SYNOPSIS
Objective
Few studies have examined the extent to which foreign-born people contribute to the human immunodeficiency virus (HIV) epidemic among non-Hispanic black people in the U.S. We sought to determine differences in the epidemiology of HIV infection among native- and foreign-born black people, using data from the national HIV surveillance system of the Centers for Disease Control and Prevention.
Methods
We estimated the number of HIV infections among black adults and adolescents diagnosed from 2001 to 2007 in 33 U.S. states. We compared annual HIV diagnosis rates, distributions of demographic characteristics and HIV-transmission risk factors, late diagnoses of HIV infection, and survival after an acquired immunodeficiency syndrome (AIDS) diagnosis for native- and foreign-born black people.
Results
From 2001 to 2007, an estimated 100,013 black adults and adolescents were diagnosed with HIV infection in 33 U.S. states, for which country-of-birth information was available. Of these, 11.7% were foreign-born, with most from the Caribbean (54.1%) and Africa (41.5%). Annual HIV diagnoses decreased by 5.5% per year (95% confidence interval [CI] −5.9, −5.0) among native-born black people. Decreases were small among foreign-born black people (−1.3%; 95% CI −2.6, −0.1), who were more likely to be female, have HIV infection attributable to high-risk heterosexual contact, be diagnosed with AIDS within 12 months of HIV diagnosis, and survive one year and three years after an AIDS diagnosis.
Conclusions
The epidemiology of HIV infection differs for foreign-born black individuals compared with their native-born counterparts in the U.S. These data can be used to develop culturally appropriate and relevant HIV-prevention interventions.
The human immunodeficiency virus (HIV) pandemic affects alarming numbers of people around the world. For more than 20 years, national HIV/acquired immunodeficiency syndrome (AIDS) surveillance data have demonstrated that non-Hispanic black people are disproportionately affected by HIV in the United States.1–4 These numbers have remained constant despite national efforts to prevent transmission in this population.5–7 Analysis of national HIV surveillance data has also shown that the percentage of annual HIV diagnoses among foreign-born people in the U.S. is growing.8,9 Despite this increase, few studies have examined HIV rates among the foreign-born black population.10–13 More importantly, few studies have examined HIV-transmission risk factors among foreign-born black populations, which may differ from those among native-born black populations. Models examining social determinants of health include community and societal characteristics as a component.14,15 Multiple studies have shown the plausibility of a causal affect between community and societal characteristics and health outcomes.14 An understanding of the differences among U.S. black people of different national origins is needed to guide development of effective health interventions for these groups.
The Centers for Disease Control and Prevention (CDC) provides national population-based monitoring of the HIV epidemic in the U.S.; however, data for native- and foreign-born black populations are typically combined in surveillance reports. These aggregate data may mask important variations in the epidemiology of HIV among black people, related to place of birth. Using data from CDC's national HIV surveillance system, we examined differences in annual rates of HIV diagnosis, distributions of demographic characteristics and HIV-transmission risk factors, late diagnoses of HIV infection, and survival after an AIDS diagnosis for native- and foreign-born black people.
METHODS
We analyzed data reported to CDC for adults and adolescents diagnosed with HIV infection (with or without AIDS) from 2001 to 2007. Through the national HIV surveillance system, CDC collects HIV surveillance data in collaboration with state and local partners. Laboratories, physicians, hospitals, and other health-care providers are required to report cases of HIV infection and AIDS confidentially to designated health departments, which transmit case report data to CDC. For this study, we used data from 33 U.S. states (Alabama, Alaska, Arizona, Arkansas, Colorado, Florida, Idaho, Indiana, Iowa, Kansas, Louisiana, Michigan, Minnesota, Mississippi, Missouri, Nebraska, Nevada, New Jersey, New Mexico, New York, North Carolina, North Dakota, Ohio, Oklahoma, South Carolina, South Dakota, Tennessee, Texas, Utah, Virginia, West Virginia, Wisconsin, and Wyoming) that have been reporting HIV diagnoses for at least four years—long enough to evaluate trends. The data in this article are estimates derived from cases reported through June 2008, with statistical adjustments made for reporting delays and for cases with missing risk-factor information.16–18
We classified cases according to transmission category—the risk factor through which HIV was most likely to have been transmitted—based on CDC's hierarchy for HIV surveillance. The transmission categories included male-to-male sexual contact, injection drug use (IDU), combined male-to-male sexual contact and IDU, high-risk heterosexual contact, and other.19 The “other” category includes mother-to-child transmission; hemophilia; receipt of transfusion of blood, blood components, or blood products; and risk factors not reported or identified. People with more than one reported risk factor were classified in the transmission category listed first in the hierarchy.
