SYNOPSIS
Pasa la Voz (spread the word) is a human immunodeficiency virus (HIV) prevention methodology inspired by respondent-driven sampling (RDS) that uses social networks to access hard-to-reach populations. As field testing showed the approach to be efficacious among at-risk women in West Texas and Southern New Mexico, we set out to evaluate the methodology in a Mexican context. A local community organization, Programa Compañeros, first implemented a traditional one-on-one outreach strategy using promotoras (outreach workers) in Ciudad Juarez, Mexico, from September 2005 to January 2006. This was followed by implementation of Pasa la Voz from February 2006 to January 2007. The percentage of women agreeing to be tested increased from 11.9% to 49.9%, and staff time declined from 22.70 hours to 3.68 hours per HIV test, comparing the one-on-one with the Pasa la Voz methodology, respectively. Pasa la Voz was successful at imparting a cost-savings prevention education program with significant increases in the number of at-risk women being tested for HIV.
The U.S.-Mexico border region, stretching from California to Texas, is a unique region with approximately 12 million inhabitants—a number that is expected to double in the next 15 years.1 On both sides of the border, there are high concentrations of migrant populations, high levels of unemployment, inequitable health conditions, and low rates of insurance.1–4 Ciudad Juarez, a Mexican city located across the border from El Paso, Texas, is no exception. In Cuidad Juarez, as in other border towns, there is an increasing need for human immunodeficiency virus (HIV) prevention services, especially services tailored to women.5–7 This need is due to natural population growth in a city of approximately two million inhabitants compounded by a steady stream of migrants from the interior of Mexico.8 More complex health problems that put these women at risk for HIV infection, such as injection drug use, sex work, and domestic violence, are further aggravated by the paucity of services geared toward women.9–11 Women's access to HIV services is further hindered by multiple social, cultural, and economic issues, ranging from stigma and relationship power to cost and transportation.7,12–14
In U.S. states bordering Mexico, community-based organizations have had success with health programs and prevention services among Latino populations through the implementation of programs that rely on promotores, community members with leadership skills who help to disseminate health messages.9,15 In particular, this model has had success in increasing the use of HIV testing and prevention services.9,10
The Pasa la Voz intervention methodology employs a similar promotores model, with an added component inspired by respondent-driven sampling (RDS). RDS, first described by Douglas Heckathorn, is a form of chain-referral sampling that uses social networks to identify and access hard-to-reach populations.16 Subsequent studies have found that the RDS technique can help increase recruitment of samples that are more representative, reducing the bias of initial selection and volunteerism.17 This sampling technique has been adapted to recruit and enroll populations at risk for HIV into prevention studies, successfully increasing HIV testing rates among hard-to-reach populations.18 The Pasa la Vozintervention borrows the idea of “seeds” (or peer motivators) from the RDS methodology, and employs a more systematic use of social network referrals to disseminate information and increase the use of available services. As this was a programmatic study focused on delivery of services, it was designed to pilot the incorporation of RDS elements into an outreach program and not to formally test RDS theories; therefore, data were not collected on network chains.
The feasibility of the Pasa la Voz intervention has been field tested in Latina populations on the U.S. side of the border;19 however, given the increasing population of at-risk women who remain on the Mexico side of the border, we set out to implement the Pasa la Voz program in Ciudad Juarez, Chihuahua, Mexico. In collaboration with a local community-based organization, Programa Compañeros, women were encouraged to recruit other women from their own social networks into the program, where they were provided with prevention knowledge and the skills necessary to access and use existing HIV prevention and testing services in the future. This program builds on the idea of promotoras, adding another layer of peer networking through seeds.19 The use of seeds allows the spread of health messages throughout social networks rather than being disseminated from a single promotora in a one-on-one approach. In this article, we describe the adaptation and implementation of the Pasa la Voz program in Ciudad Juarez and compare it with a standard promotora outreach program.
PROGRAM ELEMENTS
Three phases of the project were implemented during a two-year period, from September 2005 to January 2007. In phases I, II, and III, promotoras were trained to raise awareness of HIV as a women's issue and provide effective prevention messages to promote behaviors that reduce the risk of HIV infection. In phase II, promotoras were retrained to use social networks to increase knowledge and utilization of existing health services, including confidential referrals to testing and counseling, thereby decreasing the stigma associated with the use of prevention and treatment services. In phase III, the promotoras were retrained to conduct rapid HIV testing and counseling and to deliver these services in community settings.
