Abstract
A strong association between substance use disorders (SUD) and eating disorders (ED) in women has been established. Yet, little is known about the rates and impact of ED symptoms in women presenting to addiction treatment. The current investigation assessed the prevalence of ED symptoms and their effect on treatment outcomes in a sample of substance abusing women with co-occurring posttraumatic stress disorder (PTSD) enrolled in outpatient substance use programs. Participants were 122 women who participated in a multi-site clinical trial comparing two behavioral treatments for co-occurring SUD and PTSD. The Eating Disorder Examination-self report (EDE-Q), and measures of PTSD and SUD symptoms were administered at baseline, during treatment and at four follow-up points. Two subgroups emerged; those reporting binge eating in the 28 days prior to baseline (Binge group; n = 35) and those who reported no binge eating episodes (No Binge group; n = 87). Women in the Binge group endorsed significantly higher ED, PTSD and depression symptoms at baseline than those in the No Binge group. Though all participants showed significant reductions in PTSD symptoms and improvements in abstinence rates during the study period, the improvements for the Binge group were significantly lower. These findings suggest that a sub-group of women with co-occurring PTSD and SUDs who endorsed binge ED symptoms responded differently to SUD/PTSD group treatment. Identification of eating disorder symptoms among treatment-seeking women with SUDs may be an important element in tailoring interventions and enhancing treatment outcomes.
Introduction
Numerous studies have demonstrated a strong association between substance use (SUD) and eating disorders (ED) in women in both clinical and community samples. Women receiving treatment for ED frequently report alcohol and drug abuse, and individuals entering treatment for substance use disorders often report disordered eating and compensatory behaviors as well as preoccupation with food and body image.1-3
In their review of 51 studies Holderness and colleagues3 found that among individuals with substance abuse, co-occurring lifetime ED behaviors range from 2% to 41%, with a median of 20% prevalence for bulimic symptoms (binge eating and purging). Most recently, the National Comorbidity Survey Replication4 found that lifetime co-occurrence of alcohol use disorders and EDs was between 25 and 34% and lifetime co-occurrence of drug use disorders and EDs ranged from 18 to 26%. These rates are much higher than those found in the general population with DSM IV reporting that .5 to 3% of women will be diagnosed with an ED in their lifetimes.
Though EDs and SUDs frequently co-occur, the prevalence of EDs among those with SUDs varies depending on type of ED diagnosis. The strongest associations between SUD and ED involve subtypes characterized by bulimic behaviors such as binging and purging rather than restriction of food intake as seen in anorexia nervosa.3 In addition to bulimia nervosa, other studies have reported that the diagnosis of binge eating disorder, in which individuals binge eat without associated compensatory behaviors, was more likely in individuals with SUDs than those without.5,6
Likewise, certain substances of abuse, namely alcohol, are more highly correlated with the presence of EDs. Goldbloom and colleagues7 found that in women presenting for treatment of alcohol problems, 30.1% met criteria for an ED, while 26.9% of women seeking outpatient treatment for an ED met criteria for alcohol dependence. In a population-based study, 22.9% of bulimic women had co-occurring alcohol dependence and 48.6% had co-occurring alcohol abuse compared to 8.6% of control females who had alcohol use disorders.8 Another study reported, that by the age of 35, 50% of individuals with bulimia nervosa had met criteria for alcohol abuse or dependence at some point in their lives.9 Though alcohol appears to be the most frequent substance of choice, other substances are also often abused by bulimic women including cocaine, amphetamines and other stimulants.10
Research has pointed toward possible factors that heighten the vulnerability that ED and SUD each pose for the development or worsening of the other disorder. For example, patients diagnosed with bulimia nervosa often report alcohol consumption as a primary trigger for binge eating. Women with an ED may use alcohol and/or other substances for dietary restraint/avoidance, appetite suppression and compensatory behaviors.11 Research also suggests that individuals with bulimia report more negative substance use related consequences despite the fact that they may not drink or use drugs significantly more than non-eating disordered individuals.12
Both SUDs and EDs often co-occur in the presence of additional psychiatric disorders with depressive, posttraumatic stress and other anxiety disorders being the most common.13 Individuals with EDs and SUDs are more likely to have co-occurring psychiatric disorders than women with either SUD or ED alone.1,5,14,15 These women are also often diagnosed with personality disorders, including borderline personality disorder, and often report affective instability and impulsivity.16 In addition, higher rates of severe sexual abuse history have been reported in women with both disorders.17 Women who have been abused are at a greater risk of developing PTSD, which increases the risk of developing both ED and SUD.18 More recently, Corstorphine and colleagues19 found associations between a history of childhood sexual abuse, high levels of alcohol, amphetamine, cocaine and cannabis abuse and impulsive behaviors such as self-cutting.
