SYNOPSIS
Objective
We conducted an analysis of rates, geographic distribution, and time to treatment of chlamydia, gonorrhea, and early syphilis (ES) among Arizona American Indians (AIs) to address racial disparities affecting this group.
Methods
We used the Arizona Department of Health Services' sexually transmitted disease (STD) surveillance database to identify STD cases and calculate rates among AIs in Arizona from 2003 to 2007. We mapped AI ES cases reported during that time frame by reported resident ZIP code, calculated days elapsed from specimen collection to initial treatment, and compared rates and time to treatment for AIs with those of non-Hispanic white (NHW) individuals.
Results
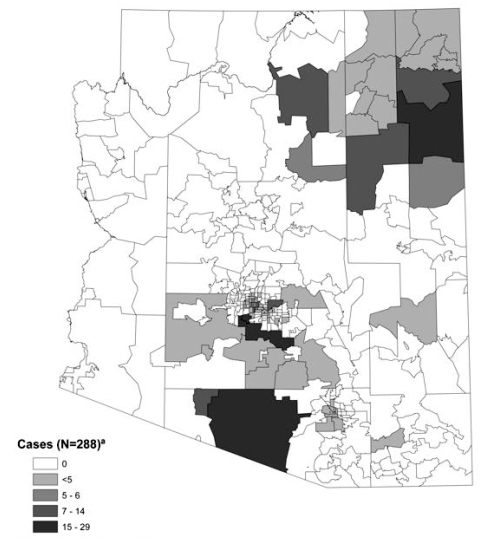
Annual Arizona AI STD rates for chlamydia, gonorrhea, and ES from 2003 to 2007 ranged from 2.7 to 7.8 times those of NHW people. During the same time period, the annual rates for all three STDs among adolescents aged 15 to 19 years were also higher among AIs and ranged from 2.0 to 14.8 times those of NHW individuals. The majority of cases for ES reported ZIP codes located in the northeastern and southern central portions of the state. The median time to treatment in AI populations was significantly longer than in NHW populations for chlamydia and gonorrhea, but not for ES.
Conclusions
High rates of STDs have been identified among AIs in certain regions of Arizona. Additionally, there are significant delays in treatment for gonorrhea and chlamydia. STD prevention and education programs that prioritize this health disparity and promote expeditious screening, diagnosis, and treatment are needed.
Sexually transmitted diseases (STDs) remain a serious, but often disregarded, public health threat in the U.S., with significant physical and economic repercussions. Untreated STDs can result in chronic pelvic pain, infertility, ectopic pregnancies, fetal demise, premature deliveries, cardiac and neurologic deficits, and death.1,2 Additionally, many STDs are asymptomatic, leaving individuals unaware that they are infected.1–3 For this reason, these infections frequently remain undetected and are quickly passed to others, including fetuses. It has been estimated that the annual direct medical costs of STDs, including human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS), in the U.S. can extend to more than several billion dollars.3,4
Even more troublesome is that certain populations carry a much larger burden of this “hidden epidemic” than others.1 Included among these are American Indian (AI) populations.5,6 The national rates among AIs/Alaska Natives for chlamydia, gonorrhea, and syphilis are two to six times the comparable rates for non-Hispanic white (NHW) people.6,7 In addition, several studies have raised a concern about racial misclassification of AIs in multiple disease-surveillance databases, including those for STDs and HIV.8,9 These studies suggest that rates in AI populations are frequently underestimated. An examination of the Oklahoma state STD surveillance system, for example, found that accounting for racial misclassification increased chlamydia rates by 32%, gonorrhea rates by 57%, and syphilis rates by 27%.8 A second study looking at HIV/AIDS reporting systems in five states and one urban health center from 1984 to 2002 found that the percentages of AIs being misclassified as non-AI ranged from nearly 4% to 55%.9
The southwestern region of the U.S. has the largest population of AIs by region and has experienced particularly high STD rates. For example, in 2004, 92% of all the primary and secondary syphilis cases among AIs in the U.S. occurred in three Indian Health Service (IHS) Areas located in the southwest region—Navajo, Phoenix, and Albuquerque.6 Arizona contains portions of two of these Areas—Phoenix and Navajo. In addition, the IHS Tucson Area is located in its entirety within the south-central portion of the state.6 In 2007 and 2008, this Area experienced a syphilis outbreak among a large AI tribe.10,11 Although African Americans had the highest rates of both chlamydia and gonorrhea in Arizona during 2007, AIs had the second-highest rate of chlamydia (649 per 100,000 population) and the second-highest rate of gonorrhea (95 per 100,000 population) when compared with all other racial/ethnic groups. These rates were 1.7 and 1.2 times the overall state rates for chlamydia and gonorrhea, respectively.10
Significant racial disparities among STD case rates have persisted in Arizona. These racial disparities occur among individuals with reported chlamydia, gonorrhea, and syphilis infections, and AI populations in Arizona are greatly affected.10 To more clearly evaluate and better address these particular racial disparities, we performed a comparison of STD rates, geographic distribution, and time to treatment to inform surveillance, prevention, and education efforts.
