Abstract
PURPOSE
The diagnosis of isolated inferior oblique muscle palsy is controversial for 2 reasons: first, clinical findings seem inconsistent with our current understanding of oculomotor neuro-anatomy and, second, similar findings can occur with other causes. Because denervated extraocular muscles atrophy, we used high-resolution magnetic resonance imaging (MRI) to assess inferior oblique muscle size in patients with clinically suspected inferior oblique muscle palsy.
METHODS
A diagnosis of inferior oblique muscle palsy in 6 patients (4 unilateral, 2 bilateral) was made clinically. High-resolution coronal and sagittal orbital MRI were obtained in subjects with clinical inferior oblique muscle palsy and in 30 age-matched control subjects. Cross sections of the inferior oblique, inferior rectus (IR), and medial rectus muscles were determined together because each is innervated by the common inferior division of the oculomotor nerve. No subject had pupillary abnormalities or other extraocular muscle weakness or restriction.
RESULTS
Mean cross-sectional area of the affected inferior oblique muscle (n = 8) at the midpoint of the inferior rectus muscle was 10.2 ± 1.05 mm2, which was significantly smaller than the value of 18.8 ± 3.6 mm2 for control subjects (n = 58, p < 0.00001). Unilaterally affected inferior oblique muscles were significantly smaller than unaffected inferior oblique muscles (p < 0.05). Mean medial rectus muscle cross section (n = 8) ipsilateral to the affected inferior oblique muscle was 36.8 ± 2.4 mm2, which was not significantly different from the 35.1 ± 3.7 mm2 value for the medial rectus muscles of control subjects (n = 61, p > 0.1). Mean inferior rectus muscle cross section (n = 8) ipsilateral to the affected inferior oblique muscle was 32.5 ± 2.3 mm2, which was significantly greater than the 29.9 ± 3.3 mm2 measurement for the control subjects (n = 61, p < 0.01).
CONCLUSIONS
We used MRI to demonstrate reduced inferior oblique muscle size in patients with clinically diagnosed inferior oblique muscle palsy, supporting the concept of isolated inferior oblique muscle weakness.
Inferior oblique muscle palsy is the least common isolated extraocular muscle palsy.1 The clinical diagnosis of inferior oblique muscle palsy is based on the presence of underelevation in adduction of the affected eye, increased hypotropia in contralateral head tilt, incyclotorsion, A pattern, and the absence of restriction on forced duction testing. The diagnosis of isolated inferior oblique muscle palsy has been controversial because the anatomic concept of the third nerve nucleus makes it unlikely that only the inferior oblique muscle could be affected.2–5
Several authors have reported patients with findings suggestive of isolated inferior oblique muscle palsy.5–10 However, no patient underwent orbital imaging to confirm atrophy of the involved inferior oblique muscle. Other extraocular muscles do reliably show atrophy when denervated,11 and recent findings in animals demonstrate superior oblique muscle atrophy when denervated (Demer JL, et al. IOVS 2008: ARVO E-Abstract 4495). As noted by Donahue et al,2 no direct evidence of secondary muscle atrophy has ever been confirmed in the setting of a clinically suspected inferior oblique muscle palsy.
Current orbital imaging enables direct visualization of the anatomy and contractility of the extraocular muscles. 11–18 As reported by several authors, muscle atrophy and hypocontractility are characteristic findings in patients with extraocular muscle paresis.12–16,19 Imaging the inferior oblique muscle was limited and difficult as the result of its thin dimensions and its oblique orientation respect to the sagittal and frontal planes.20 By using quasi-sagittal plane orbital imaging, Kono and Demer13 studied the functional anatomy of the inferior oblique muscle in normal subjects and in patients with superior oblique muscle palsy.12 They found that the inferior oblique muscle contracts in supraducted adduction and that its size and contractility did not correlate well with overelevation in adduction in superior oblique muscle palsy.
The purpose of this study was to assess, with the use of high-resolution MRI, the sizes of inferior oblique, medial rectus, and inferior rectus muscles in a group of patients with clinically suspected isolated inferior oblique muscle palsy. The hypothesis motivating our study was that we might find a smaller inferior oblique muscle in the presence of normal medial rectus and inferior rectus muscles that are innervated by the same inferior division of the oculomotor nerve.
