Abstract
Objectives. We assessed the prevalence and predictors of past-year unmet needs for 5 types of health care services in a national sample of homeless adults.
Methods. We analyzed data from 966 adult respondents to the 2003 Health Care for the Homeless User Survey, a sample representing more than 436 000 individuals nationally. Using multivariable logistic regression, we determined the independent predictors of each type of unmet need.
Results. Seventy-three percent of the respondents reported at least one unmet health need, including an inability to obtain needed medical or surgical care (32%), prescription medications (36%), mental health care (21%), eyeglasses (41%), and dental care (41%). In multivariable analyses, significant predictors of unmet needs included food insufficiency, out-of-home placement as a minor, vision impairment, and lack of health insurance. Individuals who had been employed in the past year were more likely than those who had not to be uninsured and to have unmet needs for medical care and prescription medications.
Conclusions. This national sample of homeless adults reported substantial unmet needs for multiple types of health care. Expansion of health insurance may improve health care access for homeless adults, but addressing the unique challenges inherent to homelessness will also be required.
An estimated 2.3 to 3.5 million Americans experience homelessness each year.1 The health problems of homeless people are broad and multidimensional, contributing to excess mortality.2–7 Rates of acute and chronic medical illness are high, in many cases surpassing those of the general population.8–15 More than half of homeless people have a history of mental illness, and the burden of drug and alcohol use is substantial.8,9 Clinically significant dental problems have been identified in two thirds of homeless individuals,8 and nearly 40% have functional vision impairments.16
Homeless people also experience poor access to health care,17–21 leading to delayed clinical presentation,12 increased reliance on emergency departments,22 and higher rates of hospitalization,23 often for preventable conditions.24 Yet, the extent to which homeless adults are able to obtain health care across the spectrum of health needs just described is largely unknown. Existing knowledge is based primarily on studies of single cities25,26 or single types of unmet need21,27; very few national surveys have adequately captured this difficult-to-reach population.
We used data from a unique national survey of homeless adults to determine the prevalence and predictors of unmet need for 5 types of health services, chosen to reflect multiple domains of health care access.28 A comprehensive assessment of the unmet health care needs of homeless people can inform policy and practice decisions about how to better provide care to this vulnerable population.
METHODS
We conducted a secondary analysis of the 2003 Health Care for the Homeless (HCH) User Survey, the first nationally representative survey of individuals using clinical services provided by the federally funded HCH program. The HCH program serves more than 700 000 people annually through 205 grantees in all 50 states, the District of Columbia, and Puerto Rico.29 The HCH User Survey was administered by Research Triangle Institute (RTI) International in collaboration with the Health Resources and Services Administration's Bureau of Primary Health Care.
Participants and Setting
A 3-stage sampling design was used to conduct the survey.30 A geographically stratified probability-proportional-to-size (PPS) technique was used to sample 30 HCH grantees. Interviews were conducted in person by RTI field staff at a PPS sample of 79 clinic sites that were operated by the 30 grantees. The target population consisted of individuals receiving face-to-face services from an HCH provider. Individuals were eligible if they had received such services at least once in the year prior to the survey, given that the reference period for many of the questions was 12 months. Participants were selected consecutively with a goal of 33 interviews per grantee.
Of 1444 selected individuals, 11 were subsequently found to be ineligible, and 416 refused or did not complete the survey. The total number of completed interviews was 1017, yielding a response rate of 70%. We confined our analysis to the 966 respondents who were aged 18 years or older.
Conceptual Framework
The behavioral model for vulnerable populations was the conceptual framework for our analysis.16 In this framework, realized access to health care can be viewed as a function of predisposing, enabling, and need factors. Predisposing factors are characteristics that influence a person's propensity for seeking health care services. Enabling factors are those that facilitate or impede health care access and use. Need factors are health conditions for which a person is likely to require care.
Outcomes
Our study outcomes were 5 past-year measures of unrealized access to health care, framed as having an unmet need for the following services: medical or surgical care, prescription medications, mental health care or counseling, eyeglasses, and dental care. These measures were all assessed in similar ways, with questions generally phrased as follows: “During the past 12 months, was there a time when you wanted medical care or surgery but could not get it at that time?” Unmet needs represent important measures of health care access and are frequently used as outcome variables in health services research.25–28,31–40
Predisposing Factors
Predisposing variables included age (18–29 years, 30–44 years, 45 years or older), gender, self-reported race/ethnicity (categorized as White, non-Hispanic; Black, non-Hispanic; and Hispanic/other), marital status (married/partnered vs not married/partnered), educational attainment (high school diploma or higher vs less than high school), out-of-home placement as a minor (foster home, group home, or other institutional placement before 18 years of age), veteran status, number of homeless episodes at least 30 days in duration (dichotomized at the median, 0–1 vs 2 or more), past-year victimization (physical or sexual assault while homeless), and past-year problem alcohol use or illicit drug use.
Past-year problem alcohol use was defined as consuming 5 or more drinks on a single occasion in the preceding month,41 consuming 3 or more drinks on a typical day of drinking in the preceding month,42 or any past-year alcohol treatment. Past-year drug use was defined as any past-year use of illicit or nonprescribed controlled substances or any past-year drug treatment.
Enabling Factors
Enabling variables included usual source of care, insurance status, past-year employment, and food insufficiency. We defined a usual source of care as any single “place that you usually go when you are sick or you need advice about your health.” Adults reporting no usual care source, multiple sources without a single predominant source, or an emergency department as a usual care source were classified as lacking a usual source of care. Types of insurance coverage were categorized as public, private, military/veterans, and other; insurance status was dichotomized as insured or uninsured in the multivariable analyses.
