SYNOPSIS
Effects of place or neighborhood—locations where individuals reside, shop, recreate, and work—have been widely studied as sources of environmental influences on individual behaviors, exposures, and physiology, as well as reference points for public health interventions. However, despite modern prisons' strong influence on the transmission and clinical outcomes of infectious diseases, custodial authorities and public health officials in many countries have yet to implement credible interventions to minimize the adverse impacts prison settings exert on the epidemiology of communicable diseases—particularly with respect to inmates. Among many vulnerable populations, prisons are evolving as one of the social institutions that determine their health status and health outcomes. This article highlights the effects of prisons in mediating the risk of hepatitis C virus and tuberculosis infections, as well as feasible interventions and policy approaches for limiting the deleterious consequences prisons exert on the transmission and clinical courses of these diseases.
The commonly agreed manifest functions of prisons are reformation, incapacitation, retribution, and deterrence.1 Jeremy Bentham pioneered the modern prison philosophy of incarceration and ocular surveillance (i.e., omnipresent, all-seeing custodial authorities) as a component of punishment, thus extending the use of prisons beyond that of a holding state until corporal or capital punishment is inflicted.2 In Discipline and Punish, Michel Foucault describes modern prisons as social institutions designed to sequester torture from public view while simultaneously inflicting cruel and unusual punishment on the body and soul of incarcerated individuals.3 From the early 20th century onward, the role of prisons has evolved from the periphery to the center of social policy. The Gulag system of the former Soviet Union exemplified this evolution during the first half of the 20th century, in which prisons facilitated social control and served as torture centers and sources of cheap labor.4
In the past several decades, major transformations of prisons as core social-policy instruments have been occurring in the U.S., where the number of inmates rose dramatically from 560,000 in 1978 to 2.3 million in 2008.5 Wacquant viewed mass incarceration in the U.S. as evolving from previous social institutions—slavery, Jim Crow laws, and ghettos—for the discipline and control of the underclass.6 Authoritarian rule in China since Mao's revolution facilitated the exponential growth of China's prison population to at least 1.6 million as of 2007—a substantial contribution to the nine million incarcerated individuals in the world.7
As places or neighborhoods in which individuals are physically confined and deprived of a range of personal freedoms, prisons have been shown to operate as structural factors that may influence health status and outcomes independently of individual-level attributes.8 Three empiric strategies are commonly utilized to investigate neighborhoods' effects on health—ecologic studies, multilevel studies, and comparisons of small numbers of well-defined neighborhoods. Ideally, the impacts of prison neighborhoods on health should be analyzed in relation to upstream social determinants of health (SDH) in the larger society,9,10 in view of the close links between prison settings and surrounding communities, as well as the fact that more than 95% of inmates will eventually reenter the general community.
Prison settings are commonly associated with high risk of infectious diseases.11,12 Such increased risks are attributable to both the likelihood of a high proportion of people with infectious diseases coming in contact with the criminal justice system and the increased risk of infectious disease transmission in prison settings.13–16 This article explores the roles of prisons as SDH, as well as prisons' mediating influence on the transmission and clinical course of hepatitis C virus (HCV) and tuberculosis (TB) infections. It also proposes policy approaches for reducing the adverse impact of prisons on morbidity and mortality from infectious diseases.
PRISONS AS SOCIAL DETERMINANTS OF HEALTH
Raphael17 defines SDH as “the economic and social conditions that shape the health of individuals, communities, and jurisdictions as a whole. [SDH] are the primary determinants of whether individuals stay healthy or become ill (a narrow definition of health). [SDH] also determine the extent to which a person possesses the physical, social, and personal resources to identify and achieve personal aspirations, satisfy needs, and cope with the environment (a broader definition of health). [SDH] are about the quantity and quality of a variety of resources that a society makes available to its members.” The Public Health Agency of Canada lists nine SDH: income, employment and working conditions, food security, environment and housing, early childhood development, education and literacy, social support and connectedness, health behaviors, and access to health care.18
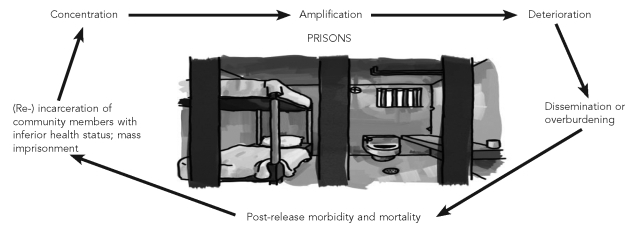
Although several recent articles have highlighted prisons as social or structural determinants of health,15,19 limited information currently exists on how prisons socially or structurally influence the health status and outcomes of the incarcerated. This article posits that prisons serve as SDH by mediating the vicious cycle of concentration, amplification, deterioration, dissemination or overburdening, and post-release morbidity and mortality (Figure).
Figure.