For geographic analyses, we used categories defined by the United Nations and listed in its annual Demographic Yearbook.20 These regions are Europe, Asia, Africa, Oceania, Latin America, and North America. Latin America was subdivided into the sub-regions of Central America (including Mexico), the Caribbean, and South America. People were assigned to one of the following four regions of the U.S., based on their area of residence at HIV diagnosis: Northeast (New Jersey and New York), Midwest (Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin), South (Alabama, Arkansas, Florida, Louisiana, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia), and West (Alaska, Arizona, Colorado, Idaho, Nevada, New Mexico, Utah, and Wyoming).
Study sample
We examined diagnoses of HIV infection (with or without AIDS) made from 2001 to 2007 among adults and adolescents (aged ≥13 years) whose race was reported as “black or African American” and ethnicity as “not Hispanic or Latino.” Data do not include people who are of multiple races. We categorized people born in one of the 50 states or the District of Columbia as native-born. People born outside of the U.S. and its dependencies (American Samoa, the Commonwealth of the Northern Mariana Islands, Guam, Puerto Rico, and the U.S. Virgin Islands) were classified as foreign-born. Of a total 124,213 black adults and adolescents diagnosed with HIV from 2001 to 2007, 24,041 (19.4%) did not have complete information on country of birth and were excluded from the analyses. We also excluded people born in U.S. dependencies (159 cases, <1%). A total of 100,013 cases were included for analysis.
Data analysis
We conducted five sets of analyses for HIV-infected native-born and foreign-born black people. First, we examined the number and percentage distributions of HIV diagnoses, by selected demographic and geographic characteristics and by HIV-transmission risk factors. Second, to examine trends over time, we used linear regression to determine the estimated annual percentage change (EAPC) in HIV diagnoses from 2001 to 2007. Third, we calculated HIV diagnosis rates for native- and foreign-born black people aged ≥18 years for 2007 using data from the U.S. Census Bureau's 2007 American Community Survey.21 Fourth, we examined differences in late diagnoses of HIV infection among native- vs. foreign-born black people by comparing the distribution of individuals diagnosed with HIV infection from 2001 to 2006 who were diagnosed with AIDS within one year. Finally, for adults and adolescents diagnosed with AIDS from 1996 to 2003 in the 50 states and the District of Columbia (143,753 cases), we used the standardized Kaplan-Meier survival method to estimate the probability of survival for one year and for three years, by gender, age, transmission category, and diagnosis year.22 Cases were followed up through December 31, 2006; however, deaths were allowed to be reported through June 30, 2008, to account for reporting delays. We assigned a follow-up time of 15 days to cases with AIDS diagnosis and death within the same month.
RESULTS
Demographic characteristics
From 2001 to 2007, in the 33 U.S. states we studied, an estimated 100,013 cases of HIV infection were eligible for analysis, based on the availability of country-of-birth information. Of these, 88.3% (88,293) were native-born and 11.7% (11,720) were foreign-born. There were significant declines (from 15,429 in 2001 to 13,189 in 2007) in annual HIV diagnoses among native-born black people (EAPC: −5.5%; 95% CI −5.9, −5.0); however, changes were small among foreign-born black people, with a 1.3% annual decrease (from 1,736 in 2001 to 1,595 in 2007; 95% CI −2.6, −0.1).