Methods
We performed high-resolution orbital MRI on 6 consecutive patients who were diagnosed with isolated inferior oblique muscle palsy (4 unilateral, 2 bilateral) to evaluate the size of the inferior oblique muscle. Patients were compared with 30 age-matched control subjects. All subjects provided written informed consent according to a protocol conforming to the Declaration of Helsinki, in compliance with Health Insurance Portability and Accountability Act regulations and approved by the local Institutional Review Board.
Control volunteers underwent complete eye examinations in which we verified normal corrected vision, normal ocular versions, orthotropia in all gaze positions, and stereopsis of 40 arcsec by Titmus testing. Subjects with inferior oblique muscle palsy were selected because they exhibited incomitant hypotropia of the affected eye larger in adduction, underelevation of the affected eye in adduction, and larger hypotropia in contralateral head tilt. Other clinical signs of inferior oblique muscle palsy included ipsilateral incyclotorsion and A pattern.
All strabismic subjects had undergone complete ophthalmologic examinations by an author who is a pediatric ophthalmologist, including measurement of binocular misalignment by prism and cover testing in upright diagnostic head positions, as well as with head tilting and the Hess screen test. Cyclodeviation was measured subjectively with the use of double Maddox rods and objectively assessed with fundus examination. Ocular versions were quantified on a 9-point scale from −4 representing maximal underaction, to 0 representing normal action, to +4 representing maximal overaction. Forced duction testing was performed in subjects who underwent strabismus surgery. No patient had pupillary abnormalities or evidence of other extraocular muscle weakness or restriction.
In all patients, the aforementioned author evaluated ocular versions, ocular alignment in all gaze positions by the prism and alternating-cover test, and sensorial status by using the Titmus Fly-Animals-Circles Stereo Test (Stereo Optical Company, Inc, Chicago, IL). This author assessed torsion with the double Maddox rod lenses and anomalous head posture subjectively while the patient was fixing at a distance target 6 m away.
High-resolution surface coil coronal and sagittal orbital MRI were obtained at 2 mm thickness in patients with clinical inferior oblique muscle palsy, as described elsewhere.11–14 Cross sections of the inferior oblique, inferior rectus, medial rectus, and superior oblique muscles were determined bilaterally in all study subjects digitally. High-resolution, T1-weighted MRI was performed with the use of a 1.5 T General Electric Signa (Milwaukee, WI) scanner. Crucial aspects of this technique, which are described in detail elsewhere,11,13–15 include use of a dual-phased surface coil array (Medical Advances, Milwaukee, WI) to improve signal-to-noise ratio and fixation targets to avoid motion artifacts.14,19 Initially, an axial localizer scan was obtained at 3 mm thickness, with a 256 × 192 matrix over a 10 cm field of view. To optimally image the inferior oblique muscle, we obtained sets of contiguous 2 mm thick MRI image planes in the quasi-coronal perpendicular to orbital plane and quasi-sagittal images parallel to the orbital axis by using a 256 × 256 matrix over a 7 cm to 9 cm field of view, creating a pixel resolution of 0.273 mm to 0.352 mm. To avoid confounding by contractile changes in extraocular muscle size induced by varying eye position due to strabismus, each orbit was scanned during fixation of a central target by the corresponding eye.
Digital MRI images were transferred to Macintosh computers (Apple Computer, Cupertino, CA), converted into a spatially calibrated, 8-bit tagged image file format with the use of locally developed software, and quantified with the program Image J (Image J, 2007, available from http://rsb.info.nih.gov/ij/). In each MRI image, the cross-sectional area of the relevant oblique extraocular muscle was computed with the “area” function of the Image J program. The inferior oblique muscle follows a straight path from its nasally located origin to its pulley conjoined with that of the inferior rectus muscle. The maximum inferior oblique muscle cross section was determined at the most temporal part of the straight path found in the quasi-sagittal image plane, passing through the center of the inferior rectus muscle that travels in this plane. More temporal image planes are unreliable for determination of inferior oblique muscle cross section, because its curved path becomes tangential to the image plane. Tangential cross sections produce unreliable measures of cross-section highly sensitive to small changes in extraocular muscle path angle relative to the plane.
