SYNOPSIS
Objective
Sex work is regulated in Tijuana, Mexico, but only half of the city's female sex workers (FSWs) are registered with the municipal health department, which requires regular screening for sexually transmitted infections (STIs) and human immunodeficiency virus (HIV). We examined correlates of registration to determine if it confers measurable health benefits.
Methods
From 2004 to 2006, we interviewed FSWs in Tijuana ≥18 years of age who reported recent unprotected sex with at least one client and were not knowingly HIV-positive, and tested them for HIV, syphilis, gonorrhea, and chlamydia. Logistic regression identified factors associated with registration.
Results
Of 410 FSWs, 44% were registered, 69% had been tested for HIV, 6% were HIV-positive, and 44% tested positive for any STI. Compared with unregistered FSWs, registered FSWs were more likely to have had HIV testing (86% vs. 56%, p<0.001) and less likely to test positive for any STI (33% vs. 53%, p<0.001) or HIV (3% vs. 8%, p=0.039). Factors independently associated with registration included ever having an HIV test (adjusted odds ratio [AOR] = 4.19) and earning >$30 per transaction without a condom (AOR=2.41), whereas working on the street (AOR=0.34), injecting cocaine (AOR=0.06), snorting or smoking methamphetamine (AOR=0.27), and being born in the Mexican state of Baja California (AOR=0.35) were inversely associated with registration.
Conclusion
Registered FSWs were more likely than unregistered FSWs to have had HIV testing and to engage in less drug use, but did not have significantly lower HIV or STI prevalence after adjusting for confounders. Current regulation of FSWs in Tijuana should be further examined to enhance the potential public health benefits of registration.
Female sex workers (FSWs) represent a vulnerable population at risk for human immunodeficiency virus (HIV) and sexually transmitted infections (STIs). Governments in many countries have regulated sex work as a public health measure, and traditionally such regulation has focused on increasing condom use or STI diagnosis and treatment.1 In Mexico, some cities (such as Tijuana) register FSWs, but the effect such registration has on health outcomes is unknown.
Other countries have shown success in decreasing HIV and STI rates through regulation of sex work. In Thailand, the federal government's “100% condom campaign” increased condom use in brothels from 14% to 94% within five years, and decreased HIV incidence from 2.48 to 0.55 per 100 person-years and STI prevalence by 79% in men.2–5 Brothels that were non-compliant faced loss of their sex-work license, which was a powerful incentive; however, this approach was less effective in increasing condom use among FSWs not working in brothels.5,6
Systems to screen and treat STIs among FSWs have been employed effectively in such low-resource settings as Senegal,7 Kenya,8 Bolivia,9 and Côte d'Ivoire,10 although evidence to disentangle their impact from other programs is lacking. A multi-city study conducted among FSWs in the Dominican Republic evaluated the addition of regional government sanctions to an intervention that included a 100% condom campaign, improved STI screening and treatment, and women's empowerment and performance reports that were shared with brothel owners. Significant improvements in FSWs' self-reported ability to reject unsafe sex and increase condom use with clients and intimate partners were observed only in the city that offered additional government enforcement through sanctions. In the one regulated city, STI prevalence was reduced by 43%.11,12
Other models of legalization and registration of sex workers exist. In Nevada, legalized brothels require that FSWs undergo mandatory weekly testing for HIV and STIs,13–15 with brothel owners being held legally liable for clients who acquire HIV from an FSW.16,17 In the Netherlands, FSWs are not registered with the government nor do they have mandatory health screenings, but STI clinics offer free, anonymous STI testing.18
In Mexico, commercial sex is culturally accepted.19 Mexico's 32 states have developed either abolitionist policies (Puebla, Guanajuato, and the Federal District), where sex work is a misdemeanor, or reglamentarist policies, where sex work is limited to zones of tolerance (zonas rojas). The latter type of state, which includes the Mexico-U.S. border states of Baja California and Tamaulipas, requires that FSWs be registered and subjected to regular health exams.20,21 Due to the unique characteristics of the border region—including the existence of zonas rojas, populations that are highly mobile, and major drug trafficking—several Mexico-U.S. border cities are experiencing rapidly escalating HIV epidemics.22
Due to Tijuana's proximity to San Diego, the city's zona roja is a destination for sex tourism.23 This area is in a neighborhood with the city's highest concentration of injection drug use, HIV infection, and STIs.24,25 In Tijuana and Ciudad Juarez, prevalence of HIV, Neisseria gonorrhoeae (N. gonorrhoeae), Chlamydia trachomatis (C. trachomatis), and active syphilis among FSWs was 6%, 6%, 13%, and 14%, respectively, in 2006.26 FSWs who inject drugs in these cities had an even higher prevalence of HIV (12%), and 46% had at least one STI.27
