SYNOPSIS
The institutional and community norms that lead to the stigmatization of tuberculosis (TB) are thought to hinder TB control. We performed a systematic review of the literature on TB stigma to identify the causes and evaluate the impact of stigma on TB diagnosis and treatment. Several themes emerged: fear of infection is the most common cause of TB stigma; TB stigma has serious socioeconomic consequences, particularly for women; qualitative approaches to measuring TB stigma are more commonly utilized than quantitative surveys; TB stigma is perceived to increase TB diagnostic delay and treatment noncompliance, although attempts to quantify its impact have produced mixed results; and interventions exist that may reduce TB stigma.
Future research should continue to characterize TB stigma in different populations; use validated survey instruments to quantify the impact of TB stigma on TB diagnostic delay, treatment compliance, and morbidity and mortality; and develop additional TB stigma-reduction strategies.
The social determinants of health refer to the institutional, community, and interpersonal factors that affect health outside of the ease with which an individual can access medical services.1 Stigma, which is shaped and promulgated by institutional and community norms and interpersonal attitudes, is a social determinant of health.2 Stigma is a process that begins when a particular trait or characteristic of an individual or group is identified as being undesirable or disvalued.3 The stigmatized individual often internalizes this sense of disvalue and adopts a set of self-regarding attitudes about the marked characteristic including shame, disgust, and guilt.4 These attitudes produce a set of behaviors that include hiding the stigmatized trait, withdrawing from interpersonal relationships, or increasing risky behavior.5,6 Stigmatization is conceptually distinct from discrimination—another social determinant of health—in that the primary goal of discrimination is exclusion, not necessarily for the target to feel ashamed or guilty.7,8 Stigmatized individuals can, however, suffer discrimination and status loss at the hands of the broader community, whose norms have caused them to be perceived as undesirable.3,9
Stigmatization is a complex process involving institutions, communities, and inter- and intrapersonal attitudes. While it has been recognized as an important social determinant of health and health disparities, the difficulties in identifying, characterizing, measuring, and tracking changes in stigmatization over time have made it challenging to justify devoting resource-intensive interventions to the problem.2,10 One exception is human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS) research, where the interactions among stigma, HIV risk behaviors, and HIV-associated outcomes have been fairly well characterized.11,12 Substantially less study has been conducted on the mechanisms through which stigma impacts the health of individuals at risk for or infected with tuberculosis (TB).
In this article, we review the available literature on TB stigma. Our goal was to identify the causes of TB stigma and to assess the impact of stigma on TB diagnosis and treatment. We identified three themes in the existing literature on TB stigma: (1) studies that characterize and measure TB stigma, (2) studies that explore the effect of TB stigma on TB diagnosis and treatment, and (3) studies that describe interventions to reduce TB stigma and the impact of these interventions on TB diagnosis and treatment. We also considered the gaps in existing research on stigma and the TB pandemic, and assessed potential interventions to reduce the health impact of TB stigma.
METHODS
Search strategy
Using the terms “tuberculosis AND stigma,” “tuberculosis AND stigmatization,” “tuberculosis AND stigmatized,” “tuberculosis AND stigmatizing,” “TB AND stigma,” “TB AND stigmatization,” “TB AND stigmatized,” and “TB AND stigmatizing,” we searched PubMed for articles addressing TB stigma. We reviewed the reference sections of identified articles to locate additional publications not found in our initial search.
We reviewed each article, noting its date of publication, geographic location, study type, use of qualitative and/or quantitative methods, and key results and conclusions. We then assigned it to one of three mutually exclusive content categories, based on the authors' primary focus. The first category involved articles characterizing and measuring TB stigma, including articles identifying the causes and socioeconomic consequences of TB stigma. This category also included articles reporting on the development or evaluation of TB assessment tools and articles using qualitative or quantitative techniques to measure TB stigma in various populations. The second category included articles focusing on the theoretical and empirical connections between TB stigma and TB diagnosis and treatment. The third category included articles on interventions to reduce TB stigma and the impact of such reductions on TB diagnostic delay and treatment compliance. We excluded articles that did not fit into these categories or were not in English.
RESULTS
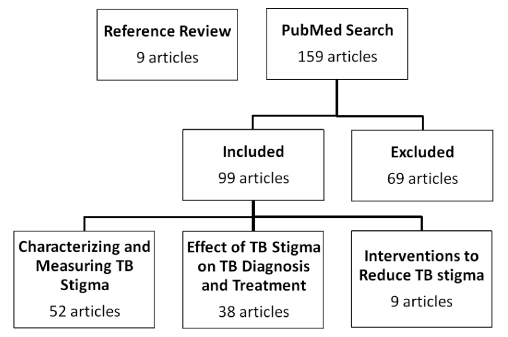
The literature review yielded 168 articles (Figure 1), 159 from the PubMed search and nine from the reference sections of identified articles. Of the 168 articles, 69 were excluded from this review. The most common reasons for exclusion included focus on the effects of HIV stigma on TB diagnosis and treatment (five articles), one or more of the authors was affiliated with TB-related institutions although the article was not on TB (13 articles), and the article was not in English (six articles). Of the 99 articles included, the majority (52 articles) characterized or measured TB stigma. A smaller number (38 articles) examined the impact of TB stigma on TB diagnosis and treatment. Relatively few (nine articles) described interventions to reduce TB stigma. Included studies were published between 1976 and 2009. Geographically, most studies involved Asia/Pacific Islands (33%) or Africa/Middle East (28%) compared with multiregional (17%), North America (9%), Latin/South America (8%), or Europe/Russia (4%).
Figure 1.
Flow diagram of literature search on TB and stigmatization (n=168)
TB = tuberculosis
Characterizing and measuring TB stigma
Characterizing TB stigma.