In phase I of the project, a traditional promotora one-on-one outreach model was implemented to establish a baseline. Promotoras provided prevention messages to promote behaviors that reduce the risk of HIV infection, increase knowledge and utilization of existing health services, and actively encourage individual women to be tested for HIV by providing them with referrals for free HIV testing at health service organizations.20
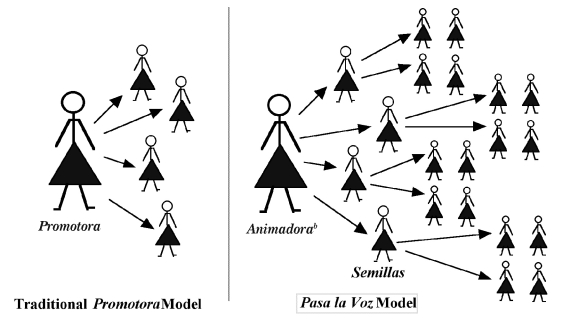
In phase II, the RDS-inspired methodology was implemented to recruit, educate, and offer the HIV test to networks of at-risk women. The promotoras started with a group of at-risk women known as semillas(seeds). semillas identified other women who were part of their social networks and who they believed were at risk for HIV infection. This second tier of women was given referrals to health centers to be tested for HIV and receive other health services (Figure 1).
Figure 1.
Theoretical comparison of the Promotora and Pasa la Voz models for HIV education and testing in Ciudad Juarez, Mexico,a from September 2005 to January 2007
aThe Promotora model, a one-on-one approach, was used in phase I of the study. The Pasa la Voz model, which incorporates seeds and uses social networks, was used in phases II and III of the study.
bAnimadora refers to a promotora who was using Pasa la Voz.
HIV = human immunodeficiency virus
Although there was an increase in the number of women enrolled and a decrease in the number of staff hours needed to obtain a test in this phase, the promotoras noticed that utilization of the free HIV testing services was impeded by transportation issues. Based on their experience in phases I and II, the promotoras implemented the use of “testing parties” organized by promotorasand held at the seeds' homes to provide a safe, comfortable environment for the women to talk about HIV and receive testing. These testing parties were designed to help attract an even larger number of women in phase III. There were no referrals to health centers in this third phase; instead, HIV testing services were brought to the community. This third phase was successful in increasing the number of HIV tests given and decreasing the number of hours required by staff to obtain a test.
EVALUATION
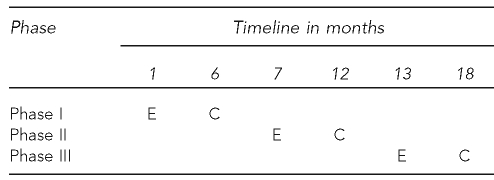
Evaluation of the Pasa la Voz project was based on a group comparison design. Phase I was used as the comparison group (group one) to evaluate the added benefit of the social network-inspired methods employed in phase II (group two) and the combination of social network and community-based rapid testing employed in phase III (group three). As there were insufficient numbers of staff to run the three phases concurrently, the phases were run in sequential six-month intervals (Figure 2). Women participating in the program provided information on their demographics at enrollment, received information from promotorason HIV and services, and were given referral coupons listing all locations where HIV testing could be accessed. Coupons were collected from all service delivery sites to assess the number of women accessing HIV testing services. Women were not eligible to participate in more than one phase of the project.
Figure 2.
Group comparison design: timeline for enrollment and coupon collection for phases I, II, and IIIa of the HIV education and testing study in Ciudad Juarez, Mexico, from September 2005 to January 2007
aPhase I used the Promotora (one-on-one) outreach model, phase II used the Pasa la Voz (social networks) model, and phase III used the enhanced Pasa la Voz (using social networks to organize HIV testing parties) model.
HIV = human immunodeficiency virus
E = enrollment
C = coupon collection
The three groups were similar in demographic profile, and there was no perceived seasonal bias; however, we cannot generalize our results to a larger population (the internal validity is not threatened, but the external validity is relatively weak). The study design had a two-directional hypothesis with respect to the key performance indicators: (1) group 1 will be different from group 2, and (2) group 2 will be different from group 3.