Conceptual framework of the central role of prisons in concentrating, amplifying, and disseminating infectious diseases among individuals in contact with the criminal justice system
Individuals with inferior health status are overrepresented among those in contact with the criminal justice system.15,19 Prisons serve as a concentration mechanism for relatively unhealthy individuals, partly because the behavioral and structural factors that lead to poor health (e.g., illicit drug use and alcoholism) are also associated with increased likelihood of incarceration. This nexus is exemplified by a 2007 national prison entrants' survey in Australia, which revealed that 35% of 740 consecutive prison entrants were HCV-antibody positive. The documented prevalence of hepatitis C and illicit drug use among the prison entrants studied was about 40 times the HCV-antibody prevalence in the Australian general community.16
Prisons amplify adverse health conditions through a culture that normalizes behaviors that are deleterious to health, such as tobacco use, injection drug use (IDU), and violence. The disease-amplification function of prisons is reflected in disproportionately high disease incidence and prevalence, which are documented in most inmate health surveys, and in reports of high rates of infectious-disease transmission in prisons.20–22 In most societies, prison settings exacerbate existing health conditions of inmates. Indeed, many inmates leave prisons less healthy, physically and mentally, compared with their health status at incarceration.21,22 Malnutrition, infectious diseases, overcrowding, austere custodial physical infrastructure, limited access to basic health services, and inhumane attitudes and practices of custodial officers toward inmates contribute to the deterioration of the physical and mental health status of individuals following incarceration.23–25 An extreme impact of deteriorating health conditions is the increasing number of deaths among inmates in custody—a phenomenon that is closely linked to inmates' deteriorating physical and mental health, coupled with limited access to basic health care.26,27
Dissemination of infectious diseases is another mechanism through which prisons serve as SDH. As more than 95% of incarcerated individuals eventually reenter the general community, amplification of infectious diseases during incarceration poses definite risks to the communities to which infected and untreated inmates return. Patients with chronic, non-communicable diseases also place an increased burden on the health system, as well as their friends and relatives.22,23,28 Increased mortality and morbidity of inmates following release from prison is another mechanism through which prisons serve as SDH. Studies have shown that inmates are at significantly high risk of suicide following release.29–31 Elevated inmate morbidity following release derives partly from the deterioration of their health status following incarceration and partly from limited opportunities for employment, social support deficiencies, and inadequate access to post-release health care. These factors perpetuate the vicious cycle that facilitates the re-incarceration of a large proportion of such individuals or their associates, due, for example, to drug-related crime, poor role models, poverty, and inadequate social support. In the U.S., approximately two out of every three people released from prisons are rearrested within three years of their release; more than 50% are re-incarcerated.32
At an ecological level, prisons as SDH operate through the phenomenon of mass imprisonment. Mass imprisonment implies not just rising numbers of inmates, but also the concentration of social and health effects of imprisonment on whole population subgroups, such as young, African American, and Aboriginal Australian males. In Australia, Aboriginal people constitute 2.5% of the general population but more than 22% of the prison population.33 In the U.S., mass imprisonment is emerging as a new stage in the life course of young, low-skilled African American people. For such disproportionately incarcerated groups, imprisonment becomes one of the social institutions that determines their health status and outcomes.34,35
PRISONS AND HCV INFECTION
HCV is a bloodborne pathogen that affects an estimated 130 million to 170 million people, or 2.2%–3.0% of the world's population. Current major risk factors for infection include IDU (more than 80% of infections) and other procedures requiring skin penetration, such as nonsterile injections, tattooing, and other body art.36 Chronic HCV infection is currently the most common indication for liver transplantation in industrialized nations.37,38 In the U.S., hepatitis C-related mortality overall increased by 123% from 1995 through 2004, with the most dramatic age-specific increase occurring among the economically productive age group of 45- to 54-year-olds.39
Socioeconomically vulnerable populations are overrepresented in American hepatitis C morbidity and mortality statistics.38–40 Global estimates indicate the cost of treating decompensated liver cirrhosis and liver transplantation (in the absence of antiviral treatment) is in the range of $24,000 to $39,000 (lifetime disease costs).36 A modeling study estimated the mean cost of achieving sustained virologic clearance for a hepatitis C patient in a U.S. correctional facility at $55,270,41 excluding costs of infection to the individual inmate, such as those related to social exclusion, depression, fatigue, and subclinical impairments in cerebral function, which are not easily quantifiable in monetary terms.42
Hepatitis C is known to be transmitted in prison settings, although probably not as frequently as in the general community of most industrialized nations. For example, reported seroconversions in Australian prisons ranged from 4.6 to 7.1 per 100 person-years,43,44 compared with 30.8 per 100 person-years in the Australian general community.45 Among inmates in Melbourne, Australia, in the early 1990s, the annual risk of HCV infection with repeat testing on reentry to prison was 18%; however, it was 41% among inmates younger than 30 years of age with reported IDU. It was difficult, however, to determine whether the studied cohort contracted the infection in prison or in the community.46 It is noteworthy that the apparent effectiveness of injecting-equipment prohibition policies in Australian prisons has not been replicated in other prison settings, such as in Ireland, where high rates of hepatitis C transmission in prison settings have been reported.47 Imprisonment, per se, is considered a major risk factor for HCV infection, with the risk of infection directly proportional to the length of incarceration.48,49