Understanding the origins of TB stigma is integral to reducing its impact on health. Using surveys, focus groups, and unstructured and focused interviews, a number of studies have explored the causes of TB stigma. Although there is geographic and cultural variation in the explanations for why TB is stigmatized, most authors identify the perceived contagiousness of TB as a leading cause of stigmatization.13–22 Lack of knowledge regarding routes of TB transmission may also contribute to TB stigma.23–26 Even among people with relatively good knowledge of TB transmission and transmissibility, however, the perceived risk of transmission can lead to stigmatization and isolation of individuals with TB.27
In areas of high HIV prevalence, where HIV and TB co-infection is common, the link between the two diseases has contributed to the stigmatization of TB.28–34 TB is perceived as a marker for HIV positivity; therefore, HIV-associated stigma is transferred to TB-infected individuals.35 Other causes of TB stigma include the perceived associations of TB with malnutrition,36 poverty,37 being foreign-born,38 and low social class.14 As with HIV, TB is stigmatized in this context because it is linked to other disvalued characteristics, which themselves are also social determinants of health. Finally, TB stigma may occur because an affected individual's community believes he or she must have done something to deserve to be infected.19,27 This judgment may reflect the belief that TB is divine punishment for a moral or personal failing, which then licenses stigmatization.14
TB-infected individuals perceive themselves to be at risk for a number of stigma-related social and economic consequences. Because the most common result of TB stigma is isolation from other members of the community, TB infection can substantially impact economic opportunities. For example, the stigmatization of TB in Ghana has led to the prohibition of TB-infected individuals from selling goods in public markets and attending community events.17 When an individual dies of TB, fear of TB stigma can lead families to hide the cause of death from other members of the community, even when such information might be useful in targeted TB screening.39 Similarly, fear of TB stigma can lead infected individuals to hide their TB status from their families.16,22 TB stigma also results in a sense of shame or guilt, leading to self-isolation as TB-infected individuals internalize their community's negative judgments about the disease.37,40
The socioeconomic consequences of TB stigma differ in men and women. In general, men are more concerned with the impact of TB stigma on their economic prospects, which include job loss and reduced income.41–43 While TB stigma also affects their financial status, women tend to be more concerned that TB stigma will adversely impact their marriage prospects or that their families will shun them.43–46 In some areas, however, men are more worried than women about the effect of TB stigma on their marriage opportunities.46 Married women with children may fear that their husbands will reject them if they are diagnosed with TB and that they will be unable to care for their families.43,47
Measuring TB stigma.
In addition to characterizing the causes of TB stigma, several authors have attempted to capture the prevalence of perceived, internalized, and actually experienced TB stigma and to compare the extent of TB stigma in different geographic regions. Many studies use qualitative instruments (e.g., in-depth interviews and focus groups) to gauge the degree to which TB is seen as stigmatized in a community. Considerable geographic variability exists in the perceived prevalence of TB stigma, with 27% to 80% of at-risk individuals reporting that TB is stigmatized in their communities.48–50 TB stigma is felt more strongly in certain subpopulations, including women, refugees, individuals from rural areas, and people with lower education levels.51–54 Discordance between perceived and actual experiences of stigmatization among at-risk and TB-infected individuals has also been documented. For example, in one study of at-risk, TB-negative Mexican Americans, half the participants believed that someone with TB would experience social isolation. In a demographically similar comparison population of individuals with documented TB infection, none had actually experienced social isolation.38
To assist in better understanding the prevalence of TB stigma, several authors have developed standardized TB stigma assessment tools. For example, Macq et al. introduced and validated a quantitative TB stigma questionnaire based on surveys designed to measure mental health stigma.55 Their instrument captures both perceived and internalized TB stigma. Van Rie et al. developed a comprehensive TB stigma assessment scale covering domains such as fear of disease transmission, attitudes toward TB, association of TB with shame and judgment, and disclosure of disease status. Their scale has good internal consistency and reasonable test-retest reliability.56 Although measuring any type of stigma is a challenge, a number of instruments have been developed to quantify the stigmatization of other conditions; these may also be adapted to measure perceived and internalized TB stigma.57
The effects of TB stigma on TB diagnosis and treatment
It is a widely held view that TB stigma contributes to delays in TB diagnosis and negatively impacts treatment compliance. A number of qualitative studies report that community members without TB, individuals with TB, and health-care providers who treat TB perceive TB stigma to be a barrier to prompt diagnosis of the disease.58–62 At-risk individuals report that fear of TB stigma and the social and economic impact of stigma affects their willingness to undergo TB screening and to seek medical care after the onset of symptoms associated with TB.63–65 Individuals with TB-like symptoms may first attempt to see private physicians so as to avoid TB stigma. Because private clinics typically have longer waits for appointments, this may translate to diagnostic delay and increased financial costs for patients.66
Several studies suggest that health-care providers and at-risk community members perceive TB stigma to have a more substantial impact on women's health-care-seeking behavior than on men's.67–70 Balasubramanian et al., however, found that although women in south India felt TB stigma more strongly than men, they were more likely to access health services.71 Only one study recommended considering the impact of TB stigma on children when designing a TB screening program.72
Individuals with TB and their health-care providers also identify TB stigma as a cause of noncompletion of treatment.73–77 Even after the start of therapy, concern about being identified as having TB and suffering the consequences of TB stigma may lead individuals to drop out of treatment programs. TB stigma has also been raised as a potential barrier to home- and work-based direct observational therapy (DOT), given that the presence of TB nurses might mark a person as infected.78,79 Collectively, these studies suggest that at-risk communities and infected individuals perceive that TB stigma causes diagnostic delay and can lead to treatment noncompliance.