The municipal government of Tijuana has developed a system of regulation that issues registration cards to FSWs through the municipal health department (Servicios Médicos Municipales; hereafter, MHD). Registration with the MHD costs $360 per person a year; fee waivers are not provided. Monthly HIV testing and quarterly STI screening is mandated and occurs at the MHD. Women registering as FSWs are treated with antibiotics according to federal STI guidelines,28 and if they are found to be HIV-positive, their registration cards are revoked, and they are referred to specialty care (Personal communication, Clark-Alfaro V, director of the Binational Center for Human Rights, Tijuana, Mexico, May 2009). At the time of this study, approximately half of the city's 5,000 sex workers were registered with the MHD,29 enabling them to work legally in the zona roja. Enforcement of registration is difficult; anecdotal reports indicate that some bars and dance halls require women to be registered to work on their premises and, to evade such requirements, many women work on street corners, where they are often harassed by police.30
No systematic evaluation of the sex-work registration system in Tijuana has been conducted. We hypothesized that registered FSWs would be more likely to ever have had an HIV test and less likely to test positive for STIs and HIV than would unregistered FSWs. Due to the financial burden registration poses, we also predicted that poorer women would be less likely to be registered. To understand the role of government registration and health screening as public health measures, we compared the characteristics and health outcomes of registered vs. unregistered FSWs. These results will help inform systems of sex-work regulation to effectively operate as public health programs.
METHODS
Population and settings
Tijuana, in the state of Baja California, Mexico, is situated on the U.S. border and is home to the busiest land border crossing in the world, with more than 46 million northbound crossings into San Diego per year.31 Due to the development of the maquiladora (factory) industry and the proximity to the U.S., more than half of the city's residents are migrants.32
From 2004 to 2006, 924 FSWs in Tijuana and Ciudad Juarez were enrolled in a behavioral intervention study to increase condom use, as previously described.33 Due to the lack of FSW registration in Ciudad Juarez, this analysis was restricted to the 474 FSWs enrolled in Tijuana. FSWs were recruited by outreach workers and at community health clinics. Eligibility requirements included aged ≥18 years (the legal age for sex work in Mexico); ability to give consent; having traded sex for money, goods, or drugs within the previous two months; and having had unprotected sex with at least one client in the last two months. Because the intervention aimed to reduce HIV incidence, women who were knowingly HIV-infected were excluded.
Data collection
Spanish-speaking counselors conducted baseline interviews. Trained study nurses obtained venous blood samples and cervical swabs. Interview questions covered demographics, socioeconomic factors, working conditions, cost per sex act with and without condoms, and sexual and drug-related behaviors. In addtion, participants were asked, “Are you currently registered with the Tijuana MHD as a sex worker?” Participants were compensated $30 for their time for the baseline interview and brief intervention session. Institutional Review Boards at the University of California—San Diego and the Universidad Autónoma de Baja California in Tijuana reviewed and approved the study protocol.
Laboratory evaluation
Specimen testing was conducted at the San Diego County Health Department. We used the Determine® rapid HIV antibody test (Abbott Pharmaceuticals, Boston, Massachusetts) to detect HIV antibodies; all positive tests were confirmed by enzyme immunoassay and western blot. N. gonorrhoeae and C. trachomatis were detected from cervical samples using the APTIMA Combo 2® collection device (Gen-Probe, San Diego). We used a rapid plasma reagin test (BD Macro-Vue™ RPR, Becton Dickinson, Cockeysville, Maryland) to detect antibody to Treponema pallidum (T. pallidum); positive samples were confirmed by T. pallidum hemagglutinin assay (Fujirebio, Wilmington, Delaware). Any level of syphilis titer was considered consistent with prior or latent infection; titers ≥1:8 were considered consistent with active infection.34 We provided all test results to participants; those with positive results were referred to the MHD for free treatment and follow-up.
Statistical analyses
Statistical analysis compared FSWs who reported being registered with the MHD to those who were not, using Wilcoxon's rank sum for continuous variables and Fisher's exact test for dichotomous variables. To preserve statistical power, we generated a combined measure reflecting test results for HIV and any STIs. We used univariate and multivariate logistic regression to evaluate factors associated with registration using manual, backward stepwise elimination; variables attaining p<0.10 significance in univariate analysis were considered in the multivariate regression, retaining only variables achieving p<0.05 significance in the final model.
RESULTS
Of 474 FSWs enrolled, registration data were missing from 64 (14%), and these participants were accordingly excluded from the analysis. Of the 410 FSWs remaining, 181 (44%) were currently registered with the MHD.