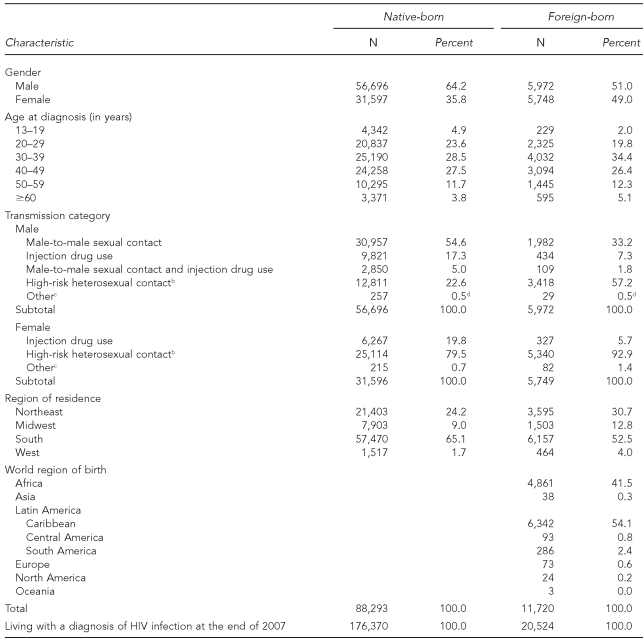
In Table 1, we present demographic characteristics and transmission categories by place of birth. Among females, a higher percentage of foreign-born black people were diagnosed with HIV infection than native-born black individuals (49.0% vs. 35.8%; p<0.001). The distribution of HIV diagnoses among black adults and adolescents was similar by place of birth and age. However, among people aged 13–19 and 20–29 years, native-born black individuals accounted for a higher percentage compared with foreign-born black people (4.9% vs. 2.0% and 23.6% vs. 19.8%, respectively; p<0.001); though among people aged 30–39 years, there was a higher percentage of HIV diagnoses in foreign-born black people than in native-born black individuals (34.4% vs. 28.5%; p<0.001).
Table 1.
Estimates of HIV diagnoses among black adults and adolescents, by place of birth, selected demographic characteristics, and transmission category, 33 U.S. states, 2001–2007a
aData have been adjusted for reporting delays and missing risk-factor information.
bHeterosexual contact with a person known to have or to be at high risk for HIV infection
cIncludes hemophilia, blood transfusion, perinatal exposure, and risk factor not reported or not identified
dNot significant; p>0.05
HIV = human immunodeficiency virus
The distribution of transmission categories differed by place of birth. From 2001 to 2007, the percentage of HIV diagnoses attributable to high-risk heterosexual contact was higher among foreign-born black people compared with native-born black people (74.7% vs. 43.0%). Among males, a higher percentage of foreign-born black people had an HIV diagnosis attributable to high-risk heterosexual contact than did native-born black individuals (57.2% vs. 22.6%; p<0.001) (Table 1). Compared with foreign-born black males, a higher percentage of native-born black males had an HIV diagnosis attributed to male-to-male sexual contact (54.6% vs. 33.2%; p<0.001), as well as combined male-to-male sexual contact and IDU (5.0% vs. 1.8%; p<0.001). HIV diagnoses attributable to high-risk heterosexual contact accounted for the highest percentages of HIV diagnoses for both native-born and foreign-born black females; however, the percentages were significantly higher among foreign-born black females (92.9% vs. 79.5%; p<0.001). HIV exposure through IDU was lower among foreign-born than native-born black individuals for both males (7.3% vs. 17.3%; p<0.001) and females (5.7% vs. 19.8%; p<0.001).
Comparing rates of HIV diagnosis in 2007 for adults aged ≥18 years, by place of birth, we found that foreign-born black people had a slightly higher HIV diagnosis rate (81.4 per 100,000) than native-born black people (78.9 per 100,000); however, differences were seen in rates by gender and U.S. or world region of birth. Native-born black males had the highest HIV diagnosis rate (115.0 per 100,000); however, the diagnosis rate for foreign-born black females (78.8 per 100,000) was nearly equal to that for foreign-born black males (84.2 per 100,000) and considerably higher than the rate for native-born black females (48.0 per 100,000).
Geographic distribution
From 2001 to 2007, most of the study group in the 33 states resided in the South (65.1% of native-born and 52.5% of foreign-born individuals) (Table 1). Higher percentages of foreign-born black people diagnosed with HIV infection resided in the Northeast, Midwest, and West compared with native-born black people, who were mostly concentrated in the South.
Comparing 2007 rates of HIV diagnosis for black adults aged ≥18 years by place of birth and region, we found the highest rates for native-born black people in the Northeast (114.6 per 100,000) and South (84.3 per 100,000) compared with foreign-born black people, for whom the highest rates were in the West (162.4 per 100,000) and Midwest (113.1 per 100,000). The highest diagnosis rates among native-born black people were in the Northeast (males: 169.3 per 100,000; females: 69.7 per 100,000) and South (males: 120.8 per 100,000; females: 53.2 per 100,000). We found differences among foreign-born black people, by region and gender. HIV diagnosis rates among foreign-born black females were highest in the West (209.6 per 100,000) and Midwest (153.1 per 100,000); however, rates among foreign-born black males were highest in the West (121.1 per 100,000) and South (105.0 per 100,000). HIV diagnosis rates among black females were higher for foreign-born compared with native-born individuals, regardless of region, except in the Northeast (69.7 per 100,000 vs. 49.5 per 100,000).
