Abstract
Objectives
To characterize the interaction of 1-Ethyl-3-[3-dimethylaminopropyl] carbodiimide Hydrochloride (EDC) with dentin matrix and its effect on the resin-dentin bond.
Methods
Changes to the stiffness of demineralized dentin fragments treated with EDC/N-hydroxysuccinimide (NHS) in different solutions were evaluated at different time points. The resistance against enzymatic degradation was indirectly evaluated by ultimate tensile strength (UTS) test of demineralized dentin treated or not with EDC/NHS and subjected to collagenase digestion. Short- and long-term evaluations of the strength of resin-dentin interfaces treated with EDC/NHS for 1 hour were performed using microtensile bond strength (µTBS) test. All data (MPa) were individually analyzed using ANOVA and Tukey HSD tests (α=0.05).
Results
The different exposure times significantly increased the stiffness of dentin (p<0.0001, control - 5.15 and EDC/NHS - 29.50), while no differences were observed among the different solutions of EDC/NHS (p=0.063). Collagenase challenge did not affect the UTS values of EDC/NHS group (6.08) (p>0.05), while complete degradation was observed for the control group (p=0.0008, control - 20.84 and EDC/NHS - 43.15). EDC/NHS treatment did not significantly increase resin-dentin µTBS, but the values remained stable after 12 months water storage (p<0.05).
Conclusions
Biomimetic use of EDC/NHS to induce exogenous collagen cross-links resulted in increased mechanical properties and stability of dentin matrix and dentin-resin interfaces.
Keywords: collagen, dentin, carbodiimide, biomimetic, mechanical properties, degradation
Introduction
Carbodiimide (1-Ethyl-3-[3-dimethylaminopropyl] carbodiimide Hydrochloride, or EDC), the most stable cyanamide isomer, is able to assemble amino acids into peptides. Its mechanism of collagen cross-linking involves the activation of the carboxylic acid groups of glutamic and aspartic acid residues by EDC to give O-acylisourea groups. Cross-links are formed after nucleophilic attack by free amino groups of lysine or hydroxylysine residues (1). The addition of N-hydroxysuccinimide (NHS) to the EDC-containing solution is very effective in increasing the number of cross-links introduced to a collagen matrix and prevents the hydrolysis of activated carboxyl groups (2,3). Increased resistance to collagenase challenge and mechanical properties of collagen-based materials have been reported following treatment with EDC (4,5). EDC presents very low cytotoxicity when compared to glutaraldehyde as the urea derivative released when the cross-link is generated is easily rinsed from the collagen, leaving no residual chemicals (6).
As the major component of the organic matrix of dentin, fibrillar type I collagen provides the tissue with viscoelasticity forming a rigid, strong space-filling biomaterial (7,8,9). The presence of native inter- and intra-molecular cross-links provides the basis for the stability and strength of the collagen fibrils. Cross-linking chemistry is controlled by a number of factors such as the extent of lysine hydroxylation, glycosylation, turnover rate, molecular packing and external forces (10). Type I collagen plays a major role on the restoration of missing tooth structure as the tooth component that provides micromechanical retention of resin-based materials. Biomodification of the collagen, mostly by changes in the amount of cross-links, provide the collagen matrix with enhanced mechanical properties and lower rates of enzymatic degradation. While several studies have investigated the use of collagen cross-linkers to provide temporary reinforcement for tissue regeneration (11,12,13), the dental application of such cross-linkers may involve their long term ability to improve the stability of the collagen. Previous studies have reported that other collagen cross-linkers such as glutaraldehyde and proanthocyanidin rich materials have the ability to improve the short-term mechanical properties of dentin (14) and the resin-dentin interface (15,16). In lieu of the current knowledge of tissue engineering, biomimetic exploitation of the tissue structure itself can provide important insights into the restorative/reparative treatment of dentin. The purpose of this study was to characterize the short and long-term effects of EDC/NHS-dentin matrix complex on the biomechanical properties of dentin matrix and dentin-resin bonded interfaces. The test null hypotheses were that EDC treatment has no effect on dentin matrix stiffness, resistance against collagenase challenge or the durability of resin-dentin bonds.
