Abstract
Social, political, and economic disruptions caused by natural and human-caused public health emergencies have catalyzed public health efforts to expand the scope of biosurveillance and increase the timeliness, quality, and comprehensiveness of disease detection, alerting, response, and prediction. Unfortunately, efforts to acquire, render, and visualize the diversity of health intelligence information are hindered by its wide distribution across disparate fields, multiple levels of government, and the complex interagency environment. Achieving this new level of situation awareness within public health will require a fundamental cultural shift in methods of acquiring, analyzing, and disseminating information. The notion of information “fusion” may provide opportunities to expand data access, analysis, and information exchange to better inform public health action.
Internet-based technologies (e.g., social-networking Web sites, wikis, and blogs) have led to an explosion in social networks that harness the “wisdom of crowds,” giving Internet users convenient instant access to information and communities.1 These new tools and novel information sources are also becoming ubiquitous in our increasingly wired (and wireless) society, such that members of the general public can readily disseminate their own interpretations of public health events outside a public health context or scientific framework. As these developments make clear, an information revolution is overdue in public health, particularly in epidemiology and surveillance (i.e., biosurveillance), where there is an increasing need to develop, “fuse,” and share critical health information for decision-making across numerous fields, communities, professions, organizations, institutions, and health systems. Public health epidemiology and surveillance that are conducted through an electronic medium (chiefly the Internet)—termed “infodemiology” and “infoveillance,” respectively—present good opportunities for practice and research.1 Public health also confronts an increasing proliferation of novel electronic surveillance approaches and multiple legacy data systems amid growing concerns about appropriateness of data release, data validity, and costs versus benefits.2,3 Although more information now exists electronically than ever before, there is no guarantee that electronic information can be successfully exchanged; in addition, the exchange of electronic information can still be constrained by organizational boundaries erected in response to technical, legal, and privacy concerns.4
In recent years, it has become evident that public health events can threaten our national security. Bioterrorism poses an obvious threat to health and life, but any public health event might weaken public confidence in a government's ability to respond to emergencies, undermine a nation's social order, catalyze regional instability, or cause adverse economic impact, including trade restrictions.5 The worldwide response to the 2009 pandemic influenza (H1N1) outbreak was a prime example of the need for rapid exchange of public health information.6 Similar recent examples include the SARS (severe acute respiratory distress syndrome) epidemic that spread from China in early 2003 in a matter of days and was associated with local transmission in 4 additional countries, with an economic impact of at least $50 billion7; the largest US foodborne disease outbreak of Salmonella Saintpaul in history, with an estimated $100 million loss to the tomato industry in 2008; and an outbreak of foot-and-mouth disease in Great Britain in 2001, with a tourism industry loss of £2.7 to £3.2 billion and a loss to agriculture and the food industry of £3.1 billion (equivalent to 0.2% of Great Britain's gross domestic product).8 A typical pandemic of influenza in the United States is estimated to result in 89 000 to 207 000 deaths and economic costs of $71.3 to $166.5 billion, excluding disruptions to commerce and society.9
To identify novel risks and address extant threats, the United States must implement a nationwide biosurveillance capability that connects domestic and international surveillance systems to provide early warning and ongoing characterization of disease outbreaks in near–real time.10 Comprehensive biosurveillance ideally would use multiple modalities of information collection, analysis, and dissemination, as well as secure yet flexible information architecture. In addition, strengthening existing surveillance networks and infrastructure, enhancing clinician awareness and participation in biosurveillance, and strengthening laboratory diagnostic capabilities and capacity would result in potential threats being recognized as soon as possible. Integration of routine surveillance information with other potential indicator sources (e.g., health care, veterinary care, agriculture, meteorology, environmental protection, and intelligence) may provide a more comprehensive picture of community health and environmental threats.
