Abstract
Background
Effective patient-clinician communication is at the heart of good health care and may be even more vital for older patients and their nurse practitioners (NPs).
Objectives
To examine contributions of older patients’ and NPs’ characteristics and the content and relationship components of their communication to patients’ proximal outcomes (satisfaction and intention to adhere) and longer-term outcomes (changes in presenting problems, physical health, and mental health), and contributions of proximal outcomes to longer-term outcomes.
Methods
Visits were videorecorded of a statewide sample of 31 NPs and 155 older patients. Patients’ and NPs’ communication during visits were measured using the Roter Interaction Analysis System for verbal activities, a check sheet for nonverbal activities, and an inventory of relationship dimension items. Proximal outcomes were measured with single items after visits. At 4 weeks, change in presenting problems was measured with a single item and physical and mental health changes were measured with the SF-12v2 Health Survey. Mixed models regression with backward deletion was conducted until only predictors with p ≤ .05 remained in the models.
Results
With the other variables in the models held constant, better outcomes were related to background characteristics of poorer baseline health, nonmanaged care settings, and more NP experience; to a content component of seeking and giving biomedical and psychosocial information; and to a relationship component of more positive talk and greater trust and receptivity and affection, depth, and similarity. Poorer outcomes were associated with higher rates of lifestyle discussion and NPs’ rapport building that patients may have perceived to be patronizing. Greater intention to adhere was associated with greater improvement in presenting problems.
Discussion
Older patient-NP communication was effective regarding seeking and giving biomedical and psychosocial information other than that involving lifestyle. Studies of ways to improve older patient-NP lifestyle discussions and rapport building are needed.
Keywords: communication, nurse-patient relations, outcome assessment (health care), aged, nurse practitioner, ambulatory care, mixed models
Effective patient-clinician communication is at the heart of good health care (Institute of Medicine, 2001) and may be even more vital for older patients and their nurse practitioners (NPs). The complex health care needs created by chronic illnesses and medication regimens of many older people require a greater exchange of information to achieve desired health outcomes. Furthermore, the number of visits by older patients to NPs is increasing. Patients age 65 years or older made an estimated 2.45 million visits to NPs or certified nurse midwives in office or hospital outpatient settings during 2003 and 4.65 million during 2006 (National Center for Health Statistics, n.d.). Therefore, understanding the association between older patient-NP communication and visit outcomes is important and timely.
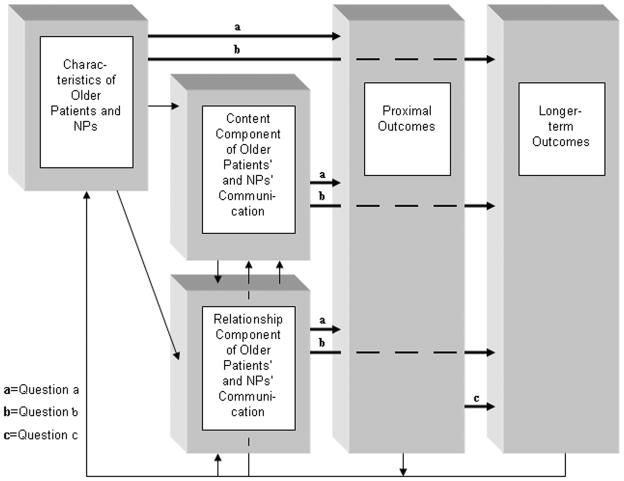
Interpersonal communication, at a minimum, is the transmission of a signal from one person to another. As in all interpersonal communication, older patient-NP communication has a content component and a relationship component (Burgoon & Hale, 1984; Watzlawick, Beavin, & Jackson, 1967; Figure 1). The content component is the literal subject matter of the communication, whereas the relationship component is information about the nature of the interpersonal relationship between the two people. The signals for both components include verbal and nonverbal activities; however, content signals usually are verbal activities only; relationship signals are both nonverbal and verbal activities. Thus, within the context of older patients’ and NPs’ background characteristics, it is by means of the content and relationship components of communication that older patients express their health problems, exchange information with their NPs about their concerns and their relationship, and understand and finalize a plan of care. When their communication is associated positively with such proximal outcomes as satisfaction with the visit and such longer-term outcomes as improvement in health status, the communication can be considered effective. Proximal outcomes are related to longer-term outcomes (Inui & Carter, 1985), and outcomes feed back to influence the content and relationship components of communication as well as those background characteristics that are modifiable. The concepts and links a, b, and c of the theoretical framework depicted in Figure 1 were examined in the present study.
Figure 1.
Framework for study of older patient-NP communication and outcomes
Background Characteristics
Numerous characteristics have been found to influence patient-physician communication. These include ethnicity (Street, Gordon, & Haidet, 2007), baseline health (Zandbelt, Smets, Oort, Godfried, & de Haes, 2007), clinicians’ specialty (Paasche-Orlow & Roter, 2003) and experience (Roter & Larson, 2001), managed vs. nonmanaged care setting (Shapiro, Tym, Eastwood, Derse, & Klein, 2003), and length of visit (Mechanic, McAlpine, & Rosenthal, 2001). However, knowledge concerning the influence of background characteristics on patient-NP communication and patients’ outcomes is not extensive. Hayes (2007) found that patients’ age, gender, and length of acquaintance with their NPs were correlated positively with the proximal outcome of patients’ satisfaction in interviews of 103 adult patients. In contrast, Green and Davis (2005) found that patients’ age, but not patients’ gender, ethnicity, education, or income; NPs’ gender; or rural vs. urban practice setting, were associated with patients’ satisfaction in a survey of 36 NPs and 817 adult patients. The different results may be due to differences in samples, variables, methods of data collection, measures, or methods of analysis.
Content Component of Communication
Within the content component of patient-NP communication, the predominant types of verbal activities during primary health care visits have been found to be seeking and giving information for diagnosis and treatment. In a content analysis of 136 videorecorded visits between younger patients and NPs at 60 clinic sites, Campbell, Mauksch, Neikirk, and Hosokawa (1990) found that 43% of NPs’ communication was related to biomedical or psychosocial diagnosis or treatment and 26% to giving information. More recently, in a content analysis of audiorecorded visits between five adult patients and NPs, Berry (2006) found that 50% of the NPs’ communication was seeking information and 37% was giving information.