Attempts to quantify the contribution of TB stigma to diagnostic delay and treatment adherence, however, have produced mixed results. Kiwuwa and colleagues surveyed newly diagnosed TB patients in Uganda to assess factors related to the duration of time between the onset of symptoms and their first health-care visit. Predictors of delays of more than two weeks included daily alcohol use and subsistence farming, but not perceived TB stigma.80 Similarly, TB stigma was not a predictor of significant delay between the onset of symptoms and seeking health care in Zambia or Syria.81,82 In a study in Cameroon, Cambanis et al. found that perceived TB stigma was a significant predictor of delays of more than four weeks, but the association disappeared with multivariate adjustment.83 The impact of TB stigma on treatment compliance is also unclear. Woith and Larson found that, among Russians with active pulmonary TB, TB stigma was actually a predictor of treatment adherence.84 In contrast, TB stigma was the most common motivation cited by HIV-infected Tanzanian patients who did not complete isoniazid preventive therapy.85 Perceived TB stigma was also associated with noncompliance among Pakistani patients on DOT.86
Interventions to reduce TB stigma
Relatively few interventions have been introduced to reduce TB stigma, and few investigators have measured whether reductions in TB stigma decrease diagnostic delay or improve treatment compliance. No studies have assessed whether decreased TB stigma affects TB morbidity or mortality. Several authors have suggested that TB education/support programs, aimed at health-care providers, individuals with TB, and at-risk community members, may reduce TB stigma, although little data exist on the effectiveness of these strategies.87–89 Rajeswari and colleagues found that perceived TB stigma did not change in a surveyed population of TB-infected individuals in south India after completion of a DOT program with an educational component.90
As is true with other stigmatized conditions including HIV and mental illness, the most promising approach to reducing TB stigma may be to empower individuals with TB to resist stigmatizing external judgments, while working to change community norms about the disease.2,91,92 For example, several studies have assessed the impact of TB clubs, particularly in Africa, on perceived TB stigma and treatment compliance.93,94 These clubs, which typically consist of three to 10 individuals with TB, are organized by TB health workers and meet weekly to offer social support, arrange transportation to clinics, encourage treatment adherence, and monitor for treatment side effects.93 They also encourage TB screening among other at-risk community members.95
Using a focus group-based approach, Demissie et al. have shown that individuals enrolled in TB clubs perceive themselves to be less affected by TB stigma than those receiving standard, clinic-run treatment.94 A likely explanation is that TB clubs reduce social isolation and offer an environment in which TB status is highly visible and accepted. Demissie et al. also found that the presence of TB clubs in the broader community appears to reduce negative attitudes and practices concerning TB. In their study, individuals enrolled in Ethiopian TB clubs were more likely to complete TB treatment than TB-infected patients with similar sociodemographic characteristics in areas without TB clubs.
Macq and colleagues conducted a similar study on the effect of TB clubs on TB stigma in rural Nicaragua.96 Compared with TB patients in municipalities without TB clubs, patients enrolled in TB clubs had a small but significant reduction in internalized TB stigma, as measured on a 10-question stigma assessment scale. There was, however, no difference in treatment completion rates between the two populations. Finally, Liefooghe and colleagues found that TB-positive Pakistani patients randomized to receive counseling to strengthen their perceived self-efficacy, which is often adversely impacted by TB stigma, had a 13% reduction in treatment defaulting compared with patients who did not receive counseling. The intervention was even more beneficial for women, especially housewives, among whom the reduction in treatment defaulting was 25%.97
DISCUSSION
Stigmatization is a social determinant of health. Stigma occurs because of community and institutional norms about undesirable or disvalued behaviors or characteristics. When diseases are stigmatized, the fear of the social and economic consequences following diagnosis can make individuals reluctant to seek and complete medical care. The structure of a community's beliefs and norms about a disease and the resulting stigma can, therefore, substantially impact health. In this article, we systematically reviewed the literature on TB stigma, including studies that characterized and measured TB stigma; assessed its impact on TB diagnosis and treatment; and explored interventions to reduce TB stigma.
The most common cause of TB stigma is the perceived risk of transmission from TB-infected individuals to susceptible community members. Depending on geographic region, however, TB is also stigmatized because of its associations with HIV, poverty, low social class, malnutrition, or disreputable behavior. TB stigma has a more significant impact on women and poor or less-educated community members, which is especially concerning given that these groups are often at higher risk for health disparities. TB stigma may, therefore, worsen preexisting gender- and class-based health disparities.
Although several survey instruments are in development for measuring perceived and internalized TB stigma, most research uses qualitative techniques for assessing TB stigma. The use of different measurement tools may explain why TB stigma is a predictor of diagnostic delay and treatment nonadherence in some studies and not in others. In general, however, health-care providers and at-risk community members perceive that TB stigma leads to TB diagnostic delay and treatment noncompletion. Some interventions, particularly TB clubs, have been shown to decrease TB stigma and improve TB treatment adherence. However, there are no studies that address whether reductions in TB stigma correspond with improved TB morbidity or mortality. TB clubs may help TB-positive individuals resist stigmatization, and they may also change community norms about TB by increasing the visibility of the disease.
Limitations
While several clear themes emerged from our literature review, it is important to note its limitations. First, although stigma is conceptually different from related experiences, such as discrimination, bias, and prejudice, not all authors make these distinctions in the same way. Given our narrowly tailored search strategy, it is possible that we may have missed articles relevant to TB stigma because they were categorized as involving TB discrimination, bias, or prejudice. Second, because we focused on the biomedical literature on TB stigma as found via PubMed and through review of the reference sections of identified articles, we may have missed articles on TB stigma from sociological or psychological resources not indexed in PubMed.
CONCLUSIONS
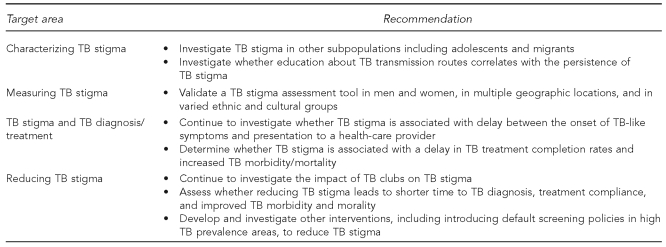
Based on our review of the available literature on TB stigma, we identified several areas where additional research is needed. Figure 2 summarizes these recommendations, which are explained more fully in the following sections.
Figure 2.