From these studies a distinct profile of women with co-occurring ED (most often bulimia or binge eating disorder) and SUD emerges. This complicated subgroup, which has been labeled by some as the multi-impulsive category,20 is characterized by multiple psychiatric and personality problems and a history of interpersonal trauma. Women in this group generally have poorer social, interpersonal and occupational functioning. The delineation of subgroups has important implications for the treatment, as women with ED and SUD may respond differently to interventions typically delivered in substance abuse programs and may be more likely to need specialized comprehensive treatment services than women without co-occurring SUD and ED.
The purpose of the current study was to assess eating disorder symptoms in a sample of substance-abusing women with co-occurring PTSD enrolled in community substance abuse treatment, and to explore the potential relationship of ED symptoms to treatment outcomes. Based on the literature presented above we predict that binge eating will be the most frequent eating disorder behavior among the sample. We hypothesize that higher ED symptoms will be associated with greater baseline PTSD, SUD and depression symptom severity, and that participants with greater ED symptoms at baseline will demonstrate significantly less improvement on PTSD and SUD outcomes during treatment and at follow-up.
Method
Participants were 122 women enrolled in community-based substance abuse treatment programs (CTPs) who were participating in a multi-site clinical trial of psychosocial treatments for PTSD. The treatment trial was conducted through the National Institute on Drug Abuse (NIDA) Clinical Trials Network (CTN). The study used a randomized, controlled, repeated measures design to assess the impact of Seeking Safety Treatment21 plus standard substance abuse treatment as compared to a control treatment (Women’s Health Education) (unpublished manual, available from the first author) plus standard substance abuse treatment, on symptoms of posttraumatic stress and substance use disorders (for more information on the larger treatment trial see Hien et al.).22 The study protocol was implemented in seven CTPs across the country, four of which agreed to include a measure of eating disorder symptoms. Analyses from the current study are based on participants from these four participating treatment sites.
All research and clinical staff from the CTPs were trained centrally by the coordinating site, led by the Principal Investigator. The coordinating site and all recruitment sites received prior protocol approval from their respective institutional review boards. Recruitment occurred over a 21-month period in 2004 and 2005. Interested CTP clients completed a brief screen to ascertain potential eligibility. This was followed by an assessment to confirm eligibility. Participants first signed an informed consent with a NIDA issued certificate of confidentiality, including appropriate HIPAA language. A third (baseline) interview was then completed, with full study consent, to gather additional information, including an assessment of eating disorder symptoms. Participants were assessed weekly during the intervention phase, and at 1-week, 3-, 6-, and 12-months post treatment.
To be eligible, participants had to have at least one lifetime traumatic event and met DSM-IV criteria for either full or sub-threshold PTSD (i.e., fulfilling criteria A, B, [either C or D], E and F). Other inclusion criteria were: 1) 18-65 years of age; 2) alcohol or illicit substance use within the past six months; and 3) a current diagnosis of drug or alcohol abuse or dependence. Women were excluded if they had: 1) impaired mental cognition based on a Mini-Mental Status Exam; 2) significant risk of suicidal/homicidal behavior; 3) history of schizophrenia; or 4) active (past two months) psychosis.
Eating disorder symptoms were assessed using The Eating Disorder Examination Questionnaire (EDE-Q),23 a self-report version of the structured interview, the Eating Disorder Examination (EDE).24 The EDE is considered the gold standard for assessing specific psychopathology associated with eating disorders.25 Like the EDE, the EDE-Q provides a comprehensive assessment of the key behavioral and attitudinal features of ED psychopathology. The EDE-Q has shown good correspondence with the EDE in both general23,26 and clinical samples,27,28 including female substance abusers.29 The EDE-Q has shown consistently shown good psychometric properties and has been found to be an effective screening instrument for detecting the presence of eating disorder symptoms.30 The EDE-Q consists of 36 items and it focuses on the timeframe of the past 28 days. It assesses the frequency (total number of episodes) of key eating disorder behaviors such as binge eating and compensatory behaviors including self-induced vomiting, use of laxatives and/or diuretics in order to control weight. Binge eating episodes are assessed by asking the respondent “Over the past four weeks, have there been any times when you felt that you have eaten what other people would regard as an unusually large amount of food given the circumstance?” and “During how many of these episodes of overeating did you have a sense of having lost control over your eating?” The EDE-Q also includes four subscales scored using a 7-point rating scale: Dietary Restraint, Eating Concern, Shape Concern, Weight Concern and a global scale, which are derived from items asking about core attitudes and beliefs characteristic of eating disorders.