Less is known about the outcomes of older patient-NP verbal activities than about those of physicians. Paasche-Orlow and Roter (2003) examined the proximal outcome of patients’ satisfaction with communication in audiorecorded primary care visits between 564 adult patients and 59 physicians using the Roter Interaction Analysis System (RIAS). They found that physicians’ psychosocial communication (e.g., seeking psychosocial information) was related positively to satisfaction. In a survey of 1,588 older patients with diabetes, Heisler, Cole, Weir, Kerr, and Hayward (2007) found that physicians’ giving information was related to longer-term outcomes of medication adherence and foot care. Overall, studies indicate that a content component of seeking and giving information tends to represent effective patient-physician communication.
Relationship Component of Communication
Within the relationship component of communication, the types of nonverbal activities most often identified as important in nursing are gazes, nods or shakes of the head, eyebrow movements, smiles, direct interpersonal orientation, interpersonal touches, and back-channels (Caris-Verhallen, de Gruijter, Kerkstra, & Bensing, 1999; Gilbert, 2004). Mast, Hall, Kockner, and Choi (2008) examined nonverbal activities among 163 adult observers of 11 videorecorded patient-physician encounters. They found that observers’ satisfaction with female physicians was correlated highly with more nodding, brow lowering, gazing, and forward leaning. Other than satisfaction, however, little is known about nonverbal activities and outcomes.
Verbal activities within the relationship component have been studied more extensively, but conceptualizations of the type of relationship information transmitted by these verbal signals differ widely. In the studies of NPs’ verbal activities described earlier, Campbell et al. (1990) examined relationship information conceptualized as affiliation (e.g., providing support) and control, whereas Berry examined relationship information conceptualized as partnership building (e.g., restatement) and positive talk (e.g., approving). In the studies of the effectiveness of physicians’ verbal activities, Paasche-Orlow and Roter (2003) found that relationship information conceptualized as rapport building (e.g., expressing concern) was correlated positively with satisfaction. Heisler et al. (2007) found that relationship information conceptualized as nondominance (i.e., participatory decision making) was related to blood glucose monitoring, exercise, and diet.
In an effort to clarify the conceptualization of relationship messages signaled by nonverbal and verbal activities, Burgoon and Hale (1984, 1987) identified as many as 12 distinct dimensions. Dimensions examined in relation to effective health care communication include nondominance, trust, and affection. Lawson (2002), in audiorecordings of 124 adult patients with 9 clinicians, found no correlation between nondominance and patient satisfaction. In a survey of 7,204 adult patients concerning their primary care physicians, Safran et al. (1998) found that trust was correlated positively with satisfaction, adherence, and health improvement. Controlling for age, gender, ethnicity, and patient’s verbal communication, Gilbert (1998) found that satisfaction ratings of 126 observers of videorecorded communication of nurses listening to a simulated patient in an outpatient setting were correlated positively with trust and receptivity and affection, depth, and similarity. The latter finding was unexpected since affection usually is considered to have higher salience in social rather than in professional relationships (Arnold & Boggs, 1999). Unfortunately, the multidimensional nature of the relationship component in health care communication remains largely unexplored.
Outcomes
Knowledge of the influence of patient-clinician visit outcomes on each other also is minimal. Jackson and Kroenke (2001) reported significant correlations between the proximal outcome of satisfaction and longer-term outcomes of symptom resolution and functional status in a pre- and postvisit survey of physicians and 750 adults with acute health problems in ambulatory settings. In contrast, Hayes (2007) noted a significant correlation between proximal outcomes of satisfaction and intention to adhere to recommendations, but not between satisfaction and recall of recommendations or between recall and intention to adhere, in interviews of 103 adult patients of NPs in eight primary care sites. For 60 adults interviewed within 6 weeks of their discharge from a home care nursing agency, Ervin, Chen, and Upshaw (2006) found a significant correlation between longer-term outcomes of patient-reported symptom reduction and well-being, but not between adherence and symptom reduction or between adherence and well-being. Thus, although the link between proximal and longer-term outcomes has been proposed (Inui & Carter, 1985), the findings from research are inconclusive.
Research Questions
Knowledge concerning effective patient-clinician communication consists largely of the background characteristics and variables within the content and relationship components of their communication that are associated positively with outcomes, especially satisfaction. However, this knowledge is limited by lack of attention to older patients and NPs, varying conceptualizations of the relationship component, and analyses often inappropriate for multiple patients per clinician. Further, knowledge is fragmented because variables usually are considered two at a time. For example, greater satisfaction has been associated with older age in many studies (e.g., Green & Davis, 2005; Hayes, 2007). However, if satisfaction were due to the way clinicians communicate with older patients, and not to older age itself, satisfaction would be unrelated to age when both age and clinicians’ manner of communication were considered in the same analysis.
To examine a fuller range of variables, the questions examined in the present study were complex: (a) Do background characteristics of older patients and NPs and the content and relationship components of their communication during visits contribute to patients’ proximal outcomes of satisfaction with the visit and intention to adhere to the recommended plan? (b) Do background characteristics of older patients and NPs and the content and relationship components of their communication during visits contribute to patients’ longer-term outcomes of changes in presenting problems, physical health, and mental health? and (c) Do the proximal outcomes contribute to the longer-term outcomes?
Methods
Sample
Study participants were 31 NPs and 155 of their older patients throughout a New England state. For inclusion in the sample, patients and NPs had to be English-speaking and had to self-identify as United States-born European Americans or African Americans. Although both male and female patients were eligible, only female NPs were included in order to manage some of the variability of gender-based combinations of patients and clinicians. Additional requirements for NPs were that they regularly provided care to older patients in clinic or office sites and that their sites had adequate space for videorecording the visits. Nurse practitioners were excluded if they had inadequate numbers of older patients during the data collection period.
Additional inclusion criteria for patients were an age of 65 years or older, a scheduled appointment to see a participating NP, an absence of cognitive impairment as judged by their NP, and a home telephone. Patients were excluded if they were acutely ill at the time of the visit, were unable to understand the data collection process, or were unable to undertake the scheduled visit without the presence of a third person.
Of the 56 NPs who were eligible and agreed to participate, 25 did not complete the study due to such reasons as job changes or absence of administrative support for the study, leaving 31 in the final NP sample. Of the eligible and interested patients, 11 had incomplete data due to videorecording equipment malfunctions, and 2 were lost to follow-up. All these patients were replaced with their NP’s other eligible patients; thus, there were 155 in the final patient sample--that is, 5 patients per NP.
