et al. [Epidemiology of human trypanosomiasis in the Luba focus, in Equatorial Guinea]. Rev Sanid Hig Publica (Madr ) 1990;64:517–34. [PubMed] [Google Scholar]
- 27.Simarro PP, Sima FO, Mir M, Mateo MJ, Roche J. [Control of human African trypanosomiasis in Luba in equatorial Guinea:evaluation of three methods]. Bull World Health Organ. 1991;69:451–7. [PMC free article] [PubMed] [Google Scholar]
- 28.Cordon-Obras C, Berzosa P, Ndong-Mabale N, Bobuakasi L, Buatiche JN, et al. Trypanosoma brucei gambiense in domestic livestock of Kogo and Mbini foci (Equatorial Guinea). Trop Med Int Health. 2009;14:535–41. doi: 10.1111/j.1365-3156.2009.02271.x. [DOI] [PubMed] [Google Scholar]
- 29.Gouteux JP, Lancien J. [The pyramidal trap for collecting and controlling tsetse flies (Diptera: Glossinidae). Comparative trials and description of new collecting technics]. Trop Med Parasitol. 1986;37:61–6. [PubMed] [Google Scholar]
- 30.Cano J, Descalzo MA, Ndong-Mabale N, Ndongo-Asumu P, Bobuakasi L, et al. Spatial and temporal variability of the Glossina palpalis palpalis population in the Mbini focus (Equatorial Guinea). Int J Health Geogr. 2007;6 doi: 10.1186/1476-072X-6-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cano J, Descalzo MA, Ndong-Mabale N, Ndong-Asumu P, Bobuakasi L, et al. Predicted distribution and movement of Glossina palpalis palpalis (Diptera: Glossinidae) in the wet and dry seasons in the Kogo trypanosomiasis focus (Equatorial Guinea). J Vector Ecol. 2007;32:218–25. doi: 10.3376/1081-1710(2007)32[218:pdamog]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 32.Sane B, Laveissiere C, Meda HA. [Diversity of feeding behavior of Glossina palpalis palpalis in the forest belt of the Ivory Coast: relation to the prevalence of human African trypanosomiasis]. Trop Med Int Health. 2000;5:73–8. doi: 10.1046/j.1365-3156.2000.00488.x. [DOI] [PubMed] [Google Scholar]
- 33.Spath J. Feeding patterns of three sympatric tsetse species (Glossina spp.) (Diptera: Glossinidae) in the preforest zone of Cote d'Ivoire. Acta Trop. 2000;75:109–18. doi: 10.1016/s0001-706x(99)00096-0. [DOI] [PubMed] [Google Scholar]
- 34.Kuzoe FAS, Schofield CJ. 2004. Strategic review of traps and targets for tsetse and African Trypanosomiasis control. Report of Special Programme for Research and Training in Tropical Disease (TDR) TDR/IDE/TRY/05.1.
- 35.Brunhes J, Cuisance D, Geoffroy B, Hervy JP, Lebbe J. Les glossines ou mouches tsé-tsé. Logiciel d'identification. Glossine Expert. Manuel illustré d'utilisation. VI, ORSTOM, Paris: Université Paris; 1998. [Google Scholar]
- 36.Jackson CN. An artificially isolated generation of tsetse flies (Diptera). Bull Entomol Res. 1946;37:291. doi: 10.1017/s0007485300022203. [DOI] [PubMed] [Google Scholar]
- 37.Laveissiere C, Penchenier L. Manuel de lutte contre la maladie du sommeil en Afrique centrale & occidentale. 2000. Ed OCEAC (IRD) Vol 5 Lutte Antivectorielle, Yaoundé, Cameroun.
