Abstract
One of the most promising ways to increase well-being is to engage in valued and enjoyable activities. Behavioral activation (BA), an intervention approach most commonly associated with the treatment of depression, is consistent with this recommendation and can easily be adapted for non-clinical populations. This study reports on a meta-analysis of randomized controlled studies to examine the effect of BA on well-being. Twenty studies with a total of 1353 participants were included. The pooled effect size (Hedges's g) indicated that the difference in well-being between BA and control conditions at posttest was 0.52. This significant effect, which is comparable to the pooled effect achieved by positive psychology interventions, was found for non-clinical participants and participants with elevated symptoms of depression. Behavioral activation would seem to provide a ready and attractive intervention for promoting the well-being of a range of populations in both clinical and non-clinical settings.
Keywords: behavioral activation, happiness, happiness interventions, intervention, meta-analysis, positive psychology, treatment, well-being
Introduction
Happiness, also known as subjective well-being (SWB), is usually defined as a combination of frequent positive affect, infrequent negative affect and a high level of satisfaction with life (Diener, 1984; Diener, Sandvik, & Pavot, 1991; Diener, Suh, Lucas, & Smith, 1999). Recently there has been greater recognition of the positive impact SWB can have on psychological adjustment and adaptation (for a review see Lyubomirsky, King, & Diener, 2005a; Pressman & Cohen, 2005). As a consequence, attention has turned to the factors that contribute to well-being and how an individual's level of well-being can be increased (e.g., Lyubomirsky, 2008; Seligman, 2002; Seligman, Rashid, & Parks, 2006; Seligman, Steen, Park, & Peterson, 2005).
Current understanding of the key determinants of SWB has been informed by the findings of twin and adoption studies, research on personality traits, investigations into the impact of changes in circumstances, along with research on the role of motivational and attitudinal factors (see Diener et al., 1999, for a review). Lyubomirsky, Sheldon, and Schkade (2005b) proposed a three-factor model in which genetics is believed to account for approximately 50% of the variance in well-being and demographics and circumstances account for approximately 10%, leaving 40% of the variance to be governed by intentional activity.
Lyubomirsky et al. (2005b) argued that intentional behavioral, cognitive or volitional activity potentially offers the best route for achieving sustainable increases in well-being. By intentional activity, the authors meant discrete actions or practices that individuals must choose to engage in and that require some effort to enact. This might include adopting new behaviors such as an exercise program, changing one's cognitive attitudes or practices such as practicing forgiveness, or volitional activity such as pursuing personal goals. They suggested that to be effective in increasing well-being, new activities should fit the individual's values and interests. They further suggested that individuals could avoid habituation, by making a habit out of initiating activity, while at the same time varying how and when they implement the activity. Individuals should be advised that trying to increase happiness by accumulating wealth or particular objects (e.g., a bigger house or a new television) may not be a successful strategy in the longer term, because they will tend to habituate to such stable factors.
Evidence supporting the idea that it is possible to increase well-being has steadily been accumulating. Sin and Lyubomirsky (2009) recently conducted a meta-analysis of positive psychology interventions (PPIs); that is, interventions or intentional activities that aim to cultivate positive feelings, behaviors and/or cognitions. The results revealed that PPIs enhance well-being and ameliorate depressive symptoms, and that these effects are enhanced for individuals with depression. Consequently, the authors recommended that clinicians incorporate positive psychology techniques into their clinical work. Importantly, interventions excluded from Sin and Lyubomirksy's meta-analysis were those aimed at ‘fixing, remedying or healing something that is pathological or deficient’ since these ‘do not fit the definition of a PPI’ (Sin & Lyubomirksy, 2009).
While there is increasing recognition for the potential of PPIs to enhance well-being, less is known about the potential of existing clinical interventions. One intervention approach that is consistent with Lyubomirksy and colleagues’ recommendations for increasing happiness is behavioral activation. Behavioral activation (BA), originally developed to treat depression, emphasizes ‘structured attempts at engendering increases in overt behavior that is likely to bring the patient into contact with reinforcing environmental contingencies’ (Hopko, Lejuez, Ruggiero, & Eifert, 2003, p. 700). The approach evolved out of the ‘reinforcement’ explanation of depression which proposes that the behavior of depression is the result of a loss or lack of response-contingent positive reinforcement (Ferster, 1973; Lewinsohn, 1974). In support of this proposal was the finding that there is a significant relationship between mood and participation in pleasant activities (Lewinsohn & Graf, 1973; Lewinsohn & Libet, 1972). Individuals with depression find fewer activities pleasant and engage in pleasant activities less frequently, and therefore obtain less positive reinforcement than other individuals (MacPhillamy & Lewinsohn, 1974).
Based on this theory, Lewinsohn and colleagues developed a behavioral treatment of depression in which an activity schedule is constructed for each patient based on activities and events that have been enjoyable, pleasant, meaningful, or interesting for them in the past. The patient then monitors their daily mood and participation in these activities in order to see the connection between them. Subsequently, each patient is encouraged and taught how to increase the frequency and quality of pleasant events in his or her life, and to decrease unpleasant ones (Lewinsohn, 1976; Lewinsohn, Sullivan, & Grosscap, 1980).
A number of other variants of BA have been developed, most notably Jacobson and colleagues’ contextual approach (Jacobson, Martell, & Dimidjian, 2001; Martell, Addis, & Jacobson, 2001; for a review of other variants see Mazzucchelli, Kane, & Rees, 2009). Jacobson and his colleagues emphasized the role of an individual's life circumstances and avoidance in depression (Jacobson, 1994). Certain aspects of a person's life circumstances can trigger depression and particular ways of responding to these circumstances can maintain it. Avoidance (e.g., of interpersonal situations, occupational or daily-life demands, and distressing thoughts or feelings) is viewed as a coping strategy to avoid the short-term distress that is often associated with pursuing potentially mood-enhancing reinforcers, at the longer-term cost of reducing opportunities to contact these very reinforcers and by creating or exacerbating life problems. Increased activation and engagement is presented as a strategy to break this cycle.
The initial treatment objective of Jacobson and colleagues’ BA approach is to increase patients’ awareness of avoidance patterns by monitoring and reviewing daily behavior. Once these patterns are recognized, the principal objective becomes one of helping the patients to identify and reengage with activities and situations that are reinforcing and consistent with their long-term goals. Many of the same behaviorally focused activation strategies used in cognitive therapy (Beck, Rush, Shaw, & Emery, 1979) are used including self-monitoring, structuring and scheduling daily activities, rating the degree of pleasure and accomplishment experienced during engagement in specific daily activities, exploring alternative behaviors related to achieving goals, and using role-play to address specific behavioral deficits. In addition, this protocol includes the establishment or maintenance of routines and behavioral strategies for targeting rumination, including an emphasis on the function of ruminative thinking and on moving attention away from the content of ruminative thoughts toward direct, immediate, experience.
Although BA interventions have traditionally been associated with the treatment of depression, there is little that differentiates these interventions from some behaviorally focused PPIs other than the intent with which they are used. It is of note that, in what many consider to be the first positive psychology intervention study, Fordyce (1977) tested an ‘activities program’ that involved increasing participation in pleasant activities against an early version of his multi-component Fundamentals happiness program. This activities program proved to be as effective as the Fundamentals program in increasing well-being over a 2-week period. In another study, Fordyce (1983) found that the behaviorally focused ‘lifestyle’ components of the Fundamentals program had a more rapid effect on measures of well-being and could account for the gains made by the full program, at least for those participants who showed a weakness in this area.
If it can be established that BA is effective in increasing the well-being of a normative sample it would indicate that BA is a parsimonious option for increasing the well-being for both individuals with and without depression. The field of positive psychology would be presented with an existing technology for increasing well-being and this might save time and energy that would otherwise be devoted to the development of new interventions focused on increasing well-being. It may also provide important insights into how to prevent illness and promote well-being. Although BA seems to be a promising intervention approach to increase psychological well-being, no formal meta-analysis of BA interventions has been conducted. We decided, therefore, to conduct a meta-analysis to examine the effects of BA on well-being.