Past-year employment was defined as any work for pay in the preceding year. We considered this variable in the enabling domain because employment demands may not allow for medical visits. Food insufficiency was defined as “sometimes” or “often” not getting enough food to eat.43–48
Need Factors
Need variables consisted of the number of self-reported medical comorbidities (0, 1, 2 or more), including hypertension, diabetes, cardiovascular disease (coronary artery disease or stroke), obstructive lung disease (asthma or chronic obstructive pulmonary disease), HIV infection, cancer, liver disease, kidney disease, and arthritis or chronic joint pain.
Consistent with the behavioral model, mental illness was considered a need factor in predicting mental health care access and a predisposing variable with respect to all other components of unmet need.16 Mental illness history was defined as any past inpatient or outpatient treatment of “emotional or mental problems.”
We considered self-reported vision impairment as a need factor in the model examining receipt of eyeglasses and as an enabling factor in all other models given the potential impact of impaired vision on mobility, navigating health systems, and collecting health information.49,50 Adults who reported trouble seeing, even while wearing glasses or contact lenses, were classified as having vision impairment. Past-year tooth or gum problem was analyzed as a need factor in the dental care model only.
Statistical Analysis
We used the χ2 test to determine the unadjusted relationships between predictor and outcome variables. We then constructed 5 multivariable logistic regression models to determine the factors independently associated with each outcome measure of unmet need among all adults. Multivariable model covariates were chosen on the basis of clinical context and hypotheses generated from the behavioral model for vulnerable populations. Participants with missing data for a model variable were excluded from any analysis involving that variable. Item nonresponse was generally minimal (range = 0%–3.6%; median = 0.6%).
Because individuals with medical comorbidities may be at higher risk of needing medical care or prescription medications and experiencing complications when such needs are unmet, we conducted subgroup analyses among those with at least one medical condition, adjusted for the same set of confounders used in the original models. Similarly, we analyzed the outcome of unmet mental health care need for the entire study sample as well as for a composite subgroup of those with any history of mental illness, past-year illicit drug or problem alcohol use, or past-year victimization, given that such individuals may be more likely to require this service.51,52
In addition, we explored the correlates of lack of health insurance coverage because insurance has been shown to be an important determinant of access to care among homeless people.21,53–55 Because employer-based health insurance remains the primary mode of coverage in the United States,56 we examined the insurance patterns of respondents with any past-year employment to determine whether those engaging in work received health insurance benefits for doing so.
As a result of the complex sampling design of the survey, all analyses were performed on SAS-Callable SUDAAN version 10.0 (RTI, Research Triangle Park, NC). We used weights developed by RTI that incorporated sampling probability, survey nonresponse, and poststratification adjustment to reduce bias in the study estimates and better reflect the target population. Descriptive data are presented as unweighted numbers and weighted percentages. Results were considered significant at P < .05.
RESULTS
The characteristics of the 966 adult respondents to the HCH User Survey are shown in Table 1. The study sample was representative of more than 436 000 adult HCH clinic users nationally.
TABLE 1.
Characteristics of the Study Sample (n = 966): Health Care for the Homeless User Survey, 2003
| No. (Weighted %)a | |
| Predisposing factors | |
| Age, y | |
| 18–29 | 113 (18.3) |
| 30–44 | 395 (50.3) |
| ≥ 45 | 458 (31.5) |
| Male | 591 (58.2) |
| Race/ethnicity | |
| White, non-Hispanic | 334 (39.2) |
| Black, non-Hispanic | 382 (38.1) |
| Hispanic/other | 238 (21.4) |
| Veteran | 119 (11.5) |
| Married/partnered | 127 (14.3) |
| High school diploma or higher | 580 (58.7) |
| Out-of-home placement as a minorb | 204 (23.8) |
| No. of homeless episodes 30 d or more in duration | |
| 0–1 | 447 (43.2) |
| ≥ 2 | 498 (55.3) |
| Physical or sexual assault in past year | 176 (20.1) |
| Substance abuse in past year | |
| Illicit drug use only | 240 (25.1) |
| Problem alcohol use only | 105 (9.0) |
| Both drug and alcohol use | 276 (30.7) |
| Mental illness history | 429 (47.6) |
| Enabling factors | |
| No usual source of care | 63 (8.3) |
| Health insurance coveragec | |
| No health insurance | 536 (59.5) |
| Public insurance | 366 (34.3) |
| Private insurance | 51 (4.7) |
| Military/veterans insurance | 16 (1.2) |
| Other insurance | 15 (1.8) |
| Employment in past year | 485 (54.5) |
| Food insufficiencyd | 235 (25.4) |
| Vision impairment | 302 (26.2) |
| Need factors | |
| No. of medical comorbiditiese | |
| 0 | 210 (22.2) |
| 1 | 276 (31.2) |
| ≥ 2 | 471 (45.9) |
| Dental problem in past year | 332 (31.1) |
Presented as unweighted numbers and weighted percentages, via sampling weights provided by Research Triangle Institute International. Percentages may not sum to 100 as a result of rounding or item nonresponse.
Defined as placement into foster care, a group home, or an institution before the age of 18 years.
Percentage total exceeds 100 because respondents were allowed to specify more than 1 type of health insurance coverage.
Defined as “sometimes” or “often” not getting enough food to eat.
Medical comorbidities included hypertension, diabetes, cardiovascular disease (coronary artery disease or stroke), obstructive lung disease (asthma or chronic obstructive pulmonary disease), HIV infection, cancer, kidney disease, liver disease, and arthritis or chronic joint problems.
Predisposing, Enabling, and Need Factors
Fifty-eight percent of the respondents were male (Table 1). The median age of the sample was 41 years. Most participants were White (39%) or Black (38%) non-Hispanics. Nearly one fourth had a history of out-of-home placement as a minor. One fifth reported past-year victimization while homeless.
Sixty percent of the respondents were uninsured. More than half reported any past-year employment. One fourth of the respondents had experienced food insufficiency.