Demographic and socioeconomic factors
Table 1 shows the baseline demographic, socioeconomic, and working conditions of the 410 FSWs. The median age was 32 (interquartile range [IQR]: 25–38), and most women were migrants to Baja California (78%). Less than one-fifth were married (19%). Although the majority had children (92%) and listed children as financial dependents (73%), only one-third rated themselves as in a bad financial situation (34%). In general, participants had little formal education, with a median of six years, and most did not speak any English (74%).
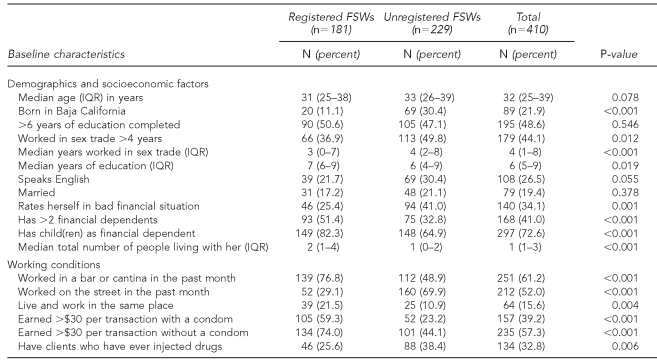
Table 1.
Characteristics of registered and unregistered FSWs in Tijuana, Mexico (n=410)a
aThe first three columns of data are displayed by number (percent) of women and median (IQR) for dichotomous and continuous variables, respectively. Dichotomous outcomes were examined using Fisher's exact test. Continuous outcomes were examined using Wilcoxon's rank sum test for differences in group distributions. Certain percentages may reflect denominators smaller than the n-value given in the column head; these discrepancies are due to missing data.
FSW = female sex worker
IQR = interquartile range
Compared with registered FSWs, unregistered FSWs were more likely to be native to Baja California (30% vs. 11%, p<0.001), to have worked longer in the sex trade (median four years vs. three years, p<0.001), and to rate their financial situation as bad (41% vs. 25%, p<0.001). Interestingly, registered FSWs were twice as likely as unregistered FSWs to have more than two financial dependents (51% vs. 33%, p<0.001) and to live with a greater number of people (median 2.0 vs. 1.0, p<0.001). Age did not differ significantly between the groups.
Working conditions
Overall, most FSWs worked in a bar (61%) for a mean of 44 hours per week, and only about one-fifth (21%) rated their working conditions as good. Registered FSWs were more likely than unregistered FSWs to work in an establishment such as a bar (77% vs. 49%, p<0.001) or live and work in the same place (22% vs. 11%, p=0.004) as opposed to working on the street (29% vs. 70%, p<0.001). There were no statistically significant differences between registered and unregistered FSWs in terms of their working at brothels, hotels, or shooting galleries (a designated place where drugs are purchased and used). Registered FSWs earned significantly more money per transaction than unregistered FSWs for sex both with a condom (earning >$30 per transaction, 59% vs. 23%, p<0.001) and without a condom (earning >$30 per transaction, 74% vs. 44%, p<0.001) (Table 1).
HIV-related risk behaviors
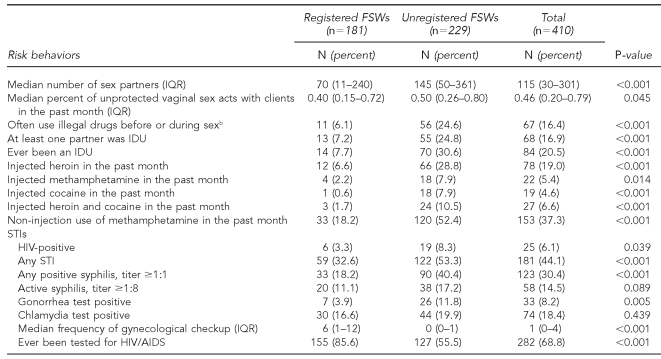
Table 2 shows the overall risk behaviors and prevalence of STIs and HIV in our sample. The median number of unprotected vaginal sex acts in the last month was five (IQR: 2–14). One-fifth of the sample had ever injected drugs, and almost 40% had used methamphetamine in the last month. Interestingly, compared with unregistered FSWs, registered FSWs had lower risk profiles for both sexual and drug-related behaviors, and fewer sex partners in the last month (median: 70 vs. 145, p<0.001). As for drug-related risk behaviors, registered FSWs were less likely than unregistered FSWs to report ever having injected drugs (8% vs. 31%, p<0.001), having clients who currently use drugs (62% vs. 83%, p<0.001), or having had a sex partner who had ever injected drugs (7% vs. 25%, p<0.001).
Table 2.