Of foreign-born black people diagnosed with HIV from 2001 to 2007, most were born in the Caribbean (54.1%) and Africa (41.5%) (Table 1). People born in South America accounted for 2.4% of those diagnosed, while people born in Europe, Asia, Central America, North America, and Oceania accounted for less than 1% each. By gender, males accounted for the majority (56.6%) of HIV diagnoses among black people born in the Caribbean; however, females accounted for most (57.4%) diagnoses among those born in Africa (Table 2).
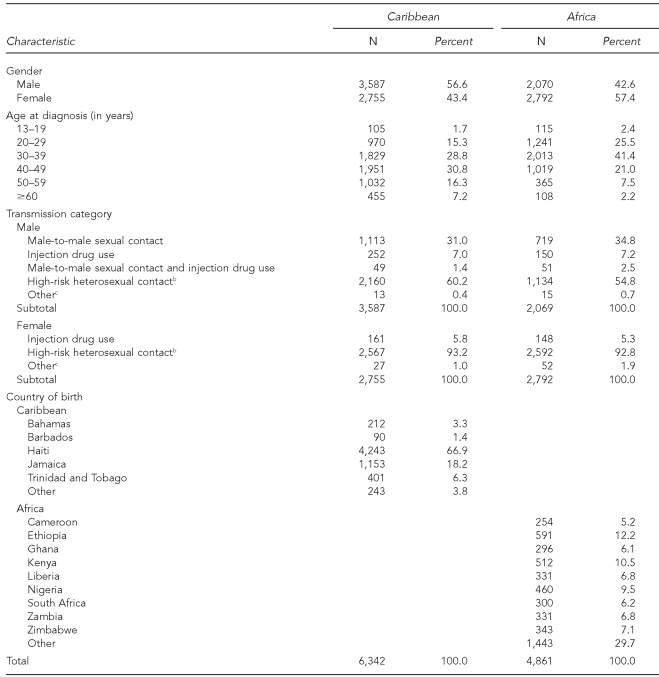
Table 2.
Estimates of HIV diagnoses among black adults and adolescents born in the Caribbean and Africa, by selected demographic characteristics and transmission category, 33 U.S. states, 2001–2007a
aData have been adjusted for reporting delays and missing risk-factor information.
bHeterosexual contact with a person known to have or to be at high risk for HIV infection
cIncludes hemophilia, blood transfusion, perinatal exposure, and risk factor not reported or not identified
HIV = human immunodeficiency virus
HIV diagnoses occurred at a younger age among black people born in Africa compared with those born in the Caribbean. The majority of black people born in Africa were aged 30–39 years at HIV diagnosis; most of those born in the Caribbean were aged 40–49 years at diagnosis (41.4% and 30.8%, respectively) (Table 2). HIV transmission among both populations was mostly attributable to high-risk heterosexual contact, regardless of gender. Most of those who were born in the Caribbean were from Haiti (66.9%). Of the remaining Caribbean black people, 18.2% were from Jamaica, 6.3% from Trinidad and Tobago, 3.3% from the Bahamas, 1.4% from Barbados, and 3.8% from other areas of the Caribbean. HIV diagnoses were more equally distributed by country of birth among black people born in Africa (12.2%, Ethiopia; 10.5%, Kenya; 9.5%, Nigeria; 7.1%, Zimbabwe; 6.8%, Liberia; 6.8%, Zambia; 6.2%, South Africa; 6.1%, Ghana; 5.2%, Cameroon; and 29.7%, other areas of Africa) (Table 2).