DEFINING BIOSURVEILLANCE
On December 18, 2006, the Pandemic and All-Hazards Preparedness Act (SB 3678) was passed, amending the Public Health Service Act to improve situation awareness in public health emergencies. Specifically, the Act recommended,
In collaboration with State, local, and tribal public health officials, [the secretary of the Department of Health and Human Services] shall establish a near real-time electronic nationwide public health situational awareness capability through an interoperable network of systems to share data and information to enhance early detection of, rapid response to, and management of, potentially catastrophic infectious disease outbreaks and other public health emergencies that originate domestically or abroad.10
More recently, Homeland Security Presidential Directive 21 (HSPD-21) required the Department of Health and Human Services to establish a nationwide biosurveillance system predicated on state and local capabilities.11 This directive defined biosurveillance as the process of “active data-gathering, analysis, and interpretation of biosphere data related to disease activity and threats to human and animal health to achieve early warning, detection, and situational awareness.”8 In response to this directive, the Centers for Disease Control and Prevention (CDC) tasked its newly formed Biosurveillance Coordination Unit with drafting a national biosurveillance strategy for human health in collaboration with federal agencies and state, local, territorial, and tribal stakeholders.12
The Biosurveillance Coordination Unit refined the working definition of biosurveillance and enlarged its scope to assess current nationwide capability. The unit defined biosurveillance as the collection and integration of timely health-related information for public health action. This collection and integration is to be achieved through early detection, characterization, and situation awareness of exposures and acute human health events of public health significance. The scope of biosurveillance is all hazards of public health significance, which includes threats and exposures (e.g., disease in animals with zoonotic potential, environmental exposures, natural disasters, and terrorism events), adverse events, instances of diseases (e.g., nationally notifiable diseases), and outbreaks. Biosurveillance capability is distributed across local and state jurisdictions and is supported and complemented at the federal level, providing value on a global scale. Biosurveillance relies upon structured public health surveillance systems, the use of nonstructured data and non–public health information sources, and information generated from epidemiologic investigations, and it is highly dependent on a skilled workforce.12
These definitions of biosurveillance are consistent with similar efforts on the part of the European Centre for Disease Prevention and Control to integrate and coordinate the development of early warning and response capabilities to meet new challenges, including implementation of the 2005 International Health Regulations.13 The International Health Regulations are an internationally binding legal instrument designed to help the international community prevent, report, and respond to acute public health risks that have the potential to cross borders and threaten people worldwide. The European Centre for Disease Prevention and Control has defined “epidemic intelligence” as encompassing all activities related to early identification of potential health hazards, including the functions of public health surveillance (both structured and unstructured) and epidemiologic investigation, with the goal of recommending public health control measures.14,15 In all efforts to strengthen integrated biosurveillance capabilities, it is critical to use a systems-based approach and to make wise investments in new technologies that build on current capabilities and efforts.12,16
This “system of systems” biosurveillance capability must be able to identify specific disease incidence and prevalence in heterogeneous populations and environments and must possess sufficient flexibility to tailor analyses to new syndromes and emerging diseases. State and local government health officials, public- and private-sector health care institutions, and practicing clinicians must be involved in biosurveillance system design, and the overall system must be constructed with the principal objective of establishing or enhancing the detection and response capabilities of state, territorial, tribal, and local government entities. Priorities for biosurveillance investment in the United States have been outlined in the Pandemic and All-Hazards Preparedness Act10 (see the box on this page).