Measures
Background characteristics
Ten characteristics of patients and NPs were measured by semistructured demographic items. For patients, these were age, gender, ethnicity, the presenting problems that prompted their visit (stable or unstable), and how long they had known the NP. Items for the characteristics of NPs were age, ethnicity, practice specialty, years of experience, and type of setting (managed or nonmanaged care). Three additional characteristics were measured: length of visit determined in minutes from the length of the videorecordings, and patients’ baseline physical health and baseline mental health measured using the SF-12v2 Health Survey, described below. Thus, there were 13 background characteristics considered in the analysis.
Roter Interaction Analysis System
Trained members of Roter’s research team measured the verbal content using the RIAS (Roter & Larson, 2002), a coding system that has been used in over 100 studies of clinicians’ communication (Roter, 2008). The RIAS consists of 69 categories to code the frequency of all verbal “utterances”; that is, all complete or partial thoughts expressed aloud by patients and NPs in recordings of the visits. The predictive validity of RIAS has been supported in numerous studies, and the intercoder reliability within Roter’s research team for both patient and clinician categories has averaged r = 0.85 (Roter & Larson, 2002). In the present study, back-channel responses (e.g., “Mm-hmm”) and NPs’ agreements (e.g., “Okay”) were considered to be nonverbal activities and were excluded from the analysis as verbal activities. Because of the difficulty in interpreting the meaning of unintelligible, other, and communication facilitators (e.g., “Well,…” when transitioning from one topic to another), given the framework of this study, these categories were excluded entirely. Categories not observed in a 10% sample of recorded visits and those with reliability of r < 0.65 were not considered further, except for the low frequency categories of seeking and giving psychosocial information by patients and NPs because of their possible importance in relation to the outcome of patients’ mental health status. Open and closed categories of NPs’ medical, therapeutic, lifestyle, and psychosocial information-seeking were combined, leaving a total of 43 verbal categories (median, r = 0.95; range, not observed to r = 1.00) for analysis. After being divided by length of the visit, the verbal categories were analyzed as rates per minute.
Nonverbal activity check sheet
Nonverbal activities for patients and NPs were scored on a grid in which the rows represented time in seconds and the columns represented the activities (Gilbert, 1993). Activities of interest during each second of a 30-second sample of the recorded visits were gazes, nods or shakes of the head, eyebrow movements, smiles, direct interpersonal orientations, interpersonal touches, and back-channels. An activity occurring at least once during a 1-second time interval was scored as 1, except that gazes were scored as 2 due to the importance of gazes in interpersonal communication (Ruusuvuori, 2001). Thus, the total scores for nonverbal activity of patients and of NPs could range from a rate of 0 to 8 per second. All activities noted on the check sheets by two trained observers were compared, second-by-second; any disagreements were resolved by the principal investigator. Coordination of NPs’ nonverbal activities with those of their patients was measured as the squared regression coefficient of the NP’s rate of activities predicted by her patient’s rate during the same second, after forcing into the model the NP’s rate of activities during the prior second (Gilbert, 1993, 2004).
Relational Themes Inventory
Dimensions of relationship messages were measured by an inventory that included 30 items based on the work of Burgoon and Hale (1984, 1987), further developed and tested in studies of patient-nurse interactions (Gilbert, 1998, 2004). On a Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree), patients were asked to respond to statements about the visit they had just had with their NP. Responses were recoded as necessary so that higher scores reflected a more positive relationship. Gilbert (1998) reported Cronbach’s alphas ranging from 0.90 for trust and receptivity to 0.71 for depth and similarity (reconfigured as affection, depth, and similarity based on subsequent analysis). In the present study, after deleting items with little variability and items with low item-to-total correlations, relationship dimensions of nondominance (2 items), trust and receptivity (2 items), and affection, depth, and similarity (6 items) had Cronbach’s alphas of 0.72, 0.80, and 0.72, respectively.
Satisfaction with the visit
The proximal outcome of satisfaction with the visit was measured using one item derived from the extensively used Consumer Assessment of Health Care Providers Survey (Agency for Healthcare Research and Quality, 2002). On a scale ranging from 1 (worst care possible) to 10 (best care possible), older patients were asked whether the visit with their NP “was an example of the worst or best health care possible.” Single-item measures have been shown to be valid measures to obtain individuals’ perceptions of a particular situation (Youngblut & Casper, 1993). As evidence for the reliability of the item in the present study, the correlation between scores on satisfaction with the visit and the mean of questions concerning satisfaction with the NP’s communication that were derived from the Patient Satisfaction Instrument (Risser, 1975; Yellen, 2003) was r = 0.72.
Intention to adhere
The proximal outcome of intention to adhere to the recommendations the patient recalled being made by the NP was measured on a scale ranging from 1 (very likely to follow the recommendation) to 5 (very unlikely to follow the recommendation). Immediately after the visit, patients identified the recommendations they recalled. Their intention to adhere to each recalled recommendation was measured by asking, “One of the things you remembered the NP told you about taking care of your health was ____. How likely are you to do that?” Intention scores were calculated by summing each patient’s responses and dividing by the number of recommendations he or she recalled, so that scores were comparable across patients regardless of the number of recommendations patients recalled. Four weeks after the visit, by telephone, adherence to each recalled recommendation was measured in a similar manner. As evidence for the reliability of the intention to adhere measure in the present study, the correlation between patients’ intention immediately after the visit and their adherence at 4 weeks was r = 0.63.
Change in presenting problems
To measure the longer-term outcome of change in presenting problems, patients were asked 4 weeks after the visit about the change, if any, in each presenting problem they had identified to investigators prior to their visit with the NPs. Scores could range from 1 (gotten a lot worse) to 7 (improved a lot). The sum of each patient’s responses, divided by the number of his or her presenting problems, was used as that patient’s score for change in presenting problems.
SF-12 Health Survey (Version 2.0)
The SF-12v2 (Ware, Kosinski, Turner-Bowker, & Gandek, 2002) was used to measure changes in the longer-term outcomes of physical health and mental health. It consisted of 12 questions to which patients responded using 3- or 5-point rating scales, depending on the item, immediately after the visit and at 4 weeks. Items were reverse-coded as needed, aggregated, norm-based for age, and transformed so that scores above 50 meant relatively good physical or mental health. The validity, reliability, and 4-week sensitivity of the SF-12 have been tested extensively. Among people age 65 years and older, Ware, Kosinski, Turner-Bowker, and Gandek (2002) reported reliability coefficients of 0.89 for physical health and 0.82 for mental health. Cronbach’s alphas for physical and mental health for the previsit administration of the SF-12v2 in the present study were 0.87 and 0.77, respectively.