Late diagnosis of HIV infection
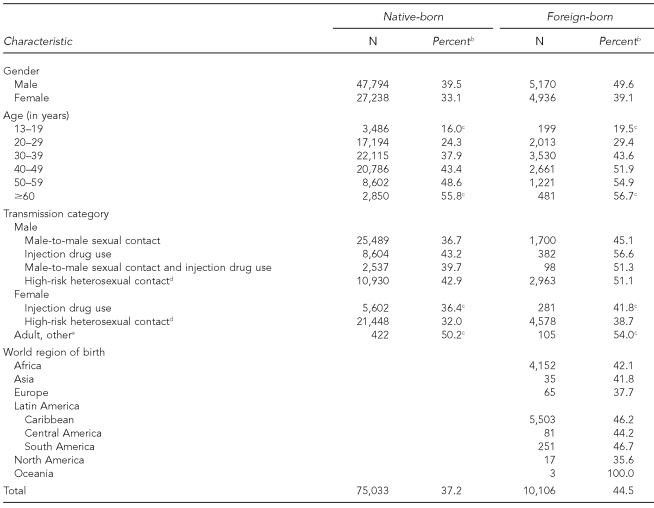
Early diagnosis of HIV infection is important both for initiation of treatment, so that the infection will not progress to AIDS, and prevention of the spread of HIV to sexual or drug-use partners. From 2001 to 2006, the percentage of foreign-born black people diagnosed with AIDS within 12 months of HIV diagnosis, regardless of gender, was significantly higher than that of native-born black people (44.5% vs. 37.2%; p<0.001) (Table 3). Foreign-born black people aged 20–59 years were significantly more likely than their native-born counterparts to be diagnosed with AIDS within 12 months of HIV diagnosis. Adults aged 60 years and older had the greatest percentage of people with late HIV diagnoses, regardless of place of birth, and nearly equal percentages of native-born and foreign-born black people in this group had late diagnoses. Percentages of late HIV diagnoses were also significantly higher among foreign-born black people, regardless of transmission category, except among female injection drug users. Male injection drug users accounted for the greatest percentage of late diagnoses, regardless of place of birth (Table 3).
Table 3.
Estimates of black adults and adolescents with an AIDS diagnosis within 12 months of HIV diagnosis, by place of birth and selected characteristics, 33 U.S. states, 2001–2006a
aData have been adjusted for reporting delays and missing risk-factor information.
bPercentage of group diagnosed with AIDS within 12 months of HIV diagnosis
cNot significant; p>0.05
dHeterosexual contact with a person known to have or to be at high risk for HIV infection
eIncludes hemophilia, blood transfusion, perinatal exposure, and risk factor not reported or not identified
AIDS = acquired immunodeficiency syndrome
HIV = human immunodeficiency virus
Survival after an AIDS diagnosis
For the 50 states and the District of Columbia, we estimated that foreign-born black people were more likely than native-born black people to survive one year after an AIDS diagnosis (87.2% vs. 84.9%). When gender and age were considered, higher proportions of foreign-born black people who were female, aged 20–29 years, or aged ≥40 years were likely to survive one year after an AIDS diagnosis, compared with native-born black people. Higher proportions of foreign-born than native-born black people were likely to survive three years after an AIDS diagnosis, regardless of gender, age, and year of diagnosis (except for adolescents aged 13–19 years, for whom there was no difference). Of foreign-born black people diagnosed with AIDS from 1996 to 2003 in the 50 states and the District of Columbia, 81.7% survived three years after diagnosis, compared with 74.9% of native-born black people. All differences were statistically significant.
DISCUSSION
Three important differences in the epidemiology of HIV among native- and foreign-born black people emerged from this study. First, heterosexual contact is the predominant mode of HIV transmission among foreign-born black people, accounting for most diagnoses, regardless of gender, and for more than 90% of infections among women. This pattern differs significantly from the native-born individuals, for whom male-to-male sexual contact is the primary mode of HIV infection.
Second, while rates of HIV diagnoses may be greatest among men for both native- and foreign-born black people, the HIV epidemic heavily affects foreign-born black women, whose rate of HIV diagnosis in 2007 was nearly equal to that of foreign-born black men and considerably higher than native-born black women.
Third, foreign-born black people are more likely than native-born black people to be diagnosed with AIDS within one year of their HIV diagnoses. This finding supports past research, which has found deficiencies in HIV knowledge, lack of access to health care, and delays in accessing HIV-related testing and care services among foreign-born people.23–26
We also found that higher proportions of foreign-born black people survived one year, and three or more years after an AIDS diagnosis. Our survival analysis included people with AIDS whose deaths may not have been due to HIV infection. With the advent of highly active antiretroviral therapy, the lifespan of HIV-infected people has been extended, and the number of HIV-attributable deaths has been reduced. Previous studies have found that, on average, foreign-born black people have better health than native-born black individuals.27–32 Foreign-born black people may possess more favorable health-behavior profiles than native-born black individuals, who have higher overall mortality rates attributable to cancer, heart disease, and homicide.27–31 Excess mortality among HIV-infected native-born black people due to deaths unrelated to HIV may explain the higher survival among foreign-born black individuals.