Risk behaviors and STIs of registered and unregistered FSWs in Tijuana, Mexico (n=410)a
aThe first three columns of data are displayed by number (percent) of women and median (IQR) for dichotomous and continuous variables, respectively. Dichotomous outcomes were examined using Fisher's exact test. Continuous outcomes were examined using Wilcoxon's rank sum test for differences in group distributions. Certain percentages may reflect denominators smaller than the n-value given in the column head. These discrepancies are due to missing data.
bThe binary variable “often use illegal drugs before or during sex” was derived by combining the responses “often” and “always” into one category and “never” and “sometimes” into the other.
STI = sexually transmitted infection
FSW = female sex worker
IQR = interquartile range
IDU = injection drug user
HIV = human immunodeficiency virus
AIDS = acquired immunodeficiency syndrome
Prevalence of HIV and STIs
More than two-thirds had been tested for HIV prior to enrollment (69%); 6% tested HIV-positive at enrollment, and almost half tested positive for at least one STI (44%). Compared with unregistered FSWs, registered FSWs were more likely ever to have been tested for HIV (86% vs. 56%, p<0.001) and less likely to test positive for HIV (3% vs. 8%, p=0.039), gonorrhea (4% vs. 12%, p=0.005), syphilis (any titer) (18% vs. 40%, p<0.001), or any STI (including HIV) (33% vs. 53%, p<0.001). However, prevalence of active syphilis (titer ≥1:8) and chlamydia were similar in both groups (Table 2).
Factors independently associated with FSW registration
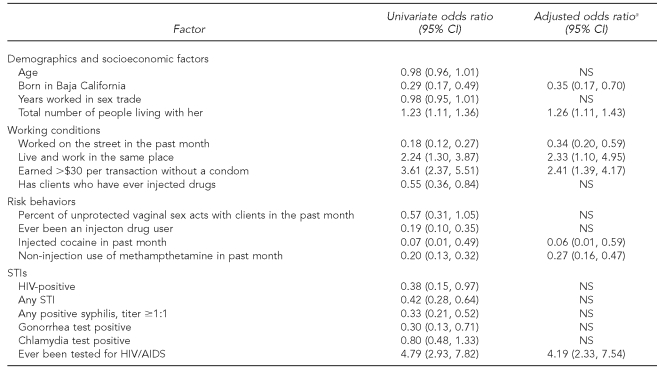
Factors associated with FSW registration identified in univariate and multivariate regression models are shown in Table 3. In univariate analyses, factors associated with increased odds of registration included having a greater number of people living with one, living and working in the same location, earning more money for sexual transactions with a condom, and ever having been tested for HIV. Factors inversely associated with registration included having migrated to Baja California; working on the street; having clients who inject drugs; ever having injected drugs; injecting cocaine; non-injection use of methamphetamine; and testing positive for HIV, syphilis, gonorrhea, or any STI (including HIV). Variables not associated with registration were age, lifetime duration of sex work, and the percent of unprotected sex acts with clients.
Table 3.
Selected factors associated with FSW registration in Tijuana, Mexico
aVariables in the multivariate model are adjusted for all other variables in the model.
FSW = female sex worker
CI = confidence interval
NS = not significant
STI = sexually transmitted infection
HIV = human immunodeficiency virus
AIDS = acquired immunodeficiency syndrome
In multivariate analyses, four factors were found to be independently associated with elevated odds of registration. FSWs who were registered were more likely ever to have had an HIV test (adjusted odds ratio [AOR] = 4.19; 95% confidence interval [CI] 2.33, 7.54) and to make more money (>$30) per transaction without a condom (AOR=2.41; 95% CI 1.39, 4.17). They also were more likely to live with more people (AOR=1.26; 95% CI 1.11, 1.43) and live and work in the same place (AOR=2.33; 95% CI 1.10, 4.95). In addition, four factors were inversely associated with registration, including working on the street (AOR=0.34; 95% CI 0.20, 0.59), injecting cocaine (AOR=0.06; 95% CI 0.01, 0.59), snorting or smoking methamphetamine (AOR=0.27; 95% CI 0.16, 0.47), and having been born in Baja California (AOR=0.35; 95% CI 0.17, 0.70). To eliminate the effects of collinearity, we repeated the model, removing the variable for previous HIV testing, and the remaining variables and their corresponding parameter estimates were essentially unchanged.
DISCUSSION
In examining the system for regulating FSWs in Tijuana, we found that registration with the MHD was associated with higher odds of HIV testing, as one would expect, but registration was not associated with lower risk of testing positive for HIV or STIs, after adjusting for other confounders associated with registration.
We identified two patterns related to sex-worker registration that have implications for HIV and STI prevention and policies. First, registered FSWs tended to work in venue-based establishments, lived and worked in the same location, and earned more money per transaction. Conversely, women who worked primarily on the street were less likely to be registered, as were FSWs who injected drugs and those who used stimulants (i.e., cocaine or methamphetamine). These results provide the first analysis of the current system of regulation of FSWs on the Mexico-U.S. border and offer an opportunity to inform HIV-prevention efforts in this region.