PRIORITY AREAS FOR US BIOSURVEILLANCE INVESTMENT
Electronic health information exchange
Electronic laboratory information exchange
Unstructured data collection and analysis
Integrated biosurveillance information
Global disease detection and connectivity
Biosurveillance workforce for the future
Note. Adapted from the Pandemic and All-Hazards Preparedness Act.10
APPLYING THE CONCEPT OF “FUSION” TO PUBLIC HEALTH
Since September 11, 2001, the intelligence community has become a pioneer in creating information-sharing environments that capitalize on new intelligence methodologies and, more importantly, that foster a culture of sharing information.17 Innovation in methods of information integration and exchange is also occurring at the 70 “fusion centers” located in every US state and many major cities; the Department of Homeland Security and the Department of Justice recognize these centers as critical elements supporting situation awareness.18 Fusion centers vary in function and capacity, but in general they serve as environments that facilitate data collection and the exchange of information across programs.19 Fusion centers are designed to provide broader access to disparate data and to integrate and complement existing data streams.20 Many are staffed by multiagency personnel across levels of government and jurisdictions, and some include collaborators in the private sector.20 However, fusion centers require evaluation, and best practices for fusion centers continue to be developed.21
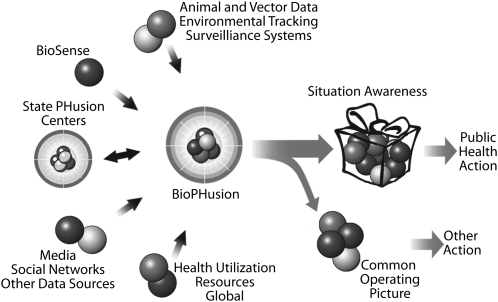
To address the need for integration and exchange of biosurveillance information and to develop ways to access and use unstructured data, the CDC implemented a pilot program called BioPHusion, which tested the operational capacity of a public health fusion center. The goal of this program, launched in July 2008 and completed in July 2009, was to examine the utility of biosurveillance integration and exchange, and potentially to create best practices for a national network of state and local public health fusion centers (Figure 1). Public health fusion centers would support and enhance current capabilities to collect, analyze, and exchange interpreted biosurveillance data (i.e., information) from existing traditional systems and nontraditional sources. Fusion centers also would provide mechanisms for disseminating information to decision makers.
FIGURE 1.
The BioPHusion pilot program of the US Centers for Disease Control and Prevention.
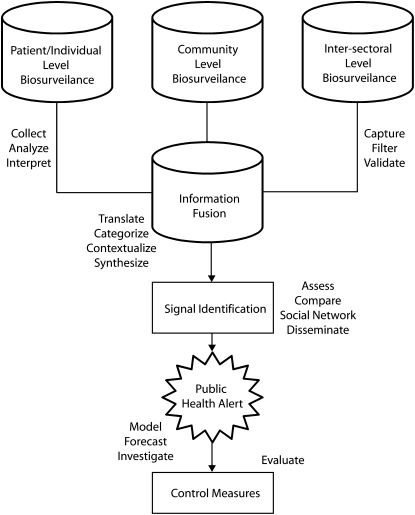
Biosurveillance information can be broadly categorized in a number of different ways: information on exposure, morbidity, and mortality at the patient or individual level; health indicator and health utilization information at the community or population level; and intersectoral information from sources outside public health (e.g., animal health, environmental monitoring, food distribution, and law enforcement; Figure 2). Biosurveillance information fusion currently rests in the hands of analysts and requires diversified subject-matter knowledge to translate, contextualize, and synthesize information across categories for meaningful dissemination to stakeholders through alerting mechanisms. However, information–fusion algorithms are being investigated as ways to use multiple data streams22 and clinical decision support systems23 to add population-based, public health–focused decision support to current outbreak detection–focused systems.
FIGURE 2.
Conceptual model of a distributed biosurveillance information fusion framework.
Note. Modelled from Paquet et al.14
The BioPHusion network was intended to specifically allow for alert verification and dissemination by routinely collecting, monitoring, and synthesizing disparate kinds of health information into actionable knowledge in order to support public health action. The program was designed to help maintain situation awareness and provide a “common public health operating picture” (e.g., epidemic intelligence).15,24 In addition, BioPHusion was designed to be a source of interpreted, fused public health information for use by other federal agencies, including the Department of Homeland Security, which is charged with national biosecurity. Enhancing early detection of, rapid response to, and effective management of potentially catastrophic infectious disease outbreaks and other public health emergencies will require a bottom-up knowledge-management approach that synthesizes information within global, federal, state, territorial, tribal, and local programs. This concept of multidirectional information flow would rely heavily on the creation of new electronic social networks for knowledge management.25,26
THE SCOPE OF FUSIBLE BIOSURVEILLANCE INFORMATION
Public health entities are using nontraditional unstructured and open-source data sources to complement and enhance traditional surveillance systems. Although these data sources present unique biosurveillance opportunities, their validity and usefulness require continued examination. Tools such as the Global Public Health Information Network (GPHIN), HealthMap, EpiSpider, ARGUS, and Google.org Flu Trends mine low-cost, unstructured data for event-based information. These data sources include news wire services, listservs, ProMED-mail, online newspapers, and search engines.27–30 GPHIN, developed by Health Canada and adopted by the World Health Organization, created revolutionary new possibilities for global outbreak response by using news media information for earlier event detection, eschewing the pyramid of official reporting and disregarding national boundaries of outbreak notification.31 By incorporating news within the emerging apparatus of global infectious disease surveillance, GPHIN enhanced the effectiveness and credibility of international public health and improved traditional national disease reporting.
