Abstract
Background
Data on likely postdischarge outcomes are important for decision making about chronically critically ill patients. It seems reasonable to categorize outcomes into “better” or overall desirable states and “worse” or generally undesirable states. Survival, being at home, and being cognitively intact are commonly identified as important to quality of life and thus may be combined to describe composite outcome states.
Objective
To categorize postdischarge outcome states of chronically critically ill patients and identify predictors of better and worse states.
Methods
Reanalysis of data from a trial of a disease management program for chronically critically ill patients. Two composite outcomes were created: (1) the “better” outcome: no cognitive impairment at 2 months after discharge and alive and at home at 4 months (ie, met all 3 criteria), and (2) the “worse” outcome: cognitive impairment 2 months after discharge, or death after discharge, or not living at home 4 months after discharge (ie, met at least 1 of these criteria).
Results
Of 218 patients not requiring ventilatory support at discharge, 111 (50.9%) had a better outcome. Of 159 patients who were cognitively intact at discharge, 111 (69.8%) had a better outcome. Of the 39 patients who required ventilatory support at discharge, only 1 (3%) achieved the better outcome. Of 98 patients who were cognitively impaired at discharge, only 29 (30%) had the better outcome.
Conclusion
Need for mechanical ventilatory support and persistent cognitive impairment at discharge were associated with worse outcomes 4 months after discharge.
Girard and Raffin1 first used the term “chronically critically ill” (CCI) in 1985 to describe patients in the intensive care unit (ICU) who survived an initial period of life-threatening illness but remained dependent on the high-technology services of the critical care unit. Since then, interest in describing the outcomes and resource utilization of these patients has increased steadily. Although no consensus has been reached about the precise definition of chronic critical illness, an ICU stay extending beyond 1 week and prolonged mechanical ventilation (>72 hours) are common criteria.2–4 Numerous investigations since the year 2000 have documented the high in-hospital mortality and continuing postdischarge morbidity in CCI patients.2–10
It is generally recognized that survival alone is not the only important outcome. Interviews with patients and their family members have consistently shown that they rate such outcomes as functional status, independence, ability to live at home, and burden on family as equal to and sometimes more important than length of survival.11,12 Patients have demonstrated the propensity to engage in rational decision making when faced with choices about treatment, weighing benefits and burdens.13 Patients’ preferences expressed in hypothetical situations are influenced by information provided by clinicians about probabilities of different outcomes and stem from preexisting beliefs, cultural and religious values, or worldviews regarding the purpose of life and the role of humanity, God, and medicine.14,15
Care of the CCI inevitably involves counseling patients, or more often family decision makers, about likely outcomes and also about probable burdens and benefits of possible interventions, such as tracheostomy, percutaneous gastrostomy for artificial nutrition and hydration, and cardiopulmonary resuscitation. Frequently asked questions of critical care clinicians include, Will he be able to come home?, Will she wake up?, or some version of, Will my family member have a good outcome? Answering these questions is difficult and often leaves both clinicians and family members with persistent uncertainty about the best course of action. In addition to factual updates about the patient’s condition and treatment options, discussion of probable long-term outcomes and eventual quality of life are often central.
Data regarding likely postdischarge outcomes may be useful and important in decision making. However, researchers in previous studies have typically reported mortality, quality of life of survivors, and post-discharge functional status as discrete, separate outcomes. We suggest that it is not only reasonable but may be more consistent with how people think about final outcomes states to categorize outcomes into “better” or overall desirable states and “worse” or generally undesirable states. Preferences regarding survival and acceptable quality of life are inherently idiosyncratic, and previous research has confirmed wide variation in decisions about aggressiveness of care and treatment limitations, often related to cultural variations.16,17 Nevertheless, studies also have shown that cognitive status, ability to return home, and freedom from dependence on technology (in this case, mechanical ventilation) all are common and important components of a desirable quality of life to most patients and their family decision makers.12–14 Therefore, combining these outcomes into final composite states may be more meaningful and helpful for some in discussions of benefits and burdens.
The purpose of this report is to examine “better” and “worse” composite outcome states through analysis of data from a large study of CCI patients and to identify predictors of these composite states. The primary outcome data from this study are presented else where,3 and the analysis provided here is offered as an alternative approach to traditional outcome evaluation.
Methods
Data from a trial of a postdischarge disease management program for CCI patients (those requiring >72 hours of in-hospital mechanical ventilation) provided the data for this analysis. The parent study was a randomized trial designed to test the effect of a disease management program on patient and family outcomes.
Sample
Subjects in the original trial were drawn from the adult intensive care units of University Hospitals of Cleveland, a 950-bed academic medical center. Data were obtained on all patients who underwent mechanical ventilation for more than 72 hours. Patients or family decision makers (for patients who were not cognitively intact) were approached for consent to participate if the patient survived to discharge, was English speaking, and had a discharge location within 80 miles of the study site. Approval was obtained from the hospital’s institutional review board before the start of the study.