Materials and Methods
Materials
Forty human molars were used under a protocol approved by the Institutional Review Board committee from the University of Illinois at Chicago (protocol #2006-0229). The following agents were used in this study : Water-soluble 1-ethyl-3-[3-dimethylaminopropyl]carbodiimide hydrochloride – EDC (ThermoScientifc Pierce, RockFord, IL, USA), N-Hydroxysuccinimide - NHS (ThermoScientifc Pierce), 2-(N-morpholino) ethanesulfonic acid – MES (Acros Organics, New Jersey, USA) and bacterial collagenase from Clostridium histolyticum - type I, ≥125 CDU/mg solid (Sigma-Aldrich, St. Louis, MO, USA).
Mechanical properties of demineralized dentin
Thick disks (1.7 ± 0.1mm) from middle coronal dentin were obtained by sectioning the occlusal and cervical portion of the crown using a diamond wafering blade (Buehler-Series 15LC Diamond, Buehler, Lake Bluff, IL, USA). The disks were then sectioned into 0.5 ± 0.1 mm thick beams (n = 5 beams per tooth) along the long axis of the tooth and further trimmed using a cylindrical diamond bur (#557D, Brasseler, Savannah, GA, USA) to a final rectangular dimension of 0.5 mm thickness × 1.7 mm width × 6.5 mm length (14). A dimple was made at one end of the surfaces to allow for repeated measurements to be performed on the same surface. Samples were fully demineralized using 10% phosphoric acid solution (LabChem Inc, Pittsburgh, PA, USA) for 5 hours, and complete demineralization was verified by x-ray. Demineralized specimens were treated with 0.3 M EDC/0.12 M NHS prepared in 3 different solutions (experimental groups): distilled water, 12% ethanol or 50 mM MES buffer, adjusted to pH 7.4. In the presence of NHS, EDC can be used to convert carboxyl groups to more stable amine-reactive sulfo-NHS esters, thus increasing the efficiency of EDC-mediated reactions (17). Chemical structures are shown in Figure 1. Dentin specimens were immersed in water for baseline measurements and then in their respective three EDC/NHS solutions for 10 min, 30 min, 1 hr, 2 hr and 4 hr of cumulative exposure time. The long-term effect was further assessed for the same samples after 12 months distilled water storage in incubator at 37°C. A schematic of the study design is shown in Figure 2.
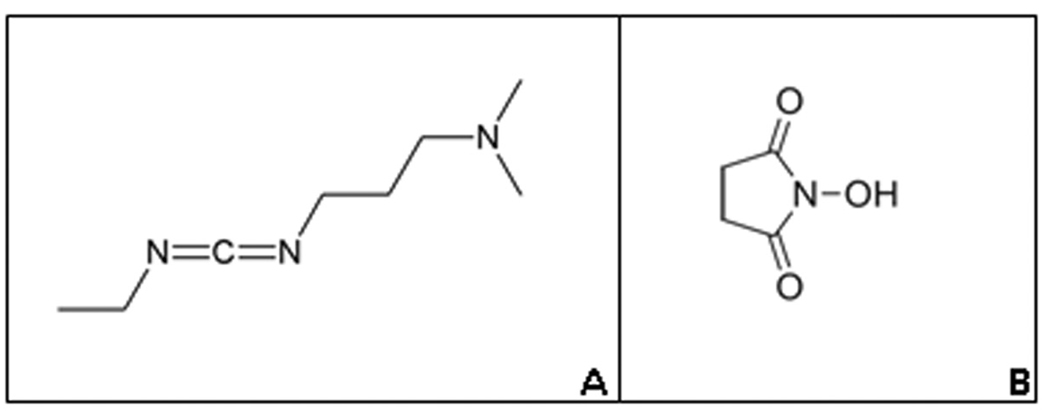
Figure 1.
Chemical structure of (A) 1-ethyl-3-[3-dimethylaminopropyl]carbodiimide hydrochloride (EDC) and (B) N-Hydroxysuccinimide (NHS).