Similarly, the publicly available Google.org Flu Trends analyzes large numbers of Google search queries to track influenza-like illness in a population.32 Because the relative frequency of certain queries is correlated with the percentage of physician visits in which a patient presents with influenza-like illness, search engine queries may be able to estimate the current level of weekly influenza activity in each region of the United States, with a reporting lag of approximately one day. The response to the 2009 influenza pandemic (H1N1) showcased the power of Web 2.0 technologies for communications purposes because the CDC and other entities have used blogs, widgets, wikis, microblogs (e.g., Twitter), RSS (real simple syndication) feeds, and podcasts for communication with other public health officials, the health care industry, and the public.33
News media reports and search engine queries are just two of many such sources of low-cost electronic information that can be used to benefit the public health need to improve detection, response, and prediction. Near–real time detection and event characterization will also likely benefit from the increasing availability and automated analysis of electronic health records.34 There is a need for an interoperable public health surveillance system that will allow exchange of information (consistent with current law) between provider organizations, contracting organizations, and local, state, and federal agencies.35 BioSense, the CDC's national, electronic, hospital-based syndromic surveillance system, is piloting methods to access and analyze electronic medical records for disease surveillance and event monitoring. These novel methods that capitalize on unstructured open-source data and electronic health records are expanding the scope of available information, but biosurveillance is still anchored in efforts to strengthen existing systems and capabilities. Existing systems include environmental monitoring, animal disease surveillance, reportable (notifiable) disease surveillance, laboratory surveillance, and laboratory networks. Many of these systems are underfunded and are maintained within disparate programs at all levels of government; consequently, they often lack the ability to readily exchange information.
CHALLENGES
Effective fusion of multiple, disparate, and often unstructured and overwhelming streams of data will require the development of new tools and a new cadre of trained public health information analysts, epidemiologists, and informaticians. Improved tools for information formatting and integration, data acquisition, data characterization, information extraction, data mining, and decision-making are needed.27 The workforce supporting a nationwide public health fusion network must acquire and maintain the skills needed to: (1) collaborate with information providers to validate and verify information (assess “signals” detected in data), (2) understand the context of this information and the likelihood of the event in question, (3) assess event magnitude (morbidity, mortality, geographic distribution, and population at risk), (4) evaluate the credibility of the information sources, and (5) provide audiences with a standardized interpretation of event likelihood, event magnitude, and information credibility. A public health biosurveillance workforce lacking adequate training, preparation, and regularly upgraded skills could impair biosurveillance and public health response efforts.36
Web-based social networks that are freely available, easy to use, and lack oversight by authorities can foster an information environment that includes biased or erroneous information that could result in harm to individual or community health.37 As a result, information sources will need to be assessed and prioritized on the basis of their potential value and relevance for detecting emergent public health events and enhancing situation awareness. A unique challenge will be to develop enhanced analytic and information validation methods that increase the sensitivity of signal detection without increasing the alert rate34 (a primary criticism of syndromic surveillance). This requires a focus on decision-making, establishing analytic techniques for qualitative information versus quantitative data (e.g., triangulation, a method used in qualitative research),38 and developing strict classification criteria for alerting (e.g., define public health threat classification and scale). An openness to new data sources and dynamic information streams as the underpinning of biosurveillance should also permit the use of forecasting methods and modeling to describe potential scenarios, for true situation awareness.24 Participants in new electronic social networks within public health could serve as distributed analysts who assess and verify this information and develop their own connections and interpretations.