To image the medial rectus, inferior rectus, and superior oblique muscles, sets of contiguous 2 mm thick quasi-coronal image planes were obtained perpendicular to the long axis of each orbit separately, with a 256 × 256 matrix over an 8 cm square field of view, creating a pixel resolution of 312 microns. In each MRI, the border of the inferior oblique, medial rectus, and inferior rectus muscles were outlined manually with a digital cursor, and its cross-sectional area was computed by the “area” function of the Image J program. A single person, masked to the presence or absence of inferior oblique muscle palsy in the orbital image, performed all measurements. Anteroposterior medial rectus and inferior rectus muscles portions in the orbit were normalized by selection of the image plane in each orbit designated zero, which included the globe-optic nerve junction in central gaze. Values for medial rectus and inferior rectus muscles cross section were averaged across subjects in 2 mm thickness referenced to image plane 0. Ipsilateral and contralateral medial rectus and inferior rectus muscles cross-sectional area were compared with normal control patients. Statistical analysis comparing preoperative and postoperative ocular alignment, sensorial status, and ocular versions was performed with a paired 2-tailed t-test.
Results
Of the 6 subjects, 5 (83.3%) with inferior oblique muscle palsy were male subjects. The mean age at diagnoses of inferior oblique muscle palsy was 34 ± 14 years (range, 23–55 years). The left inferior oblique muscle was only palsied in 3 subjects (50%). Both inferior oblique muscles were palsied in 2 subjects (30%). Five subjects had a history of strabismus since childhood. One subject with a history of thyroid disease first noted diplopia 2 years before his first visit. Neither clinical signs or symptoms nor radiological signs of thyroid ophthalmopathy, such as enlarged muscles or irregular bright signals, within the muscles were seen in this patient. None of the patients had any clinical neurological signs or symptoms of mesencephalopontine lesion, to imply skew or otolithic-MLF dysfunction, and no patient had undergone previous strabismus surgery.
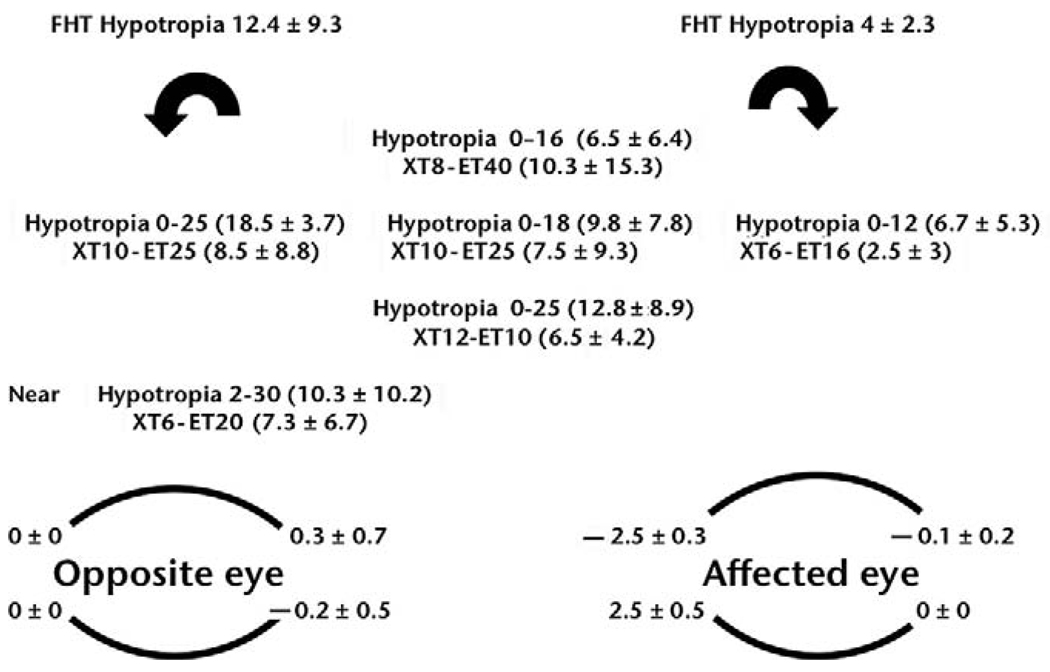
Figure 1 summarizes the ocular alignment and versions (all the eyes were considered left eyes). All patients with unilateral inferior oblique muscle palsy had preoperative hypotropia of the affected eye in central gaze, ranging from 5Δ to 18Δ (mean, 9.8Δ ± 7.8Δ). One patient with asymmetric bilateral inferior oblique muscle palsy had 14Δ of hypotropia of the more affected eye in central gaze. One patient with symmetric bilateral inferior oblique muscle palsy was orthotropic in central gaze.