Figure 2.
Schematic of the study design. The results of the micro-flexural test guided the dentin treatment for the following assays.
An aluminum alloy fixture with a 2.5 mm span between two 1-mm thick round edge supports was glued to the bottom of a glass Petri dish. Specimens were tested in compression while immersed in distilled water using a testing machine (EZ Graph, Shimadzu Co., Kyoto, Japan), with a 100 grams load cell at crosshead speed of 0.5 mm/min. Load-displacement curves were converted to stress-strain curves and the apparent modulus of elasticity calculated at 3% strain (14).
The data were statistically analyzed using General Linear Model SPSS program for ANOVA for repeated measurement and post-hoc Tukey HSD tests to evaluate different exposure time and also to assess the effect of long-term water storage (immediate 4 hr treatment and 12 month storage).
Resistance against enzymatic degradation
Dentin beams with dimensions of 0.5 mm × 1.7 mm × 6.5 mm were prepared into hour-glass shaped samples with a neck area of 0.5 ± 0.1 mm × 0.5 ± 0.1 mm at middle dentin using a cylindrical diamond bur (#557D, Brasseler, Savannah, GA, USA). Samples were prepared with dentinal tubules oriented perpendicular to the tensile force. The extremities of the beams were coated with 2 layers of cosmetic nail varnish to protect against demineralization (18). The exposed dentin was fully demineralized using 10% phosphoric acid solution (LabChem, Inc.) for 5 hours. Based on the findings of the mechanical properties of EDC/NHS treated dentin (experiment above), samples were further tested using MES buffer. Samples (n=24) were either kept in distilled water (control) or treated with EDC/NHS/MES for 1 hour, thoroughly rinsed and either subjected to enzymatic challenge for 24 hours in 0.2 M ammonium bicarbonate buffer (pH = 7.5) or left in 24 hours in the same buffer with bacterial collagenase (100 ug/ml). Following thorough rinsing (30 minutes), the specimens were glued with a cyanoacrylate adhesive (Zapit - Dental Ventures of America Inc., Corona, CA, USA) to a jig for ultimate tensile strength (UTS) evaluation, which was mounted on a microtensile tester machine (Bisco, Schaumburg, IL, USA) and tested at a crosshead speed of 1 mm/min. The data were statistically analyzed using 2-way ANOVA and post-hoc Tukey HSD tests at a 95% confidence interval.
Resin-dentin mechanical properties - Microtensile bond strength test (µTBS)
The occlusal surfaces of 30 molars were ground flat with #180 and 320 grit to remove enamel, and 600 grit silicon carbide paper (Buehler Ltd, Lake Bluff, IL, USA) under running water to expose mid-coronal dentin. The dentin surfaces were randomly divided into two groups: EDC/NHS/MES (same preparation and concentration described above) and no treatment (distilled water). Each group was then subdivided according to the bonding systems employed, Adper Single Bond Plus - SB (3M ESPE, St Paul, MN, USA) or One Step Plus - OS (Bisco, Schaumburg, Il, USA). Dentin was etched with the respective bonding system etchants and then treated for 1 hour. After one hour, samples were thoroughly rinsed for 4 minutes and bonding procedures were resumed following the manufacturers’ instructions. Filtek Supreme (3M ESPE) resin composite was used to incrementally build a 5 mm crown and specimens were stored in distilled water at 37°C for 24 h.
The bonded samples were then sectioned into 0.8 ± 0.1 by 0.8 ± 0.1 mm thick beams, glued with a cyanoacrylate adhesive (Zapit, Dental Ventures of America Inc, Corona, CA, USA) to a jig, which was mounted on a microtensile tester machine (Bisco) and subjected to tensile forces at a crosshead speed of 1 mm/min. Statistical analysis was performed for each adhesive system using 2-way ANOVA and post-hoc Tukey HSD tests at a 95% confidence interval.