The real challenge, however, is not to develop new tools or increase access to existing electronic information; rather, it is to cultivate new public health social networks of professionals at the local, state, and federal levels. These networks could serve as sources of qualitative data on health events and situation awareness; as environments for distributed investigation, validation, analysis, and interpretation of information for potential actionable associations; and, ultimately, as sources of timely action to prevent and decrease morbidity and mortality. The value of such social capital is well established.39 A Web-based social-network site would allow individuals to construct a public or semipublic profile within a bounded system, articulate a list of other users with whom they share a connection, and view and traverse their list of connections and those made by others within the system.40 Embedded resources in social networks enhance information flow, exert influence, certify social credentials, and reinforce a person's worthiness both as an individual and as a member of a group. A social-network site is also an excellent way to foster collective intelligence activities among individuals with public health interest across various domains, improving public health group cognition, coordination, and cooperation.20 Such networks are actively encouraged in business and industry, where they have already been empirically proven to provide broader access to diverse, novel information to improve group performance.41,42
There also is a significant need to cultivate a public health culture that is open to secure and timely sharing of information, in contrast to the current environment, which is mired in emphases on data ownership and privacy concerns. To address cultural barriers to information sharing, any new information revolution within public health must add value to all the components of the distributed public health system, including such sectors as health care, industry, agriculture, and academia. Information sharing will be enhanced by paying attention to legitimate issues of information security by ensuring information confidentiality, integrity, authentication, and availability. To assess information reliability resulting from fusion activities and the impact of enhanced biosurveillance capacity and capability, process standards and surveillance evaluation indicators must be defined and routinely monitored.
Securing the health of our nation depends on near–real time access to actionable, “fused” health intelligence. To ensure this access, we must collectively improve our disease detection, alerting, and prediction capabilities. The Internet revolution, increased availability of electronic heath-related information, and improved information technology have given public health practitioners unprecedented access to novel streams of information and the ability to establish social networks for analysis and dissemination. Capitalizing on this opportunity will require the public health community to change its organizational culture so that the uses of information are not limited to traditional surveillance and direct notification. Instead, we must collectively learn to share information, reward the sharing and reuse of information across domains, and expand the boundaries of public health to multiple new sectors.
Acknowledgments
We are deeply indebted to the following individuals for their comments on this article and their clarity of vision: David Bray, Benn Konsynski, Kristin Uhde, Dan Sosin, M. Kate Glynn, Carol Rubin, Tracee Treadwell, and Virginia Lee. This work also benefits from the deliberations of numerous individuals, programs, and workgroups who have been innovating surveillance and information exchange activities at the Centers for Disease Control and Prevention, local health authorities, and academia for the last decade, including Epi-X, numerous syndromic surveillance projects, HealthMap, the Office of Critical Information and Exchange, the Global Disease Detection Ops Center, and the BioSurveillance Coordinating Unit.
Note. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Human Participant Protection
No protocol approval was needed because no human research participants were involved.