Because HIV testing is a requirement for all women who are registered, we expected that 100% of registered women would have been tested, instead of 85%, as reported by our participants. This may imply that FSWs, or the establishments for which they work, are finding a way to buy a registration card and bypass the regulation system, or the FSWs may be unaware that they have been tested. These findings also may indicate that HIV testing is not a strong motivator for FSWs to register with the MHD. Although registered FSWs are more likely to have been tested for HIV, registration did not ultimately serve as an independent predictor of lower STI and HIV prevalence. Earlier studies in the Philippines have also showed that STI screening and treatment, in the absence of other prevention -strategies, are not effective for long-term control of STIs or HIV in sex workers.1,35
As in previous studies, sex-work venue was an important correlate of registration, with street-based sex workers being less likely to be registered.6,36 This finding highlights three important observations. First, street-based sex workers often have higher risk profiles, and they may have decreased access to condoms and fewer contacts with screening and treatment services for HIV and STIs. The current registration system may be excluding sex workers who operate outside of a specific venue, and thus the MHD may not be reaching women at highest risk for HIV and STIs. Because street-based FSWs are more likely to be infected with HIV and STIs and to use drugs,37 efforts are needed to reach out to these women, who may fear they will be denied registration if they test HIV-positive. Since our study was conducted, a mobile HIV-prevention campaign has been initiated in Tijuana, representing a partnership between a local nongovernmental organization and the municipal, state, and federal governments.22 Efforts such as these may encourage FSWs to seek testing for HIV and other STIs without fear of repercussions.
The HIV epidemic among FSWs living in some Mexico-U.S. border cities has increased rapidly in the last 10 years, especially among FSWs who inject drugs.26,27 Our study found that unregistered women were more likely to have injected drugs and particularly more likely to have used stimulants in the last month. Previous studies found that both injection of cocaine and non-injection use of methamphetamine are associated with high-risk sexual behavior in FSWs and are independently associated with HIV infection.26,38,39 This supports the hypothesis that the current registration system is not serving the health needs of street-based, drug-using FSWs, who are at highest risk for HIV and STIs.
A novel finding in our study was the relationship between income and registration. Registered sex workers earned more money per sex act compared with unregistered FSWs. This finding has significance for the goal of addressing social determinants of health among sex workers. Poverty, income inequality, and decreased social capital have been linked to women's decisions to engage in risky transactional sex.40–43 At the Mexico-U.S. border, financial need is a major motivation for women to initiate and continue in sex work.23 In addition to depressed economic status, FSWs at the border have other poverty-related risk factors for HIV, such as low educational level, multiple financial dependents, low literacy, and inconsistent knowledge of HIV and STIs.23,26 Due to the heavy burden that the cost of registration may pose for some FSWs, it is possible that the system is cost-prohibitive to poorer sex workers, who make less money per transaction, further marginalizing these at-risk women.
Lastly, migration status was an important correlate of registration. Unregistered women were more likely to have been born in Baja California. This finding is interesting in light of newer data associating time spent in Tijuana with risk behavior and HIV prevalence. In a study evaluating injection drug users who had recently been deported or who had migrated to Tijuana, the odds of HIV infection among females increased with time spent in Tijuana, but the trend was opposite among males.44 Our findings may suggest that women who are migrants to Tijuana are routed into sex work through establishments (such as bars) that may encourage them to become registered.
Limitations
Several limitations with our study should be noted. First, the study's cross-sectional nature does not allow us to draw causal inferences. Second, because the population was recruited via convenience sampling and the eligibility criteria for the subsequent intervention study required that women have had recent unprotected sex with clients, our sample likely had a higher risk profile than the general FSW population in Tijuana or other border cities. Our study included FSWs from Tijuana only and may not be generalizable to other cities, although the most common Mexican FSW workplace venues were represented. Participants were all ≥18 years of age (18 being the legal age for FSW registration in Mexico); therefore, our results do not address the issues of underage sex workers.
Although participants were asked if they were registered with the MHD, we were unable to confirm if women who were registered actually sought services from the department. There is potentially a reporting bias toward registration, if the women feared penalties in being unregistered; however, we found little evidence of reporting bias in other sensitive areas, with many women reporting unprotected vaginal sex with clients and drug use.
Finally, our study did not elicit details on cost of the registration card. Since this study was completed, the cost has reportedly increased from $360 per person per year to $450 per person per year (Personal communication, Clark-Alfaro V, director of the Binational Center for Human Rights, Tijuana, Mexico, May 2009). Future studies will address how the cost of the registration card may affect which women are registered, if the increase in cost has deterred registration, and if anyone other than the sex worker herself is paying for the card.