Prisons socially determine the transmission of HCV infection among inmates in several ways. First, a high proportion of inmates are addicted to illicit drugs that are injected, and some of the convicted illicit drug users manage to continue with their habit during incarceration.44,47 Health services for addiction management in most prisons are inadequate to cope with the demand for such treatments. Addicted inmates are less likely to benefit from health-education activities, such as counseling about drug abstinence, without parallel addiction-management interventions, such as methadone or buprenorphine maintenance treatment.50 Many drug-addicted inmates turn to tobacco and illicit drug use to satisfy their addictive cravings, as well as to numb the pains of imprisonment, famously classified by Sykes as deprivations of liberty, goods and services, heterosexual relationships, autonomy, and security.51
Second, as a high proportion of individuals in contact with the criminal justice system have already contracted hepatitis C prior to incarceration, prison settings magnify the probability of hepatitis C transmission among inmates who engage in IDU. For example, a 2004 survey of 612 Australian prison entrants indicated that 56% had a history of IDU and 39% had injected in the previous month.52 Of 81 inmates surveyed as part of a hepatitis C seroconversion study in New South Wales prisons, 29 (36%) gave a history of IDU, and 13 (16%) self-reported drug use in prison.44 Apart from IDU, other risk factors for hepatitis C transmission, such as assault, body piercings, tattooing, and unprotected anal sex with male injection drug users, are also commonly practiced by inmates.53–55
These risk factors are more common in custodial settings, primarily because of the structure and function of prisons. For example, limited access to harm-reduction interventions, such as needle- and syringe-exchange programs or condoms, makes it more likely that inmates will contract HCV infection. The finding that hepatitis C prevalence among custodial officers is higher compared with the general community53 suggests that prison environments may also mediate infection risks for prison workers—either directly, through occupational hazards associated with physical assaults, or through the stress of prison duties putting custodial workers at higher risk of engaging in activities such as illicit drug use, and consequently contracting HCV infection. However, proof of such a trajectory is lacking from systematic reviews.56
Third, custodial policies and practices influence the likelihood of inmates contracting HCV infection. Prisons with lax or poorly implemented policies in relation to illicit drug use make inmates more vulnerable to contracting HCV infection. Lax policies include weak surveillance of drug and injecting-equipment trafficking, and inadequate sanctions meted to inmates or custodial workers found to be involved with drug trafficking. A study in Australia in the 1990s indicated that about half of all imprisoned injection drug users injected drugs in prison, and non-random urine drug tests may reinforce and perpetuate the original reasons for drug use in prison.57
Custodial environments in which inmates are -tortured, not provided with productive outlets for their motivations, or not accorded basic human dignity are more likely to be characterized by inmates who develop ingenious or irrational ways to adapt to stressful prison regime, such as gang-affiliation tattooing and unprotected anal sex, as well as increased trafficking and use of illicit drugs. Such high-risk activities magnify their risk of contracting HCV infection in custody.58–60
Prisons mediate the dissemination of HCV infection beyond the period of incarceration. History of recent incarceration is significantly associated with contracting HCV infection in community settings.45,48 Among blood donors in community settings, history of incarceration, as well as being HCV-antibody positive, is strongly associated with IDU.61,62 History of incarceration has deleterious consequences on employment and earning prospects of released inmates, in part due to adverse employment implications of criminal records checks. Released inmates with HCV infection carry a double burden of stigma related to both imprisonment and HCV infection. A 2001 American study on the labor market consequences of incarceration determined that the earnings penalty of imprisonment ranges from 10% to 30%.63 Morbidity from HCV infection stigmatizes sufferers and impairs physical and mental fitness, thus contributing directly to reduced earnings potential. Income level is one of the established SDH through which imprisonment adversely impacts the health and welfare of released HCV-infected inmates. Individuals with HCV infection are more likely to be incarcerated, or re-incarcerated, mainly due to increased likelihood of involvement in drug-related criminal activity, homelessness, and unemployment, thus perpetuating the vicious cycle of health deterioration among HCV-infected individuals, in which prisons play a central mediating role.19,64,65
PRISONS AND TB INFECTION
TB ranks among the 10 principal causes of death and disability worldwide. In 2007, there were an estimated 9.3 million incident cases of TB and 1.8 million deaths from TB globally.66 TB causes $13 billion annually in decline in workforce productivity, its treatment using standard World Health Organization (WHO) regimens is highly cost effective in the most TB-affected countries,67 and it's one of only several diseases for which specific control strategies were set in the United Nations' 2000 Millennium Development Goals.68 Globally, prisons have been shown to have a higher prevalence of TB morbidity and mortality compared with other population cohorts.69 A 2008 WHO-supported literature review of TB in prisons70 revealed the following:
Prisons in countries of the former Soviet Union have some of the highest primary TB (e.g., prevalence of 4,560/100,000 in one Russian study) and multidrug-resistant TB (MDR-TB) prevalence rates in the world. MDR-TB rates for previously treated inmates ranged from 12% to 55%.
In an English study, 1.5% of prison staff had TB.
Spanish inmates were found to be co-infected with TB and human immunodeficiency virus (HIV) 17.9% of the time.
TB prevalence in a sample of Thailand's prisons was 568/100,000, with 19% of the patients confirmed with MDR-TB.
In a study of Tanzania's prisons, 41% of inmates had active TB. Rates of TB-HIV co-infection ranged from 26% in Tanzania to 74% in Malawi.