Forty-six percent of the participants reported 2 or more medical conditions. Almost half (48%) reported a history of treatment of mental illness. Twenty-six percent reported difficulty seeing, and more than 30% reported a past-year dental problem.
Unmet Health Care Needs
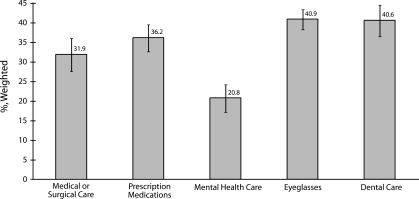
Overall, 32% (n = 284) of the respondents reported an unmet need for medical or surgical care in the preceding year, 36% (n = 335) reported an unmet need for prescription medications, 21% (n = 219) reported an unmet need for mental health care or counseling, 41% (n = 375) reported an unmet need for eyeglasses, and 41% (n = 378) reported an unmet need for dental care (Figure 1). Seventy-three percent (n = 685) reported at least 1 past-year unmet health care need, and 49% (n = 457) reported 2 or more unmet needs. The most frequently cited reasons for each type of unmet need were inability to afford care and lack of health insurance coverage.
FIGURE 1.
Prevalence of past-year unmet health care needs among homeless US adults (n = 966): Health Care for the Homeless User Survey, 2003.
Note. Percentages were weighted with sampling weights provided by Research Triangle Institute International. Tick marks indicate the bounds of 1 standard error.
Medical or surgical care.
Fifty-one percent of adults with a childhood history of out-of-home placement reported an unmet need for medical or surgical care, as compared with 26% of those without such a history (P < .001). Forty-six percent of respondents experiencing food insufficiency had an unmet need for care, whereas 27% without food insufficiency had such difficulty (P = .001). Any past-year employment (P = .001) and lack of insurance coverage (P = .01) were also significantly associated with this outcome in unadjusted analyses. Among those with one or more medical comorbidities, 36% had an unmet need for care. In the multivariable analysis, factors independently associated with having an unmet need for medical or surgical care in the preceding year included out-of-home placement as a minor, past-year employment, food insufficiency, lack of health insurance coverage, and presence of any medical comorbidities (Table 2).
TABLE 2.
Factors Associated With Past-Year Unmet Need for Medical or Surgical Care, Prescription Medications, Mental Health Care, Eyeglasses, and Dental Care Among Homeless US Adults: Health Care for the Homeless User Survey, 2003
| Unmet Need for Medical or Surgical Care, AOR (95% CI)a | Unmet Need for Prescription Medications, AOR (95% CI)a | Unmet Need for Mental Health Care, AOR (95% CI)a | Unmet Need for Eyeglasses, AOR (95% CI)a | Unmet Need for Dental Care, AOR (95% CI)a | |
| Predisposing factors | |||||
| Age, y | |||||
| 18–29 (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 30–44 | 1.04 (0.42, 2.57) | 2.71* (1.20, 6.13) | 1.61 (0.47, 5.53) | 0.94 (0.51, 1.73) | 1.21 (0.38, 3.87) |
| ≥ 45 | 1.20 (0.58, 2.52) | 2.80* (1.47, 5.34) | 1.11 (0.38, 3.21) | 1.66 (0.97, 2.84) | 0.96 (0.34, 2.70) |
| Male | 0.91 (0.34, 2.42) | 0.86 (0.36, 2.03) | 0.57 (0.32, 1.02) | 0.60 (0.35, 1.03) | 0.72 (0.47, 1.09) |
| Race/ethnicity | |||||
| White, non-Hispanic (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Black, non-Hispanic | 0.90 (0.60, 1.35) | 0.52 (0.25, 1.09) | 1.28 (0.75, 2.20) | 0.80 (0.45, 1.44) | 1.38 (0.81, 2.34) |
| Hispanic/other | 1.00 (0.47, 2.13) | 0.61 (0.29, 1.30) | 2.03* (1.17, 3.51) | 0.63 (0.29, 1.36) | 1.63 (0.77, 3.45) |
| Veteran | 1.76* (1.14, 2.70) | 0.74 (0.29, 1.85) | 0.71 (0.22, 2.33) | 2.00 (0.90, 4.44) | 1.42 (0.85, 2.38) |
| Married/partnered | 0.83 (0.43, 1.60) | 0.78 (0.41, 1.48) | 0.08* (0.02, 0.28) | 1.13 (0.51, 2.47) | 0.98 (0.49, 1.97) |
| High school diploma or higher | 1.07 (0.52, 2.18) | 1.06 (0.47, 2.40) | 1.25 (0.59, 2.65) | 0.58* (0.35, 0.95) | 1.05 (0.62, 1.76) |
| Out-of-home placement as minorb | 2.52* (1.80, 3.52) | 1.71* (1.08, 2.73) | 1.44 (0.77, 2.68) | 1.10 (0.63, 1.91) | 0.90 (0.54, 1.50) |
| Two or more homeless episodes at least 30 d in duration | 0.92 (0.65, 1.29) | 0.85 (0.49, 1.47) | 0.95 (0.49, 1.83) | 1.17 (0.70, 1.95) | 1.26 (0.72, 2.20) |
| Physical/sexual assault in past year | 0.91 (0.49, 1.67) | 2.26* (1.44, 3.55) | 1.97* (1.13, 3.42) | 1.22 (0.78, 1.93) | 0.77 (0.38, 1.54) |
| Substance abuse in past year | 0.96 (0.40, 2.31) | 1.06 (0.56, 2.01) | 1.10 (0.68, 1.77) | 1.26 (0.82, 1.96) | 1.36 (0.76, 2.43) |
| Mental illness history | 1.18 (0.51, 2.76) | 1.79 (0.91, 3.51) | 2.58* (1.27, 5.23) | 1.83* (1.14, 2.93) | 1.04 (0.53, 2.04) |
| Enabling factors | |||||
| No usual source of care | 1.72 (0.98, 3.04) | 2.16 (0.79, 5.88) | 3.36* (1.92, 5.89) | 0.89 (0.38, 2.07) | 1.17 (0.47, 2.92) |
| Uninsured | 1.75* (1.14, 2.69) | 1.94* (1.26, 3.00) | 2.03* (1.08, 3.82) | 1.72* (1.10, 2.67) | 1.08 (0.58, 1.99) |
| Employment in past year | 1.70* (1.22, 2.37) | 1.60* (1.09, 2.35) | 0.84 (0.45, 1.57) | 1.48 (0.87, 2.52) | 1.22 (0.75, 2.00) |
| Food insufficiencyc | 2.06* (1.19, 3.57) | 1.61* (1.04, 2.50) | 1.55* (1.02, 2.38) | 1.11 (0.58, 2.13) | 1.06 (0.65, 1.72) |
| Vision impairment | 1.11 (0.59, 2.09) | 1.48 (0.86, 2.56) | 2.17* (1.17, 4.01) | 1.88* (1.16, 3.04) | 1.81* (1.25, 2.63) |
| Need factors | |||||
| No. of medical comorbiditiesd | |||||
| 0 (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1 | 2.22* (1.08, 4.52) | 1.46 (0.88, 2.44) | 1.57 (0.70, 3.56) | 1.47 (0.93, 2.32) | 1.07 (0.63, 1.83) |