METHODS
Disease rates
In Arizona, physicians and laboratories are mandated by state rule (recorded in the Arizona Administrative Code) to report certain STDs within five working days after a case or suspect case is diagnosed, treated, or detected to the local health agency and the Arizona Department of Health Services (ADHS).12 The STDs (excluding HIV) that must be reported are chancroid, chlamydia, gonorrhea, genital herpes, and syphilis. ADHS maintains these data for state and local STD surveillance. We calculated rates for chlamydia, gonorrhea, and syphilis from this STD surveillance database for the years 2003–2007. We excluded herpes from this analysis, considering the lack of reliability in the database due to infrequency of provider reporting of this primarily clinical disease. Chancroid was excluded from the analysis as there were no cases reported in Arizona during the years evaluated.
For rate analyses, the total number of cases by race/ethnicity was first separated by disease: gonorrhea, chlamydia, and early syphilis (ES) (individuals with syphilis for less than one year). We then quantified each disease by year of diagnosis. The year of diagnosis was defined as the year of positive-specimen collection for each disease episode. Population denominators by race/ethnicity were obtained from the ADHS Office of Vital Statistics.13 Due to the known high rates of STDs among adolescents in Arizona, we completed the rate analysis twice—(1) all ages of cases combined and (2) cases of those aged 15 to 19 years at the time of positive STD collection—for comparison of adolescent rate trends by race.10 Arizona population denominators were not evaluated in five-year intervals by race/ethnicity until 2004.13 As a result, we used the appropriate 2004 population denominator to calculate 2003 rates. These analyses were conducted for disease surveillance purposes and, thus, did not require human subjects review.
Race classification
ADHS collects race/ethnicity information for reportable STDs according to national census guidelines, with race and ethnicity collected and coded separately. AIs were defined as those in the database who were race-coded as “AI/Alaska Native.” We also included individuals who were coded as unknown race but whose provider for the collection of the STD test was recorded as an IHS clinic or hospital as AI, based on the requirement of patients to present evidence of AI heritage when receiving care from IHS facilities.9 Individuals who were race-coded as AI and ethnicity-coded as Hispanic were included as AI. In addition, we included as AI individuals recorded with more than one race, with one of those races being AI. NHW cases were defined according to standard ADHS protocol as those cases in the ADHS STD database race-coded as white and ethnicity-coded as either non-Hispanic or unknown, given their having been identified as white race. We did not include individuals in the database who were recorded with more than one race, with one of those races being white, in the non-Hispanic group.
For disease-rate calculations only, STD cases with unknown race were redistributed according to the Centers for Disease Control and Prevention (CDC) STD surveillance guidelines for states with less than 50% missing race.6 For example, with chlamydia in the NHW population during 2003, there were 3,995 cases reported, representing 24% of the state's 17,031 total cases for the year. In 2003 in Arizona, there were also 3,057 cases reported with unknown race. As a result, 24% of the cases with unknown race (3,057 × 0.2346 = 717 cases) were added to the NHW cases to obtain the total number of NHW cases for the year when determining the annual chlamydia rate.
Geographic distribution of syphilis
We selected and mapped geographically all ES cases among AIs where the positive specimen-collection date occurred from 2003 to 2007 using the Environmental Systems Research Institute's (ESRI's) 2007 Arizona ZIP-code pattern, encompassed in the ArcGIS™ 9.3.1 software.14 The ZIP code-of-residence database among new cases of syphilis in Arizona is nearly complete, as these cases are located, investigated, and interviewed by public health disease-intervention specialists. Due primarily to a lack of resources and an abundance of STD morbidity in the state, individuals diagnosed with new cases of chlamydia and gonorrhea are, in general, not interviewed. As a result, the reliability and completeness of the ZIP code-of-residence databases for these two diseases are lower. For this reason, we did not include mapping of the geographic distribution of residence among new chlamydia and gonorrhea cases in this analysis.
We completed counts for each ZIP code of residence reported and recorded in the database. ZIP codes for post office boxes were added to the ZIP code of the area in which the post office is located using the ESRI Arizona ZIP-code/post office-box pattern. We then plotted the total count for each area ZIP code to the 2007 Arizona ZIP-code pattern. We determined classification breaks using the Jenks Natural Breaks Method,15 completed by the ArcGIS 9.3.1 mapping software. ZIP codes with fewer than five cases were presented as one classification group to preserve confidentiality.