References
- 1.Eysenbach G. Infodemiology and infoveillance: framework for an emerging set of public health informatics methods to analyze search, communication and publication behavior on the internet. J Med Internet Res 2009;11(1):e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leal J, Laupland KB. Validity of electronic surveillance systems: a systematic review. J Hosp Infect 2008;69(3):220–229 [DOI] [PubMed] [Google Scholar]
- 3.Bravata DM, McDonald KM, Smith WM, et al. Systematic review: surveillance systems for early detection of bioterrorism-related diseases. Ann Intern Med 2004;140(11):910–922 [DOI] [PubMed] [Google Scholar]
- 4.Penfield SL, Anderson KM, Edmunds M, Belanger M. Toward health information liquidity: realization of better, more efficient care from the free flow of health information. Available at: http://www.boozallen.com/media/file/Toward_Health_Information_Liquidity.pdf. Accessed October 1, 2009
- 5.Cecchine G, Moore M. Infectious diseases and national security: strategic information needs. RAND Corporation. 2006. Available at: http://www.rand.org/pubs/technical_reports/TR405. Accessed October 1, 2009
- 6.Centers for Disease Control and Prevention Outbreak of swine-origin influenza A (H1N1) virus infection—Mexico, March–April 2009. MMWR Morb Mortal Wkly Rep 2009; 58(dispatch):1–3 [PubMed] [Google Scholar]
- 7.Keogh-Brown MR, Smith M. The economic impact of SARS: how does the reality match the predictions? Health Policy 2008;88(1):110–120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dept for Environment, Food and Rural Affairs and Dept for Culture, Media and Sport Economic cost of foot and mouth disease in the UK—a joint working paper. Available at: http://archive.cabinetoffice.gov.uk/fmd/fmd_report/documents/D-GovtPublications/DEFRA_DCMS.pdf. March 2002. Accessed September 15, 2009
- 9.Meltzer MI, Cox NJ, Fukuda K. The economic impact of pandemic influenza in the United States: priorities for intervention. Emerg Infect Dis 1999;5(5):659–671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pandemic and All-Hazards Preparedness Act, S 3678, 109th Cong (2006) [Google Scholar]
- 11.Homeland security presidential directive 21: public health and medical preparedness. Available at: http://www.dhs.gov/xabout/laws/gc_1219263961449.shtm. Accessed December 1, 2009.
- 12.US Dept of Health and Human Services National biosurveillance strategy for human health. Available at: http://sites.google.com/site/nbshh10/Welcome. Accessed October 1, 2009
- 13.World Health Organization International health regulations (2005). 2nd ed. Geneva, Switzerland: World Health Organization; 2008. Available at: http://whqlibdoc.who.int/publications/2008/9789241580410_eng.pdf. Accessed May 12, 2010 [Google Scholar]
- 14.Paquet C, Coulombier D, Kaiser R, Ciotti M. Epidemic intelligence: a new framework for strengthening disease surveillance in Europe. Euro Surveill 2006;11(12):212–214 [PubMed] [Google Scholar]
- 15.Kaiser R, Coulombier D, Baldari M, Morgan D, Paquet C. What is epidemic intelligence, and how is it being improved in Europe? Euro Surveill 2006;11(5):pii=2892. Available at: http://www.eurosurveillance.org/ew/2006/060202.asp#4. Accessed October 1, 2009 [DOI] [PubMed] [Google Scholar]
- 16.Nuzzo JB. Developing a national biosurveillance program. Biosecur Bioterror 2009;7(1):37–38 [DOI] [PubMed] [Google Scholar]
- 17.US Director of National Intelligence United States intelligence community intelligence sharing strategy. Available at: http://www.dni.gov/reports/IC_Information_Sharing_Strategy.pdf. Accessed October 1, 2009
- 18.Riegle R. The future of fusion centers: potential promise and dangers. Testimony before the US Committee on Homeland Security, Subcommittee on Intelligence, Information Sharing, and Terrorism Risk Assessment. Available at: http://www.dhs.gov/ynews/testimony/testimony_1238597287040.shtm. Accessed October 15, 2009
- 19.US Dept of Justice Fusion center guidelines: developing and sharing information and intelligence in a new era. Available at: http://it.ojp.gov/documents/fusion_center_guidelines.pdf. Accessed September 15, 2009
- 20.Johnston R. Law enforcement fusion centers: where information, technology and policy intersect. Sheriff 2007;(January–February):67–70 Available at: http://www.lexisnexis.com/government/solutions/casestudy/lefusion.pdf. Accessed December 1, 2009