| ≥ 2 | 3.44* (1.61, 7.36) | 2.82* (1.39, 5.73) | 1.85 (0.61, 5.57) | 1.63 (0.89, 2.97) | 1.20 (0.57, 2.54) |
| Dental problem in past year | … | … | … | … | 2.97* (1.89, 4.67) |
Note. AOR = adjusted odds ratio; CI = confidence interval. Ellipses indicate that the factor was not applicable for that need.
Adjusted for all of the variables presented, via multivariable logistic regression.
Defined as placement into foster care, a group home, or an institution before the age of 18 years.
Defined as “sometimes” or “often” not getting enough food to eat.
Medical comorbidities included hypertension, diabetes, cardiovascular disease (coronary artery disease or stroke), obstructive lung disease (asthma or chronic obstructive pulmonary disease), HIV infection, cancer, kidney disease, liver disease, and arthritis or past-year chronic joint problems.
*P < .05.
Prescription medications.
In the multivariable analysis, factors independently associated with an unmet need for prescription medications included age, out-of-home placement as a minor, past-year victimization, past-year employment, food insufficiency, lack of health insurance coverage, and presence of 2 or more medical comorbidities (Table 2).
Mental health care.
In the multivariable analysis, factors independently associated with an unmet need for mental health care included past-year victimization, food insufficiency, lack of a usual source of care, lack of health insurance coverage, mental illness history, and vision impairment (Table 2).
High-risk subgroup analyses.
The overall pattern of results was unchanged when we confined the analyses of unmet need for medical or surgical care and prescription medications to those with at least one medical comorbidity (n = 754; see the table available as an online supplement to this article at http://www.ajph.org). Out-of-home placement as a minor, past-year employment, food insufficiency, and lack of health insurance coverage remained important predictors of both outcomes. In the composite subgroup of individuals with a history of mental illness, past-year substance abuse, or past-year victimization (n = 756), the predictors of unmet need for mental health care were very similar to those seen for the entire sample (see the table available as an online supplement to this article).
Eyeglasses and dental care.
Unadjusted rates of unmet need for eyeglasses were higher among adults with a history of mental illness (P < .001), out-of-home placement as a minor (P = .04), or any past-year employment (P = .03). Among those with symptoms of vision impairment, 56% reported an unmet need for eyeglasses. Sixty percent of those with a past-year dental problem reported an unmet need for dental care.
In the multivariable models, lack of health insurance coverage was associated with an unmet need for eyeglasses (Table 2). Vision impairment predicted unmet needs for both eyeglasses and dental care.
Insurance patterns of workers.
Adults with any past-year employment were significantly more likely to be uninsured than those who had not been employed (68% vs 49%; P < .001). In the multivariable analysis adjusted for all of the confounders previously discussed, any past-year employment was a significant independent predictor of lack of insurance coverage (adjusted odds ratio = 2.05; 95% confidence interval = 1.43, 2.94), and increasing duration of past-year employment was associated with increasing odds of lack of insurance coverage (Table 3). Respondents who had worked more than half of the preceding year were significantly less likely than were those who had not worked to have any type of public insurance (20% vs 43%; P = .02) and trended toward having lower rates of private insurance (2.8% vs 6.6%; P = .14); only 0.5% of these workers had employer-based health insurance, and 75% were uninsured.
TABLE 3.
Adjusted odds ratios (AORs) for lack of health insurance coverage, by extent of past-year employment: 2003 Health Care for the Homeless User Survey.
| AOR (95% CI) | |
| Duration of employment in the past year | |
| No employment (Ref) | 1.00 |
| 1–3 mo | 1.66 (1.01, 2.72) |
| 4–6 mo | 2.15 (1.26, 3.68) |
| ≥ 7 mo | 2.70 (1.37, 5.32) |
Note. CI = confidence interval. Odds ratios were adjusted, via multivariable logistic regression, for age, gender, race/ethnicity, veteran status, marital status, education, out-of-home placement as a minor, number of homeless episodes, past-year victimization, past-year substance abuse, history of mental illness, usual source of care, food insufficiency, vision impairment, and medical comorbidities.
DISCUSSION
This national sample of homeless adults reported substantial barriers to accessing multiple dimensions of health care. Nearly three quarters of the respondents had at least 1 past-year unmet health care need, and almost half had 2 or more unmet needs. Rates of unmet needs for specific services were 6 to 10 times higher than in the US general population.39,57 Our findings appear similar to prior estimates of unmet health need among homeless populations,21,25–27 although direct comparisons are limited by varying methodologies in terms of definitions and measurement of unmet need. Our findings may represent conservative estimates of the unmet health needs of homeless people, given that all participants had been seen in a clinic at least once in the preceding year.