The key performance indicators measured and compared among the three groups were the total number of women receiving HIV educational messages and the total number of HIV tests performed. As a secondary outcome, information was collected to compare aspects of program costs, measured by the mean number of hours spent by each promotorato obtain one HIV test. The promotoraswere paid staff hired specifically for this project; staff time was measured by the number of paid hours logged by the promotorasduring each of the three phases. Regular monitoring visits were conducted by the program coordinator to ensure the fidelity of the approach. Two sources were used to measure the number of HIV tests given during each phase of the program. The number of tests given by the promotoras was recorded throughout the study; in addition, the referral coupons handed out by promotoras were collected from other HIV testing sites in the community and counted toward the total number of HIV tests given during each phase.
PROGRAM OUTCOMES
During the two years of the study, a total of 722 women agreed to participate in one of the three phases of the intervention. The women enrolled in the intervention were aware of their risks. More than half (67.2%) believed they were at risk for contracting HIV and sexually transmitted disease (STD) infections, many (40.0%) never used condoms when having sex, 11.5% were sure that their sexual partner was not faithful to them, and 11.0% were sex workers. There was no significant difference in the demographic makeup among participants in the three phases. The median age range was 21 to 30 years of age, almost all (91.0%) had completed at least six years of schooling, and 32.8% had completed high school (data not shown).
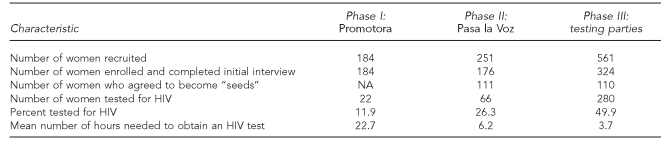
During the first phase, 184 women were exposed to prevention messages and given referrals for HIV testing by promotoras. A total of 22 women (11.9%) followed up with referrals and were tested for HIV. The number of women agreeing to be tested for HIV increased from 11.9% to 26.3% (66 of 251 women approached) after introduction of the Pasa la Voz methodology, and jumped to 49.9% (280 of 561 women) with the introduction of peer-organized testing parties (Table).
Table.
Main outreach program outcomes of an HIV education and testing study in Ciudad Juarez, Mexico, conducted from September 2005 to January 2007, comparing the Promotoraa model (phase I) with the Pasa la Voza model (phase II) and the enhancedb Pasa la Voz model (phase III)
aThe Promotora model is a one-on-one approach. The Pasa la Voz model incorporates seeds and uses social networks.
bThe enhanced model incorporates the use of testing parties, which are peer-organized gatherings at seeds' homes organized by promotoras to provide a safe, comfortable environment for the women to talk about HIV and receive testing.
HIV = human immunodeficiency virus
NA = not applicable
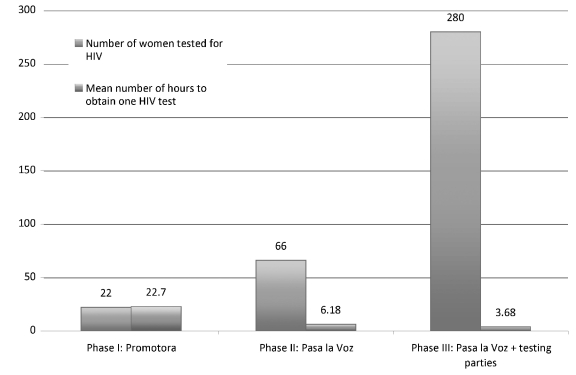
Figure 3 demonstrates the absolute number of women using HIV testing services in the three phases and the total number of staff hours expended. The program kept records of the hours of staff time spent implementing the project during each phase, as well as the approximate number of HIV tests given, allowing determination of the mean number of hours of staff time invested per HIV test. In phase I, promotoraswould spend an estimated mean of 22.7 hours per HIV test compared with 6.18 hours per test in phase II and 3.68 hours per test in phase III.
Figure 3.
Comparative effectiveness (total number of women tested) and cost-effectiveness (mean staff hours per test) of three outreach modelsa implemented during six-month intervals from September 2005 to January 2007: HIV education and testing study, Ciudad Juarez, Mexico
aPhase I used the Promotora (one-on-one) outreach model, phase II used the Pasa la Voz (social networks) model, and phase III used the enhanced Pasa la Voz (using social networks to organize HIV testing parties) model.