Post Traumatic Stress Disorder was assessed via the Clinician Administered PTSD Scale (CAPS),31 which measures frequency and intensity of signs and symptoms of PTSD in the past 30 days and overall symptom severity over time. PTSD symptoms were also measured using The Post Traumatic Stress Disorder Symptom Scale-Self Report (PSS-SR)32 a self-report inventory that assesses the frequency and severity of PTSD symptoms corresponding to DSM-IV diagnostic criteria. Alcohol and substance use data were collected using The Substance Use Inventory (SUI) (unpublished instrument, available from first author), which consists of a series of self report questions about quantity and frequency of substance use in the past 7 days adapted from the Time Line Follow-Back measure and included alcohol, cocaine, heroin, marijuana, sedatives and stimulants. Urine samples were also provided to confirm self-report. SUD symptoms were examined in 2 ways: number of days of substance use, a continuous and linear measure that takes into consideration the full range of days of use (none to daily use), and abstinence, a dichotomous variable that measures the percentage of individuals who were able to achieve abstinence from all substances. Depression Symptoms were measured using the depression subscale of The Brief Symptom Inventory (BSI),33 a self-report scale, which includes 53 items, rated on a 5-point scale.
After completing the baseline assessment, participants were randomized to 12 group sessions of Seeking Safety (SS)21 or Women’s Health Education (WHE) (unpublished manual available from first author) consisted of two sessions per week for 6 weeks. Groups ranged in size from two to eight women and operated with rolling admission so that participants could enter the group at any point in the treatment cycle.
SS is a cognitive-behavioral treatment designed to reduce substance use and the negative impact of trauma exposure. Session topics focus on increasing safety in relationships, identifying and employing healthy coping strategies, improving communication skills, identifying dangerous interpersonal situations, controlling emotions, and using better judgment. WHE is a psychoeducational intervention that focuses on topics such as female anatomy, human sexual behavior, pregnancy and childbirth, nutrition, diabetes, sexually transmitted infections, and HIV risk exposure and transmission. WHE provides equivalent facilitator attention and expectancy of benefit, but does not provide theory driven techniques such as cognitive behavioral therapy or psychoeducation specific to substance abuse or PTSD.
Data Analysis
As expected the most common eating disorder behavior reported was binge eating (28.7%; n = 35). In the current study we analyzed our data according to these findings, which indicated the presence of two subgroups of women in our sample – those who reported binge eating and those who did not report binge eating. Other studies have also used the presence of binge eating episodes as an initial screen for the presence of an eating disorder.34
Participants who reported at least one binge episode in the past 28 days prior to baseline constituted the Binge group (n = 35) and participants who reported no binge eating episodes in the past 28 days prior to baseline constituted the No Binge group (n = 87). Associations between the sociodemographic and clinical characteristics at baseline and group (Binge/No Binge) were evaluated using t-tests for the continuous variables and Chi-square or Fisher’s test on categorical variables.
The analytical strategy for investigating the relationship of group (Binge vs. No Binge) at baseline with treatment outcomes was to fit generalized linear models on the four primary outcomes: total CAPS scores, PSS-SR scores, self reported abstinence confirmed with urine and saliva tests, and a continuous measure of the number of days in the past 7 using drugs or alcohol. We modeled each of the four outcomes as a function of group (Binge vs. No Binge), treatment (SS vs. WHE), time of assessment, and baseline value of that outcome. All models were also controlled for the main effect of site. For each outcome, the possible interactions between group, treatment, the baseline level of the outcome measure, and time were tested and were included in the final model only if statistically significant (p<0.05) using backward elimination procedures. The generalized estimating equations (GEEs)35 were used to estimate and test the models. The GEE methodology is able to handle correlated data arising from repeated measurements, requires no parametric distribution assumption, and provides robust inference with respect to misspecification of the within-subject correlation.
Results
Sociodemographic and clinical characteristics are presented in Table 1. Given that there were no significant differences between Binge vs. No Binge groups on any of these characteristics data is presented for the entire sample. For women who reported binge eating episodes in the past 28 days (28.7%, n = 35) the frequency ranged from 1 to 28 episodes, with a sample mean of 6.28 episodes. Other key eating disorder behaviors such as episodes of vomiting (1.6%, n = 2), taking laxatives (1.8%, n = 4) and/or diuretics (1 .6%, n = 2) as a way of controlling weight were reported infrequently.
Table 1.