In addition to these differences, we found variations in annual trends and in the geographic makeup of cases among the foreign-born black population. From 2001 to 2007, annual HIV diagnoses declined significantly among native-born black populations; however, decreases were small among foreign-born black populations. It is unknown whether the decline in diagnoses among native-born black populations directly reflects trends in HIV incidence; analysis of historical trends indicates that HIV incidence among all black people has remained stable since the late 1990s.6
The majority of foreign-born black people diagnosed with HIV infection migrated from the Caribbean or Africa. This finding concurs with local studies from areas including New York, Los Angeles, and Seattle (King County).10–13 Foreign-born people of all races/ethnicities represent an increasing proportion of both the U.S. population and HIV diagnoses in the U.S.8,9 Our findings suggest a need to ensure that HIV prevention and treatment interventions reach Caribbean and African immigrant communities, as they were found to be the most heavily affected by HIV among foreign-born black people.
Limitations
The findings in this study were subject to several limitations. First, confidential name-based HIV surveillance data are available for only a limited number of states in which HIV reporting has been established long enough to analyze trends. Thus, the 33 states included in this analysis represent 63% of AIDS cases and may not be representative of the entire nation. Second, estimates of HIV diagnoses reflect only those cases diagnosed and reported to a state or local health department and may not be representative of new or incident infections. Third, HIV surveillance data from other states with a high percentage of foreign-born black people (including Maryland, California, Georgia, Massachusetts, and Pennsylvania) were not available.33
Fourth, the findings might be affected by statistical adjustments made for reporting delays and cases with missing risk-factor information. Fifth, the full impact of HIV on the foreign-born black population is likely to be underestimated. Although the national HIV surveillance system case report form includes country of birth, collection and reporting of these data vary, due to absence or misclassification of this information in medical records—a main source of information for HIV case reports. For example, we were unable to determine the country of birth for 24,041 black adults and adolescents (19.4%) diagnosed with HIV infection from 2001 to 2007, and, thus, we excluded these cases from the analysis. Finally, it is unknown where foreign-born people became infected, as information on date of entry into the U.S. and the time of acquisition of HIV is not collected in HIV case reports.
CONCLUSIONS
Our findings indicate that including country-of-birth information in analyses of HIV surveillance data helps to identify important differences between population groups. Given the enormous diversity among foreign-born black people in the U.S., collection of detailed demographic information, including place of birth, is needed in the national HIV surveillance system. Improved ascertainment of country-of-birth information may assist in determining differences in HIV transmission and morbidity among the foreign-born black population. To determine differences in HIV diagnosis patterns among native- and foreign-born black people, country-of-birth data should be included in analyses of HIV surveillance data for states with large foreign-born populations.
Identifying these highly affected populations is critical to ensuring that HIV-prevention funding and services are used strategically. The heterogeneity in the U.S. black population, including important variations in HIV transmission among native-born and foreign-born black individuals, has significant implications for HIV-prevention planning. Future studies should examine differences in cultural beliefs about HIV transmission, prevention, and treatment among native- and foreign-born black people.
Many HIV prevention and care programs currently focus their efforts on particular HIV risk groups, based on race/ethnicity and gender, irrespective of place of birth. Cultural and language barriers experienced by foreign-born people may affect their health status and access to relevant services. A comprehensive approach to addressing health disparities should take into account social determinants of health (structural and contextual factors, socioeconomic status, health-care service access and quality, and environmental factors) in addition to individual-level factors.34 Program collaboration and service integration will allow for a more comprehensive approach to addressing the health disparity of HIV/AIDS among black people in the U.S. Tailoring HIV prevention, testing, and treatment programs to address epidemiologic differences and social disadvantages among native- and foreign-born black people may reduce HIV transmission in these populations and increase access to HIV testing and care.