Method
Identification and selection of studies
A computer search (using PsycINFO and Medline databases) was conducted to find articles, chapters and dissertations published between January 1970 and April 2008 that included the terms activity scheduling, behavioural activation or behavioral activation, pleasant events or pleasant activities. Reference lists of all articles were searched for additional articles. Also, 23 researchers who have published on BA were contacted by email for relevant data. Studies were included in the meta-analysis if the effect of a BA intervention was compared to a comparison condition in a randomized controlled trial, and the effect was assessed using a measure of one or more components of psychological well-being (e.g., positive affect, happiness, life satisfaction, quality of life, self-esteem). No language restrictions were applied and unpublished dissertations, where available, were included so as to describe the universe of studies. Over 520 articles, chapters and theses were reviewed. A treatment was considered to be BA when it primarily involved strategies to prompt participants to engage with, or act on, the environment so as to increase positive reinforcement and undermine punishment. Thirty-seven percent of the reviewed works were not empirical studies. Other works were excluded for a variety of reasons, namely: the interventions did not reflect the BA approach (33%), the BA approach was confounded with other treatment components such as the modification of thoughts (11%), a measure of well-being was not used (8%), there was no comparison condition (6%), and insufficient information was provided to extract effect sizes (2%).
Quality assessment
The methodological quality of each study was assessed using nine criteria based on a range of important methodological features of psychotherapy research (Chambless & Hollon, 1998). The criteria were: (a) adequacy of sample size to allow a stable estimate of effect size, (b) confidence in sample description, (c) confidence in outcome assessment tools, (d) use of treatment manuals, (e) adequacy of therapist training and monitoring, (f) extent to which investigator allegiance is balanced, (g) equivalence of comparison groups at pre-test, (h) completeness of data set such that observations did not systematically exclude participants who refused treatment or dropped out, and (i) checks for therapist or site effects. We developed a numerical system for this study whereby a score of 0 to 2 (0 to 1 in the case of adequacy of sample size) was assigned according to the extent that each criterion was met. This resulted in each study being allocated a numerical rating from 0 to 17. Studies scoring a rating greater than 11 were considered to be of high quality; those between 6 and 11 were considered to be of moderate quality; and those below 6 were considered to be of low quality. No studies were excluded on the basis of methodological quality.
Meta-analysis
Standardized mean difference effect sizes (ESsm) were calculated with the following formula: ESsm = (Mc–Mt)/SDp, in which Mt = the posttest mean of the treatment group on a specific outcome, Mc = the posttest mean of the comparison group, and SDp = the pooled standard deviation of the two groups. If means or standard deviations were not provided, effect sizes were calculated from the t or F ratio, or from the significance level when t or F were not reported. If a result was reported as significant but did not provide an exact probability, the one-tailed p value was assumed to be 0.025. If a result was simply reported as nonsignificant and no data were provided to calculate an exact probability, it was conservatively assigned p (one-tailed) = 0.5.
Calculations of effect sizes relied on methods described by Lipsey and Wilson (2001). Standardized mean difference effect sizes express effect size in standard deviation units; thus, an effect size of 1.00 on a given dependent measure indicates that the treatment group scored one standard deviation better, on average, than the comparison group on that measure. Effect sizes of 0.67 or greater are assumed to be large, while effect sizes of 0.31 to 0.66 are moderate, and effect sizes of 0.00 to 0.30 are small (Lipsey & Wilson, 2001).
In calculations of effect sizes for well-being, only those instruments that were capable of measuring components of psychological well-being were used. If more than one well-being measure was used, the mean of the effect sizes was calculated, so that each study (or comparison group) only had one effect size. This approach produces conservative estimates of effect size (Rosenthal & DiMatteo, 2001). Where studies permitted two comparisons under the same category (e.g., cognitive therapy/cognitive behavior therapy and antidepressant medication) we entered these comparisons separately but halved numbers in the behavioral arm to avoid double counting and inaccurate weighting of trials. Results in the unpredicted direction (i.e., the comparison group experienced greater increases in well-being compared to the BA group) were recorded as negative values.
Hedges's (1981) correction for small sample bias was applied to all effect sizes. The resultant Hedges's gs were then combined using the formula: Mg = Σwigi/Σwi where wi is the weight for each study and gi is the effect size for each study. Because the present study accumulated data from studies that have been performed by researchers operating independently and using different populations, a common effect size was not assumed. Consequently, mean effect sizes were calculated with the random-effects model. In the random-effects model each study is weighted by the inverse of its variance, which includes both within-studies variance and the estimate of between-studies variance (Borenstein, Hedges, Higgins, & Rothstein, 2009). Comprehensive Meta-analysis (Version 2.2.046; Borenstein, Hedges, Higgins, & Rothstein, 2007) was used to calculate pooled mean effect sizes. The subgroup analyses as implemented in Comprehensive Meta-analysis Version 2.2.046 were used to examine whether the effect sizes of specific subgroups differed from each other.
As an indicator of homogeneity, Cochran's heterogeneity statistic Q was calculated. This statistic tests the null hypothesis that effect sizes from each of the studies are similar enough that they share a common effect size (Cochran, 1954). Cochran's Q was calculated using the following formula: Q = σ wi (di – dw)2, where di is the individual effect size for i = 1 to k (the number of effect sizes), dw is the weighted mean effect size over the k effect sizes, and wi is the individual weight for di. The significance of Q is evaluated against a chi-square distribution with k−1 degrees of freedom. The I2 statistic (I2 = 100% x (Q – df)/Q, where Q is Cochran's heterogeneity statistic and df the degrees of freedom) was used to estimate heterogeneity. A value of 0% indicates no observed heterogeneity, and larger values show increasing heterogeneity, with 25% as low, 50% as moderate, and 75% as high heterogeneity (Higgins, Thompson, Deeks, & Altman, 2003).
Caution is needed in interpreting meta-analytical findings because of the potential for selection and other biases that may be introduced in the process of locating, selecting, and combining studies (Egger, Davey-Smith, Schneider, & Minder, 1997). Such bias was examined using a funnel graph, a plot of sample size versus effect size estimates (Light & Pillemer, 1984). If no bias is present, this plot should be shaped like an inverted funnel, with a broad spread of points for the less precise smaller studies at the bottom and decreasing spread as the sample size increases. Asymmetry was tested using Egger's weighted regression test (Egger et al., 1997). If asymmetry was found to be significant, Duval and Tweedie's (2000) ‘trim and fill’ method was used to estimate the number of missing studies that might exist and the unbiased effect size. Finally, the fail-safe N1 and the critical number of studies2 were estimated in order to address the file drawer problem. The fail-safe N is an estimate of the number of studies with null results that would need to be added to the meta-analysis for the effect to no longer be reliable. The critical number of studies is an estimate of the number of unpublished non-significant studies. If the fail-safe N is greater than or equal to the critical number of studies it is assumed that the significance of the observed effects is unchallengeable. An alpha level of 0.05 was used for all statistical tests.