HIV = human immunodeficiency virus
DISCUSSION
The Pasa la Vozintervention was successful at increasing HIV testing among at-risk women in Ciudad Juarez. Compared with the traditional one-on-one promotora model, the addition of semillasto the regular promotoramodel to tap into existing social networks doubled the proportion of women following up on referrals for HIV testing, while the introduction of community-based testing sites quadrupled this proportion.
The number of HIV tests that were conducted in phase I using the traditional promotora model was small. During the first three months, it became apparent that the participants were not following up on the referrals for HIV testing in collaborating organizations. As the location of the HIV testing sites was thought to be a potential barrier, Programa Compañeros set up three additional HIV testing sites near the known outreach areas. This corrective action increased the number of tests from two to 22 in the final three months of this phase.
During phases II and III, the promotoras and their semillassurpassed the goals set to reach women at risk. Each semilla contacted a mean of four women instead of the three women requested by the protocol. The Pasa la Voz recruitment and enrollment methodology was efficacious and cost-effective in increasing the number of at-risk women who agreed to participate in an HIV prevention program and to be tested for HIV. To increase the number of tests, Programa Compañeros set up HIV testing sites in the outreach areas, and this corrective action managed to increase the number of tests even further.
The study had several key findings:
At-risk women (namely, seeds) can be successfully recruited and trained to assist promotorasto conduct HIV prevention among other at-risk women.
The use of the seeds' social networks was effective in increasing the number of women recruited, educated, and tested for HIV.
The testing-parties strategy greatly increased the effectiveness and cost-effectiveness of HIV prevention education and HIV testing services.
CONCLUSION
The Pasa la Voz model was effective and efficient at providing HIV testing for a larger number of at-risk women living in Ciudad Juarez as compared with a regular promotoramodel. In addition, the use of semillas and social networks allowed for the organization of informal gatherings in safe, comfortable atmospheres, where women could access information and testing for HIV. Overall, the number of staff hours per HIV test was greatly reduced in both phases II and III, and should be considered in settings where use of social networks is a feasible approach.
Acknowledgments
The authors thank the many generous women willing to engage in the search for better ways of getting services into their communities. The feasibility studies that led to the design of the Pasa la Voz intervention were financed by the Centers for Disease Control and Prevention and implemented in Texas and New Mexico thanks to the collaboration of the following community-based organizations: Camino de Vida, Centro de Mujeres de la Esperanza, Centro de Salud Familiar La Fe, and Planned Parenthood. The El Paso Community Foundation and Border AIDS Partnership have funded the Promotora Program De Mujer a Mujer in Ciudad Juarez, Mexico.
Footnotes
The National AIDS Fund supported the cost-effectiveness study with a grant from Johnson – Johnson. The authors thank the Border AIDS Partnership, National AIDS Fund, and the GENERATIONS staff, who shepherded this project toward a successful conclusion.
The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the funding agencies.
REFERENCES
- 1.United States—Mexico Border Health Commission. [Border region cited 2009 Apr 27]. Available from: URL: http://www.borderhealth.org/border_region.php.