Summary of recommendations for additional research on TB stigma
TB = tuberculosis
Recommendations for characterizing TB stigma
The origins and consequences of TB stigma have been well characterized in multiple geographic regions. Because the socioeconomic impact of TB stigma varies among different groups (e.g., men and women), it is important to continue to investigate the effects of TB stigma in other subpopulations including adolescents and individuals with latent TB. This information can be used to design and target interventions that specifically address the impact of TB stigma on a given group. For example, knowing that women are typically more concerned about the effect of TB stigma on their marriages can direct health-care providers to offer specific counseling and educational resources about partner notification. Because improved TB education has been proposed as a method of reducing TB stigma, it is important to determine whether knowledge of TB transmissibility and transmission routes actually correlates with TB stigma.
Recommendations for measuring TB stigma
The recent introduction and validation of two stigma assessment questionnaires is helpful in efforts to measure and track changes in TB stigma over time.55,56 These instruments should be tested and validated among men and women, in multiple geographic locations, and in varied ethnic and cultural groups. Widespread adoption of one or more of them, supplemented with qualitative data, will allow better comparisons among studies. A common stigma assessment tool will also assist in targeting interventions toward particular aspects of TB stigma (e.g., self-isolation or hiding one's TB status) as identified using these instruments.
Recommendations for studying the effects of TB stigma on TB diagnosis and treatment
An important challenge for future research on TB stigma is to better assess the impact of TB stigma on TB diagnostic delay and treatment compliance. While TB stigma is perceived to have a negative impact on prompt TB diagnosis and treatment completion rates, studies that formally assessed the effect of TB stigma have had mixed findings. The availability of quantitative survey instruments should allow researchers to determine whether TB stigma is associated with delay between the onset of TB-like symptoms and presentation to a health-care provider and whether a higher degree of TB stigma is associated with longer delay. Similar research should examine the impact of TB stigma on TB treatment completion rates.
Recommendations for interventions to reduce TB stigma
Although community and institutional norms ultimately mediate stigmatization, wide-scale interventions to change these norms can be difficult. A more promising approach appears to be helping TB-infected individuals resist TB stigma, particularly through TB clubs. Additional studies in regions where TB stigma is common should be conducted to validate the impact of TB clubs on TB stigma and to assess whether a reduction in TB stigma leads to improved time to TB diagnosis, treatment compliance, and, ultimately, reduced TB morbidity and mortality. This research should employ one of the standardized TB stigma measurement tools to track changes in TB stigma over time and to correlate changes in individual- and community-level TB stigma with diagnostic delay and treatment completion. Assessing TB stigma among individuals at risk for TB before and after the introduction of TB clubs can also help determine whether the increased visibility of TB-infected individuals changes broader norms about the disease. Finally, it is essential to continue to develop other interventions—for example, counseling TB-infected patients or introducing default screening policies in high TB prevalence areas—to reduce TB stigma.
It is also important to supplement this bottom-up approach to reducing TB stigma with an assessment of interventions designed to directly address stigmatizing community norms about TB. While greater education about the cause and routes of transmission of TB has been proposed as a method for reducing TB stigma, more research is required to assess whether simply providing more information about TB can change these norms. Studies from the HIV literature suggest that widespread educational efforts have had minimal effect on HIV knowledge and only a small effect on stigmatization of that disease.98,99 It would, however, be useful to assess whether interventions known to reduce HIV/AIDS stigma have any effect on TB diagnosis and treatment.
REFERENCES
- 1.World Health Organization, Commission on Social Determinants of Health. Final report of the Commission on Social Determinants of Health. Geneva: WHO; 2008. Closing the gap in a generation: health equity through action on the social determinants of health. [Google Scholar]
- 2.Heijnders M, Van Der Meij S. The fight against stigma: an overview of stigma-reduction strategies and interventions. Psychol Health Med. 2006;11:353–63. doi: 10.1080/13548500600595327. [DOI] [PubMed] [Google Scholar]
- 3.Link B, Phelan J. Conceptualizing stigma. Annu Rev Sociol. 2001;27:363–85. [Google Scholar]
- 4.Goffman E. Garden City (NY): Anchor Books; 1963. Stigma: notes on the management of spoiled identity. [Google Scholar]