Results
Description of studies
Twenty studies, with a total of 1353 participants (484 in the BA conditions, and 869 in the comparison conditions) met the inclusion criteria and were included in the current study. Selected characteristics of the included studies are described in Table 1. (Note: throughout the following sections, numbers within square brackets refer to the study numbers listed in Table 1.) Participants were mostly adult university students [3–9, 13, 16, 18], although seven studies recruited adults from the community or from clinical settings [2, 10−12, 17, 19, 20]), two studies recruited older adults from senior citizen apartment buildings [1, 14], and one study recruited children from an elementary school [15]. Most studies recruited participants showing elevated or clinical levels of depressive symptomatology [2, 7–12, 15–20], but six studies recruited participants with minimal symptoms [3–6, 13, 14] and two studies recruited some participants with minimal symptoms and some participants showing elevated symptoms [1, 9]. Most BA interventions consisted of simply encouraging participants to increase their participation in pleasant activities [2–4, 7–10, 12, 13, 15, 16, 18, 19], but two were concerned with becoming more active at a broader ‘lifestyle’ level [5, 6], three focused on increasing pleasant activities in the context of behavioral self-control (Fuchs & Rehm, 1977) [1, 14, 17], and two were consistent with Jacobson and colleagues’ (2001) contextual BA approach [11, 20]. Control conditions consisted of waiting list [1, 2, 10, 14, 15, 18, 19], treatment as usual (without BA) [17, 20], placebo course activities [4, 6], and no instruction control [13]. Cognitive and cognitive behavioral therapy (CT/CBT) conditions consisted of interventions based on Beck's (1976) or Ellis's (1962) treatment procedures [2, 18, 19], or self-control interventions that included both a behavioral and a cognitive focus (Rehm, Kaslow, & Rabin, 1987) [15]. Other psychological interventions included increasing ‘control’ activities and self-monitoring [3, 7–9, 16], Fordyce's (1977) Fundamentals happiness program and variants [4–6], nondirective support [2, 12, 18], brief psychodynamic therapy [11], relaxation [11], or problem solving [10]. One study included an antidepressant medication (ADM) condition involving amitriptyline [11]. The quality of studies ranged from low [3, 5, 6, 8–10, 16, 18, 19] to high [11, 15]. Nine studies were judged to be moderate in quality [1, 2, 4, 7, 12–14, 17, 20].
Table 1.
Selected characteristics of controlled and comparative studies on behavioral activation.
| Study | Country | Age group and age(years) | Recruitment | Inclusion criteria | Condition | Cell size at baseline | Male participants(%) | Length of intervention(weeks) | Format or Mode | Numberof sessions(sessionlength) | Attrition at posttest(%) | Measurements | Measuresof well-being | Quality ofresearchdesign (low,0–17, high) |
| [1] Barlow (1986) | US | Elderly(M = 77) | Community (Senior citizen apartment buildings) | Age > 65(Excluded if actively suicidal, moderately or severely demented, or receiving treatment for depression) Low depressed subgroup (CES-D <16, M = 8.74). High depressed subgroup (CES-D ≥16, M = 22.28) | 1. Self-control [Self-control] | 25 | ~6 | 6 | Group | 6 (90 min) | ~9 | Pre, post. | LSI-A | 9 (mod) |
| 2. Waiting-list (6 week) | 24 | ~6 | NA | NA | 6 (90 min) | ~9 | ||||||||
| [2] Besyner (1979) | US | Adults (M = 42) | Community | Self-reported depression of at least 2 weeks duration: BDI ≥ 13 | 1. Cognitive therapy | 10 | 40 | 4 | Group | 4 (120 min) | 0 | Pre, post, 1-month FU | TSCS | 9 (mod) |
| 2. Behavior therapy [Pleasant Activities] | 14 | ~27 | 4 | Group | 4 (120 min) | 21 | ||||||||
| 3. Nonspecific therapy | 10 | ~33 | 4 | Group | 4 (120 min) | 10 | ||||||||
| 4. Waiting list (4 week) | 16 | ~18 | NA | NA | 4 (120 min) | 31 | ||||||||
| [3] Dobson & Joffe (1986) | US | Young adults (M = 21) | University | Availability (students of an undergraduate psychology course) | 1. Self-monitor | 22 | 27 | 2 | NR | 3 (NR) | 0 | Average score from daily recordings over 2 1-week periods | DACL, MR | 5 (low) |
| 2. Behavior [Pleasant Activities] | 20 | 40 | 2 | NR | 3 (NR) | 0 | ||||||||
| 3. Cognitive / behavior | 23 | 26 | 2 | NR | NA | 0 | ||||||||
| [4] Fordyce (1977); study 1 | US | Young adults (M = 23) | Community College | Availability (students of undergraduate psychology courses) | 1. Insight | 48 | ~46 | 2 | Group | NR | 0 | Pre, post, 2-month FU | HM | 8 (mod) |
| 2. Fundamentals | 44 | ~46 | 2 | Group | NR | 0 | ||||||||
| 3. Activities [Pleasant Activities] | 50 | ~46 | 2 | Group | NR | 0 | ||||||||
| 4. Placebo course activities | 60 | ~46 | 2 | Group | NR | 0 | ||||||||
| [5] Fordyce (1983); study 5 | US | Young adults (M = 23) | Community College | Availability (students of undergraduate psychology courses) | 1. Fundamentals | ~57 | ~48 | 10 | Group | NR | -13 | Pre, post | POI-TR,POI-SR,HM | 5 (low) |
| 2. Life-style 1/3 [Lifestyle] | ~24 | ~48 | 10 | Group | NR | -13 | ||||||||
| [6] Fordyce (1983); study 6 | US | Young adults (M = 25) | Community College | Availability (students of undergraduate psychology courses) | 1. Fundamentals | ~14 | ~37 | 6 | Group | NR | NR | Pre, 2-weekmid, 4-weekmid, post | HM, DACL | 5 (low) |
| 2. Personality 1/3 | ~10 | ~37 | 6 | Group | NR | NR | ||||||||
| 3. Attitude and values 1/3 | ~12 | ~37 | 6 | Group | NR | NR | ||||||||
| 4. Life-style 1/3 [Lifestyle] | ~8 | ~37 | 6 | Group | NR | NR | ||||||||
| 5. Placebo course activities | ~13 | ~37 | 6 | Group | NR | NR | ||||||||
| [7] Graf (1977) | US | Young adults (M = 19) | University | BDI>12 | 1. Increased mood-related activities [Pleasant Activities] | 30 | ~43 | 2 | Individual | 1 (60 min) | 30 | Pre, post | DACL | 10 (mod) |
| 2. Increased control activities | 30 | ~43 | 2 | Individual | 1 (60 min) | 10 | ||||||||
| 3. Activity monitoring condition | 30 | -43 | 2 | Individual | 1 (60 min) | 27 | ||||||||
| [8] Hammen & Glass (1975): | US | Young adults (M = NR) | University | Mild to moderate depression (based on | 1. Increase activities [Pleasant Activities] | 10 | NR | 2 | NR | 1 (NR) | NR | Averagescore fromdaily | DACL, ED Scale | 5 (low) |
| experiment 1 | screening with D30, FCC & PFS) | recordings over 2 weeks | ||||||||||||
| 2. Expectancy control | 10 | NR | 2 | NR | 1 (NR) | NR | ||||||||
| 3. Self-monitor control | 10 | NR | 2 | NR | 1 (NR) | NR | ||||||||
| 4. No treatment control (2 weeks) | 10 | NR | NA | NR | 1 (NR) | NR | ||||||||
| [9] Hammen & Glass (1975), experiment 2 | US | Young adults (M = NR) | University | Non-depressed and depressed (based on screening with D30 & BDI) | 1. Increase activities [Pleasant Activities] | ~12 | NR | 1 | NR | 1 (NR) | NR | Average score from daily recordings over 1 week | DACL, ED Scale | 5 (low) |
| 2. Self-monitor | ~12 | NR | 1 | NR | 1 (NR) | NR | ||||||||
| [10] Lovett & Gallagher(1988) | US | Adults (M = 59) | Community | Family member caregivers of frail elders 25.9% experiencing a major depressive episode and 22.4% a minor depressive episode (based on SADS) | 1. Life satisfaction [Pleasant Activities] | ~33 | ∼17 | 10 | Group | 10 (120 min) | ~42 | Pre, post | PGCMS | 4 (low) |