Time-to-treatment analysis
We calculated and compared the time from specimen collection to treatment among chlamydia, gonorrhea, and syphilis cases collected in 2007 for the AI and NHW populations in Arizona, identified as described previously. CDC uses the time-to-treatment index as a national program performance measure, as a shorter time to treatment may decrease the probability of disease-related complications as well as disease transmission.16
We calculated the number of days from the positive-specimen collection date to the treatment date (time to treatment) for each racial group and disease (gonorrhea, chlamydia, and ES). Time to treatment was then grouped into intervals consistent with CDC performance-measure guidance: within seven days (0–7 days), within 14 days (0–14 days), within 30 days (0–30 days), and more than 30 days (>30 days). We also quantified cases with missing treatment data by racial group. Percentages of the total number of cases for each time category and median number of days from specimen collection to treatment were calculated and compared by racial group.
Statistical analysis
Unless otherwise noted, analyses were performed using SAS® version 9.2.17 Geographic distribution was completed using ESRI's ArcMap™ 9.3.1 mapping software and map databases.14 We performed a Kruskal-Wallis test of medians for time to treatment in days using SPSS® version 16.18
RESULTS
Disease rates
Our analysis found that 15,291 chlamydia cases, 2,537 gonorrhea cases, and 309 ES cases among AIs were reported in Arizona from 2003 to 2007 (Table 1). Among these cases, 79% of chlamydia cases, 79% of gonorrhea cases, and 69% of ES cases were diagnosed at an IHS clinic or hospital (data not shown). Of the total cases among AIs, less than 10% were included as a result of having been seen at an IHS facility without having been race-coded as AI. This was true for chlamydia (8%), gonorrhea (9%), and ES (5%) (Table 1).
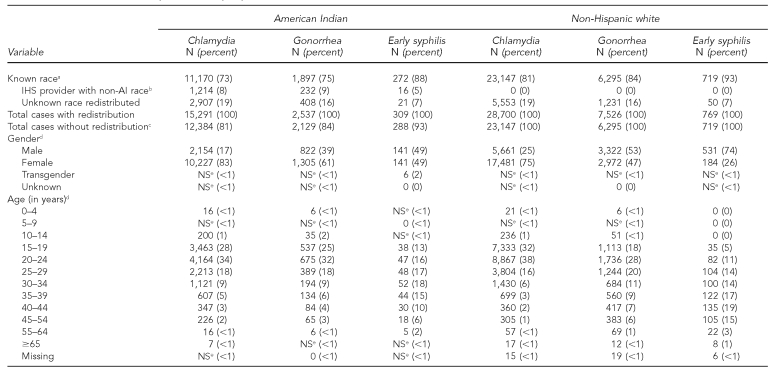
Table 1.
Demographics of chlamydia, gonorrhea, and early syphilis cases diagnosed among American Indians and non-Hispanic white people in Arizona, 2003–2007
aRace information available
bRace recorded in database as either unknown or something other than AI and diagnosed at an IHS-supported facility
cUsed to calculate percentages of total cases with gender and age analysis
dDoes not include redistributed cases with unknown race
eNumber of cases ≤4
IHS = Indian Health Service
AI = American Indian
NS = not significant
For all three diseases, the distribution by gender showed a smaller ratio of male-to-female cases among AIs as compared with NHW individuals. That is, of the total number of cases with each of the three diseases, a greater proportion of AI women were reported to have these infections than NHW women. With ES in particular, the male-to-female ratio was 1:1 (141 cases among males vs. 141 cases among females) among AIs but nearly 3:1 (531 cases among males vs. 184 cases among females) among NHW individuals (Table 1).
Minimal differences between the AI and NHW groups were noted in the age distribution of chlamydia and gonorrhea cases. However, for ES, nearly 30% of the AI cases were diagnosed among people younger than 25 years of age, as compared with 16% of ES cases among those identified as NHW (Table 1).