- 2.Rao SP. Foreword. Family & Community Health Border Communities. 2009 Jan;32:2–3. doi: 10.1097/01.FCH.0000342812.64896.65. [DOI] [PubMed] [Google Scholar]
- 3.Ruiz-Beltran M, Kamau JK. The socio-economic and cultural impediments to well-being along the U.S.-Mexico border. J Community Health. 2001;26:123–32. doi: 10.1023/a:1005229330204. [DOI] [PubMed] [Google Scholar]
- 4.Mier N, Ory MG, Zhan D, Conkling M, Sharkey JR, Burdine JN. Health-related quality of life among Mexican Americans living in colonias at the Texas-Mexico border. Soc Sci Med. 2008;66:1760–71. doi: 10.1016/j.socscimed.2007.12.017. [DOI] [PubMed] [Google Scholar]
- 5.Rangel MG, Martinez-Donate AP, Hovell MF, Santibanez J, Sipan CL, Izazola-Licea JA. Prevalence of risk factors for HIV infection among Mexican migrants and immigrants: probability survey in the North border of Mexico. Salud Publica Mex. 2006;48:3–12. doi: 10.1590/s0036-36342006000100003. [DOI] [PubMed] [Google Scholar]
- 6.Patterson TL, Semple SJ, Staines H, Lozada R, Orozovich P, Bucardo J, et al. Prevalence and correlates of HIV infection among female sex workers in 2 Mexico-US border cities. J Infect Dis. 2008;197:728–32. doi: 10.1086/527379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Monk J, Manning P, Denman C, Cornejo E. Place, positionality, and priorities: experts' views on women's health at the Mexico-US border. Health Place. 2009;15:769–76. doi: 10.1016/j.healthplace.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 8.Magis-Rodriguez C, Gayet C, Negroni M, Leyva R, Bravo-Garcia E, Uribe P, et al. Migration and AIDS in Mexico: an overview based on recent evidence. J Acquir Immune Defic Syndr. 2004;37(Suppl 4):S215–26. doi: 10.1097/01.qai.0000141252.16099.af. [DOI] [PubMed] [Google Scholar]
- 9.Ramos RL, Hernandez A, Ferreira-Pinto JB, Ortiz M, Somerville GG. Promovision: designing a capacity-building program to strengthen and expand the role of promotores in HIV prevention. Health Promot Pract. 2006;7:444–9. doi: 10.1177/1524839905278868. [DOI] [PubMed] [Google Scholar]
- 10.Ramos RL, Ferreira-Pinto JB. A transcultural case management model for HIV/AIDS care and prevention. J HIV/AIDS – Social Services. 2006;5:139–57. [Google Scholar]
- 11.Case P, Ramos R, Brouwer K, Firestone-Cruz M, Pollini RA, Fraga MA, et al. At the borders, on the edge: use of injected methamphetamine in Tijuana and Ciudad Juarez, Mexico. J Immigr Minor Health. 2008;10:23–33. doi: 10.1007/s10903-007-9051-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Horwitz RH, Roberts LW, Warner TD. Mexican immigrant women's perceptions of health care access for stigmatizing illnesses: a focus group study in Albuquerque, New Mexico. J Health Care Poor Underserved. 2008;19:857–73. doi: 10.1353/hpu.0.0053. [DOI] [PubMed] [Google Scholar]
- 13.Romero-Gutierrez G, Deigado-Macias AA, Mora-Escobar Y, Ponce-Ponce de Leon AL, Amador N. Mexican women's reasons for accepting or declining HIV antibody testing in pregnancy. Midwifery. 2007;23:23–7. doi: 10.1016/j.midw.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 14.Gomez-Dantes H, Vazquez-Martinez JL, Fernandez-Canton SB. [Violence in Mexican women using public health services] Salud Publica Mex. 2006;48(Suppl 2):S279–87. doi: 10.1590/s0036-36342006000800008. [DOI] [PubMed] [Google Scholar]
- 15.McCloskey JP. Promotores as partners in a community-based diabetes intervention program targeting Hispanics. Fam Community Health. 2009;32:48–57. doi: 10.1097/01.FCH.0000342816.87767.e6. [DOI] [PubMed] [Google Scholar]
- 16.Heckathorn DD. Respondent-driven sampling: a new approach to the study of hidden populations. Social Problems. 1997;44:174–99. [Google Scholar]
- 17.Heckathorn DD. Development of a theory of collective action: from the emergence of norms to AIDS prevention and the analysis of social structure. In: Berger J, editor. New directions in sociological theory: growth of contemporary theories. New York: Rowman and Littlefield Publishers; 2002. pp. p. 79–108. [Google Scholar]
- 18.Frost SD, Brouwer KC, Firestone MA, Ramos R, Ramos ME, Lozada RM, et al. Respondent driven sampling of injection drug users in two U.S.-Mexico border cities: recruitment dynamics and impact on estimates of HIV and syphilis prevalence. J Urban Health. 2006;83(6) Suppl:i83–97. doi: 10.1007/s11524-006-9104-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramos RL, Green NL, Shulman LC. Pasa la Voz: using peer driven interventions to increase Latinas' access to and utilization of HIV prevention and testing services. J Health Care Poor Underserved. 2009;20:29–35. doi: 10.1353/hpu.0.0124. [DOI] [PubMed] [Google Scholar]
- 20.Ramos RL, Ferreira-Pinto JB. A model for capacity-building in AIDS prevention programs. AIDS Educ Prev. 2002;14:196–206. doi: 10.1521/aeap.14.3.196.23891. [DOI] [PubMed] [Google Scholar]