- 5.Smith R, Rossetto K, Peterson BL. A meta-analysis of disclosure of one's HIV-positive status, stigma and social support. AIDS Care. 2008;20:1266–75. doi: 10.1080/09540120801926977. [DOI] [PubMed] [Google Scholar]
- 6.Collins PY, von Unger H, Armbrister A. Church ladies, good girls, and locas: stigma and the intersection of gender, ethnicity, mental illness, and sexuality in relation to HIV risk. Soc Sci Med. 2008;67:389–97. doi: 10.1016/j.socscimed.2008.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deacon H. Towards a sustainable theory of health-related stigma: lessons from the HIV/AIDS literature. J Community Appl Soc Psychol. 2006;16:418–25. [Google Scholar]
- 8.Courtwright AM. Justice, stigma, and the new epidemiology of health disparities. Bioethics. 2009;23:90–6. doi: 10.1111/j.1467-8519.2008.00717.x. [DOI] [PubMed] [Google Scholar]
- 9.Major B, O'Brien LT. The social psychology of stigma. Annu Rev Psychol. 2005;56:393–421. doi: 10.1146/annurev.psych.56.091103.070137. [DOI] [PubMed] [Google Scholar]
- 10.Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Soc Sci Med. 2003;57:13–24. doi: 10.1016/s0277-9536(02)00304-0. [DOI] [PubMed] [Google Scholar]
- 11.Mahajan AP, Sayles JN, Patel VA, Remien RH, Sawires SR, Ortiz DJ, et al. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS. 2008;22(Suppl 2):S67–79. doi: 10.1097/01.aids.0000327438.13291.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bos AE, Schaalma HP, Pryor JB. Reducing AIDS-related stigma in developing countries: the importance of theory- and evidence-based interventions. Psychol Health Med. 2008;13:450–60. doi: 10.1080/13548500701687171. [DOI] [PubMed] [Google Scholar]
- 13.AhChing LP, Sapolu M, Samifua M, Yamada S. Attitudes regarding tuberculosis among Samoans. Pac Health Dialog. 2001;8:15–9. [PubMed] [Google Scholar]
- 14.Baral SC, Karki DK, Newell JN. Causes of stigma and discrimination associated with tuberculosis in Nepal: a qualitative study. BMC Public Health. 2007;7:211. doi: 10.1186/1471-2458-7-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bennstam AL, Strandmark M, Diwan VK. Perception of tuberculosis in the Democratic Republic of Congo: wali ya nkumu in the Mai Ndombe district. Qual Health Res. 2004;14:299–312. doi: 10.1177/1049732303261822. [DOI] [PubMed] [Google Scholar]
- 16.Dodor EA, Kelly S. “We are afraid of them”: attitudes and behaviours of community members towards tuberculosis in Ghana and implications for TB control efforts. Psychol Health Med. 2009;14:170–9. doi: 10.1080/13548500802199753. [DOI] [PubMed] [Google Scholar]
- 17.Dodor EA, Neal K, Kelly S. An exploration of the causes of tuberculosis stigma in an urban district in Ghana. Int J Tuberc Lung Dis. 2008;12:1048–54. [PubMed] [Google Scholar]
- 18.Gelaw M, Genebo T, Dejene A, Lemma E, Eyob G. Attitude and social consequences of tuberculosis in Addis Ababa, Ethiopia. East Afr Med J. 2001;78:382–8. doi: 10.4314/eamj.v78i7.9014. [DOI] [PubMed] [Google Scholar]
- 19.Macq J, Solis A, Martinez G, Martiny P, Dujardin B. An exploration of the social stigma of tuberculosis in five “municipios” of Nicaragua to reflect on local interventions. Health Policy. 2005;74:205–17. doi: 10.1016/j.healthpol.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 20.Peltzer K. Perception of illness among secondary school pupils in South Africa: malaria, tuberculosis, HIV/AIDS, and alcoholism. Psychol Rep. 2001;88(3 Pt 1):847–8. doi: 10.2466/pr0.2001.88.3.847. [DOI] [PubMed] [Google Scholar]
- 21.Sharma N, Malhotra R, Taneja DK, Saha R, Ingle GK. Awareness and perception about tuberculosis in the general population of Delhi. Asia Pac J Public Health. 2007;19:10–5. doi: 10.1177/10105395070190020301. [DOI] [PubMed] [Google Scholar]
- 22.Yamada S, Caballero J, Matsunaga DS, Agustin G, Magana M. Attitudes regarding tuberculosis in immigrants from the Philippines to the United States. Fam Med. 1999;7:477–82. [PubMed] [Google Scholar]
- 23.West EL, Gadkowski LB, Ostbye T, Piedrahita C, Stout JE. Tuberculosis knowledge, attitudes, and beliefs among North Carolinians at increased risk of infection. N C Med J. 2008;69:14–20. [PubMed] [Google Scholar]
- 24.Armijos RX, Weigel MM, Qincha M, Ulloa B. The meaning and consequences of tuberculosis for an at-risk urban group in Ecuador. Rev Panam Salud Publica. 2008;23:188–97. doi: 10.1590/s1020-49892008000300006. [DOI] [PubMed] [Google Scholar]
- 25.Sengupta S, Pungrassami P, Balthip Q, Strauss R, Kasetjaroen Y, Chongsuvivatwong V, et al. Social impact of tuberculosis in southern Thailand: views from patients, care providers and the community. Int J Tuberc Lung Dis. 2006;10:1008–12. [PubMed] [Google Scholar]
- 26.Brand RC, Jr, Clairborn WL. Two studies of comparative stigma: employer attitudes and practices toward rehabilitated convicts, mental and tuberculosis patients. Community Ment Health J. 1976;12:168–75. doi: 10.1007/BF01411387. [DOI] [PubMed] [Google Scholar]
- 27.Mak WW, Mo PK, Cheung RY, Woo J, Cheung FM, Lee D. Comparative stigma of HIV/AIDS, SARS, and tuberculosis in Hong Kong. Soc Sci Med. 2006;63:1912–22. doi: 10.1016/j.socscimed.2006.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O'Donoghue M. Frontal assault on tuberculosis. Interview by Eileen Fursland. Nurs Stand. 2006;20:22–4. [PubMed] [Google Scholar]