CONCLUSION
Systems for regulating sex work constitute an important public health measure in settings where HIV and other STIs are rising, as they are in Tijuana. Our study suggests that the current system of registration of FSWs in Tijuana focuses on screening and treatment of HIV and STIs and may be structured in such a way that it excludes the highest risk subgroups, especially FSWs who are street-based and those who inject drugs or use stimulants. Future strategies to ensure the most vulnerable FSWs are reached might include an integrated model of rapid screening and treatment for HIV and STIs using mobile clinics and partner notification, and incorporating active or former FSWs as promotoras (indigenous outreach workers). Consideration should also be given to models incorporating incentivized or enforced condom use, which has been found to be successful in other settings.2–6,11,12 With regard to the latter, an important lesson should be gleaned from the Dominican Republic, where effectiveness was potentiated when a combined approach to prevention was grounded in female and community empowerment.11,12 Efforts to reach the most marginalized segments of the sex-worker population are likely to succeed when they have gained the community's trust, rather than their fear or contempt.
Acknowledgments
The authors thank the staffs of Patronato Pro-COMUSIDA, CAPASITS, the municipal and state health departments of Tijuana and Baja California, and the San Diego County Health and Human Services Agency. The authors also give special thanks to the participants for their time and cooperation.
Footnotes
Funding for this study was provided by National Institutes of Health grants R01 MH065849 (T.L. Patterson) and T32 DA023356 (S.A. Strathdee).
REFERENCES
- 1.Steen R, Dallabetta G. Sexually transmitted infection control with sex workers: regular screening and presumptive treatment augment efforts to reduce risk and vulnerability. Reprod Health Matters. 2003;11:74–90. doi: 10.1016/s0968-8080(03)02295-x. [DOI] [PubMed] [Google Scholar]
- 2.Celentano DD, Nelson KE, Lyles CM, Beyrer C, Eiumtrakul S, Go VF, et al. Decreasing incidence of HIV and sexually transmitted diseases in young Thai men: evidence for success of the HIV/AIDS control and prevention program. AIDS. 1998;12:F29–36. doi: 10.1097/00002030-199805000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Rojanapithayakorn W, Hanenberg R. The 100% condom program in Thailand. AIDS. 1996;10:1–7. doi: 10.1097/00002030-199601000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Hanenberg RS, Sokal DC, Rojanapithayakorn W, Kunasol P, Sokal DC. Impact of Thailand's HIV-control programme as indicated by the decline of sexually transmitted diseases. Lancet. 1994;344:243–5. doi: 10.1016/s0140-6736(94)93004-x. [DOI] [PubMed] [Google Scholar]
- 5.Nelson KE, Celentano DD, Eiumtrakol S, Hoover DR, Beyrer C, Suprasert S, et al. Changes in sexual behavior and a decline in HIV infection among young men in Thailand. N Engl J Med. 1996;335:297–303. doi: 10.1056/NEJM199608013350501. [DOI] [PubMed] [Google Scholar]
- 6.Morris M, Pramualratana A, Podhisita C, Wawer MJ. The relational determinants of condom use with commercial sex partners in Thailand. AIDS. 1995;9:507–15. [PubMed] [Google Scholar]
- 7.Meda N, Ndoye I, M'Boup S, Wade A, Ndiaye S, Niang C, et al. Low and stable HIV infection rates in Senegal: natural course of the epidemic or evidence for success of prevention? AIDS. 1999;13:1397–405. doi: 10.1097/00002030-199907300-00018. [DOI] [PubMed] [Google Scholar]
- 8.Kaul R, Kimani J, Nagelkerke NJ, Fonck K, Ngugi EN, Keli F, et al. Monthly antibiotic chemoprophylaxis and incidence of sexually transmitted infections and HIV-1 infection in Kenyan sex workers: a randomized controlled trial. JAMA. 2004;291:2555–62. doi: 10.1001/jama.291.21.2555. [DOI] [PubMed] [Google Scholar]
- 9.Levine WC, Revollo R, Kaune V, Vega J, Tinajeros F, Garnica M, et al. Decline in sexually transmitted disease prevalence in female Bolivian sex workers: impact of an HIV prevention project. AIDS. 1998;12:1899–906. doi: 10.1097/00002030-199814000-00022. [DOI] [PubMed] [Google Scholar]
- 10.Ghys PD, Jenkins C, Pisani E. HIV surveillance among female sex workers. AIDS. 2001;15(Suppl 3):S33–40. doi: 10.1097/00002030-200104003-00005. [DOI] [PubMed] [Google Scholar]
- 11.Kerrigan D, Ellen JM, Moreno L, Rosario S, Katz J, Celentano DD, et al. Environmental-structural factors significantly associated with consistent condom use among female sex workers in the Dominican Republic. AIDS. 2003;17:415–23. doi: 10.1097/00002030-200302140-00016. [DOI] [PubMed] [Google Scholar]
- 12.Kerrigan D, Moreno L, Rosario S, Gomez B, Jerez H, Barrington C, et al. Environmental-structural interventions to reduce HIV/STI risk among female sex workers in the Dominican Republic. Am J Public Health. 2006;96:120–5. doi: 10.2105/AJPH.2004.042200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Albert AE, Warner DL, Hatcher RA. Facilitating condom use with clients during commercial sex in Nevada's legal brothels. Am J Public Health. 1998;88:643–6. doi: 10.2105/ajph.88.4.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Albert AE, Warner DL, Hatcher RA, Trussell J, Bennett C. Condom use among female commercial sex workers in Nevada's legal brothels. Am J Public Health. 1995;85:1514–20. doi: 10.2105/ajph.85.11.1514. 1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Nevada Administrative Code. 441A.800. Testing of prostitutes; prohibition of certain persons from employment as prostitute.