FIG 1.
Patients baseline alignment. Includes all the patients (all eyes were analyzed as left eyes. Mean in absolute numbers of prism diopters). FHT, forced head tilt test; XT, exotropia; ET, esotropia; PD, prism diopters.
In subjects with unilateral inferior oblique muscle palsy, the amount of hypotropia increased 10.2Δ ± 3.9Δ (range, 8Δ–15Δ) between adduction and abduction of the affected eye. In patients with bilateral inferior oblique muscle palsy, the vertical deviation changed 27.5Δ ± 13.4Δ (range, 18Δ–37Δ) between right gaze and left gaze.
Four subjects had A-pattern strabismus, ranging from 4Δ to 30Δ. The mean A-pattern deviation of patients with suspected bilateral inferior oblique muscle palsy was 24Δ ± 8Δ compared with 7Δ ± 4Δ in patients with unilateral inferior oblique muscle palsy. All patients had a positive head tilt test to the side away from the affected inferior oblique muscle. All patients had incyclotorsion, ranging from 5° to 12°. Both patients with bilateral inferior oblique muscle palsy had incyclotorsion, one 5° and the other 12°. In all patients, there was underelevation in adduction, ranging from −2 to −3, and overdepression in adduction, ranging from +2 to +3.5 (Figure 2).
FIG 2.
Versions in a subject with bilateral inferior oblique muscle palsy. Note the underelevation in adduction and overelevation in adduction bilaterally.
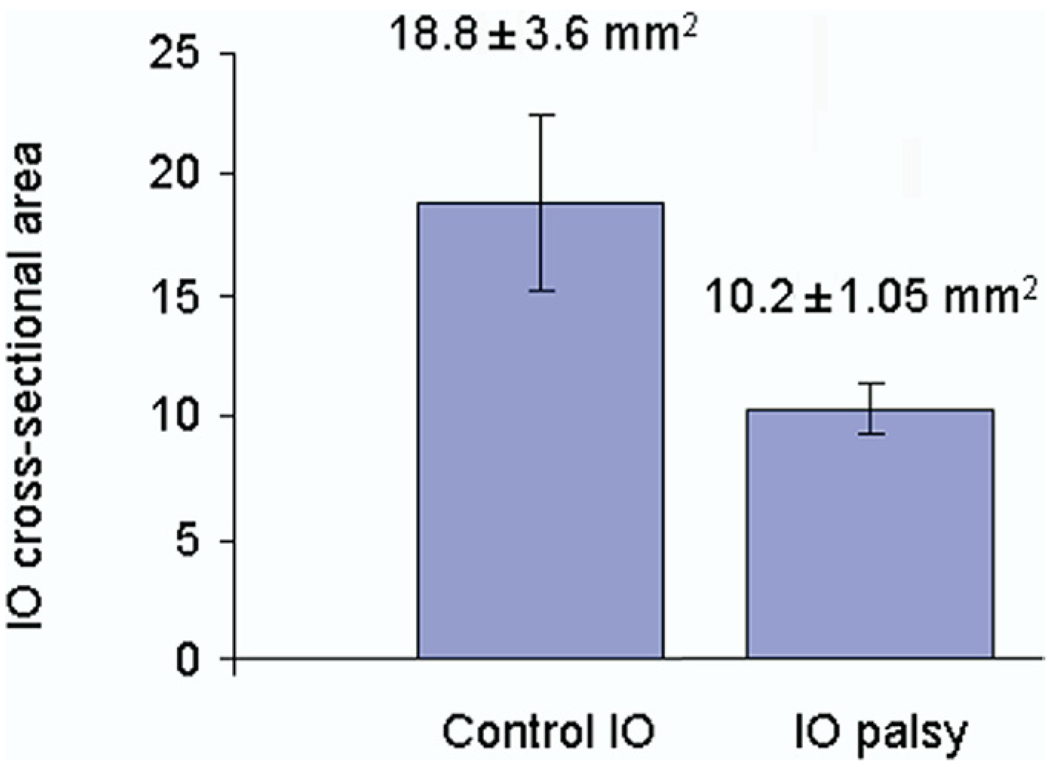
A total of 57 control inferior oblique muscles, corresponding to 53 inferior oblique muscles from 29 age-matched control subjects, and 4 inferior oblique muscles, contralateral to the palsied side from 4 suspected unilateral inferior oblique muscle palsy patients, were compared with 8 affected inferior oblique muscles, from 6 patients who met the clinical criteria for the diagnosis of inferior oblique muscle palsy. Mean cross-sectional area of the affected inferior oblique muscle (n = 8) at the midpoint of the inferior rectus muscle was significantly smaller than the value for controls (p < 0.00001; Figure 3), which corresponds to a 45.5% decrease in the cross-sectional area of the affected inferior oblique muscle (p < 0.00001). The mean