Results
The modulus of elasticity of EDC/NHS-treated dentin matrices are listed on Table 1. No statistically significant interaction was observed between the two factors (treatment vs. time, p= 0.984). EDC/NHS treatment increased the modulus of elasticity (E) of dentin (p < 0.0001) regardless of the media (p= 0.063). In addition, statistically significant (p = 0.004) lower E values were observed between immediate and 12 months water storage of all EDC/NHS treated samples. Even though an average 16.7% decrease was observed after 12 months storage they were almost 5-fold higher than initial baseline (no treatment). There were no differences between the cross-linker groups after 12 month storage (p = 0.967).
Table 1.
Modulus of elasticity [mean (standard deviation)] of dentin matrix after treatment with EDC/NHS in different media.
| Modulus of elasticity (MPa) | |||||||
|---|---|---|---|---|---|---|---|
| treatment | Exposure Time | 12 months DW storage |
|||||
| baseline | 10min | 30min | 1h | 2h | 4h | ||
| EDC/DW | 5.37 e (1.26) |
13.81 d (3.22) |
20.42 c (4.75) |
24.02 cb (5.56) |
26.76 ba (5.71) |
28.87 a (6.56) |
24.12 a,A (5.31) |
| EDC/ETH | 5.14 e (1.65) |
16.73 d (3.01) |
23.76 c (3.54) |
27.18 cb (3.90) |
28.77 ba (5.44) |
29.50 a (4.85) |
24.52 a,A (4.86) |
| EDC/MES | 5.21 e (1.77) |
14.10 d (4.17) |
20.56 c (5.83) |
24.23 cb (7.20) |
27.46 ba (8.35) |
29.15 a (8.89) |
24.26 a,A (7.50) |
Different lower case letters indicate statistically significant differences in each row (p < 0.05).
Same upper case letters indicate no statistically significant differences between 12 month stored groups (p > 0.05).
EDC: Carbodiimide; NHS: N-Hydroxysuccinimide; DW: Distilled water; ETH: 12% ethanol; MES: 2-(N-morpholino)ethanesulfonic acid.
The UTS values of dentin were significantly affected by the treatment (p = 0.0189) and collagenase challenge (p = 0.0008). EDC/NHS treatment did not affect the UTS when samples were kept only in buffer without collagenase. When specimens were incubated with bacterial collagenase for 24 h, the UTS of the untreated controls fell to zero, while the UTS values of the EDC/NHS-treated specimens were not significantly different from the untreated specimens incubated in buffer without collagenase (Table 2).
Table 2.
Indirect assessment of collagen stability using ultimate tensile strength [mean (standard deviation)] following enzymatic degradation.
| Ultimate tensile strength (MPa) | ||
|---|---|---|
| Enzymatic degradation |
Dentin Matrix treatment | |
| Control (MES) | EDC/NHS/MES | |
| Buffer | 7.34 (5.16)a | 6.25 (1.92)a |
| Collagenase/Buffer | 0 (0) | 6.08 (2.59)a |
Same letters indicate no statistically significant differences between groups (p < 0.05).
EDC: Carbodiimide; NHS: N-Hydroxysuccinimide; MES: 2-(N-morpholino)ethanesulfonic acid.
The resin-dentin bond strength data is depicted on Table 3. Two-way ANOVA revealed that there were statistically significant interaction between the factors evaluated (surface treatment vs. adhesive system) for OS groups (p = 0.034) and no significant interaction for SB groups (p = 0.451). The long term bond strength of OS was increased by EDC/NHS (p = 0.0001) but the treatment did not affect SB (p = 0.381) when compared to their respective control groups. Statistically significant decrease in the bond strength was observed after 12 months water storage for both SB groups, but the control group values yielded statistically significant lower bond strengths than EDC/NHS treated interfaces. EDC/NHS had a significant effect for all variables evaluated; therefore the null hypotheses were rejected for all the methods tested in the present study.
Table 3.