The majority of respondents were uninsured, and this factor was independently associated with unmet needs for medical or surgical care, prescription medications, mental health care, and eyeglasses, but not dental care. This pattern of findings reflects the Medicaid coverage profile for adults in most states58,59 and reinforces prior evidence that health insurance is a key determinant of access to care among both homeless21,53–55 and housed32,60–62 individuals.
Competing priorities represented substantial barriers to care as well. Food insufficiency was associated with impaired access to medical or surgical care, prescription medications, and mental health care. Although prior research has linked food insufficiency with higher rates of medical and mental illness,46 our multivariable analyses demonstrated significant relationships with unmet needs that were independent of these comorbidities. Individuals experiencing food insufficiency may assign lower priority to health care in favor of directing personal resources toward the fulfillment of basic needs.20,63,64
We also found that past-year employment was associated with unmet needs for medical or surgical care and prescription medications. This result confirms the clinical observation that when employment is the sole source of income in the setting of poverty, patients often prioritize work over health care. Because work engaged in by homeless individuals is often day labor or is intermittent in nature,9 the hours may be unpredictable and the consequences for absence (i.e., termination or replacement) unacceptable. Furthermore, health insurance benefits are often not included with these low-wage jobs.65–67 The 68% uninsured rate among past-year workers in our study was more than 3 times higher than was that for workers in the general population.68 Those with any past-year employment were much more likely than were their unemployed counterparts to be uninsured, and the odds of lacking insurance increased with the duration of employment.
Rates of public insurance coverage were significantly lower among respondents with more extensive work histories than among nonworkers, probably reflecting a lesser degree of disability. This finding was not counterbalanced by higher rates of private insurance, and very few of these workers had employer-based coverage. Homeless workers may fall in a gap in which they do not qualify for publicly sponsored health benefits yet are unable to afford private health insurance if employer-based coverage is not provided.
Out-of-home placement as a minor conferred higher odds of having an unmet need for medical or surgical care and prescription medications in this study of homeless adults. Rates of homelessness, unemployment, mental illness, substance abuse, victimization, and lack of health insurance coverage are high among individuals with a history of foster care69–75; our findings remained significant even after adjustment for these confounders. The experience of out-of-home placement may be associated with several other risk factors for poor health and access to care, including adverse childhood experiences, high rates of incarceration, civic nonengagement, and poor life skill preparation, resulting in difficult community transitions.71 Although federal funding for transitional assistance increased under the 1999 Foster Care Independence Act (HR 3443), evidence suggests that only 60% of eligible foster youths receive such services.76
Vision impairment was independently related to unmet needs for mental health care, eyeglasses, and dental care. Although the relationship with poor access to eyeglasses is probably explained in part by greater need for such services, we hypothesize that impaired vision also affects one's ability to navigate health systems and acquire health information.49,50 This impairment may impose a greater barrier to accessing more ancillary services such as mental health care, vision care, and dental care, which often entail unique referral systems and less familiar facilities.
Limitations
Our study involved certain limitations. The data analyzed were cross sectional in nature, so causality cannot be definitively determined. All measures were self-reported and may be subject to multiple biases, particularly with respect to sensitive issues and stigmatized behaviors. We defined mental illness as having ever received treatment for emotional or mental problems, a definition similar to that used in other studies of homeless people.22,77 To the extent that this definition identifies individuals who have previously accessed mental health care, the unmet need results for this variable may be biased toward the null and therefore represent a conservative estimate of effect. The survey was conducted among individuals with at least 1 prior visit to an HCH clinic site, so the findings may not be generalizable to the homeless population as a whole, particularly those who do not use HCH services.
In addition, our outcome measure of unmet need was based on a question format with some limitations. Although widely used, the question format of needing but being unable to obtain a given type of service is double barreled. Those with greater need for care are at increased risk of responding affirmatively to the question as compared with those with less or no perceived need. We addressed this limitation in 2 ways. First, we adjusted for need factors in our modeling strategy to ensure that significant predictors were not simply surrogate markers of increased need. Second, we performed subgroup analyses limited to those at high risk for requiring medical care, prescription medications, and mental health care and found that the results were very similar. Finally, because the study outcomes were relatively common (occurring among more than 10% of the respondents in each case), the adjusted odds ratios provide valid but potentially exaggerated measures of association in comparison with risk ratios, and the magnitude of findings should be interpreted accordingly.
Despite these limitations, this is the first national study of which we are aware to describe the multiple dimensions of unmet need for health care among homeless persons. Our findings reinforce prior research on the importance of health insurance in homeless populations, add to the growing literature on food insufficiency in a novel way, extend the principle of competing priorities to include employment, expand understanding of the sequelae of childhood out-of-home placement in homeless adults, and describe the contribution of low vision to poor health care access in the setting of homelessness.
Conclusions
We found high rates of unmet need for health care services in this national study of homeless adult clinic users. Unmet needs were most consistently related to being uninsured, but other factors appeared important as well, including out-of-home placement as a minor, food insufficiency, employment, and vision impairment. As currently structured, employer-based health insurance fails to reach the majority of homeless individuals who work, highlighting the need for an alternative source of affordable health coverage. Given the deficit of emergency food supplies,78 provision of adequate food services to the poor should continue to be a public health priority. In addressing the root causes of homelessness, the child welfare system provides an important safety net for at-risk youth, but further attention to life skill preparation and community transition may be required to ensure better outcomes in this population.
From a practice perspective, health services compatible with work schedules and delivered in a flexible format will be required to best serve homeless people who rely on employment as a source of income. Finally, in moving toward a more comprehensive model of health care for homeless individuals, incorporating vision screening and services may alleviate the burden of this impairment, enhance functionality, and improve access to other dimensions of care.