Study Procedures
For the parent study, research nurses made rounds in the study hospital’s 4 adult ICUs every day and identified eligible patients. Patients who were ventilator dependent before hospitalization, who were referred to hospice before discharge, or who were receiving case management from the transplant team were excluded. After informed consent was obtained, a permuted block randomization scheme was used to randomly assign patients to the intervention or control group. Patients assigned to the intervention group received the disease management program services beginning just before discharge and for the following 2 months. Control group patients were interviewed at discharge and contacted every 2 weeks for tracking of location and survival status. At 4 months after discharge, all patients (or their family member) were contacted a final time to determine the patient’s status (survival and location).
Previous analysis established that the intervention and control groups did not differ significantly in age, sex, race, number of comorbid conditions, duration of mechanical ventilation and length of hospital stay, reason for mechanical ventilation, or discharge disposition.3 The control group had a significantly higher score than the intervention group on the Acute Physiology and Chronic Health Evaluation (APACHE) at admission (74.6 vs 67.4, P = .02), and the intervention group had a significantly lower score than the control group on the physical component of the Medical Outcomes Study Short Form (SF-8) at discharge (30.6 vs 35.8, P = .003). The 2 groups did not differ significantly in postdischarge mortality or readmission rate. For the purposes of this report, intervention and control groups were combined.
All study staff were trained on the use of research instruments. Before subjects were enrolled and quarterly thereafter, research nurses participated in interrater reliability with the focus being on data from the in-hospital charts and the APACHE III. Approximately 8% of all cases (n = 83) were used; interrater reliability was maintained at acceptable levels (r, >0.80; κ, >0.70; agreement, >80%). Instruments used in the present report include the APACHE III, the SF-8, and the Katzman Short Orientation-Memory Concentration Test. Demographic and clinical data (eg, age, length of stay, number of comorbid conditions, length of mechanical ventilation, and ventilator dependency at discharge) were obtained from the medical record and from interviews of patients and their families at discharge and 2 months after discharge, either by phone or in-person interview. Patients (or their family caregivers) were contacted again by telephone 4 months after discharge from the hospital to determine their survival status and location.
The APACHE III is a well-established tool for classifying severity of illness that measures mortality risk by using physiological and chronic health data taken from the first 24 hours after ICU admission. APACHE scores range from 0 to 299, with higher scores representing higher risk of death. Reliability and validity of the APACHE III have been established.18
The SF-8 consists of 8 items and yields scores for 2 subscales of health-related quality of life (physical and mental). Scores range from 14.1 to 64.0 on the physical component subscale and from 6.8 to 70.4 on the mental component subscale. For both subscales, higher scores indicate a better health status. Reliability and validity have been established.19 The SF-8 score was obtained on the day of discharge or within 1 week of discharge as a measure of the patient’s health status at that time. Patients were also asked to complete the SF-8 in reference to their health status for the week before their hospitalization. Family proxies were asked to complete the SF-8 for those patients who were assessed as cognitively impaired. The Katzman Short Orientation-Memory Concentration Test was used to determine cognitive status (impaired vs not impaired) before the interviews were conducted. The test includes 6 questions, with possible scores of 0 (normal) to 28. For the purpose of the present study, a patient with a Katzman score greater than 6 was considered cognitively impaired. This approach has been used by others. Reliability of this tool has been established.20
Analysis
In order to describe long-term composite outcome states, patients were categorized according to the following variables: survival status at 4 months, cognitive status at 2 months after discharge (the end of the intervention period), and location at 4 months. Two composite outcomes were created: (1) the “better” outcome, consisting of no cognitive impairment at 2 months, alive at 4 months, and at home at 4 months (ie, met all 3 criteria); and (2) the “worse” outcome, consisting of cognitive impairment at 2 months after discharge, or death after discharge, or not living at home at 4 months (ie, met at least 1 of these criteria). Although independence from technological support could also be considered a criterion of a good outcome, no one in our sample who continued to require mechanical ventilation was able to return home, and therefore location at 4 months can also be seen as a proxy for liberation from mechanical ventilation. Differences between patients in each of the outcome states were tested with the Fisher exact test for categorical variables and analysis of variance for interval level variables. Survival analysis was used to examine mortality risk over time associated with ventilator status at discharge.
Results
Table 1 shows the demographic and clinical characteristics of the sample used for this report. Of the 1041 patients ventilated more than 72 hours, 393 (37.8%) died before hospital discharge. Of the remaining patients, 334 survived hospitalization, were eligible to enroll, and consented to participate in the postdischarge portion of the original study. On the whole, this sample is similar to other cohorts recently described in the literature in that participants were in their early 60s, predominantly white, evenly divided between males and females, and required 2 to 3 weeks of critical care.5,7,8 Although the mean number of comorbid conditions on admission (5.6) and the number of medications used before admission (4.8) reflect some chronic illness burden, most patients (90.7%) were living independently in their own home before admission.