Procedure
The study was approved by the investigators’ university institutional review board as well as by the appropriate boards and individuals at participating NPs’ sites. Participants were aware that the study involved older patient-NP communication and outcomes during visits and that the visits would be videorecorded. They were assured that NPs could cap the cameras if, for example, patients needed to undress, and that NPs could turn the cameras off entirely at any time.
From a list of 4,700 NPs provided by the State Board of Nursing, 2,500 NPs were selected randomly to be invited to participate. This large number of invitations was needed because NPs on the list who met the eligibility criteria could not be differentiated from NPs who did not. In addition to the NPs selected randomly, all NPs residing in ZIP codes that had a high percentage of African Americans were invited, resulting in 1,000 additional invitations for a total of 3,500 invitations mailed. Other methods of recruiting African American participants were announcements to groups such as the Black Nurses’ Association and various NP organizations.
The NPs who accepted the invitations were contacted by an investigator who obtained their informed consent and background characteristics and ascertained site approval procedures. Except for two sites requiring that researcher contact be patient-initiated, NPs contacted 10 eligible patients with visits scheduled for the days of data collection and obtained their permission for an investigator to invite their participation. Prior to the scheduled visits, an investigator randomly selected patients from the 10 until at least 5 agreed to participate.
When patients arrived for their visits, a member of the research team obtained their informed consent, read the demographic items and SF-12v2 to them, and made note of their responses. The relationship items, satisfaction, recall of NPs’ recommendations, and adherence intention data were collected in the same manner after the visit. Four weeks after the visit, adherence, SF-12v2, and improvement questions were read to patients by telephone.
Visits were videorecorded using two camcorders on tripods behind and over the shoulder of NPs and patients so that full frontal views of each could be obtained. To reduce reactivity, participants were given the opportunity to view themselves on the camcorders’ screens prior to the visit, and camcorders were unattended by the research team during the visit.
Two trained observers viewed a segment of each of the 155 video recordings in slow motion and real time to score the nonverbal activities of patients and NPs using the check sheet. This segment started with the patients’ first utterance of the problem they had said most worried them prior to their visit and ended 30 sec later. The observers were trained by scoring interactions with known reliability and comparing their scores to those previously obtained. The complete sound tracks of the video recordings were coded for patients’ and NPs’ verbal activities by Roter’s research team.
Data for this study consisted of 62 predictor variables and 5 outcomes variables. Distributions of many variables were skewed; however, results of analyses using transformed and untransformed data did not differ substantially. Therefore, the results using untransformed data are reported below. Pairwise analyses of the predictor variables revealed no collinearity.
The data were analyzed using the mixed models regression procedure of SAS 9.1 (SAS Institute Inc., Cary, NC). Use of mixed models accounts for the contribution of the variation in NPs to other variables and, thus, was appropriate for this study with multiple older patients per NP. The model that was fitted was as follows. For the jth patient on the ith NP,
where μ is the overall intercept; Ni is the random effect (with mean 0) for NP i; xijk is the kth variable--that is, a background characteristics or a variable within the content or relational components of communication, for the jth patient on the ith NP; Bk is the coefficient of xijk; and eijk is an additional noise term (also with mean 0) that is assumed to be independent. In mixed model analyses, the coefficients are robust to any assumptions about the random quantities (Ni and eijk). However, inferences about variability due to NPs (the variance of Ni) are based on normality assumptions.
To reduce the number of predictor variables, each was analyzed separately for each outcome. Forty-seven of the 62 variables were related to one or more of the outcomes with a criterion of p ≤ .15. All predictor variables that met this initial screening criterion for an outcome were analyzed for that outcome by deleting predictors backwards from the regression models, one-by-one, until only those with p values ≤ .05 remained in the final models. Analyses of the model residuals versus each predictor variable in the model revealed no unexplained structure in the data; thus, the final models were deemed adequate.
Results
A description of the older patient and NP participants at baseline is presented in Table 1. The majority of patients were European American women aged 70 to 80 years who had known their NP for 3 years on average. Most NPs were middle-aged, European American women who worked in private offices in rural or suburban locations. About half of NPs were certified as Family Nurse Practitioners. The mean length of visits was about 23 minutes.
Table 1.
Characteristics of Older Patient and Nurse Practitioner Participants at Baseline
| Variable | Patients (n = 155) | NPs (n = 31) |
|---|---|---|
| Age, in years | M = 75.37 (SD = 7.38) | M = 48.16 (SD = 7.15) |
| Female | 104 (67%) | 31 (100%) |
| European American (vs. African American) | 149 (96%) | 28 (90%) |
| Married | 65 (42%) | |
| Length of prior acquaintance with NP, in years | M = 3.01 (SD = 3.16) | |
| Certified as Family Nurse Practitioner | 15 (48%) | |
| Practice characteristics: | ||
| Private office (vs. hospital clinic) | 19 (61%) | |
| Rural or suburban location (vs. urban) | 16 (52%) | |
| Length of visit, in min | M = 23.14 (SD = 11.97) | |
Note. NP = Nurse practitioner
Outcomes, background characteristics, and variables within the content and relationship components of patients’ and NPs’ communication that were associated with patients’ outcomes at p ≤ .05 are presented in Table 2. Patients’ satisfaction with the visit and their intention to adhere to the NPs’ recommendations were high. The mean change in presenting problems was above the midpoint of the scale at 4 weeks; that is, although many patients reported that these problems improved at 4 weeks, the remainder reported that these problems stayed the same or became worse. The average changes in patients’ physical health scores and mental health scores were close to 0 at 4 weeks.
Table 2.