| 2. Problem-solving | ~28 | ~17 | 10 | Group | 10 (120 min) | ~42 | ||||||||
| 3. Waiting list | ~27 | ~17 | NA | NA | NA | ~42 | ||||||||
| [11] McLean & Hakstian (1979): McLean & Hakstian (1990) | CA | Adults(M = 39) | Community | (a) Between 20 and 60 years of age; (b) satisfying diagnostic criteria for clinical depression, and depressed for at least the last 2 months; (c) functionally impaired because of depression; (d) within or beyond the moderate range on two out of three psychometric tests for depression | 1. Psychotherapy | 37 | ∼28 | 10 | Individual | 10 (60 min) | 30 | Pre, post, 3-monthFU,2.25-yearFU | Average satisfaction index, Mood index | 12 (high) |
| MMPI-D ≥ 25/29.5, BDI ≥ 23, DACL ≥ 14: (e) fluent in English; (f) not receiving treatmenl for depression elsewhere. | ||||||||||||||
| 2. Relaxation Therapy | 38 | ∼28 | 10 | Individual | 10 (60 min) | 26 | ||||||||
| 3. Behavior Therapy [Behavioral Activation] | 40 | ∼28 | 10 | Individual | 10 (60 min) | 5 | ||||||||
| 4. Drug Therapy | 39 | ∼28 | 11 | Individual | 4 (15 min) | 36 | ||||||||
| [12] Padfield (1976) | US | Adults (range = 21–56) | Community | Women with moderate depression (SRSD, GICL) | 1. Counseling | 12 | 33 | 12 | Individual | 12 (NR) | 0 | Pre, post | DACL | 8 (mod) |
| 2. Behavioral [Pleasant Activities] | 12 | 17 | 12 | Individual | 12 (NR) | 0 | ||||||||
| [13] Reich & Zautra (1981) | US | Young adults (M = NR) | University | Availability (students of undergraduate psychology courses) | 1. Increase 12 activities [Pleasant Activities] | ~49 | NR | 2 | NR | 2(NR) | 5 | Pre, post(after 4 weeks) | PQLS | 8 (mod) |
| 2. Increase 2 activities [Pleasant Activities] | ~49 | NR | 2 | NR | 2(NR) | 5 | ||||||||
| 3. No instruction control | ~49 | NR | 2 | NR | 2(NR) | 5 | ||||||||
| [14] Rokke (1985) | US | Elderly (M = 77) | Community(subsidized housing projects) | Age > 65 (Excluded if receiving treatment for depression, suicidal, evidencing signs of dementia) | 1. Life satisfaction : [Self-control] | 21 | 5 | 6 | Group | 6 (90 min) | 0 | Pre, post | LSI-A | 7 (mod) |
| 2. Waiting-list (6 week) | 20 | 5 | NA | NA | NA | 0 | ||||||||
| [15] Stark, Reynolds, & Kaslow (1987) | US | Children (M = ll) | Elementary school | CDI> 16; parental permission | 1. Self-control | 9 | 56 | 5 | Group | 12 (45–50 min) | ~5 | Pre, post, 8-week FU | CSEI | 12 (high) |
| 10 | 60 | 5 | Group | 12 (45–50 min) | -5 | |||||||||
| 2. Behavioral problem solving [Pleasant Activities] | ||||||||||||||
| 3. Waiting list (5 week) | 9 | 56 | NA | NA | NA | 0 | ||||||||
| [16] Turner, Ward, & Turner (1979) | US | Young adults (M = 24) | University | DACL T≥70 and reported depression as primary concern. | 1. Activities increase [Pleasant Activities] | 14 | 50 | 4 | Individual | 5 (50 min) | NR | Pre, post DACL | 4 (low) | |
| 2. Expectancy control | 14 | 50 | 4 | Individual | 5 (50 min) | NR | ||||||||
| 3. Self-monitoring | 14 | 50 | 4 | Individual | 5 (50 min) | NR | ||||||||
| 4. Attention-control | 14 | 50 | 4 | Individual | 5 (50 min) | NR | ||||||||
| [17] Van den Hout, Arntz, & Kunkels (1995) | ND | Adults (M = 34; Range −20–59) | Clinical (Day treatment centre of a psychiatric | SCID-III-R, major depression and / dysthymia. Excluded if bipolar | Self-control therapy & TAU [Self-: Control] | 15 | 38 | 12 | Group | 12 (90 min) | -10 | Pre, post, SES,13-week VROPSOM FU | 8 (mod) | |
| hospital) | mood disorder: psychotic disorder, alcohol or drug dependence; anxiety disorder. PTSD. SRDS ≥ 50 | |||||||||||||
| 2. TAU (structured group therapy; creative therapy and physical exercise; social skills training and occupational therapy) | 14 | 42 | 12 | Group | NR | ~10 | ||||||||
| [18] Weinberg (1978) | US | Young adults (M = NR) | University | BDI≥8 | 1. Increased positive reinforcement [Pleasant Activities] | 10 | ~12 | 4 | Group | 4 (60 min) | 10 | Pre, post, MAAD,2-month FU POI-TR,POI-SR | 5 (low) | |
| 2. Systematic rational restructuring | 10 | ~12 | 4 | Group | 4 (60 min) | 0 | ||||||||
| 3. Emotional awareness training | 10 | ~12 | 4 | Group | 4 (60 min) | 20 | ||||||||
| 4. Waiting list (4 weeks) | 9 | ~12 | NA | NA | NA | 0 | ||||||||
| [19] Wilson, Goldin, & Charbonneau-Powis (1983) | AU | Adults (M = 40: range = 20–58) | Community | BDI≥ 17; no previous concurrent treatment with major tranquilizers or lithium: | 1. Behavior therapy [Pleasant Activities] | 9 | 25 | 8 | Individual | 8 (60 min) | 11 | Pre, mid,post,5-month FU | MRs | 5 (low) |
| absence of other major physical or | 2. Cognitive therapy | 11 | 12 | 8 | Individual | 8 (60 min) | 27 | |||||||
| psychiatric disorders; self-reported duration of depression of at least 3 months; absence of suicidal intention or ideation | 3. Waiting list (8 weeks) | 9 | 22 | NA | NA | NA | 0 | |||||||
| [20] Wright (2003) | US | Adults(M ~ 53) | Clinical (Specialized inpatient PTSD unit of a Veteran Affairs Medical Centre) | Exposed to combat during military service, having a diagnosis of PTSD. Literate in English. Aged between 18 and 75 years. Excluded if physically unable to participate in activities, actively suicidal, actively psychotic, actively using alcohol or drugs. | 1. TAU | 31 | 100 | 4 | NA | NA | 32 | Pre, 1-monthFU | ComQol | 11 (mod) |
| 2. TAU & Behavioral Activation | 29 | 100 | 4 | Group | 8 (60–90 min) | 17 |
Note: AU = Australia; BDI = Beck Depression Inventory; CA = Canada; CDI = Child Depression Inventory; CES-D = Centre for Epidemiological Studies Depression Scale; ComQol = Comprehensive Quality of Life Scale-Adult Fifth Edition; CSEI = Coopersmith Self-Esteem Inventory; D30 = D30 Depression Scale; DACL = Depression Adjective Checklist; ED Scale = Elation-Depression Scale; FCC = Feelings and Concerns Checklist; FU = follow-up; HM = Happiness Measures; LSI-A = Life Satisfaction Index A; MAAD = Multiple Affect Adjective Check-List; MMPI-D = Minnesota Multiphasic Personality Inventory–Depression Scale; MR = Mood Rating; NA = not applicable; NR = not reported; PFS = Personal Feelings Scales; PGCMS = Philadelphia Geriatric Centre Morale Scale; POI-SR = Personal Orientation Inventory-Support Ratio; POI-TR = Personal Orientation Inventory-Time Ratio; PQLS = Perceived Quality of Life Scale; PTSD = Post Traumatic Stress Disorder; SCID-III-R = Structured Clinical Interview for DSM-III-R; SADS = Schedule for Affective Disorders and Schizophrenia; SES = Self-esteem Scale; SRDS = Zung Self-Rating Depression Scale; TAU = treatment as usual; TSCS = Tennessee Self-Concept Scale; US = United States of America; VROPSOM = Dutch version of the DACL.
Effects of behavioral activation at posttest
Behavioral activation could be compared against control conditions in 10 studies [1, 2, 4, 6, 10, 13, 15, 17–19] totaling 11 contrasts involving 465 participants. These yielded a moderate and significant pooled effect size of 0.52 favoring BA. Heterogeneity was low and nonsignificant. A funnel graph showed no evidence of asymmetry providing little indication of selection bias (Egger's regression intercept = 0.73; 95% CI –1.38 to 2.84, p = 0.453). The fail-safe N resulted in a figure of 67 studies, which exceeded the critical number of 65 studies indicating that the significance of this effect is unchallengeable. This main analysis is presented as a forest plot in Figure 1.