Table 1.
Sample characteristics (N = 334)
| Variable | Mean (SD) | Median | Confidence interval |
|---|---|---|---|
| Age, y | 60.9 (16.5) | 61.0 | 59.2–62.8 |
| Acute Physiology Score | 59.0 (25.9) | 56.5 | 56.2–61.9 |
| Glasgow Coma Scale score | 8.5 (13.4) | 0 | 7.1–10.0 |
| No. of comorbid diseases | 5.6 (3.3) | 5.0 | 5.2–5.9 |
| No. of medications before admission | 4.8 (4.0) | 4.0 | 4.3–5.2 |
| Hospital stay, days | 24.2 (15.0) | 20.0 | 22.6–25.9 |
| Intensive care unit stay, days | 17.2 (13.7) | 13.0 | 15.7–18.7 |
| Mechanical ventilation, days | 11.9 (10.9) | 8.0 | 10.8–13.1 |
| No. (%) of participants |
|
|---|---|
| Female sex | 187 (56.0) |
| White race | 206 (61.9) |
| Lived at home before admission | 303 (90.7) |
| Admitted to medical intensive care unit | 163 (48.8) |
| Reason for mechanical ventilation | |
| Postoperative | 83 (24.9) |
| Respiratory insufficiency | 164 (49.1) |
| Airway protection | 69 (20.7) |
| Cardiac arrest | 18 (5.4) |
| Primary diagnosisa | |
| Pulmonary disease | 82 (24.6) |
| Coronary artery disease | 73 (21.9) |
| Neurological disorder | 59 (17.7) |
| Other (gastrointestinal, cancer, etc) | 120 (36.0) |
From the International Classification of Diseases, Ninth Revision.
Survival After Discharge
Of the 334 patients enrolled in the parent study, cognitive status at discharge was missing on 3 subjects, and 74 additional subjects were eventually lost to follow-up during the postdischarge period. Of the 257 patients for whom full data were available, 192 (74.7%) were alive 4 months after discharge from the hospital. Patients who died were on average older (68.3 vs 58.2 years old) and had more preexisting comorbid conditions before their hospitalization (6.19 vs 5.05) than did those patients who were alive 4 months after hospital discharge.
Cognitive Status After Discharge