Micromechanical properties of the resin-dentin bonded treated interfaces using microtensile bond strength [mean (standard deviation)].
| Microtensile bond strength (MPa) | ||||
|---|---|---|---|---|
| 24 hours | 12 months | |||
| Control | EDC/NHS | Control | EDC/NHS | |
| One Step Plus |
41.61 (13.24)a | 46.85 (13.24)a | 20.84 (11.97) b | 43.15 (14.16) a |
| Adper Single Bond |
51.72 (17.71)A | 52.37 (11.39)A | 26.63 (13.42) C | 39.44 (17.24) B |
Lower and upper case letters indicate statistically significant differences (p < 0.05) among One Step Plus and Adper Single Bond groups, respectively.
EDC: Carbodiimide; NHS: N-Hydroxysuccinimide.
Discussion
Bio-inspired materials and techniques have been the focus of several studies due to their ability to mimic natural processes. EDC has been used as a collagen cross-linker with a unique capacity to activate carboxylic acid groups in collagen (19). In the present study EDC/NHS was explored as a long-term biomimetic tool to enhance biomechanical interfaces that do not undergo remodeling. The repair of lost tooth structure is challenging since dentin does not have the same ability to regenerate/repair as bone. Despite the fact that current dentin reparative alternatives rely on the use of a resin-based material that can micromechanically interface with the tooth, modification of the remaining tooth structure may provide new insights to the current restorative mechanism or may provide alternative regenerative/reparative concepts for the restoration of missing tooth structure. In the present study increased biomechanical properties were observed for EDC/NHS treated dentin matrix that enhanced the long-term stability of EDC/NHS treated resin-dentin interfaces.
We have observed that regardless of the media in which EDC/NHS was delivered, the modulus of elasticity of dentin significantly increased when compared to baseline values. Different media were tested as they may affect the dentin matrix itself and/or the EDC/NHS-dentin matrix interaction. The cross-linked activity reached a plateau after 1–2 hours exposure time, which may indicate that there are limited amount of carboxyl groups on the tissue for interaction and/or the presence of reaction sites of molecule that are not linkable by EDC/NHS. Glutaraldehyde has the ability to cross-link type I collagen using a distinct mechanism in which aldehyde functional groups reacts with amino groups of lysil or hydroxylysyl residues (20,21). Condensed tannins have far more mechanisms to interact with type I collagen and can result in significantly increased mechanical properties (15,22). While higher mechanical properties are desirable, durability of the induced exogenous cross-links may be of more relevance than its short term effect. The EDC/NHS treatment did not result in stiffness values as high as those reported for other agents (14,16), however a remarkable stability of the stiffness was observed after one year water storage with an approximate 16% decrease on stiffness values. The high values after 1 year of storage may indicate that stable bonds such as covalent interactions were induced by EDC/NHS.
While the media did not affect the stiffness values, further experiments were conducted using MES buffer, due to the higher stability of EDC/NHS. Remarkable stability of the dentin matrix after EDC/NHS treatment was indirectly characterized using a UTS assay following matrix exposure to collagenase. Since residues of EDC are not present after the reaction takes place (6), it can be hypothesized that the increased stability noted was mainly due to a protective mechanism of EDC/NHS to dentin matrix. Diminished cleavage sites as well as impaired collagenase adsorption (23) through the matrix may account for the results. It is important to note that bacterial collagenase is a very potent protease and therefore it may be expected that the EDC/NHS-treated matrix will be protected against proteases commonly present in the oral environment, (24) saliva, and dentin (25), and that may be involved in the resin-bond degradation (25,26). Further investigation should be performed to confirm its protective mechanism against other proteases.
Increased modulus of elasticity of dentin matrix may result in increased resin-dentin bond strength (14,16). We believe that the 6-fold increase in the dentin stiffness was not significant enough to increase the short-term microtensile bond strength as observed for other collagen cross-linkers (14,16). On the other hand, the long term maintenance of the modulus of elasticity values may partially correlate with the long term stability of the bond strength. Hydrolytic degradation of both resin components and collagen is believed to affect the durability of resin-dentin bonds (27). The bond strength remained stable after 12 month storage for EDC/NHS treated interfaces restored with One Step Plus when compared to an un-treated control group. Decreased bond strength was observed for Adper Single Bond Plus regardless of the treatment, however control group values were statistically lower than EDC/NHS-treated group. The presence of exogenous cross-links induced by EDC/NHS may be a key contributor for the stability of the dentin bond strength values by enhanced mechanical properties and/or resistance to enzymatic degradation.