- 21.Straw J. Smashing intelligence stovepipes. Security Management 2008. Available at: http://www.securitymanagement.com/article/smashing-intelligence-stovepipes. Accessed December 1, 2009
- 22.Kulldorff M, Mostashari F, Duczmal L, Yih WK, Kleinman K, Platt R. Multivariate scan statistics for disease surveillance. Stat Med 2007;26(8):1824–1833 [DOI] [PubMed] [Google Scholar]
- 23.Mnatsakanyan ZR, Burkom HS, Coberly JS, Lombardo JS. Bayesian information fusion networks for biosurveillance applications. J Am Med Inform Assoc 2009;16(6):855–863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Endsley MR. Toward a theory of situation awareness in dynamic systems. Hum Factors 1995;37(1):32–64 [Google Scholar]
- 25.Manville B. Complex adaptive knowledge management. : Clippinger JH, III, The Biology of Business New York, NY: Jossey-Bass; 1999 [Google Scholar]
- 26.Boyd DM, Ellison NB. Social network sites: definition, history, and scholarship. J Comput Mediated Commun 2008;13(1):210–230 [Google Scholar]
- 27.Keller M, Blench M, Tolentino H, et al. Use of unstructured event-based reports for global infectious disease surveillance. Emerg Inf Dis 2009;15(5):689–695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cowen P, Garland T, Hugh-Jones ME, et al. Evaluation of ProMED-mail as an electronic early warning system for emerging animal diseases: 1996 to 2004. J Am Vet Med Assoc 2006;229(7):1090–1099 [DOI] [PubMed] [Google Scholar]
- 29.Brownstein JS, Freifeld CC, Madoff LC. Digital disease detection—harnessing the Web for public health surveillance. N Engl J Med 2009;360(21):153–157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Polgreen PM, Chen Y, Pennock DM, Nelson FD. Using Internet searches for influenza surveillance. Clin Infect Dis 2008;47(11):1443–1448 [DOI] [PubMed] [Google Scholar]
- 31.Mykhalovskiy E, Weir L. The Global Public Health Intelligence Network and early warning outbreak detection: a Canadian contribution to global public health. Can J Public Health 2006;97(1):42–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ginsberg J, Mohebbi MH, Patel RS, et al. Detecting influenza epidemics using search engine query data. Nature 2009;457(7232):1012–1014 [DOI] [PubMed] [Google Scholar]
- 33.Brownstein JS, Freifeld CC, Chan EH, et al. Information technology and global surveillance of cases of 2009 H1N1 Influenza. N Engl J Med 2010;362(18):1731–1735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tokars JI, Burkom H, Xing J, et al. Enhancing time-series detection algorithms for automated biosurveillance. Emerg Infect Dis 2009;15(4):533–539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.US Dept of Health and Human Services The decade of health information technology: delivering consumer-centric and information-rich health care. Available at: http://www.phdsc.org/health_info/dhhs-office.asp 2004. Accessed October 1, 2009
- 36.Gebbie K, Merrill J, Tilson HH. The public health workforce. Health Aff (Millwood) 2002;21(6):57–67 [DOI] [PubMed] [Google Scholar]
- 37.Cobus L. Using blogs and wikis in a graduate public health course. Med Ref Serv Q 2009;28(1):22–32 [DOI] [PubMed] [Google Scholar]
- 38.Guion LA. Triangulation: establishing the validity of qualitative studies. Gainesville, FL: Institute of Food and Agricultural Sciences, University of Florida; 2002. Publication FCS6014 [Google Scholar]
- 39.Lin N, Cook K, Burt RS, Social Capital: Theory and Research New Brunswick, NJ: Transaction Publishers; 2001 [Google Scholar]
- 40.Surowiecki J. The Wisdom of Crowds: Why the Many Are Smarter Than the Few and How Collective Wisdom Shapes Business, Economies, Societies and Nations New York, NY: Doubleday; 2004 [Google Scholar]
- 41.Aral S, Van Alstyne MW. Networks, information & brokerage: the diversity-bandwidth tradeoff. Available at: http://ssrn.com/abstract=958158. Accessed October 1, 2009
- 42.Wu L, Lin C-Y, Aral S, Brynjolfsson E. Value of social network—a large-scale analysis on network structure impact to financial revenues of information technology consultants. Paper presented at: The 2009 Winter Conference on Business Intelligence; February 26-28, 2009; Salt Lake City, UT [Google Scholar]