First we examined the postdischarge status for patients who were versus patients who were not cognitively intact at hospital discharge. Of the 257 patients for whom full follow-up data are available, 159 (61.9%) were cognitively intact at discharge and 111 (69.8%) of this group were cognitively intact at 2 months and alive and at home at four months. Of the 98 (38.1% of patients for whom full data are available) who were cognitively impaired at discharge, however, only 29 (30%) were cognitively intact at 2 months and alive and residing at home at 4 months after discharge (P = .001).
Ventilator Status After Discharge
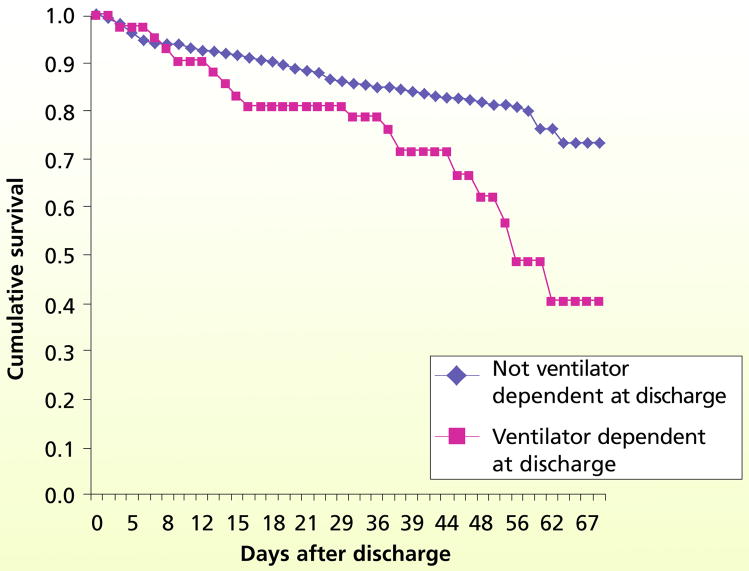
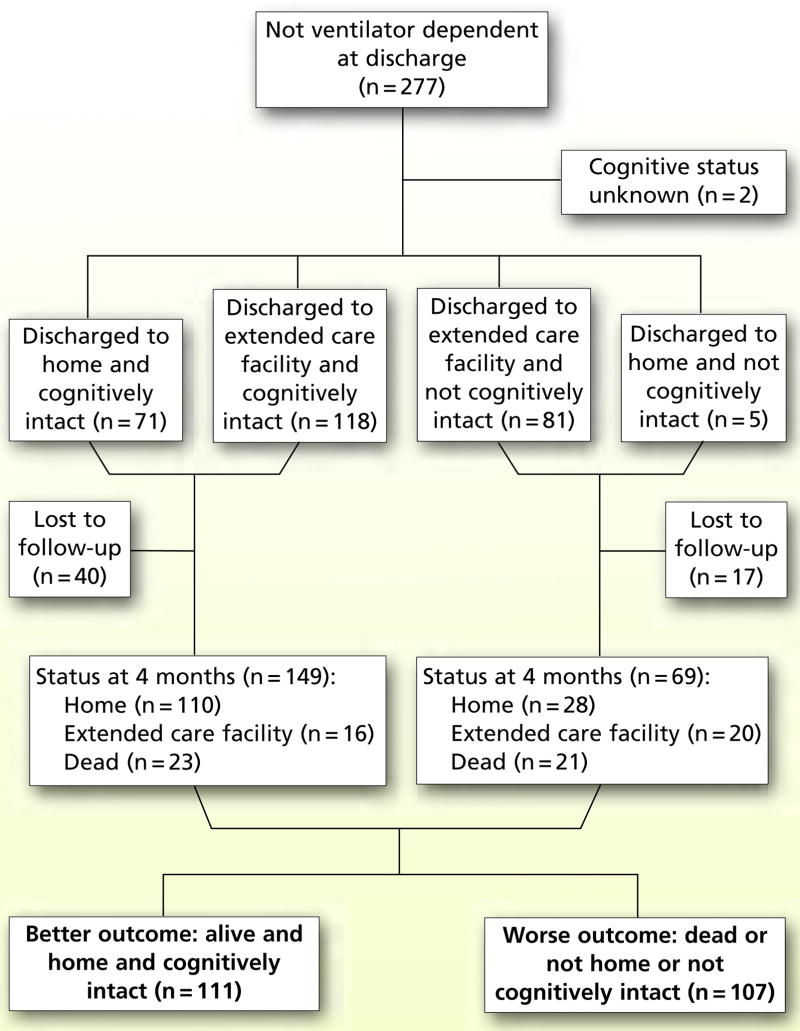
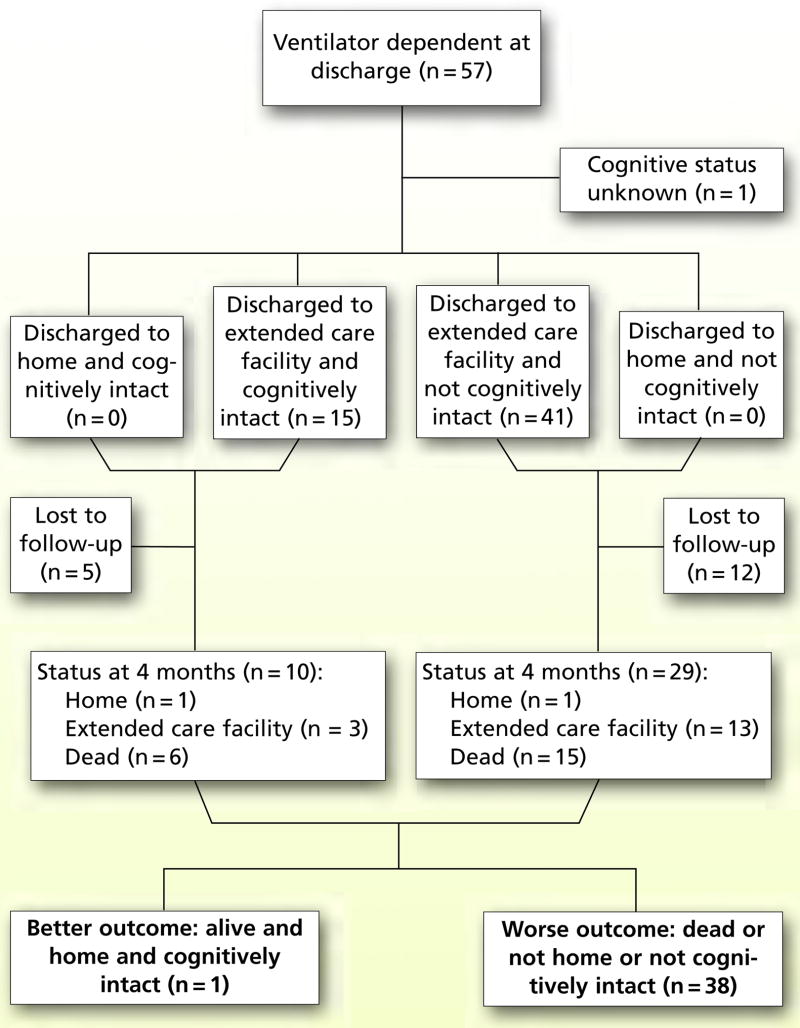
Using survival analytic techniques, we examined postdischarge mortality for patients who were ventilator dependent at discharge versus patients who were not. The survival curve (Figure 1) differs over time for the 2 groups. By 4 months after discharge, 20.2% (n = 44) of those who were not ventilator dependent at discharge had died, compared with a mortality rate of 53.8% (n = 21) for those patients who were ventilator dependent at discharge (P = .001). For patients who were ventilator dependent at discharge, 88.8% of those alive at 4 months were residing in an institutional setting, compared with 20.7% of those discharged who were not ventilator dependent (P = .001). Of the 39 patients discharged with some level of mechanical ventilatory support (eg, positive pressure mechanical ventilation for some hours each day) for whom we have complete data, 2 were home at 4 months. Only 1 of these patients had regained cognitive capacity by 2 months after discharge. Finally, 51% of patients not ventilator dependent at discharge had reached the “better outcome” (alive, cognitively intact, and living at home 4 months after discharge) as compared with only 2.5% of patients who were ventilator dependent at discharge (P = .001). Figures 2 and 3 show the composite outcomes for those patients who were and were not ventilator dependent at discharge.