Sample sociodemographic and clinical characteristics (N= 122)
| Characteristic | Mean or % | SD or n |
|---|---|---|
| Age | 37.99 | 9.96 |
| Race/Ethnicity | ||
| African American | 32.8 | 40 |
| Caucasian | 42.6 | 52 |
| Latina | 9.8 | 12 |
| Multi-racial and other | 14.8 | 18 |
| Marital Status | ||
| Married | 13.9 | 17 |
| Single | 38.6 | 47 |
| Divorced/Separated | 47.5 | 58 |
| Education (years) | 12.43 | 2.09 |
| Most Frequent Substances Used | ||
| Alcohol | 66.4 | 81 |
| Cocaine | 72.1 | 88 |
| Opioid | 25.8 | 31 |
| Lifetime Trauma Exposure | ||
| Physical Abuse | 93.1 | 114 |
| Sexual Abuse | 62.9 | 77 |
Table 2 presents a comparison between groups on the 4 EDE-Q subscales and global score as well as on PTSD, depression and SUD measures at baseline. The binge eating group had significantly higher scores on all the EDE-Q subscales at baseline, with the exception of the restraint subscale, and on the global summary score. The Binge subgroup also had significantly higher scores on baseline self-report measures of PTSD (t=2.64, df=120, p-value=0.009) and depression (t=2.62, df=120, p-value=0.01), although no statistically significant differences on baseline CAPS clinical interview scores was found. There were no significant differences between Binge and No Binge groups at baseline on either SUD measure. There was a trend but not statistically significant differences on type of drug use and drug of choice (p-value = 0.0915, Fisher’s test) with the patients in the Binge group being more likely to use cocaine.
Table 2.
Baseline Eating Disorder Examination Self-report Subscales, PTSD, Depression and Substance Use Disorder Measures for Binge and No Binge Groups
| Binge Eating Group (N= 35) |
No Binge Eating Group (N=87) |
||||||
|---|---|---|---|---|---|---|---|
| Characteristic | Mean | SD | Mean | SD | t/Chisq | df | p |
| EDE-Q subscales | |||||||
| Restraint | 0.83 | 1.03 | 0.85 | 1.31 | −0.07 | 120 | .95 |
| Eating Concern | 1.31 | 1.21 | 0.40 | 0.64 | 4.18 | 42 | .0001 |
| Weight Concern | 2.46 | 1.76 | 1.32 | 1.37 | 3.77 | 120 | .0003 |
| Shape Concern | 3.14 | 1.70 | 1.92 | 1.56 | 3.79 | 120 | .0002 |
| Global Scale | 1.93 | 1.27 | 1.12 | 1.05 | 3.61 | 120 | .0005 |
| PTSD Symptoms (CAPS) | 59.60 | 18.4 | 63.7 | 14.8 | −1.17 | 120 | .24 |
| PTSD Symptoms (PSS-SR) | 48.63 | 6.19 | 41.06 | 13.54 | 2.64 | 120 | .009 |
| Abstinence (%) | 48.6 | 49.4 | 0.0073 | 1 | 0.932 | ||
| Days of use in the past 30 | 5.40 | 9.48 | 6.12 | 10.65 | −0.35 | 120 | 0.73 |
| Depression Symptoms (BSI) | 8.23 | 4.85 | 5.75 | 4.69 | 2.62 | 120 | .01 |
NOTE: EDE-Q = Eating Disorder Examination Questionnaire; CAPS = Clinician Administered PTSD Scale; PSS SR = Post Traumatic Stress Disorder Symptom Scale-Self Report; BSI = Brief Symptom Inventory
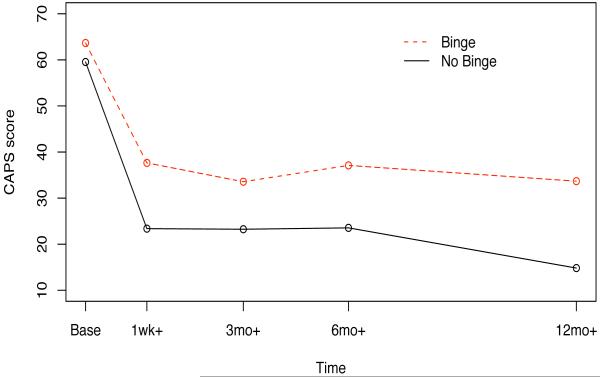
Figure 1 shows the average CAPS score over the study period at major assessment points (baseline, 1 week after treatment, 3-month follow-up, 6 month follow-up and 12-month follow-up) for the Binge vs. No Binge groups. Both groups showed a significant decrease in symptoms over the study period. Based on the final model for the total CAPS score as a function of baseline CAPS, treatment, time and EDE-Q at baseline, there was a significant effect of group on the patients total CAPS (Chisq = 7.62, df=1, p-value = 0.006). Compared with the No Binge group, the Binge group had a significantly greater mean CAPS score by 9.5 points throughout the study period.