Acknowledgments
This study was funded by a grant from the Health Resources and Services Administration of the Department of Health and Human Services (T32HP10251) to support the Harvard Medical School Fellowship in General Medicine and Primary Care.
A preliminary summary of these findings was presented as a scientific abstract at the 32nd Annual Meeting (May 13-16, 2009, Miami Beach, FL) of the Society of General Internal Medicine.
We thank Sowmya Rao from the Massachusetts General Hospital Biostatistics Center for her assistance in analyzing the data. She received financial compensation for her assistance. We thank John Ayanian from the Harvard Medical School Department of Health Care Policy for his input on the study design and analytic approach and Meridale Vaught Baggett from the General Medicine Division at Massachusetts General Hospital for her many thoughtful reviews of the article.
In addition, we thank Charles Daly and colleagues at the Health Resources and Services Administration's Bureau of Primary Health Care for their assistance in accessing the 2003 Health Care for the Homeless User Survey data. We also thank Jody Greene from Research Triangle Institute International for her assistance in accessing the survey data and for providing supporting technical documents regarding the survey design.
Note. The Health Resources and Services Administration sponsored and assisted in designing the 2003 Health Care for the Homeless User Survey but had no role in the design and conduct of this study or in the collection, management, analysis, or interpretation of the data presented. The Health Resources and Services Administration reviewed a final draft of this article but was not involved in the article preparation or revision process; the authors alone exercised final judgment in determining the form and content of the article. The views expressed in this article are the opinions of the authors and do not necessarily reflect the official policies of the US Department of Health and Human Services or the Health Resources and Services Administration, nor does mention of either department or agency imply endorsement by the US government. This article does not represent the views or work of any individuals we have thanked for their assistance nor their respective institutions.
Human Participant Protection
No protocol approval was needed for this study.
References
- 1.Burt MR, Aron LY, Lee E, Valente J. How many homeless people are there?: Helping America's Homeless: Emergency Shelter or Affordable Housing? Washington, DC: Urban Institute; 2001:23–54 [Google Scholar]
- 2.Hibbs JR, Benner L, Klugman L, et al. Mortality in a cohort of homeless adults in Philadelphia. N Engl J Med 1994;331(5):304–309 [DOI] [PubMed] [Google Scholar]
- 3.Hwang SW, Orav EJ, O'Connell JJ, Lebow JM, Brennan TA. Causes of death in homeless adults in Boston. Ann Intern Med 1997;126(8):625–628 [DOI] [PubMed] [Google Scholar]
- 4.Barrow SM, Herman DB, Cordova P, Struening EL. Mortality among homeless shelter residents in New York City. Am J Public Health 1999;89(4):529–534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hwang SW. Mortality among men using homeless shelters in Toronto, Ontario. JAMA 2000;283(16):2152–2157 [DOI] [PubMed] [Google Scholar]
- 6.Cheung AM, Hwang SW. Risk of death among homeless women: a cohort study and review of the literature. CMAJ 2004;170(8):1243–1247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morrison DS. Homelessness as an independent risk factor for mortality: results from a retrospective cohort study. Int J Epidemiol 2009;38(3):877–883 [DOI] [PubMed] [Google Scholar]
- 8.Breakey WR, Fischer PJ, Kramer M, et al. Health and mental health problems of homeless men and women in Baltimore. JAMA 1989;262(10):1352–1357 [PubMed] [Google Scholar]
- 9.Burt MR. Homelessness: Programs and the People They Serve: Findings of the National Survey of Homeless Assistance Providers and Clients: Technical Report Washington, DC: US Dept of Housing and Urban Development, Office of Policy Development and Research; 1999 [Google Scholar]
- 10.Ferenchick GS. The medical problems of homeless clinic patients: a comparative study. J Gen Intern Med 1992;7(3):294–297 [DOI] [PubMed] [Google Scholar]
- 11.Gelberg L, Linn LS. Assessing the physical health of homeless adults. JAMA 1989;262(14):1973–1979 [PubMed] [Google Scholar]
- 12.Gelberg L, Linn LS, Usatine RP, Smith MH. Health, homelessness, and poverty: a study of clinic users. Arch Intern Med 1990;150(11):2325–2330 [PubMed] [Google Scholar]
- 13.Weinreb L, Goldberg R, Perloff J. Health characteristics and medical service use patterns of sheltered homeless and low-income housed mothers. J Gen Intern Med 1998;13(6):389–397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wright JD. The health of homeless people: evidence from the National Health Care for the Homeless Program. : Brickner PW, Scharer LK, Conanan B, Savarese M, Scanlan BC, Under the Safety Net: The Health and Social Welfare of the Homeless in the United States New York, NY: WW Norton; 1990:15–31 [Google Scholar]
- 15.Zlotnick C, Zerger S. Survey findings on characteristics and health status of clients treated by the federally funded (US) Health Care for the Homeless Programs. Health Soc Care Community 2009;17(1):18–26 [DOI] [PubMed] [Google Scholar]
- 16.Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res 2000;34(6):1273–1302 [PMC free article] [PubMed] [Google Scholar]
- 17.Stark LR. Barriers to health care for homeless people. : Jahiel RI, Homelessness: A Prevention-Oriented Approach Baltimore, MD: Johns Hopkins University Press; 1992:151–164 [Google Scholar]