The degradation of the resin component seems to be somewhat unavoidable (28,29) and could not be controlled in this experiment. The differences in the behavior of both bonding systems may be related to their compositions such as type of solvent. Single Bond Plus is a water-ethanol solvent-based system and One Step Plus is an acetone-based system. Both primarily bond micromechanically to the tooth structure through the formation of a hybrid layer. Water movement through the resin-dentin interface has been reported for etch-and-rinse bonding systems (30) and it is material-dependant (31). Increased permeability indicates increased presence of water movement at the interface (32), which may increase plasticization of the resin and degradation of resin bonds. Increased silver penetration and the presence of silver deposits in the resin layer after long term water storage of water/ethanol systems is a distinct pattern of degradation that is not observed in acetone-based systems (33). Hence, the polyalkenoic acid co-polymer component of Adper Single Bond can increase permeability of the resin layer (33). The resin layer is collagen free and therefore cannot be affected by the EDC/NHS treatment. Weakening of the resin layer may have affected the bond strength values of Adper Single Bond by changing the debonding pattern. Therefore treatment with EDC/NHS resulted in increased biomechanical properties of dentin bonded interfaces, but degradation of the resin components plays an important role in the degradation process. The effectiveness of the treatment to the overall quality of the interface may be material-dependant.
The present data indicates that EDC/NHS treatment has great potential to enhance the stability of the interface, most likely due to increased mechanical properties of the dentin matrix and slower degradation rates of collagen. The effect of EDC/NHS seems to be sustained after 12 months, but its effectiveness significantly decreased overtime. The 1 hour treatment time is clinically impractical and was employed as a proof-of-concept to determine the potential use of EDC/NHS as dentin matrix biomodifiers for restorative application. Future studies will investigate shorter application times and the use of controlled drug-delivery systems to recharge the collagen at the interface over time and promote preservation and self-healing of the interface.
ACKNOWLEDGMENT
This investigation was supported by Research Grant DE017740 from the National Institute of Dental and Craniofacial Research, National Institutes of Health, Bethesda, MD 20892.
References
- 1.Timkovich R. Detection of the stable addition of carbodiimide to proteins. Anal Biochem. 1977;79:135–143. doi: 10.1016/0003-2697(77)90387-6. [DOI] [PubMed] [Google Scholar]
- 2.Olde Damink LH, Dijkstra PJ, van Luyn MJ, van Wachem PB, Nieuwenhuis P, Feijen J. In vitro degradation of dermal sheep collagen cross-linked using a water-soluble carbodiimide. Biomaterials. 1996;17:679–684. doi: 10.1016/0142-9612(96)86737-8. [DOI] [PubMed] [Google Scholar]
- 3.Staros JV, Wright RW, Swingle DM. Enhancement by N-hydroxysulfosuccinimide of water-soluble carbodiimide-mediated coupling reactions. Anal Biochem. 1986;156:220–222. doi: 10.1016/0003-2697(86)90176-4. [DOI] [PubMed] [Google Scholar]
- 4.Caruso AB, Dunn MG. Functional evaluation of collagen fiber scaffolds for ACL reconstruction: cyclic loading in proteolytic enzyme solutions. J Biomed Mater Res A. 2004;69:164–171. doi: 10.1002/jbm.a.20136. [DOI] [PubMed] [Google Scholar]