FIGURE 1. CAPs Scores Over Study Period by Group.
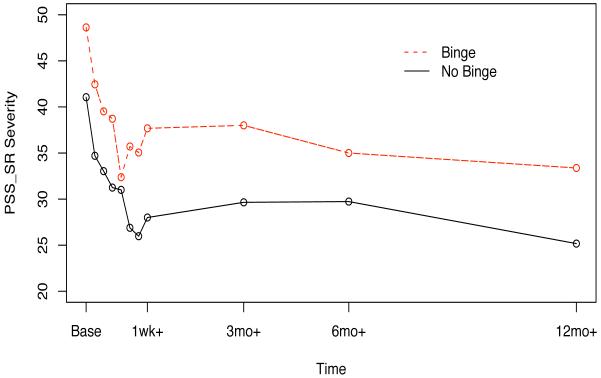
PSS-SR scores were measured weekly during active treatment as well as at major assessment points. As illustrated by Figure 2 there was a significant difference in baseline PSSR-SR between the two groups, which remained throughout the 6-week active treatment period. With the exception of the 1-week follow-up point differences between the groups were statistically significant throughout the study period. The mean value of PSS-SR scores decreased in both groups, though similar to the CAPs there was less improvement for the Binge group. Based on the final model, there was a nearly statistically significant main effect of Binge versus No Binge group on patients’ PSS-SR scores (Chisq = 3.65, df=1, p-value= 0.0559). Throughout the trial, the mean value of PSS-SR severity for participants in the Binge group was greater by 3.3 points in comparison with participants in the No Binge group.
FIGURE 2. PSS–SR Scores Over Study Period by Group.
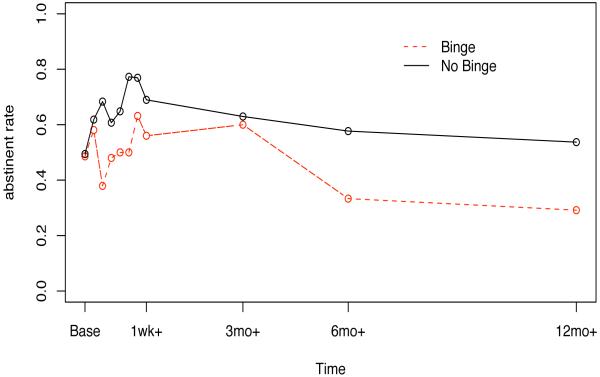
Figure 3 shows abstinent rates at weekly assessments during active treatment and at major assessment points. Based on the final model for abstinence as a function of baseline abstinence, treatment, time, and binge group at baseline there was a significant main effect of Binge vs. No Binge group on abstinence during treatment and follow-up (Chisq =4.79, df=1, p-value=0.0285). The odds of being abstinent for patients in the No Binge group was about 1.82 times of that for patients in the Binge group. During the active treatment period the abstinence rate for patients in the Binge group was 48% lower than patients in the No Binge group (p =.04), and during the whole trial the abstinent rate of patients in the Binge group was 45% lower as compared to patients in the No Binge group (p = .0285). No effect of Binge versus No Binge group was observed for patients’ number of days of use of drugs or alcohol in the past 7 during active treatment or follow-up (Chisq = 0.19, df=1, p-value= 0.6669).
FIGURE 3. Abstinence Rates Over Study Period by Group.
There were no significant interactions between group and treatment intervention indicating that although outcomes were different depending on Binge versus No Binge group they did not differ based on treatment condition received.