Prison systems serve as social determinants of TB infection in several ways. First, prison entrants generally have disproportionately higher prevalence of TB compared with their respective civil communities. The concentration function of prisons in relation to TB is attributable to homelessness, poverty, malnutrition, high rates of TB-predisposing diseases such as HIV, and marginal social status, such as unemployed, foreign-born cohorts.71,72
Second, as TB is an airborne disease, the architecture of prisons and the population of prison residents increase the risk of TB infection. For example, South Africa's prisons have a total capacity to accommodate 115,327 inmates, but recorded a mean daily count of 163,049 in 2007—a 42% excess capacity.73 Overcrowding is a demonstrated risk factor for TB transmission and a particularly common risk factor in prisons situated in developing countries with a high TB burden.74 Prison construction plans invariably accord higher priority to security than to adequate ventilation. In situations where inmates with active TB live in poorly ventilated custodial settings (as is usually the case in most developing countries), the potential for rapid transmission of TB is high.75,76 Malnutrition and bloodborne virus transmission—common health hazards associated with most prisons—also contribute to an increased risk of TB infection.77,78 The amplification function of prisons in relation to TB infection extends to custodial workers, with up to one-third of new TB infections among custodial staff in some prisons attributable to occupational exposure.79,80
Third, the quality of prison health services for TB surveillance and treatment remains inadequate in most prisons. For example, few prisons consistently undertake skin testing of new prison entrants (and annual testing thereafter) and correctional health staff, despite evidence that such surveillance activities have a strong potential to detect new TB cases early.81,82 Some of the consequences of TB surveillance and treatment failures in prison settings were highlighted during a TB outbreak in New York's prisons. A study related to this outbreak found that only nine (23%) of 39 inmates with MDR-TB received treatment prior to outbreak investigation.14 In Kyrgyzstan, as of 2006, TB prevalence in prisons exceeded 5,000/100,000 inmates—at least 40 times that of the general community—and MDR-TB rates were at least 15%. As of January 2007, less than half of all inmates with active TB had been diagnosed and had begun treatment.80
Prisons are directly linked to post-release morbidity and mortality of TB infection among inmates. The follow-up of released inmates who contract TB in custody is suboptimal, and failures to follow up imply that those with active TB are at increased risk of premature death from TB or serious TB-related morbidity. These former inmates may also endanger the health of close contacts in the community by posing serious infection risks. Increased morbidity and stigma of TB increase the risk of unemployment, homelessness, malnutrition, and drug use for released inmates. Unemployment and poverty limit the ability of TB sufferers to access effective treatment, and increase the likelihood of recidivism, thus perpetuating the vicious cycle in which prisons constitute a focal point.19,72
DISCUSSION
Documentation of the place or neighborhood effects of prison settings on the health of the incarcerated as well as elucidation of the mechanisms through which they are mediated have important policy implications for health-care delivery, health promotion, and the reduction of health inequities.9 This article adds to current literature on the role of custodial settings in determining the health of the incarcerated by positing that prisons constitute important SDH and that their impacts on the health of the incarcerated are particularly significant in relation to HCV and TB infections. Prisons exacerbate health inequities between individuals in contact with the criminal justice system and the general community. In the U.S., since 2008, one in 100 adult Americans is imprisoned at any point in time.5 Imprisonment is not an equal-opportunity punishment—as of June 2006, the adult imprisonment rates were 134/100,000 for females, 736/100,000 for white males, and 4,789/100,000 for African American males. Mass incarceration of poor, young African American males adversely influences their health outcomes for several decades following incarceration.5,6,35
Front-end policy choices that may facilitate reductions in the numbers of incarcerated individuals include alternatives to imprisonment for less serious offenders, as well as targeted use of drug courts to break the cycle of addiction, crime, and incarceration.83,84 Back-end policy options to reduce prison population growth include accountability for parole violations that do not necessarily imply imprisonment as the first punishment option. Noncustodial sanctions, such as well-managed day-reporting centers, constitute a viable noncustodial option, particularly for minor offenders or released inmates guilty of technical violation of their parole conditions, such as missing a counseling session.85
Europe's initiatives in working toward harmonizing penal and public health policies to promote the health of inmates through the Health In Prisons Project are commendable, as are the guidelines and policy positions of the National Commission for Correctional Health Care in the U.S.22,86 Advocacy for prison health-service quality equivalent to that of health care available in the respective general community is an important component of the “Prison Health as Part of Public Health” Moscow Declaration of October 2003.87,88 The implementation of the declaration's measures implies a need for adequate resources to fund health-care provision in prison settings, including optimal quality, quantity, and distribution of prison health workers. General and health-related prison policies and practices in most countries may require revision to ensure compatibility with human rights of inmates. Furthermore, inmate copayment policies need to be closely monitored, to reduce the risk of this cost-saving policy serving as an obstacle to sick but poor inmates receiving treatment.27
In relation to HCV and TB infections, adequate interventions to limit transmission and to promptly treat infected inmates constitute a public health opportunity to reduce the burden of these diseases. To facilitate control, it is important for prison health advocates and policy makers to ensure that treatment of inmates' TB and HCV infections is provided at nominal or no cost to inmates. Effective implementation of surveillance and prevention of drug and drug-equipment trafficking may minimize HCV-infection risks in prisons, as appears to be the case in many Australian prisons.43–45
Policies related to facilitating improved health of released inmates include pre-release screening to detect new health problems, documentation of existing health problems, and arrangement for community-based treatment, as well as social inclusion strategies, such as access to unemployment benefits, housing, and skills training. An inmate-reentry partnership that does not involve former inmates or members of the communities most affected by incarceration and reentry will likely find itself lacking expertise and legitimacy.88–91
Reducing the adverse impact of prisons on the health of the incarcerated and the general community requires a cooperative effort among all stakeholders. Development of quality benchmarks for core aspects of prison health care is an important component of this effort. Socio-politically, more equitable societies have a significantly greater capacity to address the upstream factors that lead individuals to prison, ensure adequate care for the incarcerated, and provide enough assistance to facilitate inmate reintegration.92,93
CONCLUSION
As social determinants, prisons exert a particularly strong influence on the epidemiology of HCV and TB infections. The threat posed by the high prevalence of hepatitis C and TB in prison settings represents both a difficult challenge and a unique opportunity. Custodial health workers have access to vulnerable populations that otherwise would be difficult to reach in the community. For some inmates whose lives prior to incarceration have been chaotic, their prison term represents an opportunity to assist them in developing an ordered approach to assessing and addressing their health needs. Each prison has a potential to be a healthy setting, provided there is political will and technical competence on the part of governments and custodial authorities to address the social, physical, spiritual, and mental well-being of inmates. Funding for prison health care is a major impediment; however, the stress on prison budgets may be reduced by penal systems being more selective about criminals who receive custodial punishment. Prison reforms have a strong potential to benefit not just inmates, but also the wider community, into which most inmates will return in the fullness of time.94
Acknowledgments
The author thanks Kim Brooklyn for assistance with proofreading.