- 5.Powell HM, Boyce ST. EDC cross-linking improves skin substitute strength and stability. Biomaterials. 2006;27:5821–5827. doi: 10.1016/j.biomaterials.2006.07.030. [DOI] [PubMed] [Google Scholar]
- 6.Khor E. Methods for the treatment of collagenous tissues for bioprostheses. Biomaterials. 1997;18:95–105. doi: 10.1016/s0142-9612(96)00106-8. [DOI] [PubMed] [Google Scholar]
- 7.Butler WT. Dentin matrix proteins and dentinogenesis. Connect Tissue Res. 1995;33:59–65. doi: 10.3109/03008209509016983. [DOI] [PubMed] [Google Scholar]
- 8.Scott JE. Extracellular matrix, supramolecular organisation and shape. J Anat. 1995;187:259–269. [PMC free article] [PubMed] [Google Scholar]
- 9.Cheng H, Caterson B, Neame PJ, Lester GE, Yamauchi M. Differential distribution of lumican and fibromodulin in tooth cementum. Connect Tissue Res. 1996;34:87–96. doi: 10.3109/03008209609021494. [DOI] [PubMed] [Google Scholar]
- 10.Yamauchi M. Collagen Biochemistry: An Overview. In: Phillips GO, editor. Advances in Tissue Banking. Vol. 6. New Jersey: World Scientific Publishing Co.; 2000. pp. 455–500. [Google Scholar]
- 11.Zeugolis DI, Paul GR, Attenburrow G. Cross-linking of extruded collagen fibers--a biomimetic three-dimensional scaffold for tissue engineering applications. J Biomed Mater Res A. 2009;89:895–908. doi: 10.1002/jbm.a.32031. [DOI] [PubMed] [Google Scholar]
- 12.Kasyanov V, Isenburg J, Draughn RA, Hazard S, Hodde J, Ozolanta I, Murovska M, Halkes SB, Vrasidas I, Liskamp RM, Pieters RJ, Simionescu D, Markwald RR, Mironov V. Tannic acid mimicking dendrimers as small intestine submucosa stabilizing nanomordants. Biomaterials. 2006;27:745–751. doi: 10.1016/j.biomaterials.2005.06.022. [DOI] [PubMed] [Google Scholar]
- 13.Mi FL, Tan YC, Liang HF, Sung HW. In vivo biocompatibility and degradability of a novel injectable-chitosan-based implant. Biomaterials. 2002;23:181–191. doi: 10.1016/s0142-9612(01)00094-1. [DOI] [PubMed] [Google Scholar]
- 14.Bedran-Russo AK, Pashley DH, Agee K, Drummond JL, Miescke KJ. Changes in stiffness of demineralized dentin following application of collagen cross-linkers. J Biomed Mater Res B Appl Biomater. 2008;86:330–334. doi: 10.1002/jbm.b.31022. [DOI] [PubMed] [Google Scholar]
- 15.Al-Ammar A, Drummond JL, Bedran-Russo AK. The use of collagen cross-linking agents to enhance dentin bond strength. J Biomed Mater Res B Appl Biomater. 2009 Jun 8; doi: 10.1002/jbm.b.31417. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bedran-Russo AK, Yoo K, Ema K, Pashley DH. Mechanical properties of tannic acid-treated dentin matrix. J Dent Res. 2009 doi: 10.1177/0022034509342556. [in press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grabarek Z, Gergely J. Zero-length crosslinking procedure with the use of active esters. Anal Biochem. 1990;185:131–135. doi: 10.1016/0003-2697(90)90267-d. [DOI] [PubMed] [Google Scholar]
- 18.Sano H, Ciucchi B, Matthews WG, Pashley DH. Tensile properties of mineralized and demineralized human and bovine dentin. J Dent Res. 1994;73:1205–1211. doi: 10.1177/00220345940730061201. [DOI] [PubMed] [Google Scholar]
- 19.Zeeman R, Dijkstra PJ, van Wachem PB, van Luyn MJ, Hendriks M, Cahalan PT, Feijen J. Successive epoxy and carbodiimide cross-linking of dermal sheep collagen. Biomaterials. 1999;20:921–931. doi: 10.1016/s0142-9612(98)00242-7. [DOI] [PubMed] [Google Scholar]