Discussion
This study examined the prevalence of eating disorder symptoms and their relationship with outcomes, among women in treatment for co-occurring substance use and posttraumatic stress disorders. Findings provided support for study hypotheses. As predicted binge eating was the most common ED behavior in this sample with almost one-third (29%) reporting at least one episode of binge eating in the past month. This prevalence of binge eating among women with SUDs is consistent with other surveys (3). Additionally, the subgroup of women who reported binge eating also reported higher scores on eating disorder attitude subscales and more severe PTSD and depression symptoms at baseline. Also as hypothesized the presence of ED symptoms had a significant impact on treatment outcomes. In our sample, although both the Binge and No Binge groups improved on PTSD symptom severity and increased abstinence rates, the Binge group showed significantly less improvement than the No Binge group in these areas. In contrast there were no significant differences between groups on days of drug use over the treatment or follow-up period. Overall these results are in line with other studies, which have found a more severe clinical profile and worse treatment outcomes in individuals with co-occurring ED and SUD.36,37
The identification of a subgroup of women with co-occurring SUD and PTSD who endorsed binge eating symptoms, reported more psychopathology and responded less favorably to SUD/PTSD group treatment has potentially important clinical implications. In general results suggest that women with ED behaviors such as binge eating may be less likely to respond to substance abuse group therapy than those without binge eating behaviors and may warrant additional treatment directed at the eating disorder behaviors. General health-focused treatment or treatment focusing on PTSD also appear to be less likely to help this subset of women.
Results such as these, suggest that these women may benefit from early diagnosis of their eating problems. Identification of ED symptoms may be an important element in tailoring interventions and enhancing treatment outcomes. These women may need more specialized and comprehensive treatment services. Unfortunately, SUD treatment programs are unlikely to provide eating disorder diagnostic or treatment services for their patients.38
It is notable that there were no significant interactions between ED group and type of treatment intervention. One possible explanation is that observed improvements in PTSD symptoms and abstinence rates were due to non-specific elements of the group treatments, such as attention from therapists, treatment alliance, or membership in a supportive group of women who share a history of trauma and PTSD, rather than the specific elements of SS and WHE. WHE was intended to serve as a neutral attention control, and its strong performance may indeed indicate that the process of group psychotherapy was more important than the content. It may also be that SS and WHE each have unique active elements (e.g. for SS the cognitive behavioral coping skills for actively managing symptoms and for WHE the body-centered approach to self-care).
This study has limitations, which need to be considered. Because the target population was women with co-occurring SUD and PTSD, results from this study may not generalize to treatment-seeking women with SUD without co-occurring PTSD. It also is possible that our Binge and No Binge groups would have differed if the EDE, a clinical interview, had been used instead of the self-report questionnaire to assess binge eating behaviors. In addition although the Binge and No Binge groups were based on the significant symptom of binge eating, they were not based on other diagnostic criteria. It would be helpful to include a more detailed diagnostic assessment of eating disorders. In terms of days of drug use the Substance Use Inventory may not have been the best assessment tool. This measure only assesses the past 7 days, which may not be representative of a larger pattern of use. It is possible that the lack of differences between groups on this outcome was due to limitations of the measure. If days of use had been measured over a longer period of time (e.g. past month as with EDE-Q and CAPS measures) findings may have differed.
Despite these limitations, this multisite study provides an important contribution to the literature. It allows for an extension of previous research by using a well-validated measurement of ED symptoms across a number of clinical treatment programs as well as multiple standard outcome measures for both PTSD and SUD in the context of a longitudinal design. The current study points to the need for increased awareness of and more research on ED symptoms in treatment seeking women with SUDs. Future research may focus on identifying factors related to the higher psychiatric severity found in women with co-occurring SUD and ED behaviors. Identification of these factors may stimulate research to develop pharmacological and behavioral treatments to lead to better outcomes for this group.
Acknowledgments
This study was supported by grant U10 DA13035 from the National Institute on Drug Abuse Clinical Trials Network, Bethesda, Md (Edward Nunes, MD, NYS Psychiatric Institute, PI). The authors would like to acknowledge grants U10 DA15831 (Dr. Greenfield), K24DA01985 (Dr. Greenfield), and U10 DA013043 (George Woody, MD, University of Pennsylvania, PI) from the National Institute on Drug Abuse, Bethesda, Md.