Figure 1.
Survival analytic curves for patients who were ventilator dependent at discharge and patients who were not (n = 272).
Figure 2.
Composite outcomes of patients who were not ventilator dependent at discharge.
Figure 3.
Composite outcomes of patients who were ventilator dependent at discharge.
Intermediate Outcomes
Cognitive status at discharge and ventilator status at discharge are both intermediate variables in that they reflect the patient’s status at a point in time that falls between admission characteristics and final outcome. In addition to these discharge or intermediate variables of cognitive status and ventilator status, we were interested in examining possible influences of characteristics of patients before admission and duration of mechanical ventilation. We used χ2 tests and analysis of variance to examine bivariate relationships between composite outcomes and demographic characteristics and commonly identified risk factors (age, ethnicity, sex, preexisting conditions, preadmission health state, and APACHE score at admission) as shown in Table 2. This analysis demonstrated that, in addition to cognitive and ventilator status at discharge, older age and greater duration of mechanical ventilation were associated with worse outcomes.
Table 2.
Bivariate relationship between final status for patients who are alive and at home 4 months and cognitively intact 2 months after discharge (n = 257) and characteristics of patientsa
| Characteristic | Alive and at home 4 months and cognitively intact at 2 months after discharge from the hospital |
Pb | |
|---|---|---|---|
| Yes (n = 112) | No (n = 145) | ||
|
No. (%) of patients |
<.001 | ||
| Cognitively intact at discharge | |||
| Yes | 108 (96.4) | 54 (37.2) | |
| No | 4 (3.6) | 91 (62.8) | |
| Racec | .50 | ||
| White | 70 (63.1) | 97 (67.8) | |
| African American | 41 (36.9) | 46 (32.2) | |
| Sex | .50 | ||
| Female | 65 (58.0) | 77 (53.1) | |
| Male | 47 (42.0) | 68 (46.9) | |
| Ventilator status at discharge | <.001 | ||
| Receiving ventilator support | 1 (0.9) | 38 (26.2) | |
| Not receiving ventilator support | 111 (99.1) | 107 (73.8) | |
| Age, years (range, 18–93) |
Mean (median) |
<.001 | |
| 55.3 (55) | 63.7 (64) | ||
| Days of mechanical ventilation (range, 3–72) | 9.1 (6) | 13.9 (9) | <.001 |
| Health-related quality of life Mental scale (SF-8) (range, 15.4–67.6) | 46.8 (52.6) | 43.8 (45.2) | .07 |
| Health-related quality of life Physical scale (SF-8) (range, 16.4–67.5) | 44.4 (47.6) | 42.5 (44.7) | .20 |
| Number of preexisting conditions (range, 0–18) | 4.98 (5) | 5.5 (5) | .20 |
| Acute Physiology Score (range, 6–155) | 61.1 (57) | 57.8 (55) | .30 |
Patients who dropped out, were lost to follow-up, or whose cognitive status or location were unknown are not included in the analyses.
Denotes 2-sided significance level for a bivariate test of association using the Fisher exact test for categorical factors and the Mann-Whitney test for interval measured factors.
One patient in the Yes category and 2 patients in the No category did not provide information on race.
Discussion
As mentioned earlier, the labeling of the composite outcomes as “better” or “worse” is unquestionably heavily value-laden. Patients and families who believe that life of any quality is valuable and worth preserving, individuals who have strong beliefs that the role of humans is to use the talents and abilities bestowed by God or a higher power and allow God to choose the time of death, and those who believe that recovery is likely despite poor prognostic indicators are all likely to reject this categorization.