Footnotes
The findings and conclusions in this article are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Racial/ethnic disparities in diagnoses of HIV/AIDS—33 states, 2001–2005. MMWR Morb Mortal Wkly Rep. 2007;56(9):189–93. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (US) HIV/AIDS Surveillance Supplemental Report Vol. 3, No. 1. Atlanta: CDC; 2008. Cases of HIV infection and AIDS in the United States and dependent areas, by race/ethnicity, 2002–2006. [Google Scholar]
- 3.CDC (US) HIV/AIDS Surveillance Supplemental Report Vol. 12, No. 1. Atlanta: CDC; 2006. Cases of HIV infection and AIDS in the United States, by race/ethnicity, 2000–2004. [Google Scholar]
- 4.Dean HD, Steele CB, Satcher AJ, Nakashima AK. HIV/AIDS among minority races and ethnicities in the United States, 1999–2003. J Natl Med Assoc. 2005;97(Suppl 7):S5–12. [PMC free article] [PubMed] [Google Scholar]
- 5.CDC (US) A heightened national response to the HIV/AIDS crisis among African Americans. Atlanta: CDC; 2007. [cited 2009 Nov 6]. Also available from: URL: http://www.cdc.gov/hiv/topics/aa/resources/reports/pdf/heightenedresponse.pdf. [Google Scholar]
- 6.Hall HI, Song R, Rhodes P, Prejean J, An Q, Lee LM, et al. Estimation of HIV incidence in the United States. JAMA. 2008;300:520–9. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Subpopulation estimates from the HIV incidence surveillance system—United States, 2006. MMWR Morb Mortal Wkly Rep. 2008;57(36):985–9. [PubMed] [Google Scholar]
- 8.Patel-Larson A, Espinoza L, Hu X. HIV/AIDS among foreign-born people in 33 states in the United States, 2001–2005. Poster presented at the 2007 National HIV Prevention Conference; 2007 Dec 2–5; Atlanta. [Google Scholar]
- 9.Dean-Gaitor HD, Fleming PL, Li J, Diaz T, Ward JW. Trends among foreign-born persons with AIDS, United States, 1993–1995: a special challenge for HIV prevention. Poster presented at the 11th International Conference on AIDS; Vancouver, British Columbia. 1996. Jul 7–12. [Google Scholar]
- 10.Kent JB. Impact of foreign-born persons on HIV diagnosis rates among blacks in King County, Washington. AIDS Educ Prev. 2005;17(6 Suppl B):60–7. doi: 10.1521/aeap.2005.17.Supplement_B.60. [DOI] [PubMed] [Google Scholar]
- 11.Kerani RP, Kent JB, Sides T, Dennis G, Ibrahim AR, Cross H, et al. HIV among African-born persons in the United States: a hidden epidemic? J Acquir Immune Defic Syndr. 2008;49:102–6. doi: 10.1097/QAI.0b013e3181831806. [DOI] [PubMed] [Google Scholar]
- 12.Hoffman S, Beckford Jarrett ST, Kelvin EA, Wallace SA, Augenbraun M, Hogben M, et al. HIV and sexually transmitted infection risk behaviors and beliefs among black West Indian immigrants and US-born blacks. Am J Public Health. 2008;98:2042–50. doi: 10.2105/AJPH.2006.106443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harawa NT, Bingham TA, Cochran SD, Greenland S, Cunningham WE. HIV prevalence among foreign- and US-born clients of public STD clinics. Am J Public Health. 2002;92:1958–63. doi: 10.2105/ajph.92.12.1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ansari Z, Carson NJ, Ackland MJ, Vaughan L, Serraglio A. A public health model of the social determinants of health. Soz Praventivmed. 2003;48:242–51. doi: 10.1007/s00038-003-2052-4. [DOI] [PubMed] [Google Scholar]
- 15.Dahlgren G, Whitehead M. Background document to WHO—strategy paper for Europe. Stockholm: Institute for Futures Studies; 1991. [cited 2009 Nov 6]. Policies and strategies to promote social equity in health. Also available from: URL: http://www.framtidsstudier.se/filebank/files/20080109$110739$fil$mz8uvqv2wqfshmrf6cut.pdf. [Google Scholar]
- 16.Green TA. Using surveillance data to monitor trends in the AIDS epidemic. Stat Med. 1998;17:143–54. doi: 10.1002/(sici)1097-0258(19980130)17:2<143::aid-sim757>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 17.Song R, Hall HI, Frey R. Uncertainties associated with incidence estimates of HIV/AIDS diagnoses adjusted for reporting delay and risk redistribution. Stat Med. 2005;24:453–64. doi: 10.1002/sim.1935. [DOI] [PubMed] [Google Scholar]
- 18.Harrison KM, Kajese T, Hall HI, Song R. Risk factor redistribution of the national HIV/AIDS surveillance data: an alternative approach. Public Health Rep. 2008;123:618–27. doi: 10.1177/003335490812300512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.CDC (US) HIV/AIDS Surveillance Report Vol. 19. Atlanta: CDC; 2009. Cases of HIV infection and AIDS in the United States and dependent areas, 2007. [Google Scholar]
- 20.United Nations, Department for Economic and Social Information and Policy Analysis, Statistics Division. 47th ed. New York: United Nations; 1997. 1995 demographic yearbook. [Google Scholar]
- 21.Census Bureau (US) American Community Survey: 2007 American Community Survey 1-year estimates. [cited 2010 Mar 15]. Available from: URL: http://www.census.gov/acs/www/Products/users_guide/2007/index.htm.