- 38.Walsh PS, Metzger DA, Higuchi R. Chelex 100 as a medium for simple extraction of DNA for PCR-based typing from forensic material. Biotechniques. 1991;10:506–13. [PubMed] [Google Scholar]
- 39.Ravel S, Mariani C, Grebaut P, Jamonneau V, Cuisance D, et al. Inhibition of the DNA amplification of trypanosomes present in tsetse flies midguts: implications for the identification of trypanosome species in wild tsetse flies. Parasite. 2004;11:107–9. doi: 10.1051/parasite/2004111107. [DOI] [PubMed] [Google Scholar]
- 40.Moser DR, Cook GA, Ochs DE, Bailey CP, McKane MR, et al. Detection of Trypanosoma congolense and Trypanosoma brucei subspecies by DNA amplification using the polymerase chain reaction. Parasitology. 1989;99 Pt 1:57–66. doi: 10.1017/s0031182000061023. [DOI] [PubMed] [Google Scholar]
- 41.Radwanska M, Claes F, Magez S, Magnus E, Perez-Morga D, et al. Novel primer sequences for polymerase chain reaction-based detection of Trypanosoma brucei gambiense. Am J Trop Med Hyg. 2002;67:289–95. doi: 10.4269/ajtmh.2002.67.289. [DOI] [PubMed] [Google Scholar]
- 42.Morrison LJ, Tait A, McCormack G, Sweeney L, Black A, et al. Trypanosoma brucei gambiense Type 1 populations from human patients are clonal and display geographical genetic differentiation. Infect Genet Evol. 2008;8:847–54. doi: 10.1016/j.meegid.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 43.Hao Z, Kasumba I, Aksoy S. Proventriculus (cardia) plays a crucial role in immunity in tsetse fly (Diptera: Glossinidiae). Insect Biochem Mol Biol. 2003;33:1155–64. doi: 10.1016/j.ibmb.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 44.Ferreira F, Cano J, Furtado A, Ndong-Mabale N, Ndong-Asumu P, et al. An alternative approach to detect Trypanosoma in Glossina (Diptera, Glossinidae) without disection. J Infect Developing Countries. 2008;1:63–7. doi: 10.3855/jidc.324. [DOI] [PubMed] [Google Scholar]
- 45.Jordan AM. Recent developments in the ecology and methods of control of tsetse flies (Glossina spp.) (Diptera, Glossinidae). Bull Entomol Res. 1974:361–99. [Google Scholar]
- 46.Dagnogo M, Traore G, Souleymane F. Determination of sleeping sickness transmission risk areas from trypanosome infection rates of tsetse flies in Daloa, Côte. d'Ivoire. Int J Trop Insect Sci. 2004:170–6. [Google Scholar]
- 47.Clausen PH, Adeyemi I, Bauer B, Breloeer M, Salchow F, et al. Host preferences of tsetse (Diptera: Glossinidae) based on bloodmeal identifications. Med Vet Entomol. 1998;12:169–80. doi: 10.1046/j.1365-2915.1998.00097.x. [DOI] [PubMed] [Google Scholar]
- 48.Simo G, Njiokou F, Mbida Mbida JA, Njitchouang GR, Herder S, et al. Tsetse fly host preference from sleeping sickness foci in Cameroon: epidemiological implications. Infect Genet Evol. 2008;8:34–9. doi: 10.1016/j.meegid.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 49.Berberof M, Perez-Morga D, Pays E. A receptor-like flagellar pocket glycoprotein specific to Trypanosoma brucei gambiense. Mol Biochem Parasitol. 2001;113:127–38. doi: 10.1016/s0166-6851(01)00208-0. [DOI] [PubMed] [Google Scholar]
- 50.Gibson W. Species-specific probes for the identification of the African tsetse-transmitted trypanosomes. Parasitology. 2009:1–7. doi: 10.1017/S0031182009006179. [DOI] [PubMed] [Google Scholar]
- 51.Rogers D. Tsetse population dynamics and distribution: a new analytical approach. J Anim Ecol. 1979;48:825–49. [Google Scholar]
- 52.Hargrove J. Tsetse: the limits to population growth. Med Vet Entomol. 1988;2:203–17. doi: 10.1111/j.1365-2915.1988.tb00184.x. [DOI] [PubMed] [Google Scholar]
- 53.Vreysen MJ, Saleh KM, Ali MY, Abdulla AM, Zhu ZR, et al. Glossina austeni (Diptera: Glossinidae) eradicated on the island of Unguja, Zanzibar, using the sterile insect technique. J Econ Entomol. 2000;93:123–35. doi: 10.1603/0022-0493-93.1.123. [DOI] [PubMed] [Google Scholar]
- 54.Da Costa B. Sleeping sickness, a record of four years war against it in Principe, Portuguese West Africa. London: Ballière, Tindall and Cox editors; 1916. 300 [Google Scholar]
- 55.De Raadt P. The history of sleeping sickness. In: Gilles HM, editor. Protozoal diseases. London: Arnold; 1999. [Google Scholar]