cross-sectional area of affected inferior oblique muscles was 21.8% smaller than the mean cross-sectional area of unaffected inferior oblique muscles in unilateral cases (10.8 ± 0.5 vs 13.9 ± 1.2 mm2). This difference was statistically significant (n = 4, p < 0.006). There were no significant differences between the mean cross-sectional area at the mid-point of the inferior rectus muscle size between orbits affected with unilateral inferior oblique muscle palsy (n = 4; mean, 10.8 ± 0.5) and orbits affected with bilateral inferior oblique muscle palsy (n = 4; mean, 9.7 ± 1.2; p = 0.18). In the bilateral cases, the inferior oblique muscle cross section was on average 1 mm2 smaller than the inferior oblique muscle cross section in unilateral cases (Figure 4).
FIG 3.
Bar graph depicts the mean cross-sectional area ± standard error of the inferior oblique muscle in the control group and the palsied inferior oblique group.
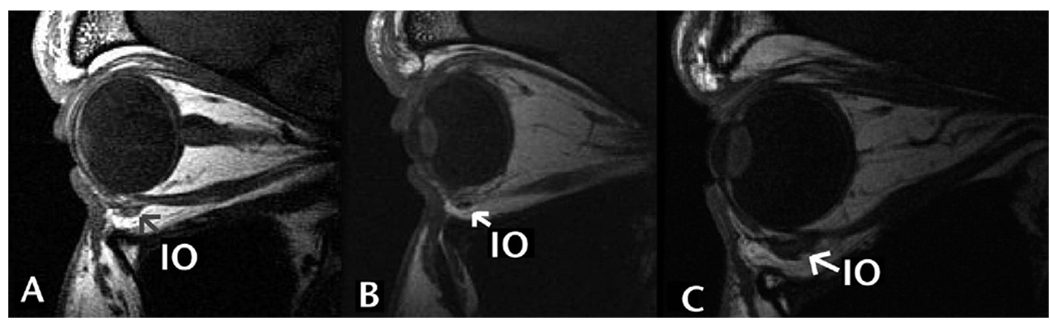
FIG 4.
High-resolution quasisagittal MRI of the right (A) and left (B) orbit of the same subject as in Figure 2. A decrease in the cross-sectional area of inferior oblique muscles (OD 9.514 mm2 and OS 8.698 mm2) is noted. Inferior oblique muscle cross section was determined at the most temporal part of the straight path found in the quasi-sagittal image plane, passing through the center of the inferior rectus muscle that travels in this plane. C, Sagittal-view MRI of a normal age-matched control patient. Note the larger size of inferior oblique muscle. IO, inferior oblique.
We examined the other extraocular muscles innervated by the same inferior division of the third nerve as palsied inferior oblique muscle. The mean medial rectus muscle cross section (n = 8), ipsilateral to the affected inferior oblique muscle, was 36.8 ± 2.4 mm2, not significantly different from the 35.1 ± 3.7 mm2 value for the control medial rectus muscle (p > 0.1). In unilateral inferior oblique muscle palsy, mean medial rectus muscle cross section (n = 4), ipsilateral to the affected inferior oblique muscle, was 35.3 ± 2.6 mm2, compared with 38.4 ± 0.8 mm2 in bilateral inferior oblique muscle palsy (n = 4; p = 0.09).