Figure 1.
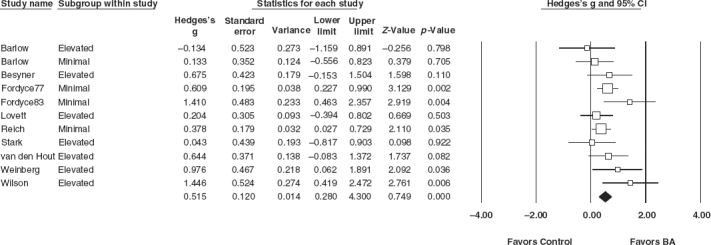
Hedges's g effect sizes of behavioral activation interventions compared to control conditions at post-test.
Subgroup analysis indicated that the interventions yielded moderate effects for both participants with minimal symptoms of depression and participants with elevated symptoms of depression, and that these effects did not differ significantly from each other (p = 0.955). Low quality studies yielded a large pooled effect whereas moderate quality studies yielded a moderate pooled effect. The one high quality study produced a negligible effect. These effects did not differ significantly from each other (p = 0.241). The effect sizes and 95% confidence intervals of these comparisons are listed in Table 2.
Table 2.
Effects of behavioral activation on measures of well-being: Overall results and subgroup analyses.
| Ncmp | Nprtcpnts | Hedges's g | 95% CI | Q | I2 | |
| Comparison to Control at Posttest | ||||||
| All Participants | 11 | 465 | 0.52∗∗∗ | 0.27 to 0.77 | 13.52 | 26.08 |
| Non-clinical | 4 | 303 | 0.53∗∗ | 0.18 to 0.88 | 5.41 | 44.53 |
| Elevated symptoms | 7 | 162 | 0.51∗∗ | 0.15 to 0.88 | 8.12 | 26.11 |
| High quality | 1 | 19 | 0.04 | −0.82 to 0.90 | 0.00 | 0.00 |
| Moderate quality | 6 | 347 | 0.45∗∗∗ | 0.23 to 0.67 | 3.44 | 0.00 |
| Low quality | 4 | 99 | 0.93∗∗ | 0.27 to 1.58 | 7.06 | 57.48 |
| Comparison to Other Interventions at Posttest | ||||||
| All other interventions | 19 | 825 | 0.09 | −0.10 to 0.29 | 27.85 | 35.38 |
| Non-clinical | 5 | 318 | ~0.02 | −0.36 to 0.32 | 6.99 | 42.77 |
| Elevated symptoms | 14 | 507 | 0.14 | −0.10 to 0.39 | 19.79 | 34.32 |
| High quality | 3 | 218 | 0.18 | 0.55 to 0.91 | 8.81∗ | 77.30 |
| Moderate quality | 5 | 272 | 0.14 | −0.16 to 0.43 | 4.81 | 16.89 |
| Low quality | 11 | 335 | −0.01 | −0.24 to 0.22 | 10.54 | 5.13 |
| CT/CBT | 4 | 71 | −0.10 | −0.73 to 0.53 | 5.20 | 42.28 |
| Other psychological | 14 | 684 | 0.09 | −0.12 to 0.31 | 19.92 | 34.75 |
| ADM | 1 | 70 | 0.47 | −0.04 to 0.98 | 0.00 | 0.00 |
| Comparison at 1–3 month follow-up | ||||||
| To Control | 3 | 78 | 0.36 | −0.31 to 1.02 | 4.32 | 53.72 |
| Non-clinical | 0 | 0 | − | − | − | − |
| Elevated symptoms | 3 | 78 | 0.36 | −0.31 to 1.02 | 4.32 | 53.72 |
| High quality | 0 | 0 | − | − | − | − |
| Moderate quality | 2 | 59 | 0.04 | −0.46 to 0.55 | 0.03 | 0.00 |
| Low quality | 1 | 19 | 1.17∗ | 0.23 to 2.11 | 0.00 | 0.00 |
| To all other interventions | 7 | 236 | 0.28 | −0.17 to 0.72 | 12.77∗ | 53.01 |
| Non-clinical | 0 | 0 | − | − | − | − |
| Elevated symptoms | 7 | 236 | 0.28 | −0.17 to 0.72 | 12.77∗ | 53.01 |
| High quality | 3 | 175 | −0.11 | −0.88 to 0.67 | 9.03∗ | 77.85 |
| Moderate quality | 2 | 31 | 0.75∗ | −0.04 to 1.46 | 0.54 | 0.00 |
| Low quality | 2 | 30 | 0.57 | −0.16 to 1.30 | 0.02 | 0.00 |
| CT/CBT | 3 | 48 | −0.04 | – 1.20 to 1.12 | 8.07∗ | 75.23 |
| Other psychological | 3 | 129 | 0.57∗∗ | 0.16 to 0.98 | 0.89 | 0.00 |
| ADM | 1 | 59 | 0.06 | −0.47 to 0.60 | 0.00 | 0.00 |
Notes: - = no data. ADM = antidepressant medication. CT/CBT = cognitive therapy and cognitive behavioral therapy. Ncmp = number of comparisons. Nprtcpnts = number of participants.
∗p <0.05.
∗∗p <0.01.
∗∗∗p <0.001.
All 10 studies attempted to increase participants’ engagement in pleasant events, it is therefore of interest to consider the impact of these interventions on activity. Posttest comparisons between BA and control conditions on measures of activity (typically, activity lists derived from the Pleasant Events Schedule; MacPhillamy & Lewinsohn, 1982) were possible in seven studies [1, 2, 13, 14, 16, 17, 18] giving a total of 294 participants. These yielded a moderate and significant mean effect size of 0.37 (95% CI 0.14 to 0.60, p = 0.002) in favor of BA. Heterogeneity was negligible and nonsignificant (Q = 5.74; p = 0.570; I2 = 0.00%). A funnel graph showed no evidence of asymmetry, providing little indication of selection bias (Egger's regression intercept = 0.52; 95% CI –1.53 to 2.8, p = 0.558). The fail-safe N resulted in a figure of 12 studies, which did not exceed the critical number of 45 studies indicating that the significance of this effect is not unchallengeable. The relationship between mean effect size for activity and mean effect size for SWB was not significant (r = 0.44, p = 0.329).
Comparison to other treatments at posttest
Behavioral activation could be compared directly to other psychological interventions in 14 studies [2–12, 15, 16, 18, 19] totaling 19 contrasts involving 825 participants. The pooled effect size indicating the difference between BA and other interventions was 0.09 (95% CI –0.10 to 0.29, p = 0.355) in favor of BA. Heterogeneity was low to moderate and nonsignificant (p = 0.064). A funnel graph showed little evidence of asymmetry providing little indication of selection bias (Egger's regression intercept = −1.04; 95% CI −2.81 to 0.73, p = 0.232).
Subgroup analyses indicated that the interventions yielded a small effect for participants with elevated symptoms of depression and a negligible effect for participants with minimal symptoms of depression and that these effects did not differ significantly from each other (p = 0.459). High and moderate quality studies yielded a small pooled effect in favor of BA, whereas low quality studies yielded a negligible pooled effect. These effects did not differ significantly from each other (p = 0.708). Studies which compared BA to CT/CBT yielded a small pooled effect size in favor of CT/CBT. Studies which compared BA to other psychological interventions yielded a small pooled effect size in favor of BA. The one study that compared BA to ADM yielded a moderate effect in favor of BA. These effects did not differ significantly from each other (p = 0.315). The effect sizes and 95% confidence intervals of these comparisons are listed in Table 2.