Description of Outcomes and Predictor Variables in the Final Regression Models (N =155 Older Patients and 31 Nurse Practitioners)
| Variable Outcome | M (SD) | % |
|---|---|---|
| Satisfaction (10 = best care possible) | 9.68 (0.75) | |
| Intention to adhere (5 = very likely to follow recommendations) | 4.75 (0.52) | |
| Change in most worrisome presenting problems (7 = improved a lot) | 5.39 (1.45) | |
| Change in physical health at 4 weeks (0 = no change) | 1.12 (7.36) | |
| Change in mental health at 4 weeks (0 = no change) | −0.36 (7.18) | |
| Background Characteristic | ||
| Physical health at baseline (50 = relatively good physical health) | 43.90 (11.45) | |
| Mental health at baseline (50 = relatively good mental health) | 53.44 (8.20) | |
| Stable presenting problem (vs. unstable) | 62a | |
| Nonmanaged care practice (vs. managed care) | 81b | |
| NPs’ experience, in years | 10.90 (6.21) | |
| Content Component of Communication, in rate per min | ||
| Patients giving medical information | 2.45 (1.27) | |
| Patients seeking information about therapy | 0.15 (0.16) | |
| NPs orienting or instructing | 0.79 (0.48) | |
| NPs giving lifestyle information | 0.54 (0.62) | |
| Patients giving lifestyle information | 2.06 (1.46) | |
| NPs seeking psychosocial information | 0.08 (0.12) | |
| Relationship Component of Communication | ||
| Patients approving | 0.10 (0.12) | |
| Patients agreeing | 2.77 (1.42) | |
| NPs approving | 0.29 (0.24) | |
| NPs saying complimentary things about other providers | 0.02 (0.05) | |
| NPs expressing concern | 0.41 (0.31) | |
| NPs expressing reassurance and optimism | 1.02 (0.64) | |
| NPs’ nonverbal activities, in rate per second | 2.80 (0.85) | |
| NPs coordinating their nonverbal activities | 0.06 (0.08) | |
| Trust and receptivity (7 = strongly agree) | 6.95 (0.20) | |
| Affection, depth, and similarity (7 = strongly agree) | 5.15 (1.13) | |
Notes. NP = Nurse practitioner
n=96 patients
n=25 practice settings
The first research question examined in this study was whether background characteristics of older patients and NPs and the content and relationship components of their communication during visits contributed to patients’ proximal outcomes (Figure 1, a links). Results of mixed model regression analysis for the proximal outcomes are presented in Table 3. For the outcome of satisfaction, 16 variables met the initial screening criterion. In the final model, greater satisfaction was associated with higher rates of patients’ approving and agreeing and lower rates of NPs’ expressing concern. Greater satisfaction also was associated with lower rates of NPs’ nonverbal activities during discussions of patients’ presenting problems and greater trust and receptivity and affection, depth, and similarity. For the outcome of intention to adhere to recommendations, 10 variables met the initial screening criterion. In the final model, greater intention to adhere was associated with nonmanaged care settings as well as higher rates of patients agreeing, higher rates of NPs orienting and instructing such as during a physical exam, and lower rates of patients giving lifestyle information.
Table 3.
Associations of Older Patients’ and NPs’ Characteristics and the Content and Relationship Components of Their Communication with Patients’ Proximal Outcomes of Satisfaction and Intention to Adhere (n =155 Older Patients and 31 Nurse Practitioners)
| Predictor Variable | Estimatea | SEb | t | p |
|---|---|---|---|---|
| Satisfaction With the Visit | ||||
| Patients approving | 1.11 | 0.47 | 2.37 | .02 |
| Patients agreeing | 0.11 | 0.04 | 2.64 | < .01 |
| NPs expressing concern | −0.53 | 0.19 | −2.79 | < .01 |
| NPs’ rate of nonverbal activities | −0.15 | 0.07 | −2.24 | .03 |
| Trust and receptivity | 0.89 | 0.28 | 3.21 | < .01 |
| Affection, depth, and similarity | 0.11 | 0.05 | 2.33 | .02 |
| Intention to Adhere | ||||
| Type of setting (managed care = 1) | −0.22 | 0.1 | −2.12 | .04 |
| Patients agreeing | 0.07 | 0.03 | 2.43 | .02 |
| Patients giving lifestyle information | −0.08 | 0.03 | −3.03 | < .01 |
| NPs orienting and instructing | 0.21 | 0.08 | 2.6 | .01 |
Notes. NP = Nurse practitioner
Estimate of the population coefficient
Standard error of the estimate
The second research question was whether background characteristics and the content and relationship components of older patient-NP communication during visits contribute to patients’ longer-term outcomes (See Figure 1, b links). Results of mixed model regression analysis for the longer-term outcomes are presented in Table 4. For the outcome of change in patients’ presenting problems, 16 variables met the initial screening criterion. In the final model, improvement in presenting problems was associated with unstable presenting problems and with higher rates of NPs approving and lower rates of NPs giving lifestyle information. For change in physical health, 14 variables met the screening criterion. In the final model, improved physical health was associated with poorer physical health at baseline and with higher rates of patients giving medical information, higher rates of NPs saying complimentary things about other providers, and lower rates of NPs giving lifestyle information. Improved physical health also was associated with lower rates of NPs coordinating their nonverbal activities with the patients’ nonverbal activities and greater trust and receptivity. For change in mental health, 14 variables met the screening criterion. In the final model, improved mental health was associated with poorer mental health of patients at baseline and more years of NPs’ experience; with higher rates of patients seeking information about their therapy, higher rates of NPs seeking psychosocial information, and lower rates of NPs expressing reassurance and optimism; and with lower rates of NPs coordinating their nonverbal activities with those of patients.
Table 4.