- 29.Godfrey-Faussett P, Ayles H. The impact of HIV on tuberculosis control—towards concerted action. Lepr Rev. 2002;73:376–85. [PubMed] [Google Scholar]
- 30.Godfrey-Faussett P, Ayles H. Can we control tuberculosis in high HIV prevalence settings? Tuberculosis (Edinb) 2003;83:68–76. doi: 10.1016/s1472-9792(02)00083-5. [DOI] [PubMed] [Google Scholar]
- 31.Grange J, Story A, Zumla A. Tuberculosis in disadvantaged groups. Curr Opin Pulm Med. 2001;7:160–4. doi: 10.1097/00063198-200105000-00008. [DOI] [PubMed] [Google Scholar]
- 32.Nnoaham KE, Pool R, Bothamley G, Grant AD. Perceptions and experiences of tuberculosis among African patients attending a tuberculosis clinic in London. Int J Tuberc Lung Dis. 2006;10:1013–7. [PubMed] [Google Scholar]
- 33.Somma D, Thomas BE, Karim F, Kemp J, Arias N, Auer C, et al. Gender and socio-cultural determinants of TB-related stigma in Bangladesh, India, Malawi and Colombia. Int J Tuberc Lung Dis. 2008;12:856–66. [PubMed] [Google Scholar]
- 34.Zolowere D, Manda K, Panulo B, Jr, Muula AS. Experiences of self-disclosure among tuberculosis patients in rural Southern Malawi. Rural Remote Health. 2008;8:1037. [PubMed] [Google Scholar]
- 35.Ngamvithayapong J, Winkvist A, Diwan V. High AIDS awareness may cause tuberculosis patient delay: results from an HIV epidemic area, Thailand. AIDS. 2000;14:1413–9. doi: 10.1097/00002030-200007070-00015. [DOI] [PubMed] [Google Scholar]
- 36.Westaway MS, Wolmarans L. Cognitive and affective reactions of black urban South Africans towards tuberculosis. Tuber Lung Dis. 1994;75:447–53. doi: 10.1016/0962-8479(94)90119-8. [DOI] [PubMed] [Google Scholar]
- 37.Mata JI. Integrating the client's perspective in planning a tuberculosis education and treatment program in Honduras. Med Anthropol. 1985;9:57–64. doi: 10.1080/01459740.1985.9965918. [DOI] [PubMed] [Google Scholar]
- 38.Joseph HA, Waldman K, Rawls C, Wilce M, Shrestha-Kuwahara R. TB perspectives among a sample of Mexicans in the United States: results from an ethnographic study. J Immigr Minor Health. 2008;10:177–85. doi: 10.1007/s10903-007-9067-5. [DOI] [PubMed] [Google Scholar]
- 39.Huy TQ, Johansson A, Long NH. Reasons for not reporting deaths: a qualitative study in rural Vietnam. World Health Popul. 2007;9:14–23. doi: 10.12927/whp.2007.18739. [DOI] [PubMed] [Google Scholar]
- 40.Kelly P. Isolation and stigma: the experience of patients with active tuberculosis. J Community Health Nurs. 1999;16:233–41. doi: 10.1207/S15327655JCHN1604_3. [DOI] [PubMed] [Google Scholar]
- 41.Long NH, Johansson E, Diwan VK, Winkvist A. Fear and social isolation as consequences of tuberculosis in VietNam: a gender analysis. Health Policy. 2001;58:69–81. doi: 10.1016/s0168-8510(01)00143-9. [DOI] [PubMed] [Google Scholar]
- 42.Atre SR, Kudale AM, Morankar SN, Rangan SG, Weiss MG. Cultural concepts of tuberculosis and gender among the general population without tuberculosis in rural Maharashtra, India. Trop Med Int Health. 2004;9:1228–38. doi: 10.1111/j.1365-3156.2004.01321.x. [DOI] [PubMed] [Google Scholar]
- 43.Nair DM, George A, Chacko KT. Tuberculosis in Bombay: new insights from poor urban patients. Health Policy Plan. 1997;12:77–85. doi: 10.1093/heapol/12.1.77. [DOI] [PubMed] [Google Scholar]
- 44.Liefooghe R, Michiels N, Habib S, Moran MB, De Muynck A. Perception and social consequences of tuberculosis: a focus group study of tuberculosis patients in Sialkot, Pakistan. Soc Sci Med. 1995;41:1685–92. doi: 10.1016/0277-9536(95)00129-u. [DOI] [PubMed] [Google Scholar]
- 45.Ganapathy S, Thomas BE, Jawahar MS, Selvi KJ, Sivasubramaniam, Weiss M. Perceptions of gender and tuberculosis in a south Indian urban community. Indian J Tuberc. 2008;55:9–14. [PubMed] [Google Scholar]
- 46.Zhang T, Liu X, Bromley H, Tang S. Perceptions of tuberculosis and health seeking behaviour in rural Inner Mongolia, China. Health Policy. 2007;81:155–65. doi: 10.1016/j.healthpol.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 47.Connolly M, Nunn P. Women and tuberculosis. World Health Stat Q. 1996;49:115–9. [PubMed] [Google Scholar]
- 48.Qureshi SA, Morkve O, Mustafa T. Patient and health system delays: health-care seeking behaviour among pulmonary tuberculosis patients in Pakistan. J Pak Med Assoc. 2008;58:318–21. [PubMed] [Google Scholar]
- 49.Ali SS, Rabbani F, Siddiqui UN, Zaidi AH, Sophie A, Virani SJ, et al. Tuberculosis: do we know enough? A study of patients and their families in an out-patient hospital setting in Karachi, Pakistan. Int J Tuberc Lung Dis. 2003;7:1052–8. [PubMed] [Google Scholar]
- 50.Ottmani S, Obermeyer Z, Bencheikh N, Mahjour J. Knowledge, attitudes and beliefs about tuberculosis in urban Morocco. East Mediterr Health J. 2008;14:298–304. [PubMed] [Google Scholar]
- 51.Eastwood SV, Hill PC. A gender-focused qualitative study of barriers to accessing tuberculosis treatment in The Gambia, West Africa. Int J Tuberc Lung Dis. 2004;8:70–5. [PubMed] [Google Scholar]
- 52.Panic E, Panic I. Some epidemiological and socio-medical peculiarities of pulmonary tuberculosis (pTB) among individuals from war affected areas (WAA)—experiences and results from north-west Yugoslavia (NWYU) Pneumologia. 2003;52:93–8. [PubMed] [Google Scholar]
- 53.Berisha M, Zheki V, Zadzhmi D, Gashi S, Hokha R, Begoli I. Level of knowledge regarding tuberculosis and stigma among patients suffering from tuberculosis. Georgian Med News. 2009;166:89–93. [PubMed] [Google Scholar]