Effects at follow-up
The effects of BA compared to a control condition at follow-up could be calculated in only three studies [17, 18, 20] totaling 78 participants. All of these participants reported elevated symptoms of depression. The pooled effect size indicated a moderate but nonsignificant (p = 0.295) difference in favor of BA. Heterogeneity was moderate but nonsignificant (p = 0.115). A funnel graph appeared somewhat asymmetrical with a smaller study having more pronounced benefits in favor of BA, however this asymmetry did not reach significance (Egger's regression intercept = 9.85; 95% CI −8.49 to 28.19, p = 0.093). Subgroup analysis indicated that the two moderate quality studies yielded a negligible pooled effect whereas the low quality study yielded a large and significant effect. These effects were significantly different from each other (p = 0.038). The effect sizes and 95% confidence intervals of these comparisons are listed in Table 2.
Behavioral activation could be compared to other treatments at follow-up in 4 studies [2, 11, 15, 18] totaling 7 contrasts involving 236 participants (Table 2). All of these participants reported elevated symptoms of depression. The pooled effect size indicated a small, but nonsignificant (p = 0.225), difference in favor of BA. Heterogeneity was moderate and significant (p = 0.047). A funnel graph appeared somewhat asymmetrical with one study [15] yielding a large effect in favor of a comprehensive self-control intervention, however this asymmetry was nonsignificant (Egger's regression intercept = −0.02; 95% CI –-4.74 to 4.70, p = 0.991).
Subgroup analyses indicated that the high quality studies yielded a small pooled effect in favor of other psychological interventions, whereas the moderate quality studies yielded a large and significant pooled effect in favor of BA and the low quality studies yielded a moderate effect in favor of BA. These effects were not found to differ significantly from each other (p = 0.254). The studies comparing BA to CT/CBT yielded a negligible pooled effect size. The studies comparing BA to other psychological interventions yielded a moderate and significant pooled effect size in favor of BA. The one study that compared BA to ADM yielded a small effect in favor of BA. These effects did not differ significantly from each other (p = 0.263). The effect sizes and 95% confidence intervals of these comparisons are listed in Table 2.
Discussion
These results provide evidence that BA interventions can increase the well-being of recipients and that they are equally effective regardless of depression status. The overall effect size of 0.52 is moderate in size and, although smaller than the large effect sizes achieved on measures of depressive symptomatology when BA interventions are applied to depressed populations (Cuijpers, van Straten, & Warmerdam, 2007; Ekers, Richards, & Gilbody, 2008; Mazzucchelli et al., 2009), is comparable in size to the mean effect on measures of well-being achieved by PPIs (0.61; Sin & Lyubomirsky, 2009). A number of studies permitted comparisons between BA interventions and other psychological interventions. These comparisons indicated that BA and other interventions are equally effective in increasing well-being at posttest, but that BA interventions and CT/CBT interventions may be more successful than other psychological interventions at maintaining increases in well-being at follow-up periods of up to 3 months.
Seligman (2002) proposed three components of a happy life: positive emotion, engagement and meaning. It might be argued that contemporary BA interventions target all three of these components by encouraging engagement in life through commitment to meaningful and achievable goals that are likely to result in increased rates of positive reinforcement and positive feelings (for discussions on how personal goals influence behavior and promote purpose, meaning and positive affect see Cantor, 1990; Deci & Ryan, 2000; Emmons, 1996; Klinger, 1975; Little, 1983). It is perhaps not surprising then that BA interventions can not only reduce symptoms of depression but also boost well-being. What is more intriguing is the evidence that other psychological interventions might be just as effective as BA and PPIs at helping recipients attain life's positives. Measures of well-being are not routinely used in psychotherapy research and it is perhaps because of this that their potential in this area has passed relatively unnoticed. This shortcoming should be redressed in future research.
The present study's finding that BA interventions can increase well-being indicates that BA should be added to the growing number of viable interventions in the field of positive psychology. Two attractive aspects of the BA approach are (1) intervention protocols already exist, and (2) in its simplest form, it is suitable for a broad range of target populations including those that cannot be treated with more complex interventions. For instance, interventions involving the presentation of favorite stimuli, or scheduling leisure activities, have been piloted with individuals with severe or profound intellectual and multiple disabilities to increase indices of happiness (e.g., Green & Reid, 1996; Lancioni et al., 2007; Yu et al., 2002). The approach would also appear to be suitable for individuals with dementia (e.g., Teri, Logsdon, Uomoto, & McCurry, 1997).
Behavioral activation interventions have been effectively delivered in a variety of formats including group therapy, brief individual therapy and longer-term individual therapy. The approach might also lend itself to self-help applications in the form of bibliotherapy (e.g., Addis & Martell, 2004; Hopko & Lejuez, 2007) or computer-based interventions (e.g., Meyer, Berger, Caspar, Beevers, Andersson, & Weiss, 2009). These formats would be suited for people who want to increase their psychological well-being with minimal cost or practitioner contact.
A moderate increase in activity (mostly reflecting increased participation in pleasant activities) for BA conditions relative to control conditions was observed. This result is consistent with the goal of increasing participation in pleasant activities, which was the focus of early versions of the BA approach (e.g., Lewinsohn, 1976). Notably 65% of the studies included in this analysis might be considered ‘traditional’ in this regard. Recent variants of the BA approach for depression have expanded on this form of BA by emphasizing an ideographic approach where each participant's circumstances, interests and values are taken into account, and avoidance behaviors are analyzed and addressed (e.g., Jacobson et al., 2001; Lejuez, Hopko, LePage, Hopko, & McNeil, 2001; Martell et al., 2001). There is some evidence that contemporary versions of BA might be more effective for depression than earlier variants (Mazzucchelli et al., 2009). It might be speculated that these contemporary versions could be adapted for non-clinical populations and that they might result in greater intervention effects.
It would also be of interest to investigate other interventions that might augment BA. Dobson and Joffe (1986) found that participants who were instructed to think about the pleasurable or beneficial aspects of their activities before and after engaging in them, in addition to increasing their participation in pleasant activities, showed a greater improvement on outcome measures over a 2-week period compared to those who increased their participation in pleasant activities alone. Bryant and Veroff (2007) have documented a number of ways the enjoyment of positive experiences might be intensified or prolonged in this way. It would be of interest to see what synergies might be achieved by combining these two approaches.
Despite the intriguing findings and possibilities of the present study they should be considered with caution because of several limitations. First, the number of studies included in the present study was small. In particular, the number of comparisons for non-clinical populations, CT/CBT interventions and for comparisons at follow-up was small. Second, several studies were included with small sample sizes, which tends to provide a less stable estimate of effect size. Third, several studies were ‘pilot like’ and short in duration. Sin and Lyubomirksy (2009) found that PPIs of longer duration were relatively more likely to produce greater gains in well-being. In this way, it is possible that some studies included in the present meta-analysis may have ‘undersold’ BA. Fourth, most studies did not assess the sustainability of effects by conducting follow-up assessments. The question of whether interventions are effective for the long-term is at least as important as their efficacy in the short-term. Finally, the quality of well-being measures used in studies varied in their focus and quality. Clearly there is much that can be done in improving the literature base of this intervention as it relates to fostering well-being. Despite these limitations, confidence in the overall conclusion that BA interventions can increase well-being is bolstered by the fact that, when compared to control conditions: (a) heterogeneity was low to moderate, (b) 91% of comparisons pointed in the same positive direction, and (c) the number of unpublished studies reporting null results needed to reduce the calculated effect to the point of non-significance is high and exceeds the critical number of studies.
This paper presents encouraging data about the potency of BA interventions to not only treat depression but also build well-being. Behavioral activation offers a ready intervention technology that can be adapted to a range of populations in both clinical and non-clinical settings. It remains to be seen what the true potential of BA might be in terms of preventing illness and promoting well-being, and what the approach might contribute to the field of positive psychology.
Notes
-
1
k0 = k[MESk/MESc−1], where k0 is the number of effect sizes with a value of zero needed to reduce the mean effect size to MESc, k is the number of studies in the mean effect size, MESk is the weighted mean effect size, and MESc is the criterion effect size level (Rosenthal, 1979).