REFERENCES
- 1.Sutherland EH, Cressey DR. Criminology. 9th ed. Philadelphia: Lippincott; 1974. [Google Scholar]
- 2.Gaonkar DP, McCarthy RJ., Jr. Panopticism and publicity: Bentham's quest for transparency. Public Cult. 1994;6:547–75. [Google Scholar]
- 3.Foucault M. Discipline and punish: the birth of the prison. New York: Vintage; 1995. [Google Scholar]
- 4.Applebaum A. Gulag: a history. New York: Doubleday; 2003. [Google Scholar]
- 5.The Pew Center on the States. One in 100: behind bars in America 2008. Washington: The Pew Charitable Trusts; 2008. [cited 2009 Oct 20]. Also available from: URL: http://www.pewcenteronthestates.org/uploadedFiles/8015PCTS_Prison08_FINAL_2-1-1_FORWEB.pdf. [Google Scholar]
- 6.Wacquant L. Deadly symbiosis: when ghetto and prison meet and mesh. In: Garland D, editor. Mass imprisonment social causes and consequences. London: Sage; 2001. pp. 82–120. [Google Scholar]
- 7.Walmsley R. World prison population list. 6th ed. London: International Centre for Prison Studies; 2007. [cited 2009 Oct 20]. Also available from: URL: http://www.scribd.com/doc/328143/World-Prison-Population-List-2007. [Google Scholar]
- 8.de Viggiani N. Unhealthy prisons: exploring structural determinants of prison health. Sociol Health Ill. 2007;29:115–35. doi: 10.1111/j.1467-9566.2007.00474.x. [DOI] [PubMed] [Google Scholar]
- 9.Roux AVD. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91:1783–9. doi: 10.2105/ajph.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. Final report of the Commission on Determinants of Health. Geneva: WHO; 2008. Closing the gap in a generation: health equity through action on the social determinants of health. [Google Scholar]
- 11.Baillargeon J, Black SA, Pulvino J, Dunn K. The disease profile of Texas prison inmates. Ann Epidemiol. 2000;10:74–80. doi: 10.1016/s1047-2797(99)00033-2. [DOI] [PubMed] [Google Scholar]
- 12.Senok AC, Botta GA. Human immunodeficiency virus and hepatitis virus infection in correctional institutions in Africa: is this the neglected source of an epidemic? J Med Microbiol. 2006;55:481–2. doi: 10.1099/jmm.0.46535-0. [DOI] [PubMed] [Google Scholar]
- 13.Marquart JW, Merianos DE, Hebert JL, Carroll L. Health conditions and prisoners: a review of research and emerging areas of inquiry. Prison J. 1997;77:184–208. [Google Scholar]
- 14.Valway SE, Greifinger RB, Papania M, Kilburn JO, Woodley C, DiFerdinando GT, et al. Multidrug-resistant tuberculosis in the New York State prison system, 1990–1991. J Infect Dis. 1994;170:151–6. doi: 10.1093/infdis/170.1.151. [DOI] [PubMed] [Google Scholar]
- 15.Freudenberg N. Adverse effects of US jail and prison policies on the health and well-being of women of color. Am J Public Health. 2002;92:1895–9. doi: 10.2105/ajph.92.12.1895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Butler T, Papanastasiou C. National prison entrants' bloodborne virus and risk behaviour survey report—2004 and 2007: prevalence of HIV, hepatitis C, hepatitis B, and risk behaviours among Australian prison entrants. Sydney: National Drug Research Institute, National Centre in HIV Epidemiology and Clinical Research; 2008. [Google Scholar]
- 17.Raphael D, editor. Social determinants of health: Canadian perspectives. 2nd ed. Toronto: Canadian Scholars' Press Inc; 2008. [Google Scholar]
- 18.Butler-Jones D. The Chief Public Health Officer's report on the state of public health in Canada 2008: addressing health inequalities. Ottawa: Public Health Agency of Canada; 2008. [Google Scholar]
- 19.Galea S, Vlahov D. Social determinants and the health of drug users: socioeconomic status, homelessness, and incarceration. Public Health Rep. 2002;117(Suppl 1):S135–45. [PMC free article] [PubMed] [Google Scholar]
- 20.Solzhenitsyn AI. The Gulag archipelago, 1918–1956: an experiment in literary investigation (volume 1) London: HarperCollins; 2007. original English translation published in 1973. [Google Scholar]
- 21.Smith C. “Healthy prisons”: a contradiction in terms? Howard J Crim Just. 2002;39:339–53. [Google Scholar]
- 22.National Commission on Correctional Health Care. The health status of soon-to-be-released inmates: a report to Congress (volumes 1 and 2) Chicago: NCCHC; 2002. [Google Scholar]
- 23.Golembeski C, Fullilove R. Criminal (in)justice in the city and its associated health consequences. Am J Public Health. 2008;98(Suppl 9):S185–90. doi: 10.2105/ajph.98.supplement_1.s185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Awofeso N. Why fund smoking cessation programmes in prisons? BMJ. 2005;330:852. [Google Scholar]
- 25.Jurnik NC. Individual and organizational determinants of correctional officer attitudes toward inmates. Criminology. 1985;23:523–39. [Google Scholar]