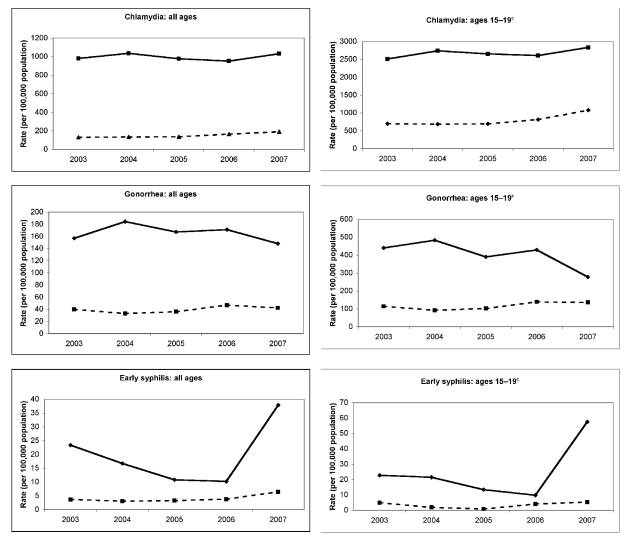
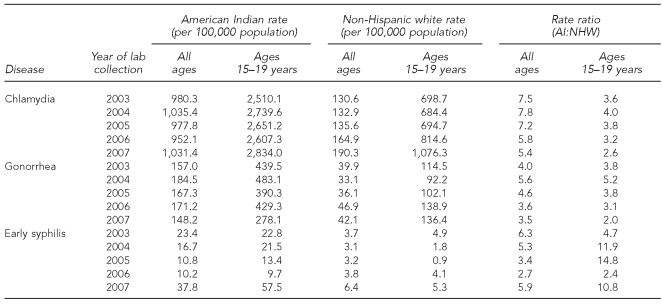
The rates for all three STDs were higher among AIs than NHW people in Arizona from 2003 to 2007 (Figure 1). For chlamydia, the AI-to-NHW rate ratio ranged from 5.4 to 7.8, with the largest rate ratio calculated for 2004 (Table 2). With gonorrhea, the AI-to-NHW rate ratio ranged from 3.5 to 5.6. Rates of ES among AIs during this time period were 2.7 to 6.3 times the rates among NHW individuals. The highest rate of ES among AIs occurred during 2007, when the rate reached 37.8 cases per 100,000 population, compared with the NHW rate of 6.4 cases per 100,000 population (Table 2). A large increase in ES rates from 2006 to 2007 reflects several syphilis outbreaks among AIs throughout the state, which began in late 2006.10
Figure 1.
Chlamydia, gonorrhea, and early syphilis ratesa among American Indians and non-Hispanic white people by all ages and by those aged 15–19 years in Arizona, 2003–2007b
aThe solid line demonstrates rates among American Indians; the broken line demonstrates rates among non-Hispanic white people.
bArizona Department of Health Services, Bureau of Public Health Statistics, Health Status and Vital Statistics Section. Population denominators [cited 2010 Jan 28]. Available from: URL: http://azdhs.gov/plan/menu/info/pd.htm
cThe population denominator for young people aged 15–19 years by race/ethnicity was not available for 2003. As a result, 2003 adolescent rates were calculated using the 2004 population denominator.
Table 2.
Annual rates and rate ratios of chlamydia, gonorrhea, and early syphilis among American Indians and non-Hispanic white people in Arizona, 2003–2007
AI = American Indian
NHW = non-Hispanic white
Chlamydia, gonorrhea, and syphilis rates among adolescents aged 15 to 19 years from 2004 to 2007 were similarly consistently higher for AIs than for NHW people (Figure 1). With chlamydia, the annual rate ratio of AIs to NHW individuals ranged from 2.6 to 4.0, and the rate among AI adolescents increased from 2,510.1 per 100,000 population to 2,834.0 per 100,000 population from 2003 to 2007 (Table 2). Annual gonorrhea AI-to-NHW rate ratios ranged from 2.0 in 2007 to 5.2 in 2004. Annual ES AI-to-NHW rate ratios ranged from 2.4 in 2006 to 14.8 in 2005, with the highest rates of ES among AIs occurring in 2007 at 57.5 cases per 100,000 population, compared with 5.3 cases per 100,000 population among NHW people for that same year (Table 2).
Time to treatment
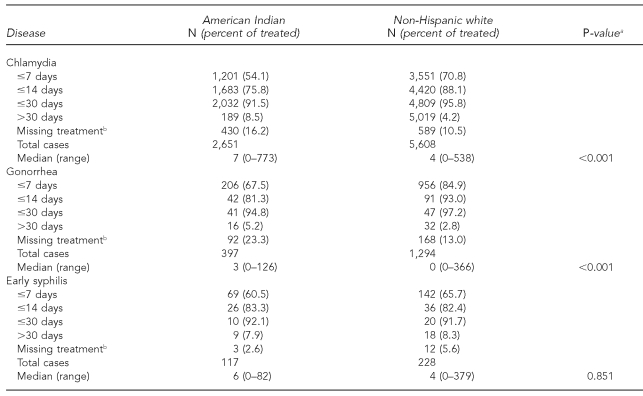
The median time to treatment for chlamydia and gonorrhea was significantly longer for AIs than for NHW individuals (Table 3). For chlamydia, the median time to treatment for AIs was seven days, with a range of 0–773 days, compared with NHW people, whose median time to treatment was four days, with a range of 0–538 days (Kruskal-Wallis one-way analysis of variance, p<0.001). For gonorrhea, the AI median treatment occurred in three days (range 0–126 days), and the NHW median treatment occurred at zero days (range 0–366 days). The median time to treatment for ES was not significantly longer for AIs (median six days, range 0–82 days) than for NHW individuals (median four days, range 0–379 days, p=0.851).