-
2
kc = 5k + 10, where kc is the critical number of studies, k is the number of studies in the mean effect size (Rosenthal, 1979).
Footnotes
References marked with an asterisk indicate studies included in the meta-analysis.
References
- Addis M.E., Martell C.R. Oakland, CA: New Harbinger; 2004. Overcoming depression one step at a time: The new behavioral activation approach to getting your life back. [Google Scholar]
- *.Barlow J. A group treatment for depression in the elderly. Dissertation Abstracts International. 1986;46(12B):4389B. (UMI No. 8602302) [Google Scholar]
- Beck A.T. New York: International Universities Press; 1976. Cognitive therapy and the emotional disorders. [Google Scholar]
- Beck A.T., Rush J., Shaw B., Emery G. New York: Guilford; 1979. Cognitive therapy of depression. [Google Scholar]
- *.Besyner J.K. The comparative efficacy of cognitive and behavioral treatments of depression: A multi-assessment approach. Dissertation Abstracts International. 1979;39(09):4568B. (UMI No. 7904956) [Google Scholar]
- Borenstein M., Hedges L., Higgins J., Rothstein H. Englewood, NJ: Biostat Inc; 2007. Comprehensive meta-analysis: A computer program for meta-analysis [Computer software] [Google Scholar]
- Borenstein M., Hedges L.V., Higgins J.P.T., Rothstein H.R. Chichester, UK: Wiley; 2009. Introduction to meta-analysis. [Google Scholar]
- Bryant F.B., Veroff J. Mahwah, NJ: Lawrence Erlbaum Associates; 2007. Savoring: A new model of positive experience. [Google Scholar]
- Cantor N. From thought to behavior: ‘Having’ and ‘doing’ in the study of personality and cognition. American Psychologist. 1990;45:735–750. [Google Scholar]
- Chambless D.L., Hollon S.D. Defining empirically supported therapies. Journal of Consulting and Clinical Psychology. 1998;66:7–18. doi: 10.1037//0022-006x.66.1.7. [DOI] [PubMed] [Google Scholar]
- Cochran W. The combination of estimates from different experiments. Biometrics. 1954;10:101–129. [Google Scholar]
- Cuijpers P., van Straten A., Warmerdam L. Behavioral activation treatments of depression: A meta-analysis. Clinical Psychology Review. 2007;27:318–326. doi: 10.1016/j.cpr.2006.11.001. [DOI] [PubMed] [Google Scholar]
- Deci E.L., Ryan R.M. The ‘what’ and ‘why’ of goal pursuits: Human needs and the self-determination of behavior. Psychological Inquiry. 2000;4:227–268. [Google Scholar]
- Diener E. Subjective well-being. Psychological Bulletin. 1984;95:542–575. [PubMed] [Google Scholar]
- Diener E., Sandvik E., Pavot W. Strack F., Argyle M., Schwarz N. Oxford: Pergamon; 1991. Happiness is the frequency not the intensity of positive versus negative affect. Subjective well-being: An interdisciplinary perspective; pp. 119–140. [Google Scholar]
- Diener E., Suh E.M., Lucas R.E., Smith H.L. Subjective well-being: Three decades of progress. Psychological Bulletin. 1999;125:276–302. [Google Scholar]
- *.Dobson K.S., Joffe R. The role of activity level and cognition in depressed mood in a university sample. Journal of Clinical Psychology. 1986;42:264–271. doi: 10.1002/1097-4679(198603)42:2<264::aid-jclp2270420207>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- Duval S., Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- Egger M., Davey-Smith G., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. British Medical Journal. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekers D., Richards D., Gilbody S. A meta-analysis of randomized trials of behavioural treatment of depression. Psychological Medicine. 2008;38:611–623. doi: 10.1017/S0033291707001614. [DOI] [PubMed] [Google Scholar]
- Ellis A. New York: Lyle Stuart; 1962. Reason and emotion in psychotherapy. [Google Scholar]
- Emmons R.A. Gollwitzer P.A., Bargh J.A. New York: Guildford Press; 1996. Striving and feeling: Personal goals and subjective well-being. The psychology of action: Linking cognition and motivation to behavior; pp. 313–337. [Google Scholar]
- Ferster C.B. A functional analysis of depression. American Psychologist. 1973;28:857–870. doi: 10.1037/h0035605. [DOI] [PubMed] [Google Scholar]
- *.Fordyce M.W. Development of a program to increase personal happiness. Journal of Counseling Psychology. 1977;24:511–521. [Google Scholar]
- *.Fordyce M.W. A program to increase happiness: Further studies. Journal of Counseling Psychology. 1983;30:483–498. [Google Scholar]
- Fuchs C.Z., Rehm L.P. A self-control behavior therapy program for depression. Journal of Consulting and Clinical Psychology. 1977;45:206–215. doi: 10.1037//0022-006x.45.2.206. [DOI] [PubMed] [Google Scholar]
- *.Graf M.A. A mood-related activities schedule for the treatment of depression. Dissertation Abstracts International. 1977;38(03):1400B. (UMI No. 7717868) [Google Scholar]
- Green C.W., Reid D.H. Defining, validating, and increasing indices of happiness among people with profound multiple disabilities. Journal of Applied Behavior Analysis. 1996;29:67–78. doi: 10.1901/jaba.1996.29-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Hammen C.L., Glass D.R. Depression, activity, and evaluation of reinforcement. Journal of Abnormal Psychology. 1975;84:718–721. doi: 10.1037//0021-843x.84.6.718. [DOI] [PubMed] [Google Scholar]
- Hedges L.V. Distribution theory for Glass's estimator of effect size and related estimators. Journal of Educational Statistics. 1981;6:107–128. [Google Scholar]
- Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analysis. British Medical Journal. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopko D.R., Lejuez C.W. Oakland, CA: New Harbinger; 2007. A cancer patient's guide to overcoming depression & anxiety: Getting through treatment & getting back to your life. [Google Scholar]
- Hopko D.R., Lejuez C.W., Ruggiero K.J., Eifert G.H. Contemporary behavioral activation treatments for depression: Procedures, principles and progress. Clinical Psychology Review. 2003;23:699–717. doi: 10.1016/s0272-7358(03)00070-9. [DOI] [PubMed] [Google Scholar]
- Jacobson N.S. Contextualism is dead: Long live contextualism. Family Process. 1994;33:97–100. [Google Scholar]
- Jacobson N.S., Martell C.R., Dimidjian S. Behavioral activation treatment for depression: Returning to contextual roots. Clinical Psychologist. 2001;8:255–270. [Google Scholar]
- Klinger E. Consequences of commitment to and disengagement from incentives. Psychological Review. 1975;82:223–231. [Google Scholar]
- Lancioni G.E., Singh N.N., O'Reilly M.F., Sigafoos J., Didden R., Oliva D., et al. Effects of microswitch-based programs on indices of happiness of students with multiple disabilities: A new research evaluation. American Journal on Mental Retardation. 2007;112:167–176. doi: 10.1352/0895-8017(2007)112[167:EOMPOI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Lejuez C.W., Hopko D.R., LePage J.P., Hopko S.D., McNeil D.W. A brief behavioral activation treatment for depression. Cognitive and Behavioral Practice. 2001;8:164–175. [Google Scholar]
- Lewinsohn P.M. Friedman R.J., Katz M.M. Washington, DC: Winston-Wiley; 1974. A behavioral approach to depression. The psychology of depression: Contemporary theory and research; pp. 157–185. [Google Scholar]
- Lewinsohn P.M. Thorensen C.E., Krumboltz J. New York: Holt, Rinehart & Winston; 1976. Activity schedules in the treatment of depression. Counseling methods; pp. 74–83. [Google Scholar]
- Lewinsohn P.M., Graf M. Pleasant activities and depression. Journal of Consulting and Clinical Psychology. 1973;41:261–268. doi: 10.1037/h0035142. [DOI] [PubMed] [Google Scholar]