There was no significant size difference between the inferior rectus muscle cross-section in unilateral inferior oblique muscle palsy compared with control inferior rectus muscle (30.9 ± 2.5 mm2 and 29.9 ± 3.3 mm2, respectively; p > 0.05). However, the inferior rectus muscle cross-section area in subjects with bilateral inferior oblique muscle palsy patients was significantly larger than that of control subjects (33.9 ± 2.5 mm2 and 29.9 ± 3.3 mm2, respectively; p < 0.01). The mean superior oblique muscle cross section (n = 8), ipsilateral to the affected inferior oblique muscle, was 16.5 ± 0.6 mm2, not significantly different from the 16.3 ± 0.9 mm2 value for the control superior oblique muscle (p > 0.1).
Discussion
We report 6 subjects with clinically suspected isolated inferior oblique muscle palsy in whom orbital MRI confirmed reduced size of the affected inferior oblique muscle in comparison to the contralateral nonaffected inferior oblique muscle, as well as in comparison to a group of 30 age-matched control subjects. The other muscles innervated by the same inferior branch of the oculomotor nerve, the inferior rectus and medial rectus muscle, did not show any radiological signs of size reduction. No increase in superior oblique muscle size was found in patients with inferior oblique muscle palsy.
Orbital imaging has been used to analyze the changes in size of paralyzed extraocular muscles.11–19 In patients with chronic abducens nerve palsy, Kang and Demer14 found a 45% reduction in the lateral rectus muscle cross-sectional area when compared with normal control subjects. Sato et al19 reported a reduction in 45.3% in the mean superior oblique muscle volume in congenital trochlear palsy and 65.8% in acquired trochlear palsy, and Kono and Demer12 found a 54% reduction in the cross-sectional area of the superior oblique muscle in patients with trochlear palsy when compared with normal subjects. A primate model indicates superior oblique muscle atrophy only in the global layer of the muscle, with sparing of the orbital layer (Demer JL, et al. IOVS 2008: ARVO E-Abstract 4495). In our study, we found a 45.5% decrease in the mean cross-sectional area of the affected inferior oblique muscle compared with inferior oblique muscles of the control group, and a 21.8% decrease in mean cross-sectional area of the affected inferior oblique muscles compared with the mean cross-sectional area of the unaffected inferior oblique muscles.
Several authors reported series of patients diagnosed with clinically isolated inferior oblique muscle palsy. However, none of those studies confirmed inferior oblique muscle atrophy or size reduction by orbital imaging.6–8 Current techniques allow high-resolution orbital imaging studies of all the extraocular muscles. Formerly, the anterior location and direction of the inferior oblique muscle made it relatively difficult to image.15 Demer and Miller21 described the quasi-coronal plane parallel to the long axes of the orbit to evaluate the rectus and superior oblique muscles. Later, Kono and Demer12 described the quasi-sagittal plane to image the inferior oblique muscle. In central gaze, this plane is parallel to the long axis of the orbit. Using high-resolution orbital quasi-sagittal imaging of the inferior oblique muscle, we were able to confirm a significant decrease in the size of the inferior oblique muscle in patients with clinically suspected isolated inferior oblique muscle palsy.
Some authors have interpreted the clinical picture compatible with isolated inferior oblique muscle palsy as superior oblique muscle overaction, skew deviation,2 or pulley heterotopy3 perhaps for good reasons in each case. There have been few speculations about possible isolated inferior oblique muscle weakness from either brain stem infarction, involving the oculomotor fascicular fibers,22 or from an early embryologic damage that could partially spare the Edinger–Westphal nucleus.23 Wu et al15 presented a case of isolated inferior division oculomotor nerve palsy in which the use of MRI demonstrated a smaller inferior division of the oculomotor nerve with absence of the motor nerve to the medial rectus muscle and the inferior rectus muscle with marked atrophy of the deep portions of both muscles, in the absence of abnormalities of the inferior oblique muscle. They suggested that congenital cranial dysinnervation in the midbrain, intrinsic brainstem disease, or direct damage of the oculomotor nucleus could explain isolated subdivisional oculomotor nerve palsy.