Footnotes
Declaration of interest:
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.Bulik CM, Sullivan PF, Carter FA, Joyce PR. Lifetime comorbidity of alcohol dependence in women with bulimia nervosa. Addict Behav. 1997;22:437–446. doi: 10.1016/s0306-4603(96)00053-6. [DOI] [PubMed] [Google Scholar]
- 2.Franko DL, Dorer DJ, Keel PK, Jackson S, Manzo MP, Herzog DB. How do eating disorders and alcohol use disorder influence each other? Int J Eat Disord. 2000;38:200–207. doi: 10.1002/eat.20178. [DOI] [PubMed] [Google Scholar]
- 3.Holderness CC, Brooks-Gunn J, Warren MP. Co-morbidity of eating disorders and substance abuse: Review of the literature. Int J Eat Disord. 1994;16:1–34. doi: 10.1002/1098-108x(199407)16:1<1::aid-eat2260160102>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 4.Hudson JI, Hiripi E, Pope HG, Kessler RC. The prevalence and correlated of eating disorders in the National Comorbidity Survey Replication Study. Biol Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grilo CM, Levy KN, Becker DF, Edell WS, McGlashan TH. Eating disorders in female inpatients with versus without substance use disorders. Addict Behav. 1995;20:255–260. doi: 10.1016/0306-4603(94)00065-4. [DOI] [PubMed] [Google Scholar]
- 6.Grilo CM, Sinha R, O’Malley SS. Eating disorders and alcohol use disorders. Alc Res Health. 2002;26:151–160. [Google Scholar]
- 7.Goldbloom DS, Naranjo CA, Bremner KE, Hicks LK. Eating disorders and alcohol abuse in women. Br J Addict. 1992;87:913–919. doi: 10.1111/j.1360-0443.1992.tb01986.x. [DOI] [PubMed] [Google Scholar]
- 8.Bulik CM. Drug and alcohol abuse by bulimic women and their families. Am J Psychiatry. 1987;144:1604–1606. doi: 10.1176/ajp.144.12.1604. [DOI] [PubMed] [Google Scholar]
- 9.Beary MD, Lacey JH, Merry J. Alcoholism and eating disorders in women of fertile age. Br J Addict. 1986;81:685–689. doi: 10.1111/j.1360-0443.1986.tb00389.x. [DOI] [PubMed] [Google Scholar]
- 10.Gordon SM, Hagan TA, Beyer E, Snyderman R. Eating disorders prevalent for female chemical dependence patients. J Addict Nur. 2001;13:209–214. [Google Scholar]
- 11.Gadalla T, Piron N. Co-occurrence of eating disorders and alcohol use disorders in women: A meta analysis. Arch Women’s Mental Health. 2007;10:133–140. doi: 10.1007/s00737-007-0184-x. [DOI] [PubMed] [Google Scholar]
- 12.Dunn EC, Larimer ME, Neighbors C. Alcohol and drug-related negative consequences in college students with bulimia nervosa and binge eating disorder. Int J Eat Disord. 2002;32:171–178. doi: 10.1002/eat.10075. [DOI] [PubMed] [Google Scholar]
- 13.Johnson JG, Cohen LK, Kasen S, Brook JS. Psychiatric disorders associated with risk for the development of eating disorders during adolescence and early adulthood. J Consult Clin Psychol. 2002;70:1119–1128. doi: 10.1037//0022-006x.70.5.1119. [DOI] [PubMed] [Google Scholar]
- 14.Lilenfeld LR, Kaye WH, Greeno CG, et al. Psychiatric disorders in women with bulimia nervosa and their first–degree relatives: Effects of comorbid substance dependence. Int J Eat Disord. 1997;22:253–264. doi: 10.1002/(sici)1098-108x(199711)22:3<253::aid-eat4>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 15.Suzuki K, Higuchi S, Yamada K, Mitzutani Y, Kono H. Young female alcoholics with and without eating disorders: A comparative study in Japan. Am J Psychiatry. 1993;150:1053–1058. doi: 10.1176/ajp.150.7.1053. [DOI] [PubMed] [Google Scholar]
- 16.Sansone RA, Fine MA, Nunn JL. A comparison of borderline personality symptomatology and self-destructive behavior in women with eating, substance abuse, and both eating and substance abuse disorders. J Pers Disord. 1994;8:219–228. [Google Scholar]
- 17.Deep AL, Lilenfeld LR, Plotnicov KH, Pollice C, Kaye WH. Sexual abuse in eating disorder subtypes and control women: The role of comorbid substance dependence in bulimia nervosa. Int J Eat Disord. 1999;25:1–10. doi: 10.1002/(sici)1098-108x(199901)25:1<1::aid-eat1>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 18.Dansky BS, Brewerton TD, Kilpatrick D. Comorbidity of bulimia nervosa and alcohol use disorders: Results from the National Women’s Study. Int J Eat Disord. 2000;27:180–190. doi: 10.1002/(sici)1098-108x(200003)27:2<180::aid-eat6>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 19.Corstorphine E, Waller G, Lawson R, Ganis C. Trauma and multi-impulsivity in the eating disorders. Eat Behav. 2007;8:23–30. doi: 10.1016/j.eatbeh.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 20.Lacey JH, Evans CH. The impulsivist: A multi-impulsive personality disorder. Br J Addict. 1986;81:641–649. doi: 10.1111/j.1360-0443.1986.tb00382.x. [DOI] [PubMed] [Google Scholar]