Nevertheless, few people would argue that surviving a life-threatening illness, regaining cognitive capacity, and being able to return to one’s own home are not important benefits and desirable outcomes. For families trying to decide whether or not their loved one would find the burdens of continued and sometimes escalated treatment to be justified by eventual benefits, the probability of achieving these outcome states is relevant.
The predictive strength of cognitive status at discharge and inability to be weaned off of ventilatory support by discharge will not surprise critical care professionals. However, ICU doctors and nurses rarely have access to postdischarge information. Given the availability of extended care facilities that can accept ventilator patients as direct transfers from the ICU, supporting patients to the point of relative physiological stability and readiness for transfer to a weaning center or long-term acute care facility is likely to be seen as a success. We believe that knowledge of exactly how rare “better” outcomes are for those patients who are cognitively impaired and ventilator dependent at discharge is important information for ICU clinicians who are counseling families about treatment decisions. Supporting this view, Fumis and colleagues21 recently reported that dissatisfaction with information about the consequences of illness was the aspect of communication most often complained about in their survey of ICU family members.
A number of decisions are faced by families of CCI patients, and these issues are presented more or less explicitly, with more or less neutrality by the ICU staff. These decisions include resuscitation status, tracheostomy, insertion of a percutaneous gastrostomy tube, and sometimes dialysis. All of these interventions are likely to be needed for patients who require long-term mechanical ventilation if the goal is survival in any state. If, however, limited (ie, <4 months) survival after discharge, inability to ever return home, and persistent impaired cognitive function would be seen as relevant and significant aspects of the benefit/burden analysis, explicit discussion of the probability of these outcome states should be a routine part of ongoing discussions with families of CCI patients. Knowledge of the significance of cognitive status and continued ventilator dependence can be used to reach consensus about important milestones to be used in judging meaningful progress. For example, for patients themselves or for those families who are confident that the patient would not find prolonged and technology-dependent survival in an extended-care facility or life without the ability to interact with others to be acceptable, progress in weaning or improvement in cognitive status can be specified as the important milestones that must be reached before further supportive interventions (eg, tracheostomy or percutaneous gastrostomy) would be justified.
The generalizability of the predictive data generated by this study is limited by the characteristics of the study sample. Although we found no clinical or demographic differences between patients who refused to participate (n = 185, 35%) and patients who were enrolled, it is possible that our sample is not representative of the CCI population. Most of our patients were either admitted for exacerbation of previously stable chronic illnesses or were postoperative patients. The sample had very few trauma patients and no burn patients. Recovery patterns and the prognostic significance of prolonged mechanical ventilation are likely to be quite different in trauma and burn patients. In addition, discharge patterns for the study site were affected by the availability of long-term acute care facilities that accepted ventilator-dependent patients in our area; lack of such facilities in other geographic locations might contribute to different prognostic implications of discharge ventilatory status. Given the age of our sample, results also may not be generalizable to younger patients.
In addition, the assessment of cognitive status and preadmission health status could be sources of some inaccuracy. The Katzman test is a widely used and well-validated instrument for screening for impairments in memory or cognition, but it is not a precise diagnostic tool. Although it has been validated in neurologically impaired samples22 and medically ill inpatients,23 reliability and validity have not been established in CCI patients. It is possible, therefore, that patients with some mild impairment may have been able to score in the adequate range and, conversely, some patients who retained adequate capacity may have simply been too tired to perform well on the day of the interview. Data on patients’ health status before admission, collected with the SF-8, were obtained primarily from family members. Although proxies have been used by others to obtain health status data,8 some differences between patients’ and family members’ rating of health states have been noted by others.24 Finally, it is possible that capturing data from the “lost to follow-up” patients or obtaining measurement of outcomes at 6 or 12 months might have resulted in differing proportions of patients who achieved the “better” outcome state.
Comparison of our results with those of others is difficult because of variation in sample eligibility, length of follow-up, and tendency of most reports to focus on survival, quality of life, or return home as single discrete outcomes. Nevertheless, some commonalities are striking. We found a 66.1% cumulative 1-year mortality rate in an earlier study2 and a 4-month cumulative mortality of 46.7% in this study. Teno et al6 reported a 44% in-hospital mortality among the SUPPORT trial patients with an ICU stay exceeding 14 days. Combes et al10 similarly reported a 44% in-hospital mortality in patients requiring mechanical ventilation for more than 14 days, and we documented a 37.7% in-hospital mortality in patients using mechanical ventilation for more than 3 days in our series. In SUPPORT, 19.6% of survivors had died by 6 months, for a cumulative mortality of 55%.6 Chelluri et al,8 studying patients who underwent more than 48 hours of mechanical ventilation, found a cumulative 1-year mortality of 56%. Thus, when we compare in-hospital and post-discharge survival, our results seem consistent with those of others.