There are 2 hypotheses that may explain the finding of reduced inferior oblique muscle size; one would be the result of a true muscle palsy and an innervational cause as described previously in this article. The other would be that these patients have isolated congenital hypoplastic inferior oblique muscles and not necessarily neurogenic atrophy, analogous to the supposition about congenital abnormalities of superior oblique tendon in patients with congenital superior oblique palsy.24 Most of our patients had symptoms of diplopia and head tilt dating back to early childhood. None of the patients had a history of a known neurological disease, an acquired lesion, or head trauma. In our study, the mean size of the contralateral inferior oblique muscle showed a trend of being smaller than the normal population. It is possible that some of these patients have bilateral asymmetric hypoplastic inferior oblique muscles. However, although congenital extraocular muscle hypoplasia has been demonstrated in association with congenital dysinnervation, primary muscle belly hypoplasia in the presence of normal innervation remains conjectural.
The bilateral, but not unilateral, inferior oblique muscle palsy cases had significantly larger inferior rectus muscles. We do not know the physiologic drive that causes this. The inferior rectus muscle discrepancy may be an epiphenomenon of reduced soft tissue mass of the more atrophied inferior oblique muscle, allowing for more expansion (noncompression) of a normal contiguous inferior rectus muscle in the coronal plane.
This study has the limitation of a small group of patients in whom extraocular muscle imaging was performed. No attempt was made to image the brain. Further studies, including imaging the course of the third nerve and, if possible, of the third nerve nucleus, are warranted.
In conclusion, high-resolution MRI demonstrates reduced inferior oblique muscle size in clinically diagnosed inferior oblique muscle palsy. This supports the concept of isolated inferior oblique muscle weakness, despite normal function of other structures innervated by the oculomotor nerve, and may serve as a tool for clinicians in diagnosing this entity.
Acknowledgments
Supported by USPHS grant EY08313 to JLD. Joseph L. Demer, MD, PhD, is Leonard Apt Professor of Ophthalmology. Arthur L. Rosenbaum, MD, is a recipient of a Research to Prevent Blindness Physician Scientist Merit Award.
References
- 1.Santiago AP, Rosenbaum AL. inferior oblique palsy: Diagnosis and management. In: Rosenbaum AL, Santiago AP, editors. Clinical Strabismus Management: Principles and Surgical Techniques. Philadelphia (PA): WB Saunders; 1999. pp. 230–236. [Google Scholar]
- 2.Donahue SP, Lavin PJ, Mohney B, Hamed L. Skew deviation and inferior oblique palsy. Am J Ophthalmol. 2001;132:751–756. doi: 10.1016/s0002-9394(01)01234-x. [DOI] [PubMed] [Google Scholar]
- 3.Clark RA, Miller JM, Rosenbaum AL, Demer JL. Heterotopic muscle pulleys or oblique muscle dysfunction? J AAPOS. 1998;2:17–25. doi: 10.1016/s1091-8531(98)90105-7. [DOI] [PubMed] [Google Scholar]
- 4.Khawam EK. Diagnosis and treatment of isolated inferior oblique muscle palsy: A report of seven cases. Binocul Vis Strabismus Q. 1998;13:85. [PubMed] [Google Scholar]
- 5.Kakizaki H, Zako M, Iwaki M, Mito H, Katori N. Incarceration of the inferior oblique muscle branch of the oculomotor nerve in two cases of orbital floor trapdoor fracture. Jpn J Ophthalmol. 2005;49:246–252. doi: 10.1007/s10384-004-0184-6. [DOI] [PubMed] [Google Scholar]
- 6.Scott WE, Nankin SJ. Isolated inferior oblique paresis. Arch Ophthalmol. 1977;95:1586–1593. doi: 10.1001/archopht.1977.04450090108009. [DOI] [PubMed] [Google Scholar]
- 7.Olivier P, von Noorden GK, Pollard ZF. Results of superior oblique tenectomy in inferior oblique paresis. Arch Ophthalmol. 1982;100:581–584. doi: 10.1001/archopht.1982.01030030583005. [DOI] [PubMed] [Google Scholar]