- 22.Amato DA. A generalized Kaplan-Meier estimator for heterogeneous populations. Commun Stat—Theor M. 1988;17:263–86. [Google Scholar]
- 23.Rodriguez AE, Metsch LR, Saint-Jean G, Molina EG, Kolber MA. Differences in HIV-related hospitalization trends between Haitian-born blacks and US-born blacks. J Acquir Immune Defic Syndr. 2007;45:529–34. doi: 10.1097/QAI.0b013e31811ed1dc. [DOI] [PubMed] [Google Scholar]
- 24.Othieno J. Understanding how contextual realities affect African born immigrants and refugees living with HIV in accessing care in the Twin Cities. J Health Care Poor Underserved. 2007;18(Suppl 3):170–88. doi: 10.1353/hpu.2007.0085. [DOI] [PubMed] [Google Scholar]
- 25.Gillespie-Johnson M. HIV/AIDS prevention practices among recent-immigrant Jamaican women. Ethn Dis. 2008;18(2 Suppl 2):S2–175–8. [PMC free article] [PubMed] [Google Scholar]
- 26.Thamer M, Richard C, Casebeer AW, Ray NF. Health insurance coverage among foreign-born US residents: the impact of race, ethnicity, and length of residence. Am J Public Health. 1997;87:96–102. doi: 10.2105/ajph.87.1.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Singh GK, Miller BA. Health, life expectancy, and mortality patterns among immigrant populations in the United States. Can J Public Health. 2004;95:I14–21. doi: 10.1007/BF03403660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Singh GK, Siahpush M. All-cause and cause-specific mortality of immigrants and native born in the United States. Am J Public Health. 2001;91:392–9. doi: 10.2105/ajph.91.3.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Singh GK, Siahpush M. Ethnic-immigrant differentials in health behaviors, morbidity, and cause-specific mortality in the United States: an analysis of two national data bases. Hum Biol. 2002;74:83–109. doi: 10.1353/hub.2002.0011. [DOI] [PubMed] [Google Scholar]
- 30.Lucas JW, Barr-Anderson DJ, Kington RS. Health status of non-Hispanic U.S.-born and foreign-born black and white persons: United States, 1992–95. Vital Health Stat. 2005;10(226) [PubMed] [Google Scholar]
- 31.Fang J, Madhavan S, Alderman MH. Nativity, race, and mortality: favorable impact of birth outside the United States on mortality in New York City. Hum Biol. 1997;69:689–701. [PubMed] [Google Scholar]
- 32.Read JG, Emerson MO, Tarlov A. Implications of black immigrant health for U.S. racial disparities in health. J Immigr Health. 2005;7:205–12. doi: 10.1007/s10903-005-3677-6. [DOI] [PubMed] [Google Scholar]
- 33.Schmidley AD. Current Population Reports, series P23-206. Washington: Government Printing Office (US); 2001. [cited 2009 Nov 6]. Profile of the foreign-born population in the United States: 2000. Also available from: URL: http://www.census.gov/prod/2002pubs/p23-206.pdf. [Google Scholar]
- 34.CDC (US) External consultation meeting report. Atlanta: CDC; 2009. [cited 2010 Mar 15]. Addressing social determinants of health: accelerating the prevention and control of HIV/AIDS, viral hepatitis, STD and TB. Also available from: URL: http://www.cdc.gov/socialdeterminants/docs/final_SDHConsultation_ForWeb_061109.pdf. [Google Scholar]