Table 3.
Time to treatment for reported chlamydia, gonorrhea, and early syphilis among American Indians and non-Hispanic white people in Arizona, 2007
aKruskal-Wallis one-way analysis of variance
bMissing treatment percentages calculated from total cases—treated and untreated
Geographic distribution of cases
The geographic distribution of ES cases among Arizona AIs by reported ZIP code of residence from 2003 to 2007 is shown in Figure 2. The majority of cases were distributed in the central-southern, central, and northeastern portions of the state.
Figure 2.
Reported early syphilis cases among American Indians in Arizona, 2003–2007
aIncludes five cases with unknown ZIP code
DISCUSSION
Disparities exist in the diagnoses of STDs in Arizona and are particularly notable for some racial/ethnic groups, including AIs. These disparate rates of STDs among Arizona AIs have persisted for more than 10 years.10 In addition, chlamydia positivity rates among AIs from CDC and the Office of Population Affairs' Infertility Prevention Project have shown a rate of nearly 10% in Region IX, which includes Arizona, California, Hawaii, and Nevada.19 The differences shown in our study in overall STD rates and adolescent rates for chlamydia, gonorrhea, and ES, and for median interval to treatment for chlamydia and gonorrhea, demonstrate disease rate inequalities. The geographic assignment of cases by ZIP code showed the regions of the state where the majority of these reported STD cases among Arizona AIs reside. These analytic methods have expanded the use of state surveillance systems in the identification of racial/ethnic determinants of diagnosis, residence, and clinical-care outcomes for AIs in Arizona.
For all three diseases, women represented a larger proportion of all AIs infected, compared with the NHW cases, by gender. The male/female ratio (1:1 in AIs vs. 3:1 in NHW people) was greatest with ES, reflecting high rates of syphilis among men who have sex with men in urban regions of Arizona.10 Our results support a more heterosexual pattern of syphilis transmission among Arizona AIs, compared with the remainder of the state.
This analysis of surveillance data found much higher rates of chlamydia, gonorrhea, and ES among AIs compared with NHW people in Arizona. AI adolescents and young adults bear the burden of these STDs. Higher rates of STDs among AIs/Alaska Natives have been reported in multiple geographic regions of the U.S.6,7,20 Contributors to these differences in rates have been found to include the high STD prevalence in the population and behavioral risk factors.20–26 In addition, IHS-supported health-care facilities in Arizona, serving members of 21 federally recognized tribes,27,28 perform chlamydia screening as a routine part of health care for women, possibly leading to increased case identification in AI populations.6 In Arizona, high rates of STDs among AI populations have decreased coincident with outbreak-response activities of increased community awareness, targeted surveillance, partner services, and expanded prevention, screening, and treatment activities with a special focus on adolescents and young adults at the local tribal level.10,29,30 This service delivery will be continued and expanded in Arizona with input from IHS and tribal representatives.10,31
The geographic distribution of ES cases showed that cases were predominantly located in urban regions and specific tribal areas. These cases from 2003 to 2008 primarily reflect syphilis outbreaks that occurred in three, large AI tribal areas beginning in 2006. Geographic distribution methods that included AIs have been used previously to identify areas with high STD morbidity.6 Distributing cases based on ZIP code of residence can identify areas experiencing the emergence of syphilis and possibly other STDs. The diagnosis of STDs among cases residing in close proximity may not be identified through surveillance methods monitoring case counts by sentinel sites. Concerns for confidentiality in rural areas may influence tribal members to seek care outside of their local health-care systems. In this analysis, 21% of AI cases for all three diseases combined (excluding cases with unknown race, which were redistributed) were diagnosed in non-IHS facilities (data not shown). Geographic distribution can be used to detect the emergence of STDs in regions where multiple provider systems are accessed by tribal members. This method should be considered as a part of outbreak surveillance in rural regions of the U.S. with emergent syphilis.