Associations of Older Patients’ and NPs’ Characteristics and the Content and Relationship Components of Their Communication with Patients’ Longer-Term Outcomes of Changes in Presenting Problem, Physical Health, and Mental Health at Four Weeks (n =155 Older Patients and 31 Nurse Practitioners)
| Predictor Variable | Estimatea | SEb | t | p |
|---|---|---|---|---|
| Change in Presenting Problems | ||||
| Stability of presenting problems (unstable = 1) | 0.49 | 0.23 | 2.14 | .03 |
| NPs approving | 1.18 | 0.47 | 2.54 | .01 |
| NPs giving lifestyle information | −0.57 | 0.18 | −3.23 | < .01 |
| Change in Physical Health | ||||
| Patients’ physical health at baseline | −0.2 | 0.05 | −4.44 | < .01 |
| Patients giving medical information | 0.94 | 0.43 | 2.18 | .03 |
| NPs complimenting | 23.5 | 9.68 | 2.43 | .02 |
| NPs giving lifestyle information | −2.36 | 0.88 | −2.68 | < .01 |
| NPs coordinating their nonverbal activities | −19.59 | 7.03 | −2.79 | < .01 |
| Trust and receptivity | 5.37 | 2.58 | 2.09 | .04 |
| Change in Mental Health | ||||
| Patients mental health at baseline | −0.28 | 0.06 | −4.49 | < .01 |
| NPs years of experience | 0.21 | 0.09 | 2.28 | 0.02 |
| Patients seeking information about therapy | 10.36 | 3.13 | 3.31 | < .01 |
| NPs seeking psychosocial information | 13.85 | 4.42 | 3.13 | < .01 |
| NPs expressing reassurance or optimism | −2.21 | 0.79 | −2.8 | < .01 |
| NPs coordinating their nonverbal activities | −13.79 | 6.44 | −2.14 | 0.03 |
Notes. NP = Nurse practitioner
Estimate of population coefficient
Standard error of the estimate
The third research question examined in this study was whether the proximal outcomes of satisfaction with the visit and intention to adhere to recommendations contributed to the longer-term outcomes of changes in patients’ presenting problems, physical health, and mental health (Figure 1, c link). The analysis revealed that greater intention to adhere contributed to improvement in patients’ presenting problems at 4 weeks (Estimate = 0.93, SE = 0.21, t = 4.34, p < .01), but otherwise proximal and longer-term outcomes were not associated at p ≤ .05.
Discussion
This study examined background characteristics of older patients and NPs and the content and relationship components of their communication that contributed to outcomes in a statewide sample. The patients and NPs in the study were comparable to those in other studies in several ways. Patients’ physical health and mental health at baseline approximated the norm for older patients (Ware et al., 2002). Their high degree of satisfaction has been reported frequently in NP studies (e.g., Hayes, 2007). The mean length of visits between the patients and NPs was comparable to the lengths of national patient-NP visits of about 27 min (Swartz et al., 2003) and older patient-physician visits of about 22 min (Mann et al., 2001). However, study NPs were about 4 years older and had about 2 more years of experience than NPs in a national survey (Swartz et al., 2003). Ten percent of the NPs were African American, which is higher than the 3% reported nationally (Swartz et al., 2003), probably due to study recruitment efforts. These NP recruitment efforts did not result in a similarly high number of African American patients. Only 4% of patients were African American, lower than the 19% reported nationally (Swartz et al.). In addition, the stability of patients’ presenting problems was higher than in other samples of NPs’ primary care practices (Deshefy-Longhi, Swartz, & Grey, 2008), probably because only patients with scheduled visits were included in the study.
Twenty-one predictor variables were associated with effective older patient-NP communication in one or more of the final models. All interpretations of results are for the coefficients being discussed with the other variables in the models held constant. Of the background characteristics, unstable presenting problems and poorer baseline physical and mental health were associated with better longer-term outcomes. A likely explanation is that unstable problems and poorer health at baseline provided a less restricted range for improvement at 4 weeks. Nonmanaged care setting and greater NP experience contributed to one outcome each. On the whole, however, background characteristics such as patients’ age did not make a major contribution to outcomes in this study, given the other variables in the models.
Within the content component of communication, there were two patterns of communication in the results. Consistent with the findings of Paasche-Orlow and Roter (2003) and Heisler et al. (2007), the first pattern was seeking and giving information (Berry, 2006; Roter & Larson, 2001) other than lifestyle discussions. Higher rates of orienting or instructing by NPs, such as during a physical exam, were associated with greater intention to adhere. Higher rates of patients giving medical information were associated with greater improvement in physical health. Patients seeking more information about therapy and NPs seeking more psychosocial information were associated with greater improvement in mental health, although the low reliability for psychosocial content is a study limitation. That said, seeking and giving biomedical and psychosocial information represented effective communication overall.
Lifestyle discussions, however, represented a second, contrasting pattern of communication: more lifestyle discussion contributed to less effective communication, given the other variables in the models. Higher rates of patients giving lifestyle information were associated with less intention to adhere and higher rates of NPs giving lifestyle information were associated with less improvement in presenting problems and physical health. Other investigators also have noted poorer outcomes of lifestyle discussions. Hayes (2007), for example, found that patients intended to adhere less to NPs’ lifestyle recommendations regarding diet, exercise, or smoking cessation than to recommendations related to medications, laboratory tests, or referrals to specialists. When good outcomes depended on lifestyle discussions in the present study, the outcomes may have been difficult to achieve within 4 weeks.
Within the relationship component of communication, there were three patterns in the results. First was a pattern of positive talk (Berry, 2006; Roter & Larson, 2001). Higher rates of patients approving of the NP or agreeing during visits were associated with better proximal outcomes. Higher rates of NPs approving of the older patient or saying complimentary things about clinicians working with the patient outside their health agencies were associated with longer-term outcomes of greater improvement in presenting problems and physical health. When older patients voiced positive expressions at the time of visits, and when NPs said they saw progress and good outside treatment, the patients tended to report better outcomes.
A second pattern within the relationship component involved the relationship dimensions. Consistent with the findings of Gilbert (1998), higher trust and receptivity and higher affection, depth, and similarity were associated with greater postvisit satisfaction. Consistent with Safran et al. (1998), higher trust and receptivity also was associated with greater improvement in physical health at 4 weeks. That trust and receptivity and satisfaction were associated is not surprising: Risser’s (1975) classic satisfaction instrument even includes trust as a measure of patients’ satisfaction with nurses in primary care. However, the contribution of trust and receptivity to improved physical health underscores the importance of the relationship component of older patient-NP communication in general and the dimension of trust in particular.
The third pattern was that of rapport building, involving both verbal (Paasche-Orlow & Roter, 2003) and nonverbal (Duggan & Parrott, 2001) activities. More verbal and nonverbal rapport building activities contributed to less effective communication, given the other variables in the models. Higher rates of NPs’ expressions of concern and nonverbal activities were associated with postvisit dissatisfaction, higher rates of NPs’ coordination of nonverbal activities were associated with less improvement in physical health, and higher rates of NPs’ reassurance and optimism and coordination of nonverbal activities were associated with less improvement in mental health. It may be that patients whose health problems were more straightforward or already resolving well had good outcomes without NPs’ rapport building. Conversely, NPs may have offered rapport building when older patients’ problems were more threatening or not resolving well, and rapport building was insufficient to have influenced the outcomes in a positive direction.