- Lewinsohn P.M., Libet J. Pleasant events, activity schedules, and depression. Journal of Abnormal Psychology. 1972;79:291–295. doi: 10.1037/h0033207. [DOI] [PubMed] [Google Scholar]
- Lewinsohn P.M., Sullivan J.M., Grosscap S.J. Changing reinforcing events: An approach to the treatment of depression. Psychotherapy: Theory, research and practice. 1980;17:322–334. [Google Scholar]
- Light R.J., Pillemer D.B. Cambridge, MA: Harvard University Press; 1984. Summing up: The science of reviewing research. [Google Scholar]
- Lipsey M.W., Wilson D.B. Thousand Oaks, CA: Sage Publications; 2001. Practical meta-analysis. [Google Scholar]
- Little B. Personal projects: A rationale and method for investigation. Environment and Behavior. 1983;15:273–309. [Google Scholar]
- *.Lovett S., Gallagher D. Psychoeducational interventions for family caregivers: Preliminary efficacy data. Behavior Therapy. 1988;19:321–330. [Google Scholar]
- Lyubomirsky S. New York: Penguin; 2008. The how of happiness: A scientific approach to getting the life you want. [Google Scholar]
- Lyubomirsky S., King L., Diener E. The benefits of frequent positive affect: Does it lead to success? Psychological Bulletin. 2005a;131:803–855. doi: 10.1037/0033-2909.131.6.803. [DOI] [PubMed] [Google Scholar]
- Lyubomirsky S., Sheldon K.M., Schkade D. Pursuing happiness: The architecture of sustainable change. Review of General Psychology. 2005b;9:111–131. [Google Scholar]
- MacPhillamy D.J., Lewinsohn P.M. Depression as a function of levels of desired and obtained pleasure. Journal of Abnormal Psychology. 1974;83:651–657. doi: 10.1037/h0037467. [DOI] [PubMed] [Google Scholar]
- MacPhillamy D.J., Lewinsohn P.M. The Pleasant Events Schedule: Studies on reliability, validity, and scale inter-correlation. Journal of Consulting and Clinical Psychology. 1982;50:363–380. [Google Scholar]
- Martell C.R., Addis M.E., Jacobson N.S. New York: W.W. Norton; 2001. Depression in context: Strategies for guided action. [Google Scholar]
- Mazzucchelli T.G., Kane R.T., Rees C.S. Behavioral activation treatments for depression in adults: A meta-analysis and review. Clinical Psychology: Science and Practice. 2009;16:383–411. [Google Scholar]
- *.McLean P.D., Hakstian A.R. Clinical depression: Comparative efficacy of outcome treatments. Journal of Consulting and Clinical Psychology. 1979;47:818–836. doi: 10.1037//0022-006x.47.5.818. [DOI] [PubMed] [Google Scholar]
- *.McLean P.D., Hakstian A.R. Relative endurance of unipolar depression treatment effects: Longitudinal follow-up. Journal of Consulting and Clinical Psychology. 1990;58:482–488. doi: 10.1037//0022-006x.58.4.482. [DOI] [PubMed] [Google Scholar]
- Meyer B., Berger T., Caspar F., Beevers C.G., Andersson G., Weiss M. Effectiveness of a novel integrative online treatment for depression (Deprexis): Randomized controlled trial. Journal of Medical Internet Research. 2009;11:e15. doi: 10.2196/jmir.1151. Retrieved May 13, 2009, from http://www.jmir.org/2009/2/e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Padfield M. The comparative effects of two counseling approaches on the intensity of depression among rural women of low socioeconomic status. Journal of Counseling Psychology. 1976;23:209–214. [Google Scholar]
- Pressman S.D., Cohen S. Does positive affect influence health? Psychological Bulletin. 2005;131:925–971. doi: 10.1037/0033-2909.131.6.925. [DOI] [PubMed] [Google Scholar]
- Rehm L.P., Kaslow N.J., Rabin A.S. Cognitive and behavioral targets in a self-control therapy program for depression. Journal of Consulting and Clinical Psychology. 1987;55:60–67. doi: 10.1037//0022-006x.55.1.60. [DOI] [PubMed] [Google Scholar]
- *.Reich J.W., Zautra A. Life events and personal causation: Some relationships with satisfaction and distress. Journal of Personality and Social Psychology. 1981;41:1002–1012. doi: 10.1037//0022-3514.41.5.1002. [DOI] [PubMed] [Google Scholar]
- *.Rokke P.D. Processes of change in depression: A self-control perspective. Dissertation Abstracts International. 1985;46(12):4413B. (UMI No. 8602306) [Google Scholar]
- Rosenthal R. The ‘file drawer problem’ and tolerance for null results. Psychological Bulletin. 1979;86:638–641. [Google Scholar]
- Rosenthal R., DiMatteo M.R. Meta-analysis: Recent developments in quantitative methods for literature reviews. Annual Review of Psychology. 2001;52:59–82. doi: 10.1146/annurev.psych.52.1.59. [DOI] [PubMed] [Google Scholar]
- Seligman M.E.P. New York: Free Press; 2002. Authentic happiness: Using the new positive psychology to realize your potential for lasting fulfillment. [Google Scholar]
- Seligman M.E.P., Rashid T., Parks A.C. Positive psychotherapy. American Psychologist. 2006;61:774–788. doi: 10.1037/0003-066X.61.8.774. [DOI] [PubMed] [Google Scholar]
- Seligman M.E.P., Steen T.A., Park N., Peterson C. Positive psychology progress: Empirical validation of interventions. American Psychologist. 2005;60:410–421. doi: 10.1037/0003-066X.60.5.410. [DOI] [PubMed] [Google Scholar]
- Sin N.L., Lyubomirsky S. Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: A practice-friendly meta-analysis. Journal of Clinical Psychology: In Session. 2009;65:467–487. doi: 10.1002/jclp.20593. [DOI] [PubMed] [Google Scholar]
- *.Stark K.D., Reynolds W.M., Kaslow N.J. A comparison of the relative efficacy of self-control therapy and a behavioral problem-solving therapy for depression in children. Journal of Abnormal Child Psychology. 1987;15:91–113. doi: 10.1007/BF00916468. [DOI] [PubMed] [Google Scholar]
- Teri L., Logsdon R.G., Uomoto J., McCurry S.M. Behavioral treatment of depression in dementia patients: A controlled clinical trial. Journal of Gerontology. Series B, Psychological Sciences Social Sciences. 1997;52:159–166. doi: 10.1093/geronb/52b.4.p159. [DOI] [PubMed] [Google Scholar]
- *.Turner R.W., Ward M.F., Turner J. Behavioral treatment for depression: An evaluation of therapeutic components. Journal of Clinical Psychology. 1979;35:166–175. doi: 10.1002/1097-4679(197901)35:1<166::aid-jclp2270350127>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- *.van den Hout J.H.C., Arntz A., Kunkels F.H.J. Efficacy of a self-control therapy program in a psychiatric day-treatment center. Acta Psychiatrica Scandinavica. 1995;92:25–29. doi: 10.1111/j.1600-0447.1995.tb09538.x. [DOI] [PubMed] [Google Scholar]
- *.Weinberg L. Behaviorally and cognitively oriented approaches to the alleviation of depressive symptoms in college students. Dissertation Abstracts International. 1978;38(07):3422B. (UMI No. 7728140) [Google Scholar]
- *.Wilson P.H., Goldin J.C., Charbonneau-Powis M. Comparative efficacy of behavioral and cognitive treatments of depression. Cognitive Therapy and Research. 1983;7:111–124. [Google Scholar]
- *.Wright T.P. The effectiveness of behavioral activation group therapy: Treating comorbid depression on a specialized inpatient posttraumatic stress disorder unit for combat veterans. Dissertation Abstracts International. 2003;64(01):436B. (UMI No. 3077387) [Google Scholar]
- Yu D.C.T., Spevack S., Hiebert R., Martin T.L., Goodman R., Martin T.G., et al. Happiness indices among persons with profound and severe disabilities during leisure and work activities: A comparison. Education and Training in Mental Retardation and Developmental Disabilities. 2002;37:421–426. [Google Scholar]