The median number of days from testing to treatment for chlamydia and gonorrhea was significantly greater among AIs than NHW people in Arizona. Evaluating and reporting differences in time to treatment is a required national performance measure for STD programs; however, differences by race/ethnicity are not included.16 Differences in time to treatment for STDs have been reported from other sites, but not by race/ethnicity. Delayed treatment may be influenced by several time intervals: specimen collection to analysis, specimen analysis to results delivery, results reported to the patient, and the patient returning for treatment.32,33 In Arizona, a longer time to patient follow-up for treatment among AIs may be affected by geographic distances to health-care facilities, population mobility, perceived lack of confidentiality, varying relationships between county and state health departments, medical provider turnover at IHS facilities, and other social conditions that affect health-care seeking behavior, such as substance abuse.5,30,34
Our analyses also found that the median time to treatment was not significantly greater for AIs with ES. In 2007 in Arizona, many of these ES cases occurred during outbreaks at a time when higher priority was given to case investigation and partner management of syphilis cases. In addition, during this period of outbreak response, providers were encouraged to provide presumptive treatment for patients with symptoms of syphilis. This period of heightened awareness likely contributed positively toward that more rapid treatment of syphilis cases, compared with chlamydia and gonorrhea.
Delays in time to treatment may result in increased disease transmission and development of complications of untreated infections. Agencies and health-care facilities delivering clinical care to AI populations should consider the use of standard guidelines that include empiric treatment of partners, expedited partner therapy, expanded partner services, and the presumptive treatment of symptomatic patients to improve this clinical-care outcome. In addition, further investigations should focus on the cause and impact of these treatment delays.
Limitations
Several limitations are inherent in these analyses. Reliance on surveillance data for these calculations may not reflect the actual rates, due to incomplete or inaccurate reporting of race, treatment, and patient-location information. For example, STD reporting forms and database categories combine AIs with Alaska Natives. Although it is presumed that the population of Alaska Natives living in Arizona is very small, this combined race classification could have led to a small overestimation in the number of reported cases among AIs. In addition, including cases coded as white race and unknown Hispanic ethnicity as NHW could have overestimated the NHW cases and rates. Assignment of AI race to patients diagnosed in an IHS-supported facility may have resulted in an overestimation of AI STD cases and rates. However, of the 10,575 cases of chlamydia, gonorrhea, and ES with known race diagnosed among patients seen at IHS clinics or hospitals from 2003 to 2007, only 403 people (4%) were coded in the database as a race other than AI. In addition, as discussed previously, the racial misclassification of AIs has been shown to occur in areas of the country, leading to the underestimation of disease rates.8,9
In Arizona, some AIs with syphilis who reside in tribal regions bordering Mexico have been misclassified as Hispanic, possibly as a result of surnames that are of Hispanic origin. Of those of known race diagnosed at an IHS center and not coded as AI, 60% were coded as Hispanic. As a result, overestimation of AI cases by including all cases diagnosed at IHS clinics and hospitals is likely minimal. Screening opportunities among AIs may be greater than in NHW individuals, and this may be reflected in the higher rates of chlamydia and gonorrhea for this group (especially for females).
Geographic distribution of cases may be limited by the accuracy and availability of recorded ZIP-code data. This limitation is likely minimal with ES, as each case was investigated, and demographic information, including zip code, was missing in only five out of the 288 ES cases reported among AIs in Arizona from 2003 to 2007 (Figure 2). In addition, post office boxes were assigned to the area ZIP code in which they exist and may not represent the true ZIP code of residence of some cases.
Time to treatment may be influenced by specimen-analysis and results-reporting intervals and not patient or provider factors; however, we assumed this bias to be equal across the comparison groups. Missing treatment information may reflect a lack of provider reporting and not untreated cases. From 2003 to 2007, for all Arizona STD cases, 14% of chlamydia, 13% of gonorrhea, and less than 1% of ES cases did not include a provider report, which would include treatment, in the state database. A final limitation to this study was that historical and social systems factors were not available, due to the use of health department surveillance data.
CONCLUSIONS
Elevated rates of STDs in AIs may reflect increased opportunities for testing, limited STD-prevention activities, limited STD-education opportunities, or other socioeconomic determinants of health. To address this health disparity in Arizona, the ADHS has used these findings to identify targets for provider, community, and individual health education through local media and multiple on-site training efforts. In addition, ADHS has worked closely with tribes experiencing increasing syphilis rates to provide specialized clinical consultation and focused case-management services. ADHS will continue to address this health disparity by working with IHS and tribal health agencies to develop and implement a standard clinical protocol for screening, diagnosing, and treating STDs, and to expand local IHS and tribal capacity through the delivery of nationally sponsored STD disease-investigation training. Continued targeted surveillance will be used to inform the allocation of state and federal resources to address this issue. Other regions should consider the use of these types of analyses to identify disparities in diagnoses, geographical distribution, and clinical services for populations with high or emergent STD rates.