- 21.Najavits LM. Seeking Safety: A Treatment Manual for PTSD and Substance Abuse. Guilford Press; New York: 2002. [Google Scholar]
- 22.Hien DA, Wells E, Jiang H, et al. Effectiveness of two behavior therapy groups for women with PTSD and comorbid substance use disorders: Findings from the National Institute on Drug Abuse Clinical Trials Network “Women and Trauma” Multi-site Study. J Consult Clin Psychol. 2009;77:607–619. [Google Scholar]
- 23.Fairburn CG, Beglin SJ. Assessment of eating disorders: Interview or self-report questionnaire. Int J Eat Disord. 1994;16:363–370. [PubMed] [Google Scholar]
- 24.Fairburn CG, Cooper Z. The eating disorder examination. In: Fairburn CG, Wilson GT, editors. Binge Eating: Nature, Assessment and Treatment. 12th ed. Guilford Press; New York: 1993. pp. 317–360. [Google Scholar]
- 25.Garner D. Measurement of eating disorder psychopathology. In: Fairburn CG, Brownell KD, editors. Eating Disorders and Obesity: A Comprehensive Handbook. 2nd ed. Guilford Press; New York: 2002. pp. 141–146. [Google Scholar]
- 26.Mond JM, Hay PJ, Ridgers B, Owen C, Beumont PJV. Validity of the eating disorder examination questionnaire (EDE-Q) in screening for eating disorders in community samples. Beh Res Ther. 2004;42:551–567. doi: 10.1016/S0005-7967(03)00161-X. [DOI] [PubMed] [Google Scholar]
- 27.Carter JC, Aime AA, Fairburn CG. Assessment of bulimia nervosa: A comparison of interview and self-report questionnaire methods. Int J Eat Disord. 2001;30:187–192. doi: 10.1002/eat.1071. [DOI] [PubMed] [Google Scholar]
- 28.Wilfely DE, Schwartz MB, Spurrell EB, Fairburn CG. Assessing the specific psychopathology of binge eating disorder patients: Interview or self-report? Beh Res Ther. 1997;35:1151–1159. [PubMed] [Google Scholar]
- 29.Black C, Wilson GT. Assessment of eating disorders: Interview versus questionnaire. Int J Eat Disord. 1996;20:43–50. doi: 10.1002/(SICI)1098-108X(199607)20:1<43::AID-EAT5>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 30.Mond JM, Rodgers B, Hay PJ, Owen C, Beumont PJV. Temporal stability of the Eating Disorders Examination Questionnaire (EDE-Q) Int J Eat Disord. 2004;36:195–203. doi: 10.1002/eat.20017. [DOI] [PubMed] [Google Scholar]
- 31.Weathers FW, Keane TM, Davidson JR. Clinician-Administered PTSD Scale: A review of the first ten years of research. Depress Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- 32.Foa E, Riggs DS, Dancu CV, Constance V, Rothbaum BO. Reliability and validity of a brief instrument for assessing posttraumatic stress disorder. J Trauma Stress. 1993;6:459–473. [Google Scholar]
- 33.Derogatis LR, Melisaratos N. The brief symptom inventory: An introductory report. Psychol Med. 1983;13:595–605. [PubMed] [Google Scholar]
- 34.Dansky BS, Brewerton DG, Kilpatrick DG, O’Neil PM. The National women study: relationship of victimization and post traumatic stress disorder to bulimia nervosa. Int J Eat Disord. 1997;21:213–228. doi: 10.1002/(sici)1098-108x(199704)21:3<213::aid-eat2>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 35.Diggle PJ, Liang KY, Zeger SL. Analysis of Longitudinal Data. Oxford University Press; London: 1994. [Google Scholar]
- 36.Bonfa F, Cabrini S, Avanzi M, Bettinardi O, Spotti R, Uber E. Treatment dropout in drug-addicted women: Are eating disorders implicated? Eat Weight Disord. 2008;13:81–86. doi: 10.1007/BF03327607. [DOI] [PubMed] [Google Scholar]
- 37.Wilson GT. Cognitive behavior therapy for eating disorders: progress and problems. Behav Res Ther. 1999;37:S79–S95. doi: 10.1016/s0005-7967(99)00051-0. [DOI] [PubMed] [Google Scholar]
- 38.Gordon S, Johnson A, Greenfield SF, Cohen LR, Killeen T, Roman P. Treatment of co-occurring eating disorders in publicly funded addiction treatment programs. Psychiatr Serv. 2008;59:1056–1059. doi: 10.1176/appi.ps.59.9.1056. [DOI] [PMC free article] [PubMed] [Google Scholar]