- 18.Robertson MJ, Cousineau MR. Health status and access to health services among the urban homeless. Am J Public Health 1986;76(5):561–563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wood D, Valdez RB. Barriers to medical care for homeless families compared with housed poor families. Am J Dis Child 1991;145(10):1109–1115 [DOI] [PubMed] [Google Scholar]
- 20.Gallagher TC, Andersen RM, Koegel P, Gelberg L. Determinants of regular source of care among homeless adults in Los Angeles. Med Care 1997;35(8):814–830 [DOI] [PubMed] [Google Scholar]
- 21.Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA 2001;285(2):200–206 [DOI] [PubMed] [Google Scholar]
- 22.Kushel MB, Perry S, Bangsberg D, Clark R, Moss AR. Emergency department use among the homeless and marginally housed: results from a community-based study. Am J Public Health 2002;92(5):778–784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martell JV, Seitz RS, Harada JK, Kobayashi J, Sasaki VK, Wong C. Hospitalization in an urban homeless population: the Honolulu Urban Homeless Project. Ann Intern Med 1992;116(4):299–303 [DOI] [PubMed] [Google Scholar]
- 24.Salit SA, Kuhn EM, Hartz AJ, Vu JM, Mosso AL. Hospitalization costs associated with homelessness in New York City. N Engl J Med 1998;338(24):1734–1740 [DOI] [PubMed] [Google Scholar]
- 25.Lewis JH, Andersen RM, Gelberg L. Health care for homeless women. J Gen Intern Med 2003;18(11):921–928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kertesz SG, Hwang SW, Irwin J, Ritchey FJ, Lagory ME. Rising inability to obtain needed health care among homeless persons in Birmingham, Alabama (1995–2005). J Gen Intern Med 2009;24(7):841–847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Desai MM, Rosenheck RA. Unmet need for medical care among homeless adults with serious mental illness. Gen Hosp Psychiatry 2005;27(6):418–425 [DOI] [PubMed] [Google Scholar]
- 28.Berk ML, Schur CL, Cantor JC. Ability to obtain health care: recent estimates from the Robert Wood Johnson Foundation National Access to Care Survey. Health Aff (Millwood) 1995;14(3):139–146 [DOI] [PubMed] [Google Scholar]
- 29.Bureau of Primary Health Care Section 330 Grantees Uniform Data System (UDS), Calendar Year 2007 Data: Health Care for the Homeless Rollup Report Washington, DC: US Dept of Health and Human Services; 2008 [Google Scholar]
- 30.Greene J, Fahrney K, Byron M. Health Care for the Homeless User/Visit Surveys Research Triangle Park, NC: RTI International; 2004 [Google Scholar]
- 31.Newacheck PW, Hughes DC, Hung YY, Wong S, Stoddard JJ. The unmet health needs of America's children. Pediatrics 2000;105(4):989–997 [PubMed] [Google Scholar]
- 32.Ayanian JZ, Weissman JS, Schneider EC, Ginsburg JA, Zaslavsky AM. Unmet health needs of uninsured adults in the United States. JAMA 2000;284(16):2061–2069 [DOI] [PubMed] [Google Scholar]
- 33.Chen J, Hou F. Unmet needs for health care. Health Rep 2002;13(2):23–34 [PubMed] [Google Scholar]
- 34.Shi L, Stevens GD. Vulnerability and unmet health care needs: the influence of multiple risk factors. J Gen Intern Med 2005;20(2):148–154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Andersen RM, McCutcheon A, Aday LA, Chiu GY, Bell R. Exploring dimensions of access to medical care. Health Serv Res 1983;18(1):49–74 [PMC free article] [PubMed] [Google Scholar]
- 36.Himmelstein DU, Woolhandler S. Care denied: US residents who are unable to obtain needed medical services. Am J Public Health 1995;85(3):341–344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sanmartin C, Berthelot J-M, Ng E, et al. Comparing health and health care use in Canada and the United States. Health Aff (Millwood) 2006;25(4):1133–1142 [DOI] [PubMed] [Google Scholar]
- 38.Diamant AL, Hays RD, Morales LS, et al. Delays and unmet need for health care among adult primary care patients in a restructured urban public health system. Am J Public Health 2004;94(5):783–789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Strunk BC, Cunningham PJ. Trends in Americans' Access to Needed Medical Care, 2001–2003 Washington, DC: Center for Studying Health System Change; 2004 [Google Scholar]
- 40.Cunningham PJ, Hadley J. Differences between symptom-specific and general survey questions of unmet need in measuring insurance and racial/ethnic disparities in access to care. Med Care 2007;45(9):842–850 [DOI] [PubMed] [Google Scholar]
- 41.NIAAA Council approves definition of binge drinking. NIAAA Newsletter Winter 2004:3 [Google Scholar]
- 42.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorders Test: Guidelines for Use in Primary Care 2nd ed Geneva, Switzerland: World Health Organization; 2001 [Google Scholar]
- 43.Alaimo K, Briefel RR, Frongillo EA, Jr, Olson CM. Food insufficiency exists in the United States: results from the Third National Health and Nutrition Examination Survey (NHANES III). Am J Public Health 1998;88(3):419–426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Alaimo K, Olson CM, Frongillo EA, Jr, Briefel RR. Food insufficiency, family income, and health in US preschool and school-aged children. Am J Public Health 2001;91(5):781–786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rose D, Oliveira V. Nutrient intakes of individuals from food-insufficient households in the United States. Am J Public Health 1997;87(12):1956–1961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vozoris NT, Tarasuk VS. Household food insufficiency is associated with poorer health. J Nutr 2003;133(1):120–126 [DOI] [PubMed] [Google Scholar]
- 47.Briefel RR, Woteki CE. Development of food sufficiency questions for the Third National Health and Nutrition Examination Survey. J Nutr Educ 1992;24(suppl 1):24S–28S [Google Scholar]