Alternatively, although rapport building has been found to be associated with satisfaction (Paasche-Orlow & Roter, 2003), it may be that higher rates of NPs’ rapport building behavior were perceived by older patients as patronizing (Ryan, Hummert, & Boich, 1995) or as constituting false reassurance (Arnold & Boggs, 1999) when the other variables in the regression models were taken into account. If so, then rapport building was not the information conveyed when rates of these activities were high and other variables in the models were held constant.
The results also provided some support for the contribution of proximal to longer-term outcomes. Intention to adhere was associated with improvement in presenting problems at 4 weeks, suggesting patients’ adherence intentions immediately after visits may have contributed to the outcome most directly related to the problems that prompted the visits.
The findings of this study have four main implications. First, the NPs communicated effectively with older patients around seeking and giving biomedical and psychosocial information rather than that involving lifestyle. Most patients reported that their NPs were trustworthy and receptive, they were very satisfied with their visits, and they intended to adhere to the NPs’ recommendations. These findings bode well for the growing number of older individuals who likely will be cared for by NPs in an increasingly complex health system.
Second, research directed at ways to improve older patient-NP lifestyle discussion is needed. Many lifestyle changes are known to be slow, difficult, and frustrating for patients and clinicians alike (Taub, 2006). Nevertheless, the poorer outcomes associated with lifestyle discussions in this study are a source of concern, and research on more effective communication strategies for disease prevention and health promotion by NPs is essential.
Of equal concern are the poorer outcomes associated with high rates of rapport building that may have been perceived as patronizing. Education of NPs would be strengthened by a review of age-appropriate communication strategies to avoid sending the wrong signals. In addition, future studies are needed to examine existing rapport building strategies, or to develop new ones at the NP-level of practice, that are associated with effective communication.
Finally, the findings of this study provide partial support for the theoretical framework that guided it. Patterns of variables within the content and relationship components of older patient-NP communication and, to a lesser extent, their background characteristics contributed to one or more proximal or longer-term outcomes, but no single pattern of predictor variables was associated with all outcomes. Further, greater intention to adhere to recommendations was associated with greater improvement in presenting problems, although proximal outcomes were not associated consistently with all longer-term outcomes. Although the framework in its present form may be useful to guide future research on effective communication during visits, it is premature to refine the framework by specifying patterns within the components until key associations are identified in additional complex studies of older patient-NP communication.
Acknowledgments
This study was funded by grant R01-NR00820 from the National Institute of Nursing Research, National Institutes of Health.
Thank you to Professor John P. Buonaccorsi, PhD, Mathematics and Statistics Department, University of Massachusetts Amherst; Research Assistants Ayesha Ali, Kate Baldor, Shannon Kearney Lyons, Susan Plante, and Jennifer Calkins, School of Nursing University of Massachusetts Amherst; Professor Debra Roter and Senior Research Associate Susan M. Larson, School of Public Health, Johns Hopkins University; and patient and nurse practitioner participants.
Contributor Information
Dorothy Ann Gilbert, School of Nursing, University of Massachusetts Amherst, Amherst, Massachusetts.
Eileen Hayes, School of Nursing, University of Massachusetts Amherst, Amherst, Massachusetts.
References
- Agency for Healthcare Research and Quality. CAHPS 2.0R health plan survey and reporting kit 2002. Rockville, MD: Author; 2002. [Google Scholar]
- Arnold E, Boggs KU. Interpersonal relationships: Professional communication skills for nurses. 3. Philadelphia: W. B. Saunders; 1999. [Google Scholar]
- Berry JA. Pilot study: Nurse practitioner communication and the use of recommended clinical preventive services. Journal of the American Academy of Nurse Practitioners. 2006;18(6):277–283. doi: 10.1111/j.1745-7599.2006.00131.x. [DOI] [PubMed] [Google Scholar]
- Burgoon JK, Hale JL. The fundamental topoi of relational communication. Communication Monographs. 1984;51:193–214. [Google Scholar]
- Burgoon JK, Hale JL. Validation and measurement of the fundamental themes of relational communication. Communication Monographs. 1987;54:19–41. [Google Scholar]
- Campbell JD, Mauksch HO, Neikirk HJ, Hosokawa MC. Collaborative practice and provider styles of delivering health care. Social Science & Medicine. 1990;30(12):1359–1365. doi: 10.1016/0277-9536(90)90316-k. [DOI] [PubMed] [Google Scholar]
- Caris-Verhallen WMCM, de Gruijter IM, Kerkstra A, Bensing JM. Factors related to nurse communication with elderly people. Journal of Advanced Nursing. 1999;30(5):1106–1117. doi: 10.1046/j.1365-2648.1999.01197.x. [DOI] [PubMed] [Google Scholar]
- Deshefy-Longhi T, Swartz MK, Grey M. Characterizing nurse practitioner practice by sampling patient encounters: An APRNet study. Journal of the American Academy of Nurse Practitioners. 2008;20(5):281–287. doi: 10.1111/j.1745-7599.2008.00318.x. [DOI] [PubMed] [Google Scholar]
- Duggan AP, Parrott RL. Research note: Physicians’ nonverbal rapport building and patients’ talk about the subjective component of illness. Health Communication Research. 2001;27(2):299–311. [Google Scholar]
- Ervin NE, Chen SP, Upshaw HS. Nursing care quality: Process and outcome relationships. The Canadian Journal of Nursing Research. 2006;38(4):174–190. [PubMed] [Google Scholar]
- Gilbert DA. Reciprocity of involvement activities in client-nurse interactions. Western Journal of Nursing Research. 1993;15(6):674–687. doi: 10.1177/019394599301500602. [DOI] [PubMed] [Google Scholar]
- Gilbert DA. Relational message themes in nurses’ listening behavior during brief patient-nurse interactions. Scholarly Inquiry for Nursing Practice. 1998;12(1):5–21. [PubMed] [Google Scholar]