- 8.Pollard ZF. Diagnosis and treatment of inferior oblique palsy. J Pediatr Ophthalmol Strabismus. 1993;30:15–18. doi: 10.3928/0191-3913-19930101-05. [DOI] [PubMed] [Google Scholar]
- 9.Dickey CF, Scott WE, Cline RA. Oblique muscle palsies fixating with the paretic eye. Surv Ophthalmol. 1988;33:97–107. doi: 10.1016/0039-6257(88)90161-0. [DOI] [PubMed] [Google Scholar]
- 10.Kutschke PJ, Scott WE. Post-operative results in inferior oblique palsy. J Pediatr Ophthalmol Strabismus. 1996;33:72–78. doi: 10.3928/0191-3913-19960301-03. [DOI] [PubMed] [Google Scholar]
- 11.Demer JL, Clark RA, Kono R, Wright W, Velez F, Rosenbaum AL. A 12-year, prospective study of extraocular muscle imaging in complex strabismus. J AAPOS. 2002;6:337–347. doi: 10.1067/mpa.2002.129040. [DOI] [PubMed] [Google Scholar]
- 12.Kono R, Demer JL. Magnetic resonance imaging of the functional anatomy of the inferior oblique muscle in superior oblique palsy. Ophthalmology. 2003;110:1219–1229. doi: 10.1016/S0161-6420(03)00331-2. [DOI] [PubMed] [Google Scholar]
- 13.Kau HC, Tsai CC, Ortube MC, Demer JL. High-resolution magnetic resonance imaging of the extraocular muscles and nerves demonstrates various etiologies of third nerve palsy. Am J Ophthalmol. 2007;143:280–287. doi: 10.1016/j.ajo.2006.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kang NY, Demer JL. Comparison of orbital magnetic resonance imaging in Duane syndrome and abducens palsy. Am J Ophthalmol. 2006;142:827–834. doi: 10.1016/j.ajo.2006.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu TE, Isenberg SJ, Demer JL. Magnetic resonance imaging demonstrates neuropathology in congenital inferior division oculomotor palsy. J AAPOS. 2006;10:473–474. doi: 10.1016/j.jaapos.2006.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sa HS, Kyung SE, Oh SY. Extraocular muscle imaging in complex strabismus. Ophthalmic Surg Lasers Imaging. 2005;36:487–493. [PubMed] [Google Scholar]
- 17.Ozkan SB, Aribal ME, Sener EC, Sanaç AS, Gürcan F. Magnetic resonance imaging in evaluation of congenital and acquired superior oblique palsy. J Pediatr Ophthalmol Strabismus. 1997;34:29–34. doi: 10.3928/0191-3913-19970101-07. [DOI] [PubMed] [Google Scholar]
- 18.Demer JL, Miller JM, Koo EY, Rosenbaum AL. Quantitative magnetic resonance morphometry of extraocular muscles: A new diagnostic tool in paralytic strabismus. J Pediatr Ophthalmol Strabismus. 1994;31:177–188. doi: 10.3928/0191-3913-19940501-10. [DOI] [PubMed] [Google Scholar]
- 19.Sato M, Yagasaki T, Kora T, Awaya S. Comparison of muscle volume between congenital and acquired superior oblique palsies by magnetic resonance imaging. Jpn J Ophthalmol. 1998;42:466–470. doi: 10.1016/s0021-5155(98)00044-6. [DOI] [PubMed] [Google Scholar]
- 20.Bourlet P, Carrie D, Garcier JM, Dalens H, Chansolme D, Viallet JF, et al. Study of the inferior oblique muscle of the eye by MRI. Surg Radiol Anat. 1998;20:119–121. doi: 10.1007/BF01628915. [DOI] [PubMed] [Google Scholar]
- 21.Demer JL, Miller JM. Magnetic resonance imaging of the functional anatomy of the superior oblique muscle. Invest Ophthalmol Vis Sci. 1995;36:906–913. [PubMed] [Google Scholar]
- 22.Castro O, Johnson LN, Mamourian AC. Isolated inferior oblique paresis from brain-stem infarction. Perspective on oculomotor fascicular organization in the ventral midbrain tegmentum. Arch Neurol. 1990;47:235–237. doi: 10.1001/archneur.1990.00530020149032. [DOI] [PubMed] [Google Scholar]
- 23.Good WV, Barkovich AJ, Nickel BL, Hoyt CS. Bilateral congenital oculomotor nerve palsy in a child with brain anomalies. Am J Ophthalmol. 1991;111:555–558. doi: 10.1016/s0002-9394(14)73697-9. [DOI] [PubMed] [Google Scholar]
- 24.Helveston EM, Krach D, Plager DA, Ellis FD. A new classification of superior oblique palsy based on congenital variations in the tendon. Ophthalmology. 1992;99:1609–1615. doi: 10.1016/s0161-6420(92)31759-2. [DOI] [PubMed] [Google Scholar]