- 48.Cristofar SP, Basiotis PP. Dietary intake and selected characteristics of women age 19–50 years and their children age 1–5 years by reported perception of food sufficiency. J Nutr Educ 1992;24(1):53–58 [Google Scholar]
- 49.Iezzoni LI, Davis RB, Soukup J, O'Day B. Satisfaction with quality and access to health care among people with disabling conditions. Int J Qual Health Care 2002;14(5):369–381 [DOI] [PubMed] [Google Scholar]
- 50.O'Day BL, Killeen M, Iezzoni LI. Improving health care experiences of persons who are blind or have low vision: suggestions from focus groups. Am J Med Qual 2004;19(5):193–200 [DOI] [PubMed] [Google Scholar]
- 51.Conway KP, Compton W, Stinson FS, Grant BF. Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry 2006;67(2):247–257 [DOI] [PubMed] [Google Scholar]
- 52.Burnam MA, Stein JA, Golding JM, et al. Sexual assault and mental disorders in a community population. J Consult Clin Psychol 1988;56(6):843–850 [DOI] [PubMed] [Google Scholar]
- 53.Glied S, Hoven C, Moore RE, Garrett AB. Medicaid and service use among homeless adults. Inquiry 1998;35(4):380–388 [PubMed] [Google Scholar]
- 54.O'Toole TP, Gibbon JL, Hanusa BH, Fine MJ. Preferences for sites of care among urban homeless and housed poor adults. J Gen Intern Med 1999;14(10):599–605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.O'Toole TP, Gibbon JL, Hanusa BH, Fine MJ. Utilization of health care services among subgroups of urban homeless and housed poor. J Health Polit Policy Law 1999;24(1):91–114 [DOI] [PubMed] [Google Scholar]
- 56.DeNavas-Walt C, Proctor BD, Smith JC. Income, Poverty, and Health Insurance Coverage in the United States: 2007 Washington, DC: US Census Bureau; 2008 [Google Scholar]
- 57.Medical Expenditure Panel Survey, 2006: Access to Care Tables 4.2–4.4 Rockville, MD: Agency for Healthcare Research and Quality; 2006 [Google Scholar]
- 58.Kaiser Family Foundation Medicaid benefits: online database. Available at: http://medicaidbenefits.kff.org. Accessed March 22, 2010
- 59.US Dept of Health and Human Services, Centers for Medicare and Medicaid Services Medicaid dental coverage overview. Available at: http://www.cms.hhs.gov/MedicaidDentalCoverage. Accessed March 22, 2010
- 60.Baker DW, Shapiro MF, Schur CL. Health insurance and access to care for symptomatic conditions. Arch Intern Med 2000;160(9):1269–1274 [DOI] [PubMed] [Google Scholar]
- 61.Hafner-Eaton C. Physician utilization disparities between the uninsured and insured: comparisons of the chronically ill, acutely ill, and well nonelderly populations. JAMA 1993;269(6):787–792 [PubMed] [Google Scholar]
- 62.Freeman HE, Blendon RJ, Aiken LH, Sudman S, Mullinix CF, Corey CR. Americans report on their access to health care. Health Aff (Millwood) 1987;6(1):6–8 [DOI] [PubMed] [Google Scholar]
- 63.Gelberg L, Gallagher TC, Andersen RM, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am J Public Health 1997;87(2):217–220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med 2006;21(1):71–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Collins SR, Schoen C, Colasanto D, Downey DA. On the edge: low-wage workers and their health insurance coverage: findings from the Commonwealth Fund 2001 Health Insurance Survey. Issue Brief (Commonw Fund) March 3, 2003:1–8 [PubMed] [Google Scholar]
- 66.Fronstin P. Employment-based health benefits: trends in access and coverage. EBRI Issue Brief August 2005:1–27 [PubMed] [Google Scholar]
- 67.Fronstin P, Helman R, Greenwald M. Small employers and health benefits: findings from the 2002 Small Employer Health Benefits Survey. EBRI Issue Brief January 2003:1–21 [PubMed] [Google Scholar]
- 68.DeNavas-Walt C, Proctor BD, Mills RJ. Income, Poverty, and Health Insurance Coverage in the United States: 2003 Washington, DC: US Census Bureau; 2004 [Google Scholar]
- 69.Tweddle A. Youth leaving care: how do they fare? New Dir Youth Dev 2007;113:15–31 [DOI] [PubMed] [Google Scholar]
- 70.Bassuk EL, Buckner JC, Weinreb LF, et al. Homelessness in female-headed families: childhood and adult risk and protective factors. Am J Public Health 1997;87(2):241–248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Courtney ME, Heuring DH. The transition to adulthood for youth “aging out” of the foster care system. : Osgood DW, Foster EM, Flanagan C, Ruth G, On Your Own Without a Net: The Transition to Adulthood for Vulnerable Populations Chicago, IL: University of Chicago Press; 2005:27–67 [Google Scholar]
- 72.Koegel P, Melamid E, Burnam A. Childhood risk factors for homelessness among homeless adults. Am J Public Health 1995;85(12):1642–1649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kushel MB, Yen IH, Gee L, Courtney ME. Homelessness and health care access after emancipation: results from the Midwest Evaluation of Adult Functioning of Former Foster Youth. Arch Pediatr Adolesc Med 2007;161(10):986–993 [DOI] [PubMed] [Google Scholar]
- 74.Herman DB, Susser ES, Struening EL. Childhood out-of-home care and current depressive symptoms among homeless adults. Am J Public Health 1994;84(11):1849–1851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Viner RM, Taylor B. Adult health and social outcomes of children who have been in public care: population-based study. Pediatrics 2005;115(4):894–899 [DOI] [PubMed] [Google Scholar]
- 76.Foster Care: Effectiveness of Independent Living Services Unknown Washington, DC: US General Accounting Office; 1999 [Google Scholar]
- 77.Kushel MB, Evans JL, Perry S, Robertson MJ, Moss AR. No door to lock: victimization among homeless and marginally housed persons. Arch Intern Med 2003;163(20):2492–2499 [DOI] [PubMed] [Google Scholar]
- 78.Hunger and Homelessness Survey: A Status Report on Hunger and Homelessness in America's Cities: A 25-City Survey Washington, DC: United States Conference of Mayors; 2008 [Google Scholar]