- 26.Wobeser WL, Datema J, Bechard B, Ford P. Causes of death among people in custody in Ontario, 1990–1999. CMAJ. 2002;167:1109–13. [PMC free article] [PubMed] [Google Scholar]
- 27.Awofeso N. Prisoner healthcare co-payment policy: a cost-cutting measure that might threaten inmates' health. Appl Health Econ Health Policy. 2005;4:159–64. doi: 10.2165/00148365-200504030-00004. [DOI] [PubMed] [Google Scholar]
- 28.Restum ZG. Public health implications of substandard correctional health care. Am J Public Health. 2005;95:1689–91. doi: 10.2105/AJPH.2004.055053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kariminia A, Butler TG, Corben S, Levy M, Grant L, Kaldor J. Extreme cause-specific mortality in a cohort of adult prisoners—1988 to 2002: a data-linkage study. Int J Epidemiol. 2007;36:310–6. doi: 10.1093/ije/dyl225. [DOI] [PubMed] [Google Scholar]
- 30.Binswanger IA, Stern MF, Deyo RA, Heagerty PJ, Cheadle A, Elmore JG, et al. Release from prison—a high risk of death for former inmates. N Engl J Med. 2007;356:157–65. doi: 10.1056/NEJMsa064115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Verger P, Rotily M, Prudhomme J, Bird S. High mortality rates among inmates during the year following their discharge from a French prison. J Forensic Sci. 2003;48:614–6. [PubMed] [Google Scholar]
- 32.Langan PA, Levin DJ. Bureau of Justice Statistics special report (NCJ 193427) Washington: Department of Justice (US); 2002. Recidivism of prisoners released in 1994. [Google Scholar]
- 33.Krieg AS. Aboriginal incarceration: health and social impacts. Med J Aust. 2006;184:534–6. doi: 10.5694/j.1326-5377.2006.tb00357.x. [DOI] [PubMed] [Google Scholar]
- 34.Pettit B, Western B. Mass imprisonment and the life course: race and class inequality in U.S. incarceration. Am Sociol Rev. 2004;69:151–69. [Google Scholar]
- 35.Garland D. The meaning of mass imprisonment. Punishm Soc. 2001;3:5–7. [Google Scholar]
- 36.Lavanchy D. The global burden of hepatitis C. Liver Int. 2009;29(Suppl 1):74–81. doi: 10.1111/j.1478-3231.2008.01934.x. [DOI] [PubMed] [Google Scholar]
- 37.Crippin JS, McCashland T, Terrault N, Sheiner P, Charlton MR. A pilot study of the tolerability and efficacy of antiviral therapy in hepatitis C virus–infected patients awaiting liver transplantation. Liver Transpl. 2002;8:350–5. doi: 10.1053/jlts.2002.31748. [DOI] [PubMed] [Google Scholar]
- 38.National Centre in HIV Epidemiology and Clinical Research. Annual surveillance report, 2001. Sydney: National Centre in HIV Epidemiology and Clinical Research, The University of New South Wales; 2001. HIV/AIDS, viral hepatitis and sexually transmissible infections in Australia. [Google Scholar]
- 39.Kim WR. The burden of hepatitis C in the United States. Hepatology. 2002;36(5 Suppl 1):S30–4. doi: 10.1053/jhep.2002.36791. [DOI] [PubMed] [Google Scholar]
- 40.Awofeso N. Hepatitis C virus infection: a disease of poverty. Trop Doct. 2001;31:184. doi: 10.1177/004947550103100329. [DOI] [PubMed] [Google Scholar]
- 41.Paris J, Pradham MM, Allen S, Cassidy WM. Cost of hepatitis C treatment in the correctional setting. J Correct Health Care. 2004;11:199–212. [Google Scholar]
- 42.Hilsabeck RC, Hassanein TI, Carlson MD, Ziegler EA, Perry W. Cognitive functioning and psychiatric symptomatology in patients with chronic hepatitis C. J Int Neuropsychol Soc. 2003;9:847–54. doi: 10.1017/S1355617703960048. [DOI] [PubMed] [Google Scholar]
- 43.Miller ER, Bi P, Ryan P. Hepatitis C virus infection in South Australian prisoners: seroprevalence, seroconversion, and risk factors. Int J Infect Dis. 2009;13:201–8. doi: 10.1016/j.ijid.2008.06.011. [DOI] [PubMed] [Google Scholar]
- 44.Butler T, Kariminia A, Levy M, Kaldor J. Prisoners are at risk for hepatitis C transmission. Eur J Epidemiol. 2004;19:1119–22. doi: 10.1007/s10654-004-1705-9. [DOI] [PubMed] [Google Scholar]
- 45.Maher L, Jalaludin B, Chant KG, Jayasuriya R, Sladden T, Kaldor JM, et al. Incidence and risk factors for hepatitis C seroconversion in injecting drug users in Australia. Addiction. 2006;101:1499–508. doi: 10.1111/j.1360-0443.2006.01543.x. [DOI] [PubMed] [Google Scholar]
- 46.Crofts N, Stewart T, Hearne P, Ping XY, Breshkin AM, Locarnini SA. Spread of bloodborne viruses among Australian prison entrants. BMJ. 1995;310:285–8. doi: 10.1136/bmj.310.6975.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Allwright S, Bradley F, Long J, Barry J, Thornton L, Parry JV. Prevalence of antibodies to hepatitis B, hepatitis C, and HIV and risk factors in Irish prisoners: results of a national cross sectional survey. BMJ. 2000;321:78–82. doi: 10.1136/bmj.321.7253.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.van Beek I, Dwyer R, Dore GJ, Luo K, Kaldor JM. Infection with HIV and hepatitis C virus among injecting drug users in a prevention setting: retrospective cohort study. BMJ. 1998;317:433–7. doi: 10.1136/bmj.317.7156.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Guimaràaes T, Granato CF, Varella D, Ferraz ML, Castelo A, Kalláas EG. High prevalence of hepatitis C infection in a Brazilian prison: identification of risk factors for infection. Braz J Infect Dis. 2001;5:111–8. doi: 10.1590/s1413-86702001000300002. [DOI] [PubMed] [Google Scholar]