- 20.Sung HW, Chang Y, Chiu CT, Chen CN, Liang HC. Mechanical properties of a porcine aortic valve fixed with a naturally occurring crosslinking agent. Biomaterials. 1999;20:1759–1772. doi: 10.1016/s0142-9612(99)00069-1. [DOI] [PubMed] [Google Scholar]
- 21.Ritter AV, Swift EJ, Jr, Yamauchi M. Effects of phosphoric acid and glutaraldehyde-HEMA on dentin collagen. Eur J Oral Sci. 2001;109:348–353. doi: 10.1034/j.1600-0722.2001.00088.x. [DOI] [PubMed] [Google Scholar]
- 22.Han B, Jaurequi J, Tang BW, Nimni ME. Proanthocyanidin: a natural crosslinking reagent for stabilizing collagen matrices. J Biomed Mater Res. 2003;65A:118–124. doi: 10.1002/jbm.a.10460. [DOI] [PubMed] [Google Scholar]
- 23.Nam K, Kimura T, Kishida A. Physical and biological properties of collagen-phospholipids polymer hybrid gels. Biomaterials. 2007;28:3153–3162. doi: 10.1016/j.biomaterials.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 24.Hannas AR, Pereira JC, Granjeiro JM, Tjäderhane L. The role of matrix metalloproteinases in the oral environment. Acta Odontol Scand. 2007;65:1–13. doi: 10.1080/00016350600963640. [DOI] [PubMed] [Google Scholar]
- 25.Mazzoni A, Pashley DH, Nishitani Y, Breschi L, Mannello F, Tjäderhane L, Toledano M, Pashley EL, Tay FR. Reactivation of inactivated endogenous proteolytic activities in phosphoric acid-etched dentine by etch-and-rinse adhesives. Biomaterials. 2006;27:4470–4476. doi: 10.1016/j.biomaterials.2006.01.040. [DOI] [PubMed] [Google Scholar]
- 26.Hebling J, Pashley DH, Tjäderhane L, Tay FR. Chlorhexidine arrests subclinical degradation of dentin hybrid layers in vivo. J Dent Res. 2005;84:741–746. doi: 10.1177/154405910508400811. [DOI] [PubMed] [Google Scholar]
- 27.Hashimoto M, Ohno H, Sano H, Tay FR, Kaga M, Kudou Y, Oguchi H, Araki Y, Kubota M. Micromorphological changes in resin-dentin bonds after 1 year of water storage. J Biomed Mater Res. 2002;63:306–311. doi: 10.1002/jbm.10208. [DOI] [PubMed] [Google Scholar]
- 28.Osorio R, Pisani-Proenca J, Erhardt MC, Osorio E, Aguilera FS, Tay FR, Toledano M. Resistance of ten contemporary adhesives to resin-dentine bond degradation. J Dent. 2008;36:163–169. doi: 10.1016/j.jdent.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 29.Breschi L, Mazzoni A, Ruggeri A, Cadenaro M, Di Lenarda R, De Stefano Dorigo E. Dental adhesion review: aging and stability of the bonded interface. Dent Mater. 2008;24:90–101. doi: 10.1016/j.dental.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 30.Hashimoto M, Tay FR, Sano H, Kaga M, Pashley DH. Diffusion-induced water movement within resin-dentin bonds during bonding. J Biomed Mater Res B Appl Biomater. 2006;79:453–458. doi: 10.1002/jbm.b.30562. [DOI] [PubMed] [Google Scholar]
- 31.Hashimoto M, Ohno H, Kaga M, Endo K, Sano H, Oguchi H. Resin-tooth adhesive interfaces after long-term function. Am J Dent. 2001;14:211–215. [PubMed] [Google Scholar]
- 32.Hashimoto M, Ito S, Tay FR, Svizero NR, Sano H, Kaga M, Pashley DH. Fluid movement across the resin-dentin interface during and after bonding. J Dent Res. 2004;83:843–848. doi: 10.1177/154405910408301104. [DOI] [PubMed] [Google Scholar]
- 33.Reis AF, Giannini M, Pereira PN. Long-term TEM analysis of the nanoleakage patterns in resin-dentin interfaces produced by different bonding strategies. Dent Mater. 2007;23:1164–1172. doi: 10.1016/j.dental.2006.10.006. [DOI] [PubMed] [Google Scholar]