- Gilbert DA. Coordination in nurses’ listening activities and communication about patient-nurse relationships. Research in Nursing & Health. 2004;27(6):447–457. doi: 10.1002/nur.20043. [DOI] [PubMed] [Google Scholar]
- Green A, Davis S. Toward a predictive model of patient satisfaction with nurse practitioner care. Journal of the American Academy of Nurse Practitioners. 2005;17(4):139–148. doi: 10.1111/j.1041-2972.2005.0022.x. [DOI] [PubMed] [Google Scholar]
- Hayes E. Nurse practitioners and managed care: Patient satisfaction and intention to adhere to nurse practitioner plan of care. Journal of the American Academy of Nurse Practitioners. 2007;19(8):418–426. doi: 10.1111/j.1745-7599.2007.00245.x. [DOI] [PubMed] [Google Scholar]
- Heisler M, Cole I, Weir D, Kerr EA, Hayward RA. Does physician communication influence older patients’ diabetes self-management and glycemic control? Results from the Health and Retirement Study (HRS) The Journals of Gerontology: Series A, Biological Sciences and Medical Sciences. 2007;62(12):1435–1442. doi: 10.1093/gerona/62.12.1435. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press; 2001. [Google Scholar]
- Inui TS, Carter WB. Problems and prospects for health services research on provider-patient communication. Medical Care. 1985;23(5):521–538. doi: 10.1097/00005650-198505000-00013. [DOI] [PubMed] [Google Scholar]
- Jackson JL, Kroenke K. The effect of unmet expectations among adults presenting with physical symptoms. Annals of Internal Medicine. 2001;134(9 pt 2):889–897. doi: 10.7326/0003-4819-134-9_part_2-200105011-00013. [DOI] [PubMed] [Google Scholar]
- Lawson MT. Nurse practitioner and physician communication styles. Applied Nursing Research. 2002;15(2):60–66. doi: 10.1053/apnr.2002.29522. [DOI] [PubMed] [Google Scholar]
- Mann S, Sripathy K, Siegler EL, Davidow A, Lipkin M, Roter DL. The medical interview: Differences between adult and geriatric outpatients. Journal of the American Geriatrics Society. 2001;49(1):65–71. doi: 10.1046/j.1532-5415.2001.49011.x. [DOI] [PubMed] [Google Scholar]
- Mast MS, Hall JA, Kockner C, Choi E. Physician gender affects how physician nonverbal behavior is related to patient satisfaction. Medical Care. 2008;46:1212–1218. doi: 10.1097/MLR.0b013e31817e1877. [DOI] [PubMed] [Google Scholar]
- Mechanic D, McAlpine DD, Rosenthal M. Are patients’ office visits with physicians getting shorter? The New England Journal of Medicine. 2001;344(3):198–204. doi: 10.1056/NEJM200101183440307. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. (n.d.) National ambulatory medical care survey [Data files] Available from National Center for Health Statistics Web site: http://www.cdc.gov/nchs/about/major/ahcd/ahcd1.htm.
- Paasche-Orlow M, Roter D. The communication patterns of internal medicine and family practice physicians. The Journal of the American Board of Family Practice. 2003;16(6):485–493. doi: 10.3122/jabfm.16.6.485. [DOI] [PubMed] [Google Scholar]
- Risser NL. Development of an instrument to measure patient satisfaction with nurses and nursing care in primary care settings. Nursing Research. 1975;24(1):45–52. [PubMed] [Google Scholar]
- Roter D. RIAS: Roter Interaction Analysis System. 2008 Available from the RIAS Web site: http://www.rias.org/articles.
- Roter DL, Larson S. The relationship between residents’ and attending physicians’ communication during primary care visits: An illustrative use of the Roter Interaction Analysis System. Health Communication. 2001;13(1):33–48. doi: 10.1207/S15327027HC1301_04. [DOI] [PubMed] [Google Scholar]
- Roter D, Larson S. The Roter Interaction Analysis System (RIAS): Utility and flexibility for analysis of medical interactions. Patient Education and Counseling. 2002;46(4):243–251. doi: 10.1016/s0738-3991(02)00012-5. [DOI] [PubMed] [Google Scholar]
- Ruusuvuori J. Looking means listening: Coordinating displays of engagement in doctor-patient interaction. Social Science & Medicine. 2001;52(7):1093–1108. doi: 10.1016/s0277-9536(00)00227-6. [DOI] [PubMed] [Google Scholar]
- Ryan EB, Hummert ML, Boich LH. Communication predicaments of aging: Patronizing behavior toward older adults. Journal of Language and Social Psychology. 1995;14(12):144–166. [Google Scholar]
- Safran DG, Taira DA, Rogers WH, Kosinski M, Ware JE, Tarlov AR. Linking primary care performance to outcomes of care. The Journal of Family Practice. 1998;47(3):213–220. [PubMed] [Google Scholar]
- Shapiro RS, Tym KA, Eastwood D, Derse AR, Klein JP. Managed care, doctors, and patients: Focusing on relationships, not rights. Cambridge Quarterly of Healthcare Ethics. 2003;12(3):300–307. doi: 10.1017/s0963180103123134. [DOI] [PubMed] [Google Scholar]
- Street RL, Jr, Gordon H, Haidet P. Physicians’ communication and perceptions of patients: Is it how they look, how they talk, or is it just the doctor? Social Science & Medicine. 2007;65(3):586–598. doi: 10.1016/j.socscimed.2007.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartz MK, Grey M, Allan JD, Ridenour N, Kovner C, Walker PH, et al. A day in the lives of APNs in the U.S. The Nurse Practitioner. 2003;28(10):32–39. doi: 10.1097/00006205-200310000-00012. [DOI] [PubMed] [Google Scholar]
- Taub LM. Concordance of provider recommendations with American Diabetes Association’s Guidelines. Journal of the American Academy of Nurse Practitioners. 2006;18(3):124–133. doi: 10.1111/j.1745-7599.2006.00111.x. [DOI] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Turner-Bowker DM, Gandek B. How to score version 2 of the SF-12 Health Survey. Lincoln, RI: Quality Metric Incorporated; 2002. [Google Scholar]
- Watzlawick P, Beavin JH, Jackson DD. Pragmatics of human communication. A study of interactional patterns, pathologies, and paradoxes. New York: W.W. Norton; 1967. [Google Scholar]
- Yellen E. The influence of nurse-sensitive variables on patient satisfaction. AORN Journal. 2003;78(5):783–793. doi: 10.1016/s0001-2092(06)60638-8. [DOI] [PubMed] [Google Scholar]
- Youngblut JM, Casper GR. Single-item indicators in nursing research. Research in Nursing & Health. 1993;16(6):459–465. doi: 10.1002/nur.4770160610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandbelt LC, Smets EMA, Oort FJ, Godfried MH, de Haes HCJM. Medical specialists’ patient-centered communication and patient-reported outcomes. Medical Care. 2007;45(4):330–339. doi: 10.1097/01.mlr.0000250482.07970.5f. [DOI] [PubMed] [Google Scholar]