- 54.Panic E, Panic I. Chronic alcoholics' knowledge regarding tuberculosis. Pneumologia. 2001;50:232–5. [PubMed] [Google Scholar]
- 55.Macq J, Solis A, Martinez G. Assessing the stigma of tuberculosis. Psychol Health Med. 2006;11:346–52. doi: 10.1080/13548500600595277. [DOI] [PubMed] [Google Scholar]
- 56.Van Rie A, Sengupta S, Pungrassami P, Balthip Q, Choonuan S, Kasetjaroen Y, et al. Measuring stigma associated with tuberculosis and HIV/AIDS in southern Thailand: exploratory and confirmatory factor analyses of two new scales. Trop Med Int Health. 2008;13:21–30. doi: 10.1111/j.1365-3156.2007.01971.x. [DOI] [PubMed] [Google Scholar]
- 57.Van Brakel WH. Measuring health-related stigma—a literature review. Psychol Health Med. 2006;11:307–34. doi: 10.1080/13548500600595160. [DOI] [PubMed] [Google Scholar]
- 58.Jaramillo E. Pulmonary tuberculosis and health-seeking behaviour: how to get a delayed diagnosis in Cali, Colombia. Trop Med Int Health. 1998;3:138–44. doi: 10.1046/j.1365-3156.1998.00202.x. [DOI] [PubMed] [Google Scholar]
- 59.Liefooghe R, Baliddawa JB, Kipruto EM, Vermeire C, De Munynck AO. From their own perspective. A Kenyan community's perception of tuberculosis. Trop Med Int Health. 1997;2:809–21. doi: 10.1046/j.1365-3156.1997.d01-380.x. [DOI] [PubMed] [Google Scholar]
- 60.Dimitrova B, Balabanova D, Atun R, Drobniewski F, Levicheva V, Coker R. Health service providers' perceptions of barriers to tuberculosis care in Russia. Health Policy Plan. 2006;21:265–74. doi: 10.1093/heapol/czl014. [DOI] [PubMed] [Google Scholar]
- 61.Noyes J, Popay J. Directly observed therapy and tuberculosis: how can a systematic review of qualitative research contribute to improving services? A qualitative meta-synthesis. J Adv Nurs. 2007;57:227–43. doi: 10.1111/j.1365-2648.2006.04092.x. [DOI] [PubMed] [Google Scholar]
- 62.Rubel AJ, Garro LC. Social and cultural factors in the successful control of tuberculosis. Public Health Rep. 1992;107:626–36. [PMC free article] [PubMed] [Google Scholar]
- 63.Coreil J, Lauzardo M, Heurtelou M. Cultural feasibility assessment of tuberculosis prevention among persons of Haitian origin in South Florida. J Immigr Health. 2004;6:63–9. doi: 10.1023/B:JOIH.0000019166.80968.70. [DOI] [PubMed] [Google Scholar]
- 64.Watkins RE, Plant AJ. Pathways to treatment for tuberculosis in Bali: patient perspectives. Qual Health Res. 2004;14:691–703. doi: 10.1177/1049732304263628. [DOI] [PubMed] [Google Scholar]
- 65.Johansson E, Diwan VK, Huong ND, Ahlberg BM. Staff and patient attitudes to tuberculosis and compliance with treatment: an exploratory study in a district in Vietnam. Tuber Lung Dis. 1996;77:178–83. doi: 10.1016/s0962-8479(96)90035-0. [DOI] [PubMed] [Google Scholar]
- 66.Sagbakken M, Frich JC, Bjune GA. Perception and management of tuberculosis symptoms in Addis Ababa, Ethiopia. Qual Health Res. 2008;18:1356–66. doi: 10.1177/1049732308322596. [DOI] [PubMed] [Google Scholar]
- 67.Thorson A, Johansson E. Equality or equity in health care access: a qualitative study of doctors' explanations to a longer doctor's delay among female TB patients in Vietnam. Health Policy. 2004;68:37–46. doi: 10.1016/j.healthpol.2003.07.010. [DOI] [PubMed] [Google Scholar]
- 68.Johansson E, Long NH, Diwan VK, Winkvist A. Gender and tuberculosis control: perspectives on health seeking behaviour among men and women in Vietnam. Health Policy. 2000;52:33–51. doi: 10.1016/s0168-8510(00)00062-2. [DOI] [PubMed] [Google Scholar]
- 69.Hudelson P. Gender differentials in tuberculosis: the role of socio-economic and cultural factors. Tuber Lung Dis. 1996;77:391–400. doi: 10.1016/s0962-8479(96)90110-0. [DOI] [PubMed] [Google Scholar]
- 70.Johansson E, Long NH, Diwan VK, Winkvist A. Attitudes to compliance with tuberculosis treatment among women and men in Vietnam. Int J Tuberc Lung Dis. 1999;3:862–8. [PubMed] [Google Scholar]
- 71.Balasubramanian R, Garg R, Santha T, Gopi PG, Subramani R, Chandrasekaran V, et al. Gender disparities in tuberculosis: report from a rural DOTS programme in south India. Int J Tuberc Lung Dis. 2004;8:323–32. [PubMed] [Google Scholar]
- 72.Reznik M, Ozuah PO. Tuberculin skin testing in children. Emerg Infect Dis. 2006;12:725–8. doi: 10.3201/eid1205.050980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jackson L, Yuan L. Family physicians managing tuberculosis. Qualitative study of overcoming barriers. Can Fam Physician. 1997;43:649–55. [PMC free article] [PubMed] [Google Scholar]
- 74.Suri A, Gan K, Carpenter S. Voices from the field: perspectives from community health workers on health care delivery in rural KwaZulu-Natal, South Africa. J Infect Dis. 2007;196(Suppl 3):S505–11. doi: 10.1086/521122. [DOI] [PubMed] [Google Scholar]
- 75.Naidoo P, Dick J, Cooper D. Exploring tuberculosis patients' adherence to treatment regimens and prevention programs at a public health site. Qual Health Res. 2009;19:55–70. doi: 10.1177/1049732308327893. [DOI] [PubMed] [Google Scholar]
- 76.Edginton ME, Sekatane CS, Goldstein SJ. Patients' beliefs: do they affect tuberculosis control? A study in a rural district of South Africa. Int J Tuberc Lung Dis. 2002;6:1075–82. [PubMed] [Google Scholar]