Footnotes
This article was supported by Cooperative Agreement #1H25PS001385-01 from the Centers for Disease Control and Prevention (CDC). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of CDC.
REFERENCES
- 1.Centers for Disease Control and Prevention (US) Tracking the hidden epidemics: trends in STDs in the United States, 2000. Atlanta: CDC; 2000. [Google Scholar]
- 2.Executive summary. Committee on Prevention and Control of Sexually Transmitted Diseases, Institute of Medicine. In: Eng TR, Butler WT, editors. The hidden epidemic confronting sexually transmitted diseases. National Academy Press; 1997. pp. 1–18. [Google Scholar]
- 3.Weinstock H, Berman S, Cates W., Jr Sexually transmitted diseases among American youth: incidence and prevalence estimates 2000. Perspect Sex Reprod Health. 2004;36:6–10. doi: 10.1363/psrh.36.6.04. [DOI] [PubMed] [Google Scholar]
- 4.Chesson HW, Blandford JM, Gift TL, Tao G, Irwin KL. The estimated direct medical cost of sexually transmitted diseases among American youth, 2000. Perspect Sex Reprod Health. 2004;36:11–9. doi: 10.1363/psrh.36.11.04. [DOI] [PubMed] [Google Scholar]
- 5.Kaufman CE, Shelby L, Mosure DJ, Marrazzo J, Wong D, de Ravello L, et al. Within the hidden epidemic: sexually transmitted diseases and HIV/AIDS among American Indians and Alaska Natives. Sex Transm Dis. 2007;34:767–77. doi: 10.1097/01.olq.0000260915.64098.cb. [DOI] [PubMed] [Google Scholar]
- 6.Wong D, Swint E, Paisano EL, Cheek JE. Indian health surveillance report—sexually transmitted diseases 2004. Atlanta: CDC and Indian Health Service (US); 2006. [cited 2010 Feb 3]. Also available from: URL: http://www.cdc.gov/std/stats-ihs-2004/IHS-STD-Report-2004.pdf. [Google Scholar]
- 7.CDC (US) Sexually transmitted disease surveillance 2007. Atlanta: CDC; 2008. [Google Scholar]
- 8.Thoroughman DA, Frederickson D, Cameron HD, Shelby LK, Cheek JE. Racial misclassification of American Indians in Oklahoma State surveillance data for sexually transmitted diseases. Am J Epidemiol. 2002;155:1137–41. doi: 10.1093/aje/155.12.1137. [DOI] [PubMed] [Google Scholar]
- 9.Bertolli J, Lee LM, Sullivan PS AI/AN Race/Ethnicity Data Validation Workgroup. Racial misidentification of American Indians/Alaska Natives in the HIV/AIDS Reporting Systems of five states and one urban health jurisdiction, U.S., 1984–2002. Public Health Rep. 2007;122:382–92. doi: 10.1177/003335490712200312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arizona Department of Health Services, Office of HIV, STD and Hepatitis Services, STD Control Program. Arizona STD annual report. 2008. [cited 2010 Jan 28]. Available from: URL: http://www.azdhs.gov/phs/oids/std/pdf/Arizona%20STD%20Annual%20Report%202008.pdf.
- 11.CDC, Indian Health Service (US) Indian health surveillance report—sexually transmitted diseases 2007. Atlanta: CDC and IHS; 2009. [cited 2010 Feb 3]. Also available from: URL: http://www.cdc.gov/std/stats/IHS/IHS-SurvRpt_Web508Nov2009.pdf. [Google Scholar]
- 12.Arizona Administrative Code. A.A.C. R9-6-202 and A.A.C R9-6-204. [cited 2010 Jan 28]. Available from: URL: http://www.azsos.gov/public_services/Title_09/9-06.htm#Article_2.
- 13.Arizona Department of Health Services, Bureau of Public Health Statistics, Health Status and Vital Statistics Section. Population denominators. [cited 2010 Jan 28]. Available from: URL: http://azdhs.gov/plan/menu/info/pd.htm.
- 14.Environmental Systems Research Institute, Inc. ArcGIS™ 9.3.1. Redlands (CA): ESRI; 2008. [Google Scholar]
- 15.Environmental Systems Research Institute, Inc. Introduction to map design. [cited 2010 Jan 28]. Available from: URL: http://www.esri.com/industries/k-12/PDFs/intrcart.pdf.