- 16.Brents BG, Hausbeck K. Violence and legalized brothel prostitution in Nevada: examining safety, risk, and prostitution policy. J Interpers Violence. 2005;20:270–95. doi: 10.1177/0886260504270333. [DOI] [PubMed] [Google Scholar]
- 17.Brents BG, Hausbeck K. State-sanctioned sex: negotiating formal and informal regulatory practices in Nevada brothels. Sociol Perspect. 2001;44:307–32. [Google Scholar]
- 18.Brants C. The fine art of regulated tolerance: prostitution in Amsterdam. J Law Soc. 1998;25:621–35. [Google Scholar]
- 19.Carrier JM. Mexican male bisexuality. J Homosex. 1985;11:75–85. doi: 10.1300/J082v11n01_07. [DOI] [PubMed] [Google Scholar]
- 20.Uribe-Zúñiga P, Hernández-Tepichín G, del Río-Chiriboga C, Ortiz V. [Prostitution and AIDS in the city of Mexico] Salud Publica Mex. 1995;37:592–601. [PubMed] [Google Scholar]
- 21.del Rio C, Sepúlveda J. AIDS in Mexico: lessons learned and implications for developing countries. AIDS. 2002;16:1445–57. doi: 10.1097/00002030-200207260-00001. [DOI] [PubMed] [Google Scholar]
- 22.Strathdee SA, Magis-Rodríguez C. Mexico's evolving HIV epidemic. JAMA. 2008;300:571–3. doi: 10.1001/jama.300.5.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bucardo J, Semple SJ, Fraga-Vallejo M, Davila W, Patterson TL. A qualitative exploration of female sex work in Tijuana, Mexico. Arch Sex Behav. 2004;33:343–51. doi: 10.1023/B:ASEB.0000028887.96873.f3. [DOI] [PubMed] [Google Scholar]
- 24.Brouwer KC, Case P, Ramos R, Magis-Rodríguez C, Bucardo J, Patterson TL, et al. Trends in production, trafficking, and consumption of methamphetamine and cocaine in Mexico. Subst Use Misuse. 2006;41:707–27. doi: 10.1080/10826080500411478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Strathdee SA, Fraga WD, Case P, Firestone M, Brouwer KC, Perez SG, et al. “Vivo para consumirla y la consumo para vivir” [“I live to inject and inject to live”]: high-risk injection behaviors in Tijuana, Mexico. J Urban Health. 2005;82(3 Suppl 4):iv58–73. doi: 10.1093/jurban/jti108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patterson TL, Semple SJ, Staines H, Lozada R, Orozovich P, Bucardo J, et al. Prevalence and correlates of HIV infection among female sex workers in 2 Mexico-US border cities. J Infect Dis. 2008;197:728–32. doi: 10.1086/527379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Strathdee SA, Philbin MM, Semple SJ, Pu M, Orozovich P, Martinez G, et al. Correlates of injection drug use among female sex workers in two Mexico-U.S border cities. Drug Alcohol Depend. 2008;92:132–40. doi: 10.1016/j.drugalcdep.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Secretaría de Salud. Norma oficial Mexicana NOM-039-SSA2-2002, para la prevención y control de las infecciones de transmisión sexual [Mexican federal guidelines for the treatment of STIs—2002] [cited 2010 Feb 3]. Available from: URL: http://www.salud.gob.mx/unidades/cdi/nom/039ssa202.html.