This report is intended to offer clinicians a new and potentially more informative way to think about and discuss eventual outcomes. Broad consensus exists among critical care professionals that survival alone is an inadequate measure of benefit and that the subjective perceptions and experience of the patient must be included in evaluating treatment outcomes.9,25,26 Patients and their families, of course, do not just experience survival, or freedom from ventilator dependency, or the ability to think clearly, or return home; they experience a composite state of all of these dimensions and weigh each according to unique preferences and values. For some, single discrete outcomes such as survival alone or cognitive capacity alone may outweigh all other considerations.
Nevertheless, explicit discussion of probabilities of outcome states that provide patients and families with a comprehensive picture of what lies ahead may be more meaningful than focusing on limited aspects of recovery. Lilly and colleagues27 have demonstrated that early and frequent discussions using concrete milestones that assist families in evaluating progress or lack of improvement can improve consensus and minimize prolonged use of ineffective resources. Continued measurement and prospective evaluation of composite outcomes, such as reported here, can only help us in these essential discussions. Future studies to explicitly test the extent to which family decision makers find information about composite outcomes to be meaningful and useful, and validation of the components of desirable outcome states should be pursued.
Notice to CE enrollees
A closed-book, multiple-choice examination following this article tests your under standing of the following objectives:
Describe a method used to categorize the post-discharge outcomes states of chronically critically ill patients.
Discuss the potential benefits associated with explicit discussions focused on the probable outcomes for chronically critically ill patients and families.
Recognize the limitations of using survival alone as a measure of benefit for chronically critically ill patients.
To read this article and take the CE test online, visit www.ajcconline.org and click “CE Articles in This Issue.” No CE test fee for AACN members.
eLetters
Now that you’ve read the article, create or contribute to an online discussion on this topic. Visit www.ajcconline.org and click “Respond to This Article” in either the full-text or PDF view of the article.
Footnotes
To purchase electronic or print reprints, contact The InnoVision Group, 101 Columbia, Aliso Viejo, CA 92656. Phone, (800) 899-1712 or (949) 362-2050 (ext 532); fax, (949) 362-2049; reprints@aacn.org.
FINANCIAL DISCLOSURES
This work was supported by funding from the National Institutes of Health (NR-8941).
References
- 1.Girard K, Raffin TA. The chronically critically ill: To save or let die? Resp Care. 1985;30(5):339–347. [PubMed] [Google Scholar]
- 2.Douglas SL, Daly BJ, Gordon N, Brennan PF. Survival and quality of life: short-term versus long-term ventilator patients. Crit Care Med. 2002;30:2655–2662. doi: 10.1097/00003246-200212000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Daly BJ, Douglas SL, Kelley CG, O’Toole E, Montenegro H. Trial of a disease management program to reduce hospital readmissions of the chronically critically ill. Chest. 2005;128:507–517. doi: 10.1378/chest.128.2.507. [DOI] [PubMed] [Google Scholar]
- 4.MacIntyre NR, Epstein SK, Carson S, et al. Management of patients requiring prolonged mechanical ventilation: report of a NAMDRC consensus conference. Chest. 2005;128:3937–3954. doi: 10.1378/chest.128.6.3937. [DOI] [PubMed] [Google Scholar]
- 5.Im K, Belle SH, Schultz R, Mendelsohn AB, Chelluri L QOL-MV Investigators. Prevalence and outcomes of caregiving after prolonged (>48 hours) mechanical ventilation in the ICU. Chest. 2004;125:597–606. doi: 10.1378/chest.125.2.597. [DOI] [PubMed] [Google Scholar]
- 6.Teno JM, Fisher E, Hamel MB, et al. Decision-making and outcomes of prolonged ICU stays in seriously ill patients. J Am Geriatr Soc. 2000;48(5 suppl):S70–S74. doi: 10.1111/j.1532-5415.2000.tb03144.x. [DOI] [PubMed] [Google Scholar]