- 50.Nunn A, Zaller N, Dickman S, Trimbur C, Nijhawan A, Rich JD. Methadone and buprenorphine prescribing and referral practices in US prison systems: results from a nationwide survey. Drug Alcohol Depend. 2009;105:83–8. doi: 10.1016/j.drugalcdep.2009.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sykes GM. The society of captives: a study of a maximum security prison. Princeton (NJ): Princeton University Press; 1958. [Google Scholar]
- 52.Butler T, Boonwaat L, Hailstone S, Falconer T, Lems P, Ginley T, et al. The 2004 Australian prison entrants' blood-borne virus and risk behaviour survey. Aust N Z J Public Health. 2007;31:44–50. doi: 10.1111/j.1753-6405.2007.00009.x. [DOI] [PubMed] [Google Scholar]
- 53.Adjei AA, Armah HB, Gbagbo F, Ampofo WK, Quaye IKE, Hesse IF, et al. Prevalence of human immunodeficiency virus, hepatitis B virus, hepatitis C virus and syphilis among prison inmates and officers at Nsawan and Accra, Ghana. J Med Microbiol. 2006;55:593–7. doi: 10.1099/jmm.0.46414-0. [DOI] [PubMed] [Google Scholar]
- 54.Holsen DS, Harthug S, Myrmel H. Prevalence of antibodies to hepatitis C virus and association with intravenous drug abuse and tattooing in a national prison in Norway. Eur J Clin Microbiol Infect Dis. 1993;12:673–6. doi: 10.1007/BF02009378. [DOI] [PubMed] [Google Scholar]
- 55.Fox RK, Currie SL, Evans J, Wright TL, Tobler L, Phelps B, et al. Hepatitis C virus infection among prisoners in the California state correctional system. Clin Infect Dis. 2005;41:177–86. doi: 10.1086/430913. [DOI] [PubMed] [Google Scholar]
- 56.Rischitelli G, Harris J, McCauley L, Gershon R, Guidotti T. The risk of acquiring hepatitis B or C among public safety workers: a systematic review. Am J Prev Med. 2001;20:299–306. doi: 10.1016/s0749-3797(01)00292-6. [DOI] [PubMed] [Google Scholar]
- 57.Crofts N. A cruel and unusual punishment. Med J Aust. 1997;166:116. doi: 10.5694/j.1326-5377.1997.tb140036.x. [DOI] [PubMed] [Google Scholar]
- 58.Awofeso N. Prison argot and penal discipline. [cited 2009 Oct 20];J Mundane Behav. 2004 5(1) serial online. Available from: URL: http://mundanebehavior.org/issues/v5n1/awofeso5-1.htm. [Google Scholar]
- 59.Laumann AE, Derick AJ. Tattoos and body piercings in the United States: a national data set. J Am Acad Dermatol. 2006;55:413–21. doi: 10.1016/j.jaad.2006.03.026. [DOI] [PubMed] [Google Scholar]
- 60.Andía JF, Deren S, Robles RR, Kang SY, Colón HM, Oliver-Velez D, et al. Factors associated with injection and noninjection drug use during incarceration among Puerto Rican drug injectors in New York and Puerto Rico. Prison J. 2005;85:329–42. [Google Scholar]
- 61.Delage G, Infante-Rivard C, Chiavetta J, Williems B, Pi D, Fast M. Risk factors for acquisition of hepatitis C virus infection in blood donors: results of a case-control study. Gastroenterology. 1999;116:893–9. doi: 10.1016/s0016-5085(99)70072-7. [DOI] [PubMed] [Google Scholar]
- 62.Wood E, Li K, Small W, Montaner JS, Scheter MT, Kerr T. Recent incarceration independently associated with syringe sharing by injection drug users. Public Health Rep. 2005;120:150–6. doi: 10.1177/003335490512000208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Western B, Kling JR, Weiman D. Princeton University, Industrial Relations Section working paper 450. Princeton (NJ): Princeton University; 2001. The labor market consequences of incarceration. [Google Scholar]
- 64.Bushway S, Stoll MA, Weiman DF, editors. Barriers to reentry? The labor market for released prisoners in post-industrial America. New York: Russell Sage Foundation; 2007. [Google Scholar]
- 65.Iguchi MY, Bell J, Ramchand RN, Fain T. How criminal system racial disparities may translate into health disparities. J Health Care Poor Underserved. 2005;16(4 Suppl B):48–56. doi: 10.1353/hpu.2005.0114. [DOI] [PubMed] [Google Scholar]
- 66.World Health Organization. Global tuberculosis control 2009: epidemiology, strategy, financing. Geneva: WHO; 2009. [Google Scholar]
- 67.Laxminarayan R, Klein E, Dye C, Floyd K, Darley S, Adeyi O. Policy research working paper 4295. Washington: The World Bank; 2007. Economic benefit of tuberculosis control. [Google Scholar]
- 68.United Nations, Statistics Division. Millennium development goals indicators. [cited 2010 Feb 2]. Available from: URL: http://unstats.un.org/unsd/mdg/Data.aspx.