- 16.CDC (US), National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Division of STD Prevention. 2007 performance measures. Atlanta: CDC; 2006. [cited 2010 Jan 28]. Also available from: URL: http://www.cdc.gov/STD/program/PMList2007.pdf. [Google Scholar]
- 17.SAS Institute, Inc. SAS®: Version 9.2. Cary (NC): SAS Institute, Inc; 2005. [Google Scholar]
- 18.SPSS, Inc. SPSS®: Version 16. Chicago: SPSS, Inc; 2007. [Google Scholar]
- 19.CDC (US), National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Division of STD Prevention. STDs in ethnic and racial minorities: sexually transmitted disease surveillance 2007. [cited 2009 Apr 17]. Available from: URL: http://www.cdc.gov/std/stats07/slides/minorities.ppt.
- 20.Gorgos L, Fine D, Marrazzo J. Chlamydia positivity in American Indian/Alaska Native women screened in family planning clinics, 1997–2004. Sex Transm Dis. 2008;35:753–7. doi: 10.1097/OLQ.0b013e31816d1f7d. [DOI] [PubMed] [Google Scholar]
- 21.Kaufman CE, Desserich J, Big Crow CK, Holy Rock B, Keane E, Mitchell CM. Culture, context, and sexual risk among Northern Plains American Indian youth. Soc Sci Med. 2007;64:2152–64. doi: 10.1016/j.socscimed.2007.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Walters KL, Simoni JM, Evans-Campbell T. Substance use among American Indians and Alaska Natives: incorporating culture in an “indigenist” stress-coping paradigm. Public Health Rep. 2002;117(Suppl 1):S104–17. [PMC free article] [PubMed] [Google Scholar]
- 23.Hellerstedt WL, Peterson-Hickey M, Rhodes KL, Garwick A. Environmental, social, and personal correlates of having ever had sexual intercourse among American Indian youths. Am J Public Health. 2006;96:2228–34. doi: 10.2105/AJPH.2004.053454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Spear S, Longshore D, McCaffrey D, Ellickson P. Prevalence of substance use among white and American Indian young adolescents in a Northern Plains state. J Psychoactive Drugs. 2005;37:1–6. doi: 10.1080/02791072.2005.10399743. [DOI] [PubMed] [Google Scholar]
- 25.Arizona Department of Education, Standards and Assessment Division, School Safety and Prevention. 2007 youth risk behavior survey results. [cited 2010 Jan 28]. Available from: URL: http://www.ade.az.gov/sa/health/matrix/2007AZBHSummaryTables.pdf.
- 26.Denny CH, Holtzman D, Cobb N. Surveillance for health behaviors of American Indians and Alaska Natives. Findings from the Behavioral Risk Factor Surveillance System, 1997–2000. MMWR Surveill Summ. 2003;52(7):1–13. [PubMed] [Google Scholar]
- 27.National Conference of State Legislatures. Federal and state recognized tribes. [cited 2010 Jan 28]. Available from: URL: http://www.ncsl.org/?tabid=13278.
- 28.Department of Health and Human Services, Indian Health Service (US) Area offices and facilities. [cited 2010 Jan 28]. Available from: URL: http://www.ihs.gov/index.cfm?module=AreaOffices.
- 29.Reilley B, Redd J, Kittredge J, Speakman R, Bigbey M, Giberson S. Expanded HIV testing in two service units, July–December 2007. The IHS Prim Care Provid. 2009;34:37–41. [Google Scholar]
- 30.Syphilis outbreak among American Indians—Arizona, 2007–2009. MMWR Morb Mortal Wkly Rep. 2010;59(6):158–61. [PMC free article] [PubMed] [Google Scholar]
- 31.Allison MT, Rivers PA, Fottler MD. Future public health delivery models for Native American tribes. Public Health. 2007;121:296–307. doi: 10.1016/j.puhe.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 32.Wong D, Berman SM, Furness BW, Gunn RA, Taylor M, Peterman TA. Time to treatment for women with chlamydial or gonococcal infections: a comparative evaluation of sexually transmitted disease clinics in 3 US cities. Sex Transm Dis. 2005;32:194–8. doi: 10.1097/01.olq.0000154494.95138.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen SY, Johnson M, Sunenshine R, England B, Komatsu K, Taylor MM. Missed and delayed syphilis treatment and partner elicitation: a comparison between STD clinic and non-STD clinic patients. Sex Transm Dis. 2009;36:445–51. doi: 10.1097/OLQ.0b013e3181a2aa95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.CDC (US) HIV/AIDS among American Indians and Alaska Natives. CDC HIV/AIDS fact sheet. [cited 2009 Apr 27]. Available from: URL: http://www.cdc.gov/hiv/resources/factsheets/PDF/aian.pdf.