- 7.Nasraway SA, Button GJ, Rand WM, Hudson-Jinks T, Gustafson M. Survivors of catastrophic illness: outcomes after direct transfer from intensive care to extended care facilities. Crit Care Med. 2000;28:19–25. doi: 10.1097/00003246-200001000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Chelluri L, Im KA, Belle SH, et al. Long-term mortality and quality of life after prolonged mechanical ventilation. Crit Care Med. 2004;32(1):61–69. doi: 10.1097/01.CCM.0000098029.65347.F9. [DOI] [PubMed] [Google Scholar]
- 9.Carson SS, Bach PB. The epidemiology and costs of chronic critical illness. Crit Care Clin. 2002;18:461–476. doi: 10.1016/s0749-0704(02)00015-5. [DOI] [PubMed] [Google Scholar]
- 10.Combes A, Costa MA, Trouillet JL, et al. Morbidity, mortality, and quality of life outcomes of patients requiring >14 days of mechanical ventilation. Crit Care Med. 2003;31:1373–1381. doi: 10.1097/01.CCM.0000065188.87029.C3. [DOI] [PubMed] [Google Scholar]
- 11.Fried TR, Bradley EH, Towle VR, Allore H. Understanding the treatment preferences of the seriously ill. N Engl J Med. 2002;346:1061–1066. doi: 10.1056/NEJMsa012528. [DOI] [PubMed] [Google Scholar]
- 12.Pearlman RA, Cain KC, Patrick DL, et al. Insights pertaining to patient assessments of states worse than death. J Clin Ethics. 1993;4(1):33–40. [PubMed] [Google Scholar]
- 13.Lloyd CB, Nietert PJ, Silvestri GA. Intensive care decision making in the seriously ill and elderly. Crit Care Med. 2004;32:649–654. doi: 10.1097/01.ccm.0000115636.29294.2f. [DOI] [PubMed] [Google Scholar]
- 14.Schonwetter RS, Walker RM, Solomon M, Indurkhya A, Robinson BE. Life values, resuscitation preferences, and applicability of living wills in an older population. J Am Geriatr Soc. 1996;44:954–958. doi: 10.1111/j.1532-5415.1996.tb01867.x. [DOI] [PubMed] [Google Scholar]
- 15.Carlsen MS, Pomeroy C, Moldow DG. Optimizing discussions about resuscitation: development of a guide based on patients’ recommendations. J Clin Ethics. 1998;9:263–272. [PubMed] [Google Scholar]
- 16.Degenholtz HB, Thomas SB, Miller MJ. Race and the intensive care unit: disparities and preferences for end-of-life care. Crit Care Med. 2003;31:S373–S378. doi: 10.1097/01.CCM.0000065121.62144.0D. [DOI] [PubMed] [Google Scholar]
- 17.Kwak J, Haley WE. Current research findings on end-of-life decision making among racially or ethnically diverse groups. Gerontology. 2005;45:634–641. doi: 10.1093/geront/45.5.634. [DOI] [PubMed] [Google Scholar]
- 18.Knaus W, Wagner D, Draper EA, et al. The APACHE III prognostic system: risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100(6):1619–1636. doi: 10.1378/chest.100.6.1619. [DOI] [PubMed] [Google Scholar]
- 19.Ware J, Kosinski M, Dewey J, Gandek B. How to Score and Interpret Single-Item Health Status Measures: A Manual for Users of the SF-8 Health Survey. Lincoln, RI: Quality Metric; 2001. [Google Scholar]
- 20.Katzman R, Brown T, Fuld P, Peck A, Schechter R, Schimmel H. Validation of a short orientation-memory-concentration test of cognitive impairment. Am J Psychiatry. 1983;140(6):734–739. doi: 10.1176/ajp.140.6.734. [DOI] [PubMed] [Google Scholar]
- 21.Fumis RR, Nishimoto IN, Deheinzelin D. Families’ interactions with physicians in the intensive care unit; the impact on family’s satisfaction. J Crit Care. 2008;23(3):281–286. doi: 10.1016/j.jcrc.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 22.Wade DT, Vergis E. The Short Orientation-Memory-Concentration Test: a study of its reliability and validity. Clin Rehab. 1999;13:164–170. doi: 10.1191/026921599673848768. [DOI] [PubMed] [Google Scholar]
- 23.Goring H, Baldwin R, Marriott A, Pratt H, Roberts C. Validation of short screening tests for depression and cognitive impairment in older medically ill in-patients. Int J Geriatr Psychiatry. 2004;19(5):465–471. doi: 10.1002/gps.1115. [DOI] [PubMed] [Google Scholar]
- 24.Nelson LM, Longstreth WT, Koepsell TD, Checkoway H, van Belle G. Completeness and accuracy of interview data from proxy respondents: demographic, medical, and life-style factors. Epidemiology. 1994;5(2):204–217. doi: 10.1097/00001648-199403000-00011. [DOI] [PubMed] [Google Scholar]
- 25.Curtis JR. The long-term outcomes of mechanical ventilation: What are they and how should they be used? Respir Care. 2002;47:496–505. [PubMed] [Google Scholar]
- 26.Nelson JE. Palliative care of the chronically critically ill patient. Crit Care Clin. 2002;18:659–681. doi: 10.1016/s0749-0704(02)00004-0. [DOI] [PubMed] [Google Scholar]
- 27.Lilly CM, DeMeo DL, Sonna LA, et al. An intensive communication intervention for the critically ill. Am J Med. 2000;109:469–475. doi: 10.1016/s0002-9343(00)00524-6. [DOI] [PubMed] [Google Scholar]