- 29.Patterson TL, Semple SJ, Fraga M, Bucardo J, de la Torre A, Salazar J, et al. Comparison of sexual and drug use behaviors between female sex workers in Tijuana and Ciudad Juarez, Mexico. Subst Use Misuse. 2006;41:1535–49. doi: 10.1080/10826080600847852. [DOI] [PubMed] [Google Scholar]
- 30.Ojeda VD, Strathdee SA, Lozada R, Rusch ML, Fraga M, Orozovich P, et al. Associations between migrant status and sexually transmitted infections among female sex workers in Tijuana, Mexico. Sex Transm Infect. 2009;85:420–6. doi: 10.1136/sti.2008.032979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Department of Transportation (US), Bureau of Transportation Statistics. Border crossing: U.S.-Mexico border crossing data. [cited 2010 Feb 3]. Available from: URL: http://www.bts.gov/programs/international/border_crossing_entry_data/us_mexico/pdf/entire.pdf#search=Border%20crossing%20statistics%20US%20Mexico'.
- 32.Instituto Nacional de Estadística y Geografía (INEGI) Resultados preliminares del XII censo nacional de población y vivienda 2000 [Preliminary results for the XII national population and housing census 2000] [cited 2010 Feb 3]. Available from: URL: http://www.inegi.org.mx/est/contenidos/Proyectos/ccpv/cpv2000/default.aspx.
- 33.Patterson TL, Mausbach B, Lozada R, Staines-Orozco H, Semple SJ, Fraga-Vallejo M, et al. Efficacy of a brief behavioral intervention to promote condom use among female sex workers in Tijuana and Ciudad Juarez, Mexico. Am J Public Health. 2008;98:2051–7. doi: 10.2105/AJPH.2007.130096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Golden MR, Marra CM, Holmes KK. Update on syphilis: resurgence of an old problem. JAMA. 2003;290:1510–4. doi: 10.1001/jama.290.11.1510. [DOI] [PubMed] [Google Scholar]
- 35.Wi T, Ramos ER, Steen R, Esguerra TA, Roces MC, Lim-Quizon MC, et al. STI declines among sex workers and clients following outreach, one time presumptive treatment, and regular screening of sex workers in the Philippines. Sex Transm Infect. 2006;82:386–91. doi: 10.1136/sti.2005.018283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shahmanes M, Patel V, Mabey D, Cowan F. Effectiveness of interventions for the prevention of HIV and other sexually transmitted infections in female sex workers in resource poor setting: a systematic review. Trop Med Int Health. 2008;13:659–79. doi: 10.1111/j.1365-3156.2008.02040.x. [DOI] [PubMed] [Google Scholar]
- 37.Larios SE, Lozada R, Strathdee SA, Semple SJ, Roesch S, Staines H, et al. An exploration of contextual factors that influence HIV risk in female sex workers in Mexico: the Social Ecological Model applied to HIV risk behaviors. AIDS Care. 2009;21:1335–42. doi: 10.1080/09540120902803190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Drumright LN, Colfax GN. HIV risk and prevention for non-injection substance users. In: Mayer KH, Pizer HF, editors. HIV prevention: a comprehensive approach. London: Elsevier/Academic Press; 2009. pp. 340–75. [Google Scholar]
- 39.Lorvick J, Martinez A, Gee L, Kral AH. Sexual and injection risk among women who inject methamphetamine in San Francisco. J Urban Health. 2006;83:497–505. doi: 10.1007/s11524-006-9039-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Holtgrave DR, Crosby RA. Social capital, poverty, and income inequality as predictors of gonorrhoea, syphilis, chlamydia and AIDS case rates in the United States. Sex Transm Infect. 2003;79:62–4. doi: 10.1136/sti.79.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gillespie S, Kadiyala S, Greener R. Is poverty or wealth driving HIV transmission? AIDS. 2007;(21 Suppl 7):S5–16. doi: 10.1097/01.aids.0000300531.74730.72. [DOI] [PubMed] [Google Scholar]
- 42.Putnam R. Social capital: measurement and consequences. Can J Policy Res. 2001;2:41–51. [Google Scholar]
- 43.Weiser SD, Leiter K, Bangsberg DR, Butler LM, Percy-de Korte F, Hlanze Z, et al. Food insufficiency is associated with high-risk sexual behavior among women in Botswana and Swaziland. PLoS Med. 2007;4:1589–97. doi: 10.1371/journal.pmed.0040260. discussion 1598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Strathdee SA, Lozada R, Ojeda VD, Pollini RA, Brouwer KC, Vera A, et al. Differential effects of migration and deportation on HIV infection among male and female injection drug users in Tijuana, Mexico. PLoS One. 2008;3:e2690. doi: 10.1371/journal.pone.0002690. [DOI] [PMC free article] [PubMed] [Google Scholar]