- 69.Coninx R, Maher D, Reyes H, Grzemska M. Tuberculosis in prisons in countries with high prevalence. BMJ. 2000;320:440–2. doi: 10.1136/bmj.320.7232.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.World Health Organization. Literature review on tuberculosis in prisons. [cited 2009 Oct 20]. Available from: URL: http://www.who.int/tb/challenges/prisons/tb_in_prisons_lit_review_10feb08.pdf.
- 71.Saunders DL, Olive DM, Wallace SB, Lacy D, Leyba R, Kendig NE. Tuberculosis screening in the federal prison system: an opportunity to treat and prevent tuberculosis in foreign-born populations. Public Health Rep. 2001;116:210–8. doi: 10.1016/S0033-3549(04)50036-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Haddad MB, Wilson TW, Ijaz K, Marks SM, Moore M. Tuberculosis and homelessness in the United States, 1994–2003. JAMA. 2005;293:2762–6. doi: 10.1001/jama.293.22.2762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Luyt WFM. Contemporary corrections in South Africa after more than a decade of transformation. Acta Criminologica. 2008;21:176–95. [Google Scholar]
- 74.Maher D, Grzemska M, Coninx R, Reyes H. Guidelines for the control of tuberculosis in prisons. Geneva: WHO; 1998. [Google Scholar]
- 75.MacIntyre CR, Kendig N, Kummer L, Birago S, Graham NM. Impact of tuberculosis control measures and crowding on the incidence of tuberculosis infection in Maryland prisons. Clin Infect Dis. 1997;24:1060–7. doi: 10.1086/513632. [DOI] [PubMed] [Google Scholar]
- 76.Noeske J, Kuaban C, Amougou G, Piubello A, Pouillot R. Pulmonary tuberculosis in the Central Prison of Douala, Cameroon. East Afr Med J. 2006;83:25–30. doi: 10.4314/eamj.v83i1.9357. [DOI] [PubMed] [Google Scholar]
- 77.Liang-Fenton D. Failing to protect: food shortages and prison camps in North Korea. Asian Perspect. 2007;31:47–74. [Google Scholar]
- 78.Laniado-Loborín R. Tuberculosis in correctional facilities: a nightmare without end in sight. Chest. 2001;119:681–3. doi: 10.1378/chest.119.3.681. [DOI] [PubMed] [Google Scholar]
- 79.Steenland K, Levine AJ, Sieber K, Schulte P, Aziz D. Incidence of tuberculosis infection among New York State prison employees. Am J Public Health. 1997;87:2012–4. doi: 10.2105/ajph.87.12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.International Crisis Group. Kyrgyzstan's prison system nightmare. Asia Report No. 118. 2006. Aug 16, [cited 2009 Oct 24]. Available from: URL: http://www.crisisgroup.org/library/documents/asia/central_asia/118_kyrgyzstans_prison_system_nightmare.pdf.
- 81.Spencer SS, Morton AR. Tuberculosis surveillance in a state prison system. Am J Public Health. 1989;79:507–9. doi: 10.2105/ajph.79.4.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Levy MH, Butler TG, Zhou J. Prevalence of Mantoux positivity and annual risk of infection for tuberculosis in New South Wales prisoners, 1996 and 2001. N S W Public Health Bull. 2007;18:119–24. doi: 10.1071/nb07051. [DOI] [PubMed] [Google Scholar]
- 83.Turner S, Longshore D, Wenzel S, Deschenes E, Greenwood P, Fain T, et al. A decade of drug treatment court research. Subst Use Misuse. 2002;37:1489–527. doi: 10.1081/ja-120014420. [DOI] [PubMed] [Google Scholar]
- 84.Indermaur D, Roberts L. Drug courts in Australia: the first generation. Curr Issues Crim Justice. 2003;15:136–54. [Google Scholar]
- 85.Jones PR. Expanding the use of non-custodial sentencing options: an evaluation of the Kansas Community Corrections Act. Howard J Crim Just. 1990;29:114–29. [Google Scholar]
- 86.Gatherer A, Moller L, Hayton P. The World Health Organization European Health In Prisons Project after 10 years: persistent barriers and achievements. Am J Public Health. 2005;95:1696–700. doi: 10.2105/AJPH.2003.057323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.World Health Organization. Declaration on prison health as part of public health. [cited 2009 Oct 25]. Available from: URL: http://www.euro.who.int/Document/HIPP/moscow_declaration_eng04.pdf.
- 88.Awofeso N. Prison health advocacy and its changing boundaries. Int J Prison Health. 2008;4:175–83. doi: 10.1080/17449200802473081. [DOI] [PubMed] [Google Scholar]
- 89.Baldry E, McDonnell D, Maplestone P, Peeters M. Ex-prisoners, homelessness and the state in Australia. Aus NZ J Criminol. 2006;39:20–33. [Google Scholar]
- 90.Hammett TM, Roberts C, Kennedy S. Health-related issues in prisoner reentry. Crime Delinquency. 2001;47:390–409. [Google Scholar]
- 91.La Vigne NG, Cowan J, Brazzell D. Mapping prisoner reentry: an action research guidebook. 2nd ed. Washington: The Urban Institute; 2006. [Google Scholar]
- 92.Wilkinson R, Pickett K. The spirit level: why more equal societies almost always do better. London: Penguin; 2009. [Google Scholar]
- 93.Lappi-Seppälä T. Penal policy in Scandinavia. In: Tonry M, editor. Crime and justice, volume 36: crime, punishment, and politics in comparative perspective. Chicago: University of Chicago Press; 2007. pp. 217–9. [Google Scholar]
- 94.Williams NH. Prison health and the health of the public: ties that bind. J Correct Health Care. 2007;13:80–92. [Google Scholar]