- 77.Sumartojo E. When tuberculosis treatment fails. A social behavioral account of patient adherence. Am Rev Respir Dis. 1993;147:1311–20. doi: 10.1164/ajrccm/147.5.1311. [DOI] [PubMed] [Google Scholar]
- 78.Ngamvithayapong J, Yanai H, Winkvist A, Saisorn S, Diwan V. Feasibility of home-based and health centre-based DOT: perspectives of TB care providers and clients in an HIV-endemic area of Thailand. Int J Tuberc Lung Dis. 2001;5:741–5. [PubMed] [Google Scholar]
- 79.Dick J, Schoeman JH. Tuberculosis in the community: 2. The perceptions of members of a tuberculosis health team towards a voluntary health worker programme. Tuber Lung Dis. 1996;77:380–3. doi: 10.1016/s0962-8479(96)90106-9. [DOI] [PubMed] [Google Scholar]
- 80.Kiwuwa MS, Charles K, Harriet MK. Patient and health service delay in pulmonary tuberculosis patients attending a referral hospital: a cross-sectional study. BMC Public Health. 2005;5:122. doi: 10.1186/1471-2458-5-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Godfrey-Faussett P, Kaunda H, Kamanga J, van Beers S, van Cleeff M, Kumwenda-Phiri R, et al. Why do patients with a cough delay seeking care at Lusaka urban health centres? A health systems research approach. Int J Tuberc Lung Dis. 2002;6:796–805. [PubMed] [Google Scholar]
- 82.Maamari F. Case-finding tuberculosis patients: diagnostic and treatment delays and their determinants. East Mediterr Health J. 2008;14:531–45. [PubMed] [Google Scholar]
- 83.Cambanis A, Ramsay A, Yassin MA, Cuevas LE. Duration and associated factors of patient delay during tuberculosis screening in rural Cameroon. Trop Med Int Health. 2007;12:1309–14. doi: 10.1111/j.1365-3156.2007.01925.x. [DOI] [PubMed] [Google Scholar]
- 84.Woith WM, Larson JL. Delay in seeking treatment and adherence to tuberculosis medications in Russia: a survey of patients from two clinics. Int J Nurs Stud. 2008;45:1163–74. doi: 10.1016/j.ijnurstu.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 85.Munseri PJ, Talbot EA, Mtei L, Fordham von Reyn C. Completion of isoniazid preventive therapy among HIV-infected patients in Tanzania. Int J Tuberc Lung Dis. 2008;12:1037–41. [PubMed] [Google Scholar]
- 86.Meulemans H, Mortelmans D, Liefooghe R, Mertens P, Zaidi SA, Solangi MF, et al. The limits to patient compliance with directly observed therapy for tuberculosis: a socio-medical study in Pakistan. Int J Health Plann Manag. 2002;17:249–67. doi: 10.1002/hpm.675. [DOI] [PubMed] [Google Scholar]
- 87.Dick J, Van De Walt H. Working with communities. Education and training. AIDS Action. 1996;31:12–3. [PubMed] [Google Scholar]
- 88.Chalco K, Wu DY, Mestanza L, Munoz M, Llaro K, Guerra D, et al. Nurses as providers of emotional support to patients with MDR-TB. Int Nurs Rev. 2006;53:253–60. doi: 10.1111/j.1466-7657.2006.00490.x. [DOI] [PubMed] [Google Scholar]
- 89.Hoa NP, Diwan VK, Co NV, Thorson AE. Knowledge about tuberculosis and its treatment among new pulmonary TB patients in the north and central regions of Vietnam. Int J Tuberc Lung Dis. 2004;8:603–8. [PubMed] [Google Scholar]
- 90.Rajeswari R, Muniyandi M, Balasubramanian R, Narayanan PR. Perceptions of tuberculosis patients about their physical, mental and social well-being: a field report from south India. Soc Sci Med. 2005;60:1845–53. doi: 10.1016/j.socscimed.2004.08.024. [DOI] [PubMed] [Google Scholar]
- 91.Hadley M, Maher D. Community involvement in tuberculosis control: lessons from other health care programmes. Int J Tuberc Lung Dis. 2000;4:401–8. [PubMed] [Google Scholar]
- 92.Macq J, Torfoss T, Getahun H. Patient empowerment in tuberculosis control: reflecting on past documented experiences. Trop Med Int Health. 2007;12:873–85. doi: 10.1111/j.1365-3156.2007.01858.x. [DOI] [PubMed] [Google Scholar]
- 93.Getahun H. Partners against tuberculosis: Ethiopia's “TB clubs”. Afr Health. 1998;21:20. [PubMed] [Google Scholar]
- 94.Demissie M, Getahun H, Lindtjorn B. Community tuberculosis care through “TB clubs” in rural North Ethiopia. Soc Sci Med. 2003;56:2009–18. doi: 10.1016/s0277-9536(02)00182-x. [DOI] [PubMed] [Google Scholar]
- 95.Getahun H, Maher D. Contribution of “TB clubs” to tuberculosis control in a rural district in Ethiopia. Int J Tuberc Lung Dis. 2000;4:174–8. [PubMed] [Google Scholar]
- 96.Macq J, Solis A, Martinez G, Martiny P. Tackling tuberculosis patients' internalized social stigma through patient centred care: an intervention study in rural Nicaragua. BMC Public Health. 2008;8:154. doi: 10.1186/1471-2458-8-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Liefooghe R, Suetens C, Meulemans H, Moran MB, De Muynck A. A randomised trial of the impact of counselling on treatment adherence of tuberculosis patients in Sialkot, Pakistan. Int J Tuberc Lung Dis. 1999;3:1073–80. [PubMed] [Google Scholar]
- 98.Bertrand JT, O'Reilly K, Denison J, Anhang R, Sweat M. Systematic review of the effectiveness of mass communication programs to change HIV/AIDS-related behaviors in developing countries. Health Educ Res. 2006;21:567–97. doi: 10.1093/her/cyl036. [DOI] [PubMed] [Google Scholar]
- 99.O'Leary A, Kennedy M, Pappas-DeLuca KA, Nkete M, Beck V, Galavotti C. Association between exposure to an HIV story line in “The Bold and the Beautiful” and HIV-related stigma in Botswana. AIDS Educ Prev. 2007;19:209–17. doi: 10.1521/aeap.2007.19.3.209. [DOI] [PubMed] [Google Scholar]